Abstract
Objective:
Message framing can be leveraged to motivate adult smokers to quit, but its value for parents in pediatric settings is unknown. Understanding parents’ preferences for smoking cessation messages may help clinicians tailor interventions to increase quitting.
Methods:
We conducted a discrete choice experiment in which parent smokers of pediatric patients rated the relative importance of 26 messages designed to increase smoking cessation treatment. Messages varied on who the message featured (child, parent, family), whether the message was gain- or loss-framed (emphasizing benefits of engaging or costs of failing to engage in treatment), and the specific outcome included (e.g. general health, cancer, respiratory illnesses, financial impact). Participants included 180 parent smokers at 4 pediatric primary care sites. We used latent class analysis of message ratings to identify groups of parents with similar preferences. Multinomial logistic regression described child and parent characteristics associated with group membership.
Results:
We identified 3 groups of parents with similar preferences for messages: Group 1 prioritized the impact of smoking on the child (n=92, 51%), Group 2 favored gain-framed messages (n=63, 35%), and Group 3 preferred messages emphasizing the financial impact of smoking (n=25, 14%). Parents in Group 2 were more likely to have limited health literacy and have a child over age 6 and with asthma, compared to Group 1.
Conclusions:
We identified 3 groups of parent smokers with different message preferences. This work may inform testing of tailored smoking cessation messages to different parent groups, a form of behavioral phenotyping supporting motivational precision medicine.
Keywords: Secondhand smoke (SHS), smoking cessation, behavioral economics, message framing, discrete choice
Introduction
Parents who quit smoking increase their life expectancy by an average of 10 years,1 decrease the risk of their children becoming smokers when they become adults,2 and eliminate the majority of their children’s secondhand smoke (SHS) exposure.3 More than 40% of the US pediatric population is regularly exposed to SHS, most often by a parent or caregiver.3,4 Pediatric clinicians are well-positioned to protect children from SHS exposure by promoting tobacco cessation treatment for parents who smoke5; yet, appropriate treatments to parent smokers are rarely delivered in pediatric settings.6 Pediatric clinicians cite lack of knowledge and training in the best ways to communicate with parents as major barriers to consistently offering treatment.6,7,8 Systematic reviews have demonstrated both individual counselling increases cessation rates9 and brief advice from a physician for adult smokers when they attend clinical services for their health increases quit attempts.10 Trials of interventions for parent smokers attending their child’s health visit, however, do not detect this effect, suggesting new approaches adapted to the unique aspects of a pediatric visit are needed.8
Strategies from behavioral economics may help. Research in behavioral economics suggests the effectiveness of messages for health behavior change differs by whether a message emphasizes the benefits of engaging (a gain-frame) or the costs of failing to engage (a loss-frame) in a targeted health behavior.11,12 In adult healthcare settings, gain-framed messages are more effective than loss-framed in enhancing tobacco cessation efforts.11,12,13 How messages are presented to parent smokers in a pediatric setting, when the parent is the recipient of a health message that potentially benefits both the parent and the child, likely influences parental decisions to engage in treatment.
Limited work has explored tobacco cessation message framing in pediatric healthcare settings.14 Parental smoking cessation interventions have identified successful quitting for parents may be most strongly associated with a parent’s belief that quitting will benefit the child, rather than the parent.15,16 Building upon that finding, initial work identified parent preference for messages that emphasized the impact of smoking on their child as most likely to prompt acceptance of cessation treatment.14 That preference was identified among a series of messages varied upon who was featured (child, parent, or the larger family unit), whether the message was gain or loss framed, and what outcome was included (general health, cancer, respiratory illnesses, child becoming a smoker, or financial impact). A broader understanding of how parent preferences for smoking cessation messages differ may support the tailoring of smoking cessation efforts to different parents, based on observable characteristics. This concept is often termed behavioral phenotyping, reflecting a form of precision medicine in which interventions are not targeted towards individuals with different molecular signatures, as in cancer genomics, but different behavioral signatures.17,18 Rather than apply a one-size-fits-all approach to a behavioral strategy to advance health, pediatric clinicians adjust their messaging and approaches in response to the particular needs or preferences of the patient or parent (i.e., their phenotype).
We sought to phenotype groups of parents sharing preferences for smoking cessation messages, and identify the demographic, clinical characteristics or potential smoking cessation behaviors associated with those groups. Though prior work suggested the child might be most important, we began this study without wanting to limit to one featured group (e.g., the child). Instead, the goal was to leave in a range of preferences and let the responses inform what ought to be prioritized. Thus, we hypothesized that groups of parents with different preferences (i.e. phenotypes) would emerge, with preferences varied based upon who is featured, gain or loss framing, and the outcome emphasized in the message.
Methods
Study Design, Setting and Participants
This latent class analysis was part of a prospective discrete choice experiment with parent smokers to assess the relative impact of a range of framed messages on their intention to start tobacco cessation treatment.14 Parent smokers were recruited through 4 diverse, high-volume outpatient primary care practices from CHOP’s Pediatric Research Consortium (PeRC), a primary care practice-based research network. Inclusion criteria included parents/caregivers (hereafter “parents”) ≥18 years in age, present at their child’s healthcare visit during the study period, able to communicate in English, and a smoker. Potential parent smokers were identified through standard screening for SHS exposure embedded within clinical practice. Parents were approached in the office visit to ascertain interest, obtain consent, and conduct the discrete choice experiment. After completing the experiment, all parents were offered a prescription for nicotine replacement therapy (patch and/or gum) and were provided information for free smoking cessation counseling via the quitline. In total, we recruited 180 parent smokers through the 4 practices from September 2017 to February 2019. Participants were contacted via phone or text at 4 weeks to ascertain any parent, self-reported quit attempts. Parents were given $15 for their participation. The study protocol was approved under expedited review by the institutional review board at CHOP.
Development of Framed Messages
We developed messages using an iterative process, as described previously.14 We used feedback from tobacco control experts and pediatricians combined with input and testing from 30 parent smokers to ensure that the messages were meaningful to the reader and understandable by those with basic health literacy.19,20 This development and testing process led to a final list of 26 messages. Messages were tailored based on 3 dimensions of interest: who the message featured (child, parent, or family), whether the message was gain- or loss-framed, and the specific outcome included (general health, cancer, respiratory illnesses, child becoming a smoker or financial impact) (Table 1).
