Abstract
Context:
Anterior cruciate ligament (ACL) reconstruction (ACLR) is frequently performed in patients younger than 20 years whose goal is to return to sport (RTS). Varying reinjury rates have been reported, and the factors responsible are unclear. Studies differ with regard to age, graft type, surgical techniques, postoperative rehabilitation, RTS guidelines, and methods used to determine ACL failures.
Objective:
To determine RTS rates; the effect of participation in high-risk sports, sex, and graft type on ACL reinjury rates; and whether objective test criteria before RTS correlate with lower reinjury rates.
Data Sources:
A systematic review of the literature from inception to May 31, 2019, was conducted using the PubMed and Cochrane databases.
Study Selection:
Studies on transphyseal ACLR in athletes <20 years old with a minimum mean follow-up of 2 years that reported reinjury rates, the number that RTS, and detailed the type of sport were included.
Study Design:
Systematic review.
Level of Evidence:
Level 4.
Results:
A total of 1239 patients in 8 studies were included; 87% returned to sport and 80% resumed high-risk activities. Of the patients, 18% reinjured the ACL graft and/or the contralateral ACL. Nine percent of patellar tendon autografts and 15% of hamstring autografts failed (odds ratio [OR], 0.52; P = 0.002). Of reinjuries, 90% occurred during high-risk sports. Male patients had a significantly higher rate of ACL graft failure than female patients (OR, 1.64; P = 0.01). There was no sex-based effect on contralateral ACL injuries. Only 1 study cited objective criteria for RTS.
Conclusion:
A high percentage of athletes returned to sport, but 1 in 5 suffered reinjuries to either knee. Male patients were more likely to reinjure the ACL graft. Objective criteria for RTS were rarely mentioned or not detailed. The need for testing of knee stability, strength, neuromuscular control, agility, and psychological measures before RTS remains paramount in young athletes.
Keywords: ACL reconstruction, return to sport, ACL reinjury, transphyseal ACL reconstruction
The rate of anterior cruciate ligament (ACL) reconstruction (ACLR) in patients younger than 20 years has increased dramatically18,40,104; 1 study reported a 5.7-fold increase in the rate of ACLR between 2004 and 2014 in patients aged 18 years or younger.97 Adolescents are frequently treated with ACLR to prevent further injury to the menisci and articular cartilage and allow for return to sport (RTS).25,28,38,49,79,100 Although variability exists in RTS rates of adolescents after ACLR,60,63,85 several studies have reported that 90% or more returned.26,50,75,86,95 However, there is a justifiable concern over the potential for reinjury in this population. Investigations that compared reinjury rates (to either knee) after ACLR between adolescent and adult cohorts have shown significantly higher rates in adolescents.2,3,7,30,91,98,102 For instance, Webster et al102 compared reinjury rates in patients <20 years with those ≥20 years; ACL graft rupture rates were 14% and 2%, respectively (odds ratio [OR], 6.3; P = 0.0001), and contralateral ACL rupture rates were 16% and 5%, respectively (OR, 3.1; P = 0.001).
There are many potential risk factors for reinjuries after ACLR in younger patients. Although several authors have cited age <20 years as a risk factor,14,15,22,45,55,59,73,86,102 few have also included RTS in a multivariate analysis.23,76 Individual studies have cited return to high-risk sports involving jumping/landing, cutting, and pivoting37,52,71,82,102; use of an allograft13,27; and neuromuscular deficiencies on landing from a jump and cutting70,72 as other risk factors. Problems incurred when analyzing the literature in this young population include the combination of different types of ACLR techniques and grafts within studies, limited information regarding rehabilitation, detailed RTS data not provided, inclusion of only ACL revisions as failures (as is done in registry or questionnaire-based studies3,29,30,59,60,71,73), and inclusion of patients >20 years of age in the cohort.1,37,46,105 For instance, 1 meta-analysis of 5 studies reported a secondary ACL injury rate of 23% in patients ≤25 years of age who returned to high-risk sports.105 However, these 5 studies varied with regard to age, graft type, surgical techniques, postoperative rehabilitation, RTS guidelines, and methods used to determine ACL failures.
ACLR techniques for children and adolescents differ according to skeletal maturity and are generally categorized as physeal-sparing (extraphyseal and all-physeal), partial transphyseal, and transphyseal (adult reconstruction). Investigators have reported varying reinjury rates after ACLR in high school and collegiate athletic populations that usually undergo transphyseal procedures.10,40,42,44,83,93,94 A recent systematic review of 20 studies involving 1156 patients <20 years old reported that 92% returned to sport, 13% suffered ACL graft reinjuries, and 14% tore the contralateral ACL.48 This study combined all types of ACL techniques and grafts, with the patient age ranging from 6 to 19 years. An analysis of the effect of return to high-risk sports on reinjury rates was not performed.
To analyze a homogeneous cohort, this review systematically assessed RTS and reinjury rates in patients <20 years old after primary unilateral transphyseal ACLR. The goals were to determine (1) RTS rates, (2) the effect of resuming high-risk sports (involving jump/land, pivot, or cut maneuvers) on reinjury rates to the ACL of either knee, (3) the effect of sex and graft type on reinjury rates, and (4) whether the use of objective testing and specific discharge criteria before RTS correlates with lower reinjury rates. To our knowledge, this is the first systematic review that addresses these objectives in this population.
Methods
Literature Search Strategy
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines were followed in conducting this study.54 The PubMed and Cochrane databases were searched for literature on the subject matter from the date of inception to May 31, 2019. The following key phrases and words were used: anterior cruciate ligament pediatrics, ACL return to sport, anterior cruciate ligament children, anterior cruciate ligament reconstruction children, anterior cruciate ligament reconstruction adolescent, ACL adolescent, ACL skeletally immature, and ACL transphyseal. No limits were set other than English language. All evidence levels were included. The full text was accessed if the abstract suggested that this might be a clinical study in the topic of interest. In addition, the reference lists from general review articles, systematic reviews, and meta-analyses obtained from the search were examined to find any other original research investigations not otherwise obtained.
Study Selection and Quality Assessment
To be included in the review, studies were required to be original research investigations, be published in English, include primary transphyseal ACL reconstruction in patients <20 years old, have a minimum mean follow-up of 2 years postoperatively, report the ACL graft reinjury rate, and report the percentage of patients that returned to sport postoperatively.
Exclusionary criteria were studies that (1) were non–peer reviewed; (2) included patients treated for tibial avulsion fractures; (3) included patient treated with direct ACL suture repair, partial physeal, or all-physeal sparing procedures; or (4) failed to describe the type of sport activity for any patient postoperatively. General or systematic reviews, meta-analyses, editorials, case reports, and all other off-topic articles were also excluded.
