Abstract
Coronavirus disease 2019 (COVID-19) is a novel infectious disease that has spread world-wide. In the United States, COVID-19 disproportionately affects racial and ethnic minorities, particularly African Americans, with an observed two-fold higher rate for hospitalization and greater than two-fold higher rate for death as compared to White Americans. The disparity seen with COVID-19 is consistent with patterns of disparities observed for cancer; it is well-documented that 5-year survival rates for multiple cancers are lower in African Americans compared to White Americans. Root cause contributions for the disparity overlap between COVID-19 and cancer. While cancer is a genetic disease that is influenced by tissue microenvironment, COVID-19 is an infectious disease that is enabled by cellular expression of angiotensin converting enzyme 2 (ACE2) receptors. However, socioeconomic disadvantages, level of education, lifestyle factors and health co-morbidities, and limited access to medical care appear to fuel underlying risk for both cancer and COVID-19 disparities. In addition to African Americans demonstrating higher risk of acquiring and dying from either disease, they are under-represented in clinical trials involving cancer or COVID-19. Long-term disparities are present with survivorship from cancer and may be likely with survivorship from COVID-19; both have revealed untoward effects on post-diagnosis economic viability for African Americans. Collaborative strategies that include community engagement, diverse participation in cancer and COVID-19 clinical trials, providing insurance for affected persons who lost employment due to either disease, and supporting safety-net and public hospitals for healthcare access will be critical to stem these disparities.
Keywords: COVID-19, disparity, African American, cancer disparity, clinical trial, cancer outcome, cancer survival
Perspective
Outbreak of coronavirus disease 2019 (COVID-19) in the human population caused widespread morbidity and mortality throughout the world. The United States has borne a disproportionate amount of the disease burden. Furthermore, disparately-high COVID-19 incidence, death-rates, and socioeconomic consequences of the pandemic-related recession on racial and ethnic minorities have forced the country to confront the harsh reality of systemic racism effects on public health. The U.S. Centers for Disease Control and Prevention (CDC) reports that more than 20% of COVID-19 cases occur in African Americans, which comprise only 13% of the population. Similarly, while Latinx ethnicity account for nearly 17% of the U.S. population, this group has 32% of the COVID-19 infections [1]. Differences in population-based COVID-19 mortality rates are also stark; death rates for African Americans are 85/100,000, 52/100,000 for Latinx, 53/100,000 for Native Americans, and 35/100,000 for White Americans [2]. In surveys regarding the financial impact of COVID-19, 61% of Latinx, 44% of African American and 38% of Whites stated that “they or someone in their household has lost a job or taken a pay cut due to the coronavirus outbreak”; 78% of African American, 70% of Latinx and 47% of Whites stated “they do not have rainy day funds to cover expenses for 3 months in case of emergency” [3]. It is clear that the profound impact of COVID-19 on medical and socioeconomic health is disproportionately shouldered by race/ethnicity.
Disparities in COVID-19 are consistent with patterns observed in cancer, particularly in African Americans where data are the most robust. Differences in cancer incidence, stage distribution, and mortality for African Americans compared to White Americans are well-documented. For example, 5-year stage-specific survival from breast, colorectal, esophagus, kidney, liver, lung, melanoma, lymphoma, ovarian, bladder, cervical, uterine and head & neck cancer are lower for African Americans compared to Whites [4]. Causes of cancer disparities are multifactorial and include germline genetic susceptibility, but this risk can be enhanced or moderated by the macro- (socioeconomic and living conditions) and micro- (local microbiome, inflammation, toxin exposures) environment. [5-7].
