Abstract
Background:
Current anterior cruciate ligament reconstruction (ACLR) guidelines utilize single-leg hop tests (SLHTs) to assist in return-to-sport decision making. A limb symmetry index (LSI) of ≥90% is often required; however, after ACLR, most youth athletes cannot achieve this standard. Reporting the performance of age-matched normative controls will allow clinicians to compare post-ACLR performance with noninjured peers, improving the utility of SLHTs. The purpose of this study was to report hop test LSI within healthy youth athletes and determine whether athlete performance surpasses post-ACLR requirements.
Hypothesis:
The LSI for the majority of healthy youth athletes will be ≥90%.
Study Design:
Cross-sectional cohort study.
Level of Evidence:
Level 3.
Methods:
Each participant performed a single hop (SH), triple hop (TrH), crossover hop (CrH), and timed hop (TiH). A 3-trial mean was utilized to calculate an LSI (nondominant/dominant leg [self-reported kicking leg]) for each hop. The frequency of pass/fail at ≥90% LSI was calculated. Pearson correlation coefficients analyzed the relationship between the different hops, and a 2-way analysis of variance determined the effects of age and sex on LSI.
Results:
A total of 340 participants (54% male; mean age, 10.9 ± 1.5 years; range, 8-14 years) were included. The mean LSI was >95% for each SLHT (SH, 97.9% [SD, 0.7]; TrH, 96.6% [SD, 0.6]; CrH, 96.8% [SD, 0.8]; TiH, 96.5% [SD, 0.6]). When analyzed as a test battery, only 45% of participants achieved this standard. Significantly weak to moderate correlations existed among hop tests (P < 0.01; r = 0.342-0.520). Age and sex had no effect on LSI (P < 0.05).
Conclusion:
While the mean LSI in our sample was >95% for each individual hop test, participant performance across all SLHT components varied, such that less than half of healthy athletes could achieve ≥90% LSI across all hops.
Clinical Relevance:
Current guidelines require ≥90% LSI on SLHTs. The majority of healthy youth athletes could not achieve this standard, which questions the validity of this LSI threshold in youth athletes after ACLR.
Keywords: anterior cruciate ligament, rehabilitation, functional hop testing
The incidence of anterior cruciate ligament (ACL) injuries and surgical reconstructions among adolescent athletes has been steadily increasing over the past 20 years.5,6,10,30,33 Because of the potential long-term consequences of early knee injuries, the rising rate of ACL injuries among pediatric or skeletally immature patients is of particular concern.37,44 Although historically ACL injuries within this population were treated nonoperatively, recent evidence suggesting higher rates of additional cartilage or meniscal injury2,22,36 and reduced activity levels within conservatively managed children36 has led most surgeons within the United States to prefer earlier surgical intervention.29,35,41 Current postoperative rehabilitation guidelines emphasize strength and functional performance testing to assist in the determination of recovery and ability to safely return to sports.46 Since being introduced in the early 1990s, the battery of single-leg hop tests (SLHTs) described by Barber et al3 and Noyes et al32 has become one of the most widely utilized functional performance tests after ACL reconstruction (ACLR).1,12,13 This test battery consists of 4 different single-leg hopping activities, and the patient’s performance is compared between the uninvolved and involved limbs to calculate a limb symmetry index (LSI). While the threshold of LSI required to return to sports activities is somewhat contested, most contemporary guidelines recommend an LSI of ≥90% as best practice.9,20,25,40,45 Interestingly, recent evidence demonstrates that after ACLR, a large proportion of pediatric athletes are unable to achieve ≥90% LSI on these and other physical performance tests near the time of return to sports.14,19,39 The low level of performance in postoperative cohorts questions the validity of these established performance requirements.
Data documenting normative hop test performance among uninjured peers would assist clinicians in the interpretation of recovery and patient function after ACLR. While these data are available for older high school and collegiate athletes,31 only limited published data documenting hop test performance in healthy pediatric athletes exist,4 and there are no studies that evaluate performance within this most frequently utilized SLHT battery. In addition, while several investigations have documented age- or sex-related differences in strength and neuromuscular control among pediatric athletes,4,17,23,30 to our knowledge, there have been no investigations evaluating the effect of these characteristics as they relate to SLHT LSI. Thus, the primary purpose of this study was to report SLHT performance within a group of uninjured pediatric athletes and establish normative LSI reference values. The secondary purpose was to evaluate the effects of sex or age on LSI performance.
