Abstract
Observational studies suggest that a heart failure (HF) diagnosis carries a poor prognosis in subjects with severe SARS-CoV2 (COVID-19) infection, but it is unknown whether this association reflects direct myocardial damage due to COVID-19 or the consequence of preexisting cardiac defects and related cardiovascular disease (CVD) risk burden. Although the close relation between CVD and COVID-19 outcomes is well established, contrasting data exists about the occurrence of HF complications during COVID-19 infection. Therefore, a specific algorithm focused on diagnostic differentiation in acute patients distinguishing between acute HF and acute respiratory distress syndrome related to COVID-19 is needed. Further, several concerns exist for the management of patients with an uncertain diagnosis and acute dyspnea, the exact relationship existing between COVID-19 and HF. Therefore, the treatment for subjects with both COVID-19 and HF and which criteria may be defined for domiciliary or hospital management, remain poorly defined. Herein, we describe practices to be adopted in order to address these concerns and avoid further virus spread among patients, l and their familiars involved in such patients’ care.
Keywords: SARS-CoV-2, COVID-19, Acute heart failure, Hospitalization management
Introduction
The coronavirus disease 2019 (COVID-19) pandemic originated in Whuan, China, and is associated with severe acute respiratory syndrome (SARS), resulting in significant mortality risk, despite ventilation support therapy [1]. Many patients admitted to the intensive care unit (ICU) for primitive respiratory deterioration have underlying cardiovascular disease (CVD). Common factors associated with mortality are hypertension, obesity, history of coronary disease, heart failure (HF), atherosclerosis, diabetes, and related metabolic disturbances [2, 3]. Although the close relation between CVD and COVID-19 outcomes is described and well established, no extensive data exists about HF complications occurring during COVID-19 infection. The question regarding whether COVID-19 infection leads to hemodynamic HF deterioration or if chronic HF (CHF) is itself a predisposing factor for ARDS occurrence, remains unexplored [4, 5]. Interestingly, during the period of high COVID-19-related admissions, a reduction in CVD hospitalizations has been noted; this could contribute to an increased rate of cardiovascular death outside of the hospital setting [6, 7]. These topics merit further discussion in order to determine the best management for patients and to safeguard healthcare personnel involved in such patients’ care.
Diagnostic tests and screening in patients with acute dyspnea
COVID-19 infection manifestation ranges from modest flu to SARS, which can result in mortality increase [5, 8]. The wide clinical symptoms and the lack of effective management lead to a heterogeneous approach based on personal experience rather than large solid registries or data from clinical trials [4, 9]. A majority of acutely ill patients are not diagnosed from community testing, but rather from in-hospital testing after presentation. Because acute HF (AHF) syndromes are characterized by sudden symptom onset, increasing dyspnea, and orthopnea requiring prompt hospitalization, as well as acute respiratory failure due to COVID-19 infection, there is an impelling need to distinguish the two syndromes by an accurate diagnostic protocol. In both cardiac and respiratory complications (AHF and ARDS, respectively), dyspnea represents the most common symptom [10, 11]. Therefore, a customized diagnostic route could be useful in order to reduce contact between AHF and ARDS patients and to avoid in-hospital infection spread. We suggest that the following diagnostic screenings may be appropriately considered during COVID-19 era for patients presenting with the aforementioned symptoms and history: respiratory rate, natriuretic peptides, lymphocyte count, C-reactive protein, D-dimer, fibrinogen, electrocardiogram, and chest X-ray. Analysis of the arterial blood gas could be performed as an additional test to identify the culprit behind the patient’s destabilization [12]. Additionally, lung ultrasound could be used as an alternative method to discern a pulmonary lesion associated with interstitial pneumonia or increased comet related to water content [13]. Using these principles, we present an algorithm which assigns the culprit of destabilization as either AHF or COVID-19 with high, uncertain, or low probability. For instance, in the setting of elevated natriuretic peptide levels associated with significant chest X-ray, electrocardiographic alterations, congestion signs, history of previous HF episodes, normal hemocrome and leucocyte formula, D-dimer and fibrinogen levels into the normal range, there is an high probability for AHF diagnosis. Whereas, in the case of increased C-reactive protein