Abstract
The coronavirus disease 2019 (COVID-19), which is caused by a novel coronavirus (SARS-COV-2), has compromised health care systems and normal management of patients with cardiovascular diseases [1–3]. Patients with non-communicable diseases, including acute myocardial infarction (AMI) are vulnerable to this stress [4, 5]. Acute ST segment elevation myocardial infarction (STEMI), the most critical type of AMI, is associated with high mortality even with modern medicine [6–8]. Timely reperfusion therapy is critical for STEMI patients because a short ischemia time is associated with better clinical outcomes and lower acute and long -term mortality [9–12]. The COVID-19 pandemic placed the management of STEMI patients in a difficult situation due to the need to balance timely reperfusion therapy and maintaining strict infection control practices [13, 14]. Telemedicine, which is used to deliver health care services using information or communication technology, provides an opportunity to carry out the evaluation, diagnosis, and even monitor the patients after discharge when social distancing is needed [15]. In this article, we reported our preliminary experience with the usefulness of telemedicine in managing STEMI patients during the COVID-19 pandemic. We also provided a review of this topic.
Keywords: ST segment elevation myocardial infarction, Telemedicine, COVID-19, Door-to-balloon time
The COVID-19 pandemic impact on STEMI patient management
The adverse impact of the COVID-19 pandemic on the normal management of STEMI patients includes decreased numbers of STEMI admissions and catheter activation, prolonged systemic delay, altered reperfusion strategies, increased psychological stress in hospitalized patients, and disruption in cardiac rehabilitation programs.
Decreased numbers of STEMI admissions and catheter activations during the pandemic
The incidence rate of STEMI should be relatively stable in the current society or possibly even higher due to increased psychological stress and lack of exercise due to “lockdown policies” [16, 17]. However, reduced STEMI patients admissions were observed in multiple studies. Zitelny E, et al. reported a 14.6% drop in STEMI admissions in the first three months of 2020 compared with the same period in 2019, even in a region with a relatively low burden of confirmed COVID-19 cases [18]. Zaleski AL, et al. reported a 16 to 38% reduction in STEMI activation per month [19]. De Filippo O, et al. performed a retrospective analysis of clinical and angiographic characteristics of consecutive patients who were admitted for acute coronary syndrome (ACS) at 15 hospitals in northern Italy during the COVID-19 pandemic. They compared the hospitalization rates between the study period and two control periods that included a corresponding period during the previous year (February 20 to March 31, 2019) and an earlier period during the same year (January 1 to February 19, 2020) [20]. The mean admission rate for ACS during the study period was 13.3 admissions per day, which was significantly lower than the rate during the earlier period in the same year (18.0 admissions per day) or the rate during the previous year (18.9 admissions per day) [20]. Later, a survey that attempted to assess the impact of the COVID-19 pandemic on STEMI patient admissions demonstrated that 78.8% of the health professionals who responded indicated that the number of patients presenting with STEMI was reduced, and 65.2% of health professionals believed that the reduction in STEMI presentations was greater than 40% [21]. The underlying reasons for the reduction in STEMI admissions included the fear of cross-infection and failure to distinguish cardiac ischemia and COVID-19 related symptoms [22–24].
A reduction in total numbers of STEMI patients who underwent primary percutaneous coronary intervention (PCI) also was observed in several studies. Mayol J et al. reported a 51.2% reduction in PCI for STEMI patients in Latin America during the pandemic [25]. Garcia S, et al. estimated that STEMI patients who underwent primary PCI decreased by approximately 38% in the United States of America during the COVID-19 pandemic [26]. The decrease in primary PCI was associated with a total reduction of STEMI admissions and an increased rate of fibrinolytic treatment or other conservative medical therapies during the pandemic [27]. In a retrospective study conducted by Primessnig U, et al. showed that significantly less patients with AMI were admitted during the pandemic [28].
Prolonged systemic delay in STEMI patients during the pandemic
Multiple investigators have reported increased systemic delay for STEMI patients who underwent primary PCI since the outbreak of the COVID-19 pandemic. Abdelaziz HK, et al. reported a significantly longer symptom-to-first medical contact (FMC) time in STEMI patients during the COVID-19 pandemic (227 [65–790] vs. 119 [27–203] min, P=0.01) and 26.1% of STEMI patients experienced late presentation (symptom-to-FMC time that was greater than 12 h) during the COVID-19 pandemic compared with 0% of STEMI patients who experienced late presentation before the pandemic [29]. Gramegna M, et al. reported that 50% of STEMI patients experienced late presentation during the COVID-19 pandemic compared with 4.8% with late presentation before the COVID-19 pandemic [30]. Tam CF, et al. reported significant post-hospital delays in STEMI patients due to the implementation of necessary infection control measures [31]. In a study performed at our center, prolonged pre- and post-hospital delays were observed with STEMI patients during the COVID-19 pandemic compared with patients before the pandemic [32]. This prolonged systemic delay during the pandemic would ultimately cause adverse clinical outcomes [33].
Altered reperfusion strategies in STEMI patients during the COVID-19 pandemic
Reperfusion therapy, including primary PCI and fibrinolytic therapy, are key therapeutic procedures for STEMI patients [9–11]. The essential goal to achieve better clinical outcomes is to reduce the total ischemia time as much as possible [12, 13]. Current guidelines indicate that primary PCI is the preferred reperfusion therapy because it provides improved clinical benefits with lower rates of re-infarction and bleeding compared with fibrinolytic therapy [9–11]. However, it is still controversial whether primary PCI is the preferred reperfusion therapy during the COVID-19 pandemic when the clinical benefit is largely dependent on rapidly achieving FMC-to-device time within 90 to 120 min [34]. The COVID-19 pandemic has significantly increased the post-hospital delay because isolation catheter labs are not as available, and increased infection control measures are necessary. Experts from China have recommended that fibrinolytic therapy should be considered the first-line therapy during the COVID-19 pandemic [35]. In a retrospective study from our center (paper in submission), fibrinolytic therapy combined with deferred PCI within 24 h resulted in better post-procedure thrombolysis in myocardial infarction (TIMI) flow and similar in-hospital adverse clinical outcomes compared with primary PCI when the screening protocol was used during the pandemic.