Table 1:
Message List, Varied by Who Was Featured, Framing, and Outcome Included
| Gain-Framed | Loss-Framed | |
|---|---|---|
| Featured: Child Outcome: General Health | 1. Quitting smoking will improve your child’s health by keeping them away from secondhand smoke. | 14. Continuing to smoke will harm your child’s health by continuing to expose them to secondhand smoke. |
| Featured: Child Outcome: Respiratory Illness | 2. Quitting smoking will improve your child’s health by preventing respiratory illnesses like coughs, colds and wheezing. | 15. Continuing to smoke will harm your child’s health by causing respiratory illnesses like coughs colds, and wheezing. |
| Featured: Child Outcome: Cancer | 3. Quitting smoking will decrease your child’s risk of getting lung cancer and other cancers by keeping them away from secondhand smoke. | 16. Continuing to smoke will increase your child’s risk of getting lung cancer and other cancers by continuing to expose them to secondhand smoke. |
| Featured: Child Outcome: Financial Impact | 4. If you quit smoking, you will save $250 a month by not buying cigarettes. You will gain $250 a month that could be spent on your child. | 17. If you continue to smoke, you will spend $250 a month buying cigarettes. You will lose $250 a month that you could have spent on your child. |
| Featured: Child Outcome: Risk of becoming an adult smoker | 5. If you quit smoking, your child will be less likely to become a smoker. | 18. If you continue to smoke, your child will be more likely to become a smoker. |
| Featured: Parent Outcome: General Health | 6. Quitting smoking will improve your health. | 19. Continuing to smoke will harm your health. |
| Featured: Parent Outcome: Respiratory Illness | 7. Quitting smoking will improve your health by preventing breathing problems like coughs, colds, wheezing or bronchitis. | 20. Continuing to smoke will harm your health by causing breathing problems like coughs, colds, wheezing or bronchitis. |
| Featured: Parent Outcome: Cancer | 8. Quitting smoking will decrease your risk of lung cancer and other cancers. | 21. Continuing to smoke will increase your risk of lung cancer and other cancers. |
| Featured: Parent Outcome: Financial Impact | 9. If you quit smoking, you will save $250 a month by not buying cigarettes. You will gain $250 a month | 22. If you continue to smoke, you will spend $250 a month buying cigarettes. You will lose $250 a month. |
| Featured: Family Outcome: General Health | 10. Quitting smoking will improve your families’ health. | 23. Continuing to smoke will harm your families’ health. |
| Featured: Family Outcome: Respiratory Illness | 11. Quitting smoking will improve your families’ health by preventing breathing problems like coughs, colds, wheezing or bronchitis in you and your child. | 24. Continuing to smoke will harm your families’ health by causing breathing problems like coughs, colds, wheezing or bronchitis in you and your child. |
| Featured: Family Outcome: Cancer | 12. Quitting smoking will decrease your families’ risk of lung cancer and other cancers. | 25. Continuing to smoke will increase your families’ risk of lung cancer and other cancers. |
| Featured: Family Outcome: Financial Impact | 13. If you quit smoking, you will save $250 a month by not buying cigarettes. You will gain $250 a month that could be spent on your family. | 26. If you continue to smoke, you will spend $250 a month buying cigarettes. You will lose $250 a month that could have been spent on your family. |
Discrete Choice Experiment
To identify what smoking cessation messages were deemed most important, parents completed a MaxDiff exercise in which they were shown a subset of the total messages and asked to pick messages most and least salient in response to the question: “If it came from your child’s doctor, which message would make you most likely to accept a referral to a Free Quitline or a medication prescription today.” The discrete choice experiment and the analysis were performed with Sawtooth Software (Lighthouse Studio, version 9.7.0), which generates a score for each of the original items on a scale of 0 (not important) to 100 (very important), enabling a person-level rank ordering of messages.
Latent Class Analysis
We performed a latent class analysis on the 26 item scores generated from the MaxDiff to identify subgroups of parents with similar preferences for smoking cessation messages.21 Latent class analysis, a type of structural equation modeling, is used to define groups within a population that have different characteristics, in this case, patterns of preferences between groups but similar responses within groups.21 In other words, a latent class analysis involves studying individuals as a whole on the basis of their response patterns across a number of individual characteristics relevant for a particular phenomenon (e.g., parent smoking cessation message preferences).22 To identify the optimal number of latent classes, we evaluated solutions with 2–5 latent class groups and replicated each latent class solution 5 times, using different random start values. The final number of groups was based on goodness of fit statistics and likelihood ratio tests available in Sawtooth software that compared the log-likelihood between a model based on k versus k + 1 groups, starting with k = 2. At each stage, the groups were also evaluated with respect to their size and meaning.23 We stopped the expansion once we had obtained a number of groups of reasonable size, with meaningful interpretation, and that were based on a model that fit the data well. Even though the fit statistics (e.g. Consistent Akaike Information Criterion (CAIC), AIC (Akaike Information Criterion), BIC (Bayesian Information Criterion), ABIC (Akaike Bayesian Information Criterion)) favored a 4 or 5 group solution, we ultimately chose a 3 group solution because it yielded the most meaningful groups and contained no subgroups with fewer than 20 parents. This approach assigned parents to the group for which they had the highest probability of membership.
Baseline Measures
Child (patient) and parent sociodemographic characteristics were collected at the in-office recruitment visit. Parents completed measures of health literacy using The Newest Vital Sign, a validated measure,24 and the Fagerström Test for Nicotine Dependence.25 Quit motivation was measured using the Contemplation Ladder, an efficient and face-valid measure, generalizable to diverse populations and associated with objective measures of readiness to quit smoking and actual quit attempts.26
Follow-up Measures
At the 4-week follow-up contact via telephone or electronic survey, we asked about smoking cessation efforts (quit attempts, medication use, and/or quitline use) to explore the potential relationship between message preference and potential behaviors. We assessed perceived quality of primary care with a validated measure adapted from Consumer Assessment of Healthcare Providers and Systems (CAHPS) questions.27 We assessed social support using the modified Medical Outcomes Study Social Support survey, a brief instrument validated across populations, including adult smokers.28
Statistical Analysis
We characterized the sample with descriptive statistics. After creating the latent class groups, we ran separate unadjusted, univariable multinomial logistic regression models to identify which parent and child characteristics were associated with latent class group. For a sample size calculation, approximately 30 to 60 respondents are needed per latent class for investigational work in a new area.29 Thus, prior to our analyses, we determined a sample size of 180 parent smokers was adequate to identify 3 to 5 potential latent classes. The follow-up exploratory smoking cessation behavior measures were compared across latent class groups via chi-square analysis. All P values represent 2-sided hypothesis tests with a significance level of .05.