associated with lymphocytopenia, increased respiratory rate, elevated D-dimer and fibrinogen, and significant hypoxemia, the diagnosis of respiratory failure related to COVID-19 is high. Conversely, when natriuretic peptide levels (NP) are low, chest X-ray is negative, and congestion is present, the probability of HF is low. Similarly, in the case of coagulative test alterations, normal arterial blood gas, and lack of lymphopenia, even in the presence of increased C-reactive protein associated with radiographic signal suggestive of pneumonia, the probability of COVID-19 lung involvement is low [14]. In order to differentiate the two diseases, the blood gas analysis became mandatory: hypoxemia and hypocapnia associated with low oxygen saturation below 90% respiratory acidosis are specific signs of respiratory distress or related thromboembolic complication; conversely, hypoxemia without CO2 alteration and relative acidosis or respiratory alkalosis are more typical for hemodynamic derangement [15]. We did not include troponin among laboratory variables because it could be altered in the settings of myocardial cell loss due to increased parietal stress and in reduced oxygen delivery secondary to altered pulmonary gas exchange. Notably, this biomarker is not specific for diagnostic differentiation, although it has demonstrated a remarkable prognostic significance [16, 17].
Among these two pictures, there are several gray situations in which some clinical variables are suggestive for HF, while others are for COVID-19 infection. In those cases, further investigation with more advanced diagnostic tools is required as a second step in the algorithm. Echocardiography may be performed when AHF is more likely, and CT scan may be needed in cases suggestive of interstitial pneumonia and related ARDS [18]. Both diagnostic examinations should be executed in safe conditions with the previous and succeeding rooms disinfected, and mono use material for sound and scan protection [19]. We report below a detailed framework of potential possibilities occurring in clinical practice. In all the other cases, both diagnosis of AHF and COVID-19-related ARDS may be excluded and physicians could shift toward other potential diseases responsible for incremental dyspnea.
Table 1 summarizes the accounted parameters and the related specific variables included in this flowchart.
Table 1.
Clinical, laboratory and diagnostic tests useful for initial screening and diagnosis in patients presenting with dyspnoea
| High HF/low ARDS-COVID | Uncertain HF ARDS-COVID | Low HF/High ARDS-COVID |
|---|---|---|
|
• ↑ BNP/NTproBNP • Congestion signs • History of HF • ECG alterations • Positive chest X-ray • Low C-reactive protein • No hemocrome alteration • Normal D-dimer and fibrinogen |
LikelyAHF • Mild ↑BNP/proBNP • None or 1 congestion sign • Mild hypoxemia without hypocapnia • Chest X-ray doubtful • Positive chest B lines ultrasound Likely ARDS • ↑C-reactive protein • Mild ↑BNP/proBNP increase • Hypoxemia with mild hypocapnia • ↑D-dimer and fibrinogen increase • Limited chest |
• ↓ BNP/NTproBNP • Relevant hypoxemia • Tachipnea • Respiratory acidosis • ↑ C-reactive protein • ↑ Procalcitonin • Localized subpleural and scissural chest X-ray signs • Hemocrome alteration with lymphocitopenia • No history of HF • ↑ D-dimer and fibrinogen |
Care management and ward distribution according to clinical presentation
Beyond the initial screening and diagnostic course, many concerns remain unclarified regarding the location and distribution for patients with both AHF and COVID-19 infection, with diagnosis unknown at admission. First, it is imperative to distinguish separate routes for AHF patients with confirmed/suspected COVID-19 and those negative for COVID-19. In the case of a positive test result or those exhibiting symptoms and awaiting a test result, patients should be hospitalized in a well-defined and isolated “red zone” area located in the emergency department: in this site, all patients presenting with dyspnea can be screened by the application of the abovementioned diagnostic algorithm. All the diagnostic tests might be performed in safe condition with face mask worn by patients and health staff (nurses, technicians and doctors). Additional protection of hospital personnel may provide showerproof, single-use coat, gloves, facial protection and FFP3 mask [20]. AHF diagnosis should be performed according to guideline-directed criteria, including traditional blood sample and natriuretic peptide measurement, electrocardiogram and chest X-ray [21]. Lung ultrasound provides additive accuracy in diagnostic differentiation and interstitial pneumonia identification [22]. The second step may require chest CT scan execution in case of high probability for interstitial pneumonia and related ARDS. Conversely, echocardiographic examination could be performed in patients with high HF probability [23].
