Abstract
Despite being considered “standard of care” by many organizations, fertility and reproductive health communications and counseling practices remain inconsistent for adolescents and young adults (AYAs) newly diagnosed with cancer and during survivorship. One factor known to affect how information is provided and received in the medical setting is health literacy. Providers should consider health literacy to optimize reproductive health communication with AYAs as they cope with their diagnosis, understand what it means for their future, process information about treatment options, learn about their potential harmful effects on fertility, make quick decisions about fertility preservation, and navigate a future family planning course. Thus, the objectives of this manuscript are to: a) summarize literature on reproductive health literacy; b) describe health literacy frameworks; c) examine ways to assess health literacy; and d) identify ways to enhance clinician-patient communication in the AYA oncofertility setting.
Keywords: Adolescents, Young adults, Health Literacy, Cancer, Reproductive health
An expanding body of literature has focused on fertility impairment after cancer therapy and its negative psychosocial implications. Although there are an increasing number of technologies available for fertility preservation and assisted reproduction, access to timely and comprehensive fertility and reproductive health care still remains a challenge in many cancer centers across the United States and beyond. Despite being considered “standard of care” by many organizations,1,2 fertility and reproductive health counseling practices and communications remain inconsistent for adolescents and young adults (AYAs) newly diagnosed with cancer and during survivorship.3
Research shows health care providers, parents, and patients often experience difficulties in communicating with one another about fertility and reproductive health in the cancer setting.4 Even when discussions do occur, there are frequent reports of: 1) discordance between what patients/families are told by providers and what they perceive (e.g. about level of infertility risk5); 2) discordance between adolescents’ reproductive attitudes/goals and those of their parents6,7; 3) poor recall of information about fertility and reproductive health among AYAs and families8; 4) uncertainty about fertility status and misconceptions about various reproductive health topics9 (e.g. risk of future offspring having cancer); 5) overall dissatisfaction with reproductive communications regarding fertility, contraception, and sexual health; and 6) scarce printed and digital educational resources. Limited research has been conducted to clarify why these gaps exist or to examine how these issues impact reproductive health decision-making and outcomes.10
One factor known to affect how information is provided and received in the medical setting is health literacy. Health literacy is defined by the U.S. Department of Health and Human Services as the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.11 Other definitions further depict health literacy as a constellation of essential skills required to understand and assimilate information, and perform health-related tasks and behaviors. For example, health literacy may affect a patient/parent’s ability to understand the current and future impact of cancer on sperm production or ovarian reserve, generate questions to ask a reproduction specialist, make decisions about fertility preservation options, or access and understand resources for supplemental information and/or guidance. Health literacy may also impact a patient’s understanding of medical terms related to reproductive health; for instance, a patient may incorrectly perceive “sterile” to mean “clean”12 or believe that if there is need to preserve fertility, then contraception is not needed.
Several factors affect health literacy including13,14: 1) baseline knowledge of providers and patients and communication skills of providers and patients/families; 2) patient age, developmental stage and cognitive capacity; 3) cultural and religious perspectives of providers and patients; 4) literacy of patients/families; and 5) competing psychological/emotional demands related to increasingly complex health care situations. Furthermore, individuals across any socioeconomic strata (high or low education or income) are at risk for low health literacy due to the many system demands placed on them once they become immersed in a health care system. For AYAs with cancer, the potential for low health literacy is coupled with the need to quickly gain understanding of diagnosis and treatment as well as fertility/infertility, preservation, and contraception. AYAs with cancer are often faced with making decisions about fertility preservation and family planning in a very short window of time (24–48 hours), in the setting of physical/psychological distress related to a new cancer diagnosis, and often at ages/ developmental stages where capacity for future oriented thinking is limited.15
Providers should consider health literacy in order to optimize reproductive health communication with AYAs as they cope with their diagnosis, understand what it means for their future, process information about treatment options, learn about their potential harmful effects on reproduction, make quick decisions about fertility preservation, and navigate a future family planning course. Thus, the objectives of this manuscript are to: a) summarize literature on reproductive health literacy, b) describe health literacy frameworks, c) examine ways to assess health literacy, and d) identify ways to enhance provider-patient communication in the AYA oncofertility setting.
Health literacy models and communication frameworks
A number of health literacy conceptual theories, models, and frameworks have been developed (Table 1) which can be used as the basis for the development and validation of health literacy measures (Table 2).16–19 They include different moderator factors that influence the development of health literacy such as age, education level, and socioeconomic status and different mediator factors which influence patient’s relationships between health literacy and health outcomes.19 These can be divided into personal factors such as attitudes, beliefs systems, personal experience, and motivations and external factors such as support systems and environmental factors. Unfortunately, no unifying framework exists and the currently available frameworks use various definitions of health literacy so they are not directly comparable.19,20 Nutbeam’s Model of Health Literacy (2000), offers an attractive empowerment approach because of its three progressive levels of health literacy: functional/basic, interactive and critical thinking (Table 1).21
Table 1.