Study quality was evaluated using the Methodological Index for Non-Randomized Studies (MINORS) instrument.90 The MINORS score is reported as a percentage of the total available points, as recommended by Wylie et al.107 In addition, a modified Coleman score based on criteria described by Longo et al56 was calculated for each study to achieve reproducibility and relevancy for the systematic review of ACL reconstruction in skeletally immature patients. The scores were categorized as excellent (85-100 points), good (70-84 points), fair (50-69 points), or poor (<50 points). Evidence levels of all articles as determined by the publishers were noted.
Data Extraction
The data extracted are shown in Appendix Table A1 (available in the online version of this article) and were reviewed by both authors, with agreement reached.
Results
The search identified 4762 articles, of which 4754 were excluded (Appendix Table A2, available online), leaving 8 studies published between 2004 and 2018 for our review.33,34,50,53,60,86,87,95 Because there were 2 studies from the same institution,86,89 personal correspondence with the authors resulted in the correct combination of data that avoided duplication. The mean MINORS score was 66% (range, 56%-75%), and the mean Coleman score was 60 points (range, 48-77 points). The quality of the studies was rated as good in 1, fair in 6, and poor in 1 study. The level of evidence was rated as level 4 in 6 studies,33,34,50,53,60,87 level 3 in 1,95 and level 2 in 1 study.86
There were 1239 patients followed for a mean 5.2 years (range, 2.0-20.6 years) (Table 1). Validated functional questionnaires were used in 6 studies (Appendix Table A3, available online). Sports or activity level rating assessments (Tegner,17,96 International Knee Documentation Committee [IKDC],39 or the Cincinnati Sports Activity Scale9) were used in 4 studies,33,34,50,53 and nonvalidated sports activity surveys were used in 3 studies.50,86,87,95
Table 1.
Patient demographics (N = 1239)
| Factor | n, n (%), or Mean (Range) |
|---|---|
| Sex, n | |
| Male | 579 |
| Female | 660 |
| Chronological age, y, mean (range) | 14.9 (8.0-19.0) |
| Time from injury to ACL reconstruction, n | |
| Acute/subacute | 173 |
| Chronic | 69 |
| Not provided | 997 |
| Original ACL injury information, n | |
| Sport related | 337 |
| Not provided | 902 |
| Follow-up, y, mean (range) | 5.2 (2.0-20.6) |
| Tanner staging, n | |
| Stage 1 | 5 |
| Stage 2 | 17 |
| Stage 1 or 2 | 15 |
| Stage 3 | 73 |
| Stage 4 | 9 |
| Not done | 1120 |
| Physes, n | |
| Open | 73 |
| Closed | 241 |
| Not provided | 925 |
| ACL grafts, n (%) | |
| Bone–patellar tendon–bone autograft | 730 (59) |
| Hamstring autograft (isolated) | 409 (33) |
| Hamstring autograft and Telos artificial ligament | 58 (5) |
| Hamstring allograft | 32 (2) |
| Tibialis anterior allograft | 8 (<1) |
| Fascia lata autograft | 2 (<1) |
| Concurrent operative procedures, n | |
| Meniscectomy | 124 |
| Meniscal repair | 123 |
| Either repaired or left in situ (1 study) | 73 |
| Data regarding meniscal procedures not provided (2 studies) | 930 |
| Anterolateral ligament reconstruction (1 study a ) | 33 |
ACL, anterior cruciate ligament.
Geffroy et al33; indications for this procedure were not provided.
Return to Sport
Overall, 1083 patients (87%) returned to any sport, of whom 994 (80%) resumed high-risk activities (Table 2). The mean time to RTS was provided in 3 studies33,86,95 and ranged from 4.6 months86 to 12.3 months33 postoperatively.
Table 2.
Return-to-sport data
| Participation in High-Risk Sport, n (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Patients in Study, n | Preinjury | Follow-up | |||||||
| Study | Total | Male | Female | Total | Male | Female | Total | Male | Female |
| Geffroy et al33 | 178 | 80 | 98 | 157 (88) |
NP | NP | 99 (56) | NP | NP |
| Goddard et al34 | 32 | 21 | 11 | 27 (84) |
17 (81) |
10 (91) |
25 (78) | 16 (76) |
9 (82) |
| Kocher et al50 | 59 | 23 | 36 | 59 (100) |
23 (100) |
36 (100) |
59 (100) | 23 (100) |
36 (100) |
| Larson et al53 | 30 | 14 | 16 | 30 (100) |
14 (100) |
16 (100) |
30 (100) | 14 (100) |
16 (100) |
| Morgan et al60 | 242 | 138 | 104 | 220 (91) |
NP | NP | 131 (54) | NP | NP |
| Shelbourne et al87 | 16 | 11 | 5 | 16 (100) |
11 (100) |
5 (100) |
16 (100) | 11 (100) |
5 (100) |
| Shelbourne et al86,89 | 624 | 234 | 390 | 582 (93) |
NP | NP | 582 (93) | NP | NP |
| Takazawa et al95 | 58 | 58 | 0 | 58 (100) |
58 (100) |
0 | 52 (90) | 52 (90) | 0 |
| Total | 1239 | 579 | 660 | 1149 (94) |
123/127a (97) |
67/68a (99) |
994 (80) |
116/127a (91) |
66/68a (97) |
aThe denominators are the total number of males and females in the studies when the sex data were provided. NP, not provided.
Reinjuries
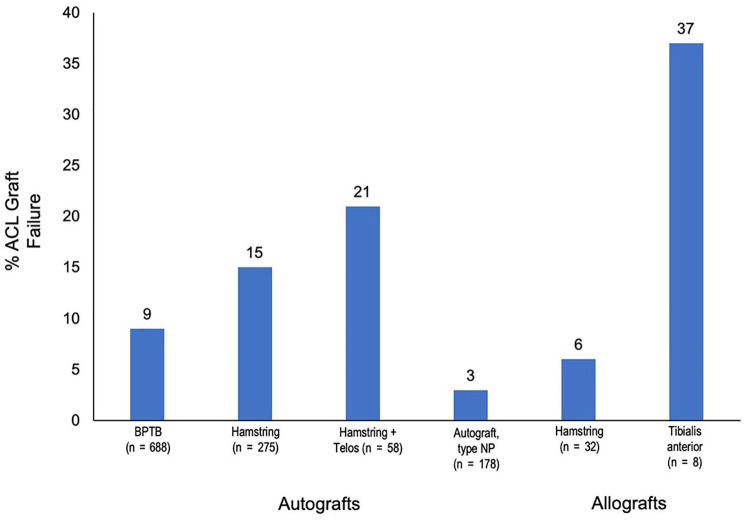
Failure of the ACL grafts was reported in 123 patients (10%) and ranged from 3% to 21% in each study (Appendix Table A4, available online). Of the reinjuries, 90% occurred during high-risk sports (Table 3). The time postoperatively that the ACL grafts failed ranged from 4 weeks34 to a mean of 51 months.60 Male patients had a significantly higher rate of failure compared with female patients (13% and 8%, respectively; OR, 1.64; P = 0.01). Overall, 15% of hamstring autografts and 9% of bone–patellar tendon–bone autografts failed (OR, 0.52; P = 0.002) (Figure 1).