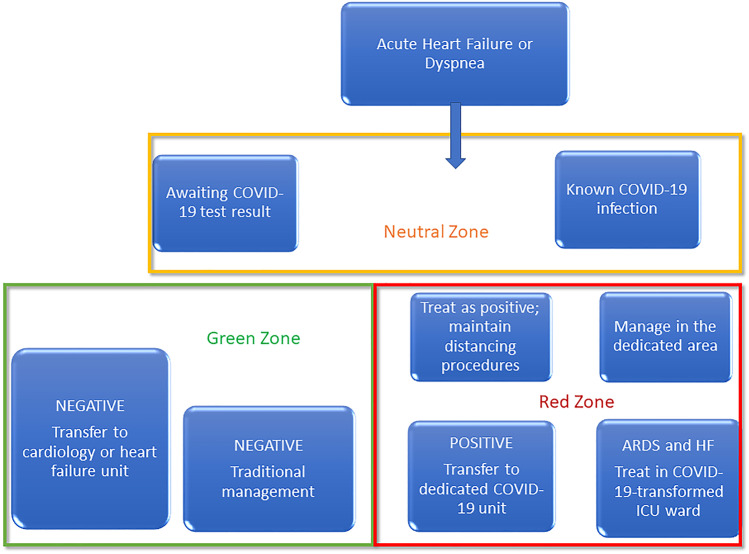
In AHF COVID-19-positive patients, echocardiography should be performed only in the case of new-onset AHF or unexplored reasons of hemodynamic destabilization such as suspected pericardial tamponade, suspected acute pulmonary embolism, suspected acute coronary syndrome (ACS) and suspected acute valvular heart diseases [24]. In case of contemporary occurrence of infection and AHF, treatment should be customized according to prevalent respiratory or cardiogenic disorder. Because of some interaction between antiarrythmic, anti-inflammatory and antiviral drugs, a consensus treatment decided by cardiologist advisor, infectiologist and pulmonologist may be encouraged. Therefore, because many patients are treated with corticosteroids, which universally influence idro saline and glycemic status, daily diuresis, electrolyte imbalance and metabolic profile may be monitored. Both ARDS and hemodynamic complications should be managed in the “red zone” reassessed as ICU wars. In case of pulmonary embolism or diffuse intravascular coagulopathy suspicion by laboratory measurements (i.e. D dimer and fibrinogen increase associated with persistent hypocapnia and hypoxigenation), an echocardiographic examination to ascertain right ventricle (RV morphology and noninvasive pulmonary pressure estimation) [25]. In case of AHF patients with uncertain COVID-19 diagnosis, it became priority to avoid eventual diffusion among patients and healthcare workers. In all these case, it could be worth to identify a “neutral zone” within the emergency department in which patients can wait for laboratory swab or blood culture response avoiding contagious risk. In this “gray zone,” patients should maintain a minimum distance of 2 m and dedicated medical staff should wear showerproof single-use coat, gloves, facial protection, and FFP3 mask [26]. A dedicated cardiologist consultant should support ED clinicians for AHF management during this period following similar procedures and modalities of COVID-dedicated staff. In case of positive coronavirus nasopharyngeal swab, AHF patients should be addressed in “red zone,” whereas in case of negative nasopharyngeal swab test, AHF patients could be transferred to the cardiology ward (“green zone”) and managed using traditional modalities. In the “green zone,” cardiologists and other healthcare workers should keep surgical masks and gloves. All patients may wear surgical masks during hospitalization period. The isolation and disinfection must involve not only healthcare staff but also the environments in which patients remain during transitional period independently from virus test response. Accordingly, ultrasound and radiographic devices must be cleaned with alcoholic solution before and after every examination. All parts nearest to the patient (bed employed for examination, probe, and radiographic scan) must be covered by a plastic mono use protection [19, 27, 28] (Fig. 1).
