Abstract
Nursing skill education plays a very important part for the nursing education. It’s necessary to analyze the role of the case-based teaching (CBT) in nursing skill education, to provide insights into the nursing education. The sophomore nursing students who received nursing skill teaching from September 2019 to January 2020 were selected. The students either underwent traditional teaching (control group) or CBT (CBT group) intervention. The objective structure clinical examination (OSCE), autonomous learning ability, questionnaire for effects evaluation of CBT, and student’s satisfaction level on CBT were analyzed. A total of 146 participants were included. There were no significant differences in the gender, age and the final exam score as freshman between 2 groups (all P > .05). The OSCE scores and autonomous learning ability in CBT group were significantly higher than that of control group (all P < .05). The most students favored the use of CBT, and most students were satisfied with CBT. CBT is beneficial to improve the nursing skill and comprehensive ability of students, and it’s conducive to increase the interest of students, which merits application in nursing education.
Keywords: case-based teaching, nursing, education, student
What do we already know about this topic?
Nursing skill education is a very important part of nursing education. The role of the case-based teaching (CBT) in nursing skill education remains unclear.
How does your research contribute to the field?
CBT is beneficial to improve the nursing skill and comprehensive ability of students. CBT is conducive to increase the interest of students.
What are your research’s implications toward theory, practice, or policy?
Cases should be introduced for application in nursing skill education.
Background
Basic nursing course is the core course of nursing major, and it is one of the main courses to cultivate the core competence of nursing students.1 Basic nursing course is a comprehensive subject in clinical nursing with coverage of a wide range of content. Previous studies2,3 have reported that students in nursing colleges have poor cultural foundations, unclear learning motivation, weak self-learning ability, and easy to waste the after-school time. At present, the mainstream 1-way teaching model of “teach-accept” is very common in the university.4 It is difficult for teachers to understand that whether the review and consolidation have been carried out after class, so that teachers cannot teach according to student’s progress, and students reflect that it is difficult to learn and teachers feel difficult to teach.5 Therefore, it is imperative to explore reasonable and effective nursing teaching.
Nursing skill teaching is an important part of basic nursing course. In the teaching course structure of basic nursing for undergraduate nursing students, the proportion of class hours accounts for 50% to 60%.6 The traditional nursing skill teaching method is “demonstration-practice-guidance,” which focuses on nursing students to master the skill operation through imitation of the experimental process.7 For this method, the students often lack in-depth thinking and joint discussion, and cannot combine clinical flexibly in practice.8 The case-based teaching (CBT) is a mixed teaching method emphasizing case-based guidance, which is integrated with teaching objectives.9 It’s been reported that CBT may have the advantage of emphasizing the enthusiasm of teaching, stimulating students’ interest in learning and improving students’ independent learning and interpersonal communication ability.10,11 However, currently there are still few reports about the application of CBT in nursing teaching,12 and its application in nursing skills teaching needs further investigation. Furthermore, there are very few studies on the CBT use in nursing education in China. Therefore, we aimed to conduct this study to evaluate the role of CBT in nursing skill education, thereby providing reliable evidence to medical education.
Methods
This study was designed as a randomized controlled study without blind design. We aimed to conduct and reported this trial in comply with the guideline of Consolidated Standards of Reporting Trial (CONSORT). And since our study was a part of course reform in our university, and no potential harm might pose to students, and we had informed the students on the details of course changes before intervention. We did not register our trial prospectively.