Table 3.
Details of reinjuries
| Knee | Variable | Factors | n (%) |
|---|---|---|---|
| ACLR (n = 123) |
Cause of reinjury n (%) |
High-risk sport (jump/land, pivot, cut) Fall, other Not provided |
111 (90) 5 (4) 7 (6) |
| Type of graft n failed (% of total that received the graft) |
Bone–patellar tendon–bone autograft (n = 688) Hamstring autograft (n = 275) Hamstring autograft + Telos ligament (n = 58) Tibialis anterior allograft (n = 8) Hamstring allograft (n = 32) Autograft, graft not provided (n = 178, 1 study) |
59 (9) 42 (15) a 12 (21) 3 (37) 2 (6) 5 (3) |
|
| Sexn failed (% of sex) | Male (n = 556) Female (n = 624) Not provided (1 study, 23 male, 36 female) |
70 (13)
b
51 (8) 2 |
|
| Contralateral ACL (n = 115) |
Cause of injury n (%) |
High-risk sport (jump/land, pivot, cut) Not provided |
92 (80) 23 (20) |
| Sexn failed (% of sex) | Male (n = 538) Female (n = 559) Not provided (2 studies, 25 male, 21 female) |
54 (10) 54 (10) 7 |
ACL, anterior cruciate ligament; ACLR, ACL reconstruction.
Compared with bone–patellar tendon–bone autograft odds ratio, 0.52; P = 0.002.
Odds ratio, 1.64; P = 0.01.
Figure 1.
Percentages of anterior cruciate ligament (ACL) reconstruction failure according to the type of graft. BPTB, bone–patellar tendon–bone; NP, not provided.
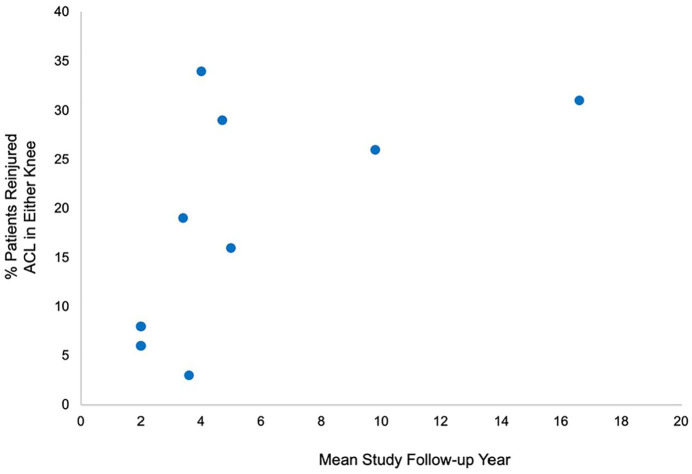
Contralateral ACL ruptures were reported in 115 patients (10%) in 6 studies.33,53,60,86,87,95 The time these injuries occurred postoperatively was only provided in 2 studies.60,87 Of the injuries, 80% occurred during high-risk sports; however, the mechanism of these injuries (contact or noncontact) was not described in any study. There was no significant difference in the rate of contralateral ACL injury between male and female patients. Overall, 223 patients (18%) experienced either an ACL graft failure and/or rupture of the contralateral ACL. This includes 15 patients from 1 study60 who sustained bilateral ACL tears postoperatively. Failure of either knee ranged from 3% to 34% per study (Figure 2). Subsequent operative procedures were performed in 19 patients in 5 studies (Appendix Table A5, available online).34,50,53,87,95
Figure 2.
The percentage of patients that suffered tears to the anterior cruciate ligament (ACL) graft, contralateral ACL, and either knee are shown for each study.
Parameters for Return to Sport
Six studies described parameters required for RTS (Table 4). Shelbourne et al89 required 85% quadriceps strength before patients were allowed to return to team competition. Larson et al53 recommended 90% limb symmetry index (LSI) on single-leg hop and triple hop tests, a time frame of 6 to 8 months postoperatively, and restoration of jump landing and pivoting mechanics that were not further detailed. Morgan et al60 stated RTS was allowed when an objective assessment had been performed but did not detail the variables in this assessment. Three studies34,50,95 provided only the time postoperatively RTS was usually allowed.
Table 4.
Criteria for release to sports activities
| Time Postoperatively, mo | Failure Rate, % | |||||||
|---|---|---|---|---|---|---|---|---|
| Study | n | Muscle Strength | Hop Test | Subjective Parameters | ACLR | Contralateral ACL | Either Knee | |
| Shelbourne et al86,89 | 624 | 85% quadriceps strength for team competition | 9 | 7 | 16 | |||
| Larson et al53 | 30 | 90% LSI single-leg hop and triple hop | 6-8 | “restoration of jump landing and pivoting mechanics” | 17 | 17 | 34 | |
| Morgan et al60 | 242 | 6-9 | “according to an objective assessment of whether the rehabilitation goals had been met” | 17 | 20 | 37 | ||
| Kocher et al50 | 59 | 6 | 3 | 0 | 3 | |||
| Takazawa et al95 | 52 | 6 | 21 | 9 | 29 | |||
| Goddard et al34 | 32 | 12 | 6 | 0 | 6 | |||
ACL, anterior cruciate ligament; ACLR, ACL reconstruction; LSI, limb symmetry index.
Discussion
Return to High-Risk Activities and Reinjury Rates
Of 1149 patients who participated in high-risk sports before their injury, 994 (80%) returned to these activities postoperatively. Overall, 1 in 5 patients sustained a reinjury to either knee, 90% of which occurred while participating in high-risk sports. There exist many other studies that reported high reinjury rates in patients <20 years old that did not report the sport or activity level (ie, IKDC level I) patients were participating in when the ACLR failure occurred, and these could not be included in this review.7,41,58,84,91,98,101 Therefore, the risk of sustaining an ACL reinjury during either low-risk sports or other accidents in this patient population remains elusive. Questionnaires and interviews were used in 3 studies60,86,95 to obtain reinjury data, and these investigations reported 100 ACL graft tears in 828 patients. There is the potential for other atraumatic graft failures that would have been detected on physical examination, and it is not possible to speculate on the impact of these missing data on the true ACL failure rate in this young population.