Cancer results from cellular genetic alterations yielding growth advantages over other cells, and the acquired ability to metastasize. The development of cancer as well as its biological behavior are shaped by environmental influences such as lifestyle choices or exposures. For instance, ingesting a high fat/high caloric diet, and prolonged use of tobacco and/or alcohol increase cancer risk by altering the lung and gut microbiome, thereby changing levels of systemic inflammation and immunity that ultimately influence genetic alterations in cells [5,8,9]. In addition to modifying cancer risk, these lifestyle factors cause physiological changes increasing risk for various inter-related co-morbidities such as obesity and diabetes; asthma and chronic obstructive pulmonary disease, as well as hypertension, cardiovascular and kidney disease [5,7,10,11]. These co-morbidities can influence cancer treatment [12,13] and have been correlated with adverse outcomes from cancer surgery, impaired ability to deliver effective chemotherapy, and radiation toxicity. Primary prevention of selected cancers can be achieved by avoiding known carcinogens such as tobacco, or by utilizing chemoprevention such as tamoxifen for patients at high risk for breast cancer. Substantial reductions in cancer burden are also attained through screening modalities for early detection of cervical, breast, colorectal, and prostate cancer. [7,14].
COVID-19 is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The virus enters respiratory (and other) cells via angiotensin converting enzyme 2 (ACE2) receptors on the human cell surface [15]. COVID-19 ranges phenotypically from completely asymptomatic to severe disease, with pulmonary, thromboembolic, cardiovascular, and renal sequelae. Risk factors for severe COVID-19 illness include older age, male gender, race/ethnicity, and pre-existing co-morbid diseases. Co-morbidities furthermore magnify disease severity within the other the high-risk subsets of advanced-age and male patients [16,17]. At present, treatment for COVID-19 is limited to supportive medical care, and primary prevention is promoted by avoiding infection through social distancing and use of personal protective equipment such as masks.
African Americans develop severe COVID-19 disease requiring hospitalization at twice the rate of White Americans [17,18]. COVID-19 has now lengthened an already formidable list of diseases that affect African Americans disproportionately, including cancer, diabetes, hypertension, and asthma. The high incidence of COVID-19 among African Americans compared to White Americans is attributed to environmental viral load exposures. Currently, there is no evidence of genetic susceptibility, however, germline ancestral genetics that can influence cancer risk as well as inflammatory response to infectious disease are topics of ongoing COVID-19 research. African Americans are disproportionately represented among essential workers that were exempted from shelter-in-place mandates during the pandemic surge; they are also more likely to share households with more than six residents [19]. Housing disadvantages that are more prevalent in African American communities undermine social distancing efforts via reduced indoor space, limited open-air access, and smaller elevator sizes. These issues of increased residential housing density are particularly relevant in urban areas, where African American populations are more heavily-concentrated. African Americans are more than three times as likely to use public transportation on a regular basis compared to White Americans [20].
While the genetic versus infectious etiologies of COVID-19 and cancer greatly differ, risk factors for outcome disparities in both diseases intersect with regard to co-morbidities and socioeconomic disadvantage (Figure 1). The history of African Americans is characterized by a plethora of human rights violations dating back to the slavery era but persisting today through the effects of implicit biases and systemically-compromised educational, professional and residential opportunities. In addition to the irrefutable association between impaired access to medical care and the two-fold-higher rates of poverty among African Americans compared to White Americans, the cumulative result of this history has been a pervasive negative impact on the overall health of African Americans. Housing disadvantages correlate with food deserts and lack of recreational park spaces, which ultimately affect nutritional and exercise practices. Optimal utilization of available medical care and clinical trial participation is further limited by longstanding fears and mistrust derived from past exploitation of African Americans, as with the Tuskegee Syphilis Study and non-permissive utilization of Henrietta Lacks’ cells [21]. Additionally, African Americans are under-represented in the physician workforce, and access to proper medical care among African American patients in the past was further compromised by restrictions placed on the few African American physicians that were available. For example, many hospitals denied admitting privileges to African American physicians and they were denied membership into the American Medical Association until 1964 [22]. Implicit biases persist in contemporary healthcare and inequities in delivery of medical treatment as well as health education might also contribute to COVID-19 disparities [23].
Figure 1.