Participants
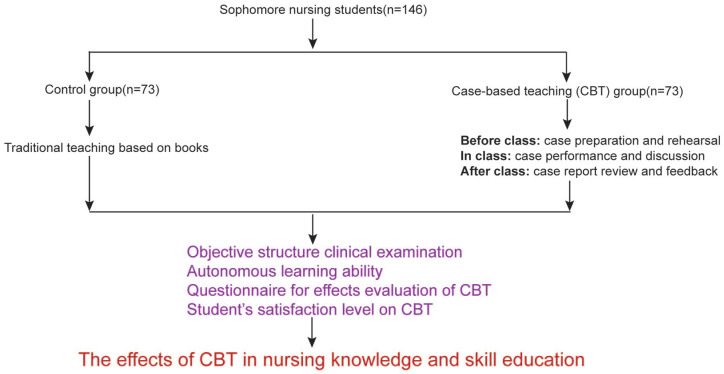
The sophomore undergraduate nursing students of class 2018 who received nursing skill teaching from September 2019 to January 2020 were selected as the potential participants. The students were randomly assigned to the experimental and control groups based on the random number generated by computer. The inclusion criteria for the participants were: age ≥18 years; sophomore students voluntarily participated in this study. And the exclusion criteria were: students who have previously undergone the course of nursing skill, and the students who were unwilling to participant were also excluded. The included participants were randomly divided into control and CBT group, the control group underwent traditional teaching, whereas the CBT group underwent CBT. The flow chart of study design is presented in Figure 1.
Figure 1.
The flow chart of study design.
The Traditional Teaching
Nursing skill teaching was a required course in our school. The objectives of this course were to input nursing skill to students to ensure that they obtained necessary basic nursing skills in clinical settings. The ratio of professors to students was 1:8 both for 2 groups. For control group, the traditional teaching mode was adopted. That is, “teaching-accepting,” the teacher leads the teaching process, and the students passively accept. In order to reduce the difficulty of learning, teachers arranged problems before class, and instructed students to consult textbooks and related basic knowledge to prepare for classroom teaching. During the class, the teacher inserted teaching materials such as pictures and videos, and personally demonstrated the nursing operation skills, and interspersed their key and difficult contents. After class, assignments were conducted to consolidate knowledge.
CBT
For CBT intervention, we used the preset typical clinical cases as the main body of the case, started the nursing skill teaching with situation simulation, and drove the problem setting as the link to finally achieve the teaching goals. In the course of teaching, it emphasized the students’ ability to learn actively and cooperated with each other, as well as the consistency and integration of nursing students’ personal knowledge, abilities and attitudes when providing nursing services to patients.
Before class, according to the teaching progress and arrangement, the teacher prepared a typical case, which was based on the common clinical diseases, and raised 3 to 4 questions related to the implementation of the operation to cultivate students’ clinical thinking and humanities care. A total of 23 cases were used, and the themes of all the 23 cases were presented in Table 1. All the cases were selected and validated by our teachers of CBT. For example, the oral care case: “Patient Wang, female, 65 years old, cough, expectoration and asthma for 3 weeks, was admitted to the community hospital for 5 days after infusion of antibacterial drugs with a history of diabetes. Physical examination: body temperature 38.5°C, pulse 80 times/min, 20 breaths/min, blood pressure 140/90 mmHg, dry oral mucosa and it’s covered with large white pseudo-membrane. Diagnosis: acute bronchitis, oral fungi Infection. Doctor’s order: oral care 2 times/d.” Questions: “a. The patient is in a poor condition. From what aspects will you conduct nursing evaluation? How will you arrange and fully reflect it in the communication? b. The patient has dry and cracked lips and bad breath, but patient refuses to touch to open the month, what will you do as a nurse on duty? c. The patient suddenly experiences discomfort symptoms such as nausea and vomiting during oral care, what may happen? How do you deal with it? d. How to carry out disease health education for this patient?” Teachers uploaded the case data and experimental report content to the WeChat (a kind of software like Facebook for social interaction) for the preparation of students 1 week in advance. There were 8 groups of nursing students, and each group was required for case performance. The task is to perform role-playing in the classroom according to the case design. The content was designed as a link, and the goal was to complete the implementation of nursing skill. The roles of case included at least 3 kinds, including nurses, patients, and family members. And the contents should include the disease-related knowledge interpretation, nursing evaluation, nurse-patient communication, and disease-oriented health education. All students could reserve an independent classroom 1 to 2 days in advance to conduct pre-rehearsal and practical practice of the scene display, and invited teachers to guide when necessary.
Table 1.