Health Literacy Conceptual Frameworks
| Health Literacy Conceptual Framework/Theory | Main Theoretical Concepts of Framework |
|---|---|
| Baker Model 83 | This model identifies moderators and mediators and emphasizes the role of prior health knowledge. |
| Health literacy, social support, and health Framework 84 | This framework focuses on identifying intermediate factors through which health literacy affects outcomes such as disease knowledge, health risk behavior and compliance with medication. |
| Manganello Framework 85 | This framework includes modifiable factors which may influence an adolescents’ health literacy. |
| Institute of Medicine (IOM) Health Literacy Framework 86 | This framework focuses on culture and society, education and health system as factors in the development of health literacy skills which can be modified. |
| Nutbeam Conceptual Model of Health Literacy 21 | This model adopts an empowerment approach that identifies three progressive levels of health literacy which include basic/functional skills (ability to read and write); communication/interactivity literacy (ability to coordinate social skills and literacy and participate in communication; critical literacy (ability to evaluate information that has been given). |
| Media Literacy conceptual Framework 87 | This framework uses the ability to critically evaluate media messages across a number of different platforms. |
| Expectancy theory 88,89 | Patients engage in certain behaviors based on three determinants which include expectancy (the amount of effort in achieving an outcome; instrumentality (the intrinsic or extrinsic rewards a person gets when they achieve their goals and valence (the value a patient places on the outcome). |
| Expanded Model of Health Literacy 90 | This model is characterized by four domains – fundamental literacy (the skills required in reading, speaking, writing and interpreting information); science literacy (the level of understanding of science and technology); civic literacy (patients understanding on public issues which may influence decision making); and cultural literacy (to be ability to recognise and use collective beliefs and customs to interpret information). |
| Concept Analyses of Health Literacy 91 | This model uses concept analysis to clarify attributes (reading, numeracy, comprehension, decision making and capacity to use the information, antecedents (literacy and health related experience) and consequences of health literacy (improvements in health outcomes, reduce health costs and reduced in and outpatient admissions). |
| Media Health Literacy Theoretical Framework 92,93 | Two different models which combine health and media literacy together and include domains such as identification, influences, analysis, understanding and action. |
| Outcome Expectation from Social Cognitive Theory 94 | Asserts that behavior is shaped by individuals’ anticipation of consequence and rewards. |
| Combination of Interpretation Model and Social Cognitive Theory 95 | Asserts that behavior is a product of interaction between cognitive and social environmental influences. |
| Causal Pathway Model 96 | This model focuses on pathways between health literacy and outcomes influenced by access and uptake of health care, patient clinician relationship, and patient self-care. |
| Distributed Health Literacy Model 24 | This model utilizes a patient’s social networks and family caregivers as a potential resource for managing one’s health, communicating with health professionals, and making health decisions. |
Table 2.
Measures to Assess Health Literacy
|
Considerations at the time of cancer diagnosis
Patient perspective/Parent perspective
Even without a cancer diagnosis, reproductive health literacy of AYAs is limited,22,23 and most AYAs have not discussed reproductive health values with their parents/caregivers.7,24 Establishing health literacy about fertility impairment and preservation not only requires receiving and understanding the information provided but also thinking critically about this information in order to make decisions21,24 about possible future scenarios within a short timeframe. Prior to a cancer diagnosis, many AYAs are developing emotional and cognitive maturity and are starting to make independent decisions. When initially diagnosed with cancer, AYA patients become increasingly reliant on their parents/partners to guide discussions and share in decision-making.25 A recent model of health literacy supports distribution of health information and decision-making among patients and their families in order to optimize information acquisition and utilization.24 This framework is highly relevant at the time of cancer diagnosis when most AYA patients hear information and make decisions collaboratively with their parents/partners.26
There is limited research dedicated to reproductive health literacy of AYA patients at the time of a cancer diagnosis. Research has shown adolescents and their parents inaccurately report and estimate their infertility risk within one week of the discussion, highlighting significant barriers to adequate healthy literacy.5 Both male and female AYAs have discordant views from their parents on the subject of fertility preservation; current research shows parents are poor predictors of their child’s wishes and are less likely to prioritize future biological children in comparison to AYAs.6,7,27 AYA males are more likely to attempt sperm-banking based on provider or parental recommendation28,29 and parents, in turn, rely on informed providers for comprehensive information and advice.30 In comparison, adolescent females tend to have thought more about future parenthood at the time of diagnosis and therefore show greater interest in fertility preservation; however, cost and the need to delay treatment have been shown to be barriers.31–33 Efforts to improve family/caregiver health literacy can favorably modify health outcomes.34 In one study, parental self-efficacy to coordinate/facilitate sperm banking was associated with increased likelihood to pursue fertility preservation.29 These studies underscore the importance of considering both the patient and parents’ health literacy during fertility consultations.
Providers/system perspective
Although there is a consensus as to the timing and level of fertility preservation information that should be provided to patients by a clinician at the time of diagnosis,35 poor clinician knowledge (e.g. regarding impacts of cancer treatment on future fertility, fertility preservation options and logistics to completion), low clinician confidence or discomfort, alongside clinician biases and misconceptions all negatively impact fertility discussions.36–38 Clinicians have reported a lack of education and a desire for further guidance in communicating with patients about fertility,39–42 indicating a need for clinician training and guidelines to aid in clinician health literacy. There is also ambiguity at times as to whose role it is to assist the patient in navigating oncofertility care given the multi-disciplinary approach that is required. Patient care navigators can be useful assets to the clinical team, in coordinating services, informing patients of treatment options and ensuring timely referral for fertility preservation.43,44
There is a paucity of research into how clinicians consider patient health literacy when communicating risk of infertility and fertility preservation options at the time of a cancer diagnosis. Oncology clinicians perceive the emotional distress of patients and parents/caregivers of pediatric patients to hinder fertility risk information comprehension37 and thus this factor may impact health literacy.45 Positive clinician-patient rapport and sound clinician communication skills may improve interactions with AYA cancer patients and assist in health literacy.46,47 Taking a patient-centered approach and providing oncofertility written materials and age appropriate information may assist with effective information communication.43
Considerations during and after oncological treatment
During and after the completion of cancer therapy, patients and families often have questions about reproductive health and the possibility for future fertility. To provide accurate counseling regarding infertility risk, providers may discuss cancer therapy exposures associated with infertility (e.g. alkylating agents, radiation to the gonads), offer opportunities for assessment of fertility status (e.g. hormone levels, semen analysis, or antral follicle count), and present potential options for future family-building. These discussions often require patients to have some underlying knowledge of reproductive processes including pubertal development, and related terminology, therefore health literacy is particularly important to consider among both patients and parents. Among adult women in the general population, health literacy is related to reproductive health knowledge,48 and increased health literacy has been associated with an understanding of fertility and assistive reproductive technology.49 While there has been little research exploring reproductive health literacy among survivors of childhood cancer, or their parents, there are several factors that may influence health literacy in this population.