Increased adverse psychological stress in hospitalized STEMI patients during the COVID-19 pandemic
The COVID-19 pandemic is a major health crisis resulting in excessive adverse psychological stress in the general population as well as in health care providers. For hospitalized patients, this impact is increasingly evident due to their isolation and when accompanied by any preexisting mental illness [36–38]. This psychological stress can compromise adherence to treatment protocols and subsequently increase the incidence risk of major cardiovascular events [39, 40].
Disrupted cardiac rehabilitation programs
Cardiac rehabilitation (CR) is a valuable treatment and plays an essential role in managing patients experiencing a broad spectrum of cardiovascular diseases [41]. Current guidelines highlight the importance of CR in patients with acute myocardial infarction [9–11]. A typical CR program consists of inpatient rehabilitation and post-discharge rehabilitation, which provide clinical benefits to patients with cardiovascular disease [42, 43]. Both in-hospital and post-discharge CR programs have been compromised due to the COVID-19 pandemic due to the necessary infection control measures.
The role of telemedicine in managing STEMI patients during the COVID-19 pandemic
As mentioned above, the main reasons for the reduction in STEMI admissions are the fear of infection and limited medical knowledge concerning STEMI. Telemedicine provides an alternative avenue to provide medical education for STEMI patients and avoid unnecessary mortality. Observational studies and meta-analyses have revealed that telemedicine can be used to reduce the pre-hospital delay for patients who underwent primary PCI [32, 44–46]. Telemedicine services also provide additional clinical information, which can help cardiologists carry out diagnoses and differential diagnoses without in-person visits [47, 48]. Remote patient monitoring is another promising aspect of telemedicine, which involves more complex strategies, including smartphone applications (apps), global positioning systems (GPS), and Bluetooth technologies [49–51]. The efficacy of remote telemedicine monitoring in improving clinical outcomes for patients with cardiovascular disease has been discussed previously [52–54]. Because health care services will continue to be compromised during the COVID-19 pandemic, telemedicine provided an effective method to manage patients with cardiovascular disease, including online consultation, video inquiry, internet-based drug prescriptions, pre-hospital diagnoses and patient distribution, post-discharge patient follow up, and CR monitoring.
Preliminary experiences with using telemedicine to manage STEMI patients at our center
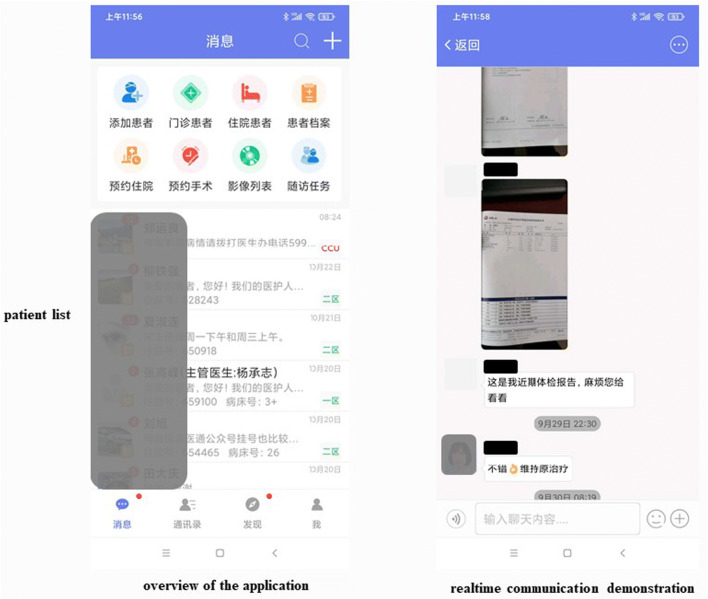
The Tiantanzhixin application (app) is a smartphone-based interactive application developed by the department of cardiovascular and macrovascular disease, Beijing Tiantan Hospital, Capital Medical University. It was launched in August 2019, and more than 6000 patients who have visited our out-patient clinic or were hospitalized in our patient ward have been registered in the program (Fig. 1). This free-of-charge application allows real-time, two-way communication between registered patients and doctors from our center. We compared the critical time interval and clinical outcomes for STEMI patients who used the app with those who did not. The patients who used the app exhibited shorter systemic delays compared to those who did not [32]. Although the short-term adverse clinical outcomes were comparable between the two groups, results from the three-month follow-up interactions indicated that the STEMI patients who used the app presented higher left ventricular ejection fractions and lower left ventricular end-diastolic diameters (paper in submission).
Fig. 1.
Cockpit view of the control panel for the Tiantanzhixin app
This app also allows online communication between patients’ registered relatives and the doctor in charge of the patient, which helps reduce the psychological stress for the patients and their relatives. The use of the app also increased patient satisfaction during hospitalization (paper in submission). Finally, this app could facilitate STEMI patients to remotely perform the CR programs and optimize medical therapies through online and video chats (Fig. 2).
Fig. 2.
