Abstract
Hematological malignancies require intensive and long-term treatment, which brings a significant burden on patients, leading to unmet supportive care needs. The purpose of this review was to investigate the unmet supportive care needs of patients with hematological malignancies during and after active treatment as well as the factors that affect them. A systematic bibliographic search was carried out in the PubMed database for English articles published between 2009 and 2020 according to the Preferred Reporting Items for Systematic Reviews guidelines and under the terms: “unmet needs”, “supportive care”, “hematological malignancy” and “hematological cancer.” Twenty studies were evaluated and reviewed. Hierarchical frequently reported unmet supportive care needs were informational, emotional, physical, daily living/practical (accessibility, transportation, and financial problems), and family life/relational needs. In particular, patients with multiple myeloma most frequently reported unmet needs at the informational, physical, emotional, and daily living/practical domain. Patients with myelodysplastic syndromes reported physical, emotional, practical, and relational needs. Patients with leukemia and lymphoma rated their needs as informational, physical, psychological, daily living, and sexual. Sexual and spiritual unmet needs were reported at a low level. Predictive indicators for increased unmet supportive care needs were the type of the hematological malignancy, younger age, marital status, female gender, monthly income, coexistence of anxiety and depression, and altered quality of life. To conclude with, the literature reports a significant number of unmet supportive care needs in patients with hematological malignancies, whose frequency and intensity were influenced by a variety of factors. However, the large heterogeneity of studies (design, sample, and needs assessment tools) makes the generalization of the results difficult.
Keywords: Hematological cancers, hematological malignancies, supportive care, unmet needs
Introduction
Hematological malignancies are a heterogeneous group of diagnoses, often grouped as Hodgkin versus non-Hodgkin lymphoma, lymphoid versus myeloid leukemia, and acute versus chronic disease.[1,2] They are often aggressive, requiring urgent, prolonged, and demanding treatment. Many hematological cancer patients, particularly those suffering from lymphoma and myeloma, experience psychological distress and poor quality of life throughout their illness trajectory.[3,4,5] Moreover, hematological cancer has an impact on multiple aspects of a person's life, resulting in fatigue; anxiety and depression; spiritual concerns; and social life disruptions, such as limited leisure time, absence of a supportive family environment, transportation and financial issues, and effects on patients' employment.[3] Therefore, they report increased supportive care needs that require high-quality care in the domains of psychosocial, informational, and relational perspective.[6,7] In particular, these patients have high unmet psychosocial and many other supportive care needs. Factors that induce these needs are younger age, female gender, employment, and altered quality of life.[3,7] Understanding their needs is a crucial step to design effective care plans for improving not only their satisfaction but also their quality of life.
The term “supportive care needs” is an umbrella term covering the physical, informational, emotional, practical, social, and spiritual needs of a person affected by cancer.[7] Unmet supportive care needs are those which lack the level of service or support that a patient perceives as necessary to achieve well-being.[8,9] Assessment of unmet supportive care needs can encompass worries across a broad range of domains, reflecting the multidimensional impact of cancer.[8]
In the past, researchers reviewed the supportive care needs[3] and the unmet psychosocial needs[7] in patients with hematological malignancies. The aim of this review was to explore the relevant literature regarding (a) the types of the perceived unmet supportive care needs of patients with hematological malignancies during and after active treatment and (b) the factors (demographical, clinical) that affect the appearance of these needs.
Methods
This systematic review was based on Preferred Reporting Items for Systematic Reviews (PRISMA) guidelines.[10] A search was conducted throughout the PubMed database (June 19, 2020). The inclusion criteria for studies revealed using the following terms: unmet needs, supportive care, haematological malignancy, hematological malignancy, haematological cancer, hematological cancer (unmet needs AND supportive care AND [hematological malignancy OR haematological malignancy OR hematological cancer OR haematological cancer]) were as follows: studies published between 2009 and 2020, in English, in peer-reviewed journals, and restricted only to adults (>18 years of age).
In addition, reference lists of relevant articles were screened. Studies were excluded if they were reviews, guidelines, letters, expert opinions, books, chapters, and studies that included mixed populations with hematological malignancies and solid tumors and solely transplanted patients. All studies were evaluated independently by two co-authors according to the title and summary, while for studies that met the inclusion criteria, a full text was retrieved.
A total of 49 articles were initially identified on the PubMed database, and five articles were identified after further investigation of the reference lists of the selected studies [Figure 1]. First, 29 articles were excluded after screening the titles/abstracts. In particular, two review articles and 27 research articles of nonrelevance to the subject and the inclusion criteria were excluded. From the remaining 25 articles, five were excluded after the full-text assessment[11,12,13,14,15] because of nonrelevance to the end points of the study. Finally, twenty studies that met all the inclusion criteria were included in this review [Table 1].
Figure 1.
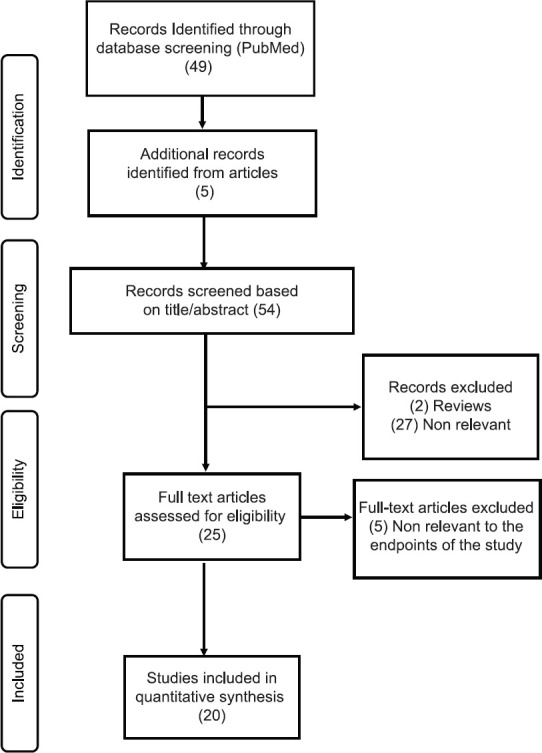
PRISMA flow diagram of literature reviewing process
Table 1.