Results
We approached 271 eligible parent smokers regarding potential participation; 180 (66.4%) agreed to enroll. Enrolled parents were typically women (66%) and within the 25–34 year (43%) or 35–44 year (34%) age category. Approximately half of parents displayed adequate health literacy (52%), and the majority of children of the parent sample had Medicaid insurance (69%). About half of the children were boys (51%); many were reported by parents as black or African American (57%) and not Hispanic or Latino (86%), and many had a history of an asthma diagnosis (31%). The median child age was 5 years (interquartile range [IQR:] 1.0–9.3). (Table 2)
Table 2:
Characteristics for Overall Sample and Latent Class Group
| Parent or Child Characteristic | Overall (N = 180) | Impact on Child (n = 92, 51%) | Gain-Framing (n = 63, 35%) | Financial Impact (n = 25, 14%) | P-value | |
|---|---|---|---|---|---|---|
| Child gender | 0.67 | |||||
| Male | 92(51%) | 50 (54%) | 30 (48%) | 12 (48%) | ||
| Female | 88 (49%) | 42 (46%) | 33 (52%) | 13 (52%) | ||
| Child race | 0.61 | |||||
| White | 39 (22%) | 20 (22%) | 13 (20%) | 6 (24%) | ||
| Black or African American | 103 (57%) | 50 (54%) | 41 (65%) | 12 (48%) | ||
| Other | 7 (4%) | 3 (3%) | 3 (5%) | 1 (4%) | ||
| Multi-racial | 31 (17%) | 19 (21%) | 6 (10%) | 6 (24%) | ||
| Child ethnicity | 0.30 | |||||
| Hispanic or Latino | 26 (14%) | 13 (14%) | 7 (11%) | 6 (24%) | ||
| Not Hispanic or Latino | 154 (86%) | 79 (86%) | 56 (89%) | 19 (76%) | ||
| Child age | 0.035 | |||||
| < 1 year | 31 (17%) | 17 (19%) | 9 (14%) | 5 (20%) | ||
| 1 – 5 years | 66 (37%) | 43 (47%) | 16 (25%) | 7 (28%) | ||
| 6 – 12 years | 62 (34%) | 21 (23%) | 30 (48%) | 11 (44%) | ||
| 13+ years | 21 (12%) | 11 (12%) | 8 (13%) | 2 (8%) | ||
| Child Insurance status | 0.45 | |||||
| Medicaid | 125 (70%) | 60 (65%) | 46 (73%) | 19 (76%) | ||
| Private | 51 (28%) | 29 (32%) | 17 (27%) | 5 (20%) | ||
| Self-Pay | 4 (2%) | 3 (3%) | 0 (0%) | 1 (4%) | ||
| Child health | 0.18 | |||||
| Excellent | 92 (51%) | 47 (51%) | 34 (54%) | 11 (44%) | ||
| Very Good | 59 (33%) | 26 (28%) | 21 (33%) | 12 (48%) | ||
| Good | 22 (12%) | 17 (19%) | 4 (6%) | 1 (4%) | ||
| Fair | 6 (3%) | 2 (2%) | 3 (5%) | 1 (4%) | ||
| Poor | 1 (1%) | 0 (0%) | 1 (2%) | 0 (0%) | ||
| Asthma | 0.011 | |||||
| No | 125 (69%) | 70 (76%) | 35 (56%) | 20 (80%) | ||
| Yes | 55 (31%) | 22 (24%) | 28 (44%) | 5 (20%) | ||
| Chronic Lung Disease | 0.27 | |||||
| No | 178 (99%) | 91 (99%) | 63 (100%) | 24 (96%) | ||
| Yes | 2 (1%) | 1 (1%) | 0 (0%) | 1 (4%) | ||
| Parent gender | 0.66 | |||||
| Male | 61 (34%) | 32 (35%) | 19 (30%) | 10 (40%) | ||
| Female | 119 (66%) | 60 (65%) | 44 (70%) | 15 (60%) | ||
| Parent age | 0.14 | |||||
| 18 to 24 | 15 (8%) | 9 (10%) | 4 (6%) | 2 (8%) | ||
| 25 to 34 | 78 (43%) | 42 (46%) | 22 (35%) | 14 (56%) | ||
| 35 to 44 | 61 (34%) | 33 (36%) | 21 (33%) | 7 (28%) | ||
| 45 to 54 | 20 (11%) | 8 (9%) | 11 (18%) | 1 (4%) | ||
| 55 to 64 | 4 (2%) | 0 (0%) | 3 (5%) | 1 (4%) | ||
| 65 to 74 | 2 (1%) | 0 (0%) | 2 (3%) | 0 (0%) | ||
| Parent education level | 0.848 | |||||
| Some high school, but did not graduate | 25 (14%) | 13(14%) | 9 (15%) | 3 (12%) | ||
| High school graduate or GED | 61 (34%) | 27 (29%) | 26 (41%) | 8 (32%) | ||
| Some college or 2-year degree | 70 (39%) | 40 (44%) | 21 (33%) | 9 (36%) | ||
| 4-year college graduate | 15 (8%) | 7 (8%) | 5 (8%) | 3 (12%) | ||
| More than 4-year college degree | 9 (5%) | 5 (5%) | 2 (3%) | 2 (8%) | ||
| Nicotine dependence1 | 0.139 | |||||
| Low dependence | 72 (40%) | 39 (42%) | 27 (43%) | 6 (24%) | ||
| Low to moderate dependence | 52 (29%) | 24 (26%) | 18(28%) | 10 (40%) | ||
| Moderate dependence | 46 (26%) | 26 (28%) | 15 (24%) | 5 (20%) | ||
| High dependence | 10 (6%) | 3 (3%) | 3 (5%) | 4 (16%) | ||
| Quit motivation2 | 0.624 | |||||
| Mean (SD) | 6.4 (1.4) | 6.5 (1.3) | 6.6 (1.3) | 6.2 (1.2) | ||
| Health literacy3 | 0.003 | |||||
| Adequate literacy | 93 (52%) | 60 (65%) | 22 (35%) | 11 (44%) | ||
| Limited literacy possible | 73 (41%) | 27 (29%) | 33 (52%) | 13 (52%) | ||
| Limited literacy likely | 14 (8%) | 5 (5%) | 8 (13%) | 1 (4%) | ||
| Site | 0.773 | |||||
| Urban, Predominantly Medicaid Clinic | 90 (50%) | 44 (48%) | 32 (51%) | 14 (56%) | ||
| Urban/Suburban, Predominantly Private Insurance | 40 (22%) | 21 (23%) | 14 (22%) | 5 (20%) | ||
| Urban, Mixed Insurance | 28 (16%) | 14 (15%) | 12 (19%) | 2 (8%) | ||
| Suburban, Predominantly Private Insurance | 22 (12%) | 13 (14%) | 5 (8%) | 4 (16%) | ||
Via the Fagerström Test for Nicotine Dependence
Via the Contemplation Ladder, an efficient and face-valid measure, which asks: “Which of the following best describes you?” with response options ranging from 1 (“I enjoy using cigarettes and have decided never to change it. I have no interest in changing the way that I use cigarettes”) to 10 (“I have quit using cigarettes and will never go back”).