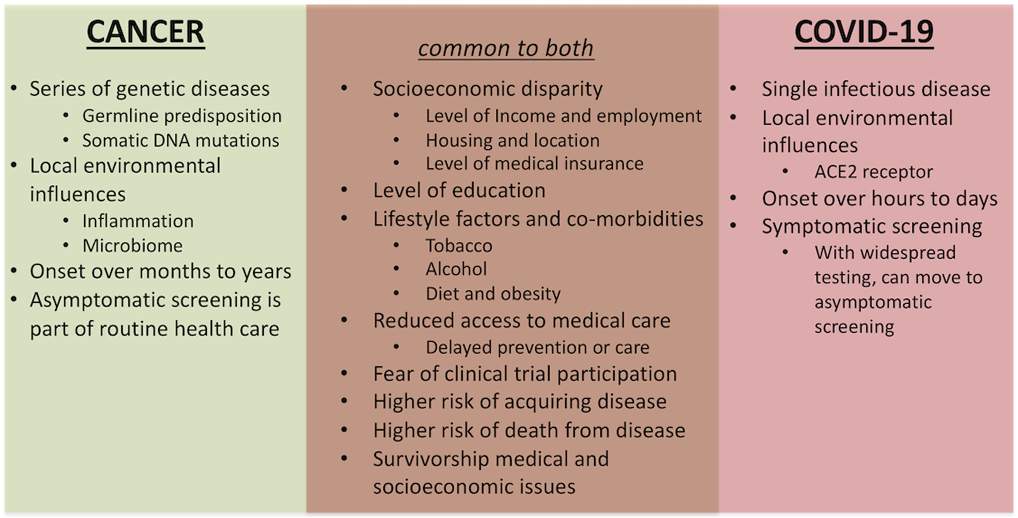
Differences and overlap similarities for the pathogenesis, incidence and mortality risks between cancer and COVID-19.
This confluence of circumstances create conditions that allow co-morbidities to develop disproportionately in the African American population. These co-morbidities place African Americans at higher risk for poor cancer outcomes, as well as at increased risk and severity for COVID-19 infection (Figure 1). Cancer survivorship for African Americans has also been associated with reduced health-related quality of life [24]. Long-term effects of COVID-19 are uncertain; lingering symptoms including fatigue, dyspnea, cognitive impairment, and tachy-arrhythmias have been reported [25]. The 1918 Spanish flu experience revealed decades-later developmental effects on the birth cohort from that pandemic [26].
The COVID-19-induced recession tripled unemployment rates between March and April 2020 [27]. Modest evidence of recovery reflected in declining unemployment rates for June and July 2020 prompted some to describe a “V-shaped” economic rebound. Such an optimistic proclamation is premature in the face of the ongoing pandemic impact, and it completely overlooks the disproportionate and enduring effects of the COVID-19-induced recession on the African American population. Unemployment rates for White Americans were 4.0%, 14.2% and 9.2% in March, April, and July 2020 respectively; corresponding rates for African Americans were 6.7%, 16.7% and 14.6% [27], with losses of employment-based insurance for these individuals and their dependents. Downstream adverse effects on COVID-19 and cancer care are then somewhat predictable with little medical insurance.
Safety-net and public hospitals deliver health care to patients that are underinsured or non-insured; these facilities are more highly-concentrated in inner-city locations. African Americans comprise a substantial proportion of their patient population because of insurance factors as well as geography and household income and resources. Urban safety-net facilities are often located within African American neighborhoods, thereby serving as employment hubs for these communities. The pandemic impact on safety-net hospitals was disproportionately devastating and initiated a disastrous cycle of worsening disparities for African Americans with regard to feasible options for both COVID-19 and cancer care. Costs of COVID-19 medical care became exorbitant for hospitals. Providing this care to patients that are unable to pay and that often have poorly-controlled co-morbidities has left many safety-net hospitals on the brink of bankruptcy [28,29]. When these facilities attempt returning towards pre-COVID-19 usual health care practices, they face challenges in catching up with cancer screening backlogs because of social distancing space and scheduling arrangements that were never designed to be optimized in these facilities [30]. Many African Americans rely on safety-net institutions for routine medical care, COVID-19 care and cancer care, further escalating their risk for health outcome disparities. The importance of safety-net institutions is also relevant to the discussion of clinical trial research for cancer as well as COVID-19. The regulatory, administrative, and personnel costs of medical research in humans is a huge financial burden for hospitals, and these expenses are often beyond the fiscal plans of safety-net facilities.