Methods
The Children’s Hospital of Philadelphia Institutional Review Board reviewed and approved this research protocol prior to engagement. This was a single-episode, cross-sectional study of active, healthy youth athletes between the ages of 8 and 14 years. All data were collected on-site at athletic fields or courts during practice or between games during tournaments. To be eligible for the study, all adolescents had to be without any history of ACLR, no current lower extremity injuries, and presently participating in organized competitive sports. In addition, any athlete with a history of lower extremity injury within the past year and those with any type of neurological dysfunction or other medical issue that could affect function of their lower extremities or alter sports participation were excluded from this study.
Consent, demographics, injury history, and sports participation information were obtained first, followed by height, weight, and limb dominance. Limb dominance was determined by having each participant answer the question “Which leg would you use to kick a ball as far as you could?” Each participant received verbal and visual instruction in the performance of a series of SLHTs at the time of data collection. The battery of SLHTs included a single hop (SH), triple hop (TrH), crossover triple hop (CrH), and 6-m timed hop (TiH). The SH consists of a single hop for maximal distance, the TrH involves 3 consecutive maximal distance hops, and the CrH involves 3 maximal distance hops while obliquely crossing over a line 15 cm wide. In order for the hop test to be valid, the athlete was required to land in a controlled manner without any loss of balance or secondary hopping to steady oneself. Participants were allowed 2 to 5 practice trials for each hop, and limb testing order was determined by participant preference. For distance-based hops, the distance from the starting line to the participant’s heel was recorded to the nearest half-inch, then converted to centimeters prior to data analysis. For the TiH, participants were required to hop as fast they could, on a single leg, over a distance of 6 m. The time required to complete this task was recorded in seconds. The average distance or time of 3 successful trials was utilized for data analysis. An LSI was calculated using the formula (nondominant/dominant) × 100 for all hops with the exception of the TiH, which was expressed as (dominant/nondominant) × 100, as better performance on this test was indicated by a lower score (ie, decreased time taken to the complete task).
Statistical Analysis
Descriptive summary statistics of participant characteristics and frequency rates of primary sport were calculated. The calculated LSI served as the dependent variable for all analyses. Data were screened for normality using Kolmogorov-Smirnov tests and visual inspection of histrograms, while equality of variance was assessed with the Levene test. After the removal of outliers, all necessary assumptions were satisfied. Separate 2-way analyses of variance were performed to determine the effects of age and sex on each individual hop test LSI. The relationship between the LSI on the various hopping tests that make up the test battery were analyzed using Pearson correlation coefficients. As most contemporary guidelines recommend an LSI of ≥90% as satisfactory performance after ACLR,9,20,25,40,45 a “passing” threshold of ≥90% was selected to categorize participants into “passing” or “failing” categories. Frequency of pass/fail rates were calculated for each hop test and as a complete SLHT battery (ie, performance on all 4 hop tests). All statistical analyses were performed using SPSS Version 24.0 (IBM Corp). A P value of <0.05 was set a priori and considered statistically significant.
Results
A total of 347 athletes met the inclusion criteria; 7 athletes were excluded from analysis due to missing data, leaving a total of 340 participants. The sample was 54% male (n = 184), with a mean age 10.9 ± 1.5 years. Although most participants identified as multisport athletes, the top self-reported primary sports were soccer (52%; n = 178) and basketball (22%; n = 73). Complete demographic and descriptive data can be found in Table 1.
Table 1.