Screenshots of the Tiantanzhixin app
Other designated telemedicine tools besides the Tiantanzhixin app have been shown to be effective in managing patients with different types of cardiovascular disease. Liu H et al. reported that pre-hospital electrocardiography (ECG) transfer using the Wechat app (a popular social media application in China) resulted in earlier reperfusion of ST elevation myocardial infarction patients who were transferred from the non-percutaneous coronary intervention center [55]. Hur S et al. observed that the automated Fast Healthcare Interoperability Resources (FHIR)-based 12-lead ECG mobile alert system was successfully implemented in an emergency department, especially for older patients [56]. In a study that enrolled 897 suitable AMI patients, Ben-Assa E, et al. demonstrated that telemedicine technology exhibited considerable promise in reducing 30-day readmission rates for post-AMI patients [57]. The efficacy and safety of telemedicine in managing hypertension have been proven in multiple studies [58–61]. Recently, a meta-analysis revealed that telemedicine positively affected blood pressure control and could be a promising alternative in managing hypertension [62]. The potential role of telemedicine in managing heart failure patients has also been reported in multiple articles. Frederix I, et al. revealed that an initial six-month telemonitoring program was not associated with a reduction in mortalities from all causes in chronic heart failure patients at long-term follow-up [63]. However, they did observe a reduced number of days lost due to heart failure readmissions [63].
The telemedical interventional management in heart failure II (TIM-HF2) is a randomized, controlled, parallel-group, unmasked trial, which indicated that a structured remote patient management intervention, when used in a well-defined heart failure population, could reduce the percentage of days lost due to unplanned cardiovascular hospital admissions and mortality of all-causes [64]. Guo X et al. demonstrated the efficacy of a hospital-community-family-based telehealth program for patients with chronic heart failure [65]. The efficacy of telemedicine in patients with arrhythmia also was proven in several studies. The mAF App trial was based on a smartphone AF app (mAFA) designed to incorporate clinical decision-support tools. The pilot mAFA trial was the first prospective randomized trial using mobile health technology in patients with atrial fibrillation [66]. The results demonstrated that the mAF app, with integration of clinical decision support, education, and patient involvement strategies, significantly improved patient knowledge, drug adherence, quality of life, and anticoagulation outcomes [66]. The Apple Heart Study is a large-scale, app-based study that has been carried out to identify cardiac arrhythmias using a smartwatch, which will provide the initial evidence that a smartwatch algorithm can identify pulse irregularity and variability, which might reflect previously unknown atrial fibrillation [67]. The detailed functional comparisons for the Tiantanzhixin app and other different types of telemedicine tools are shown in Table 1.
Table 1.
Functional comparison of the Tiantanzhixin app and other telemedicine tools used to manage patients with cardiovascular diseases
| Name of the telemedicine | Type of telemedicine | Target population | Medical education | Pre-hospital diagnose and evaluation | ECG transmission | Online consult | Medical professionals online service | Vital signs and test results monitor during hospitalization | Vital signs monitor after discharge | Cardiac follow up after discharge |
|---|---|---|---|---|---|---|---|---|---|---|
| Tiantanzhixin App | Smartphone application | All | √ | √ | √ | √ | √ | × | × | √ |
| Social media App (Wechat,Ticktock,Facebook,etc) | Smartphone application | All | √ | √ | √ | × | × | × | × | × |
| Brunetti et al | Pre-hospital transmission | Acute myocardial infarction patients | × | √ | √ | × | × | × | × | × |
| Boman, et al | consultation | All | × | √ | × | × | × | × | × | × |
| Corrie Health Digital Platform (iShare) | Smartphone application | Acute myocardial infarction patients | √ | × | NA | √ | NA | × | √ | √ |
| iVitality app | Smartphone application, website, BP monitor | Hypertension patients | × | × | × | × | × | NA | √ | × |
| Medisafe app | Smartphone application | Hypertension patients | √ | × | × | × | × | × | × | × |
| CONNECT website/app | Website and Smartphone application | All | √ | × | × | × | × | NA | √ | NA |
| CardioMobile | Smartphone application | Cardiac rehabilitation after PCI or ACS | √ | × | × | × | × | NA | √ | √ |
| EU-CaRE | Smartphone, HR monitor | Older patients who declined traditional cardiac rehabilitation | √ | × | × | × | × | NA | √ | √ |
| iCor | Tablet with Bluetooth connection to BP monitor, scale; video conferencing | Symptomatic heart failure patients | √ | × | × | NA | NA | NA | √ | √ |
| CarePartner | Interactive automated voice response calls, automated e-mails | heart failure patients | NA | × | × | × | × | × | × | × |
| mAFA | smartphone application | Atrial fibrillation patients | √ | × | × | × | × | NA | √ | × |
| mSTOPS | Portable ECG (iRhythm Zio) self-applied patch | Atrial fibrillation patients | × | × | × | × | × | NA | √ | × |
| eMocial | smartphone-based support tool | ACS patients | × | × | NA | NA | × | NA | √ | × |
A proposed telemedicine-based protocol to manage STEMI patients during the COVID-19 pandemic
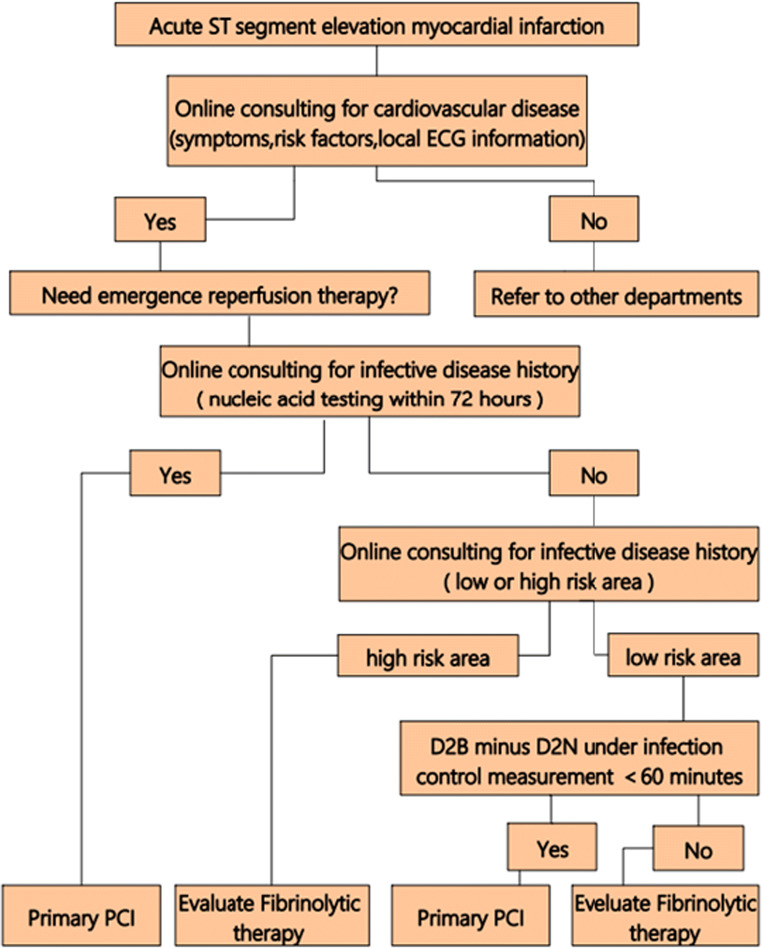
The COVID-19 pandemic has changed the normal medical services and telemedicine, and these techniques offer alternative strategies to evaluate patients and help doctors make better decisions for their patients, especially when social distancing is necessary. Thus, we have proposed a telemedicine-based protocol to manage STEMI patients during the COVID-19 pandemic, illustrated in Fig. 3.
