Abstract
Objectives:
Little is known about emergency department (ED) utilization among the nearly 1 million older adults residing in assisted living (AL) settings. Unlike federally regulated nursing homes, states create and enforce AL regulations with great variability, which may affect the quality of care provided. The objective of this study was to examine state variability in all-cause and injury-related ED use among residents in AL.
Design:
Observational retrospective cohort study.
Setting and Participants:
We identified a cohort of 293,336 traditional Medicare beneficiaries residing in larger AL communities (25+ beds).
Methods:
With Medicare enrollment and claims data, we identified ED visits and classified those because of injury. We present rates of all-cause and injury-related ED use per 100 person-years in AL, by state, adjusting for age, sex, race, dual-eligibility, and chronic conditions.
Results:
Risk-adjusted state rates of all-cause ED visits ranged from 102.3 visits/100 AL person-years [95% confidence interval (CI) 95.3, 111.6/100 AL person-years] in New Mexico to 167.2 visits/100 AL person-years (95% CI 157.6, 179.6) in Rhode Island. The risk-adjusted rate of injury-related ED visits ranged from 19.8 visits/100 AL person-years (95% CI 18.3, 21.6) in New Mexico to 36.8 visits/100 AL person-years (95% CI 36.0, 38.1) in North Carolina.
Conclusions and Implications:
We observed significant variability among states in all-cause and injury-related ED use among AL residents. There is an urgent need to better understand why this variability is occurring to prevent avoidable visits to the ED.
Keywords: Emergency department, assisted living, injury
Emergency departments (EDs) are crowded, can cause infections, have long wait times, lack privacy, and are a poor alternative to routine primary care.1 ED visits among frail, older adults are associated with functional decline, nursing home admission, and mortality.2 Nearly 1 million older adults reside in assisted living (AL) settings throughout the United States.3 AL communities provide room and board and services to residents who need assistance with activities of daily living but not the level of care provided in nursing homes. Approximately 14% of AL residents had at least 1 ED visit within the past 90 days in 2016, which is similar to the rate of nursing home residents.3 Previous research indicates that many ED visits are avoidable through the early treatment and management of medical conditions4,5 and the prevention of injuries.6 Thus, rates of ED use in AL may be amenable to intervention.
Although previous studies have examined ED use among AL residents,3,5,7–10 none have addressed whether rates of ED use vary by state. Rates of ED use in AL are likely to differ by state based on numerous factors including differences in state regulations.8 Compared with nursing homes where regulations are generally federally mandated, states vary in their AL policies regarding staffing levels, admission/discharge criteria, training, the provision of third-party services, building design, and level of care provided.11 Identifying geographic variations in the rates of ED visits by AL residents is an important first step to ultimately identify whether individual state policies are associated with higher levels of visits to the ED.
Further, no studies have examined rates of injury-related ED visits among AL residents. Injuries in congregate settings are sometimes avoidable with adequate supervision and can be caused by a variety of mechanisms such as falls, resident-to-resident aggression, and burns.12 Injuries can result in decreased independence, chronic pain, and death.13 Therefore, the objective of this study was to characterize all-cause and injury-related ED use among AL residents in 2017 and how that varied across the country.
Methods
Data
We utilized data from the Medicare Master Beneficiary Summary File (MBSF), the inpatient Medicare Provider Analysis and Review files, outpatient Medicare claims, and nursing home Minimum Data Set assessments. To identify Medicare recipients residing in AL, we used an established methodology reliant on validated 9-digit zip codes reported in the MBSF that represented larger (25+ bed) ALs.14 To identify ED visits, we used the 2017 inpatient Medicare Provider Analysis and Review and outpatient Medicare claims data.15 For additional information on the identification of AL residents and ED visits, please see the supplementary material.
We used the 2016 MBSF to derive beneficiaries’ enrollment characteristics. The Chronic Conditions Warehouse segment of the MBSF details whether a beneficiary had a Medicare fee-for-service claim for treatment of chronic conditions. To calculate the person years spent in AL, we used the zip code History File merged with the Residential History File, which provides a chronological history of health services utilization for Medicare beneficiaries using Medicare claims and Minimum Data Set assessments.16 Additional information about the data and methods used for these analyses can be found in the Brown University Digital Repository (https://doi.org/10.26300/87mc-rk93).