Patient demographics
| Age, y, mean ± SD | 10.9 ± 1.5 |
| Height, cm, mean ± SD | 146.6 ± 11.2 |
| Weight, kg, mean ± SD | 40.7 ± 10.8 |
| Body mass index, kg/m2, mean ± SD | 18.7 ± 3.09 |
| Sex, n (%) | |
| Male | 184 (54) |
| Female | 156 (46) |
| Race/ethnicity, n (%) | |
| Caucasian | 289 (85) |
| African American | 13 (3.8) |
| Asian | 9 (2.6) |
| Hispanic/Latino | 8 (2.4) |
| Primary sport, n (%) | |
| Soccer | 178 (52) |
| Basketball | 73 (22) |
| Baseball | 34 (10) |
| Football | 7 (2.1) |
| Lacrosse | 6 (1.8) |
| Other | 35 (10.3) |
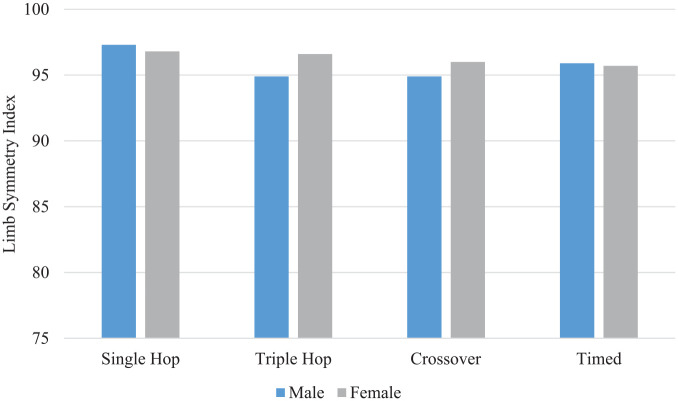
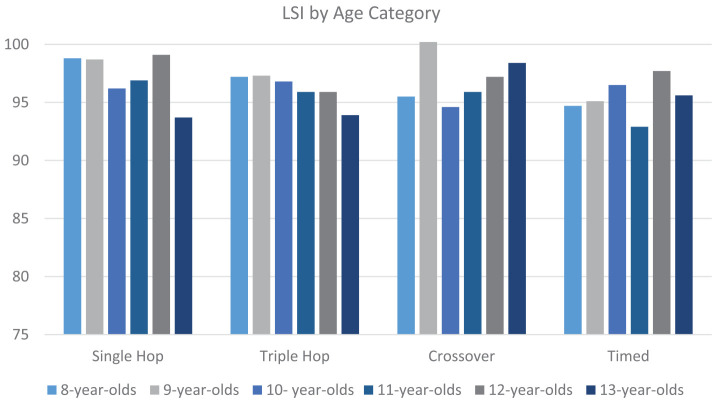
Across the entire sample, the mean LSI on each individual hop test indicated near symmetrical performance between limbs (SH [mean ± SD], 97.9% ± 13.3%; TrH, 96.6% ± 11.8%; CrH, 96.8% ± 15.4%; TiH, 96.5% ± 11.1%). Analysis of main effects of age or sex indicated that there were no significant differences in LSI for any of the SLHTs (Figures 1 and 2). Pearson analysis revealed statistically significant weak to moderate correlations among all hop tests (P < 0.01; r = 0.342-0.520) (Table 2).
Figure 1.
Single-leg hop test performance categorized by sex. Results of 2-way analysis of variance demonstrated no significant differences for any test: single hop (P = 0.990), triple hop (P = 0.105), crossover hop (P = 0.298), and timed hop (P = 0.524).
Figure 2.
Single-leg hop test performance categorized by age. Results of the 2-way analysis of variance demonstrated no significant differences between tests for any age group: single hop (P = 0.350), triple hop (P = 0.504), crossover hop (P = 0.892), and timed hop (P = 0.891). LSI, limb symmetry index.
Table 2.
Pearson correlation coefficient
| Single Hop | Triple Hop | Crossover Hop | Timed Hop | |
|---|---|---|---|---|
| Single hop | 1 | |||
| Triple hop | 0.477* (340) | 1 | ||
| Crossover hop | 0.404* (340) | 0.520* (340) | 1 | |
| Timed hop | 0.360* (339) | 0.469* (339) | 0.342* (339) | 1 |
The numbers in parentheses are the values of the Pearson correlation coefficient. The asterisks indicate statistically significant correlations.