Fig. 3.
Telemedicine-based management protocol used with STEMI patients during the COVID-19 pandemic. D2B:door-to-balloon time, D2N:door-to-needle time
Future prospects for telemedicine to successfully manage STEMI patients during the COVID-19 pandemic
The COVID-19 pandemic has resulted in reduced numbers of STEMI admissions and catheter activation. The pandemic also has prolonged the systemic delay before and after hospitalization. To resolve these issues, improved essential medical education is needed for high-risk patients, especially patients who have experienced STEMI. With the help of modern technology, telemedicine could provide needed medical services without in-person visits. Wearable medical devices could provide additional patient information, including heart rate, body weight, blood pressure, and others [68–71]. Also, 5G, virtual reality could be used in telemedicine [72, 73].
The need to pool data from multiple sources also is essential. During the COVID-19 pandemic, many academic and commercial entities have been using smartphone apps and online websites to collect data by encouraging patients to submit their symptoms and basic demographic data. These apps are collectively known as Symptom Tracking apps. The OASIS project collects data from third-party app providers to help the NHS respond to the COVID-19 pandemic. By pooling the data from these resources, valuable clinical data can be efficiently collected and analyzed.
Acknowledgments
The authors would like to express their gratitude to EditSprings (https://www.editsprings.com/) for the expert linguistic services provided.
Funding
This research was supported by the Chinese Cardiovascular Association-V.G. fund (2017-CCA-VG-042).
Compliance with ethical standards
Conflict of interest
None.
Footnotes
This article is part of the Topical Collection on Patient Facing Systems
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jing Nan, Ruofei Jia and Shuai Meng contributed equally to this work.
Contributor Information
Wei Chen, Email: 514705693@qq.com.
Hongyu Hu, Email: huhongyu968@hotmail.com.
References
- 1.Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, Brown TS, Der Nigoghossian C, Zidar DA, Haythe J, Brodie D, Beckman JA, Kirtane AJ, Stone GW, Krumholz HM, Parikh SA. Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the COVID-19 Pandemic. J Am Coll Cardiol. 2020;75(18):2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tan W, Parikh RV, Chester R, Harrell J, Franco V, Aksoy O, Dave R, Rafique A, Press M. Single Center Trends in Acute Coronary Syndrome Volume and Outcomes During the COVID-19 Pandemic. Cardiol Res. 2020;11(4):256–259. doi: 10.14740/cr1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DeFilippis EM, Reza N, Donald E, Givertz MM, Lindenfeld J, Jessup M. Considerations for Heart Failure Care During the COVID-19 Pandemic. JACC Heart Fail. 2020;8(8):681–691. doi: 10.1016/j.jchf.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mahmud E, Dauerman HL, Welt FGP, Messenger JC, Rao SV, Grines C, Mattu A, Kirtane AJ, Jauhar R, Meraj P, Rokos IC, Rumsfeld JS, Henry TD. Management of Acute Myocardial Infarction During the COVID-19 Pandemic: A Position Statement From the Society for Cardiovascular Angiography and Interventions (SCAI), the American College of Cardiology (ACC), and the American College of Emergency Physicians (ACEP) J Am Coll Cardiol. 2020;76(11):1375–1384. doi: 10.1016/j.jacc.2020.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trabattoni D, Montorsi P, Merlino L. Late STEMI and NSTEMI Patients' Emergency Calling in COVID-19 Outbreak. Can J Cardiol. 2020;36(7):1161.e7–1161.e8. doi: 10.1016/j.cjca.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elbadawi A, Elgendy IY, Mahmoud K, Barakat AF, Mentias A, Mohamed AH, Ogunbayo GO, Megaly M, Saad M, Omer MA, Paniagua D, Abbott JD, Jneid H. Temporal Trends and Outcomes of Mechanical Complications in Patients With Acute Myocardial Infarction. JACC Cardiovasc Interv. 2019;12(18):1825–1836. doi: 10.1016/j.jcin.2019.04.039. [DOI] [PubMed] [Google Scholar]
- 7.Alabas OA, Jernberg T, Pujades-Rodriguez M, Rutherford MJ, West RM, Hall M, Timmis A, Lindahl B, Fox KAA, Hemingway H, Gale CP. Statistics on mortality following acute myocardial infarction in 842 897 Europeans. Cardiovasc Res. 2020;116(1):149–157. doi: 10.1093/cvr/cvz197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Granger CB, Bates ER, Jollis JG, Antman EM, Nichol G, O'Connor RE, Gregory T, Roettig ML, Peng SA, Ellrodt G, Henry TD, French WJ, Jacobs AK. Improving Care of STEMI in the United States 2008 to 2012. J Am Heart Assoc. 2019;8(1):e008096. doi: 10.1161/JAHA.118.008096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimský P, ESC Scientific Document Group 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2018;39(2):119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 10.Endorsed by the Latin American Society of Interventional Cardiology; PCI WRITING COMMITTEE. Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Ting HH, STEMI WRITING COMMITTEE. O'Gara PT, Kushner FG, Ascheim DD, Brindis RG, Casey DE, Jr, Chung MK, de Lemos JA, Diercks DB, Fang JC, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Kristin Newby L, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Joseph Woo Y, Zhao DX, ACC/AHA TASK FORCE MEMBERS. Halperin JL, Levine GN, Anderson JL, Albert NM, Al-Khatib SM, Birtcher KK, Bozkurt B, Brindis RG, Cigarroa JE, Curtis LH, Fleisher LA, Gentile F, Gidding S, Hlatky MA, Ikonomidis J, Joglar J, Kovacs RJ, Magnus Ohman E, Pressler SJ, Sellke FW, Shen WK, Wijeysundera DN. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial Infarction: An update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention and the 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv. 2016;87(6):1001–19. doi: 10.1002/ccd.26325. [DOI] [PubMed] [Google Scholar]
- 11.Wong GC, Welsford M, Ainsworth C, Abuzeid W, Fordyce CB, Greene J, Huynh T, Lambert L, Le May M, Lutchmedial S, Mehta SR, Natarajan M, Norris CM, Overgaard CB, Perry Arnesen M, Quraishi A, Tanguay JF, Traboulsi M, van Diepen S, Welsh R, Wood DA, Cantor WJ, members of the Secondary Panel 2019 Canadian Cardiovascular Society/Canadian Association of Interventional Cardiology Guidelines on the Acute Management of ST-Elevation Myocardial Infarction: Focused Update on Regionalization and Reperfusion. Can J Cardiol. 2019;35(2):107–132. doi: 10.1016/j.cjca.2018.11.031. [DOI] [PubMed] [Google Scholar]
- 12.Foo CY, Bonsu KO, Nallamothu BK, Reid CM, Dhippayom T, Reidpath DD, Chaiyakunapruk N. Coronary intervention door-to-balloon time and outcomes in ST-elevation myocardial infarction: a meta-analysis. Heart. 2018;104(16):1362–1369. doi: 10.1136/heartjnl-2017-312517. [DOI] [PubMed] [Google Scholar]
- 13.Scholz KH, Maier SKG, Maier LS, Lengenfelder B, Jacobshagen C, Jung J, Fleischmann C, Werner GS, Olbrich HG, Ott R, Mudra H, Seidl K, Schulze PC, Weiss C, Haimerl J, Friede T, Meyer T. Impact of treatment delay on mortality in ST-segment elevation myocardial infarction (STEMI) patients presenting with and without haemodynamic instability: results from the German prospective, multicentre FITT-STEMI trial. Eur Heart J. 2018;39(13):1065–1074. doi: 10.1093/eurheartj/ehy004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zeng J, Huang J, Pan L. How to balance acute myocardial infarction and COVID-19: the protocols from Sichuan Provincial People's Hospital. Intensive Care Med. 2020;46(6):1111–1113. doi: 10.1007/s00134-020-05993-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mahajan V, Singh T, Azad C. Using Telemedicine During the COVID-19 Pandemic. Indian Pediatr. 2020;57(7):652–657. [PubMed] [Google Scholar]
- 16.Tanner R, MacDaragh Ryan P, Caplice NM. COVID-19-Where Have All the STEMIs Gone? Can J Cardiol. 2020;36(7):1161.e9–1161.e10. doi: 10.1016/j.cjca.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kapoor A, Yadav R. Will the hidden specter of acute coronary syndrome (ACS) and ST-segment elevation myocardial infarction (STEMI) emerge from the avalanche of COVID-19? Indian Heart J. 2020;72(3):192–193. doi: 10.1016/j.ihj.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zitelny E, Newman N, Zhao D. STEMI during the COVID-19 Pandemic - An Evaluation of Incidence. Cardiovasc Pathol. 2020;48:107232. doi: 10.1016/j.carpath.2020.107232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zaleski AL, Taylor BA, McKay RG, Thompson PD. Declines in Acute Cardiovascular Emergencies During the COVID-19 Pandemic. Am J Cardiol. 2020;129:124–125. doi: 10.1016/j.amjcard.2020.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.De Filippo O, D’Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, Secco GG, Campo G, Gallone G, Verardi R, Gaido L, Iannaccone M, Galvani M, Ugo F, Barbero U, Infantino V, Olivotti L, Mennuni M, Gili S, Infusino F, Vercellino M, Zucchetti O, Casella G, Giammaria M, Boccuzzi G, Tolomeo P, Doronzo B, Senatore G, Grosso Marra W, Rognoni A, Trabattoni D, Franchin L, Borin A, Bruno F, Galluzzo A, Gambino A, Nicolino A, Truffa Giachet A, Sardella G, Fedele F, Monticone S, Montefusco A, Omedè P, Pennone M, Patti G, Mancone M, De Ferrari GM. Reduced Rate of Hospital Admissions for ACS during Covid-19 Outbreak in Northern Italy. N Engl J Med. 2020;383(1):88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pessoa-Amorim G, Camm CF, Gajendragadkar P, De Maria GL, Arsac C, Laroche C, Zamorano JL, Weidinger F, Achenbach S, Maggioni AP, Gale CP, Poppas A, Casadei B. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: a survey by the European Society of Cardiology. Eur Heart J Qual Care Clin Outcomes. 