Data regarding race-stratified outcomes in patients with both COVID-19 infection and cancer are limited at present. Recent studies have implicated germline genetics and epigenetics in the etiology of cancer disparities [10,11]; inflammatory pathways linked to these genetic patterns might also play a role in the cytokine storm linked to COVID-19 severity. A multicenter study of COVID-19 patients in New York City undergoing treatment for gynecologic oncology malignancies demonstrated higher mortality among the African American cases, but this association was no longer present in multivariable modeling accounting for socioeconomics and co-morbidities [31]. As reviewed by Phillips et al [32], African ancestral polymorphisms in angiotensin converting enzyme 2 (ACE2) and acetylcholinesterase represent genetic patterns that have been correlated with co-morbidities such as hypertension and diabetes; these genes contribute to COVID-19 infectivity and compound the difficulties of disentangling the effects of socioeconomic status, co-morbidities and race/ethnicity on COVID-19 outcomes. Research regarding the interplay of germline genetics and ancestry with cancer, co-morbidities and infectious disease is clearly warranted.
How can we mitigate disparities in cancer and COVID-19? Efforts to eliminate co-morbidities such as obesity and diabetes are ideal, but have proven challenging on a population basis. We should also strive to reverse the systemic/structural disadvantages that exist for certain racial/ethnic populations and which establish conditions that predispose to co-morbidities. Achieving health equity through improved access to educational and professional opportunities requires the will of the nation as well as political forces to enact broad-sweeping anti-racism programs. In the short term, we suggest several strategies that can be implemented at the federal and local government levels, the hospital and community levels, and the provider and research levels to address COVID-19 disparities and lessen the downstream pandemic-induced recession consequences on cancer disparities (Table 1). Important “lessons learned” in cancer research include the facts that inadequate diversity in contemporary clinical trial accruals is largely secondary to provider-level impediments with failure to offer participation opportunities to African Americans and co-morbidity exclusion criteria that disproportionate affect African Americans; these problems will need to be addressed in COVID-19 research. Efforts to improve diversity in the accrual of patients to cancer and COVID-19 research are necessary so that results can be generalized with confidence, and these efforts deserve to be supported through creative investments by academia, industry and federal funding sources into safety-net institutions to: (a) develop enduring relationships and infrastructure with safety-net hospitals in diverse communities, (b) increase diversity representation in clinical trials, and (c) be financially feasible for safety-net hospitals to conduct meaningful clinical trials. Issues such as the “digital divide” that exist between racial/ethnic communities create barriers to effective telehealth and video visits. COVID-19 has had a dual effect on undermining cancer outreach programs of healthcare institutions and professional advocacy organizations; the pandemic-induced recession has reduced revenue overall, and fundraising efforts such as walkathons and public events that depend on large gatherings for their success are not feasible in the context of social distancing policies.
Table 1.
Strategies for collaborative advocacy designed to mitigate disparities related to the COVID-19 pandemic and cancer burden.
| CANCER | CANCER and COVID-19 | COVID-19 |
|---|---|---|
| Race/ethnic minority populations should be targeted for aggressive cancer screening programs as access to these services return in the post-COVID-19 era to prevent deterioration of prior gains in screening | Cancer clinical trials teams should leverage community engagement and patient navigator networks to ensure diverse accrual onto COVID-19 testing, treatment and vaccine studies | COVID-19 research proposals should be designed a priori with disparities-related research questions, such as correlative science studies looking at genetic ancestry |
| The cancer community must work proactively to protect cancer disparity research projects and community outreach/education efforts in the post-COVID-19 era of budget constraints. Disparities research and health education efforts targeting diverse communities must not be perceived as expendable items | Public hospitals (which were disproportionately devastated by the costs of COVID-19 pandemic care) must be supported so that they can meet the safety-net health care needs of communities that are disproportionately represented among the medically-underserved | Health insurance coverage opportunities such as expanded Medicaid programs should be made readily-available to financially-constrained individuals that lost their employment-based coverage as a consequence of the COVID-19 pandemic |
| Cancer-related advocacy organizations that provide community engagement activities addressing disparities should be supported | Need for improved access to technologies and devices that support telehealth services to reach minority populations | COVID-19 vaccine and treatment trials should be statistically designed to oversample racial-ethnic minority populations, so that results can be generalized with confidence |
The healthcare community and the population-at-large need to be cognizant of similarities in risk for COVID-19 as well as cancer disparities, and eliminating these disparities should be a public health imperative.