Reviewed studies in chronological order
| Author (year) Country | Research Question | Methods | Questionnaires-Assessments | Results | Limitations |
|---|---|---|---|---|---|
| Konstantinidis et al (2019) Greece[16] | What are the unmet needs of hematological cancer patients? | Sample size: 102 patients with leukemia, HL, NHL, and MM Sampling: Convenience Design: Cross-sectional Setting: General Hospital |
NEQ | Informational/educational: 47% in total, “more information about my future condition” (44.1%). Social: “support” needs (66.7%). Daily living/practical: “financial” (total: 61.8%), “assistance and treatment needs” (50%) “to have more help with eating, dressing and going to the bathroom” (13.7%). Family-related/relational: 55.9% in total, “to receive less commiseration from other people” (48%), and “to feel more useful within my family” (42.2%). Health system related needs:” communication needs” (46%),” structure related needs” (41%) “better attention from nurses” (18.6%). Spirituality: “to speak with a spiritual advisor” (11.8%), Patients with acute and chronic leukemia expressed more needs than those with other diseases (P=0.037). The less satisfied patients (<8/10) reported more informational needs about their diagnosis and their future condition (P=0.002), about their exams and treatments (P=0.001), communicative (P<0.001), assistance and treatment (P<0.001) and hospital infrastructure (P<0.001). |
Comparisons between the prevalence of needs among patients with different hematological malignancies could not be made in detail because of the small sample size of those subgroups. Generalization should be made by caution since all patients came from the one region of Greece. First use of NEQ in Greek hematological cancer patients |
| Troy et al (2018) USA[17] | What is the patient-reported sources of distress, and its associations with clinical outcomes? | Sample size: 124 MDS patients who contributed a PL only (n=14), or both DT and PL (n=110) Sampling: Convenience Design: Retrospective cohort study Setting: Tertiary care medical left |
NCCN Distress Thermometer (DT) DT ≥4 should be evaluated for referral to specialty services to address unmet needs Problem List (PL) | Most frequently reported categories of problems were: Physical (233 reports), emotional (104 reports), practical (49 reports), and family related (41 reports). Spirituality needs were reported only once during the study. Within each of these categories, the number of problems reported per patient was not strongly associated with DT scores. 89% reported 1,379 problems during 23,613 person-days of follow-up (median=4 problems/patient/visit, range=1-23). The 5 most frequent were fatigue (n=78), pain (n=46), worry (n=45), sleep (n=41), and tingling hands/feet (n=33). The total number of problems reported per patient was significantly correlated with the maximum distress level reported by each patient (P<0.0001). 49% had at least 1 DT ≥4 and 18% had 2 or more DT ≥4. The therapy itself was associated with greater maximum distress (n=75) compared with no therapy (n=35). Treatment with hypomethylating agents (P=0.75) or lenalidomide (P=0.09) was not associated with distress. The use of growth factors was associated with higher distress (n=32) compared with non-use of growth factors (n=78) (P=0.02). Receipt of red blood cells was associated with higher maximum distress (n=54) compared with never receiving packed red cells (n=56) (P=0.03). Patients who received platelets reported higher distress (n=22) compared with patients who did not receive platelets (n=88); this difference approached statistical significance (P=0.06). |
Study design The cohort was not measured from a common baseline DT findings was not validated against other measures |
| Tzelepis et al (2017) Australia[18] | Which are the differences between the unmet needs of rural and urban hematological cancer survivors? | Sample size: 1417 patients (1145 urban, 272 rural) with leukemia, lymphoma, and myeloma Sampling: Recruitment from five Australian state cancer registries Design: Cross-sectional Setting: Outpatient |
SUNS | Physical: Dealing with feeling tired was the most common “high/very high” unmet need for rural (15.2%) and urban (15.5%) survivors. “Coping with having a bad memory or lack of focus” was the second highest “high/very high” unmet need for urban survivors (13.1%) and the third highest for rural survivors (11.8%). Psychological/emotional: Emotional health domain had the highest mean unmet need score for rural and urban survivors (P=0.01). Daily living/practical: “Finding car parking that I can afford at the hospital or clinic” (11.0%) for rural survivors, “Having access to cancer services close to my home” were the second highest high/very high unmet need for rural survivors (14.3%). Family-related/relational: “Dealing with feeling guilty about what I have put others through” (11.1%) for rural survivors. Rurality was associated with a decreased unmet emotional health domain score (P=0.01) whereas travelling for more than 1h to place of treatment was associated with increased unmet financial concerns and unmet access and continuity of care (P<0.0001). Depression, anxiety, and stress were associated with increased unmet need scores for all five domains (P<0.0001). |
Heterogeneous sample of hematological cancer survivors |
| Boucher et al (2018) USA[19] | Which are the changes in the experience of illness (symptoms, needs) in the AML population changes over time? | Sample size: 22 patients with high-risk AML Sampling: Convenience Design: Qualitative, semi-structured interviews, content analysis Setting: Inpatient, University Hospital in New York |
T1-T2: baseline (initiation of treatment)- 3 months after initiation | Four themes were analyzed: physical symptoms, psychological issues, uncertainty regarding prognosis, and patients’ sources of support. Patients reported pain and/or fatigue, most often describing low energy levels, or feeling “weak” or “tired.” Patients reported restrictions in activities as a result of feeling weak or tired. Specific challenges noted by patients included feelings of helplessness/hopelessness, activity restriction, fatigue, fevers, caregiver stress, and lack of clarity regarding treatment decision making. | Small, single-site study, The study also focuses on high-risk patients with aggressive treatment |
| Swash et al (2018) United Kingdom[20] | What are the types of needs that patients had throughout their experiences of diagnosis, treatment and survivorship and how these needs shaped the patients’ experience? | Sample size: 6 NHL patients Sampling: Convenience Design: Qualitative, in-depth interpretative phenomenological approach, 3 small focus groups Setting: Hospital in the North West of England |
The themes that emerged were concerns for family, information needs and the need for psychological support. Other more specific areas of psychological needs were fear of recurrence, maintaining hope, coping, and struggling with emotions (guilt and anger). Participants reported feeling different to other cancer patients. Lack of understanding of their diagnosis by friends and family and lack of access to relevant support services are notable unmet needs that differ from previous findings. Feeling supported was important to all, and where there was no support the consequent unmet need was felt strongly |
Small sample Single left |
|
| Monterosso et al (2018) Australia[21] | What are the unmet informational, psychological, emotional, social, practical, and physical needs and preferences for posttreatment survivorship care of individuals living with MM? | Sample size: 14 patients (6 to 49 months postdiagnosis) Sampling: Participants were identified through the hospital cancer registry patient records Design: Qualitative and descriptive design with 2 focus groups and thematic analysis Setting: Tertiary hospital in Western Australia |
Seven categories of needs were revealed : informational, health-system related (experience with health-care professionals), physical (coping with side effects: hair loss, fatigue, peripheral neuropathy) , psychological ( dealing with emotions , hope and positivity, living with the chronicity of myeloma) , support needs (peer support, need for a link person), relational (communicating with family and friends, relationship with children). Treatment side effects were described as one of the worst aspects of the experience, with many people reporting feeling unprepared to recognize or cope with them. Participants in this study described unmet needs across a breadth of domains that varied over time. | Small sample size Single site recruitment Self-selection of participants | |
| Oberoi et al (2017) Australia[22] | Which is the course of anxiety, depression and unmet needs in DLBCL and MM survivors in the first 2 years post diagnosis? | Sample size: 236 DLBCL and 178 MM survivors Sampling: Recruitment from the population-based Victorian Cancer Registry. Design: Longitudinal study Setting: Outpatient |
HADS SCNS-SF34 T1-T2: Approximately 7- and 15-months post diagnosis | Changes in unmet needs was generally similar for the two groups, except for moderate to high psychological needs (P<0.05). For both groups, unmet needs in the psychological, physical and daily living domains were most common at T1. Analyses for each need’s domain showed an effect of time for psychological needs (P=0.02) and information needs (P=0.03), but not for sexuality, physical and daily living and patient care needs. There was no significant effect of cancer type on any need’s domains. At T1 and T2, psychological, physical and daily living domains were still the main areas of need. Time affected the psychological (P=0.00), physical, daily living (P=0.02) and information needs (P=0.03). Cancer type affected psychological needs (P=0.02) and information needs survivors reporting “moderate to high” needs. A significant interaction between time and cancer type was found only for psychological needs domain (P=0.03). In the MM group, receiving chemotherapy before T1 was associated with higher moderate to high psychological needs at T1. | A relatively low response rate at T1. Low representation of patients in the 65 to 85-year age groups in the DLBCL group and in the 75 to 85-year age group in MM patients may affect the generalizability of the findings to the larger population of MM and DLBCL survivors. |
