Abstract
Hypertriglyceridemia (HTG) is an uncommon but well-established cause of acute pancreatitis.
The patients with pancreatitis are at risk for both local and systemic complications.
Abdominal compartment syndrome is underdiagnosed and undertreated in this patient population. We report a case of 39-year-old male with medical history of diabetes mellitus who presented with abdominal pain and was diagnosed with HTG induced pancreatitis, complicated by abdominal compartment syndrome requiring surgical decompression and plasmapheresis.
Keywords: Hypertriglyceridemia, Pancreatitis, Plasmapheresis, Abdominal compartment syndrome, Intra-abdominal hypertension, Decompression surgical, Laparotomy
Introduction
Acute pancreatitis is a leading gastrointestinal cause of hospitalization in the United States. The diagnosis of acute pancreatitis is defined by the presence of two of the following: acute onset of persistent, severe, epigastric pain often radiating to the back, elevation in serum lipase or amylase to 3 times or greater than the upper limit of normal, or characteristic findings of acute pancreatitis on imaging (contrast-enhanced computed tomography, magnetic resonance imaging, or transabdominal ultrasonography) [1].
Hypertriglyceridemia (HTG) is the third leading cause of pancreatitis after gallstone and alcohol [2]. HTG can be caused by genetic and acquired causes. Acquired common causes include obesity, diabetes mellitus, hypothyroidism, pregnancy, and medications [2]. We report a case of year-old man with medical history of diabetes mellitus who presented with abdominal pain and was diagnosed with HTG induced pancreatitis complicated by abdominal compartment syndrome (ACS) requiring surgical decompression and plasmapheresis.
Case presentation
A 39-year-old male with history of diabetes mellitus on oral hypoglycemic agents and dyslipidemia presented with 1-day history of epigastric abdominal pain, nausea, and vomiting.
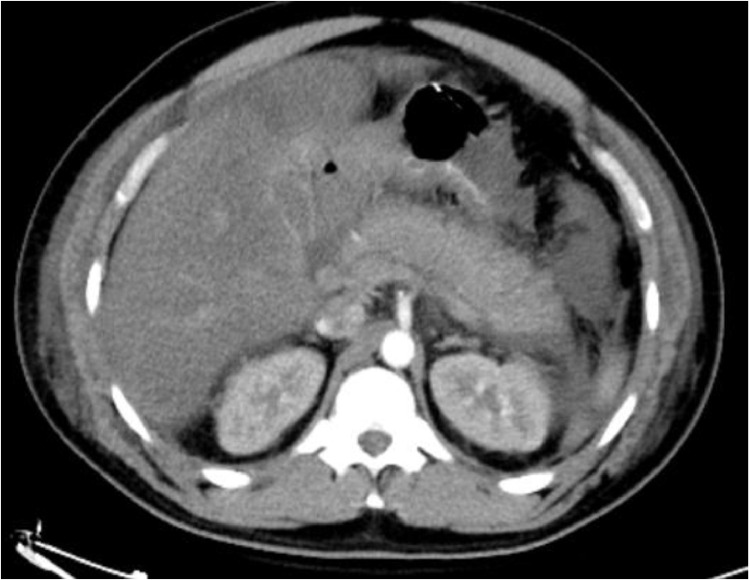
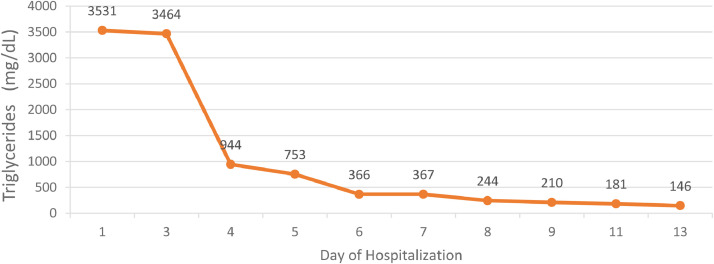
Vital signs on presentation - heart rate 81 per minute, blood pressure - 151/82 mm hg, respiratory rate 20 per minute, oxygen saturation 100% on room air, and temperature of 37.1°C. Physical examination was notable for distension and tenderness in the epigastrium to palpation without organomegaly, or rigidity. On initial laboratory evaluation, patient was found to have elevated white cell count of 14 × 103/µL (4.5-11 × 103/µL), hyponatremia with sodium level of 125 mEq/L (135-145 mEq/L), hyperglycemia with glucose level of 308 mg/dL (70-110 mg/dL), lactic acidosis of 5 mmol/L (0.5-2.2 mmol/L), creatinine of 1.64 mg/dL (0.6-1.3 mg/dL). Other lab values – hemoglobin, platelets, potassium, bicarbonate, calcium, albumin, total protein, liver function test were unremarkable, and acetone was negative. Lipase level at admission was 3500 U/L (11-82 U/L) and initial triglyceride level was 3531 mg/dL (<149 mg/dL). He denied any history of binge drinking, abdominal trauma, recent change in medications and any recent procedures including endoscopic retrograde cholangiopancreatography. Computed tomography of the abdomen revealed diffuse pancreatitis (Fig. 1). Abdominal ultrasound showed hepatic steatosis with no evidence of gall stones. The patient was admitted to intensive care