Among survivors of childhood cancer, health literacy may be influenced by individual factors, patient age and developmental stage, and the receipt of neurotoxic cancer therapy. Individual factors can include functional literacy and educational attainment; among healthy adolescents, educational attainment and academic success are positively associated with health literacy.50 Educational attainment and academic milestones are often delayed among survivors due to cancer diagnosis and cancer treatment.51 Understanding different levels of risk for infertility can be challenging and, depending on the value placed on fertility by the patient or parent, emotions can also impact understanding of risk. The emotions attached to an outcome may influence the reaction to risk communication and health decision-making.52 Infertility is a highly emotional and distressful outcome of some pediatric cancers53; education regarding infertility risk should address the emotional distress related to potential infertility and incorporating low health literacy approaches may be helpful.
Age and developmental stage will influence survivors’ understanding of reproductive health and desire for information about their potential future fertility. Survivors and their parents may be more interested in discussing infertility during later adolescent years and near the time of transition to adult healthcare. Male and female AYA survivors often report inaccurate perceptions of risk for infertility after treatment54–56 and desire repeated and more comprehensive information regarding their reproductive health.57 As AYA cancer survivors transition from a pediatric-centered institution to the adult healthcare system, they often continue to have questions about their reproductive health.58 Survivors who received neurotoxic therapy may have poorer health literacy due to their neurocognitive deficits.59 Cranial radiation, intrathecal chemotherapy, and brain tumor/brain surgery are known to impact attention and executive functioning.59,60 Survivors with neurocognitive deficits may require interventions using low health literacy models to ensure they understand their reproductive health risks.
How to assess and improve health literacy
A number of countries have prioritized the availability of health literacy measures and health system awareness of health literacy.61,62 Clinicians agree the identification of health literacy is important in clinical practice but no consensus exists on a ‘gold standard’ measure and what components of health literacy should be tested. The literature identifies numerous formal and informal ways to assess health literacy. For example, some tools are currently available that offer significant correlations between the measure and a value of individual patients’ health literacy.20 However these tools mainly assess reading proficiency and do not comprehensively assess other components of health literacy which include print literacy (reading, writing, numeracy); communication (listening, speaking and negotiating;) and information seeking and eHealth (navigating health services).18 Many tools are emerging in languages other than English and Spanish.63,64 Table 2 provides examples of measures of health literacy, based on theoretical frameworks/models that may be useful in developing communication and educational patient-centered information.
An informal approach that has been increasingly used to assess health literacy are the Single Item Literacy Screener (SILS) measures.65,66 These items can be easily incorporated into patient’s assessment intake forms. Examples of questions are: How would you rate your ability to read?; How often do you need to have someone help you when you read instructions, pamphlets, or other written material from your doctor or pharmacy?; How confident are you filling out medical forms by yourself?
Various strategies can be implemented at a local national and international level to improve the development and implementation of health literacy measures to improve patient education (Tables 2 and 3).16–18,67 It is also important to look at organizational health literacy barriers that reduce the implementation of these measures once they have been developed and validated, such as a lack of commitment and priority, work place culture not supporting implementation, lack of training, lack of time and lack of awareness or need.16,17 The American Health Research and Quality has created a helpful resource toolkit: https://www.ahrq.gov/health-literacy/quality-resources/tools/literacy-toolkit/index.html Another strategy for improving literacy is re-educating patients and parents/caregivers at different time points (with the patient’s consent), as patients’ needs and circumstances change over time. This strategy has the added benefit of providing multiple opportunities to support families and validate what they already know.
Table 3.
Options to Enhance Literacy
|
Decision support tools, resources, and training
Healthcare providers and healthcare systems can assess and optimize patient and parent understanding of personal risk for infertility by proactively addressing health literacy in their plans for patient education (Table 3). However, health literacy is not just education – it requires an assessment of comprehension and the ability to use the information and make critical decisions.61 Koh and colleagues describe The Arc of Health literacy and recommend clinicians “assume” patients may not understand unless proven otherwise and they suggest the use of the Teach Back method and language that welcomes questions.68 An example of this would be “I’ve just given you a lot of information about your contraception options – what questions do you have? Can you tell me how you will explain what you have learned to your partner?”
By nature of the technical nomenclature commonly used within the reproductive health field (e.g., oocyte, premature ovarian failure, pre-implantation genetic testing) this area of cancer care is especially steeped in communication complexities. As such, deconstructing (breaking down) or substituting these difficult terms is key for improved communications. Oncofertility patient educational materials are recommended as supplements to the initial fertility consultations. However, a minority of clinicians routinely provide fertility preservation patient educational materials to patients14 and there are discrepancies in the quality of materials available.69 As such, there is a need for clinicians to be aware of how to access appropriate patient education resources, while considering preferred information type/language, and level of health literacy.70 Moreover, further rigor in the development of these resources is required moving forward, to ensure consistency and clarity in information provision. Proposed strategies and steps to enhance literacy in the reproductive setting are outlined in Table 3.
Systems like the Oncofertility Consortium are well positioned to create working groups of experts in the field to develop materials that are mindful of health literacy. These materials can take the complex information around fertility/infertility and fertility preservation and reduce them into digestible components that can be used to make an actionable decision. Key concepts can be identified that the patient/parent should understand. Materials used in education sessions should be developed using recommended developmental processes and should be pilot tested.17 In general, less jargon and less complex terminology should be used, more attention should be given to common faulty assumptions, and reading level and numeracy skills should be accommodated.17,18,19 Once finalized, the Oncofertility Consortium could disseminate the materials throughout their global network of providers, thus improving provider and patient communication in a consistent amplified manner.