The mechanism of reinjury was not provided for 90% of the ACL graft failures and 100% of the contralateral ACL injuries. It is unknown whether these reinjuries occurred as a result of muscle weakness, neuromuscular deficiencies, psychological problems (fear), poor aerobic fitness, fatigue, direct contact with an opponent, or other risk factors. Several authors have published extensive recommendations for future reporting of the outcome of ACLR in young patients.5,19,24,48 We agree with Ardern et al5 that a standardized approach is necessary to define the injury, classify preinjury and postoperative sport activity, and describe RTS outcomes.
Effect of Sex and Graft Type on Reinjury Rates
Male patients had a significantly higher reinjury rate to the ACLR knee than female patients (13% and 8%, respectively). This is in agreement with Shelbourne et al,86 who reported that, in 528 patients <18 years old, male patients had a greater reinjury rate to the ACLR knee than female patients (10.6% and 7.4%, respectively; P < 0.05). Webster and Feller,101 reporting on 354 patients <18 years old, found that male patients had a higher ACL graft rupture rate than female patients (28% and 13%, respectively; P = 0.01). There was no sex-based effect on the rate of contralateral ACL tears, which has also been reported in other studies of adolescents.98,101
The Importance of RTS Testing
One of our original goals was to determine whether studies that included objective testing and specific discharge criteria before RTS had lower reinjury rates compared with those that did not include testing. Only 2 studies cited any objective criteria for RTS,53,89 and thus, this goal could not be achieved. We acknowledge that other investigators may have used specific criteria that were not included in the article. A prior systematic review of 264 studies found that only 13% listed objective criteria for RTS.8 A battery of tests for release to full sports was recommended, including an isokinetic quadriceps and hamstrings strength assessment, 4 single-leg hop tests,66 knee arthrometer, video drop-jump,69 single-leg squat,106 and a comprehensive knee examination. Since then, the issue of RTS criteria has received much attention in light of the unacceptable failure rates in young athletes cited by multiple investigations.7,19,41,47,58,84,91,98,101 In 2016, Ardern et al5 presented consensus statements regarding recommendations for RTS decision making from the First World Congress in Sports Physical Therapy. These authors identified the need to validate clinical tests for RTS, which include strength (rate of force development, eccentric, and endurance), neuromuscular control (dynamic functional tests and reactive agility tasks), psychological measures, and performance and skill execution.
Several studies have reported that many patients were unable to pass strength, balance, and neuromuscular tests in the time period when many authors allow RTS, typically 6 to 9 months postoperative.6,16,21,35,43,61,62,81,92,99,103 Boyle et al16 tested 39 adolescents and 16 adults who underwent transphyseal hamstring ACLR 9 months postoperatively with the functional movement screen and lower quarter Y-Balance tests. An increased risk for lower extremity injury was reported based on an inferior active straight-leg raise score on the functional movement screen. In addition, the adolescents had wider ranges of anterior reach asymmetry compared with the adult group. Toole et al99 assessed 115 adolescents at a mean 8 months postoperatively with isokinetic testing (180 deg/s), 4 single-leg hop tests, and the IKDC self-reported knee function scale. An LSI ≥90% was required to pass the strength and hop tests, and the IKDC score was required to be ≥90 points. Although all patients had been cleared by their surgeon to RTS, only 13.9% passed all tests. Petersen et al,74 in a systematic review of 61 articles, concluded that most studies reported muscular imbalances in the ACLR leg, which were most pronounced ≤6 months postoperatively, but could persist up to 2 years and longer.
Reducing the Risk of Reinjury
Studies of adult populations reported decreases in ACLR reinjury rates when objective tests were used before release to full competition. Kyritsis et al51 devised discharge criteria from isokinetic testing, 3 single-leg hop tests, and an agility test in 158 male professional athletes (mean age, 22 ± 5 years). Athletes who did not meet the criteria for all tests and who had a decreased hamstring-to-quadriceps ratio had a 4 times greater risk of ACL graft failure compared with those who met the criteria (33.3% and 10.3%, respectively; hazard ratio, 4.1; P < 0.001). Grindem et al37 reported that patients (mean age, 24.3 ± 7.3 years) who returned to high-risk sports were 4 times more likely to suffer a reinjury (including ACL, meniscal, and cartilage injuries) than those who did not. Their RTS test battery included isokinetic quadriceps testing, 4 single-leg hop tests, and 2 self-reported outcome measures. Patients who passed all test measures had substantial reductions in reinjury rates compared with those who failed (5.6% vs 38.2%, respectively; P = 0.07).
Historically, as early as the 1990s, many authors recommended strength testing prior to the initiation of running and RTS.4,20,57,64,65,67,68,88 In a study of 40 patients who underwent a bone–patellar tendon–bone allograft and iliotibial band extra-articular procedure, ≥85% quadriceps strength, no symptoms, and a period of 10 to 12 months postoperative were required before patients could return to running.64 In this group, 92% returned to sport and 3% experienced a graft failure. In a study of 53 patients who received a bone–patellar tendon–bone autograft and in whom noteworthy articular cartilage deterioration was present at surgery, return to recreational sports was allowed using similar criteria.67 The study reported that 79% returned to mostly low-impact sports and 6% experienced a graft failure.
Postoperative Rehabilitation for the Adolescent Athlete
Postoperative rehabilitation programs and progression to RTS in the adolescent athlete may require differences compared with programs used for adult patients to adjust for issues related to this age group, such as physiological and psychological maturity and psychosocial factors. Forrester et al32 identified 21 pediatric rehabilitation protocols from an internet-based search. Only 24% recommended passing specific tests, and 19% required surgeon approval for RTS. Greenberg et al36 surveyed members of the Pediatric Research in Sports Medicine Society to identify clinical practice patterns during ACLR rehabilitation for progression to jogging, modified sports activity, and unrestricted RTS. A total of 60 surgeons (response rate, 91%) participated, the majority of whom were board certified and performed >25 ACLRs each year. Variability was found for time allowed for modified sports activities (4-8 months) and RTS (6-12 months). Objective criteria to begin jogging included measurement of quadriceps strength, which was done using manual muscle testing in 70% and isokinetic testing in 22%, the single-leg squat test in 31%, and straight-leg raise test in 20%. There was no consensus for the LSI goal for initiation of modified sports activity, which ranged from >75% to >95%. Of concern was the finding that 32% of surgeons did not require objective testing for RTS. No surgeon used fear or self-efficacy questionnaires in their RTS assessment.
