Abstract
Purpose:
The study aimed to explore the prevalence and possible risk factors to prevent the face mask related adverse skin reactions during the ongoing COVID-19 after a recommendation of face mask wearing for public use in Thailand.
Results:
The prevalence of face mask related adverse skin reactions was 454 cases (54.5%), of which acne was the most frequent (399; 39.9%), followed by rashes on the face (154; 18.4%), and itch symptoms (130; 15.6%). Wearing a surgical mask showed a higher risk of adverse skin reaction compared to a cloth mask, OR (95% CI) = 1.54 (1.16-2.06). A duration of face mask wearing of more than 4 hours/day and the reuse of face masks increased the risk of adverse skin reactions compared to changing the mask every day, adjusted OR(95% CI) = 1.96 (1.29-2.98), and 1.5 (1.11-2.02).
Conclusion:
Suggestions were made for wearing a cloth mask in non-health care workers (HCW) to decrease the risk of face mask related adverse skin reactions. This suggestion could potentially help in decreasing the demand of surgical masks which should be reserved for the HCW population during the ongoing COVID-19 pandemic.
Keywords: adverse skin reaction, face mask, COVID-19
Introduction
A novel coronavirus was identified as a causative agent and was subsequently termed COVID-19 by the World Health Organization (WHO).1 This active widespread disease affects the lower respiratory tract, manifests as pneumonia in some humans1-3 and is now still actively transmitted through-out the world. Person-to-person transmission of COVID-19 infection has led to the isolation of patients that were subsequently administered a variety of treatments.2 A recommendation for wearing hygienic masks is currently used in the general population through-out Thailand. In combination with other recommendations such as physical distancing4 and hand hygiene, wearing a face mask5 helps in preventing the spread of the virus and results in decreasing the number of infected cases in Thailand. A recent publication suggested that wearing face masks by the general public is potentially of high value in curtailing community transmission.6 Thus, public face mask wearing is now claimed as a new habit for the Thai population during the COVID-19 pandemic.
In dermatology practice, it is therefore postulated that some adverse skin reactions could occur on the face that might be related to the regular use of this new normal of face mask wearing. There were several reports7-11of adverse skin reaction related to the personal protective equipment, for example, masks, gloves, etc, during this pandemic, however, the need to use this protective equipment is still necessary. This came to the purpose of the present research to focus on the prevalence of adverse reactions on the skin covered by the face mask and the associated factors that might cause adverse skin reactions. The results may help in preventing further adverse skin reactions while the need to wear a face mask during this COVID-19 pandemic is still necessary.
Methods
Participants
All participants age above 18 years old were eligible. It was a survey in a general population by using a publicized announcement and consecutive convenience sample participated to answer the questionnaires based on their interest. These included both health care workers (HCW) and non-HCW participants. A total number of 833 participants were enrolled based on the sample size calculation. The study was planned to determine what proportion of adverse skin reactions resulting from face mask wearing. An estimate of proportion (p) was .35 from the previous study.12 A confidence coefficient of 95% was desired, and an absolute precision (d) of .05 was used.
The study was approved as exemption research by the institutional review board of the Khon Kaen University, Human Research Ethic Committee (#HE631290). The study was funded by a grant from the Khon Kaen University, Faculty of Medicine in Thailand: (Grant Number IN63306).
Methods
This was a prospective cross-sectional study conducted at the Khon Kaen University, Faculty of Medicine, Thailand between 27 May 2020 and 30 June 2020. All participants of an age above 18 years old were eligible. Consecutive convenience samples entered into the Faculty of Medicine, Khon Kaen University, were asked to participate in the study. A structured questionnaire was used to collect the data with the main outcome of identifying adverse skin reactions that occurred on the area covered by a face mask at the time of answering the questionnaire. The demographic background information included in the questionnaire were age, sex, general condition, and underlying skin diseases. The possible risk factors of adverse reactions on the skin covered by the face mask, included types of face masks, average duration of face mask wearing per day, cleaning methods after face mask use, and the underlying skin conditions before the face mask wearing policy, were also addressed in a structured questionnaire.