unit for acute pancreatitis secondary to severe HTG and was started on aggressive intravenous fluid resuscitation, electrolyte management and intravenous insulin drip. Due to tachypnea, altered mental status and worsening acidosis on arterial blood gas, he was intubated for respiratory failure on day 3 of admission. After 48 hours of intravenous insulin infusion, triglycerides remained elevated at 3000 mg/dL, and patient deteriorated clinically with abdominal distension, oliguria, worsening acidosis, and renal failure (creatinine of 8.76 mg/dL). Due to deteriorating clinical condition and lack of improvement of triglycerides with insulin drip, plasmapheresis was initiated on day 2 of admission - triglycerides improved to less than 500 mg/dL after 2 sessions of plasmapheresis (Fig. 2). He was also initiated on hemodialysis on day 4 of hospitalization for renal failure from acute tubular necrosis. Patient's bladder pressure was being serially monitored for suspicion of ACS. On day 5 of hospitalization, the patient was found to have elevated bladder pressures of 27 mmHg (normal range - 5-7 mmHg) and peak airway pressures more than 40 cm H2O (normal range - 10-14 cm H2O), measured after paralyzed with neuromuscular blocking agent cisatracurium. The patient was taken to operating room for emergent decompressive laparotomy, 700 cc of serous ascitic fluid was drained and areas of saponification were noted on omentum. The patient postoperative course was complicated by sepsis and delirium. Eventually the patient stabilized and was downgraded to medical floor. His renal function improved, and hemodialysis was stopped and was discharged to home in a stable condition. Initially the patient was started on icosapent ethyl and omega 3 fatty acids and fenofibrate was added once his kidney function improved.
Fig. 1.
CT scan showing diffuse pancreatitis without ascites.
Fig. 2.
Showing trend of triglycerides with corresponding day of hospitalization.
Discussion
HTG is classified based on the degree of elevation as follows Mild (150-199 mg/dL 1.7 to 2.2 mmol/L), Moderate (200-999 mg/dL, 2.3-11.2 mmol/L), Severe HTG (1000-1999 mg/dL, 11.3-22.5 mmol/L), Very severe HTG (≥2000 mg/dL, >22.6 mmol/L) [3]. HTG-induced pancreatitis should be suspected in patients with acute pancreatitis and risk factors for HTG. The degree of triglyceride elevation is associated with the severity of acute pancreatitis. In a retrospective study of 1539 patients with acute pancreatitis in which 461 (30%) had elevated triglyceride levels, the rates of severe acute pancreatitis increased with increasing triglyceride levels [4].
Management of patients with hypertriglyceridemic pancreatitis (HTGP) includes treatment of acute pancreatitis with supportive care (fluid resuscitation, pain control) and reduction of serum triglyceride levels. The main treatment modalities for initial acute management of HTG are apheresis and insulin. Limited literature is available regarding the use of apheresis in patients with HTGP. Click et al performed a systematic review of available literature and found that data on the efficacy of apheresis was mostly limited to improvement in clinical symptoms (eg, abdominal pain, nausea, vomiting) and laboratory tests with little information provided on the impact of apheresis on AP severity [5].
