Study participants and definitions
This study was a single-center, retrospective observational study of 123 critically ill patients with COVID-19 in Wuhan Huo Shen-shan Hospital, China. The patients analyzed in this report were admitted to the ICU between February 9th and April 6th, 2020, and were either discharged or died during their ICU hospitalization. Clinical data were collected by experienced physicians during the ICU admission and hospitalization. The study design and procedures were approved by the ethics committees of Wuhan Huo Shen-shan Hospital (HSSLL030) and Jiangnan University (JNU20200927RB02).
The onset of symptoms was defined as the time when COVID-19-associated symptoms were initially noted. The criteria of successful treatment prior to discharge were resolved clinical symptoms and inflammation and at least two consecutive negative results (24-h interval) on laboratory tests for COVID-19 infection. The endpoint in the ICU was specified as the point at which patients died or were cured from COVID-19 infection and transferred. The hypertension grades were defined according to the Chinese guidelines for the management of hypertension as follows: Stage 1 hypertension [S1 HT], systolic blood pressure [SBP] between 140 and 159 mmHg, and/or diastolic blood pressure [DBP] between 90 and 99 mmHg; Stage 2 hypertension [S2 HT], SBP 160–179 mmHg, and/or DBP 100–109 mmHg; and Stage 3 hypertension [S3 HT], SBP ≥ 180 mmHg, and/or DBP ≥ 110 mmHg) [1]. BP values were based on previous medical records or measured during the ICU admission without antihypertensive medications.
Case-series report
Among 123 patients admitted to the ICU, 29 were prediagnosed with S1 HT, 24 with S2 HT, and 22 with S3 HT. Forty-eight patients did not have hypertension. Only eight hypertensive patients were medicated with RAAS inhibitors. The mortality among the S3 HT patients (14/22, 63.6%) was the highest, while 44.9% (22/48) of patients without HT, 44.8% (13/28) of patients with S1 HT, and 33.3% (8/24) of those with S2 HT died during ICU hospitalization. Compared with normotensive patients, those prediagnosed with S3 HT had significantly higher rates of diabetes and coronary heart disease but not cerebrovascular disease, chronic kidney disease, or COPD. All hypertensive patients had longer durations in the ICU compared with normotensive patients, particularly the S3 HT group, which had a significantly extended duration vs. those without HT (mean, 36.8 [range, 12–55] days vs. 28.5 [range, 9–55] days; P < 0.05). Kaplan–Meier survival curves were plotted from the time of symptom onset to the endpoint (Fig. 1). There were significant differences in the time from symptom onset to the endpoint between the S3 HT patients and those without HT but not in the other groups. According to multivariate Cox regression analysis, patients with S3 HT presented a significantly higher risk of death from symptom onset than those without S3 HT (hazard ratio, 1.26 [95% CI, 1.02–1.56]) after adjusting for age, sex, comorbidities, and complications (Table 1).
Fig. 1.
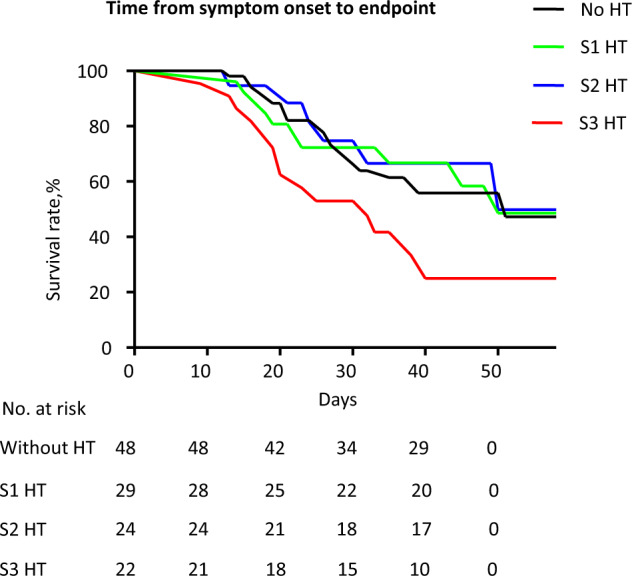
Kaplan–Meier survival curves for mortality during the time from symptom onset to either death or discharge from the ICU. Patients were divided into four groups (No HT, S1 HT, S2 HT, S3 HT) according to their blood pressure levels
Table 1.