Decision support tools can also be utilized to guide fertility preservation clinician-patient conversations and assist decision-making processes at diagnosis and after oncological treatment.71 Clinician administered decision trees allow clinicians to select appropriate preservation options; considering factors such as urgency to commence oncological treatment, fertility risk and patient’s desire for family planning.72 Decision aids used at the time of diagnosis can augment reproductive health literacy and should not only include evidence-based educational materials but must incorporate values clarification exercises to stimulate discussion of a previously unaddressed topic.73 Parents have responded positively to decision aids at the time of diagnosis when they otherwise would have been too focused on immediate cancer diagnosis and treatment.73 In a recent study, parents and AYA males described that the use of a family-centered decision aid promoted conversation and consideration of future fertility goals.74 The use of this framework of distributed health literacy is more likely to limit decisional regret.9 Preliminary findings from randomized controlled trials investigating the utility of online fertility preservation decision aids, either alone75,76 or combined with care navigation,77 in comparison to standard care (fertility consult, counselling or brochure), indicate that decision aid resources significantly benefit decision-making outcomes. However, historically clinician utilization of such tools has been low,78 many decision aids remain unavailable for clinical use,79 and few tools consider low health literacy.80 In an ideal, resource rich setting, we would recommend developing, validating, and adapting tools for diverse cultures and languages (Table 3), with formal assessments of clinical impact.
In addition to provision of written materials and decision aids for patients and families, creating reproductive health communication training opportunities for clinicians is essential. The Enriching Communication Skills for Health Professionals in Oncofertility (ECHO) program offers comprehensive training for social workers, psychologists, nurses, and physician assistants to improve communication skills about reproductive health with AYA patients and their families.81,82 This program has a validated curriculum and has shown to significantly improve knowledge, confidence, and practice behaviors among allied health professionals. The Oncofertility Consortium is another source of training, offering on-line access to educational materials, patient testimonials, and training opportunities. The ASCO “Focus Under Forty” also offers physician-based training to improve and enhance discussions of fertility preservation for AYAs diagnosed with cancer.
Conclusion
Reproductive health literacy is a complex topic requiring clinicians to use judgement about the amount and type of information required at the time of a cancer diagnosis for AYAs and their parents/partners to make informed decisions about fertility preservation, family building goals and contraceptive needs. Assessing patient/family health literacy is critical to the care of AYA patients and awareness of the variety of factors such as patient age, developmental status, pubertal status, congruence of patient/caregiver perspectives, urgency of cancer treatment and disease stage which may impact these conversations is paramount. There are several resources available to improve reproductive health literacy which include training physicians/providers on how to have these difficult conversations and creating patient educational materials that facilitate decision-making. Although there is no ‘gold standard’ for assessing and improving health literacy, a plethora of resources, tools and strategies exist to optimize health literacy, which can be applied to the reproductive health setting. To illustrate how these best practices can converge, we have developed a framework that brings together multi-level perspectives (caregiver/family, provider, and system/organization) for enhancing the AYA clinical environment (Figure 1).
Figure 1. Integrative Framework to Enhance Literacy.
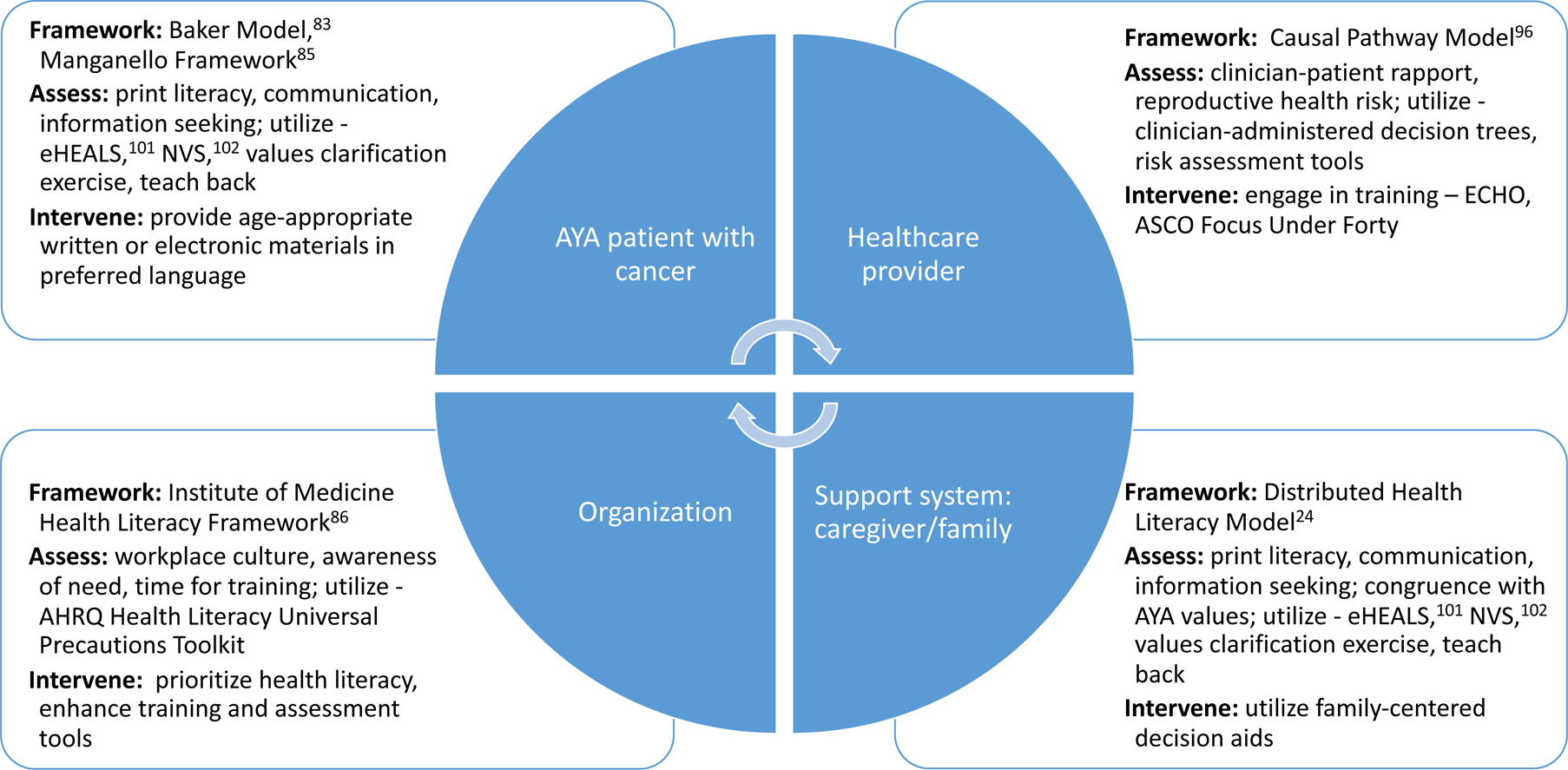
AYA – adolescent and young adult; eHEALS – eHealth Literacy Scale; NVS – Newest Vital Sign; AHRQ – Agency for Healthcare Research and Quality (https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/quality-resources/tools/literacy-toolkit/healthlittoolkit2.pdf); ECHO – Enriching Communication Skills for Health Professionals in Oncofertility (https://echo.rhoinstitute.org/); ASCO – American Society of Clinical Oncology
Acknowledgements:
Dr. Nahata is funded by the National Cancer Institute, 1K08CA237338-01
Abbreviation
- AYAs
Adolescents and young adults
Footnotes
Conflicts of Interest: None
References
- 1.Oktay K, Harvey BE, Partridge AH, et al. Fertility preservation in patients with cancer: ASCO clinical practice guideline update. 2018;36(19):1994–2001. [DOI] [PubMed] [Google Scholar]
- 2.Abusief ME, Hornstein MD, Jain TJF, sterility. Assessment of United States fertility clinic websites according to the American Society for Reproductive Medicine (ASRM)/Society for Assisted Reproductive Technology (SART) guidelines 2007;87(1):88–92. [DOI] [PubMed] [Google Scholar]
- 3.Kudesia R, Talib HJ, Pollack SEJJop, gynecology a. Fertility awareness counseling for adolescent girls; guiding conception: the right time, right weight, and right way 2017;30(1):9–17. [DOI] [PubMed] [Google Scholar]