The Themes of All the 23 Cases.
| Number | Themes | Number | Themes |
|---|---|---|---|
| 1 | Vital sign monitoring technology | 13 | Restraint use |
| 2 | Aseptic technique | 14 | Gastric lavage technique |
| 3 | Oral care skill | 15 | Prevention and care of pressure related injuries |
| 4 | Nasal feeding technique | 16 | Wound and stoma care |
| 5 | Urinary catheterization technique and nursing | 17 | Infusion pump/micro pump use skill |
| 6 | Enema skill | 18 | Bladder irrigation care |
| 7 | Oxygen inhalation technology | 19 | Nursing care of closed thoracic drainage |
| 8 | Intravenous indwelling needle technique | 20 | Light therapy |
| 9 | Drug injection skills | 21 | Prevention of patient falls |
| 10 | Defibrillation technology | 22 | Physical cooling skill |
| 11 | Cardiopulmonary resuscitation skill | 23 | Umbilical care of newborns |
| 12 | Sputum suction skill |
In class, the teacher briefly analyzed and explained the case. After the teacher commented and emphasized the key content, the students began to case performance in groups, including that the team members took turns to play the roles of patient, family member, nurse and observer, etc, and carry out nursing care, communication and interaction according to the case information. Teachers toured between classes, answered students’ questions at any time, helping to correct operation details and adjusting communication orientation.
After class, students were required to submit the case reports, teachers reviewed and summarized the key points of nursing care amongst cases. And we reserved an open laboratory for case review and practice in groups.
Outcome Assessment
Objective structure clinical examination
Objective structure clinical examination (OSCE) required the students to finish multiple examination within the prescribed time to complete the examination content of each station, and the final comprehensive score was used for the result evaluation.13 (1) Scope of skill test items: including bed sheet replacement, oral care, pressure ulcer prevention care, vital signs measurement, oxygen supply, and intradermal injection; (2) Test method: case-based assessment. According to the scope of the skill test, 1 clinical case was set for each operation, and a total of 6 test cases were composed; (3) Examination format: OSCE 3-stop assessment, that is, nursing evaluation-nursing care practice-health education. Candidates draw a case number in the station, and the test begins to time. The completion time of each station is 10 minutes. The weight ratio was 10% for nursing assessment, 70% for nursing care practice, and 20% for health education. The interrater reliability of OSCE was 0.785, and the OSCE was rated by the same 2 teachers.
Autonomous learning ability
The self-learning ability of 2 groups of nursing students was evaluated using the scale of nursing students’ autonomous ability compiled by Lin and Jiang .14 The scale included 28 items in 3 dimensions of self-management ability, information analysis ability and learning cooperation ability. We used Likert 5 grades (1-5 points), the score range was 28~140, the higher the score, the better the autonomous learning ability. The scale Cronbach α coefficient was 0.863, and the split-half reliability was 0.766.
Questionnaire for effects evaluation of CBT
Based on previous reports,15,16 we designed a questionnaire for the effect evaluation of CBT. The questionnaire had a total of 18 items, and each item had a score range of 1 to 5 points, and the highest score was 90. The Cronbach α coefficient of this questionnaire was 0.723 with good reliability. The content included 4 aspects: effect on knowledge learning, feelings about CBT implementation and feelings about self-improvement, and further perfect strategy. The scale of Cronbach α coefficient was 0.801, and the split-half reliability was 0.738.
Student’s satisfaction level on CBT
The satisfaction of the nursing students on CBT were investigated, and the content included 5 aspects: was it better than traditional teaching; was it reduce the learning difficulty; was it increase learning interest; was it improve the communication skills; was it improve cooperation skills. And every aspect could be rated into strongly agree, agree and disagree.
Statistical analysis
SPSS 23.0 was used to analyze the data. Continuous data were expressed as mean ± standard deviation, and binary data were expressed as frequency and percentage. Comparison between 2 groups were conducted using independent sample t test or Wilcoxon rank test. And P < .05 was considered that the difference between groups was statistically significant.
Results
The Characteristics of Included Students
As Table 2 presented, a total of 146 participants were included, with 73 students in each group. The response rate of the survey was 100%, and no student dropped out during the intervention. There were no significant differences in the gender, age and the final exam score as freshman between 2 groups (all P > .05), indicating that the baseline data of the 2 groups of participants were comparable.
Table 2.