Statistical Analysis
At the end of the study, the collected data were analyzed using STATA software version 10 (StataCorp LP). Descriptive statistical methods, means, standard deviations (SDs), medians, and frequencies were used to analyze the demographic data. Univariate and multivariate logistic regression analyses were performed to test the associations between the proposed factors and adverse skin reactions from face mask wearing. Values of P < .05 were considered to indicate statistical significance. Incomplete questionnaires and missing data were addressed as imputed data, and final calculations included all recorded data.
Results
A total number of 833 participants were enrolled. There were 222 (26.7%) male and 611 (73.3%) female participants. Making a male to female ratio of .36. The age ranged from 18 to 87 years with the median age of 32 years (IQR 25-41). There were 357 (42.9%) participants who worked as HCW and the rest of the 476 (57.1%) participants were non-HCW. There were 4 types of face masks documented as most frequently used in the study population; surgical masks (526; 63.15%), cloth masks (292; 35.05%), surgical masks covered by a piece of cloth (9; 1.0%) (Figure 1), and N95 masks (6; 0.72%).
Figure 1.

A surgical mask covering by a piece of cloth in the study population.
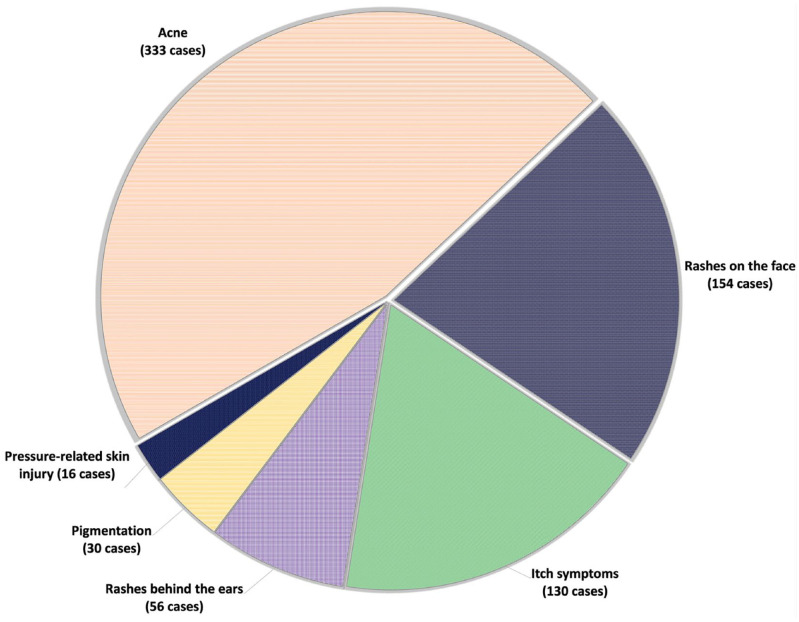
The prevalence of adverse skin reactions on the skin underneath the face masks was found in 454 cases (54.5%). Acne was the most frequent adverse skin reaction found in the study population (333; 39.9%), followed by rashes on the face (154; 18.4%), and itch symptoms (130; 15.6%). Figure 2 shows the list of adverse skin reactions along with the numbers of cases.
Figure 2.
List of adverse skin reactions along with the numbers of case.
Bivariate analysis among factors associated with the present of rashes on the face are presented in Table 1. HCW had adverse skin reaction related to face masks higher than non-HCW participants, (OR (95%CI) = 1.39(1.05-1.83), P .021). Different types of face masks showed significant differences in the presence of adverse skin reactions on the face; wearing a surgical mask showed a higher risk of adverse skin reactions compared to wearing a cloth mask, (OR (95% CI) = 1.54 (1.16-2.06), P .32). Other types of face mask; a surgical mask covered by a piece of cloth and an N95 mask were also shown to be of a higher risk to have adverse skin reaction on the face, (OR(95% CI) = 1.38 (0.36-5.23) and 1.1 (0.22-5.54), P .32). Other factors related to the occurrence of adverse skin reactions in the study population were duration of face mask wearing and the frequency of face mask changing (Table 1).
Table 1.