- 4.Flink DM, Sheeder J, Kondapalli LAJJoa, oncology ya. A review of the oncology patient’s challenges for utilizing fertility preservation services 2017;6(1):31–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lehmann V, Flynn JS, Foster RH, Russell KM, Klosky JL. Accurate understanding of infertility risk among families of adolescent males newly diagnosed with cancer. Psycho-oncology. 2018;27(4):1193–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Quinn GP, Knapp C, Murphy D, Sawczyn K, Sender LJP. Congruence of reproductive concerns among adolescents with cancer and parents: pilot testing an adapted instrument. 2012;129(4):e930–e936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nahata L, Morgan TL, Ferrante AC, et al. Congruence of Reproductive Goals and Fertility-Related Attitudes of Adolescent and Young Adult Males and Their Parents After Cancer Treatment. 2019;8(3):335–341. [DOI] [PubMed] [Google Scholar]
- 8.Ferrante AC, Gerhardt CA, Yeager ND, et al. Interest in Learning about Fertility Status Among Male Adolescent and Young Adult Survivors of Childhood Cancer. 2019;8(1):61–66. [DOI] [PubMed] [Google Scholar]
- 9.Jayasuriya S, Peate M, Allingham C, et al. Satisfaction, disappointment and regret surrounding fertility preservation decisions in the paediatric and adolescent cancer population. J Assist Reprod Genet. 2019;36(9):1805–1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murphy D, Klosky JL, Termuhlen A, Sawczyn KK, Quinn GPJC. The need for reproductive and sexual health discussions with adolescent and young adult cancer patients. 2013;88(2):215–220. [DOI] [PubMed] [Google Scholar]
- 11.People HJP. Volume II. Department of Health and Human Services. 2000. Healthy 2010. [Google Scholar]
- 12.Eastman P The Link Between Health Literacy & Cancer Communication. 2019;41(16):1,5–6. [Google Scholar]
- 13.Zebrack B, Mathews-Bradshaw B, Siegel S, Alliance LYAJJCO. Quality cancer care for adolescents and young adults: a position statement. 2010;28(32):4862–4867. [DOI] [PubMed] [Google Scholar]
- 14.Quinn GP, Vadaparampil ST, Malo T, et al. Oncologists’ use of patient educational materials about cancer and fertility preservation. Psycho-oncology. 2012;21(11):1244–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morgan TL, Clark OE, Whiteside S, et al. Recruiting families and children newly diagnosed with cancer for behavioral research: Important considerations and successful strategies. 2019;28(4):928–930. [DOI] [PubMed] [Google Scholar]
- 16.Manganello JAJHer. Health literacy and adolescents: a framework and agenda for future research. 2007;23(5):840–847. [DOI] [PubMed] [Google Scholar]
- 17.Sørensen K, Van den Broucke S, Fullam J, et al. Health literacy and public health: a systematic review and integration of definitions and models. 2012;12(1):80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Squiers L, Peinado S, Berkman N, Boudewyns V, McCormack LJJohc. The health literacy skills framework. 2012;17(sup3):30–54. [DOI] [PubMed] [Google Scholar]
- 19.Fleary SA, Joseph P, Pappagianopoulos JEJJoa. Adolescent health literacy and health behaviors: a systematic review. 2018;62:116–127. [DOI] [PubMed] [Google Scholar]
- 20.Zarcadoolas C, Pleasant A, Greer DSJHpi. Understanding health literacy: an expanded model. 2005;20(2):195–203. [DOI] [PubMed] [Google Scholar]
- 21.Nutbeam D Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promotion International. 2000;15(3):259–267. [Google Scholar]
- 22.Vamos CA, Thompson EL, Logan RG, et al. Exploring college students’ sexual and reproductive health literacy. Journal of American college health : J of ACH. 2018:1–10. [DOI] [PubMed] [Google Scholar]
- 23.Kransdorf LN, Raghu TS, Kling JM, et al. Reproductive Life Planning: A Cross-Sectional Study of What College Students Know and Believe. Matern Child Health J. 2016;20(6):1161–1169. [DOI] [PubMed] [Google Scholar]
- 24.Edwards M, Wood F, Davies M, Edwards A. ‘Distributed health literacy’: longitudinal qualitative analysis of the roles of health literacy mediators and social networks of people living with a long-term health condition. Health expectations : an international journal of public participation in health care and health policy. 2015;18(5):1180–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sansom-Daly UM, Wakefield CE. Distress and adjustment among adolescents and young adults with cancer: an empirical and conceptual review. Transl Pediatr. 2013;2(4):167–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gessler D, Juraskova I, Sansom-Daly UM, Shepherd HL, Patterson P, Muscat DM. Clinician-patient-family decision-making and health literacy in adolescents and young adults with cancer and their families: A systematic review of qualitative studies. Psychooncology. 2019;28(7):1408–1419. [DOI] [PubMed] [Google Scholar]
- 27.Klosky JL, Simmons JL, Russell KM, et al. Fertility as a priority among at-risk adolescent males newly diagnosed with cancer and their parents. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2015;23(2):333–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Klosky JL, Lehmann V, Flynn JS, et al. Patient factors associated with sperm cryopreservation among at-risk adolescents newly diagnosed with cancer. Cancer. 2018;124(17):3567–3575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Klosky JL, Flynn JS, Lehmann V, et al. Parental influences on sperm banking attempts among adolescent males newly diagnosed with cancer. Fertility and sterility. 2017;108(6):1043–1049. [DOI] [PubMed] [Google Scholar]