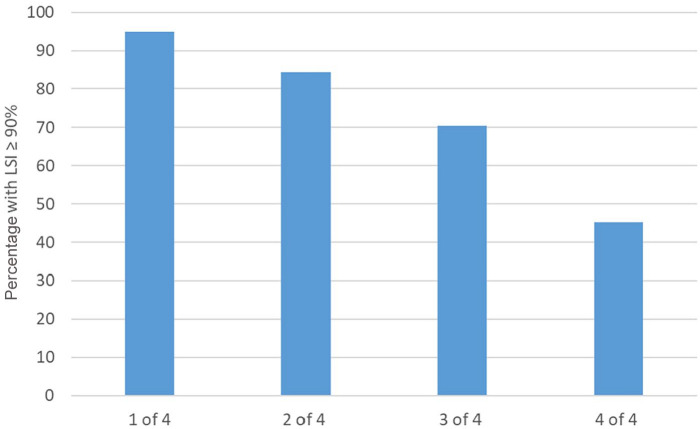
Analysis of performance, when dichotomized into “pass” or “fail” based on the achievement of ≥90 LSI, demonstrated a decreasing level of success when requiring passing more than 1 isolated component. While 95% of participants were able to achieve adequate performance on any one component of the SLHT, individual performance varied such that 84% passed 2 of 4 components, 71% passed 3 of 4 components, and only 45.1% were able to achieve satisfactory performance on all 4 components of the test battery (Figure 3).
Figure 3.
Percentage of participants meeting recommended return-to-sport criteria of ≥90% limb symmetry index (LSI) on progressive components of the hop test battery.
Discussion
The main purpose of this study was to examine the capacity for uninjured youth athletes to achieve a threshold of performance (ie, ≥90% LSI) on a battery of SLHTs commonly utilized to evaluate an athlete’s readiness to return to sports after ACLR. While a high proportion of these athletes were able to achieve satisfactory levels of performance on isolated tests, when utilized as a test battery requiring ≥90% LSI on all hop tests, only 45% of the sample was able to achieve this standard.
The development of a return-to-sport assessment protocol that is capable of identifying athletes with low levels of performance and high risk of secondary injury after ACLR is a goal of utmost importance. While there is no agreement on an ideal testing protocol, SLHTs are almost universally adopted as a necessary component of functional performance testing to assist in return-to-play decision making after ACLR.9,12,13,25 The battery of hop tests used within the present study have demonstrated good discriminative accuracy and predictive abilities7,24,32; however, the clinical utility of these and other commonly utilized return-to-sports assessment methods have recently been questioned due to a lack of association with secondary ACL injury risk.26,27,34,42 In addition, several reports have identified that many athletes cleared to return to sports after ACLR are unable to achieve the contemporary standard of ≥90% LSI,11,14,27,39 further challenging the clinical utility of these measures and raising concerns about the validity of the 90% LSI criteria to which post-ACLR athletes are held.
The standard of ≥90% LSI is of particular interest within the skeletally immature youth population, as this demographic demonstrates increasing frequency of ACL injuries5,10,28 and only a limited pool of performance-related outcomes research exists. While many published protocols specifically designed to be employed with skeletally immature athletes require LSI values of ≥90%,46 our results indicate that the majority of healthy athletes are unable to perform at these standards on the complete test battery. Interestingly, the level of performance within this healthy cohort is similar to published values within patients after ACLR. Toole et al39 recently conducted a prospective cohort study evaluating SLHT performance in 115 youth athletes (mean age, 17.5 years) 8.2 months after ACLR. Similar to the current study, patients within the Toole et al cohort were able to achieve ≥90% LSI on each hop test (SH, 93.7%; TrH, 94.9%; CrH, 92.8%; TiH, 96.3%); however, only 53% of the sample achieved this threshold on all hop tests combined.