In the future, objective criteria regarding graft maturation using magnetic resonance imaging (MRI) may be of vital importance in the battery of testing for RTS clearance.77,78 Ultrashort echo-time MRI techniques offer improved image quality that allow for the assessment of the status of the ACL graft because they show excellent graft/implant contrast and low metal artifact.80 In animal models, ultrashort echo-time MRI modifications have allowed high-resolution 3-dimensional images that predicted linear stiffness, yield load, maximum load, and failure load after 1 year postoperatively.11,12,31
Study Limitations
There are limitations to this review, including low evidence levels in 7 of the 8 studies, potential for unrecognized failures because not all studies conducted clinical examinations, inability to determine whether reinjuries were contact or noncontact, and exclusion of at least 100 studies due to missing data regarding sport or reinjuries. The heterogeneity of the studies prevented conclusions regarding the effect of resuming high-risk sports compared with low-risk activities on reinjury rates. Whether the use of objective testing and discharge criteria before RTS correlated with lower reinjury rates could not be determined.
Conclusion
A high rate of athletes <20 years old returned to sport, but 1 in 5 suffered reinjuries to either knee, and the majority of these occurred during high-risk sports activities. Male patients were more likely than their female counterparts to reinjure the ACL graft. Objective criteria for RTS was rarely mentioned or not detailed. The need for testing of knee stability, strength, neuromuscular control, agility, and psychological measures before RTS remains paramount in young athletes.
Supplemental Material
Supplemental material, 37820_Appendix for One in 5 Athletes Sustain Reinjury Upon Return to High-Risk Sports After ACL Reconstruction: A Systematic Review in 1239 Athletes Younger Than 20 Years by Sue Barber-Westin and Frank R. Noyes in Sports Health: A Multidisciplinary Approach
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Allen MM, Pareek A, Krych AJ, et al. Are female soccer players at an increased risk of second anterior cruciate ligament injury compared with their athletic peers? Am J Sports Med. 2016;44:2492-2498. [DOI] [PubMed] [Google Scholar]
- 2. Andernord D, Desai N, Bjornsson H, Gillen S, Karlsson J, Samuelsson K. Predictors of contralateral anterior cruciate ligament reconstruction: a cohort study of 9061 patients with 5-year follow-up. Am J Sports Med. 2015;43:295-302. [DOI] [PubMed] [Google Scholar]
- 3. Andernord D, Desai N, Bjornsson H, Ylander M, Karlsson J, Samuelsson K. Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: a cohort study of 16,930 patients with 2-year follow-up. Am J Sports Med. 2015;43:121-127. [DOI] [PubMed] [Google Scholar]
- 4. Anderson AF, Snyder RB, Lipscomb AB., Sr Anterior cruciate ligament reconstruction using the semitendinosus and gracilis tendons augmented by the loose iliotibial band tenodesis. A long-term study. Am J Sports Med. 1994;22:620-626. [DOI] [PubMed] [Google Scholar]
- 5. Ardern CL, Glasgow P, Schneiders A, et al. 2016 Consensus statement on return to sport from the First World Congress in Sports Physical Therapy, Bern. Br J Sports Med. 2016;50:853-864. [DOI] [PubMed] [Google Scholar]
- 6. Arundale AJH, Capin JJ, Zarzycki R, Smith A, Snyder-Mackler L. Functional and patient-reported outcomes improve over the course of rehabilitation: a secondary analysis of the ACL-SPORTS trial. Sports Health. 2018;10:441-452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Astur DC, Cachoeira CM, da Silva Vieira T, Debieux P, Kaleka CC, Cohen M. Increased incidence of anterior cruciate ligament revision surgery in paediatric verses adult population. Knee Surg Sports Traumatol Arthrosc. 2018;26:1362-1366. [DOI] [PubMed] [Google Scholar]
- 8. Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:1697-1705. [DOI] [PubMed] [Google Scholar]
- 9. Barber-Westin SD, Noyes FR, McCloskey JW. Rigorous statistical reliability, validity, and responsiveness testing of the Cincinnati knee rating system in 350 subjects with uninjured, injured, or anterior cruciate ligament–reconstructed knees. Am J Sports Med. 1999;27:402-416. [DOI] [PubMed] [Google Scholar]
- 10. Beck NA, Lawrence JT, Nordin JD, DeFor TA, Tompkins M. ACL tears in school-aged children and adolescents over 20 years. Pediatrics. 2017;139:e20161877. [DOI] [PubMed] [Google Scholar]
- 11. Biercevicz AM, Miranda DL, Machan JT, Murray MM, Fleming BC. In situ, noninvasive, T2*-weighted MRI-derived parameters predict ex vivo structural properties of an anterior cruciate ligament reconstruction or bioenhanced primary repair in a porcine model. Am J Sports Med. 2013;41:560-566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Biercevicz AM, Murray MM, Walsh EG, Miranda DL, Machan JT, Fleming BC. T2* MR relaxometry and ligament volume are associated with the structural properties of the healing ACL. J Orthop Res. 2014;32:492-499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Borchers JR, Pedroza A, Kaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure: a case-control study. Am J Sports Med. 2009;37:2362-2367. [DOI] [PubMed] [Google Scholar]
- 14. Bourke HE, Gordon DJ, Salmon LJ, Waller A, Linklater J, Pinczewski LA. The outcome at 15 years of endoscopic anterior cruciate ligament reconstruction using hamstring tendon autograft for “isolated” anterior cruciate ligament rupture. J Bone Joint Surg Br. 2012;94:630-637. [DOI] [PubMed] [Google Scholar]
- 15. Bourke HE, Salmon LJ, Waller A, Patterson V, Pinczewski LA. Survival of the anterior cruciate ligament graft and the contralateral ACL at a minimum of 15 years. Am J Sports Med. 2012;40:1985-1992. [DOI] [PubMed] [Google Scholar]
- 16. Boyle MJ, Butler RJ, Queen RM. Functional movement competency and dynamic balance after anterior cruciate ligament reconstruction in adolescent patients. J Pediatr Orthop. 2016;36:36-41. [DOI] [PubMed] [Google Scholar]
- 17. Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009;37:890-897. [DOI] [PubMed] [Google Scholar]
- 18. Buller LT, Best MJ, Baraga MG, Kaplan LD. Trends in anterior cruciate ligament reconstruction in the United States. Orthop J Sports Med. 2015;3:2325967114563664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Burgi CR, Peters S, Ardern CL, et al. Which criteria are used to clear patients to return to sport after primary ACL reconstruction? A scoping review. Br J Sports Med. 2019;53:1154-1161. [DOI] [PubMed] [Google Scholar]