- 30.Ginsberg JP, Ogle SK, Tuchman LK, et al. Sperm banking for adolescent and young adult cancer patients: sperm quality, patient, and parent perspectives. Pediatric blood & cancer. 2008;50(3):594–598. [DOI] [PubMed] [Google Scholar]
- 31.Crawshaw M, Glaser A, Hale J, Sloper PJEJoCC. Male and female experiences of having fertility matters raised alongside a cancer diagnosis during the teenage and young adult years. 2009;18(4):381–390. [DOI] [PubMed] [Google Scholar]
- 32.Burns KC, Boudreau C, Panepinto JAJJoPho. Attitudes regarding fertility preservation in female adolescent cancer patients. 2006;28(6):350–354. [DOI] [PubMed] [Google Scholar]
- 33.Shnorhavorian M, Harlan LC, Smith AW, et al. Fertility preservation knowledge, counseling, and actions among adolescent and young adult patients with cancer: A population-based study. Cancer. 2015;121(19):3499–3506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wittenberg E, Goldsmith J, Ferrell B, Ragan SL. Promoting improved family caregiver health literacy: evaluation of caregiver communication resources. Psychooncology. 2017;26(7):935–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Garvelink MM, Ter Kuile MM, Louwe LA, Hilders CG, Stiggelbout AM. A Delphi consensus study among patients and clinicians in the Netherlands on the procedure of informing young breast cancer patients about Fertility Preservation. Acta oncologica (Stockholm, Sweden). 2012;51(8):1062–1069. [DOI] [PubMed] [Google Scholar]
- 36.Barlevy D, Wangmo T, Elger BS, Ravitsky V. Attitudes, Beliefs, and Trends Regarding Adolescent Oncofertility Discussions: A Systematic Literature Review. Journal of Adolescent & Young Adult Oncology. 2016;5(2):119–134. [DOI] [PubMed] [Google Scholar]
- 37.Armuand GM, Nilsson J, Rodriguez-Wallberg KA, et al. Physicians’ self-reported practice behaviour regarding fertility-related discussions in paediatric oncology in Sweden. Psycho-oncology. 2017;26(10):1684–1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vindrola-Padros C, Dyer KE, Cyrus J, Lubker IM. Healthcare professionals’ views on discussing fertility preservation with young cancer patients: a mixed method systematic review of the literature. Psycho-oncology. 2016;26(1):4–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Miller EJN, Cookingham LM, Woodruff TK, et al. Fertility preservation training for obstetrics and gynecology fellows: a highly desired but non-standardized experience. Fertility research and practice. 2017;3:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Quinn GP, Woodruff TK, Knapp CA, Bowman ML, Reinecke J, Vadaparampil ST. Expanding the Oncofertility Workforce: Training Allied Health Professionals to Improve Health Outcomes for Adolescents and Young Adults. J Adolesc Young Adult Oncol. 2016;5(3):292–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Quinn GP, Vadaparampil ST, Bell-Ellison BA, Gwede CK, Albrecht TL. Patient-physician communication barriers regarding fertility preservation among newly diagnosed cancer patients. Social science & medicine (1982). 2008;66(3):784–789. [DOI] [PubMed] [Google Scholar]
- 42.Logan S, Perz J, Ussher J, Peate M, Anazodo A. Clinician provision of oncofertility support in cancer patients of a reproductive age: A systematic review. Psycho-oncology. 2018;27(3):748–756. [DOI] [PubMed] [Google Scholar]
- 43.Anazodo A, Laws P, Logan S, et al. How can we improve oncofertility care for patients? A systematic scoping review of current international practice and models of care. Human reproduction update. 2019;25(2):159–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smith K, Efymow B, Gracia C. Patient Navigation and Coordination of Care for the Oncofertility Patient: A Practical Guide. In: Gracia C, Woodruff TK, eds. Oncofertility Medical Practice: Clinical Issues and Implementation. New York, NY: Springer New York; 2012:175–185. [Google Scholar]
- 45.Gessler D, Juraskova I, Sansom-Daly UM, Shepherd HL, Patterson P, Muscat DM. Clinician-patient-family decision-making and health literacy in adolescents and young adults with cancer and their families: A systematic review of qualitative studies. 2019;28(7):1408–1419. [DOI] [PubMed] [Google Scholar]
- 46.Siembida EJ, Bellizzi KM. The Doctor-Patient Relationship in the Adolescent Cancer Setting: A Developmentally Focused Literature Review. J Adolesc Young Adult Oncol. 2015;4(3):108–117. [DOI] [PubMed] [Google Scholar]
- 47.Lin M, Sansom-Daly UM, Wakefield CE, McGill BC, Cohn RJ. Health Literacy in Adolescents and Young Adults: Perspectives from Australian Cancer Survivors. Journal of adolescent and young adult oncology. 2017;6(1):150–158. [DOI] [PubMed] [Google Scholar]
- 48.Kilfoyle KA, Vitko M, O’Conor R, Bailey SC. Health Literacy and Women’s Reproductive Health: A Systematic Review. J Womens Health (Larchmt). 2016;25(12):1237–1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gossett DR, Nayak S, Bhatt S, Bailey SC. What do healthy women know about the consequences of delayed childbearing? J Health Commun. 2013;18 Suppl 1:118–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fleary SA, Joseph P, Pappagianopoulos JE. Adolescent health literacy and health behaviors: A systematic review. J Adolesc. 2018;62:116–127. [DOI] [PubMed] [Google Scholar]