The Characteristics of Students Between 2 Groups.
| Items | Control group (n = 73) | CBT group (n = 73) | χ2/t | P |
|---|---|---|---|---|
| Gender | ||||
| Female | 70 | 69 | 1.198 | .244 |
| Male | 3 | 4 | ||
| Age (y) | 20.38 ± 1.84 | 20.29 ± 1.78 | 3.104 | .095 |
| The final exam score as freshman | 76.13 ± 8.10 | 75.97 ± 7.21 | 6.170 | .072 |
The OSCE Scores
As Table 3 showed, OSCE scores in CBT group were significantly higher than that of control group (all P < .05), indicating that CBT was beneficial to improve the OSCE scores of students.
Table 3.
The Results of OSCE Between 2 Groups.
| Items | Control group (n = 73) | CBT group (n = 73) | χ2/t | P |
|---|---|---|---|---|
| Nursing evaluation | 6.55 ± 1.14 | 7.12 ± 1.48 | 1.285 | .041 |
| Nursing skill performance | 55.97 ± 5.13 | 58.28 ± 5.02 | 9.042 | .036 |
| Health education | 12.84 ± 2.80 | 14.21 ± 3.18 | 3.114 | .023 |
| Total scores | 77.08 ± 7.94 | 80.12 ± 8.29 | 12.192 | .037 |
The Autonomous Learning Ability
As Table 4 presented, the autonomous learning ability in CBT group were significantly higher than that of control group (all P < .05), indicating that the CBT was beneficial to improve the autonomous learning ability of students.
Table 4.
The Autonomous Learning Ability Between 2 Groups.
| Items | Control group (n = 73) | CBT group (n = 73) | χ2/t | P |
|---|---|---|---|---|
| Self-management ability | 31.86 ± 6.15 | 33.19 ± 6.29 | 7.482 | .031 |
| Information analysis ability | 30.17 ± 6.08 | 32.97 ± 5.66 | 5.107 | .045 |
| Learning cooperation ability | 21.19 ± 5.36 | 23.25 ± 5.10 | 3.353 | .018 |
| Total scores | 84.53 ± 9.15 | 89.07 ± 9.47 | 11.149 | .012 |
The Effects Evaluation of CBT
As Table 5 presented, the most students favored the use of CBT and CBT was effective, indicating that CBT was prone to improve the teaching effects.
Table 5.
The Questionnaire Results for Effects Evaluation of CBT.
| Items | Full scores | Students’ average score |
|---|---|---|
| Effect on knowledge learning | 15 | 12.03 ± 2.44 |
| Feelings about CBT implementation | 20 | 16.11 ± 3.15 |
| Feelings about self-improvement | 30 | 25.03 ± 5.75 |
| Further perfect strategy | 25 | 21.18 ± 4.37 |
Student’s Satisfaction Level on CBT
As Table 6 presented, most students were satisfied with CBT, indicating that students support the use of CBT in the nursing skill education.
Table 6.
Student’s Satisfaction Level on CBT (n = 73).
| Items | Strongly agree | Agree | Disagree |
|---|---|---|---|
| Better than traditional teaching | 62 (84.93%) | 11 (15.07%) | 0 (0%) |
| Reduce the learning difficulty | 47 (64.38%) | 34 (46.58%) | 2 (2.74%) |
| Increase learning interest | 66 (90.41%) | 7 (9.59%) | 0 (0%) |
| Improve communication skills | 52 (71.23%) | 21 (28.77%) | 0 (0%) |
| Improve cooperation skills | 64 (87.67%) | 8 (10.96%) | 1 (1.37%) |
Discussion
Traditionally, teacher’s teaching focuses on the technical operation process itself, and the students form the simplest operation awareness and operation imitation.17 The lack of situational experience and simple imitation is not conducive to the master of nursing skills.18,19 Therefore, to a some extent, it limits the combination of student skills learning of knowledge theory and practice. The results of this present study have found that the CBT is beneficial to the master of nursing skills, and it’s conducive to the intrigue the interests of students and improve the communication and cooperative ability among students. Furthermore, students are pleased to accept CBT and favored the use of CBT.