Via the Newest Vital Sign, a reliable and validated measure
Common Patterns of Responsiveness to Framed Cessation Messages
The parent smokers could be assigned to 3 non-overlapping cessation message preference groups: messaging that focused on the impact on the child (n=92, 51% of sample), on gain-framing (n=63, 35%), and on financial impact (n=25, 14%). Figure 1 compares the ranked preferences for smoking cessation messages among groups, with groups defined by their top preferences. Messages that emphasized the impact of smoking on the child’s health were the top 5 preferences in the impact on the child group. For the gain-framing group, gain-framed messages were the top 5 out of 6 preferences, which included preferences for messages that focused on impact of smoking on the child as well as the family or parent. In contrast, messages that focused on the financial impact of quitting smoking or continuing to smoke were the top 4 preferences in the financial impact group but were the least important preferences for both of the other parent smoker groups.
Figure 1: Relative Importance of Smoking Cessation Messages in 3 Groups.
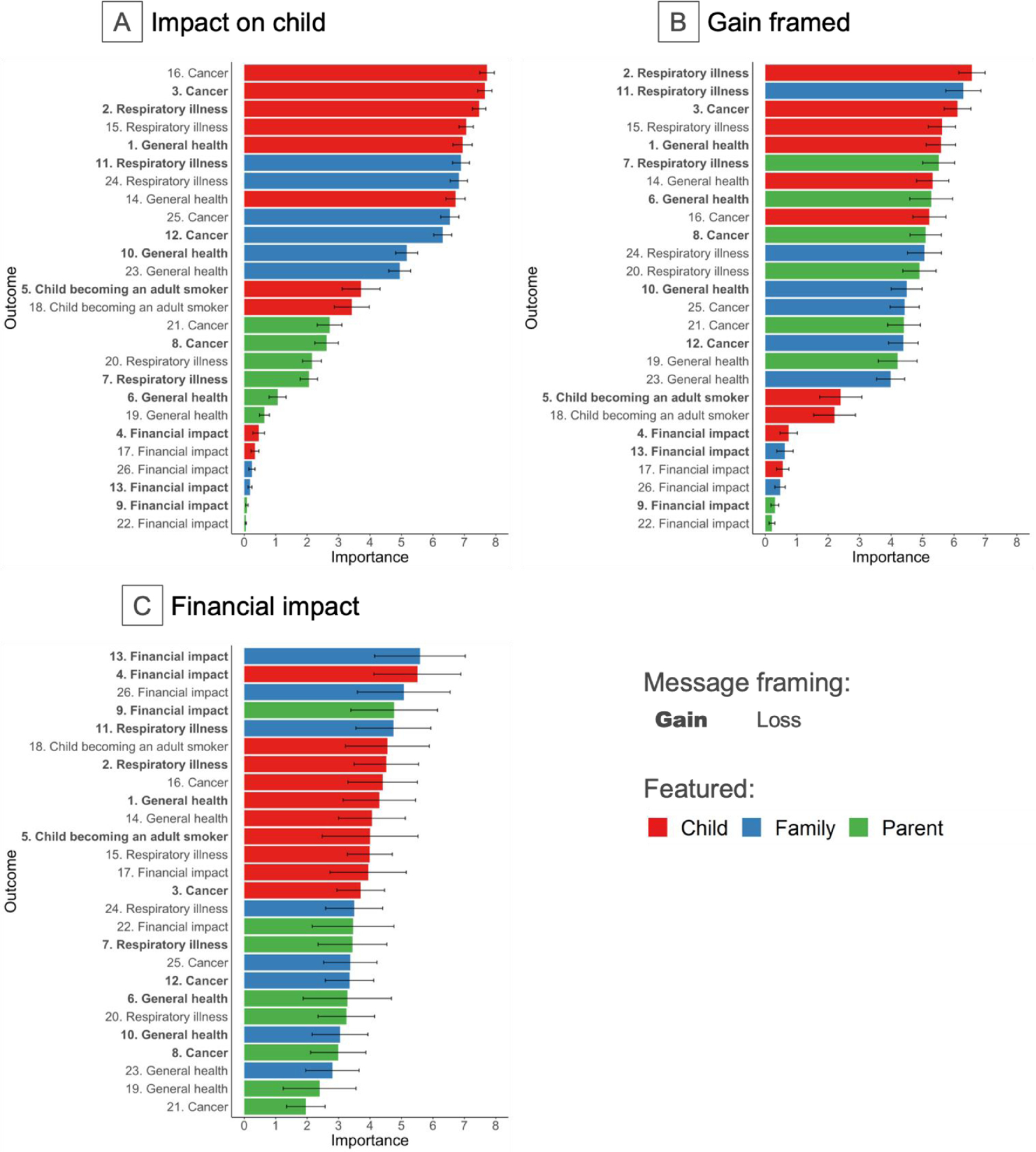
Importance scores for the different messages reflect important relative to each other (presented with 95% confidence intervals). Numbers on the y-axis correspond to the messages listed in Table 1. These scores are individual-level item scores which range from 0 to 100 and are ratio-scaled, meaning, for example, that a message with a score of 6 is twice as important as a message with a score of 3.