Sample Selection
We identified a total of 439,272 Medicare beneficiaries with a zip code representing an AL community in the 48 contiguous states who were not in any other healthcare setting on December 31, 2016. Because utilization and claims data are not available for Medicare Advantage beneficiaries, we excluded AL residents with any Medicare Advantage coverage during calendar years 2016 and 2017, resulting in a sample of 293,336 Medicare fee-for-service beneficiaries. To compare our sample of AL residents with community residing older adults, we identified a sample of residents who were not in AL, an inpatient setting, or an nursing home on December 31, 2016, and without any Medicare Advantage enrollment during 2016 and 2017 (n = 34,391,052).
Measures
We classified whether each ED visit represented an injury using the New York University (NYU) algorithm.4,17 This algorithm provides the probability that an ED visit primary discharge diagnosis code falls into 8 categories based on the severity of the diagnosis.4 For additional information, please see the supplementary material.
We controlled for diagnoses of chronic conditions, which included anemia, atrial fibrillation, cancer, chronic kidney disease, chronic obstructive pulmonary disease, depression, diabetes, heart failure, hyperlipidemia, hypertension, ischemic heart disease, stroke, and Alzheimer’s disease and related dementia (ADRD). We additionally categorized the number of these chronic conditions into 4 groups (<2, 2–3,4–5, and 6+) to account for comorbidity. We categorized age into five 10-year age groups (≤64, 65–74, 75–84, 85–94, and 95+). We defined dual eligibility as beneficiaries who were eligible for Medicare and Medicaid at the end of December 2016.
Analysis
We compared individual characteristics among all residents in ALand those who had an all-cause visit or an injury-related ED visit during the past year. We calculated the risk-adjusted rates of all-cause and injury-related ED use by state, as the ratio of observed events over expected events in each state multiplied by the national rate. We used the bootstrap resampling method to estimate the 95% confidence intervals of the adjusted rates and compare our estimates with the national rate.
Rates were expressed as the number of visits per 100 person years in AL. We mapped the state variability in adjusted all-cause and injury-related ED visits for the AL sample. In addition, we performed analysis to examine whether state variability simply reflects differences in pr actice patterns and access to hospitals. We plotted risk-adjusted state rates of ED use in a community-dwelling sample of Medicare beneficiaries against the risk-adjusted state rates of ED use among our sample of AL residents. We conducted data analysis and visualization using SAS v 9.4 (SAS Institute, Cary, NC) and ArcMap v 10.6 (ESRI, Redlands, CA).
Results
Table 1 displays the demographic characteristics of AL residents in our cohort. A total of 142,468 AL residents made 312,876 ED visits during the year. Approximately 49% of the cohort visited the ED at least 1 time during the year. Seventeen percent of residents visited the ED for injury at least once during 2017. Residents who visited the ED for an injury were more likely to be diagnosed with ADRD than residents who did not have an ADRD diagnosis: approximately 42% of residents that had an injury-related visit had ADRD. Residents with a greater number of chronic conditions were also more likely to have an injury-related ED visit: approximately 29% of residents with 6 or more chronic conditions visited the ED for an injury.
Table 1.