For CBT, the teachers introduce typical cases into the classroom, integrate nursing practice into nursing situations, and create a medical atmosphere for students through scenario simulation and role-playing, which improves the authenticity experience of nursing students in the implementation of nursing.20-22 It leads nursing students into professional roles and cultivate professional consciousness to complete nursing behaviors with high degree of personal awareness. Nursing students enhance their social understanding by playing the positions and demands of fully experiencing different roles, and solidify the concept of vocational education that puts learning into practice.23 During the question and dialogue session of the patient/family for the implementation of nursing care, on one hand, it can guide the nursing students to think professionally and quickly use the medical knowledge they have to answer.24 On the other hand, the teacher can promptly correct possible omissions, deficiencies and even errors in the practice.25 Promoting the learning and application of knowledge by nursing students through personal experience and personal experience is the original intention and goal of teaching design based on CBT methods.26,27 CBT is conducive to the reserve and enhancement of medical nursing knowledge for nursing students, and is conducive to flexibility and application when they are exposed to similar situations again.28,29
The CBT design is closely linked before, during, and after class. Nursing students are prepared to enter the classroom through team learning and independent learning to pave the way for the internalization of CBT knowledge, and it will be relatively easy to complete knowledge assimilation in the classroom.30 In class, we systematize the learning of knowledge, to have a more comprehensive grasp of what they have learned. And the diversification of teaching methods further stimulates the learning motivation and interest of nursing students.31 Nursing students actively participate, and good classroom interaction helps the nursing students complete the internalization of knowledge.32 After class, the design of exercises and cases is designed for students to distinguish knowledge points that are easy to be confused. After-class exercises are an extension of classroom discussion,33 so that the knowledge learned in the classroom can be effectively consolidated and strengthened. The CBT arouses the interest of nursing students in learning, and it facilitates the internalization of nursing skills.34-36
The social desirability in studies among the students with CBT should be considered. The school’s teaching methods are diversified, and on the basis of learning majors, more attention is paid to the cultivation of students’ comprehensive abilities in the CBT. The role of teachers has changed from the traditional “instructor” to “designer” and “guider.” Furthermore, students have more opportunities to choose and participate in “how to teach” and “how to learn.”37 In CBT, teachers need to further play a guiding role in knowledge learning, encourage students to express personal considerations for patients’ benefits, and build confidence in learning.33,38 Moreover, it’s necessary to organize students to reflect and discuss in a timely manner, and cultivate the ability to actively find problems and deal with problems.39 CBT is an exploratory reform carried out on the basis of traditional teaching. It is a change that pose great impacts on the study habits of nursing students.40-42 For the different obstacles faced by nursing students in case implementation, it’s necessary to point out their own shortcomings and the direction of making up later.43 Therefore, in the cultivation of ability of nursing students, it is necessary to take the implementation and communication ability as 2 important evaluation indicators to measure in the ability assessment of nursing students.44 At the same time, in nursing skill assessment, it is necessary to increase the proportion of the performance of nursing evaluation and nursing communication, making it more in line with the social needs of personnel training.45,46 However, even rough the response rate was 100% in our study, the students might have feel coerced to participate, thus biases might be existed.
Several limitations must be concerned in this study. Firstly, the case-based learning cases and OSCE cases were the same in our study, the same cases might be over-rated and might be not innovative for the nursing skills in clinical settings, the choices and verifications of cases should be considered discreetly in the future studies. It’s note-worthy that the OSCE was case-based, thus it potentially favored the CBT group. And it’s a major limitation that we did not have the data on validity of our survey questionnaire, thus, the significant biases might be existed. Secondly, WeChat is very popular amongst students, there may be some the cross-contaminations among 2 groups. Thirdly, the choice of satisfaction in this present study only included strongly agree, agree and disagree, it may direct students towards positive side of that scale, future studies with details on the level of satisfaction are needed. Furthermore, when reporting Cronbach of multi-dimensional tool, we only reported the overall tool alpha, but we did not obtain each subcategory alpha, future studies with checks on the subcategory alpha can be more convincing.