| Oberoi et al (2017) Australia[23] | What is the influence of anxiety, depression and unmet supportive care needs on QoL in MM and DLBCL patients? | Sample size: 414 patients with MM and DLBCL Sampling: Recruitment from the population-based Victorian Cancer Registry. Design: Longitudinal study Setting: Outpatient |
FACT-G HADS SCNS-SF34 T1-T2: 8 months apart |
Informational/educational: 24% of respondents reported at least one “moderate-to-high” informational need. Physical: 30% of respondents reported at least one “moderate-to-high” unmet need at the physical and daily living needs domain. Psychological/emotional: 30% of respondents reported at least one “moderate-to-high” unmet need in the psychological and emotional needs domain. Daily living/practical: 30% of respondents reported at least one “moderate-to-high” unmet need in the daily living needs domain. 11% reporting a patient care need. Sexuality: 8.5% reporting at least one sexuality need. At T1, 15% of participants had elevated anxiety and 18% had elevated depression scores. While most unmet needs domains had “weak-to-moderate” correlations with anxiety and depression, T1 physical needs were strongly correlated with T1 depression (r=0.51). Except physical well- being, all other QoL subscales and overall QoL were significantly associated with T1 anxiety (P=0.000, P=0.001). All QoL subscales and overall QoL were significantly associated with T1 depression (P=0.000, P=0.001. Only patient care needs were associated with physical (P=0.040) and social well-being (P=0.003) and overall QoL (P=0.020). |
Use of a general measure for QoL rather than a measure specific to hematological patients Low response rate |
| Oberoi et al (2017) Australia[24] | Which are the patient-reported unmet needs and anxiety and depression for survivors of DLBCL and MM? | Sample size: 414 patients with MM and DLBCL Sampling: Recruitment from the population-based Victorian Cancer Registry Design: Longitudinal study Setting: Outpatient |
HADS SCNS-SF34 T1-T2: 8 months apart |
Informational/educational: 24% of participants reported at least one “moderate to high unmet need” (T1) and 14% information needs at T2. Physical: 30% of participants reported at least one “moderate to high unmet need” (T1) and 23% at T2. Psychological/emotional: 30% of participants reported at least one “moderate to high unmet need” (T1)) and 23% at T2. Daily living/practical: 30% of participants reported at least one “moderate to high unmet need” (T1) and 23% at T2, 11% “patient care needs” (T1) and 8% at T2. Sexuality: 9% of participants reported at least one “moderate to high unmet need” (T1) and 8% at T2. The most common “moderate to high” unmet supportive care needs at T1 “Not being able to do the things you used to do “(21.8%) (physical domain) and at T2 “ Concerns about the worries of those close to you” (13.5%) (psychological domain).T1 psychological needs were associated with T1 information needs (r=0.54) and physical and daily living needs (r=0.56). T2 anxiety was associated with T1 anxiety (OR 4.75, 95% CI 1.86-11.09), T2 psychological needs (OR 1.68, 95% CI1.34-2.11) and with T1 social problems (OR2.33,95% CI 1.03-5.05) in multivariate analysis. T2 depression was associated with both T1 (OR 1.28, 95% CI 1.06-1.57) and T2 psychological needs (OR 1.35, 95% CI 1.06-1.70), T2 physical needs (OR 1.89, 95% CI 1.27-2.81) and T1 depression (OR 4.52, 95% CI 1.88-10.86). |
Not able to adjust for the impact of response to treatment on outcomes The interval between the two assessments was long Low response rate |
| Monterosso et al (2017) Australia[25] | What are the post-treatment experiences and preferences for follow-up support of lymphoma survivors? | Sample size: 17 patients (NHL: 16, HL: 1) Sampling: Participants were identified through the hospital cancer registry patient records\ Design: Qualitative and descriptive design with 2 focus groups and thematic analysis Setting: Tertiary hospital with a comprehensive cancer left in Western Australia |
Five key themes were revealed: information; loss and uncertainty; family, support, and post-treatment experience; transition, connectivity and normalcy, and person-centered post treatment care. Survivors described a sense of loss as they transitioned away from regular interaction with the hospital at the end of treatment, but also talked about the need to find a “new normal”. Establishing post-treatment support structures that can provide individualized information, support, reassurance and referrals to community and peer support were identified as a helpful way to navigate the transition from patient to post-treatment survivor. | Small sample size Single site recruitment Self-selection of participants The use of a clinical psychologist as the facilitator for the focus groups |
|
| Yu et al (2017) China[26] | Which are the unmet supportive care needs, with concomitant influencing factors, in adult acute leukemia patients in China? | Sample size: 311 patients with acute leukemia Sampling: Convenience Design: Cross-sectional Setting: 5 medical centers in Xian, China |
SCNS-SF34 | Informational: Health information dimension scored the highest rate of 55%. “Being informed about your test results as soon as possible”, “Being informed about things you can do to help yourself to get well” and “Being informed about cancer which is under control or in remission” were the three highest scoring entries. Psychological: The psychological needs dimension scored the second highest unmet needs, scoring 35 (IQR: 32.50). Physical and daily living needs scored 25 (IQR: 35.00) and 25 (IQR: 40.00), respectively. Sexuality: Sexual need scored the lowest rate of 0.00 (IQR: 24.99). Age (P<0.005) and “whether the treatment was the initial one or not” (P<0.005) influenced sexual need dimension. KPS score (P<0.001) and income (P<0.05) were the common factors influencing the rest of the three dimensions with treatment stage adding to two of them except “physiological and daily living needs” dimension. The dimensions of “psychological needs” and “care and support needs” were associated with “monthly average income” (P<0.001) KPS score”(P<0.01) and “treatment stage” (P<0.01) factors, whereas the “marital status” (P<0.01), “KPS score” (P<0.05) and “treatment stage” (P<0.001) were the significant variables for the dimension of “health information need”. |
|
| Kim et al (2016) South Korea[27] | Which are the unmet needs of NHL survivors in Korea and their associations with HRQoL? | Sample size: 826 NHL survivors Sampling: Survivors identified from electronic medical records of the hospitals Design: Cross-sectional Setting: 3 university hospitals in South Korea |
Need Scale for Cancer Patients Undergoing Follow-up Care (NS-C) developed in Korea EORTC QLQ-C30 | Informational/educational: Most frequently reported unmet needs were “being informed about prevention of recurrence” (50.7%), “being informed about prevention of metastasis” (49.7%). Psychological/emotional: The third most frequently reported need was “having self-confidence of overcoming cancer” (42.7%). Among six domains, unmet need prevalence ranged from 1.7% to 38.3%. Most commonly reported domains with unmet needs were “treatment and prognosis” (38.3%) and “keeping mind under control” (30.5%). Multivariate logistic analyses revealed that younger age (domain: Diet and exercise P=0.002), being unmarried (domain: Relationship with health professionals P=0.013, Keeping mind under control P=0.025), and low monthly income (domain: Diet and exercise P=0.003, Support P=0.008) were associated with unmet needs of multiple domains. Participants with unmet needs demonstrated significantly poorer HRQOL, and the most clinically meaningful differences were found in social function (P<0.001) and emotional function (P<0.001). |
Study design Low response rate Selection bias Not consider potential psychosocial predictors |
| Boyes et al (2015) Australia[28] | Which is the prevalence and which are the correlates of the unmet supportive care needs of patients with hematological malignancy? | Sample size: 311 patients Sampling: Convenience Design: Cross-sectional Setting: Outpatient hematology clinics at three comprehensive cancer treatment centers in Australia |
SCNS-SF34 | Psychological/emotional: Most commonly reported (35%; 95% CI 30-41%). The third most common “moderate to high “unmet need was “uncertainty about the future” (21%; 95% CI 16-25%). Daily living/practical: Most commonly reported in physical aspects of daily living (35%; 95% CI 30-41%) domains. The second “moderate to high “unmet need was “not being able to do the things you used to do” (21%; 95% CI 17-26%). Physical: Highest “moderate to high “unmet need for lack of energy/tiredness (24%; 95% CI 20-30%). 51% of participants reported having at least one “moderate to high” level unmet need, while 25% reported “no need” for help with any items. Females, aged <55 years, not in the labour force, had higher odds of reporting “moderate to high” level unmet supportive care needs. |
Sample characteristics SCNS-SF34 is not a specific tool for hematological cancer patients |
| Hall et al (2015) Australia[29] | Which are the most prevalent unmet needs of hematological cancer survivors? | Sample size:
715 survivors Sampling: Australian state-based cancer registries Design: Cross-sectional Setting: Outpatient |