Characteristics of Parent Smokers in Framed Cessation Message Group
We examined whether membership in the 3 framed cessation message groups was associated with characteristics of either the parent or the child (Table 2). Of the characteristics examined (Table 3), parent smokers in the gain-framing group were more likely to have a child over age 6 (48% of children in the gain-framing group vs 23% in the impact on child health group; odds ratio [OR] = 2.85; 95% CI, 1.47–5.53) and with asthma (44% vs 24% of children; OR = 2.40; 95% CI, 1.21–4.76) as well as have limited health literacy (65% vs 34% of parents; OR = 3.49; 95% CI, 1.78–6.85), compared to the impact on child health group. No other characteristics were associated with group membership.
Table 3:
Parent or Child Characteristics Associated with Latent Class Group
| Gain Framed (vs. Impact of Smoking on Child) | Financial Impact (vs. Impact of Smoking on Child) | Financial Impact (vs. Gain Framed) | ||||
|---|---|---|---|---|---|---|
| Unadjusted Odds Ratio (95% CI) | P-Value | Unadjusted Odds Ratio (95% CI) | P-Value | Unadjusted Odds Ratio (95% CI) | P-Value | |
|
Child Sex Female (vs. Male) |
1.31 (0.69, 2.49 | 0.41 | 1.29 (0.53, 3.13) | 0.57 | 0.99 (0.39, 2.49) | 0.97 |
|
Child Age 6+ Years (vs. Younger, < 6 years) |
2.85 (1.47, 5.53) | 0.0019 | 2.03 (0.83, 4.97) | 0.12 | 0.71 (0.28, 1.81) | 0.48 |
|
Child Race Black (vs. Non-black) |
1.04 (0.50, 2.20) | 0.92 | 0.91 (0.34, 2.44) | 0.85 | 0.88 (0.31, 2.48) | 0.80 |
|
Child Ethnicity Hispanic (vs. Non-Hispanic) |
0.76 (0.29, 2.03) | 0.58 | 1.92 (0.65, 5.70) | 0.24 | 2.53 (0.76, 8.46) | 0.13 |
|
Child Insurance Private/Self Pay (vs. Medicaid) |
0.69 (0.34, 1.40) | 0.31 | 0.59 (0.22, 1.63) | 0.31 | 0.86 (0.29, 2.50) | 0.77 |
|
Child Health Rating Excellent (vs. Poorer health rating) |
1.12 (0.60, 2.13) | 0.72 | 0.75 (0.31, 1.83) | 0.53 | 0.67 (0.26, 1.70) | 0.40 |
|
Child Health Asthma (vs. None) |
2.40 (1.21, 4.76) | 0.012 | 0.95 (0.34, 2.66) | 0.92 | 0.40 (0.14, 1.12) | 0.081 |
|
Parent Age 35+ (vs. Younger, age < 35) |
1.77 (0.93, 3.39) | 0.084 | 0.70 (0.28, 1.75) | 0.44 | 0.40 (0.15, 1.03) | 0.058 |
|
Parent Sex Female (reference=Male) |
1.24 (0.62, 2.46) | 0.55 | 0.80 (0.32, 1.98) | 0.63 | 0.65 (0.25, 1.70) | 0.38 |
|
Parent Education College or more (vs. High school or less) |
0.62 (0.32, 1.17) | 0.14 | 0.98 (0.40, 2.39) | 0.96 | 1.60 (0.63, 4.04) | 0.33 |
|
Nicotine Dependence Moderate-High (vs. Low/Lower) |
0.87 (0.41, 1.75) | 0.69 | 1.22 (0.48, 3.09) | 0.67 | 1.41 (0.53, 3.76) | 0.50 |
|
Quit Motivation Later (vs. earlier) |
1.28 (0.59, 2.77) | 0.53 | 0.71 (0.27, 1.86) | 0.48 | 0.55 (0.20, 1.56) | 0.26 |
|
Health Literacy Limited Literacy possible/likely (vs. Adequate) |
3.49 (1.78, 6.85) | <0.001 | 2.39 (0.97, 5.86) | 0.057 | 0.68 (0.27, 1.76) | 0.43 |
Cessation Message Group and Smoking Cessation Behaviors
We were able to obtain follow-up information for 114 (64%) of the parent sample. There were no statistically significant differences in baseline demographic and clinical measures between completers and those lost to follow-up (data not shown). The majority of parents at follow-up had made a quit attempt (75%), with a large group of parents (33%) reporting current use of tobacco cessation medications (most often nicotine patch and/or gum), and a smaller group of parents (7%) reporting current quitline use. Quitting behaviors - quit attempts, medications used, and/or quitline use - did not differ meaningfully among the parents by latent class groups (P values 0.61, 0.51, 0.96, respectively; Table 4). Similarly, there was no meaningful difference between groups for other clinical measures, including perceived quality of the pediatric primary care delivered or parent social support scores.