2020;6(3):210–216. doi: 10.1093/ehjqcco/qcaa046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Masroor S. Collateral damage of COVID-19 pandemic: Delayed medical care. J Card Surg. 2020;35(6):1345–1347. doi: 10.1111/jocs.14638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahmed T, Lodhi SH, Kapadia S, Shah GV. Community and healthcare system-related factors feeding the phenomenon of evading medical attention for time-dependent emergencies during COVID-19 crisis. BMJ Case Rep. 2020;13(8):e237817. doi: 10.1136/bcr-2020-237817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rangé G, Hakim R, Motreff P. Where have the ST-segment elevation myocardial infarctions gone during COVID-19 lockdown? Eur Heart J Qual Care Clin Outcomes. 2020;6(3):223–224. doi: 10.1093/ehjqcco/qcaa034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mayol J, Artucio C, Batista I, Puentes A, Villegas J, Quizpe R, Rojas V, Mangione J, Belardi J. STEMI Working Group of Stent-Save a Life! LATAM and SOLACI (Latin American Society of Interventional Cardiology). An international survey in Latin America on the practice of interventional cardiology during the COVID-19 pandemic, with a particular focus on myocardial infarction. Neth Heart J. 2020;28(7-8):424–430. doi: 10.1007/s12471-020-01440-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, Dixon S, Rade JJ, Tannenbaum M, Chambers J, Huang PP, Henry TD. Reduction in ST-Segment Elevation Cardiac Catheterization Laboratory Activations in the United States During COVID-19 Pandemic. J Am Coll Cardiol. 2020;75(22):2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xiang D, Xiang X, Zhang W, Yi S, Zhang J, Gu X, Xu Y, Huang K, Su X, Yu B, Wang Y, Fang W, Huo Y, Ge J. Management and Outcomes of Patients With STEMI During the COVID-19 Pandemic in China. J Am Coll Cardiol. 2020;76(11):1318–1324. doi: 10.1016/j.jacc.2020.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Primessnig, U., Pieske, B.M., Sherif, M., Increased mortality and worse cardiac outcome of acute myocardial infarction during the early COVID-19 pandemic. ESC Heart Fail. 2020 Dec 6. 10.1002/ehf2.13075.Epubaheadofprint. [DOI] [PMC free article] [PubMed]
- 29.Abdelaziz HK, Abdelrahman A, Nabi A, Debski M, Mentias A, Choudhury T, Patel B, Saad M. Impact of COVID-19 pandemic on patients with ST-segment elevation myocardial infarction: Insights from a British cardiac center. Am Heart J. 2020;226:45–48. doi: 10.1016/j.ahj.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gramegna M, Baldetti L, Beneduce A, Pannone L, Falasconi G, Calvo F, Pazzanese V, Sacchi S, Pagnesi M, Moroni F, Ajello S, Melisurgo G, Agricola E, Camici PG, Scandroglio AM, Landoni G, Ciceri F, Zangrillo A, Cappelletti AM. ST-Segment-Elevation Myocardial Infarction During COVID-19 Pandemic: Insights From a Regional Public Service Healthcare Hub. Circ Cardiovasc Interv. 2020;13(8):e009413. doi: 10.1161/CIRCINTERVENTIONS.120.009413. [DOI] [PubMed] [Google Scholar]
- 31.Tam CF, Cheung KS, Lam S, Wong A, Yung A, Sze M, Lam YM, Chan C, Tsang TC, Tsui M, Tse HF, Siu CW. Impact of Coronavirus Disease 2019 (COVID-19) Outbreak on ST-Segment-Elevation Myocardial Infarction Care in Hong Kong. China. Circ Cardiovasc Qual Outcomes. 2020;13(4):e006631. doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nan J, Meng S, Hu H, Jia R, Chen W, Li Q, Zhang T, Song K, Wang Y, Jin Z. Comparison of Clinical Outcomes in Patients with ST Elevation Myocardial Infarction with Percutaneous Coronary Intervention and the Use of a Telemedicine App Before and After the COVID-19 Pandemic at a Center in Beijing, China, from August 2019 to March 2020. Med Sci Monit. 2020;26:e927061. doi: 10.12659/MSM.927061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moroni F, Gramegna M, Ajello S, Beneduce A, Baldetti L, Vilca LM, Cappelletti A, Scandroglio AM, Azzalini L. Collateral Damage: Medical Care Avoidance Behavior Among Patients With Myocardial Infarction During the COVID-19 Pandemic. JACC Case Rep. 2020;2(10):1620–1624. doi: 10.1016/j.jaccas.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Daniels MJ, Cohen MG, Bavry AA, Kumbhani DJ. Reperfusion of ST-Segment-Elevation Myocardial Infarction in the COVID-19 Era: Business as Usual? Circulation. 2020;141(24):1948–1950. doi: 10.1161/CIRCULATIONAHA.120.047122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang, L., Fan, Y., Lu, Z., Compromised STEMI reperfusion strategy in the era of COVID-19 pandemic: pros and cons. Eur Heart J. 2020 Sep 30:ehaa744. [DOI] [PMC free article] [PubMed]
- 36.Rajkumar RP. COVID-19 and mental health: A review of the existing literature. Asian J Psychiatr. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shi L, Lu ZA, Que JY, Huang XL, Liu L, Ran MS, Gong YM, Yuan K, Yan W, Sun YK, Shi J, Bao YP, Lu L. Prevalence of and Risk Factors Associated With Mental Health Symptoms Among the General Population in China During the Coronavirus Disease 2019 Pandemic. JAMA Netw Open. 2020;3(7):e2014053. doi: 10.1001/jamanetworkopen.2020.14053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pinkham AE, Ackerman RA, Depp CA, Harvey PD, Moore RC. A Longitudinal Investigation of the Effects of the COVID-19 Pandemic on the Mental Health of Individuals with Pre-existing Severe Mental Illnesses. Psychiatry Res. 2020;294:113493. doi: 10.1016/j.psychres.2020.113493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gorbunova EV, Sedykh DY, Maksimov SA. Psychological and social factors of adherence to treatment in patients with myocardial infarction. Ter Arkh. 2018;90(12):34–38. doi: 10.26442/00403660.2018.12.000006. [DOI] [PubMed] [Google Scholar]