SUNS | Psychological/emotional: “Dealing with feeling tired” (17%), was the most frequently endorsed “high/very high” unmet need. “Coping with having a bad memory or lack of focus” was the second (14%) and “Dealing with feeling worried (anxious)” was the third. Following were: “Dealing with feeling stressed “(12%),” Dealing with not feeling able to set future goals or make long-term plans “(12%) and “Dealing with being told I had cancer” (12%). Daily living/practical (financial problems): “Finding car parking that I can afford at the hospital or clinic “(12%). Family-related/relational: “Finding someone to talk to who understands and has been through a similar experience” (13%) and “Dealing with people who expect me to be “back to normal” (12%). Higher levels of psychological distress (e.g., anxiety, depression and stress) and indicators of financial burden as a result of cancer (e.g., having used up savings and trouble meeting day-to-day expenses due to cancer) were consistently identified as characteristics associated with the three most prevalent “high/very high” unmet needs. |
Sample was not representative of the entire population of hematological cancer survivors, with non-participants and participants differing with regard to age at diagnosis and cancer type Low response rate |
| Hall et al (2014) Australia[30] | Which are the subgroups of hematological cancer survivors who report “high/very high” level of unmet need on multiple (≥7) items of supportive care? | Sample size: 696 survivors Sampling: Australian state-based cancer registries Design: Cross-sectional Setting: Outpatient | SUNS DASS-21 | 25% reported a “high/very high” level of unmet need on seven or more items of the SUNS. Survivors who: had relocated due to their cancer (OR: 2.04; 95% CI: 1.18, 3.52), had difficulty paying bills (OR: 2.42; 95% CI: 1.34, 4.38), had used up their savings as a result of cancer (OR: 1.90;95% CI: 1.06, 3.40), and were classified as having above normal symptoms of depression (OR: 3.65; 95% CI: 2.17, 6.15) and stress (OR: 5.94; 95% CI: 3.22, 10.95) on DASS-21 had statistically significantly higher odds of reporting seven or more “high/very high” unmet needs. | Low response rate No clinically standardized cut-off point for use with the SUNS to help determine which cancer survivors would benefit most from additional intervention |
| Hall et al (2013) Australia[31] | What are the differences between the unmet needs of Australian and Canadian hematological cancer survivors? | Sample size: 207 Australian & 127 Canadian survivors Sampling: Australian sample: data from a sub-sample of respondents participating in a larger, national study Canadian sample: all hematological cancer survivors who participated in the Canadian Survivors Unmet Needs study Design: Cross-sectional Setting: Outpatient |
SUNS | Psychological/emotional: “Dealing with feeling tired” was identified as the highest concern by survivors. Country (P=0.045) was associated with survivors reporting a “high/very high” unmet need with “worry about earning money” with Australians reporting marginally non significantly higher odds than Canadians (OR 2.1; 95% CI; 0.99, 4.3). Country was not significantly associated with any other outcome. Australians reported a higher level of “financial concerns” (P<0.049) and “relationships” (P<0.024) unmet needs compared with Canadians. Having additional financial burden in the previous month due to cancer treatment, younger age at diagnosis, female sex, vocational or other level of education, and consulting a health care professional for cancer treatment or concerns about cancer in the last month were factors associated with multiple areas of unmet needs. Australian and Canadian hematological cancer survivors were found to experience similar levels of unmet needs. |
Low response rate Low consent rate Distribution of the residuals from the final linear regression models was slightly to moderately skewed, with some heteroscedasticity Eligibility criteria for the countries’ participants |
| Zimmerman et al (2013) Canada[32] | What are the symptoms and referral rates to specialized palliative care and psychosocial oncology services of patients with acute leukemia? | Sample size: 249 patients with acute leukemia Sampling: Convenience Design: Cross-sectional Setting: University Cancer Centre |
MSAS | Physical: Patients reported a median of 9 physical symptoms. The most common were lack of energy (79%), drowsiness (56%), dry mouth (54%), weight loss (54%) and pain (49%). Physical symptoms were associated with poorer functional status (P<0.0001). Psychological/emotional: Patients reported a median of 2 psychological symptoms. The most prevalent psychological symptoms were difficulty sleeping (55%), worrying (43%), difficulty concentrating (39%), and feeling sad (36%). Psychological symptoms were associated with past psychiatric history (P=0.007) and acute lymphocytic leukemia (ALL) (P=0.013). Patients with intense lack of energy, difficulty sleeping, and pain were more likely to report intense worrying/sadness (P<0.001). No patients with moderate-severe pain were referred for specialized symptom control and only 13% of those with severe worrying/sadness were referred to psychiatry/psychology within one month of the assessment. |
Study design Eligibility criteria of the participants |
| Parry et al (2012) USA[33] | Which are the Unmet Service Needs in Adult Leukemia and Lymphoma Survivors After Treatment? | Sample size: 477 leukemia and lymphoma survivors Sampling: Recruitment from Colorado Central Cancer Registry Design: Cross-sectional Setting: Outpatient |
The Houts et al. service need inventory | Sexuality: Sexual Issues (41%) were the highest unmet needs. Daily living/practical: The second most prevalent unmet need was “handling medical and living expenses” (38%), employment (32%), and health insurance (30%). Psychological/emotional: Emotional difficulties (37%) were the third most prevalent unmet needs. Women were more likely to report unmet childcare needs than men (P=0.004); younger individuals were more likely to report needing help with emotional difficulties and family problems (P=0.000). Family-related/relational: Individuals who had experienced a recurrence reported more unmet needs on family problems (P=0.027) than patients who had not experienced recurrence. Lower income was related to greater unmet need regarding medical and living expenses (P=0.000). Relationships were also observed among the service needs, suggesting overlapping areas of unmet need. |
Study design Under-representation in the sample of individuals experiencing socioeconomic disadvantage and multiple comorbidities |
| Molassiotis et al (2011) United Kingdom[34] | Which are the unmet needs and QOL of patients with MM and their partners? | Sample size: 132 patients with MM Sampling: Convenience Design: Cross-sectional Setting: Specialist referral left in the United Kingdom and three district general hospitals |
CaSUN HADS EORTC QLQ-C30 EORTC QLQ-MY20 |
Psychological/emotional: About 27.4% of patients reported signs of anxiety and 25.2% reported signs of depression. Anxious/depressed patients had more than double unmet needs than non-anxious/depressed patients (P<0.05). About 40.8% were worried about their health in the future. Physical: QOL was moderate, with key areas of impairment being physical, emotional, social and cognitive functioning, and patients complained of several symptoms, including tiredness (40.7%), pain (35.9%), insomnia (32.3%), peripheral neuropathies (28.3%) and memory problems (22.3%). The presence of “side effects of treatment” (EORTC MY20 module subscale) was the single most important variable in predicting unmet supportive care patients’ needs, explaining 25% of the total variance in the “unmet patient needs” item (P<0.001). Daily living/practical: 1/4 of the patients reported unmet supportive care needs. The most common needs were related to accessibility of hospital car parking, obtaining life and/or travel insurance, and managing their concerns about myeloma coming back. |
Low response rate The CaSUN is tested in patients free of disease Sample characteristics |
| Lobb et al (2009) Australia[35] | Which are the informational, emotional and support needs of patients with hematological malignancy at the completion of? treatment? | Sample size: 66 survivors Sampling: Convenience Design: Cross-sectional Setting: Hematological departments from two hospitals |
CaSUN | The most frequently endorsed unmet needs included managing the fear of recurrence (73%) and health system related (33% the need for a case-manager, 31% the need for communication between doctors) especially the first year after treatment. Predictors of unmet needs included younger patients (P=0.01), marital status (P=0.03) and employment (P=0.03). 59% reported they would have found it helpful to talk with a health-care professional about their experience of diagnosis and treatment at the completion of treatment and endorsed significantly more need in the areas of quality of life (P=0.03), psychological/emotional and relational (P=0.04) needs. Younger patients reported significantly more emotional and relationship needs (P=0.007). | Small sample Study design |
*IQR: interquartile range, HL: Hodgkin's lymphoma, NHL: Non-Hodgkin's lymphoma, MM: Multiple myeloma, MDS: Myelodysplastic syndromes , DLBCL: Diffuse large B- cell lymphoma patients, AML: Acute myeloid leukemia , NCCN: National Comprehensive Cancer Center, QOL: Quality of life, HRQOL: Health related quality of life, NEQ: Needs Evaluation Questionnaire, SUNS: Survivor Unmet Needs Survey, SCNS-SF34: Supportive care needs survey-short form, CaSUN: Cancer Survivors Unmet Needs measure, MSAS: Memorial Symptom Assessment Scale , KPS : Karnofsky performance status, FACT-G: Functional Assessment of Cancer Therapy-General, EORTC QLQ-C30: European organization for research and treatment of cancer-Quality of life, EORTC-QLQ-MY20: European organization for research and treatment of cancer-Quality of life for Multiple Myeloma, HADS: Hospital Anxiety and Depression Scale, DASS-21: Depression Anxiety Stress Scale
Moreover, the final twenty studies were evaluated based on the scientific levels of evidence from the Agency for Healthcare Research and Quality (AHRQ)[36] [Table 2]. In particular, no studies of Levels I and V were identified. Three studies were evaluated at Level II,[22,23,24] 12 studies were evaluated at Level III,[16,18,26,27,28,29,30,31,32,33,34,35] and five studies at Level IV.[17,19,20,21,25]
Table 2.