Sample Characteristics, Overall and by Type of ED Visit (2017)
| Characteristics | Medicare Beneficiaries Residing in AL (%) (n = 293,336) | Medicare Beneficiaries Residing in AL with at Least 1 All-Cause ED Visit (48.6%) (n = 142,468) | Medicare Beneficiaries Residing in AL with at Least 1 Injury-Related Visit (16.9%) (n = 49, 508) |
|---|---|---|---|
| Age group (%) | |||
| <65 y | 7.3 | 6.7 | 6.3 |
| 65–74 y | 14.7 | 10.7 | 9.4 |
| 75–84 y | 23.5 | 21.7 | 20.5 |
| 85–94 y | 43.5 | 48.1 | 49.6 |
| 95+ y | 11.0 | 12.7 | 14.3 |
| Sex (%) | |||
| Male | 33.9 | 32.5 | 29.6 |
| Female | 66.2 | 67.5 | 70.4 |
| Race (%) | |||
| White | 91.8 | 92.6 | 93.8 |
| Black | 3.8 | 3.8 | 2.9 |
| Hispanic | 1.9 | 1.8 | 1.6 |
| Other | 2.5 | 1.9 | 1.7 |
| Dually eligible for Medicare and Medicaid+ (%) | 18.1 | 20.2 | 19.9 |
| Chronic conditions (%) | |||
| Alzheimer’s disease and related dementias | 30.3 | 37.1 | 42.1 |
| Anemia | 33.2 | 40.2 | 41.5 |
| Atrial fibrillation | 16.1 | 20.4 | 20.5 |
| Cancer | 9.9 | 11.2 | 10.6 |
| Chronic kidney disease | 30.0 | 37.0 | 35.9 |
| Chronic obstructive pulmonary disease | 15.7 | 20.9 | 19.9 |
| Depression | 28.0 | 34.2 | 37.8 |
| Diabetes | 26.9 | 31.2 | 30.0 |
| Heart failure | 24.5 | 32.2 | 31.6 |
| Hyperlipidemia | 50.1 | 54.4 | 53.6 |
| Hypertension | 70.7 | 78.8 | 79.1 |
| Ischemic heart disease | 36.4 | 44.5 | 44.0 |
| Stroke | 6.3 | 8.2 | 8.6 |
| Fewer than 2 chronic conditions*,† | 23.5 | 15.0 | 15.0 |
| 2-3 Chronic conditions*,† | 30.3 | 27.5 | 27.8 |
| 4-5 Chronic conditions*,† | 25.3 | 28.4 | 28.3 |
| 6+ Chronic conditions*,† | 20.9 | 29.1 | 29.0 |
MedPAR, Medicare Provider Analysis and Review.
Data come from the 2016 and 2017 Medicare Master Beneficiary Summary File and Chronic Conditions, MedPAR file, and Medicare outpatient claims. Residents were in assisted living on December 31, 2016.
Columns are not mutually exclusive.
As of December 31, 2016.
Condition counts are created from aforementioned listed conditions.
Figure 1 displays the geographic variability in risk-adjusted allcause, and injury-related ED visits. Please see Supplementary Table 1 for the estimates and confidence intervals (CIs). The national average risk-adjusted rate was 135.3 visits/100 AL person-years. The risk-adjusted state rates of all-cause visits ranged from 102.3 visits/100 AL person-years (95% CI 95.3,111.6) in New Mexico to 167.2 visits/100 AL person-years (95% CI 157.6,179.6) in Rhode Island. The 5 states with the highest rates of risk-adjusted ED visits were Rhode Island, Wyoming, Arkansas, Oregon, and Massachusetts. The 5 states with the lowest rates were South Dakota, Utah, New Jersey, Maryland, and New Mexico.
Fig. 1.