While Toole et al39 did not specifically investigate the relationship between hop tests, it appears the weak to moderate correlations between hop tests noted within our healthy cohort are consistent with performance post-ACLR. The low correlations and within-participant variability in hop test performance suggests these tests may assess different constructs of performance in both healthy and ACLR individuals and supports practice recommendations calling for use of the full battery of hop tests to obtain a well-rounded view of athlete performance during return-to-play assessments.9,21,25 Nonetheless, our data suggest that clinicians should expect variability in test performance and perhaps consider performance criteria references differently based on how the individual clinician is utilizing the test components. For example, a recent survey of physical therapists indicated that only 27% of clinicians utilized all 4 components of this series of hop tests within routine clinical practice.13 The data within the current study indicate that if a clinician is only using a single test, holding the patient accountable to a stringent ≥90% LSI performance level is a valid indicator of normal performance. However, if utilizing the complete test battery, our results question the validity of holding a young individual post-ACLR to this threshold of ≥90% LSI on all 4 tests, as only 45% of our healthy participants were able to achieve such performance.
Our results may help explain why other studies have identified similar low functional hop test “passing” rates within ACLR populations11,14,43 and why a recent systematic review and meta-analysis identified that only 23% of patients post-ACLR are able to pass return-to-play assessments at a 90% LSI threshold.42 Future research should seek to determine whether other factors such as strength or balance may affect hop test performance within young athletes and focus on examining hop test performance across a wider age range of healthy individuals. This information will help derive a standard of normal performance to improve functional testing interpretation and the utility of these tests in return-to-play decision making.
Comparison of hop test performance to age-matched athletes is difficult, as there is variability in specific hop testing protocols and a limited number of studies focusing on skeletally immature athletes. Recently, Sugimoto et al38 analyzed hop test performance using the same battery of tests within 2 groups of pediatric patients (n = 93; mean age, 12.5-13.6 years) 6 months after ACLR. They found comparable levels of performance with our healthy sample, with limb symmetry values ranging from 89.3% to 98.1% on isolated hop tests. Similarly, Ithurburn et al19 published data from a prospective cohort study of post-ACLR youth athletes (n = 16; mean age, 12.9 years), showing that the majority of patients (88% to 100%) were able to achieve >90% LSI on isolated components of the same hop test battery for all hops, with the exception of the TiH, of which only 81% of their sample achieved this threshold. Unfortunately, neither study included frequency counts of individual patients able to achieve a threshold of ≥90% LSI on the entire battery of tests, which limits our ability to make further comparisons between those data and the current study.
Ekas et al11 recently published a case series evaluating the functional abilities of a cohort of young athletes who sustained an ACL injury before the age of 13 years. Among this group of patients, the mean age at the time of injury was 11 years, and the average follow-up occurred 8 years postinjury, yielding a mean age of 19.1 years at time of testing. A total of 44 patients were seen at final follow-up, with 54.5% (n = 24) of them undergoing surgical reconstruction approximately 4 years prior to data collection. Results demonstrated that patients in the conservative treatment group had a mean LSI of 94% to 95.8% on individual hop tests; however, only 50% (10/20) were able to achieve ≥90% LSI across all 4 hop tests. Similarly, among those patients who underwent ACLR, the mean LSI ranged from 88.2% to 94.4% on isolated tests, but only 29.2% of patients (7/24) achieved ≥90% across the entire test battery.
Taken together, the data within the current study and previously published cohorts show a similar trend in which a high percentage of young athletes can achieve ≥90% LSI on isolated hop tests; however, performance varies in such a way that most of them are unable to achieve this standard across all hop test dimensions. This trend seems to remain consistent whether the athletes are healthy, have undergone ACLR, or have been treated conservatively. The 90% LSI is a commonly cited criterion utilized to progress athletes to sports-related activities after ACLR. The low “passing” rate of our healthy athletes may help explain the low rate of passing among ACLR individuals and supports the need to improve the methods we utilize to assess an athlete’s performance after ACLR.