Description of scientific levels of evidence adapted from AHRQ[36]
| Level of evidence | Description |
|---|---|
| Level I | Randomized controlled trials with adequate follow-up Meta-analysis of multiple randomized control trials |
| Level II | Non-randomized, controlled prospective trial Prospective cohort studies |
| Level III | Well-designed observational studies (e.g., comparative studies, correlation study, case control study) |
| Level IV | Retrospective observational studies without controls |
| Case series | |
| Level V | Expert opinions or committee recommendations |
In this review, we considered the terms of patients and survivors of hematological malignancies identical following the definition of the National Cancer Institute that a cancer survivor “is someone who remains alive and continues to function during and after facing a serious or life-threatening illness. In cancer, a person is considered a survivor from the time of diagnosis to the end of life.”[37]
The unmet supportive care needs were classified in the following nine clinically and empirically driven domains, but also research guided:[6,38,39] informational/educational, physical/cognitive, psychological/emotional, social, daily living/practical (unmet needs for accessibility, transportation, and financial problems), family-related/relational, health system related (communication between health professionals and patients), interpersonal/intimacy needs (unmet needs for sexuality, loss of fertility, and altered body image), and spiritual/religious needs.
Results
Twelve cross-sectional studies,[16,18,26,27,28,29,30,31,32,33,34,35] three prospective studies,[22,23,24] one retrospective study,[17] and four qualitative studies[19,20,21,25] were included. Studies were mainly single centered. There was a heterogeneity in the sample of the studies. Seven studies included patients with all the hematological malignancies (lymphoma, leukemia, and myeloma),[16,18,28,29,30,31,35] three studies included patients with diffuse large B-cell lymphoma and myeloma,[22,23,24] three with acute leukemia,[19,26,32] three with lymphoma,[20,25,27] two with myeloma,[21,34] one study included patients with myelodysplastic syndromes,[17] and one with leukemia and lymphoma.[33]
There were also many questionnaires used for the assessment of the supportive care needs. The most frequently scales used were the Survivor Unmet Needs Survey (SUNS)[40] and the Supportive Care Needs Survey-Short Form (SCNS-SF34).[41] Moreover, a cultural diversity of the samples is observed. There is a mass representation of the Australian population,[21,22,23,24,25,28,29,30,31,35] followed by patients from the USA and Canada.[17,19,32,33] Two studies were conducted in the UK,[20,34] and one study in Greece,[16] China,[26] and Korea.[27]
The main characteristics of the examined articles were authors, country, research question, method (study design, sample, sampling, and setting), questionnaires used and assessments performed, results regarding the unmet supportive care need domains, and limitations [Table 1]. The results obtained from the studies were considered statistically significant at P = 0.05 in the statistical analysis. The studies investigated the following, regarding the unmet supportive care needs of the patients:
Categories of unmet supportive care needs
Hierarchical higher reported unmet supportive care needs were informational/educational, psychological/emotional, physical, daily living/practical needs, and family related.[16,17,20,21,22,23,24,25,26,27,28,29,30,31]
The most frequently reported categories of needs in various studies were informational/educational which ranged from 24% to 55%.[16,18,23,24,26,27] Patients were mostly concerned about obtaining information about their future condition.[16,19,21,25,27,28] At the psychological/emotional health domain, unmet needs were reported at 17%–37% of patients and were correlated with distress, worry, anxiety, and depression.[18,23,24,29,30,31,32,33,34] In the physical needs domain, the most frequently reported symptoms were fatigue,[17,18,19,21,28,29,30,31,34] memory problems,[18,29,30,31,34] pain, sleep disturbances, and tingling hands and feet.[17,21,34] Health system-related needs (care co-ordination, communication between doctors, and the need for a case manager) were present at 32%.[35]
Zimmermann et al.[32] assessed physical and psychological symptoms in patients with acute leukemia that have been dealt with inadequately. The most common physical symptoms were lack of energy, drowsiness, dry mouth, weight loss, and pain. The most prevalent psychological symptoms were sleep disturbances, worry, inability to concentrate, and feeling sad.[32] In Yu et al.'s study,[26] a high number of unmet needs were informational, followed by needs in the psychological domain, regarding patients with acute leukemia. Whereas, Boucher et al.[19] found the following unmet needs in their qualitative study on high-risk leukemia patients: physical, psychological, uncertainty regarding prognosis and support.
Leukemia and lymphoma survivors[33] rated their unmet needs as sexual (41%), daily living/practical (handling medical and living expenses, 38%; employment, 32%; and health insurance, 30%) and having emotional difficulties (37%). Informational (24%), physical (30%), psychological (30%), daily living/practical (30%), and sexuality needs (9%) were also recorded as the most prevalent among lymphoma and myeloma patients.[22,23,24] In addition, psychological, physical, and daily living unmet needs were present for 15 months post diagnosis.[22]
Two qualitative studies interviewed lymphoma patients.[20,25] Common themes emerged from both studies. Informational needs were the most common followed by emotional/psychological, health system related, and family related/relational needs. Kim et al. concluded on the same categories of needs for lymphoma survivors, through a quantitative study.[27]
The most common unmet supportive care needs of multiple myeloma (MM) patients[34] were daily living/practical (accessibility of hospital car parking and obtaining life and/or travel insurance) and managing their disease-related concerns. Nearly 27% of the patients reported signs of anxiety and 25% reported signs of depression. When interviewing MM patients,[21] the unmet needs reported were informational, health system related, physical, psychological, support, and family-life/relational. In addition, patients with myelodysplastic syndromes[17] reported most frequently physical, emotional, practical, and family-related problems.