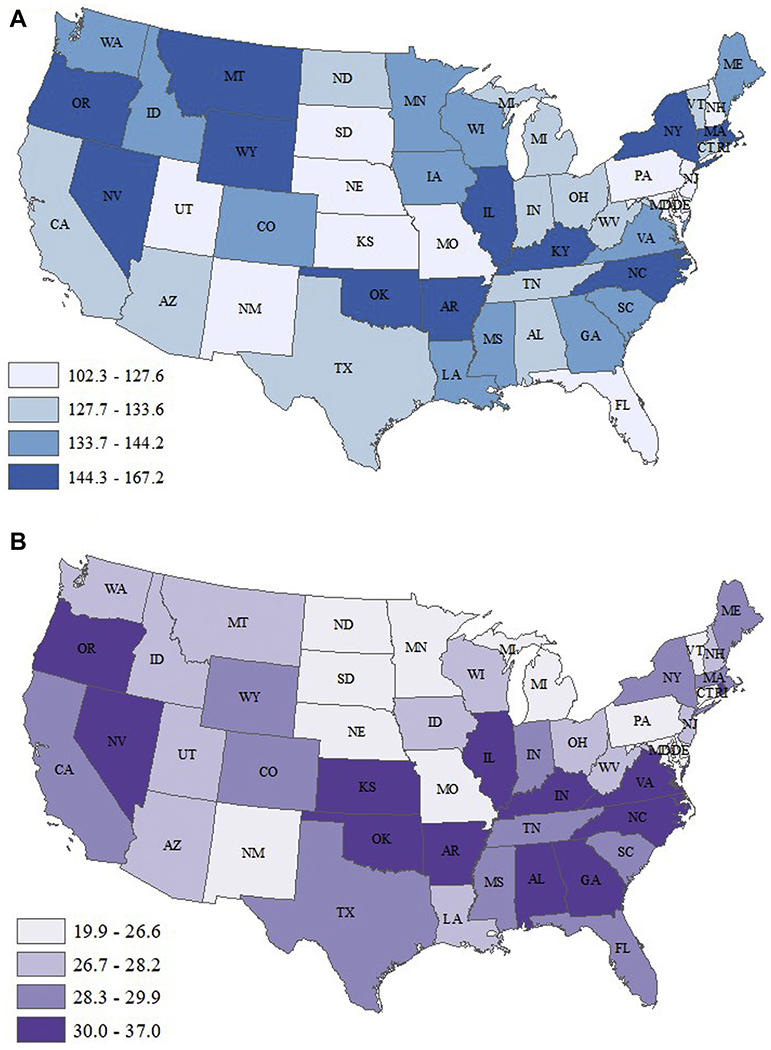
(A) Adjusted* state rates of ED visits per 100 AL person-years, presented by quartile (2017). (B) Adjusted* state rates of injury-related ED visits per 100 AL person-years, presented by quartile (2017). Data come from the 2016 and 2017 Medicare Master Beneficiary Summary File and Chronic Conditions segment, the inpatient MedPAR file, and the Medicare outpatient claims. Categories represent quartiles. *Rate adjusted for age, race, sex, dual-eligibility, and chronic conditions.
The national average rate of risk-adjusted injury-related visits was 28.5 visits/100 AL person-years, and states’ risk-adjusted rates of injury-related visits ranged from 19.8 visits/100 AL person-years (95% CI 18.3,21.6) in New Mexico to 36.8 visits/100 AL person-years (95% CI 26.4, 29.0) in North Carolina. The 5 states with the highest rates were North Carolina, Oklahoma, Rhode Island, Kansas, and Georgia. The 5 states with the lowest rates were Vermont, Maryland, North Dakota, South Dakota, and New Mexico. The lower and upper bounds of the CIs for these aforementioned states did not contain the national rate, suggesting significant state variability.
We also examined whether state rates differed for residents in the community compared to AL residents. Rates of ED use in the community sample were lower than the sample in AL; the unadjusted rate of visits was 59.8 visits/100 community person-years. The Pearson correlation coefficient between the 2 measures was not statistically significant (P > .10), suggesting that the state variability in ED visits was not merely a reflection of geographic variations in access and practice patterns. Figure 2 provides a scatter plot comparing risk-adjusted community rates to AL rates.
Fig. 2.