Table 4:
Behaviors at Follow-up by Latent Class Group
| Characteristic/Behavior | Total1 (n=180) | Impact on Child (n=92) | Gain-Framing (n=63) | Financial Impact (n=25) | P-value |
|---|---|---|---|---|---|
| Follow-up | 0.57 | ||||
| Completed | 107 (59%) | 52 (57%) | 39 (62%) | 16 (64%) | |
| Partially Completed | 7 (4%) | 4 (4%) | 1 (2%) | 2 (8%) | |
| Incomplete | 66 (37%) | 36 (39%) | 23 (37%) | 7 (28%) | |
| Quit attempt | 0.61 | ||||
| Yes | 86 (75%) | 44 (79%) | 28 (70%) | 14 (78%) | |
| No | 28 (25%) | 12 (21%) | 12 (30%) | 4 (22%) | |
| Used Medications | |||||
| Yes | 37 (33%) | 17 (30%) | 12 (31%) | 8 (44%) | 0.51 |
| No | 76 (67%) | 39 (70%) | 27 (69%) | 10 (55%) | |
| Medication Types | 0.69 | ||||
| None | 76 (67%) | 39 (70%) | 27 (69%) | 10 (56%) | |
| Gum and patch | 16 (14%) | 9 (16%) | 5 (13%) | 2 (11%) | |
| Gum only | 11 (10%) | 5 (9%) | 3 (8%) | 3 (17%) | |
| Patch only | 7 (6%) | 2 (4%) | 3 (8%) | 2 (11%) | |
| Chantix | 2 (2%) | 1 (2%) | 0 (0%) | 1 (6%) | |
| Unknown | 1 (1%) | 0 (0%) | 1 (3%) | 0 (0%) | |
| Quitline Use | 0.96 | ||||
| Yes | 8 (7%) | 4 (7%) | 3 (8%) | 1 (6%) | |
| No | 105 (93%) | 52 (93%) | 36 (92%) | 17(94%) | |
| Quality Access | 0.25 | ||||
| Highest-quality care | 100 (93%) | 47 (89%) | 37 (95%) | 16(100%) | |
| Lower-quality care | 8 (7%) | 6(11%) | 2 (5%) | 0 (0%) | |
| Quality Family Centeredness | 0.72 | ||||
| Highest-quality care | 103 (93%) | 49 (91%) | 37 (95%) | 17 (94%) | |
| Lower-quality care | 8 (7%) | 5 (9%) | 2 (5%) | 1 (6%) | |
| Quality Timeliness | 0.79 | ||||
| Highest-quality care | 73 (70%) | 36 (69%) | 28 (74%) | 9 (64%) | |
| Lower-quality care | 31 (30%) | 16 (31%) | 10 (26%) | 5 (36%) | |
| Social Support Score2 | 0.99 | ||||
| 84 (61–97) | 83 (63–97) | 88 (59–95) | 83 (58–100) |
Total n=180; completed follow-up n=107; partially completed follow-up n=7
The Social Support Score provides an overall functional social support index, on a scale from 0–100. A higher score indicates more support, presented as median (interquartile range) within group.
Discussion
This study sought to better understand groups of parents with similar preferences for smoking cessation messages in order to support pediatric clinicians in their efforts to help parents quit. Using the combination of discrete choice methodology with latent class analysis, we identified groups of parent smokers with preferences for messages that focused on the impact of smoking on the child, gain-framed messages over loss-framed messages, and messages that focused on the financial impact of smoking. Compared to parents who preferred messages focused on the impact of smoking on their child’s health, parents who preferred gain-framed messages were more likely to have limited health literacy and a child over age 6 and with asthma. Finally, smoking cessation behaviors at follow-up were high in all parent groups, but the groups themselves did not differ meaningfully in quit efforts.
Personalizing the smoking cessation message for parent smokers may maximize treatment engagement. Incorporating the preferred language of patients in smoking cessation messages may increase perceived clinician empathy, patient engagement, and intrinsic motivation.30 Similar to efforts to identify the preferred language that clinicians use to discuss obesity management with parents and adolescents,31 these messages can improve conversations around parent smoking. For example, the majority of parents in this study preferred messaging focused on their child. The family context of decision making in pediatric settings may create different emotional reactions to parent-child health messages than adult-focused messages.32 This may relate to what others have identified as parents’ impulse to make a treatment decision for their child that a “good parent” would make.33 At the same time, a sizable subset of parents, especially those with limited health literacy and who have a child with asthma, may prefer messages that focus on the benefits of quitting smoking, especially as it relates to reducing respiratory illnesses. Parents who smoke often fail to spontaneously link their smoking to their child’s asthma.34 In smoking cessation interventions focused on parents of children with asthma, making this relationship more salient may increase motivation to quit among parents.8,35,36,37 Thus, for parent smokers with children who have asthma, gain-framed messages that succinctly highlight the connection between quitting smoking and the respiratory health of their child may prove particularly motivational. Finally, a minority of parent smokers have a clear preference for messages that focus on the financial impact of smoking, regardless of the frame, who the message features, or their own finances. This finding may relate to the role financial incentives play in smoking cessation and the emerging evidence of adult smoker preference for financial-based messages over health-focused messages in promoting smoking cessation.38 Overall, this study shows the preliminary potential of tailoring smoking cessation message to the behavioral needs of the parent. Though results should be interpreted with caution (meaning this may have been a particularly motivated sample of parents and/or completing the discrete choice experiment itself was uniquely motivational), at follow-up, parent smokers in our study reported higher rates of quit attempts and use of cessation counseling and/or medication compared to nationally representative surveys of current and former smokers.39
Further work will explore how to best incorporate these messages into clinical practice and the relationship between these tailored messages and subsequent behavior change, the goal of behavioral phenotyping. In the interim, particular messages could be matched to individual parent preference, just as clinicians already adjust individual therapeutic approaches to parent preferences or in response to past failures.18 While a gain-framed message focused on the health of the child may match the preferences of the majority of parents, the ideal goal would be to have messages tailored to all parents. Thus, motivating all smokers to quit or engage in treatment, not just a subset. In practice, a system could be created that has the parent choose an exemplar message from 1 of the 3 groups: a message focused on the child, one on all the benefits of quitting smoking, and one emphasizing the financial impact of quitting. Once a parent chooses their preferred message, the message may be reinforced during the office encounter by the pediatric clinician, then may be reinforced through ongoing engagement in the office setting, via telephone, text messaging, and/or other forms of office electronic communications.
Our findings suggest that behavioral economics approaches, more widely studied in adult healthcare contexts40,41 and based on foundational work in psychology and economics,42 will need to be adapted for the pediatric setting. While gain-framed messages are more effective than loss-framed in enhancing tobacco cessation efforts in adult healthcare settings,11,12,13 that same conclusion may not generalize to the pediatric setting. The largest group of parents preferred messages that focused on the impact of smoking on their child, regardless of gain- or loss-framing. These results highlight that best practices regarding motivating adult decision-makers to improve their own health may not directly translate when motivating the parent to adopt health promoting behaviors that impact their family. Parental smoking cessation is a particular relevant example, with negative health effects of tobacco impacting the entire family.