This study is not without limitations. All data collection occurred on-site at athletic competitions, and therefore, the playing surface varied between data collection outings. It is possible that the variability in hop testing surface (grass vs gym floor vs turf) and shoe wear (cleats vs sneaker) may have affected hop test performance. While the number of hop test practice trials was controlled, the level of participant activity prior to engaging in data collection was not. Thus, it is possible that participants were tested at variable levels of fatigue, which may have affected their overall hop test performance. However, it is unlikely that preexisting fatigue related to sports participation would have selectively affected one limb more than the other. Given that the main dependent variable in this study was a comparison of between-limb performance, it is felt that any effects related to fatigue would be minimal. Similarly, while varying methods of determining limb dominance have been described,15,18 because of the high degree of limb symmetry on each individual testing parameter, the choice of limb dominance determination used would not affect the results of the current study. While the hop test battery utilized in this study has demonstrated high intra- and interrater reliability, with intraclass correlation coefficient values ranging from 0.88 to 0.97,8 the authors did not perform an independent reliability study, which may affect the generalizability of the data. Last, although this study characterizes hop test performance among healthy individuals, it is unknown whether the 65% of individuals who were unable to achieve ≥90% LSI on the hop test battery are at an elevated risk of sustaining an ACL injury. While previous research has shown single-leg hop tests cannot reliably predict future knee injury in athletes,16 this may be a factor to consider and suggests future research analyzing this possibility be conducted.
Conclusion
This study describes the abilities of a large group of healthy, young athletes to achieve ≥90% LSI on a battery of single-leg hop tests commonly utilized to assess patient performance prior to returning to unrestricted sports after ACLR. Athlete age or sex did not affect hop test LSI performance. While a high percentage of participants were able to achieve ≥90% LSI on any one component of the hop test battery, less than half of participants were able to achieve this standard across all 4 hop tests. The results of this study question the validity of holding young post-ACLR individuals accountable to achieving a ≥90% LSI on all components of the hop test battery, as the majority of their healthy counterparts cannot. Future research evaluating the criteria standards and interpretation of functional hop testing among different-aged populations is necessary to improve the clinical utility of these measures.
Acknowledgments
We would like to thank Benjamin Ruley, Miranda Dabbous, and Gabriella Marinaccio for their assistance with data collection for this study.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Abrams GD, Harris JD, Gupta AK, et al. Functional performance testing after anterior cruciate ligament reconstruction: a systematic review. Orthop J Sports Med. 2014;2:2325967113518305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Anderson AF, Anderson CN. Correlation of meniscal and articular cartilage injuries in children and adolescents with timing of anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:275-281. [DOI] [PubMed] [Google Scholar]
- 3. Barber SD, Noyes FR, Mangine RE, McCloskey JW, Hartman W. Quantitative assessment of functional limitations in normal and anterior cruciate ligament-deficient knees. Clin Orthop Relat Res. 1990;255:204-214. [PubMed] [Google Scholar]
- 4. Barber-Westin SD, Noyes FR, Galloway M. Jump-land characteristics and muscle strength development in young athletes: a gender comparison of 1140 athletes 9 to 17 years of age. Am J Sports Med. 2006;34:375-384. [DOI] [PubMed] [Google Scholar]
- 5. Beck NA, Lawrence JTR, Nordin JD, DeFor TA, Tompkins M. ACL tears in school-aged children and adolescents over 20 years. Pediatrics. 2017;139:e20161877. [DOI] [PubMed] [Google Scholar]
- 6. Beynnon BD, Vacek PM, Newell MK, et al. The effects of level of competition, sport, and sex on the incidence of first-time noncontact anterior cruciate ligament injury. Am J Sports Med. 2014;42:1806-1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bolgla LA, Keskula DR. Reliability of lower extremity functional performance tests. J Orthop Sports Phys Ther. 1997;26:138-142. [DOI] [PubMed] [Google Scholar]