Fig. 1.
Diagnostic course and in hospital permanence for patients admitted with acute dyspnea. Patients awaiting serological or swab test might stay in neutral uncontaminated ward, after virus test they can accede in the appropriate area for a customized management
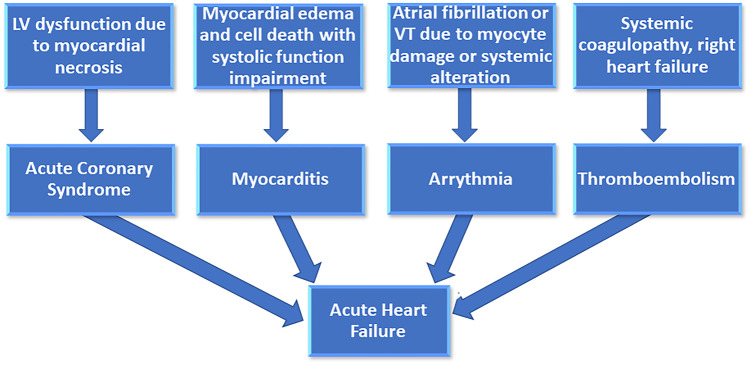
During early hospitalization, the role of cardiac biomarkers (D-dimer, troponin, and NP) and all the other are key features for both cardiovascular complication recognition and diagnostic differentiation [14, 29]. Therefore, specific laboratory biomarkers should be systematically measured in all patients to recognize treatment efficacy, clinical trend, and cardiovascular and respiratory complications related to COVID-19. Several studies have been reported about potential virus-related complications although a more detailed prevalence is relatively unknown: acute pulmonary embolism, myocarditis, ACS and arrhythmic events, acute kidney injury, sudden cardiac function deterioration, and intravascular disseminated coagulopathy are widely described, but it remains unclear which patients are much more prone to develop current complication and the exact reason of their significant reduction over the last summer period [12, 30] More specifically, although recent magnetic resonance study demonstrated that 60% of COVID patients experienced some signs of cardiac involvement, it remains unknown if current findings lead to significant cardiac dysfunction and which is the primary pathophysiological driver of deterioration (systolic or diastolic dysfunction) potentially causes for HF occurrence during COVID-19 (Fig. 2).
Fig. 2.
Potential causes of cardiac complications induced by infection. Different clinical manifestations are related to the main virus location and spread ( coronary district, myocites, venous system)
The broad clinical scenario and the lack of a standardized management, lead to an inhomogeneous approach mainly based on personal experience local hospital practice, rather than solid registries and protocols. Before, to address the relationship existing between COVID-19 and HF, it appears priority to recognize the specific diagnostic algorithm for each diseases and the related course that patients may follow during hospitalization. Of note, diagnostic management should be started in each patients presenting with acute dyspnea at ED, with individualized laboratory and imaging tests. Current approach may lead to a better diagnostic differentiation as well as improvement of in hospital avenues with virus spread avoidance.