Bivariate Analysis Among Factors Associated With Face Mask Related Adverse Skin Reactions.
| Factors | Adverse skin reaction on the face covering by face mask | Crude OR (95% CI) | P-value | |
|---|---|---|---|---|
| No adverse skin reaction (n = 379) | Present adverse skin reaction (n = 454) | |||
| Gender | .059 | |||
| Male | 113 (29.82) | 109 (24.01) | 1 | |
| Female | 266 (70.18) | 345 (75.99) | 1.34 (0.99-1.83) | |
| Average time (hours) of face mask wearing duration/day | .004 | |||
| <4 h/day | 112 (29.55) | 107 (23.57) | 1 | |
| 4-8 h/day | 198 (52.24) | 222 (48.9) | 1.17 (0.85-1.63) | |
| >8 h/day | 69 (18.21) | 125 (27.53) | 1.90 (1.28-2.82) | |
| Occupation | .021 | |||
| Non-Health Care Worker | 233 (61.48) | 243 (53.52) | 1 | |
| Health Care Worker | 146 (38.52) | 211 (46.48) | 1.39 (1.05-1.83) | |
| The most frequent type of face mask used during the study | .032 | |||
| Cloth face mask | 153 (40.37) | 139 (30.62) | 1 | |
| Surgical mask | 219 (57.78) | 307 (67.62) | 1.54 (1.16-2.06) | |
| Surgical mask with cloth covering | 4 (1.06) | 5 (1.1) | 1.38 (0.36-5.23) | |
| N95 mask | 3 (0.79) | 3 (0.66) | 1.1 (0.22-5.54) | |
| Frequency of mask changing | (n = 378) | (n = 453) | .055 | |
| Changing mask everyday | 253 (66.93) | 274 (60.49) | 1 | |
| Use at least 2-3 days before changing | 125 (33.07) | 179 (39.51) | 1.32 (0.99-1.76) | |
Significant risk factors from bivariate analysis were further tested for multivariate regression. The result revealed that wearing a face mask 4 to 8 hours/day and more than 8 hours/day increased the risk of adverse skin reactions on the face compared to wearing a face mask fewer or longer than 4 hours/day, (OR (95% CI) = 1.24 (0.89-1.75) and 1.96 (1.29-2.98), P .006). Another risk factor was the disposition of not changing the mask after use every day. This factor showed a 1.5 times risk of having an adverse skin reaction compared to the group that had the face mask changed every day (OR (95% CI) = 1.50 (1.11-2.02), P .008) (Table 2).
Table 2.
Multivariate Regression Among Significant Risk Factors (From Bivariate Analysis) With Adverse Skin Reactions.
| Factors | Crude OR (95% CI) | P-value | Adjusted OR (95% CI) | P-value |
|---|---|---|---|---|
| Average time (hours) of face mask wearing duration/day | .004 | .006 | ||
| <4 h/day | 1 | 1 | ||
| 4-8 h/day | 1.17 (0.85-1.63) | 1.24 (0.89-1.75) | ||
| >8 h/day | 1.90 (1.28-2.82) | 1.96 (1.29-2.98) | ||
| Frequency of mask changing | .055 | .008 | ||
| Changing mask every day | 1 | 1 | ||
| Used at least 2-3 days before changing | 1.32 (0.99-1.76) | 1.50 (1.11-2.02) | ||
| The most frequent type of face mask used during the study | .032 | .157 | ||
| Cloth face mask | 1 | 1 | ||
| Surgical mask | 1.54 (1.16-2.06) | 1.41 (1.05-1.89) | ||
| Surgical mask with cloth covering | 1.38 (0.36-5.23) | 1.28 (0.33-4.93) | ||
| N95 mask | 1.1 (0.22-5.54) | 0.93 (0.12-6.94) |
The most frequent type of face mask used during the study was a confounding factor that could not be excluded from the model.
Discussion
The situation of the COVID-19 pandemic is widespread and affects to all populations through-out the world. The recommendation for wearing the hygienic mask in general use was announced in Thailand as a manner to prevent spreading of the virus during the pandemic since the end of January, 2020. It clearly confirmed that this was an effective policy indicated by a time-lapse number of confirmed COVID-19 cases in Thailand.