- 40.Pino EC, Zuo Y, Borba CP, Henderson DC, Kalesan B. Clinical depression and anxiety among ST-elevation myocardial infarction hospitalizations: Results from Nationwide Inpatient Sample 2004-2013. Psychiatry Res. 2018;266:291–300. doi: 10.1016/j.psychres.2018.03.025. [DOI] [PubMed] [Google Scholar]
- 41.Sumner J. Cardiac rehabilitation guidelines informing Universal Health Coverage. Eur J Prev Cardiol. 2020;27(9):909–911. doi: 10.1177/2047487319890777. [DOI] [PubMed] [Google Scholar]
- 42.Thomas RJ, Brewer LC. Strengthening the Evidence for Cardiac Rehabilitation Benefits. JAMA Cardiol. 2019;4(12):1259–1260. doi: 10.1001/jamacardio.2019.4077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bellmann B, Lin T, Greissinger K, Rottner L, Rillig A, Zimmerling S. The Beneficial Effects of Cardiac Rehabilitation. Cardiol Ther. 2020;9(1):35–44. doi: 10.1007/s40119-020-00164-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brunetti ND, Dell'Anno A, Martone A, Natale E, Rizzon B, Di Cillo O, Russo A. Prehospital ECG transmission results in shorter door-to-wire time for STEMI patients in a remote mountainous region. Am J Emerg Med. 2020;38(2):252–257. doi: 10.1016/j.ajem.2019.04.046. [DOI] [PubMed] [Google Scholar]
- 45.Goebel M, Bledsoe J. Push Notifications Reduce Emergency Department Response Times to Prehospital ST-segment Elevation Myocardial Infarction. West J Emerg Med. 2019;20(2):212–218. doi: 10.5811/westjem.2018.12.40375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brunetti ND, De Gennaro L, Correale M, Santoro F, Caldarola P, Gaglione A, Di Biase M. Pre-hospital electrocardiogram triage with telemedicine near halves time to treatment in STEMI: A meta-analysis and meta-regression analysis of non-randomized studies. Int J Cardiol. 2017;232:5–11. doi: 10.1016/j.ijcard.2017.01.055. [DOI] [PubMed] [Google Scholar]
- 47.Baker J, Stanley A. Telemedicine Technology: a Review of Services, Equipment, and Other Aspects. Curr Allergy Asthma Rep. 2018;18(11):60. doi: 10.1007/s11882-018-0814-6. [DOI] [PubMed] [Google Scholar]
- 48.Weinstein RS, Krupinski EA, Doarn CR. Clinical Examination Component of Telemedicine, Telehealth, mHealth, and Connected Health Medical Practices. Med Clin North Am. 2018;102(3):533–544. doi: 10.1016/j.mcna.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 49.Sasangohar F, Davis E, Kash BA, Shah SR. Remote Patient Monitoring and Telemedicine in Neonatal and Pediatric Settings: Scoping Literature Review. J Med Internet Res. 2018;20(12):e295. doi: 10.2196/jmir.9403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ateriya N, Saraf A, Meshram VP, Setia P. Telemedicine and virtual consultation: The Indian perspective. Natl Med J India. 2018;31(4):215–218. doi: 10.4103/0970-258X.258220. [DOI] [PubMed] [Google Scholar]
- 51.Buvik A, Bugge E, Knutsen G, Småbrekke A, Wilsgaard T. Patient reported outcomes with remote orthopaedic consultations by telemedicine: A randomised controlled trial. J Telemed Telecare. 2019;25(8):451–459. doi: 10.1177/1357633X18783921. [DOI] [PubMed] [Google Scholar]
- 52.Brunetti ND, Scalvini S, Molinari G. Innovations in telemedicine for cardiovascular care. Expert Rev Cardiovasc Ther. 2016;14(3):267–80. doi: 10.1586/14779072.2016.1140572. [DOI] [PubMed] [Google Scholar]
- 53.Hamilton SJ, Mills B, Birch EM, Thompson SC. Smartphones in the secondary prevention of cardiovascular disease: a systematic review. BMC Cardiovasc Disord. 2018;18(1):25. doi: 10.1186/s12872-018-0764-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Andrès E, Zulfiqar AA, Talha S, Hajjam M, Hajjam J, Ervé S, El Hassani Hajjam A. Telemedicine in elderly patients with heart failure. Geriatr Psychol Neuropsychiatr Vieil. 2018;16(4):341–348. doi: 10.1684/pnv.2018.0758. [DOI] [PubMed] [Google Scholar]
- 55.Liu, H., Wang, W., Chen, H., Li, Z., Feng, S., Yuan, Y., Can WeChat group-based intervention reduce reperfusion time in patients with ST-segment myocardial infarction? A controlled before and after study. J Telemed Telecare. 2019 Jun 25:1357633X19856473. [DOI] [PubMed]
- 56.Hur S, Lee J, Kim T, Choi JS, Kang M, Chang DK, Cha WC. An Automated Fast Healthcare Interoperability Resources-Based 12-Lead Electrocardiogram Mobile Alert System for Suspected Acute Coronary Syndrome. Yonsei Med J. 2020;61(5):416–422. doi: 10.3349/ymj.2020.61.5.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ben-Assa E, Shacham Y, Golovner M, Malov N, Leshem-Rubinow E, Zatelman A, Oren Shamir A, Rogowski O, Roth A. Is telemedicine an answer to reducing 30-day readmission rates post-acute myocardial infarction? Telemed J E Health. 2014;20(9):816–21. doi: 10.1089/tmj.2013.0346. [DOI] [PubMed] [Google Scholar]