Conclusion
In conclusion, CBT is beneficial to expand teachers’ teaching ideas and mobilize students’ interest in learning, and the autonomous learning ability of nursing students has improved, and good teaching effects have been achieved. However, in the implementation process, it should be noted that the teachers should spend more energy and time on case teaching design, supervising students’ learning and answering questions. Future researches are needed to further explore the efficiency and quality of CBT.
Footnotes
Author Contributions: LL, ML designed research; LL, HJ conducted research; LL, QZ analyzed data; LL wrote the first draft of manuscript; HJ had primary responsibility for final content. All authors read and approved the final manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Jiangxi Province’s “Thirteenth Five-Year” Plan 2020(20YB327).
Ethical Approval and Consent to Participate: Our study has been approved by the ethics committee of Jingganshan University(2019094), and written informed consents have been obtained from all the participants.
ORCID iD: Hua Jiang  https://orcid.org/0000-0002-2433-3753
https://orcid.org/0000-0002-2433-3753
Availability of Data and Materials: All data generated or analyzed during this study are included in this published article.
References
- 1. Scott Barss K. Spiritual care in holistic nursing education: a spirituality and health elective rooted in T.R.U.S.T. and contemplative education. J Holist Nurs. 2020;38:122-130. doi: 10.1177/0898010119889703. [DOI] [PubMed] [Google Scholar]
- 2. Fares S, Dumit NY, Dhaini SR. Basic and continuing education needs of nurses instrument: development and validation. Int Nurs Rev. 2020;67:92-100. doi: 10.1111/inr.12520. [DOI] [PubMed] [Google Scholar]
- 3. Green G. Examining professional values among nursing students during education: a comparative study [published online ahead of print June 2, 2020]. Nurs Forum. doi: 10.1111/nuf.12474. [DOI] [PubMed] [Google Scholar]
- 4. Devido JA, Appelt CJ, Simpson AT, et al. The future of nursing education: multidisciplinary community-engaged research for undergraduate nursing students. J Nurs Educ. 2020;59: 341-344. doi: 10.3928/01484834-20200520-08. [DOI] [PubMed] [Google Scholar]
- 5. Representatives of the Global Familial Hypercholesterolemia C, Wilemon KA, Patel J, et al. Reducing the clinical and public health burden of familial hypercholesterolemia: a global call to action. JAMA Cardiol. 2020;5(2):217-229. doi: 10.1001/jamacardio.2019.5173. [DOI] [PubMed] [Google Scholar]
- 6. Yune SJ, Park KH, Min YH, et al. Perceptions of the interprofessional education of the faculty and the level of interprofessional education competence of the students perceived by the faculty: a comparative study of medicine, nursing, and pharmacy. Korean J Med Educ. 2020;32:23-33. doi: 10.3946/kjme.2020.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Campbell E. Faculty perspectives of teaching pain management to nursing students. Pain Manag Nurs. 2020;21:179-186. doi: 10.1016/j.pmn.2019.07.010. [DOI] [PubMed] [Google Scholar]
- 8. Luciani M, Rampoldi G, Ardenghi S, et al. Personal values among undergraduate nursing students: a cross-sectional study. Nurs Ethics. 2020;27(6):10-18. doi: 10.1177/0969733020914350. [DOI] [PubMed] [Google Scholar]
- 9. Aluko A, Rana J, Burgin S. Teaching & learning tips 9: case-based teaching with patients. Int J Dermatol. 2018;57:858-861. doi: 10.1111/ijd.13781. [DOI] [PubMed] [Google Scholar]
- 10. Bi M, Zhao Z, Yang J, et al. Comparison of case-based learning and traditional method in teaching postgraduate students of medical oncology. Med Teach. 2019;41:1124-1128. doi: 10.1080/0142159X.2019.1617414. [DOI] [PubMed] [Google Scholar]