Low number of unmet sexual needs were reported (3.5%–9%),[23,24,26] except one study,[33] reporting a significant percentage (41%). Similarly, low number (12%)[16] or absence (only one report)[17] of spiritual needs was also reported. Finally, in one study, patients stated that at the first year after treatment, they needed help to manage their fear of recurrence (73%).[35]
Associations with demographic and clinical factors
Factors that induce a high number of unmet needs in multiple domains, across patients with hematological malignancies, included younger patients,[26,27,28,31,33,35] marital status,[26,27,33,35] female gender,[28,31,33] employment-monthly income,[26,27,28,31,33,35] depression, and anxiety.[18,22,23,24,29,30,34] The therapy itself, the use of growth factors, the receipt of red blood cells, and platelets were associated with greater levels of distress.[17] In addition, acute and chronic leukemia patients expressed more unmet needs than those with other hematological malignancies.[16]
Unmet psychological needs were associated with informational, physical, and daily living needs;[22,23,24] past psychiatric history; disease type (acute lymphocytic leukemia,[32] MM[22]); rurality;[18] monthly income; performance status; and treatment stage.[26]
Unmet physical needs were strongly correlated with depression[22,23,34] and poorer functional status,[32] whereas patient care needs were associated with physical and social well-being, overall quality of life,[22,23,24] monthly income, performance status, treatment stage,[26] and treatment side effects in MM patients.[21,22,34]
Unmet financial needs, lack of access, and continuity of care were associated with long traveling to treatment (>1 h).[18] Financial burden as a result of cancer effects (e.g., having exhausted savings and difficulties of dealing with daily expenses due to cancer) was consistently identified as a characteristic associated with the three most prevalent “high/very high” unmet needs (psychological/emotional, daily living, and family/relational).[29,30,31] Survivors who had relocated due to their cancer, had difficulty paying bills, had used up their savings as a result of cancer, were classified as having above-normal symptoms of depression and stress, and had statistically significantly higher odds of reporting seven or more “high/very high” unmet needs.[29,30,31] Health system-related needs (care co-ordination) were linked with younger age, active employment, and being close to treatment completion.[35]
Sexual needs were related with younger age, the stage of treatment, and whether the therapy was initial or not.[26] Informational needs were associated with marital status, performance status, treatment stage,[26] and patient satisfaction.[16] The less satisfied patients reported more informational needs about their diagnosis, future condition, exams, and treatments. They also reported health system-related needs (communicative, assistance, treatment, and hospital infrastructure needs).[16] Individuals who had experienced a recurrence reported more unmet needs related to family than patients who had not experienced recurrence.[33] Participants with unmet needs demonstrated significantly poorer quality of life, especially in social and emotional function.[27] Moreover, unmet supportive care needs seemed to be similar with small differences in survivors of hematological malignancies across different geographical regions.[31]
Discussion
This systematic review analyzed twenty studies evaluating the unmet supportive care needs of patients with hematologic malignancies. The findings demonstrate the variety and the abundance of the unmet supportive care needs of patients affected by hematological malignancies across different aspects of life. Prevalent needs were mainly informational, followed by psychological/emotional and physical needs. In terms of the physical ones, fatigue and memory loss appeared to be the most common.
From the existing research on unmet supportive care needs of hematological cancer patients, younger age was associated with higher risk of reporting supportive care needs.[3] This also applies on the research on patients with solid tumors.[42] Similarly, according to the findings of our review, among other factors, younger age affects many domains of unmet needs.
Culture encompasses ideas, customs, social behavior, attitudes, and characteristics of a particular social group and influences on peoples' cancer beliefs. These beliefs are also affected by other economic, social, and health-related determinants,[43] shaping the report and kind of needs. However, the studies were conducted in different countries (Australia, the USA, Canada, Greece, the UK, China, and Korea), with diverse populations and cultural standards. The report of needs is clearly connected to culture, so, inevitably, some of them may have been overmentioned or underreported. It is obvious that cancer survivors' diverse cultural attributes certainly affect their behavior.[44]
Furthermore, informational needs of cancer patients are high and often not fulfilled. In a study of 4000 German cancer patients, the unmet informational needs were prevalent up to 48%. Patients who were less satisfied with the receiving information, reported higher levels of unmet needs, anxiety, depression, and lower level of quality of life.[45] Specifically, in patients with hematological malignancy, the perceived informational needs were moderate to high, up to 70%.[46] Almost all the reviewed studies have shown unmet informational needs up to 55%. The high percentage of informational unmet needs found in these studies should be under health-care professionals' consideration in order to fulfill them.
Unmet spiritual needs were reported only in two studies,[16,17] but with low prevalence. Evidently, spirituality correlates to both culture and religion. It seems that all the three domains influence patients' perceptions of health and illness.[47] In fact, spiritual needs are common to several national, religious, and linguistic populations of cancer patients, but may differ on their cultural background. The impact of culture and religion on spiritual needs and expectations regarding cancer care is very complex. Health-care professionals need to evaluate each patient individually, considering that patients' preferences and reports may be influenced by religion, culture, or ethnicity.[48]
In addition, the unmet sexuality needs were reported with low prevalence[23,24,26] unlike the study of Parry et al.,[33] in which patients reported sexual needs at 41%. In this particular study, the researchers used “The Houts et al. service need inventory”[49] that includes only one item regarding sexuality: “Sexual issues (e.g.: sexual interest, activity, and satisfaction).” A general question like this can lead to invalid responses, whereas multiple and more specific questions may lead to more accurate answers. Other researchers[23,24,26] used the SCNS-SF34 that includes the following sex-related entries: change in sexual feeling, change in sexual relationship, and knowledge about sexual relationship. Moreover, in the study by Yu et al.,[26] conducted in China, both young age and stage of treatment significantly affected the sexual needs domain. This might be explained by the complex psychological status of a young adult facing a life-threatening disease. Earlier studies[50,51] among young adults treated for non-Hodgkin lymphoma, reported higher levels of sexuality and/or fertility needs. In the reviewed studies, the type of hematological malignancy was not associated with unmet sexuality needs.
Regarding the type of hematological malignancy and the reported unmet supportive care needs, we found some discordances between studies especially for acute leukemia. The studies by Zimmermann et al.[32] and Yu et al.[26] examined patients with acute leukemia. The first study concluded that unfulfilled physical needs precede psychological needs, whereas the second concluded that unfulfilled information needs precede psychological needs. However, these studies used different instruments to assess the patients' needs. Zimmermann et al.[32] used the Memorial Symptom Assessment Scale which solely states a number of symptoms, whereas Yu et al.[26] used a tool specific for supportive care needs of people with cancer, the SCNS-SF34. Hence, a tool like this is conceptually more appropriate for the needs' assessment. Moreover, the qualitative findings obtained, derived from a single study,[19] included only high-risk acute leukemia patients (complex karyotype, over 60 years old, or had a secondary leukemia). These patients underwent more aggressive treatment, which might be the reason why they put the physical needs first and then the psychological ones.
Limitations of this review are the strict criteria used for the selection of studies, the heterogeneity of the studies regarding the study design, the sample and the measurement tools, and the relatively small sample of most studies, with the possibility of nonsignificant results due to a lack of statistical power (Type II error). The included studies in this review may be biased because unpublished studies have not been identified (publication bias). A number of methodological problems limit the applicability of the available research, which needs to be addressed.
On the other hand, we used the PRISMA[10] guidelines to conduct the review and evaluated the studies based on acknowledged scientific criteria (AHRQ).[36] Moreover, this article is the first systematic review of the literature of the last decade that focuses on the unmet supportive care needs of patients with hematological malignancies.
Conclusions
Overall, this systematic review identifies some relatively similar areas of perceived unmet supportive care needs of patients with hematological malignancies. Unmet informational needs are at the top of the list, followed by psychological/emotional and physical needs. Nevertheless, the wide variation in study methodologies, sample characteristics, and needs assessment measures used in the reviewed studies, made the synthesis, analysis, and generalization οf the results difficult.