- 20. Carter TR, Edinger S. Isokinetic evaluation of anterior cruciate ligament reconstruction: hamstring versus patellar tendon. Arthroscopy. 1999;15:169-172. [DOI] [PubMed] [Google Scholar]
- 21. Cristiani R, Mikkelsen C, Forssblad M, Engstrom B, Stalman A. Only one patient out of five achieves symmetrical knee function 6 months after primary anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27:3461-3470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Csintalan RP, Inacio MC, Funahashi TT, Maletis GB. Risk factors of subsequent operations after primary anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:619-625. [DOI] [PubMed] [Google Scholar]
- 23. Dekker TJ, Godin JA, Dale KM, Garrett WE, Taylor DC, Riboh JC. Return to sport after pediatric anterior cruciate ligament reconstruction and its effect on subsequent anterior cruciate ligament injury. J Bone Joint Surg Am. 2017;99:897-904. [DOI] [PubMed] [Google Scholar]
- 24. Dingenen B, Gokeler A. Optimization of the return-to-sport paradigm after anterior cruciate ligament reconstruction: a critical step back to move forward. Sports Med. 2017;47:1487-1500. [DOI] [PubMed] [Google Scholar]
- 25. Dunn KL, Lam KC, Valovich McLeod TC. Early operative versus delayed or nonoperative treatment of anterior cruciate ligament injuries in pediatric patients. J Athl Train. 2016;51:425-427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ekas GR, Moksnes H, Grindem H, Risberg MA, Engebretsen L. Coping with anterior cruciate ligament injury from childhood to maturation: a prospective case series of 44 patients with mean 8 years’ follow-up. Am J Sports Med. 2019;47:22-30. [DOI] [PubMed] [Google Scholar]
- 27. Ellis HB, Matheny LM, Briggs KK, Pennock AT, Steadman JR. Outcomes and revision rate after bone–patellar tendon–bone allograft versus autograft anterior cruciate ligament reconstruction in patients aged 18 years or younger with closed physes. Arthroscopy. 2012;28:1819-1825. [DOI] [PubMed] [Google Scholar]
- 28. Fabricant PD, Kocher MS. Management of ACL injuries in children and adolescents. J Bone Joint Surg Am. 2017;99:600-612. [DOI] [PubMed] [Google Scholar]
- 29. Faltstrom A, Hagglund M, Magnusson H, Forssblad M, Kvist J. Predictors for additional anterior cruciate ligament reconstruction: data from the Swedish national ACL register. Knee Surg Sports Traumatol Arthrosc. 2016;24:885-894. [DOI] [PubMed] [Google Scholar]
- 30. Fauno P, Rahr-Wagner L, Lind M. Risk for revision after anterior cruciate ligament reconstruction is higher among adolescents: results from the Danish registry of knee ligament reconstruction. Orthop J Sports Med. 2014;2:2325967114552405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fleming BC, Vajapeyam S, Connolly SA, Magarian EM, Murray MM. The use of magnetic resonance imaging to predict ACL graft structural properties. J Biomech. 2011;44:2843-2846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Forrester LA, Schweppe EA, Popkin CA. Variability in rehabilitation protocols following pediatric anterior cruciate ligament (ACL) reconstruction. Phys Sportsmed. 2019;47:448-454. [DOI] [PubMed] [Google Scholar]
- 33. Geffroy L, Lefevre N, Thevenin-Lemoine C, et al. Return to sport and re-tears after anterior cruciate ligament reconstruction in children and adolescents. Orthop Traumatol Surg Res. 2018;104(8)(suppl):S183-S188. [DOI] [PubMed] [Google Scholar]
- 34. Goddard M, Bowman N, Salmon LJ, Waller A, Roe JP, Pinczewski LA. Endoscopic anterior cruciate ligament reconstruction in children using living donor hamstring tendon allografts. Am J Sports Med. 2013;41:567-574. [DOI] [PubMed] [Google Scholar]
- 35. Gokeler A, Welling W, Zaffagnini S, Seil R, Padua D. Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25:192-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Greenberg EM, Greenberg ET, Albaugh J, Storey E, Ganley TJ. Anterior cruciate ligament reconstruction rehabilitation clinical practice patterns: a survey of the PRiSM Society. Orthop J Sports Med. 2019;7:2325967119839041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50:804-808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Guenther ZD, Swami V, Dhillon SS, Jaremko JL. Meniscal injury after adolescent anterior cruciate ligament injury: how long are patients at risk? Clin Orthop Relat Res. 2014;472:990-997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226-234. [DOI] [PubMed] [Google Scholar]
- 40. Herzog MM, Marshall SW, Lund JL, Pate V, Mack CD, Spang JT. Incidence of anterior cruciate ligament reconstruction among adolescent females in the United States, 2002 through 2014. JAMA Pediatr. 2017;171:808-810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hettrich CM, Dunn WR, Reinke EK, MOON Group, Spindler KP. The rate of subsequent surgery and predictors after anterior cruciate ligament reconstruction: two- and 6-year follow-up results from a multicenter cohort. Am J Sports Med. 2013;41:1534-1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Johnsen MB, Guddal MH, Smastuen MC, et al. Sport participation and the risk of anterior cruciate ligament reconstruction in adolescents: a population-based prospective cohort study (the Young-HUNT Study). Am J Sports Med. 2016;44:2917-2924. [DOI] [PubMed] [Google Scholar]
- 43. Johnson AK, Palmieri-Smith RM, Lepley LK. Contribution of neuromuscular factors to quadriceps asymmetry after anterior cruciate ligament reconstruction. J Athl Train. 2018;53:347-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Joseph AM, Collins CL, Henke NM, Yard EE, Fields SK, Comstock RD. A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. J Athl Train. 2013;48:810-817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Kaeding CC, Aros B, Pedroza A, et al. Allograft versus autograft anterior cruciate ligament reconstruction: predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3:73-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, MOON Consortium, Spindler KP. Risk factors and predictors of subsequent acl injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43:1583-1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kaplan Y, Witvrouw E. When is it safe to return to sport after ACL reconstruction? Reviewing the criteria. Sports Health. 2019;11:301-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kay J, Memon M, Marx RG, Peterson D, Simunovic N, Ayeni OR. Over 90% of children and adolescents return to sport after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2018;26:1019-1036. [DOI] [PubMed] [Google Scholar]