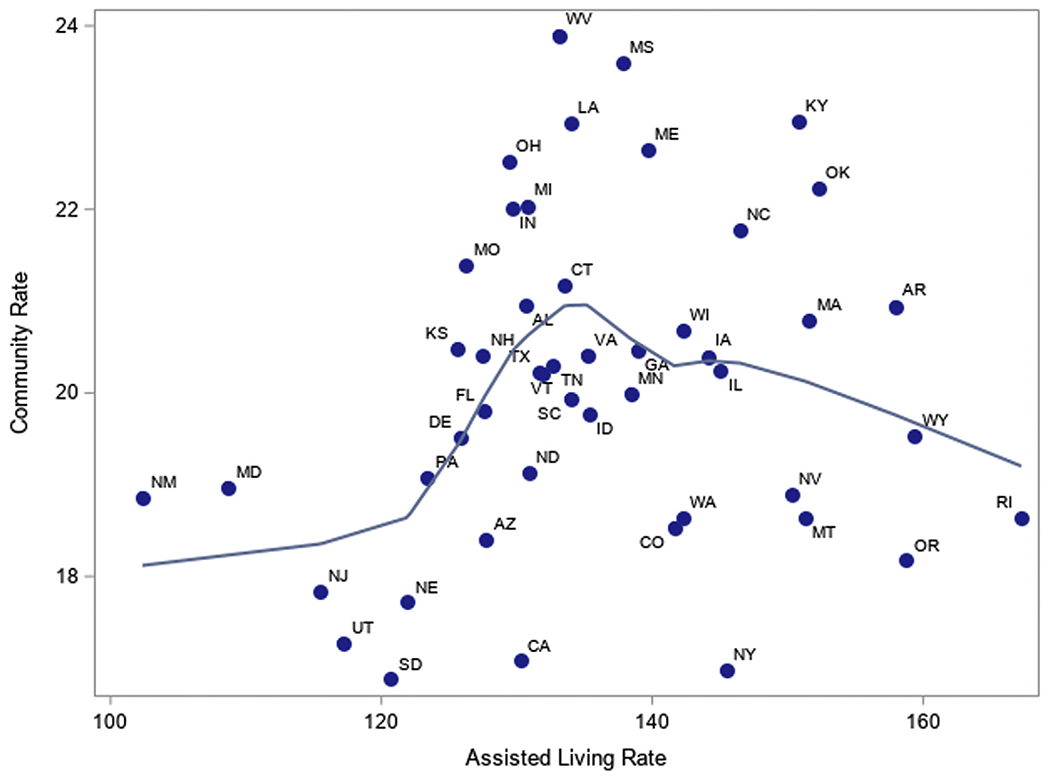
Adjusted* rate of ED visits among all community residing Medicare beneficiaries per 100 person-years compared with AL residents. *Rates adjusted for age, race, sex, dual-eligibility, and chronic conditions. Data come from the 2016 and 2017 Medicare Master Beneficiary Summary File and Chronic Conditions, the inpatient Medicare Provider Analysis and Review, and the Medicare outpatient claims. The line represents a loess regression curve that best fits the data.
Discussion
Our study observed significant variations in state rates of all-cause and injury-related ED use among AL residents after adjusting for resident characteristics and comparing rates with the community. There are many mechanisms that may be attributable to the state variation observed (eg, state regulations, resident populations, market factors). For example, compared with nursing homes that require around-the-clock nursing, only 24 states require that a licensed nurse is on staff.18 Higher staffing levels are associated with lower rates of hospitalization in long-term care settings.19,20 Rhode Island, Nevada, Oregon, and Arkansas have some of the highest risk-adjusted rates of ED visits in the nation and do not have a requirement for the presence of a licensed nurse.18 For example, North Carolina has no specifications for awake, overnight staffing,18 which may be related to high rates of injury-related visits. Injuries in nursing homes occur late at night more frequently than they do in the community, which has been attributed to reduced nightly staffing levels.21
In addition, admissions and discharge criteria vary. For example, New Mexico, a state with low rates of ED use, does not allow residents to be admitted to AL if they require more than 24 hours of skilled nursing care.22 Rhode Island, a state with one of the highest rates of ED use, allows residents to be exempt from discharge requirements if their skilled nursing needs are expected to last fewer than 21 days. The state also grants extensions to this rule.22
States also differ in whether they allow the use of hospice services. Hospice use is associated with lower rates of ED during the last 6 months of life because symptom management is provided at home.23 Utah, a state with lower rates of ED use, allows ALs to admit and retain residents who receive hospice care. One study found that AL residents in Utah spend the longest time in ALs before death compared with residents in other states,24 which may reflect a greater focus on palliative care provided in the AL. States also differ in the ways they license AL communities, often reflecting both differences in the intensity of services provided and the acuity levels of the residents.25 Finally, states vary in their enforcement of regulations, which may differentially affect compliance.26
Our study is subject to limitations. First, we only included residents who were enrolled in traditional Medicare; thus, we cannot generalize our findings to residents who were enrolled in Medicare Advantage or not enrolled in Medicare. Second, our study only included a sample of Medicare beneficiaries residing in ALs with a licensed capacity to serve 25+ residents. Therefore, we cannot make generalizations to smaller ALs. However, previous research suggests that unadjusted ED utilization rates do not differ by AL size.27 Nonetheless, understanding ED use among smaller ALs, and how that may differ from larger ALs, is an important area for further exploration. Third, we were not able to examine AL community-level characteristics that may play a role in the variability in ED use. For example, many ALs require transport to the ED despite the severity of a fall.28 We were also not able to observe other state-level differences in practice patterns that may also likely play a role in the variability. Maryland, for example, operates on a global hospital budget that disincentivizes the use of the ED.29 Finally, we present a cross-section of data and do not formally examine the effects of state regulations, enforcement, or market factors on ED use. This is an important area for future study.