Acute pancreatitis can lead to both local and systemic complications. ACS is a lethal complication of acute pancreatitis and is defined as a sustained intra-abdominal pressure >20 mmHg (with or without APP <60 mmHg) that is associated with new organ dysfunction [6]. Mortality in acute pancreatitis patients with ACS was 49% vs 11% without ACS [6]. Patients with severe pancreatitis are at increased risk for ACS due to tissue edema from aggressive fluid resuscitation, peripancreatic inflammation, ascites, and ileus. Definitive diagnosis of ACS requires measurement of the intra-abdominal pressure [7]. Transbladder measurement is the most commonly used method for measuring intra-abdominal pressure. A high index of suspicion is needed for prompt diagnosis and management. Management of ACS consists of supportive care and, when needed, abdominal decompression. Supportive care includes nasogastric decompression, prokinetics, sedation, neuromuscular blockers, diuretics or ultrafiltration, or percutaneous drainages of ascites [7]. Muresan et al reported a longitudinal prospective study of 134 patients with risk factors for ACS. Of 134 patients, 66 developed ACS. The highest mortality rate in the study group was reported in patients with necrotizing pancreatitis and the lowest in trauma group and decompression laparotomy was protective against mortality reducing it by 8.7% and should be used as soon as possible in case of medical resuscitation failure [8].
Limited literature is available regarding HTGP complicated by ACS. Chibber et al describe a fatal case of ACS due to severe triglyceride-induced pancreatitis in early pregnancy [9]. Our case adds to the limited literature available firstly regarding use of plasmapheresis for HTGP and secondly, ACS complication in HTGP requiring surgical decompression.
Consent
Authors confirm that written patient consent has been taken for publication.
Footnotes
Competing Interests: None.
Funding: None.
References
- 1.Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG. Classification of acute pancreatitis–2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62(1):102–111. doi: 10.1136/gutjnl-2012-302779. [DOI] [PubMed] [Google Scholar]
- 2.Parhofer KG, Laufs U. The diagnosis and treatment of hypertriglyceridemia. Dtsch Arztebl Int. 2019;116(49):825–832. doi: 10.3238/arztebl.2019.0825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berglund L, Brunzell JD, Goldberg AC, Goldberg IJ, Sacks F, Murad MH. Evaluation and treatment of hypertriglyceridemia: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012;97(9):2969–2989. doi: 10.1210/jc.2011-3213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wan J, He W, Zhu Y, Zhu Y, Zeng H, Liu P. Stratified analysis and clinical significance of elevated serum triglyceride levels in early acute pancreatitis: a retrospective study. Lipids Health Dis. 2017;16(1):124. doi: 10.1186/s12944-017-0517-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Click B, Ketchum AM, Turner R, Whitcomb DC, Papachristou GI, Yadav D. The role of apheresis in hypertriglyceridemia-induced acute pancreatitis: a systematic review. Pancreatology. 2015;15(4):313–320. doi: 10.1016/j.pan.2015.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Brunschot S, Schut AJ, Bouwense SA, Besselink MG, Bakker OJ, van Goor H. Abdominal compartment syndrome in acute pancreatitis: a systematic review. Pancreas. 2014;43(5):665–674. doi: 10.1097/MPA.0000000000000108. [DOI] [PubMed] [Google Scholar]
- 7.Newman RK, Dayal N, Dominique E. StatPearls Publishing LLC; 2020. Abdominal compartment syndrome. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2020. [PubMed] [Google Scholar]
- 8.Muresan M, Muresan S, Brinzaniuc K, Voidazan S, Sala D, Jimborean O. How much does decompressive laparotomy reduce the mortality rate in primary abdominal compartment syndrome?: A single-center prospective study on 66 patients. Medicine (Baltimore) 2017;96(5):e6006. doi: 10.1097/MD.0000000000006006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chibber T, Gibson PS. Fatal abdominal compartment syndrome due to severe triglyceride-induced pancreatitis in early pregnancy. J Obstet Gynaecol Can. 2018;40(5):609–613. doi: 10.1016/j.jogc.2017.06.035. [DOI] [PubMed] [Google Scholar]