- 49. Kay J, Memon M, Shah A, et al. Earlier anterior cruciate ligament reconstruction is associated with a decreased risk of medial meniscal and articular cartilage damage in children and adolescents: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2018;26:3738-3753. [DOI] [PubMed] [Google Scholar]
- 50. Kocher MS, Smith JT, Zoric BJ, Lee B, Micheli LJ. Transphyseal anterior cruciate ligament reconstruction in skeletally immature pubescent adolescents. J Bone Joint Surg Am. 2007;89:2632-2639. [DOI] [PubMed] [Google Scholar]
- 51. Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50:946-951. [DOI] [PubMed] [Google Scholar]
- 52. Laboute E, Savalli L, Puig P, et al. Analysis of return to competition and repeat rupture for 298 anterior cruciate ligament reconstructions with patellar or hamstring tendon autograft in sportspeople. Ann Phys Rehabil Med. 2010;53:598-614. [DOI] [PubMed] [Google Scholar]
- 53. Larson CM, Heikes CS, Ellingson CI, et al. Allograft and autograft transphyseal anterior cruciate ligament reconstruction in skeletally immature patients: outcomes and complications. Arthroscopy. 2016;32:860-867. [DOI] [PubMed] [Google Scholar]
- 54. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:B2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med. 2012;40:1551-1557. [DOI] [PubMed] [Google Scholar]
- 56. Longo UG, Ciuffreda M, Casciaro C, et al. Anterior cruciate ligament reconstruction in skeletally immature patients: a systematic review. Bone Joint J. 2017;99-B:1053-1060. [DOI] [PubMed] [Google Scholar]
- 57. MacDonald PB, Hedden D, Pacin O, Huebert D. Effects of an accelerated rehabilitation program after anterior cruciate ligament reconstruction with combined semitendinosus-gracilis autograft and a ligament augmentation device. Am J Sports Med. 1995;23:588-592. [DOI] [PubMed] [Google Scholar]
- 58. Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28:526-531. [DOI] [PubMed] [Google Scholar]
- 59. Maletis GB, Chen J, Inacio MC, Funahashi TT. Age-related risk factors for revision anterior cruciate ligament reconstruction: a cohort study of 21,304 patients from the Kaiser Permanente Anterior Cruciate Ligament Registry. Am J Sports Med. 2016;44:331-336. [DOI] [PubMed] [Google Scholar]
- 60. Morgan MD, Salmon LJ, Waller A, Roe JP, Pinczewski LA. Fifteen-year survival of endoscopic anterior cruciate ligament reconstruction in patients aged 18 years and younger. Am J Sports Med. 2016;44:384-392. [DOI] [PubMed] [Google Scholar]
- 61. Nawasreh Z, Logerstedt D, Cummer K, Axe M, Risberg MA, Snyder-Mackler L. Functional performance 6 months after ACL reconstruction can predict return to participation in the same preinjury activity level 12 and 24 months after surgery. Br J Sports Med. 2018;52:375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Nawasreh Z, Logerstedt D, Cummer K, Axe MJ, Risberg MA, Snyder-Mackler L. Do patients failing return-to-activity criteria at 6 months after anterior cruciate ligament reconstruction continue demonstrating deficits at 2 years? Am J Sports Med. 2017;45:1037-1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Nikolaou P, Kalliakmanis A, Bousgas D, Zourntos S. Intraarticular stabilization following anterior cruciate ligament injury in children and adolescents. Knee Surg Sports Traumatol Arthrosc. 2011;19:801-805. [DOI] [PubMed] [Google Scholar]
- 64. Noyes FR, Barber SD. The effect of an extra-articular procedure on allograft reconstructions for chronic ruptures of the anterior cruciate ligament. J Bone Joint Surg Am. 1991;73:882-892. [PubMed] [Google Scholar]
- 65. Noyes FR, Barber SD. The effect of a ligament-augmentation device on allograft reconstructions for chronic ruptures of the anterior cruciate ligament. J Bone Joint Surg Am. 1992;74:960-973. [PubMed] [Google Scholar]
- 66. Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19:513-518. [DOI] [PubMed] [Google Scholar]
- 67. Noyes FR, Barber-Westin SD. Anterior cruciate ligament reconstruction with autogenous patellar tendon graft in patients with articular cartilage damage. Am J Sports Med. 1997;25:626-634. [DOI] [PubMed] [Google Scholar]
- 68. Noyes FR, Barber-Westin SD. Arthroscopic-assisted allograft anterior cruciate ligament reconstruction in patients with symptomatic arthrosis. Arthroscopy. 1997;13:24-32. [DOI] [PubMed] [Google Scholar]
- 69. Noyes FR, Barber-Westin SD, Fleckenstein C, Walsh C, West J. The drop-jump screening test: difference in lower limb control by gender and effect of neuromuscular training in female athletes. Am J Sports Med. 2005;33:197-207. [DOI] [PubMed] [Google Scholar]
- 70. Numata H, Nakase J, Kitaoka K, et al. Two-dimensional motion analysis of dynamic knee valgus identifies female high school athletes at risk of non-contact anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2018;26:442-447. [DOI] [PubMed] [Google Scholar]
- 71. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42:1567-1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968-1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Persson A, Fjeldsgaard K, Gjertsen JE, et al. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004-2012. Am J Sports Med. 2014;42:285-291. [DOI] [PubMed] [Google Scholar]
- 74. Petersen W, Taheri P, Forkel P, Zantop T. Return to play following ACL reconstruction: a systematic review about strength deficits. Arch Orthop Trauma Surg. 2014;134:1417-1428. [DOI] [PubMed] [Google Scholar]
- 75. Placella G, Bartoli M, Peruzzi M, Speziali A, Pace V, Cerulli G. Return to sport activity after anterior cruciate ligament reconstruction in skeletally immature athletes with manual drilling original all inside reconstruction at 8 years’ follow-up. Acta Orthop Traumatol Turc. 2016;50:635-638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Ponce BA, Cain EL, Jr, Pflugner R, et al. Risk factors for revision anterior cruciate ligament reconstruction. J Knee Surg. 2016;29:329-336. [DOI] [PubMed] [Google Scholar]
- 77. Qian Y, Williams AA, Chu CR, Boada FE. High-resolution ultrashort echo time (UTE) imaging on human knee with AWSOS sequence at 3.0 T. J Magn Reson Imaging. 2012;35:204-210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Qian Y, Williams AA, Chu CR, Boada FE. Repeatability of ultrashort echo time-based two-component T2* measurements on cartilages in human knee at 3 T. Magn Reson Med. 2013;69:1564-1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Raad M, Thevenin Lemoine C, Berard E, Laumonerie P, Sales de Gauzy J, Accadbled F. Delayed reconstruction and high BMI z score increase the risk of meniscal tear in paediatric and adolescent anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2019;27:905-911. [DOI] [PubMed] [Google Scholar]