In dermatology practice, it was noticed that there were some episodic adverse skin reactions related to face mask wearing even in the general population. This became an objective to study the prevalence of adverse skin reaction related to face mask wearing and the possible risk factors to prevent the occurrence of face mask related adverse skin reactions since there is still an active need to wear a face mask during this COVID-19 pandemic. This study was aimed to focus in both HCW and non-HCW because its effect not only to HCW, reported in similar previous pandemic diseases12 but also to the general population. The present study showed that more than half of the participants (454 cases; 54.5%) reported at least one of adverse skin reaction related to a face mask. This is a high prevalence compared to another previous study that had a prevalence of 35.5% of adverse skin reaction resulting from face mask wearers among HCW in Singapore during the severe acute respiratory syndrome (SARS) pandemic.12 The most frequent adverse skin reaction related to the face mask from a previous study12 was acne (59.6%), followed by an itch symptoms (51.4%), and rashes (35.8%). The present study showed data in a similar way. It was found that the most frequent adverse skin reaction was also acne (333; 39.9%), followed by rashes on the face (154; 18.4%), and itch symptoms (130; 15.6%). The occurrence of acne may be caused by an irritation while wearing a face mask which increases the risk of pilosebaceous gland occlusion. A recommendation of taking appropriate breaks from the mask: 15 minutes off every 2 hours was proposed.7 Moreover, a suggestion for avoiding facial make up, washing the face with gentle, mild fragrance free, noncomedogenic cleanser in the morning and at the end of the day were also recommended.7 The present study tried to find an association between different types of cleanser, skin care products and the presence of acne, however, no statistical significances were found.
Rashes behinds the ears were found in 56 cases (6.72%). Majority of them were the result of the skin breakdown from ear straps. The use of ear savers to allow ear straps to rest on these items instead of the ears was addressed as a suggestion for those who suffered with rashes behinds the ears.
A recent publication of skin damage among HCW managing COVID-19 patients reported a prevalence as high as 97.7%.11 The mentioned study, however, did not focus on the effect of the face mask but included all symptoms that occurred during the study period such as hand eczema and other symptoms on the other areas of the skin. This, was in contrast to the present study that was aimed to explore the factors associated with face mask related adverse skin reactions.
There were 4 types of face masks that were documented as the most frequently used in the study population; surgical mask (526; 63.15%), cloth mask (292; 35.05%), surgical mask covered by a piece of cloth (9; 1.0%), and N95 mask (6; 0.72%). Surgical masks had a higher risk of adverse skin reaction compared to cloth masks (OR (95% CI) = 1.54(1.16-2.06), P .032). There was a way of making a cloth cover on top of a surgical mask (surgical mask covered by a piece of cloth) in Thailand. This method showed a higher risk of adverse skin reaction compared to cloth masks (OR (95% CI) = 1.38 (0.36-5.23), P .032), however, the risk was still less than the group with surgical masks.
Different types of face mask represent differ effectiveness for preventing respiratory virus infections.13 The N95 mask is highly efficient at filtration of airborne particles, blocking at least 95% of very small [0.3 micron] particles.14 HCW who has close contact to infected cases should prefer this type of mask as the most efficient of prevention. Surgical masks are loose-fitting, disposable devices designed to create a physical barrier between the mouth and nose of the wearer and the immediate environment. This type of mask should be reserved for HCW in general medical practice aiming to block the particles and splashes or spatters. Cloth masks are non-medical, face coverings that vary in the cloth material used. Even though, cloth masks should not be recommended for HCW, particularly in high-risk situations,15 it is at least worth for the prevention of respiratory diseases compared to not wearing a mask.16 This type of mask is suited for the general population in public setting. The finding of lower the risk of face mask related adverse skin reaction by using cloth mask from the present study, may encourage the general population to choose a cloth mask for daily use to prevent face mask related adverse skin reactions during this pandemic.
A consideration for wearing a cloth mask to reduce the spread of COVID-19 when they are widely used by people in public settings was mentioned by CDC.17 The recommendation, however, was that this method should not be worn by children under the age of 2 or anyone who has trouble breathing, is unconscious, incapacitated, or otherwise unable to remove the mask without assistance.17
Another factor that caused a higher risk of adverse skin reaction was the duration of face mask wearing of more than 4 hours/day. A previous study proposed that the duration of more than 6 hours/day was a risk factor.11 The current study, however, showed that even only more than 4 hours/day can increase the risk. The longer duration of 4 to 8 hours/day, and more than 8 hours/day revealed a higher risk of an adverse skin reaction (OR (95% CI) = 1.24 (0.89-1.75) and 1.96 (1.29-2.98), P .004). This finding may encourage individuals wearing a mask longer than 4 hours to take a short break for the skin underneath as a mask-free breaks8 to prevent face mask related adverse skin reactions.