- 11. Slieman TA, Camarata T. Case-based group learning using concept maps to achieve multiple educational objectives and behavioral outcomes. J Med Educ Curric Dev. 2019;6: 2382120519872510. doi: 10.1177/2382120519872510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. McLean SF. Case-based learning and its application in medical and health-care fields: a review of worldwide literature. J Med Educ Curric Dev. 2016;3:JMECD-S20377. doi: 10.4137/JMECD.S20377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fischer MA, Kennedy KM, Durning S, et al. Situational awareness within objective structured clinical examination stations in undergraduate medical training - a literature search. BMC Med Educ. 2017;17:262. doi: 10.1186/s12909-017-1105-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lin Y, Jiang A. Development of a self-learning ability assessment scale for college nursing students. People’s Liberation Army Nursing Magazine. 2004;21:1-4. [Google Scholar]
- 15. Wang G. A Study on the Effect of Applying Situational Simulation Teaching Method on the Autonomous Learning Ability of Undergraduate Nursing Students in the Experimental Teaching of “Basic Nursing Science”. Dalian Medical University; 2013. [Google Scholar]
- 16. Ye T, Zhu H, Chen J. Effect of scene simulation teaching method and case learning method for developing independent learning capabiliey of nursing students. Chin Nur Res. 2014;18:3832-3834. [Google Scholar]
- 17. Turk B, Ertl S, Wong G, et al. Does case-based blended-learning expedite the transfer of declarative knowledge to procedural knowledge in practice? BMC Med Educ. 2019;19:447. doi: 10.1186/s12909-019-1884-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Waliany S, Caceres W, Merrell SB, et al. Preclinical curriculum of prospective case-based teaching with faculty- and student-blinded approach. BMC Med Educ. 2019;19:31. doi: 10.1186/s12909-019-1453-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kovacevic P, Dragic S, Kovacevic T, et al. Impact of weekly case-based tele-education on quality of care in a limited resource medical intensive care unit. Crit Care. 2019;23:220. doi: 10.1186/s13054-019-2494-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Raurell-Torreda M, Olivet-Pujol J, Romero-Collado A, et al. Case-based learning and simulation: useful tools to enhance nurses’ education? Nonrandomized controlled trial. J Nurs Scholarsh. 2015;47:34-42. doi: 10.1111/jnu.12113. [DOI] [PubMed] [Google Scholar]
- 21. Bullock A, Barnes E, Ryan B, et al. Case-based discussion supporting learning and practice in optometry. Ophthalmic Physiol Opt. 2014;34:614-621. doi: 10.1111/opo.12151. [DOI] [PubMed] [Google Scholar]
- 22. Harman T, Bertrand B, Greer A, et al. Case-based learning facilitates critical thinking in undergraduate nutrition education: students describe the big picture. J Acad Nutr Diet. 2015; 115:378-388. doi: 10.1016/j.jand.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 23. MacKinnon K, Marcellus L, Rivers J, et al. Student and educator experiences of maternal-child simulation-based learning: a systematic review of qualitative evidence protocol. JBI Database Syst Rev Implement Rep. 2015;13:14-26. doi: 10.11124/jbisrir-2015-1694. [DOI] [PubMed] [Google Scholar]
- 24. Durmaz A, Dicle A, Cakan E, et al. Effect of screen-based computer simulation on knowledge and skill in nursing students’ learning of preoperative and postoperative care management: a randomized controlled study. Comput Inform Nurs. 2012;30:196-203. doi: 10.1097/NCN.0b013e3182419134. [DOI] [PubMed] [Google Scholar]
- 25. Johnston S. An evaluation of simulation bebriefings on student nurses’ perceptions of clinical reasoning and learning transfer: a mixed methods study. Int J Nurs Educ Scholarsh. 2019;16(1):5-9. doi: 10.1515/ijnes-2018-0045. [DOI] [PubMed] [Google Scholar]
- 26. Weatherspoon DL, Wyatt TH. Testing computer-based simulation to enhance clinical judgment skills in senior nursing students. Nurs Clin North Am. 2012;47:481-491. doi: 10.1016/j.cnur.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 27. McFee RM, Cupp AS, Wood JR. Use of case-based or hands-on laboratory exercises with physiology lectures improves knowledge retention, but veterinary medicine students prefer case-based activities. Adv Physiol Educ. 2018;42:182-191. doi: 10.1152/advan.00084.2017. [DOI] [PubMed] [Google Scholar]
