Abstract
Babesiosis is a tick-borne disease that shares the Lyme disease tick vector. Prompt microbiological smear examination and a parasitemia index guide further therapy. In severe cases with a parasitemia index >10%, exchange transfusion should be carried out quickly, along with administration of antibiotics, to prevent death and improve patient outcomes. A clinic follow-up should be advocated to check for relapse. Here we present a case of babesiosis requiring exchange transfusion.
Keywords: Babesiosis, exchange transfusion, parasitemia
Babesia infections range from asymptomatic to severe and are sometimes fatal.1 The severity of infection depends on the Babesia species and the immune status of the host.2 Babesiosis is a tick-borne disease that shares the Lyme disease tick vector. Other pathogens transmitted by Ixodes scapularis ticks include Borrelia burgdorferi, Anaplasma phagocytophilum, Borrelia miyamotoi, Borrelia mayonii, Powassan virus, and Ehrlichia muris–like agent. As many as two-thirds of patients with babesiosis experience concurrent Lyme disease, and one-third experience concurrent human granulocytic anaplasmosis.3 B. microti is the predominant species that infects humans in the United States. The incubation period of B. microti infection following a tick bite is typically 1 to 4 weeks. This case highlights the importance of exchange transfusion in severe cases of babesiosis.
CASE DESCRIPTION
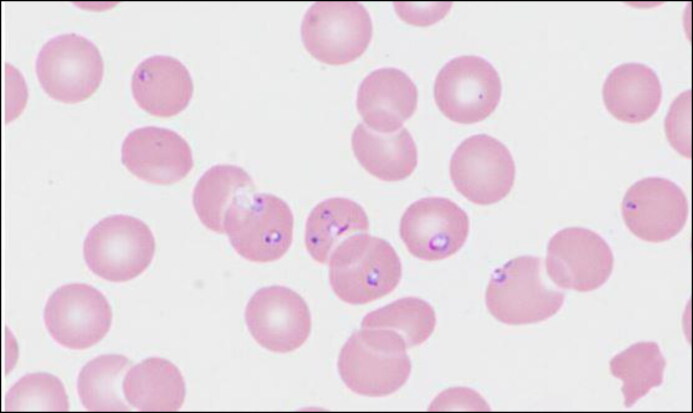
An 81-year-old previously healthy man from upstate New York transferred from an outside hospital with a 5- to 6-day history of fevers, malaise, vague abdominal pain, and worsening confusion. He had not traveled outside of the local area in the previous 6 months. The patient was an avid golfer. He reported no recent tick bites. Blood smear testing (Figure 1) on the day of admission was positive for babesiosis with a parasite index of 13%. DNA polymerase chain reaction sequencing confirmed the species to be B. microti. He was started on oral atovaquone, intravenous azithromycin, and doxycycline in the setting of a high rate of co-infection among Ixodes scapularis ticks for both Borrelia burgdorferi and B. microti. Within the next 3 h, he developed massive hematemesis, respiratory failure, and oliguric renal failure. He was subsequently intubated and transferred to the intensive care unit. Clindamycin was added to the antiparasitic regimen. A repeat blood parasite index level returned at 25% and the patient was urgently started on an exchange transfusion. He was also started on piperacillin-tazobactam therapy for broad coverage in the setting of septic shock and multiorgan dysfunction. Lyme serology returned negative, while Anaplasma serology was not sent. Following 48 h of antiparasitic therapy and exchange transfusion, his parasitemia level dropped to 0.7% (Table 1). He was slowly weaned off vasopressor therapy and extubated in 72 h. His disseminated intravascular coagulation resolved with improved fibrinogen levels, and creatinine levels returned to baseline over a course of 7 days.
Figure 1.
Ring form trophozoites of Babesia spp. observed in the peripheral blood smear using Wright stain.
Table 1.
Serial laboratory values
| Test | Admission | 3 h | 12 h | 48 h | Day 3 | Day 4 | Day 5 |
|---|---|---|---|---|---|---|---|
| Hemoglobin (g/dL) | 10.7 | 8.3 | 4.7 | 5.6 | 7.1 | 7.6 | 9.1 |
| White blood cells (103/μL) | 4.2 | 5.0 | 3.7 | 4.4 | 4.5 | 5.8 | 6.3 |
| Platelets (103/μL) | 34 | 33 | 10 | 40 | 46 | 59 | 64 |
| Creatinine (mg/dL) | 2.21 | 3.2 | 3.45 | 2.41 | 2.14 | 1.75 | 1.5 |
| Parasitemia index (%) | 13 | – | 25 | 1.9 | 0.7 | 0.25 | – |
DISCUSSION
Severe babesiosis often occurs in older and/or immunocompromised patients and is associated with parasitemia >10%.4 Severe babesiosis may also lead to complications, including persistent or relapsing disease. The most common complication is acute respiratory distress syndrome requiring intensive care.5 Shock, intravascular hemolytic anemia, and multiorgan dysfunction are also observed. Exchange transfusion facilitates partial to complete removal of patients’ red blood cells and replacement with allogeneic red blood cells. It is warranted for patients who have high-grade parasitemia >10%, severe hemolysis (hemoglobin <10 g/dL), or organ impairment, particularly pulmonary, liver, and/or renal impairment.6 Early use of exchange transfusion may prevent organ dysfunction and possibly death.7 The preferred antimicrobial regimen for mild to moderate babesiosis consists of oral azithromycin plus atovaquone; as an alternative, oral clindamycin plus quinine can also be used. The preferred treatment of severe babesiosis consists of intravenous azithromycin plus oral atovaquone; intravenous clindamycin plus oral quinine is an alternative option along with exchange transfusion.8
References
- 1.Homer MJ, Aguilar-Delfin I, Telford SR 3rd, Krause PJ, Persing DH.. Babesiosis. Clin Microbiol Rev. 2000;13(3):451–469. doi: 10.1128/cmr.13.3.451-469.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parija SC, Kp D, Venugopal H.. Diagnosis and management of human babesiosis. Trop Parasitol. 2015;5(2):88–93. doi: 10.4103/2229-5070.162489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mareedu N, Schotthoefer AM, Tompkins J, Hall MC, Fritsche TR, Frost HM.. Risk factors for severe infection, hospitalization, and prolonged antimicrobial therapy in patients with babesiosis. Am J Trop Med Hyg. 2017;97(4):1218–1225. doi: 10.4269/ajtmh.17-0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hatcher JC, Greenberg PD, Antique J, Jimenez-Lucho VE.. Severe babesiosis in Long Island: review of 34 cases and their complications. Clin Infect Dis. 2001;32(8):1117–1125. doi: 10.1086/319742. [DOI] [PubMed] [Google Scholar]
- 5.Mylonakis E. When to suspect and how to monitor babesiosis. Am Fam Physician. 2001;63(10):1969–1974. [PubMed] [Google Scholar]
- 6.Sanchez E, Vannier E, Wormser GP, Hu LT.. Diagnosis, treatment, and prevention of Lyme disease, human granulocytic anaplasmosis, and babesiosis: a review. JAMA. 2016;315(16):1767–1777. doi: 10.1001/jama.2016.2884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spaete J, Patrozou E, Rich JD, Sweeney JD.. Red cell exchange transfusion for babesiosis in Rhode Island. J Clin Apher. 2009;24(3):97–105. doi: 10.1002/jca.20197. [DOI] [PubMed] [Google Scholar]
- 8.Vannier E, Krause PJ.. Human babesiosis. N Engl J Med. 2012;366(25):2397–2407. doi: 10.1056/NEJMra1202018. [DOI] [PubMed] [Google Scholar]