Alternative management for chronic heart failure patients
Over the last several months, the COVID-19 pandemic has negatively modified patients’ attitudes toward receiving routine healthcare and it has modified medical staff conduct [31]. Many patients with CHF followed medical advice (and government indication, if relevant) and carefully isolated, avoiding crowded places and potential sites for virus infection and transmission. While doing so, many did not (or could not continue to) respect HF guidelines regarding diet and exercise: many patients increased their body weight and total body fat, while reducing their physical activity and aerobic capacity. Such situations increase CVD burden by reducing glycemic control and increasing cholesterol levels, insulin resistance, and blood pressure, with consequent metabolic risk elevation [32]. Such features contribute to HF exacerbation in those with known diagnosis or to HF onset in those with high CVD risk. Otherwise, fear of the virus contributed to delayed diagnosis and preventive/early treatment for congestion. The resultant extremely exacerbated AHF presentation could have caused the healthcare system (hospital ambulatory and peripheral) primarily engaged in virus struggle, to misdiagnose the disease, and those patients requiring hospitalization experienced hemodynamic and congestion deterioration [33, 34]. Current issues raise several concerns about the optimal strategy for patients with CHF and AHF. Indeed, no precise guidelines exist in terms of clinical and laboratory parameters to be evaluated during isolation, and criteria for hospital admission in case of new diagnosis or HF impairment. Although medical devices may be poorly distributed among peripheral environments, telemedicine software should be encouraged [35]. The daily measurement and central registration of some easily measurable variables such as body weight, heart rate, blood pressure, and oxygen saturation could identify the prodromal signs of HF and permit treatment initiation at home in hopes of avoiding hospitalization. Accordingly, asymptomatic patients with sudden increase of CVD risk with known cardiac defects might be closely monitored using telemedicine applications [36, 37]. Different concerns involve AHF patients: diagnostic screening is well established but has been shown to be poorly available with the higher levels of requirements of environmental sanitization and disinfection [38]. A few position papers proposed a multi-modality diagnostic approach with an easier and more rapid protocol compared with traditional examination; however, they do not explain which route or modality should be used to avoid potential virus transmission [4, 25, 39, 40]. In clinical practice, during the COVID-19 era, the possibility to execute a complete examination is often difficult as it requires a substantial amount of time and more personal involvement. Thus, every application should be customized in relation to clinical presentation, patient history, and biomarker profile. Similarly, to avoid virus spread and resource expenditure, each examination needs to be planned in order to achieve useful and additive information [41, 42]. In this setting, a primary role of cardiac biomarkers may be warranted, although no specific studies have been focused on the importance of laboratory examination for early diagnosis and related management. We recognize that the well-supported strategy of early home treatment of SARS-CoV2 infection at the earliest recognition of symptoms is likely to change the natural history of COVID-19 infection including its late cardiac manifestations. Future studies of early treatment with antivirals, immunomodulators, and antithrombotics with attention to short- and longer-term cardiovascular outcomes are warranted.
Conclusions