Multivariate Cox regression analysis of the risk factors for mortality among critically ill patients
| From symptom onset to endpoint | ||
|---|---|---|
| Factor | Hazard ratio (95% Cl) | P value |
| Age | 0.99 (0.97–1.03) | 0.99 |
| Gender | 1.36 (0.73–2.54) | 0.32 |
| Stage 3 hypertension | 1.26 (1.02–1.56) | 0.02 |
| Diabetes | 1.02 (0.56–1.89) | 0.93 |
| Coronary heart disease | 1.91 (0.97–3.78) | 0.06 |
| COPD | 1.82 (0.61–5.46) | 0.28 |
| ARDS | 1.55 (0.89–2.73) | 0.12 |
| Cardiac injury | 1.37 (0.73–2.56) | 0.31 |
From the laboratory findings (Table 2), S3 HT patients had significantly higher levels of inflammatory, cardiac and kidney biomarkers, including CRP, procalcitonin, myoglobin, high-sensitivity troponin I, creatine kinase, BNP, and creatinine, than patients without hypertension. Patients with S1 HT and S2 HT did not show any significant differences in these levels compared with normotensive patients, except that S2 HT cases had significantly higher levels of myoglobin and creatinine than normotensive cases. In terms of complications, more S3 HT patients had ARDS than S2 HT, S1 HT, and normotensive patients, although the differences were not statistically significant. Compared with normotensive patients, significantly more patients in the S2 HT and S3 HT groups had cardiac injury during hospitalization. In addition, kidney injury was more common among patients with S3 HT than among those without hypertension.
Table 2.
Vascular-system-related parameters among clinical data of critically ill patients with COVID-19a
| Without HT | S1 HT | S2 HT | S3 HT | |
|---|---|---|---|---|
| No. of patients (%) | 48 (39.0) | 29 (23.6) | 24 (20.0) | 22 (17.9) |
| RAAS inhibitors (%) | 0 | 2 (6.8) | 2 (8.3) | 4 (18.2) |
| Comorbidities, no. (%) | ||||
| Diabetes | 8 (16.3) | 6 (20.7) | 4 (16.7) | 11 (50.0)** |
| Coronary heart disease | 5 (10.2) | 7 (24.1) | 2 (8.3) | 7 (31.8)* |
| Cerebrovascular disease | 5 (10.2) | 5 (17.2) | 7 (29.2) | 5 (22.7) |
| Chronic kidney disease | 4 (8.2) | 5 (17.2) | 2 (8.3) | 5 (22.7) |
| COPD | 2 (4.1) | 3 (10.3) | 3 (12.5) | 2 (9.1) |
| Laboratory tests on admission, median (IQR) | ||||
| CRP, mg/L | 48.2 (11.1–105.4) | 27.2 (8.9–95.7) | 80.0 (8.7–128.3) | 92.8 (32.2–136.6)* |
| Procalcitonin, ng/mL | 0.21 (0.07–0.57) | 0.20 (0.08–0.30) | 0.27 (0.10–0.50) | 0.86 (0.12–2.60)* |
| Myoglobin, ng/mL | 29.7 (7.1–126.5) | 32.7 (20.3–381.0) | 113.9 (8.2–485.3)* | 103.2 (19.6–406.6)* |
| High-sensitivity troponin I, ng/mL | 0.02 (0.01–0.07) | 0.01 (0.02–0.20) | 0.01 (0.01–0.20) | 0.04 (0.03–0.89)* |
| Creatine kinase, IU/L | 52.7 (31.9–108.3) | 33.2 (20.7–75.0) | 48.3 (37.4–111.4) | 95.2 (33.6–713.5)* |
| BNP, pg/mL | 104.3 (46.5–186.6) | 395.0 (47.0–524.7) | 46.6 (0.01–60.0) | 285.6 (53.9–1401.0)* |
| Creatinine, μmol/L | 58.6 (48.8–76.0) | 68.7 (43.7–90.0)* | 73.1 (62.5–146.0)* | 104.0 (56.8–185.0)* |
| Complications [No. of patients (%)] | ||||
| ARDS | 20 (41.7) | 14 (48.3) | 14 (58.3) | 15 (68.2) |
| Cardiac injury | 13 (27.1) | 13 (44.8) | 15 (62.5)* | 20 (90.9)** |
| Kidney injury | 8 (16.7) | 7 (24.1) | 4 (16.7) | 9 (40.9)* |
| Died | 22 (44.9) | 13 (44.8) | 8 (33.3) | 14 (63.6) |
COPD chronic obstructive pulmonary disease, CRP C-reactive protein, BNP type B natriuretic peptide, ARDS acute respiratory distress syndrome
aCategorical variables are presented as numbers and percentages. Continuous variables are shown as the median and interquartile range (IQR). Proportions for categorical variables were compared using the χ2 test. Fisher’s exact test was used if the sample size was small. Continuous variables were compared using independent group t-tests when the data were normally distributed, otherwise the Mann–Whitney test was used. *P < 0.05; **P < 0.001 vs. group without HT
Discussion
This single-center, retrospective, and objective report provides comprehensive information on the association between S3 HT and mortality among critically ill patients during ICU hospitalization. Hypertension has been widely documented as a risk factor associated with the severity of COVID-19 and was suggested to be associated with high mortality in the ICU in some reports [2, 3]. Consistent with these reports, we found a high fatality rate in hypertensive patients during ICU hospitalization in Wuhan Huo Shen-shan Hospital, particularly in the S3 HT group; 14 of 22 (63.6%) patients ultimately died of COVID-19. Among patients with S3 HT, four were medicated with RAAS inhibitors as antihypertensive treatment, while the rest were treated with calcium-channel blockers, beta-blockers, or thiazide diuretics. Two of four S3 HT patients taking RAAS inhibitors died. Despite the limited number of subjects, this is consistent with other reports that the use of RAAS inhibitors is not associated with the risk of severe COVID-19 and in-hospital deaths [4, 5].