- 8. Brosky JA, Jr, Nitz AJ, Malone TR, Caborn DN, Rayens MK. Intrarater reliability of selected clinical outcome measures following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1999;29:39-48. [DOI] [PubMed] [Google Scholar]
- 9. Dingenen B, Gokeler A. Optimization of the return-to-sport paradigm after anterior cruciate ligament reconstruction: a critical step back to move forward. Sports Med. 2017;47:1487-1500. [DOI] [PubMed] [Google Scholar]
- 10. Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42:675-680. [DOI] [PubMed] [Google Scholar]
- 11. Ekas GR, Moksnes H, Grindem H, Risberg MA, Engebretsen L. Coping with anterior cruciate ligament injury from childhood to maturation: a prospective case series of 44 patients with mean 8 years’ follow-up. Am J Sports Med. 2019;47:22-30. [DOI] [PubMed] [Google Scholar]
- 12. Greenberg EM, Greenberg ET, Albaugh J, Storey E, Ganley TJ. Anterior cruciate ligament reconstruction rehabilitation clinical practice patterns: a survey of the PRiSM Society. Orthop J Sports Med. 2019;7:2325967119839041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Greenberg EM, Greenberg ET, Albaugh J, Storey E, Ganley TJ. Rehabilitation practice patterns following anterior cruciate ligament reconstruction: a survey of physical therapists. J Orthop Sports Phys Ther. 2018;48:801-811. [DOI] [PubMed] [Google Scholar]
- 14. Greenberg EM, Greenberg ET, Ganley TJ, Lawrence JT. Strength and functional performance recovery after anterior cruciate ligament reconstruction in preadolescent athletes. Sports Health. 2014;6:309-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gresham-Fiegel CN, House PD, Zupan MF. The effect of nonleading foot placement on power and velocity in the fencing lunge. J Strength Cond Res. 2013;27:57-63. [DOI] [PubMed] [Google Scholar]
- 16. Hegedus EJ, McDonough S, Bleakley C, Cook CE, Baxter GD. Clinician-friendly lower extremity physical performance measures in athletes: a systematic review of measurement properties and correlation with injury, part 1. The tests for knee function including the hop tests. Br J Sports Med. 2015;49:642-648. [DOI] [PubMed] [Google Scholar]
- 17. Hewett TE, Myer GD, Ford KR. Decrease in neuromuscular control about the knee with maturation in female athletes. J Bone Joint Surg Am. 2004;86:1601-1608. [DOI] [PubMed] [Google Scholar]
- 18. Huurnink A, Fransz DP, Kingma I, Hupperets MD, van Dieen JH. The effect of leg preference on postural stability in healthy athletes. J Biomech. 2014;47:308-312. [DOI] [PubMed] [Google Scholar]
- 19. Ithurburn MP, Paljieg A, Thomas S, Hewett TE, Paterno MV, Schmitt LC. Strength and function across maturational levels in young athletes at the time of return to sport after ACL reconstruction. Sports Health. 2019;11:324-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Joreitz R, Lynch A, Rabuck S, Lynch B, Davin S, Irrgang J. Patient-specific and surgery-specific factors that affect return to sport after ACL reconstruction. Int J Sports Phys Ther. 2016;11:264-278. [PMC free article] [PubMed] [Google Scholar]
- 21. Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50:946-951. [DOI] [PubMed] [Google Scholar]
- 22. Lawrence JT, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med. 2011;39:2582-2587. [DOI] [PubMed] [Google Scholar]
- 23. Lephart SM, Ferris CM, Riemann BL, Myers JB, Fu FH. Gender differences in strength and lower extremity kinematics during landing. Clin Orthop Relat Res. 2002;401:162-169. [DOI] [PubMed] [Google Scholar]
- 24. Logerstedt D, Grindem H, Lynch A, et al. Single-legged hop tests as predictors of self-reported knee function after anterior cruciate ligament reconstruction: the Delaware-Oslo ACL cohort study. Am J Sports Med. 2012;40:2348-2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Logerstedt DS, Snyder-Mackler L, Ritter RC, Axe MJ, Godges JJ; Orthopaedic Section of the American Physical Therapist Association. Knee stability and movement coordination impairments: knee ligament sprain. J Orthop Sports Phys Ther. 2010;40:A1-A37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Losciale JM, Bullock G, Cromwell C, Ledbetter L, Pietrosimone L, Sell TC. Hop testing lacks strong association with key outcome variables after primary anterior cruciate ligament reconstruction: a systematic review. Am J Sports Med. 2020;48:511-522. [DOI] [PubMed] [Google Scholar]