Future studies on the field of unmet supportive care needs should focus on specific types of hematological malignancies and patients with advanced disease. Research must also focus on needs such as sexual, psychological, and spiritual that are not well recognized and managed by health-care professionals. It is of note that there is a significant discordance between physician and patient perspectives of unmet needs.[52] This review could also guide health-care professionals to more easily recognize high-risk patients to report unmet supportive care needs. A clear understanding of the specific issues that are more important to this group of patients, through systematic assessment, will help to identify their most relevant concerns during treatment and design appropriate interventions in order to offer more individualized, high-quality care and subsequent patient satisfaction. The continuous investigation of the changing needs of this specific group of patients will contribute to their successful coverage.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sant M, Allemani C, Tereanu C, De Angelis R, Capocaccia R, Visser O, et al. Incidence of hematologic malignancies in Europe by morphologic subtype: Results of the HAEMACARE project. Blood. 2010;116:3724–34. doi: 10.1182/blood-2010-05-282632. [DOI] [PubMed] [Google Scholar]
- 2.Campo E, Swerdlow SH, Harris NL, Pileri S, Stein H, Jaffe ES. The 2008 WHO classification of lymphoid neoplasms and beyond: Devolving concepts and practical applications. Blood. 2011;117:5019–32. doi: 10.1182/blood-2011-01-293050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hall A, Lynagh M, Bryant J, Sanson-Fisher R. Supportive care needs of hematological cancer survivors: A critical review of the literature. Crit Rev Oncol Hematol. 2013;88:102–16. doi: 10.1016/j.critrevonc.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 4.Allart-Vorelli P, Porro B, Baguet F, Michel A, Cousson-Gélie F. Haematological cancer and quality of life: A systematic literature review. Blood Cancer J. 2015;5:e305. doi: 10.1038/bcj.2015.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Allart P, Soubeyran P, Cousson-Gélie F. Are psychosocial factors associated with quality of life in patients with haematological cancer.A critical review of the literature? Psychooncology. 2013;22:241–9. doi: 10.1002/pon.3026. [DOI] [PubMed] [Google Scholar]
- 6.Konstantinidis T, Philalithis A. Supportive care needs of advanced cancer patients.The nursing perspective. Arch Hellenic Med. 2014;31:412–22. [Google Scholar]
- 7.Swash B, Hulbert-Williams N, Bramwell R. Unmet psychosocial needs in haematological cancer: A systematic review. Support Care Cancer. 2014;22:1131–41. doi: 10.1007/s00520-014-2123-5. [DOI] [PubMed] [Google Scholar]
- 8.Fitch M. Supportive care for cancer patients. Hosp Q. 2000;3:39–46. doi: 10.12927/hcq..16542. [DOI] [PubMed] [Google Scholar]
- 9.Sanson-Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P. The unmet supportive care needs of patients with cancer.Supportive Care Review Group. Cancer. 2000;88:226–37. doi: 10.1002/(sici)1097-0142(20000101)88:1<226::aid-cncr30>3.3.co;2-g. [DOI] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyzes: The PRISMA statement. Ann Internal Med. 2009;151:264–9. [PMC free article] [PubMed] [Google Scholar]
- 11.Payne JB, Dance KV, Farone M, Phan A, Ho CD, Gutierrez M, et al. Patient and caregiver perceptions of lymphoma care and research opportunities: A qualitative study. Cancer. 2019;125:4096–104. doi: 10.1002/cncr.32401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hochman MJ, Yu Y, Wolf SP, Samsa GP, Kamal AH, LeBlanc TW. Comparing the palliative care needs of patients with hematologic and solid malignancies. J Pain Symptom Manage. 2018;55:82–80. doi: 10.1016/j.jpainsymman.2017.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hudson KE, Wolf SP, Samsa GP, Kamal AH, Abernethy AP, LeBlanc TW. The surprise question and identification of palliative care needs among hospitalized patients with advanced hematologic or solid malignancies. J Palliat Med. 2018;21:789–95. doi: 10.1089/jpm.2017.0509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lowe JR, Yu Y, Wolf S, Samsa G, LeBlanc TW. A cohort study of patient-reported outcomes and healthcare utilization in acute myeloid leukemia patients receiving active cancer therapy in the last six months of life. J Palliat Med. 2018;21:592–7. doi: 10.1089/jpm.2017.0463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paul C, Hall A, Oldmeadow C, Lynagh M, Campbell S, Bradstock K, et al. Dyadic interdependence of psychosocial outcomes among haematological cancer survivors and their support persons. Support Care Cancer. 2017;25:3339–46. doi: 10.1007/s00520-017-3751-3. [DOI] [PubMed] [Google Scholar]
- 16.Konstantinidis TI, Spinthouri M, Ramoutsaki A, Marnelou A, Kritsotakis G, Govina O. Assessment of unmet supportive care needs in haematological cancer survivors. Asian Pac J Cancer Prev. 2019;20:1487–95. doi: 10.31557/APJCP.2019.20.5.1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Troy JD, de Castro CM, Pupa MR, Samsa GP, Abernethy AP, LeBlanc TW. Patient-reported distress in myelodysplastic syndromes and its association with clinical outcomes: A retrospective cohort study. J Natl Compr Canc Netw. 2018;16:267–73. doi: 10.6004/jnccn.2017.7048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tzelepis F, Paul CL, Sanson-Fisher RW, Campbell HS, Bradstock K, Carey ML, et al. Unmet supportive care needs of haematological cancer survivors: Rural versus urban residents. Ann Hematol. 2018;97:1283–92. doi: 10.1007/s00277-018-3285-x. [DOI] [PubMed] [Google Scholar]
- 19.Boucher NA, Johnson KS, LeBlanc TW. Acute leukemia patients' needs: Qualitative findings and opportunities for early palliative care. J Pain Symptom Manage. 2018;55:433–9. doi: 10.1016/j.jpainsymman.2017.09.014. [DOI] [PubMed] [Google Scholar]
- 20.Swash B, Hulbert-Williams N, Bramwell R. 'Haematological cancers, they're a funny bunch: A qualitative study of non-Hodgkin's lymphoma patient experiences of unmet supportive care needs. J Health Psychol. 2018;23:1464–75. doi: 10.1177/1359105316660179. [DOI] [PubMed] [Google Scholar]
- 21.Monterosso L, Taylor K, Platt V, Lobb E, Musiello T, Bulsara C, et al. Living with multiple myeloma: A focus group study of unmet needs and preferences for survivorship care. J Patient Exp. 2018;5:6–15. doi: 10.1177/2374373517715011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oberoi D, White V, Seymour J, Prince HM, Harrison S, Jefford M, et al. The course of anxiety, depression and unmet needs in survivors of diffuse large B cell lymphoma and multiple myeloma in the early survivorship period. J Cancer Surviv. 2017;11:329–38. doi: 10.1007/s11764-016-0591-y. [DOI] [PubMed] [Google Scholar]
- 23.Oberoi DV, White VM, Seymour JF, Prince HM, Harrison S, Jefford M, et al. Distress and unmet needs during treatment and quality of life in early cancer survivorship: A longitudinal study of haematological cancer patients. Eur J Haematol. 2017;99:423–30. doi: 10.1111/ejh.12941. [DOI] [PubMed] [Google Scholar]
- 24.Oberoi D, White VM, Seymour JF, Miles Prince H, Harrison S, Jefford M, et al. The influence of unmet supportive care needs on anxiety and depression during cancer treatment and beyond: A longitudinal study of survivors of haematological cancers. Support Care Cancer. 2017;25:3447–56. doi: 10.1007/s00520-017-3766-9. [DOI] [PubMed] [Google Scholar]