In light of the COVID-19 pandemic, some diagnostic procedures and in-hospital routes must be adopted in order to guarantee the best clinical management, and avoid infection diffusion following admission. Our protocol suggests to initially screen all patients with worsening dyspnea using a rapid diagnostic clinical and laboratory test, and then offers an additional diagnostic step to identify the most probable cause of admission. Other specific procedures, such as diffusion of telemedicine software, should be encouraged. The systematic application of simple rules will lead to time optimization and prioritize the safety of both patients and healthcare staff.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T (2020) Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 2.Liang WH, Guan WJ, Li CC, et al. Clinical characteristics and outcomes of hospitalised patients with COVID-19 treated in Hubei (epicentre) and outside Hubei (non-epicentre): a nationwide analysis of China. Eur Respir J. 2020;55(6):2000562. doi: 10.1183/13993003.00562-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu C, Chen X, Cai Y et al (2020) Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China [published online ahead of print. 2020 Mar 13]. JAMA Intern Med. 2020;e200994. 10.1001/jamainternmed.2020.0994 [DOI] [PMC free article] [PubMed]
- 4.Zhang Y, Coats AJ, Zheng Z, Adamo M, Ambrosio G, Anker SD, Butler J, Xu D, Mao J, Khan MS, Bai L, Mebazaa A, Ponikowski P, Tang Q, Ruschitzka F, Seferovic P, Tschöpe C, Zhang S, Gao C, Zhou S, Senni M, Zhang J, Metra M (2020) Management of heart failure patients with COVID-19. A Joint Position Paper of the Chinese Heart Failure Association & National Heart Failure Committee and the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 10.1002/ejhf.1915 [DOI] [PubMed]
- 5.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T (2020) Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 6.Andersson C, Gerds T, Fosbøl E, et al. Incidence of new-onset and worsening heart failure before and after the COVID-19 epidemic lockdown in Denmark: a nationwide cohort study. Circ Heart Fail. 2020;13(6):e007274. doi: 10.1161/CIRCHEARTFAILURE.120.007274. [DOI] [PubMed] [Google Scholar]
- 7.Frankfurter C, Buchan TA, Kobulnik J et al (2020) Reduced rate of hospital presentations for heart failure during the Covid-19 pandemic in Toronto, Canada [published online ahead of print, 2020 Jul 16]. Can J Cardiol. 2020;S0828–282X(20)30599–7. 10.1016/j.cjca.2020.07.006 [DOI] [PMC free article] [PubMed]
- 8.Fried JA, Ramasubbu K, Bhatt R, et al. The variety of cardiovascular presentations of COVID-19. Circulation. 2020;141(23):1930–1936. doi: 10.1161/CIRCULATIONAHA.120.047164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lal S, Hayward CS, De Pasquale C, et al. COVID-19 and acute heart failure: screening the critically ill - a position statement of the Cardiac Society of Australia and New Zealand (CSANZ) Heart Lung Circ. 2020;29(7):e94–e98. doi: 10.1016/j.hlc.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang K, Zhang J, Wu W, et al. A retrospective analysis of the epidemiology, clinical manifestations, and imaging characteristics of familial cluster-onset COVID-19. Ann Transl Med. 2020;8(12):747. doi: 10.21037/atm-20-3759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen Q, Xu L, Dai Y, et al. Cardiovascular manifestations in severe and critical patients with COVID-19. Clin Cardiol. 2020;43(7):796–802. doi: 10.1002/clc.23384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Assandri R, Buscarini E, Canetta C, Scartabellati A, Viganò G, Montanelli A (2020) Laboratory biomarkers predicting COVID-19 severity in the emergency room [published online ahead of print, 2020 May 21]. Arch Med Res. 2020;S0188–4409(20)30776–1. 10.1016/j.arcmed.2020.05.011 [DOI] [PMC free article] [PubMed]
- 13.Volpicelli G, Gargani L . Sonographic signs and patterns of COVID-19 pneumonia. Ultrasound J. 2020;12(1):22. doi: 10.1186/s13089-020-00171-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Inciardi RM, Adamo M, Lupi L, et al. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur Heart J. 2020;41(19):1821–1829. doi: 10.1093/eurheartj/ehaa388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park JJ, Choi DJ, Yoon CH, et al. The prognostic value of arterial blood gas analysis in high-risk acute heart failure patients: an analysis of the Korean Heart Failure (KorHF) registry. Eur J Heart Fail. 2015;17(6):601–611. doi: 10.1002/ejhf.276. [DOI] [PubMed] [Google Scholar]