Statement of Translational Relevance.
Documented disparities in cancer incidence and mortality for racial and ethnic minorities and the medically-underserved appear to be replicated with infection and survival outcome from COVID-19; the similarities are striking, with the underpinnings rooted in systemic structural socioeconomic disadvantages. Implementation of strategies to alleviate both cancer and COVID-19 disparities through governmental advocacy and action, hospital and community involvement, and provider and researcher participation must be proactively undertaken as a public health imperative. Adequate representation of racial and ethnic minorities in both cancer clinical trials and COVID-19 vaccine trials will boost confidence within those communities for uniform acceptance of results, enhance future clinical trial participation based on partnerships with the communities, and improve overall medical long-term compliance.
Acknowledgements:
LAN is supported by the Susan B. Komen Foundation (SAC160072) and Fashion Footwear Association of New York Charitable Foundation. RAW is supported by the U.S. Public Health Service (U54CA202997 and U54MD012523). JMC is supported by the U.S. Public Health Service (R01CA206010) and the A. Alfred Taubman Medical Research Institute of the University of Michigan.
Footnotes
Disclosure of Potential Conflicts of Interest: JMC, RAW, and LAN declare no potential conflict of interests or disclosures.
References
- 1.https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html (Accessed August 24, 2020)
- 2.https://covidtracking.com/race (Accessed August 24, 2020)
- 3.https://www.pewresearch.org/fact-tank/2020/05/05/financial-and-health-impacts-of-covid-19-vary-widely-by-race-and-ethnicity/ (Accessed August 24, 2020)
- 4.Seigel RL, Miller KD, Jemal A, Cancer Statistics, 2020. CA Cancer J Clin 2020;70:7–30. [DOI] [PubMed] [Google Scholar]
- 5.Carethers JM, Doubeni CA. Causes of socioeconomic disparities in colorectal cancer and intervention framework and strategies. Gastroenterol 2020;158:354–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ashktorab H, Brim H, Kupfer SS, Carethers JM. Racial disparity in gastrointestinal cancer risk. Gastroenterol 2017;153:910–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Newman LA. Breast Cancer Disparities: Socioeconomic Factors versus Biology. Ann Surg Oncol. 2017;24:2869–2875. [DOI] [PubMed] [Google Scholar]
- 8.Grady WM and Carethers JM. Genomic and epigenetic instability in colorectal cancer pathogenesis. Gastroenterol 2008;135:1079–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carethers JM, Jung BH. Genetics and genetic biomarkers in sporadic colorectal cancer. Gastroenterol 2015;149:1177–1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carethers JM. Clinical and Genetic Factors to Inform Reducing Colorectal Cancer Disparities in African Americans. Front Oncol. 2018;8:531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Newman LA, Jenkins B, Chen Y, et al. Hereditary Susceptibility for Triple Negative Breast Cancer Associated with Western Sub-Saharan African Ancestry: Results from an International Surgical Breast Cancer Collaborative. Ann Surg. 2019;270(3):484–492. [DOI] [PubMed] [Google Scholar]
- 12.Mu L, Zhu N, Zhang J, Xong F. Li D, Wang X. Type 2 diabetes, insulin treatment and prognosis of breast cancer. Diabetes Metab Res Rev 2017;33(1). [DOI] [PubMed] [Google Scholar]
- 13.Protani M, Coory M, Martin JH. Effect of obesity on survival of women with breast cancer: systematic review and meta-analysis. Breast Cancer Res Treat 2010;123:627–635. [DOI] [PubMed] [Google Scholar]
- 14.Carethers JM. Screening for colorectal cancer in African Americans: Determinants and rationale for an earlier age to commence screening. Dig Dis Sci 2015;60:711–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matheson NJ, Lehner PJ. How does SARS-CoV-2 cause COVID-19? Science 2020;369:510–511. [DOI] [PubMed] [Google Scholar]