- 80. Rahmer J, Bornert P, Dries SP. Assessment of anterior cruciate ligament reconstruction using 3D ultrashort echo-time MR imaging. J Magn Reson Imaging. 2009;29:443-448. [DOI] [PubMed] [Google Scholar]
- 81. Raoul T, Klouche S, Guerrier B, et al. Are athletes able to resume sport at six-month mean follow-up after anterior cruciate ligament reconstruction? Prospective functional and psychological assessment from the French Anterior Cruciate Ligament Study (FAST) cohort. Knee. 2019;26:155-164. [DOI] [PubMed] [Google Scholar]
- 82. Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:948-957. [DOI] [PubMed] [Google Scholar]
- 83. Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med. 2016;44:1502-1507. [DOI] [PubMed] [Google Scholar]
- 84. Schlumberger M, Schuster P, Schulz M, et al. Traumatic graft rupture after primary and revision anterior cruciate ligament reconstruction: retrospective analysis of incidence and risk factors in 2915 cases. Knee Surg Sports Traumatol Arthrosc. 2017;25:1535-1541. [DOI] [PubMed] [Google Scholar]
- 85. Schmale GA, Kweon C, Larson RV, Bompadre V. High satisfaction yet decreased activity 4 years after transphyseal ACL reconstruction. Clin Orthop Relat Res. 2014;472:2168-2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37:246-251. [DOI] [PubMed] [Google Scholar]
- 87. Shelbourne KD, Gray T, Wiley BV. Results of transphyseal anterior cruciate ligament reconstruction using patellar tendon autograft in tanner stage 3 or 4 adolescents with clearly open growth plates. Am J Sports Med. 2004;32:1218-1222. [DOI] [PubMed] [Google Scholar]
- 88. Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med. 1990;18:292-299. [DOI] [PubMed] [Google Scholar]
- 89. Shelbourne KD, Sullivan AN, Bohard K, Gray T, Urch SE. Return to basketball and soccer after anterior cruciate ligament reconstruction in competitive school-aged athletes. Sports Health. 2009;1:236-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73:712-716. [DOI] [PubMed] [Google Scholar]
- 91. Snaebjornsson T, Hamrin Senorski E, Sundemo D, et al. Adolescents and female patients are at increased risk for contralateral anterior cruciate ligament reconstruction: a cohort study from the Swedish National Knee Ligament Register based on 17,682 patients. Knee Surg Sports Traumatol Arthrosc. 2017;25:3938-3944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Sousa PL, Krych AJ, Cates RA, Levy BA, Stuart MJ, Dahm DL. Return to sport: does excellent 6-month strength and function following ACL reconstruction predict midterm outcomes? Knee Surg Sports Traumatol Arthrosc. 2017;25:1356-1363. [DOI] [PubMed] [Google Scholar]
- 93. Stanley LE, Kerr ZY, Dompier TP, Padua DA. Sex differences in the incidence of anterior cruciate ligament, medial collateral ligament, and meniscal injuries in collegiate and high school sports: 2009-2010 through 2013-2014. Am J Sports Med. 2016;44:1565-1572. [DOI] [PubMed] [Google Scholar]
- 94. Swenson DM, Collins CL, Best TM, Flanigan DC, Fields SK, Comstock RD. Epidemiology of knee injuries among U.S. high school athletes, 2005/2006-2010/2011. Med Sci Sports Exerc. 2013;45:462-469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Takazawa Y, Ikeda H, Saita Y, et al. Return to play of rugby players after anterior cruciate ligament reconstruction using hamstring autograft: return to sports and graft failure according to age. Arthroscopy. 2017;33:181-189. [DOI] [PubMed] [Google Scholar]
- 96. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43-49. [PubMed] [Google Scholar]
- 97. Tepolt FA, Feldman L, Kocher MS. Trends in pediatric ACL reconstruction from the PHIS database. J Pediatr Orthop. 2018;38:e490-e494. [DOI] [PubMed] [Google Scholar]
- 98. Thompson SM, Salmon LJ, Waller A, Linklater J, Roe JP, Pinczewski LA. Twenty-year outcome of a longitudinal prospective evaluation of isolated endoscopic anterior cruciate ligament reconstruction with patellar tendon or hamstring autograft. Am J Sports Med. 2016;44:3083-3094. [DOI] [PubMed] [Google Scholar]
- 99. Toole AR, Ithurburn MP, Rauh MJ, Hewett TE, Paterno MV, Schmitt LC. Young athletes cleared for sports participation after anterior cruciate ligament reconstruction: how many actually meet recommended return-to-sport criterion cutoffs? J Orthop Sports Phys Ther. 2017;47:825-833. [DOI] [PubMed] [Google Scholar]
- 100. Vavken P, Tepolt FA, Kocher MS. Concurrent meniscal and chondral injuries in pediatric and adolescent patients undergoing ACL reconstruction. J Pediatr Orthop. 2018;38:105-109. [DOI] [PubMed] [Google Scholar]
- 101. Webster KE, Feller JA. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44:2827-2832. [DOI] [PubMed] [Google Scholar]
- 102. Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:641-647. [DOI] [PubMed] [Google Scholar]
- 103. Welling W, Benjaminse A, Seil R, Lemmink K, Zaffagnini S, Gokeler A. Low rates of patients meeting return to sport criteria 9 months after anterior cruciate ligament reconstruction: a prospective longitudinal study. Knee Surg Sports Traumatol Arthrosc. 2018;26:3636-3644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Werner BC, Yang S, Looney AM, Gwathmey FW., Jr. Trends in pediatric and adolescent anterior cruciate ligament injury and reconstruction. J Pediatr Orthop. 2016;36:447-452. [DOI] [PubMed] [Google Scholar]
- 105. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44:1861-1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Willson JD, Dougherty CP, Ireland ML, Davis IM. Core stability and its relationship to lower extremity function and injury. J Am Acad Orthop Surg. 2005;13:316-325. [DOI] [PubMed] [Google Scholar]
- 107. Wylie JD, Hartley MK, Kapron AL, Aoki SK, Maak TG. Failures and reoperations after matrix-assisted cartilage repair of the knee: a systematic review. Arthroscopy. 2016;32:386-392. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, 37820_Appendix for One in 5 Athletes Sustain Reinjury Upon Return to High-Risk Sports After ACL Reconstruction: A Systematic Review in 1239 Athletes Younger Than 20 Years by Sue Barber-Westin and Frank R. Noyes in Sports Health: A Multidisciplinary Approach