- 25.Monterosso L, Taylor K, Platt V, Lobb E, Krishnasamy M, Musiello T, et al. A qualitative study of the post-treatment experiences and support needs of survivors of lymphoma. Eur J Oncol Nurs. 2017;28:62–8. doi: 10.1016/j.ejon.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 26.Yu FF, Bai YN, He H, Zhu L, Zhang RL, Jiao HX, et al. Identifying the unmet supportive care needs, with concomitant influencing factors, in adult acute leukemia patients in China. Eur J Oncol Nurs. 2017;30:67–74. doi: 10.1016/j.ejon.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 27.Kim SH, Lee S, Kim SH, Ok ON, Kim IR, Choi E, et al. Unmet needs of non-Hodgkin lymphoma survivors in Korea: Prevalence, correlates, and associations with health-related quality of life. Psychooncology. 2017;26:330–6. doi: 10.1002/pon.4136. [DOI] [PubMed] [Google Scholar]
- 28.Boyes AW, Clinton-McHarg T, Waller AE, Steele A, D'Este CA, Sanson-Fisher RW. Prevalence and correlates of the unmet supportive care needs of individuals diagnosed with a haematological malignancy. Acta Oncol. 2015;54:507–14. doi: 10.3109/0284186X.2014.958527. [DOI] [PubMed] [Google Scholar]
- 29.Hall AE, Sanson-Fisher RW, Lynagh MC, Tzelepis F, D'Este C. What do haematological cancer survivors want help with.A cross-sectional investigation of unmet supportive care needs? BMC Res Notes. 2015;8:221. doi: 10.1186/s13104-015-1188-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hall A, D'Este C, Tzelepis F, Lynagh M, Sanson-Fisher R. Factors associated with haematological cancer survivors experiencing a high level of unmet need across multiple items of supportive care: A cross-sectional survey study. Support Care Cancer. 2014;22:2899–909. doi: 10.1007/s00520-014-2264-6. [DOI] [PubMed] [Google Scholar]
- 31.Hall A, Campbell HS, Sanson-Fisher R, Lynagh M, D'Este C, Burkhalter R, et al. Unmet needs of Australian and Canadian haematological cancer survivors: A cross-sectional international comparative study. Psychooncology. 2013;22:2032–8. doi: 10.1002/pon.3247. [DOI] [PubMed] [Google Scholar]
- 32.Zimmermann C, Yuen D, Mischitelle A, Minden MD, Brandwein JM, Schimmer A, et al. Symptom burden and supportive care in patients with acute leukemia. Leuk Res. 2013;37:731–6. doi: 10.1016/j.leukres.2013.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Parry C, Lomax JB, Morningstar EA, Fairclough DL. Identification and correlates of unmet service needs in adult leukemia and lymphoma survivors after treatment. J Oncol Pract. 2012;8:e135–41. doi: 10.1200/JOP.2011.000464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Molassiotis A, Wilson B, Blair S, Howe T, Cavet J. Unmet supportive care needs, psychological well-being and quality of life in patients living with multiple myeloma and their partners. Psychooncology. 2011;20:88–97. doi: 10.1002/pon.1710. [DOI] [PubMed] [Google Scholar]
- 35.Lobb EA, Joske D, Butow P, Kristjanson LJ, Cannell P, Cull G, et al. When the safety net of treatment has been removed: Patients' unmet needs at the completion of treatment for haematological malignancies. Patient Educ Couns. 2009;77:103–8. doi: 10.1016/j.pec.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 36.Shojania KG, Duncan BW, McDonald KM, Wachter RM, Markowitz AJ. Making health care safer: A critical analysis of patient safety practices. Evid Rep Technol Assess (Summ) 2001;43:668. [PMC free article] [PubMed] [Google Scholar]
- 37.National Cancer Institute. National Cancer Institute Dictionary of Cancer Terms. [Last accessed on 2020 Mar 10]. Available from: https://wwwcancergov/search/resultsswKeyword=survivor .
- 38.Kotronoulas G, Papadopoulou C, Burns-Cunningham K, Simpson M, Maguire R. A systematic review of the supportive care needs of people living with and beyond cancer of the colon and/or rectum. Eur J Oncol Nurs. 2017;29:60–70. doi: 10.1016/j.ejon.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 39.Sanson-Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P. The unmet supportive care needs of patients with cancer. Cancer. 2000;88:226–37. doi: 10.1002/(sici)1097-0142(20000101)88:1<226::aid-cncr30>3.3.co;2-g. [DOI] [PubMed] [Google Scholar]
- 40.Campbell HS, Sanson-Fisher R, Turner D, Hayward L, Wang XS, Taylor-Brown J. Psychometric properties of cancer survivors' unmet needs survey. Support Care Cancer. 2011;19:221–30. doi: 10.1007/s00520-009-0806-0. [DOI] [PubMed] [Google Scholar]
- 41.Boyes A, Girgis A, Lecathelinais C. Brief assessment of adult cancer patients' perceived needs: Development and validation of the 34-item Supportive Care Needs Survey (SCNS-SF34) J Eval Clin Pract. 2009;15:602–6. doi: 10.1111/j.1365-2753.2008.01057.x. [DOI] [PubMed] [Google Scholar]
- 42.Miroševič Š, Prins JB, Selič P, Zaletel Kragelj L, Klemenc Ketiš Z. Prevalence and factors associated with unmet needs in post-treatment cancer survivors: A systematic review. Eur J Cancer Care. 2019;28:e13060. doi: 10.1111/ecc.13060. [DOI] [PubMed] [Google Scholar]
- 43.Dein S. Explanatory models of and attitudes towards cancer in different cultures. Lancet Oncol. 2004;5:119–24. doi: 10.1016/S1470-2045(04)01386-5. [DOI] [PubMed] [Google Scholar]
- 44.Guidry JJ, Torrence W, Herbelin S. Closing the divide: Diverse populations and cancer survivorship. Cancer. 2005;104:2577–83. doi: 10.1002/cncr.21251. [DOI] [PubMed] [Google Scholar]
- 45.Faller H, Koch U, Brähler E, Härter M, Keller M, Schulz H, et al. Satisfaction with information and unmet information needs in men and women with cancer. J Cancer Surviv. 2016;10:62–70. doi: 10.1007/s11764-015-0451-1. [DOI] [PubMed] [Google Scholar]
- 46.Rood JA, Van Zuuren FJ, Stam F, Van der Ploeg T, Eeltink C, Verdonck-de Leeuw IM, et al. Perceived need for information among patients with a hematological malignancy: Associations with information satisfaction and treatment decision-making preferences. Hematol Oncol. 2015;33:85–98. doi: 10.1002/hon.2138. [DOI] [PubMed] [Google Scholar]
- 47.Townsend M, Kladder V, Ayele H, Mulligan T. Systematic review of clinical trials examining the effects of religion on health. South Med J. 2002;95:1429–34. [PubMed] [Google Scholar]
- 48.Astrow AB, Kwok G, Sharma RK, Fromer N, Sulmasy DP. Spiritual needs and perception of quality of care and satisfaction with care in hematology/medical oncology patients: A multicultural assessment. J Pain Symptom Manage. 2018;55:56–640. doi: 10.1016/j.jpainsymman.2017.08.009. [DOI] [PubMed] [Google Scholar]
- 49.Houts PS, Yasko JM, Kahn SB, Schelzel GW, Marconi KM. Unmet psychological, social, and economic needs of persons with cancer in Pennsylvania. Cancer. 1986;58:2355–61. doi: 10.1002/1097-0142(19861115)58:10<2355::aid-cncr2820581033>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 50.Hammond CT, Beckjord EB, Arora NK, Bellizzi KM, Jeffrey DD, Aziz NM. Non-Hodgkin's lymphoma survivors' fertility and sexual function-related information needs. Fertil Steril. 2008;90:1256–8. doi: 10.1016/j.fertnstert.2007.08.081. [DOI] [PubMed] [Google Scholar]
- 51.Jonker-Pool G, Hoekstra HJ, van Imhoff GW, Sonneveld DJ, Sleijfer DT, van Driel MF, et al. Male sexuality after cancer treatment--needs for information and support: Testicular cancer compared to malignant lymphoma. Patient Educ Couns. 2004;52:143–50. doi: 10.1016/s0738-3991(03)00025-9. [DOI] [PubMed] [Google Scholar]
- 52.Nair SC, Hassen WA, Sreedharan J, Qawasmeh K, Ibrahim H. Comparison of perceptions of unmet supportive care needs between cancer patients and their oncologists. Support Care Cancer. 2019;27:4229–35. doi: 10.1007/s00520-019-04705-4. [DOI] [PubMed] [Google Scholar]