Conclusions and Implications
In conclusion, we found significant variability in rates of ED use among residents in the AL setting across the country. The reasons for these state variations merit further investigation.
Supplementary Material
Acknowledgments
This work was supported by research awards from the National Institute on Aging (R01 AG057746), the Veterans Health Administration (CDA 14–422) and the AHRQ T32 training grant (T32HS000011).
Footnotes
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs, the National Institutes of Health, or the United States government.
References
- 1.Liang SY, Theodoro DL, Schuur JD, Marschall J. Infection prevention in the emergency department. Ann Emerg Med 2014;64:299–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nagurney JM, Fleischman W, Han L, et al. Emergency department visits without hospitalization are associated with functional decline in older persons. Ann Emerg Med 2017;69:426–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harris-Kojetin L, Sengupta M, Lendon J, et al. Long-term care providers and services users in the United States: Data from the National Study of Long-Term Care Providers, 2015-2016. Vital Health Stat Ser 3 Anal Epidemiol Stud 2019; 43:1–88. [PubMed] [Google Scholar]
- 4.Ballard DW, Price M, Fung V, et al. Validation of an algorithm for categorizing the severity of hospital emergency department visits. Med Care 2010;48: 58–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abate B, VanGraafeiland B. Improving education and communication in an assisted living facility to reduce avoidable emergency department transfers: A quality improvement project. J Gerontol Nurs 2019;45:23–29. [DOI] [PubMed] [Google Scholar]
- 6.Goldberg EM, Marks SJ, Ilegbusi A, et al. GAPcare: The geriatric acute and post-acute fall prevention intervention in the emergency department: Preliminary data. J Am Geriatr Soc 2020;68:198–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gillespie SM, Wasserman EB, Wood NE, et al. High-intensity telemedicine re-duces emergency department use by older adults with dementia in senior living communities. J Am Med Dir Assoc 2019;20:942–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah MN, Wasserman EB, Gillespie SM, et al. High-intensity telemedicine de-creases emergency department use for ambulatory care sensitive conditions by older adult senior living community residents. J Am Med Dir Assoc 2015;16: 1077–1081. [DOI] [PubMed] [Google Scholar]
- 9.Sharpp TJ, Young HM. Experiences of frequent visits to the emergency department by residents with dementia in assisted living. Geriatr Nurs 2016; 37:30–35. [DOI] [PubMed] [Google Scholar]
- 10.Wiener JM, Feng Z, Coots LA, Johnson R. What is the effect of dementia on hospitalization and emergency department use in residential care facilities. Washington, DC: US Department of Health and Human Services, 2014. ASPE. Available at: https://aspe.hhs.gov/basic-report/what-effect-dementia-hospitalization-and-emergency-department-use-residential-care-facilities. Accessed December 1, 2016. [Google Scholar]
- 11.Carder PC. State regulatory approaches for dementia care in residential care and assisted living. Gerontologist 2017;57:776–786. [DOI] [PubMed] [Google Scholar]
- 12.Bugeja L, Woolford MH, Willoughby M, et al. Frequency and nature of coroners’ recommendations from injury-related deaths among nursing home residents: A retrospective national cross-sectional study. Inj Prevent 2018;24: 418–423. [DOI] [PubMed] [Google Scholar]
- 13.Kelley-Quon L, Min L, Morley E, et al. Functional status after injury: A longi-tudinal study of geriatric trauma. Am Surg 2010;76:1055–1058. [PMC free article] [PubMed] [Google Scholar]