- 58.Omboni S, Caserini M, Coronetti C. Telemedicine and M-Health in Hypertension Management: Technologies, Applications and Clinical Evidence. High Blood Press Cardiovasc Prev. 2016;23(3):187–96. doi: 10.1007/s40292-016-0143-6. [DOI] [PubMed] [Google Scholar]
- 59.Omboni S, Panzeri E, Campolo L. E-Health in Hypertension Management: an Insight into the Current and Future Role of Blood Pressure Telemonitoring. Curr Hypertens Rep. 2020;22(6):42. doi: 10.1007/s11906-020-01056-y. [DOI] [PubMed] [Google Scholar]
- 60.Omboni S. Connected Health in Hypertension Management. Front Cardiovasc Med. 2019;6:76. doi: 10.3389/fcvm.2019.00076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Frias J, Virdi N, Raja P, Kim Y, Savage G, Osterberg L. Effectiveness of Digital Medicines to Improve Clinical Outcomes in Patients with Uncontrolled Hypertension and Type 2 Diabetes: Prospective, Open-Label, Cluster-Randomized Pilot Clinical Trial. J Med Internet Res. 2017;19(7):e246. doi: 10.2196/jmir.7833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.TMa Y, Cheng HY, Cheng L, Sit JWH. The effectiveness of electronic health interventions on blood pressure control, self-care behavioural outcomes and psychosocial well-being in patients with hypertension: A systematic review and meta-analysis. Int J Nurs Stud. 2019;92:27–46. doi: 10.1016/j.ijnurstu.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 63.Frederix I, Vanderlinden L, Verboven AS, Welten M, Wouters D, De Keulenaer G, Ector B, Elegeert I, Troisfontaines P, Weytjens C, Mullens W, Dendale P. Long-term impact of a six-month telemedical care programme on mortality, heart failure readmissions and healthcare costs in patients with chronic heart failure. J Telemed Telecare. 2019;25(5):286–293. doi: 10.1177/1357633X18774632. [DOI] [PubMed] [Google Scholar]
- 64.Koehler F, Koehler K, Deckwart O, Prescher S, Wegscheider K, Kirwan BA, Winkler S, Vettorazzi E, Bruch L, Oeff M, Zugck C, Doerr G, Naegele H, Störk S, Butter C, Sechtem U, Angermann C, Gola G, Prondzinsky R, Edelmann F, Spethmann S, Schellong SM, Schulze PC, Bauersachs J, Wellge B, Schoebel C, Tajsic M, Dreger H, Anker SD, Stangl K. Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet. 2018;392(10152):1047–1057. doi: 10.1016/S0140-6736(18)31880-4. [DOI] [PubMed] [Google Scholar]
- 65.Guo X, Gu X, Jiang J, Li H, Duan R, Zhang Y, Sun L, Bao Z, Shen J, Chen F. A Hospital-Community-Family-Based Telehealth Program for Patients With Chronic Heart Failure: Single-Arm. Prospective Feasibility Study. JMIR Mhealth Uhealth. 2019;7(12):e13229. doi: 10.2196/13229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Guo Y, Chen Y, Lane DA, Liu L, Wang Y, Lip GYH. Mobile Health Technology for Atrial Fibrillation Management Integrating Decision Support, Education, and Patient Involvement: mAF App Trial. Am J Med. 2017;130(12):1388–1396.e6. doi: 10.1016/j.amjmed.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 67.Turakhia MP, Desai M, Hedlin H, Rajmane A, Talati N, Ferris T, Desai S, Nag D, Patel M, Kowey P, Rumsfeld JS, Russo AM, Hills MT, Granger CB, Mahaffey KW, Perez MV. Rationale and design of a large-scale, app-based study to identify cardiac arrhythmias using a smartwatch: The Apple Heart Study. Am Heart J. 2019;207:66–75. doi: 10.1016/j.ahj.2018.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Majumder S, Mondal T, Deen MJ. Wearable Sensors for Remote Health Monitoring. Sensors (Basel). 2017;17(1):130. doi: 10.3390/s17010130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Loncar-Turukalo T, Zdravevski E, Machado da Silva J, Chouvarda I, Trajkovik V. Literature on Wearable Technology for Connected Health: Scoping Review of Research Trends, Advances, and Barriers. J Med Internet Res. 2019;21(9):e14017. doi: 10.2196/14017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mohsin AH, Zaidan AA, Zaidan BB, Albahri AS, Albahri OS, Alsalem MA, Mohammed KI. Real-Time Remote Health Monitoring Systems Using Body Sensor Information and Finger Vein Biometric Verification: A Multi-Layer Systematic Review. J Med Syst. 2018;42(12):238. doi: 10.1007/s10916-018-1104-5. [DOI] [PubMed] [Google Scholar]
- 71.Steinberg C, Philippon F, Sanchez M, Fortier-Poisson P, O'Hara G, Molin F, Sarrazin JF, Nault I, Blier L, Roy K, Plourde B, Champagne J. A Novel Wearable Device for Continuous Ambulatory ECG Recording: Proof of Concept and Assessment of Signal Quality. Biosensors (Basel). 2019;9(1):17. doi: 10.3390/bios9010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Stefano GB, Kream RM. The Micro-Hospital: 5G Telemedicine-Based Care. Med Sci Monit Basic Res. 2018;24:103–104. doi: 10.12659/MSMBR.911436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Schröder J, van Criekinge T, Embrechts E, Celis X, Van Schuppen J, Truijen S, Saeys W. Combining the benefits of tele-rehabilitation and virtual reality-based balance training: a systematic review on feasibility and effectiveness. Disabil Rehabil Assist Technol. 2019;14(1):2–11. doi: 10.1080/17483107.2018.1503738. [DOI] [PubMed] [Google Scholar]