- 16.McMichael TM, Currie DW, Clark S, Pogosjans S, Kay M, Schwartz NG, et al. Epidemiology of Covid-19 in a long-term care facility in King County, Washington. N Eng J Med 2020;382:2005–2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Price-Haywood E, Burton J, Fort D, Seoane L. Hospitalization and mortality among Black patients and White patients with Covid-19. N Engl J Med 2020;382:2534–2543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Poulson M, Geary A, Annesi C, Allee L, Kenzik, Sanchez S, Tseng J, Dechert T. National disparities in COVID-19 outcomes between Black and White Americans. J Natl Med Assoc 2020. August 7;S0027-9648(20)30149–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Selden TM, Berdahl TA. COVID-19 and Racial/Ethnic Disparities in Health Risk, Employment, And Household Composition. Health affairs. 2020:101377hlthaff202000897. [DOI] [PubMed] [Google Scholar]
- 20.Anderson M Who relies on public transportation in the U.S. https://www.pewresearch.org/fact-tank/2016/04/07/who-relies-on-public-transit-in-the-u-s/ (Accessed August 17, 2020) [Google Scholar]
- 21.Kaltenmeier C, Malik J, Yazdani H, Geller DA, Medich D, Zureikat A, Tohme S. Refusal of cancer-directed treatment by colon cancer patients: Risk factors and survival outcomes. Am J Surg. 2020;S0002-9610(20)30226–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baker RB, Washington HA, Olakanmi O, et al. African American physicians and organized medicine, 1846-s1968: origins of a racial divide. JAMA. 2008;300(3):306–313. [DOI] [PubMed] [Google Scholar]
- 23.Duque RB. Black Health Matters Too... Especially in the Era of Covid-19: How Poverty and Race Converge to Reduce Access to Quality Housing, Safe Neighborhoods, and Health and Wellness Services and Increase the Risk of Co-morbidities Associated with Global Pandemics. J Racial Ethn Health Disparities. 2020. September 18. doi: 10.1007/s40615-020-00857-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Belachew AA, Reyes ME, Ye Y, raju GS, Rodriguez MA, Wu X, Hildebrandt MAT. Patterns of racial/ethnic disparities in baseline health-related quality of life and relationship with overall survival in patients with colorectal cancer. Qual Life Res 2020. July 3. doi: 10.1007/s11136-020-02565-8. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Couzin-Frankel J The long haul: some COVID-19 survivors are still sick months later. Doctors want to learn why and what they can do. Science 2020;369:614–617. [DOI] [PubMed] [Google Scholar]
- 26.https://marginalrevolution.com/marginalrevolution/2020/03/the-lasting-effects-of-the-1918-influenza-pandemic.html (Accessed August 24, 2020)
- 27.https://www.bls.gov/charts/employment-situation/civilian-unemployment-rate.htm (Accessed August 17, 2020)
- 28.Eisenberg A New York's safety-net hosptials were the front lines of the coronavirus. Now they're facing ruin. https://www.cssny.org/news/entry/structural-inequalities-in-new-yorks-health-care-system (Accessed August 17, 2020). [Google Scholar]
- 29.Dunker A, Ryden Benjamin E. How structural inequalities in New York's health care system exacerbate health disparities during the COVID-19 pandemic: A call for equitable reform. https://www.cssny.org/news/entry/structural-inequalities-in-new-yorks-health-care-system (Accessed August 17, 2020) [Google Scholar]
- 30.Carethers JM, Sengupta R, Blakey R, Ribas A, D’Souza G. Disparities in cancer prevention in the COVID-19 era. Cancer Prev Res 2020. September 17:canprevres.0447.2020. doi: 10.1158/1940-6207.CAPR-20-0447. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lara OD, O'Cearbhaill RE, Smith MJ, et al. COVID-19 outcomes of patients with gynecologic cancer in New York City. Cancer. 2020. July 30. doi: 10.1002/cncr.33084. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Phillips N, Park IW, Robinson JR, Jones HP. The Perfect Storm: COVID-19 Health Disparities in US Blacks. J Racial Ethn Health Disparities. 2020. September 23. doi: 10.1007/s40615-020-00871-y. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]