- 51.Gurney JG, Krull KR, Kadan-Lottick N, et al. Social outcomes in the Childhood Cancer Survivor Study cohort. J Clin Oncol. 2009;27(14):2390–2395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zikmund-Fisher BJ, Fagerlin A, Ubel PA. Risky feelings: why a 6% risk of cancer does not always feel like 6%. Patient Educ Couns. 2010;81 Suppl:S87–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gorman JR, Su HI, Roberts SC, Dominick SA, Malcarne VL. Experiencing reproductive concerns as a female cancer survivor is associated with depression. Cancer. 2015;121(6):935–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gilleland Marchak J, Elchuri SV, Vangile K, Wasilewski-Masker K, Mertens AC, Meacham LR. Perceptions of Infertility Risks Among Female Pediatric Cancer Survivors Following Gonadotoxic Therapy. Journal of pediatric hematology/oncology. 2015;37(5):368–372. [DOI] [PubMed] [Google Scholar]
- 55.Gilleland Marchak J, Seidel KD, Mertens AC, et al. Perceptions of risk of infertility among male survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Cancer. 2018;124(11):2447–2455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lehmann V, Chemaitilly W, Lu L, et al. Gonadal Functioning and Perceptions of Infertility Risk Among Adult Survivors of Childhood Cancer: A Report From the St Jude Lifetime Cohort Study. J Clin Oncol. 2019;37(11):893–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cherven B, Mertens A, Meacham LR, Williamson R, Boring C, Wasilewski-Masker K. Knowledge and risk perception of late effects among childhood cancer survivors and parents before and after visiting a childhood cancer survivor clinic. J Pediatr Oncol Nurs. 2014;31(6):339–349. [DOI] [PubMed] [Google Scholar]
- 58.Crawshaw MA, Sloper P. ‘Swimming against the tide’--the influence of fertility matters on the transition to adulthood or survivorship following adolescent cancer. Eur J Cancer Care (Engl). 2010;19(5):610–620. [DOI] [PubMed] [Google Scholar]
- 59.Hutchinson AD, Pfeiffer SM, Wilson C. Cancer-related cognitive impairment in children. Curr Opin Support Palliat Care. 2017;11(1):70–75. [DOI] [PubMed] [Google Scholar]
- 60.Children’s Oncology Group. Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers, Version 5.0 Monrovia, CA: Children’s Oncology Group; 2018. [Google Scholar]
- 61.Prevention OoD, Health HPUDo, Services H. National action plan to improve health literacy. US Department of Health & Human Services; 2010. [Google Scholar]
- 62.Apfel F, Tsouros AD. Health literacy: The solid facts. 2013. [Google Scholar]
- 63.AbuAlreesh A, Alburikan KA. Health literacy among patients with poor understanding of prescription drug label instructions in Saudi Arabia. Saudi pharmaceutical journal : SPJ : the official publication of the Saudi Pharmaceutical Society. 2019;27(6):900–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zotti P, Cocchi S, Polesel J, et al. Cross-cultural validation of health literacy measurement tools in Italian oncology patients. BMC health services research. 2017;17(1):410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Family medicine. 2004;36(8):588–594. [PubMed] [Google Scholar]
- 66.Bishop WP, Craddock Lee SJ, Skinner CS, Jones TM, McCallister K, Tiro JA. Validity of Single-Item Screening for Limited Health Literacy in English and Spanish Speakers. American journal of public health. 2016;106(5):889–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.National Academies of Sciences E, Medicine. Commissioned Paper on a Proposed Framework for Integration of Health Care Quality Measures Related to Health Literacy, Language Access, and Cultural Competence. Paper presented at: A Proposed Framework for Integration of Quality Performance Measures for Health Literacy, Cultural Competence, and Language Access Services: Proceedings of a Workshop 2018. [PubMed] [Google Scholar]
- 68.Koh HK, Rudd REJJ. The arc of health literacy. 2015;314(12):1225–1226. [DOI] [PubMed] [Google Scholar]
- 69.Mahmoodi N Are publicly available internet resources enabling women to make informed fertility preservation decisions before starting cancer treatment: an environmental scan? BMC health services research. 2018;18(1):104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Grace JG, Schweers L, Anazodo A, Freyer DR. Evaluating and providing quality health information for adolescents and young adults with cancer. Pediatric blood & cancer. 2019;66(10):e27931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Speller B, Sissons A, Daly C, et al. An evaluation of oncofertility decision support resources among breast cancer patients and health care providers. 2019;19(1):101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gardino SL, Jeruss JS, Woodruff TK. Using decision trees to enhance interdisciplinary team work: the case of oncofertility. Journal of Assisted Reproduction and Genetics. 2010;27(5):227–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Allingham C, Gillam L, McCarthy M, et al. Fertility Preservation in Children and Adolescents With Cancer: Pilot of a Decision Aid for Parents of Children and Adolescents With Cancer. JMIR Pediatr Parent. 2018;1(2):e10463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nahata L, Morgan TL, Lipak KG, et al. Perceptions of participating in family-centered fertility research among adolescent and young adult males newly diagnosed with cancer: A qualitative study. Pediatric blood & cancer. 2019;66(11):e27966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ehrbar V, Urech C, Rochlitz C, et al. Randomized controlled trial on the effect of an online decision aid for young female cancer patients regarding fertility preservation. Human reproduction (Oxford, England). 2019. [DOI] [PubMed] [Google Scholar]