We found that compared to patients without hypertension, those who had a history of S3 HT were more likely to develop cardiac injury during ICU hospitalization and had significantly increased levels of cardiac biomarkers at ICU admission (myoglobin, high-sensitivity troponin I, creatine kinase, and BNP). Cardiac injury has been extensively reported as an important risk factor associated with the severity and mortality of COVID-19 [6–8]. Given the close relationship between hypertension and cardiac injury [9, 10], it is reasonable to hypothesize that higher blood pressure causing more frequent cardiac injury eventually leads to increased mortality among critically ill patients in the ICU. Compared with normotensive patients, markedly more patients with S3 HT also had more kidney injuries in the ICU, accompanied by significantly increased levels of creatinine on ICU admission. This implies that the higher fatality rate in critically ill patients with S3 HT may result from the increased likelihood of developing kidney dysfunction. In addition, it should be noted that critically ill patients with S3 HT were more likely to have more severe prognoses, even after multiple organ dysfunction occurred. Consequently, they may face a higher risk of death. Overall, it would be helpful to give special care to patients with S3 HT in the ICU. More prioritized and aggressive treatment strategies, together with appropriate prevention of organ damage, should be applied to these patients. Monitoring associated biomarkers or parameters at the early stage in the ICU would be helpful to reduce mortality.
Acknowledgements
The authors would like to thank Prof Iain C Bruce for the critical reading of this manuscript.
Funding
This work is funded by Wuxi Municipal Health Commission, CN (M202044) and Shanghai Municipal Health Commission, CN (201740171).
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Li Geng, Chao He
Contributor Information
Wenfang Li, Email: chzhedlwf@163.com.
Lei Feng, Email: feng2008lei@163.com.
References
- 1.Liu LS, Writing Group of Chinese Guidelines for the Management of Hypertension [2010 Chinese guidelines for the management of hypertension] Zhonghua Xin Xue Guan Bing Za Zhi. 2011;39:579–615. [PubMed] [Google Scholar]
- 2.Wang Y, Lu X, Li Y, Chen H, Chen T, Su N, et al. Clinical Course and Outcomes of 344 Intensive Care Patients with COVID-19. Am J Respir Crit Care Med. 2020;201:1430–4. doi: 10.1164/rccm.202003-0736LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574–81. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jarcho JA, Ingelfinger JR, Hamel MB, D’Agostino RB, Sr., Harrington DP. Inhibitors of the renin-angiotensin-aldosterone system and Covid-19. N Engl J Med. 2020;382:2462–4. doi: 10.1056/NEJMe2012924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reynolds HR, Adhikari S, Pulgarin C, Troxel AB, Iturrate E, Johnson SB, et al. Renin-angiotensin-aldosterone system inhibitors and risk of Covid-19. N Engl J Med. 2020;382:2441–8. doi: 10.1056/NEJMoa2008975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bonow RO, Fonarow GC, O’Gara PT, Yancy CW. Association of Coronavirus Disease 2019 (COVID-19) With Myocardial Injury and Mortality. JAMA Cardiol. 2020;5:751–3. doi: 10.1001/jamacardio.2020.1105. [DOI] [PubMed] [Google Scholar]
- 7.Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, et al. Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5:802–10. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, et al. Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19) JAMA Cardiol. 2020;5:811–8. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kemp CD, Conte JV. The pathophysiology of heart failure. Cardiovasc Pathol. 2012;21:365–71. doi: 10.1016/j.carpath.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 10.Mozaffari MS, Schaffer SW. Effect of hypertension and hypertension-glucose intolerance on myocardial ischemic injury. Hypertension. 2003;42:1042–9. doi: 10.1161/01.HYP.0000095614.91961.40. [DOI] [PubMed] [Google Scholar]