- 14.Thomas KS, Dosa D, Gozalo PL, et al. A methodology to identify a cohort of Medicare beneficiaries residing in large assisted living facilities using admin-istrative data. Med Care 2018;56:e10–e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaskie B, Obrizan M, Cook EA, et al. Defining emergency department episodes by severity and intensity: A 15-year study of Medicare beneficiaries. BMC Health Serv Res 2010;10:173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Intrator O, Hiris J, Berg K, et al. The residential history file: Studying nursing home residents’ long-term care histories. Health Serv Res 2011;46:120–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnston KJ, Allen L, Melanson TA, Pitts SR. A “Patch” to the NYU emergency department visit algorithm. Health Serv Res 2017;52:1264–1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Trinkoff AM, Yoon J, Storr CL, et al. Residential long-term care regulations: Comparison between nursing homes and assisted living facilities. Nurs Outlook 2019;68:114–122. [DOI] [PubMed] [Google Scholar]
- 19.Intrator O, Zinn J, Mor V. Nursing home characteristics and potentially pre-ventable hospitalizations of long-stay residents. J Am Geriatr Soc 2004;52: 1730–1736. [DOI] [PubMed] [Google Scholar]
- 20.Stearns SC, Park J, Zimmerman S, et al. Determinants and effects of nurse staffing intensity and skill mix in residential care/assisted living settings. Gerontologist 2007;47:662–671. [DOI] [PubMed] [Google Scholar]
- 21.Dubucs X, de Souto Barreto P, de Mazieres CL, et al. The temporal trend in the transfer of older adults to the emergency department for traumatic injuries: A retrospective analysis according to their place of residence. J Am Med Dir Assoc 2019;20:1462–1466. [DOI] [PubMed] [Google Scholar]
- 22.Carder PC, O’Keeffe J, O’Keeffe C. Compendium of Residential Care and Assisted Living Regulations and Policy: 2015 Edition Executive Summary. 2015. June/15/2015. Available at: https://aspe.hhs.gov/basic-report/compendium-residential-care-and-assisted-living-regulations-and-policy-2015-edition. Accessed October 9, 2019.
- 23.Smith AK, McCarthy E, Weber E, et al. Half of older Americans seen in emergency department in last month of life; Most admitted to hospital, and many die there. Health Affairs 2012;31:1277–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thomas KS, Belanger E, Zhang W, Carder P. State variability in assisted living residents’ end-of-life care trajectories. J Am Med Dir Assoc 2020;21:415–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Street D, Burge S, Quadagno J. The effect of licensure type on the policies, practices, and resident composition of Florida assisted living facilities. Gerontologist 2009;49:211–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaskie B, Kingsley K. State Enforcement Actions Pertaining to Persons with Dementia Residing in Assisted Living Facilities. Washington, DC: Alzheimer’s Association National Public Policy Office; 2009. [Google Scholar]
- 27.Caffrey C, Sengupta M. Variation in residential care community resident characteristics, by size of community: United States, 2016. NCHS Data Brief, no 299. Hyattsville, MD: National Center for Health Statistics; 2018. [PubMed] [Google Scholar]
- 28.Williams JG, Bachman MW, Lyons MD, et al. Improving decisions about transport to the emergency department for assisted living residents who fall. Ann Intern Med 2018;168:179–186. [DOI] [PubMed] [Google Scholar]
- 29.Patel A, Rajkumar R, Colmers JM, et al. Maryland’s global hospital budgets—Preliminary results from an all-payer model. N Engl J Med 2015;373: 1899–1901. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