Because of a high demand for surgical masks and a situation of a surgical mask crisis during the COVID-19 outbreak,18 the phenomena of reusing face masks has occurred. Many people reused their masks several times before changing. This factor also increased the risk of having face mask related adverse skin reactions in the Thai population. The risk was increased up to 1.5 times in a group that reused the mask and changed them every 2 to 3 days compared to a group that changed the mask every day (adjusted OR (95% CI) = 1.5 (1.11-2.02), P .008).
HCW showed a higher risk to have an adverse skin reaction compared to non-HCW (OR (95% CI) = 1.39(1.05-1.83), P .021). The present study found associated factors after performing subgroup analysis. These factors included a longer duration of face mask wearing in HCW, the more frequent use of surgical masks, and the disposition of not changing masks after use every day compared to non-HCW (Table 3). Even though there was a proposed method to sterilize mask for reuse in a previous study,19 this method is better suited for general use especially where people cannot have enough surgical masks to protect themselves. It is especially effective for people who have to be in a crowded place for a short period of time, however, for the HCW setting, reuse is generally not recommended. Therefore, the factors that can be adjusted beside mask-free breaks in order to prevent face mask related adverse skin reaction in HCW is a policy to provide an adequate number of surgical masks for daily use. Thus, HCW would be able to change surgical masks every day in routine practice.
Table 3.
Subgroup Analysis of Factors Associated With Face Mask Related Adverse Skin Reactions Between HCW and Non-HCW.
| Factors | HCW (n = 357) | Non-HCW (n = 476) | P-value |
|---|---|---|---|
| Average time (hours) of face mask wearing duration/day | <.001 | ||
| <4 h/day | 43 (12.04) | 176 (36.97) | <.001a |
| 4-8 h/day | 172 (48.18) | 248 (52.1) | .294a |
| >8 h/day | 142 (39.78) | 52 (10.92) | <.001a |
| Types of face mask | <.001 | ||
| Cloth mask | 37 (10.36) | 255 (53.57) | <.001a |
| Surgical mask | 315 (88.24) | 211 (44.33) | <.001a |
| Surgical mask with cloth covering | 4 (1.12) | 5 (1.05) | >.999a |
| N95 mask | 1 (0.28) | 5 (1.05) | >.999a |
| Reuse of face mask | <.001 | ||
| Change every day | 256 (71.71) | 271 (57.17) | <.001a |
| Change every 2-3 days | 86 (24.09) | 155 (32.7) | .006a |
| Used more than 3 days before changing | 15 (4.2) | 48 (10.13) | .001a |
Post-hoc test after a chi square test, by using the Bonferroni test.
Limitations
Although our study is the one of the first to describe the face mask effect to the skin and propose risk factors to prevent face mask related adverse skin reactions during the ongoing COVID-19 pandemic, some limitations need to be acknowledged. First, although this study has shown a lower risk of adverse skin reaction in the group who wore a cloth mask compared to a surgical mask, the type of fabric used in a cloth mask needs to be explored. There were many types of fabric used in cloth masks and this factor may cause different outcome. Second, the present study was explored a warm climate in Thailand, where the temperature was 29°C to 35°C during May and June 2020. The climate issue may affect the result of face mask related adverse skin reaction. A future study during the winter season or in a different part of the world may affect the results.
Conclusion
The prevalence of face mask related adverse skin reactions during COVID-19 pandemic was 54.5%. The most frequent adverse skin reaction was acne. HCW had a higher risk compared to non-HCW. There were several risk factors including duration of face mask wearing more than 4 hours/day, and the reuse of face masks. The present study found that wearing a cloth mask had the lowest risk of adverse skin reactions. This study results suggest that the general population, especially non-HCW, to use this cloth type of mask instead of a surgical mask. Besides lowering the risk of face mask related adverse skin reaction, this suggestion could potentially help in decreasing the demand of surgical masks which should be reserved for the HCW population during the ongoing COVID-19 pandemic.
Acknowledgments
We would like to acknowledge Prof James Arthur Will, for editing the MS via Publication Clinic KKU, Thailand. The participants in this manuscript have given written informed consent to publication of their information details.