- 16.Ni W, Yang X, Liu J, et al. Acute myocardial injury at hospital admission is associated with all-cause mortality in COVID-19. J Am Coll Cardiol. 2020;76(1):124–125. doi: 10.1016/j.jacc.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shi S, Qin M, Cai Y, et al. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur Heart J. 2020;41(22):2070–2079. doi: 10.1093/eurheartj/ehaa408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rudski L, Januzzi JL, Rigolin VH et al (2020) Multimodality Imaging in Evaluation of Cardiovascular complications in Patients with COVID-19 [published online ahead of print, 2020 Jul 20]. J Am Coll Cardiol. 2020;S0735–1097(20)36039–3. 10.1016/j.jacc.2020.06.080 [DOI] [PMC free article] [PubMed]
- 19.DeFilippis EM, Reza N, Donald E, Givertz MM, Lindenfeld J, Jessup M (2020) Considerations for heart failure care during the COVID-19 pandemic [published online ahead of print, 2020 Jun 3]. JACC Heart Fail. 2020;S2213–1779(20)30273–0. 10.1016/j.jchf.2020.05.006 [DOI] [PMC free article] [PubMed]
- 20.Ong SWX, Tan YK, Chia PY, Lee TH, Ng OT, Wong MSY (2020) Surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020 Mar 4 10.1001/jama.2020.3227. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 21.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis T, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, ESC Scientific Document Group (2016) ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37:2129–2200. 10.1093/eurheartj/ehw128(Epub 2016 May 20)
- 22.Dargent A, Chatelain E, Kreitmann L et al (2020) Lung ultrasound score to monitor COVID-19 pneumonia progression in patients with ARDS. PLoS One. 2020;15(7):e0236312. Published 2020 Jul 21. 10.1371/journal.pone.0236312 [DOI] [PMC free article] [PubMed]
- 23.Larici AR, Cicchetti G, Marano R et al (2020) Multimodality imaging of COVID-19 pneumonia: from diagnosis to follow-up. A comprehensive review [published online ahead of print, 2020 Aug 17]. Eur J Radiol. 131:109217. 10.1016/j.ejrad.2020.109217 [DOI] [PMC free article] [PubMed]
- 24.Drake DH, De Bonis M, Covella M, et al. Echocardiography in pandemic: front-line perspective, expanding role of ultrasound, and ethics of resource allocation. J Am Soc Echocardiogr. 2020;33(6):683–689. doi: 10.1016/j.echo.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Skulstad H, Cosyns B, Popescu BA, et al. COVID-19 pandemic and cardiac imaging: EACVI recommendations on precautions, indications, prioritization, and protection for patients and healthcare personnel. Eur Heart J Cardiovasc Imaging. 2020;21(6):592–598. doi: 10.1093/ehjci/jeaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ruocco G, Feola M, Palazzuoli A (2020) In hospital routes in acute heart failure admission during COVID 19 Frontiers Cardiov Medicine [DOI] [PMC free article] [PubMed]
- 27.Bromage DI, Cannatà A, Rind IA, et al. The impact of COVID-19 on heart failure hospitalization and management: report from a Heart Failure Unit in London during the peak of the pandemic. Eur J Heart Fail. 2020;22(6):978–984. doi: 10.1002/ejhf.1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anker SD, Butler J, Khan MS, et al. Conducting clinical trials in heart failure during (and after) the COVID-19 pandemic: an Expert Consensus Position Paper from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC) Eur Heart J. 2020;41(22):2109–2117. doi: 10.1093/eurheartj/ehaa461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lombardi CM, Carubelli V, Iorio A et al (2020) Association of troponin levels with mortality in italian patients hospitalized with coronavirus disease 2019: results of a multicenter study [published online ahead of print, 2020 Aug 26]. JAMA Cardiol. 10.1001/jamacardio.2020.3538 [DOI] [PMC free article] [PubMed]