- 76.Velikova G, Collins K, Stark D, et al. Feasibility and effects of a decision aid about fertility preservation. BMJ open. 2017;20(2):104–112. [DOI] [PubMed] [Google Scholar]
- 77.Woodard TL, Hoffman AS, Crocker LC, et al. Pathways: patient-centred decision counselling for women at risk of cancer-related infertility: a protocol for a comparative effectiveness cluster randomised trial. BMJ open. 2018;8(2):e019994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Brace C, Schmocker S, Huang H, Victor JC, McLeod RS, Kennedy ED. Physicians’ awareness and attitudes toward decision aids for patients with cancer. Journal of Clinical Oncology.28(13):2286–2292. [DOI] [PubMed] [Google Scholar]
- 79.Wang Y, Anazodo A, Logan S. Systematic review of fertility preservation patient decision aids for cancer patients. 2019;28(3):459–467. [DOI] [PubMed] [Google Scholar]
- 80.Peate M, Smith SK, Pye V, et al. Assessing the usefulness and acceptability of a low health literacy online decision aid about reproductive choices for younger women with breast cancer: the aLLIAnCE pilot study protocol. Pilot and feasibility studies. 2017;3:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Vadaparampil ST, Gwede CK, Meade C, et al. ENRICH: A promising oncology nurse training program to implement ASCO clinical practice guidelines on fertility for AYA cancer patients. Patient education and counseling. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Quinn GP, Bowman Curci M, Reich RR, et al. Impact of a web-based reproductive health training program: ENRICH (Educating Nurses about Reproductive Issues in Cancer Healthcare). Psycho-oncology. 2019;28(5):1096–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Baker DW. The meaning and the measure of health literacy. J Gen Intern Med. 2006;21(8):878–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lee SY, Arozullah AM, Cho YI. Health literacy, social support, and health: a research agenda. Social science & medicine (1982). 2004;58(7):1309–1321. [DOI] [PubMed] [Google Scholar]
- 85.Manganello JA. Health literacy and adolescents: a framework and agenda for future research. Health Education Research. 2007;23(5):840–847. [DOI] [PubMed] [Google Scholar]
- 86.Institute of Medicine Committee on Health L. In: Nielsen-Bohlman L, Panzer AM, Kindig DA, eds. Health Literacy: A Prescription to End Confusion. Washington (DC): National Academies Press (US) Copyright 2004 by the National Academy of Sciences. All rights reserved.; 2004. [PubMed] [Google Scholar]
- 87.Page RM, Huong NT, Chi HK, Tien TQ. Smoking media literacy in Vietnamese adolescents. The Journal of school health. 2011;81(1):34–41. [DOI] [PubMed] [Google Scholar]
- 88.Chang L-C. Health literacy, self-reported status and health promoting behaviours for adolescents in Taiwan. Journal of Clinical Nursing. 2011;20(1‐2):190–196. [DOI] [PubMed] [Google Scholar]
- 89.Chisolm DJ, Manganello JA, Kelleher KJ, Marshal MP. Health literacy, alcohol expectancies, and alcohol use behaviors in teens. Patient education and counseling. 2014;97(2):291–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zarcadoolas C, Pleasant A, Greer DS. Understanding health literacy: an expanded model. Health Promot Int. 2005;20(2):195–203. [DOI] [PubMed] [Google Scholar]
- 91.Speros C Health literacy: concept analysis. Journal of advanced nursing. 2005;50(6):633–640. [DOI] [PubMed] [Google Scholar]
- 92.Levin-Zamir D, Lemish D, Gofin R. Media Health Literacy (MHL): development and measurement of the concept among adolescents. Health Education Research. 2011;26(2):323–335. [DOI] [PubMed] [Google Scholar]
- 93.Primack BA, Hobbs R. Association of various components of media literacy and adolescent smoking. American journal of health behavior. 2009;33(2):192–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Paek H-J, Hove T. Social Cognitive Factors and Perceived Social Influences That Improve Adolescent eHealth Literacy. Health Communication. 2012;27(8):727–737. [DOI] [PubMed] [Google Scholar]
- 95.Chang FC, Miao NF, Lee CM, Chen PH, Chiu CH, Lee SC. The association of media exposure and media literacy with adolescent alcohol and tobacco use. Journal of health psychology. 2016;21(4):513–525. [DOI] [PubMed] [Google Scholar]
- 96.Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. American journal of health behavior. 2007;31 Suppl 1:S19–26. [DOI] [PubMed] [Google Scholar]
- 97.Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25(6):391–395. [PubMed] [Google Scholar]
- 98.Davis TC, Wolf MS, Arnold CL, et al. Development and Validation of the Rapid Estimate of Adolescent Literacy in Medicine (REALM-Teen): A Tool to Screen Adolescents for Below-Grade Reading in Health Care Settings. Pediatrics. 2006;118(6):e1707. [DOI] [PubMed] [Google Scholar]
- 99.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults. J Gen Intern Med. 1995;10(10):537–541. [DOI] [PubMed] [Google Scholar]
- 100.Nurss JR, Parker RM, Williams MV, Baker DW. Short test of functional health literacy in adults. Case-Western Reserve University, Metro Health Medical Center. 1998. [Google Scholar]
- 101.Chung S-Y, Nahm E-S. Testing reliability and validity of the eHealth Literacy Scale (eHEALS) for older adults recruited online. Comput Inform Nurs. 2015;33(4):150–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Annals of family medicine. 2005;3(6):514–522. [DOI] [PMC free article] [PubMed] [Google Scholar]