Footnotes
Author Contributions: SL, WT, KW, SP, SS, DM, CS, PK, and PK, contributed to the study design and analysis, drafted the manuscript, gave final approval, and agrees to be accountable for all aspects of work ensuring the integrity and accuracy of this work. DM provided the figure in the manuscript. JC, contributed to analysis and interpretation, gave final approval, and agrees to be accountable for all aspects of ensuring integrity and accuracy of this work. LT and RU, contributed to the study design, analysis, and interpretation, critically revised manuscript. LT drafted and revised the manuscript, gave final approval, and agrees to be accountable for ensuring the integrity and accuracy of this work. All authors gave final approval, and agrees to be accountable for ensuring the integrity and accuracy of this work.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was funded by a grant from the Khon Kaen University, Faculty of Medicine in Thailand (grant number #IN63306).
ORCID iD: Leelawadee Techasatian  https://orcid.org/0000-0003-4668-6792
https://orcid.org/0000-0003-4668-6792
References
- 1. Sohrabi C, Alsafi Z, O’Neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg Lond Engl. 2020;76:71-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. El Hachem M, Diociaiuti A, Concato C, et al. A clinical, histopathological and laboratory study of 19 consecutive Italian paediatric patients with chilblain-like lesions: lights and shadows on the relationship with COVID-19 infection [published online May 31, 2020]. J Eur Acad Dermatol Venereol JEADV. doi: 10.1111/jdv.16682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet Lond Engl. 2020;395:1973-1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Esposito S, Principi N, Leung CC, Migliori GB. Universal use of face masks for success against COVID-19: evidence and implications for prevention policies. Eur Respir J. 2020;55:2001260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Eikenberry SE, Mancuso M, Iboi E, et al. To mask or not to mask: modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect Dis Model. 2020;5:293-308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Desai SR, Kovarik C, Brod B, et al. COVID-19 and personal protective equipment: treatment and prevention of skin conditions related to the occupational use of personal protective equipment. J Am Acad Dermatol. 2020;83:675-677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Payne A. Covid-19: skin damage with prolonged wear of FFP3 masks. BMJ. 2020;369:m1743. [DOI] [PubMed] [Google Scholar]
- 9. Chowdhury MM, Bevan N, Ryan K. Covid-19: virtual occupational skin health clinics for healthcare workers. BMJ. 2020;369:m2281. [DOI] [PubMed] [Google Scholar]
- 10. Hadjieconomou S, Hughes J, Kamath S. Occupational skin disease during the COVID-19 pandemic, as captured in a Dermatology staff clinic in the United Kingdom [published online June 14, 2020]. J Eur Acad Dermatol Venereol JEADV. doi: 10.1111/jdv.16754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lan J, Song Z, Miao X, et al. Skin damage among health care workers managing coronavirus disease-2019. J Am Acad Dermatol. 2020;82:1215-1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Foo CCI, Goon ATJ, Leow Y-H, Goh C-L. Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome–a descriptive study in Singapore. Contact Dermatitis. 2006;55:291-294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chou R, Dana T, Jungbauer R, Weeks C, McDonagh MS. Masks for prevention of respiratory virus infections, including SARS-CoV-2, in health care and community settings. Ann Intern Med. 2020;173:542-555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Loeb M, Dafoe N, Mahony J, et al. Surgical mask vs N95 respirator for preventing influenza among health care workers: a randomized trial. JAMA. 2009;302:1865-1871. [DOI] [PubMed] [Google Scholar]
- 15. MacIntyre CR, Seale H, Dung TC, et al. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015;5:e006577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Konda A, Prakash A, Moss GA, Schmoldt M, Grant GD, Guha S. Aerosol filtration efficiency of common fabrics used in respiratory cloth masks. ACS Nano. 2020;14:6339-6347. [DOI] [PubMed] [Google Scholar]
- 17. Centers for Disease Control and Prevention (CDC). Coronavirus Disease 2019 (COVID-19). https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover-guidance.html. Published February 11, 2020. Accessed July 28, 2020.
- 18. Wang M-W, Zhou M-Y, Ji G-H, et al. Mask crisis during the COVID-19 outbreak. Eur Rev Med Pharmacol Sci. 2020;24:3397-3399. [DOI] [PubMed] [Google Scholar]
- 19. Phan TL, Ching CT-S. A reusable mask for coronavirus disease 2019 (COVID-19). Arch Med Res. 2020;51:455-457. [DOI] [PMC free article] [PubMed] [Google Scholar]