- 30.Lala A, Johnson KW, Januzzi JL, et al. Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. J Am Coll Cardiol. 2020;76(5):533–546. doi: 10.1016/j.jacc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baldi E, Sechi GM, Mare C et al (2020) COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests [published online ahead of print, 2020 Jun 20]. Eur Heart J. 2020;ehaa508. 10.1093/eurheartj/ehaa508 [DOI] [PMC free article] [PubMed]
- 32.Samsky MD, DeVore AD, McIlvennan CK et al (2020) Heart failure clinical trial operations during the COVID-19 pandemic: results from a multicenter survey [published online ahead of print, 2020 Jul 23]. Circ Heart Fail. 10.1161/CIRCHEARTFAILURE.120.007456 [DOI] [PMC free article] [PubMed]
- 33.Cannata A, Bromage DI, Rind IA et al (2020) Temporal trends in decompensated heart failure and outcomes during COVID-19: a multisite report from heart failure referral centres in London [published online ahead of print, 2020 Aug 18]. Eur J Heart Fail. 10.1002/ejhf.1986. [DOI] [PMC free article] [PubMed]
- 34.Rey JR, Caro-Codón J, Rosillo SO et al (2020) Heart failure in Covid-19 patients: prevalence, incidence and prognostic implications [published online ahead of print, 2020 Aug 24]. Eur J Heart Fail. 10.1002/ejhf.1990. [DOI] [PMC free article] [PubMed]
- 35.Agostoni P, Mapelli M, Conte E, et al. Cardiac patient care during a pandemic: how to reorganise a heart failure unit at the time of COVID-19. Eur J Prev Cardiol. 2020;27(11):1127–1132. doi: 10.1177/2047487320925632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Meschi T, Rossi S, Volpi A, Ferrari C, Sverzellati N, Brianti E, Fabi M, Nouvenne A, Ticinesi A. Reorganization of a large academic hospital to face COVID-19 outbreak: the model of Parma, Emilia-Romagna Region, Italy. Eur J Clin Invest. 2020;50(6):e13250. doi: 10.1111/eci.13250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McCullough PA, Kelly RJ, Ruocco G et al (2020) Pathophysiological basis and rationale for early outpatient treatment of SARS-CoV-2 (COVID-19) infection [published online ahead of print, 2020 Aug 6]. Am J Med. 2020;S0002–9343(20)30673–2. 10.1016/j.amjmed.2020.07.003 [DOI] [PMC free article] [PubMed]
- 38.Cleland JGF, Clark RA, Pellicori P, Inglis SC, et al. Caring for people with heart failure and many other medical problems through and beyond the COVID-19 pandemic: the advantages of universal access to home telemonitoring. Eur J Heart Fail. 2020;22(6):995–998. doi: 10.1002/ejhf.1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ng ACT, Delgado V, Bax JJ (2020) An international, multicentre survey of echocardiographic abnormalities in COVID-19 patients [published online ahead of print, 2020 Jul 30]. Eur Heart J Cardiovasc Imaging. 2020;jeaa218. 10.1093/ehjci/jeaa218 [DOI] [PMC free article] [PubMed]
- 40.Ruocco G, McCullough PA, Tecson KM, Mancone M, De Ferrari GM, D'Ascenzo F, De Rosa FG, Paggi A, Forleo G, Secco GG, Pistis G, Monticone S, Vicenzi M, Rota I, Blasi F, Pugliese F, Fedele F, Palazzuoli A (2020) Mortality risk assessment using CHA(2)DS(2)-VASc scores in patients hospitalized with coronavirus disease 2019 infection. Am J Cardiol. 2020 Dec 15;137:111–117. 10.1016/j.amjcard.2020.09.029 Epub 2020 Sep 28. PMID: 32991860; PMCID: PMC7521434. [DOI] [PMC free article] [PubMed]
- 41.Salzano A, D'Assante R, Stagnaro FM, et al. Heart failure management during the COVID-19 outbreak in Italy: a telemedicine experience from a heart failure university tertiary referral centre. Eur J Heart Fail. 2020;22(6):1048–1050. doi: 10.1002/ejhf.1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gómez-Ochoa SA, Franco OH, Rojas LZ et al (2020) COVID-19 in Healthcare workers: a living systematic review and meta-analysis of prevalence, risk factors, clinical characteristics, and outcomes [published online ahead of print, 2020 Sep 1]. Am J Epidemiol. 2020;kwaa191. 10.1093/aje/kwaa191 [DOI] [PMC free article] [PubMed]