This study has several limitations. While identifying parent smoker perceived importance of smoking cessation messages is important and fundamental work,7,8 this study does not demonstrate what would actually make a difference in practice. Further, while parents completed the discrete choice experiment via tablet computer and were assured that individual results were anonymous, social desirability bias may have affected these results. Additionally, since the study population was exclusively English-speaking and from one geographic area, testing of messages with non-English speakers and in other regions is warranted to confirm generalizability of findings to the broader US population. Further, the study did not explore how the preceding relationship between the pediatric clinician and parent/child may have affected the impact of messaging. Finally, this study captured parent preferences for messages at one point in time. Rather than being static, preferences for certain messages may change over time or vary based on the ongoing relationship with their child’s pediatric clinician, similar to, for example, the changes in parent preferences and goals over time regarding ADHD decision-making and initiating treatment.43 Future studies will evaluate methods to deliver these smoking messages to parents in clinical practice, preference patterns over time, and the impact of these messages on subsequent smoking cessation.
Conclusions
Using rigorous methods to develop and test messages targeted at parents, we identified 3 message groups, each with similar message preferences (impact on child, gain-framing, or financial impact). Further work should explore the potential to tailor cessation messages to different parent groups, leveraging what matters most to them to maximize treatment engagement.
What’s New:
Using discrete choice methodology with latent class analysis, we identified groups of parent smokers with preferences for motivational messages that focused on the impact of smoking on the child, gain-framed over loss-framed messages, and the financial impact of smoking.
Acknowledgements
We thank the network of primary care clinicians, their patients, and families for their contribution to this project and clinical research facilitated through the Pediatric Research Consortium at CHOP.
Funding:
Dr. Jenssen was awarded grants through the National Cancer Institute of the National Institutes of Health under Award Number K08CA226390 and the Flight Attendant Medical Research Institute through a grant to the American Academy of Pediatrics Julius B. Richmond Center to support the study described in this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Potential Conflicts of Interest: The authors have no financial relationships relevant to this article to disclose.
References:
- 1.Jha P, Ramasundarahettige C, Landsman V, et al. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368(4):341–350. doi: 10.1056/NEJMsa1211128 [DOI] [PubMed] [Google Scholar]
- 2.den Exter Blokland EAW, Engels RCME, Hale WW, et al. Lifetime parental smoking history and cessation and early adolescent smoking behavior. Prev Med. 2004;38(3):359–368. doi: 10.1016/j.ypmed.2003.11.008 [DOI] [PubMed] [Google Scholar]
- 3.U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General, 2014. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. Accessed February 11, 2016 http://www.surgeongeneral.gov/library/reports/50-years-of-progress/ [Google Scholar]
- 4.Tsai J, Homa DM, Gentzke AS, et al. Exposure to Secondhand Smoke Among Nonsmokers - United States, 1988–2014. MMWR Morb Mortal Wkly Rep. 2018;67(48):1342–1346. doi: 10.15585/mmwr.mm6748a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farber HJ, Walley SC, Groner JA, Nelson KE, Section on Tobacco Control. Clinical Practice Policy to Protect Children From Tobacco, Nicotine, and Tobacco Smoke. Pediatrics. 2015;136(5):1008–1017. doi: 10.1542/peds.2015-3108 [DOI] [PubMed] [Google Scholar]
- 6.Winickoff JP, Nabi-Burza E, Chang Y, et al. Implementation of a parental tobacco control intervention in pediatric practice. Pediatrics. 2013;132(1):109–117. doi: 10.1542/peds.2012-3901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daly JB, Mackenzie LJ, Freund M, et al. Interventions by health care professionals who provide routine child health care to reduce tobacco smoke exposure in children: A review and meta-analysis. JAMA Pediatr. 2016;170(2):138–147. doi: 10.1001/jamapediatrics.2015.3342 [DOI] [PubMed] [Google Scholar]
- 8.Behbod B, Sharma M, Baxi R, et al. Family and carer smoking control programmes for reducing children’s exposure to environmental tobacco smoke. Cochrane Database Syst Rev. 2018;1:CD001746. doi: 10.1002/14651858.CD001746.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. Cochrane Database Syst Rev. 2017;3:CD001292. doi: 10.1002/14651858.CD001292.pub3 [DOI] [PubMed] [Google Scholar]
- 10.Stead LF, Buitrago D, Preciado N, et al. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2013;5:CD000165. doi: 10.1002/14651858.CD000165.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rothman AJ, Salovey P. Shaping perceptions to motivate healthy behavior: the role of message framing. Psychol Bull. 1997;121(1):3–19. [DOI] [PubMed] [Google Scholar]
- 12.Gallagher KM, Updegraff JA. Health message framing effects on attitudes, intentions, and behavior: a meta-analytic review. Ann Behav Med Publ Soc Behav Med. 2012;43(1):101–116. doi: 10.1007/s12160-011-9308-7 [DOI] [PubMed] [Google Scholar]
- 13.Moorman M, van den Putte B. The influence of message framing, intention to quit smoking, and nicotine dependence on the persuasiveness of smoking cessation messages. Addict Behav. 2008;33(10):1267–1275. doi: 10.1016/j.addbeh.2008.05.010 [DOI] [PubMed] [Google Scholar]
- 14.Jenssen BP, Kelly MK, Faerber J, et al. Parent Preferences for Pediatric Clinician Messaging to Promote Smoking Cessation Treatment. Pediatrics. 2020;146(1). doi: 10.1542/peds.2019-3901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mahabee-Gittens EM, Collins BN, Murphy S, et al. The parent-child dyad and risk perceptions among parents who quit smoking. Am J Prev Med. 2014;47(5):596–603. doi: 10.1016/j.amepre.2014.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosen LJ, Noach MB, Winickoff JP, Hovell MF. Parental Smoking Cessation to Protect Young Children:A Systematic Review and Meta-analysis. Pediatrics. 2012;129(1):141–152. doi: 10.1542/peds.2010-3209 [DOI] [PubMed] [Google Scholar]