- 27. Losciale JM, Zdeb RM, Ledbetter L, Reiman MP, Sell TC. The association between passing return-to-sport criteria and second anterior cruciate ligament injury risk: a systematic review with meta-analysis. J Orthop Sports Phys Ther. 2019;49:43-54. [DOI] [PubMed] [Google Scholar]
- 28. Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91:2321-2328. [DOI] [PubMed] [Google Scholar]
- 29. Milewski MD, Beck NA, Lawrence JT, Ganley TJ. Anterior cruciate ligament reconstruction in the young athlete: a treatment algorithm for the skeletally immature. Clin Sports Med. 2011;30:801-810. [DOI] [PubMed] [Google Scholar]
- 30. Myer GD, Sugimoto D, Thomas S, Hewett TE. The influence of age on the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a meta-analysis. Am J Sports Med. 2013;41:203-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Myers BA, Jenkins WL, Killian C, Rundquist P. Normative data for hop tests in high school and collegiate basketball and soccer players. Int J Sports Phys Ther. 2014;9:596-603. [PMC free article] [PubMed] [Google Scholar]
- 32. Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19:513-518. [DOI] [PubMed] [Google Scholar]
- 33. Padua DA, DiStefano LJ, Hewett TE, et al. National Athletic Trainers’ Association position statement: prevention of anterior cruciate ligament injury. J Athl Train. 2018;53:5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Paterno MV, Rauh M, Thomas S, Hewett TE, Schmitt L. Current return to sport criteria after ACL reconstruction fail to identify increased risk of second ACL injury in young athletes. Orthop J Sports Med. 2018;6 (7 suppl 4):2325967118S2325900060. [Google Scholar]
- 35. Popkin CA, Wright ML, Pennock AT, et al. Trends in management and complications of anterior cruciate ligament injuries in pediatric patients: a survey of the PRiSM Society. J Pediatr Orthop. 2018;38:e61-e65. [DOI] [PubMed] [Google Scholar]
- 36. Ramski DE, Kanj WW, Franklin CC, Baldwin KD, Ganley TJ. Anterior cruciate ligament tears in children and adolescents: a meta-analysis of nonoperative versus operative treatment. Am J Sports Med. 2014;42:2769-2776. [DOI] [PubMed] [Google Scholar]
- 37. Shaw L, Finch CF. Trends in pediatric and adolescent anterior cruciate ligament injuries in Victoria, Australia 2005-2015. Int J Environ Res Public Health. 2017;14:599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sugimoto D, Heyworth BE, Collins SE, Fallon RT, Kocher MS, Micheli LJ. Comparison of lower extremity recovery after anterior cruciate ligament reconstruction with transphyseal hamstring versus extraphyseal iliotibial band techniques in skeletally immature athletes. Orthop J Sports Med. 2018;6:2325967118768044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Toole AR, Ithurburn MP, Rauh MJ, Hewett TE, Paterno MV, Schmitt LC. Young athletes cleared for sports participation after anterior cruciate ligament reconstruction: how many actually meet recommended return-to-sport criterion cutoffs? J Orthop Sports Phys Ther. 2017;47:825-833. [DOI] [PubMed] [Google Scholar]
- 40. van Melick N, van Cingel RE, Brooijmans F, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;50:1506-1515. [DOI] [PubMed] [Google Scholar]
- 41. Vavken P, Murray MM. Treating anterior cruciate ligament tears in skeletally immature patients. Arthroscopy. 2011;27:704-716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Webster KE, Hewett TE. What is the evidence for and validity of return-to-sport testing after anterior cruciate ligament reconstruction surgery? A systematic review and meta-analysis. Sports Med. 2019;49:917-929. [DOI] [PubMed] [Google Scholar]
- 43. Wellsandt E, Failla MJ, Snyder-Mackler L. Limb symmetry indexes can overestimate knee function after anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2017;47:334-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Werner BC, Yang S, Looney AM, Gwathmey FW., Jr. Trends in pediatric and adolescent anterior cruciate ligament injury and reconstruction. J Pediatr Orthop. 2016;36:447-452. [DOI] [PubMed] [Google Scholar]
- 45. Wilk KE, Arrigo CA. Rehabilitation principles of the anterior cruciate ligament reconstructed knee: twelve steps for successful progression and return to play. Clin Sports Med. 2017;36:189-232. [DOI] [PubMed] [Google Scholar]
- 46. Yellin JL, Fabricant PD, Gornitzky A, et al. Rehabilitation following anterior cruciate ligament tears in children: a systematic review. JBJS Rev. 2016;4:01874474-201601000-00004. [DOI] [PubMed] [Google Scholar]