- 17.Kangovi S, Asch DA. Behavioral Phenotyping in Health Promotion: Embracing or Avoiding Failure. JAMA. 2018;319(20):2075–2076. doi: 10.1001/jama.2018.2921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Volpp KG, Krumholz HM, Asch DA. Mass Customization for Population Health. JAMA Cardiol. 2018;3(5):363–364. doi: 10.1001/jamacardio.2017.5353 [DOI] [PubMed] [Google Scholar]
- 19.Kutner M, Greenberg E, Jin Y, Paulsen C. The Health Literacy of America’s Adults: Results From the 2003 National Assessment of Adult Literacy (NCES 2006–483). U.S. Department of Education; 2006. [Google Scholar]
- 20.Yin HS, Johnson M, Mendelsohn AL, et al. The health literacy of parents in the United States: a nationally representative study. Pediatrics. 2009;124 Suppl 3:S289–298. doi: 10.1542/peds.2009-1162E [DOI] [PubMed] [Google Scholar]
- 21.McCulloch CE, Lin H, Slate EH, Turnbull BW. Discovering subpopulation structure with latent class mixed models. Stat Med. 2002;21(3):417–429. [DOI] [PubMed] [Google Scholar]
- 22.Hopfer S, Wright ME, Pellman H, et al. HPV vaccine recommendation profiles among a national network of pediatric practitioners: understanding contributors to parental vaccine hesitancy and acceptance. Hum Vaccines Immunother. 2019;15(7–8):1776–1783. doi: 10.1080/21645515.2018.1560771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Software Sawtooth. Latent Class v4: Software for Latent Class Estimation for CBC Data. Sawtooth Software, Inc; 2007. http://www.sawtoothsoftware.com/download/ssiweb/LClass_Manual.pdf [Google Scholar]
- 24.Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3(6):514–522. doi: 10.1370/afm.405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86(9):1119–1127. [DOI] [PubMed] [Google Scholar]
- 26.Biener L, Abrams DB. The Contemplation Ladder: validation of a measure of readiness to consider smoking cessation. Health Psychol Off J Div Health Psychol Am Psychol Assoc. 1991;10(5):360–365. [DOI] [PubMed] [Google Scholar]
- 27.Brousseau DC, Hoffmann RG, Nattinger AB, et al. Quality of primary care and subsequent pediatric emergency department utilization. Pediatrics. 2007;119(6):1131–1138. doi: 10.1542/peds.2006-3518 [DOI] [PubMed] [Google Scholar]
- 28.Moser A, Stuck AE, Silliman RA, et al. The eight-item modified Medical Outcomes Study Social Support Survey: psychometric evaluation showed excellent performance. J Clin Epidemiol. 2012;65(10):1107–1116. doi: 10.1016/j.jclinepi.2012.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Orne B Sample size issues for conjoint analysis In: Getting Started with Conjoint Analysis: Strategies for Product Design and Pricing Research. 2nd ed Research Publishers LLC; :57–66. [Google Scholar]
- 30.Fiore MC, Jaén CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. U.S. Department of Health and Human Services. Public Health Service; 2008. [Google Scholar]
- 31.Puhl RM, Peterson JL, Luedicke J. Parental perceptions of weight terminology that providers use with youth. Pediatrics. 2011;128(4):e786–793. doi: 10.1542/peds.2010-3841 [DOI] [PubMed] [Google Scholar]
- 32.Lipstein EA, Brinkman WB, Fiks AG, et al. An emerging field of research: challenges in pediatric decision making. Med Decis Mak Int J Soc Med Decis Mak. 2015;35(3):403–408. doi: 10.1177/0272989X14546901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Feudtner C, Walter JK, Faerber JA, et al. Good-parent beliefs of parents of seriously ill children. JAMA Pediatr. 2015;169(1):39–47. doi: 10.1001/jamapediatrics.2014.2341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mahabee-Gittens M Smoking in parents of children with asthma and bronchiolitis in a pediatric emergency department. Pediatr Emerg Care. 2002;18(1):4–7. doi: 10.1097/00006565-200202000-00002 [DOI] [PubMed] [Google Scholar]
- 35.Borrelli B, McQuaid EL, Tooley EM, et al. Motivating parents of kids with asthma to quit smoking: the effect of the teachable moment and increasing intervention intensity using a longitudinal randomized trial design. Addict Abingdon Engl. 2016;111(9):1646–1655. doi: 10.1111/add.13389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Halterman JS, Borrelli B, Conn KM, Tremblay P, Blaakman S. Motivation to quit smoking among parents of urban children with asthma. Patient Educ Couns. 2010;79(2):152–155. doi: 10.1016/j.pec.2009.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Office on Smoking and Health (US). The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Centers for Disease Control and Prevention (US); 2006. Accessed February 11, 2016 http://www.ncbi.nlm.nih.gov/books/NBK44324/ [PubMed] [Google Scholar]
- 38.Sindelar JL, O’Malley SS. Financial versus health motivation to quit smoking: a randomized field study. Prev Med. 2014;59:1–4. doi: 10.1016/j.ypmed.2013.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Babb S, Malarcher A, Schauer G, et al. Quitting Smoking Among Adults - United States, 2000–2015. MMWR Morb Mortal Wkly Rep. 2017;65(52):1457–1464. doi: 10.15585/mmwr.mm6552a1 [DOI] [PubMed] [Google Scholar]
- 40.Asch DA, Troxel AB, Stewart WF, et al. Effect of financial incentives to physicians, patients, or both on lipid levels: A randomized clinical trial. JAMA. 2015;314(18):1926–1935. doi: 10.1001/jama.2015.14850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Halpern SD, Loewenstein G, Volpp KG, et al. Default options in advance directives influence how patients set goals for end-of-life care. Health Aff Proj Hope. 2013;32(2):408–417. doi: 10.1377/hlthaff.2012.0895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tversky A, Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211(4481):453–458. [DOI] [PubMed] [Google Scholar]
- 43.Fiks AG, Mayne S, Debartolo E, et al. Parental preferences and goals regarding ADHD treatment. Pediatrics. 2013;132(4):692–702. doi: 10.1542/peds.2013-0152 [DOI] [PMC free article] [PubMed] [Google Scholar]