- 28. Thistlethwaite JE, Davies D, Ekeocha S, et al. The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME Guide No. 23. Med Teach. 2012;34:e421-e444. doi: 10.3109/0142159X.2012.680939. [DOI] [PubMed] [Google Scholar]
- 29. Kantar LD, Massouh A. Case-based learning: what traditional curricula fail to teach. Nurse Educ Today. 2015;35:e8-e14. doi: 10.1016/j.nedt.2015.03.010. [DOI] [PubMed] [Google Scholar]
- 30. Lovink MH, Laurant MG, van Vught AJ, et al. Substituting physicians with nurse practitioners, physician assistants or nurses in nursing homes: a realist evaluation case study. BMJ Open. 2019;9:e028169. doi: 10.1136/bmjopen-2018-028169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nickles D, Dolansky M, Marek J, et al. Nursing students use of teach-back to improve patients’ knowledge and satisfaction: a quality improvement project. J Prof Nurs. 2020;36:70-76. doi: 10.1016/j.profnurs.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 32. Huang CY, Wang YH. Toward an integrative nursing curriculum: combining team-based and problem-based learning with emergency-care scenario simulation. Int J Environ Res Public Health. 2020;17(12):4612. doi: 10.3390/ijerph17124612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pilcher J. Promoting learning using case-based strategies in nursing professional development. J Nurses Prof Dev. 2018; 34:199-205. doi: 10.1097/NND.0000000000000458. [DOI] [PubMed] [Google Scholar]
- 34. Ardian P, Hariyati RTS, Afifah E. Correlation between implementation case reflection discussion based on the Graham Gibbs Cycle and nurses’ critical thinking skills. Enferm Clin. 2019;29(Suppl 2):588-593. doi: 10.1016/j.enfcli.2019.04.091.31303519 [DOI] [Google Scholar]
- 35. Hallock AB. A case for leadership development in nursing practice. Nephrol Nurs J. 2019;46:325-328. [PubMed] [Google Scholar]
- 36. Padilha JM, Machado PP, Ribeiro A, et al. Clinical virtual simulation in nursing education: randomized controlled trial. J Med Internet Res. 2019;21:e11529. doi: 10.2196/11529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Nunohara K, Imafuku R, Saiki T, et al. How does video case-based learning influence clinical decision-making by midwifery students? An exploratory study. BMC Med Educ. 2020;20:67. doi: 10.1186/s12909-020-1969-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kim TW, Singh S, Miller C, et al. Efficacy and cost comparison of case-based learning to simulation-based learning for teaching malignant hyperthermia concepts to anesthesiology residents. J Educ Perioper Med. 2019;21:E631. [PMC free article] [PubMed] [Google Scholar]
- 39. Kresevic D, Heath B, Fine-Smilovich E, et al. Simulation training, coaching, and cue cards improve delirium care. Fed Pract. 2016;33:22-28. [PMC free article] [PubMed] [Google Scholar]
- 40. Knopf-Amelung S, Gotham H, Kuofie A, et al. Comparison of instructional methods for screening, brief intervention, and referral to treatment for substance use in nursing education. Nurse Educ. 2018;43:123-127. doi: 10.1097/NNE.0000000000000439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Thiel CE, Connelly S, Harkrider L, et al. Case-based knowledge and ethics education: improving learning and transfer through emotionally rich cases. Sci Eng Ethics. 2013;19:265-286. doi: 10.1007/s11948-011-9318-7. [DOI] [PubMed] [Google Scholar]
- 42. Eseonu O, Carachi R, Brindley N. Case-based anatomy teaching: a viable alternative? Clin Teach. 2013;10:236-241. doi: 10.1111/tct.12013. [DOI] [PubMed] [Google Scholar]
- 43. Daniels FM, Fakude LP, Linda NS, et al. Nurse educators’ experiences of case-based education in a South African nursing programme. Curationis. 2015;38:1523. doi: 10.4102/curationis.v38i2.1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lei JH, Guo YJ, Chen Z, et al. Problem/case-based learning with competition introduced in severe infection education: an exploratory study. Springerplus. 2016;5:1821. doi: 10.1186/s40064-016-3532-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Li Y, Liu Y, Zeng L, et al. Knowledge and practice of hand hygiene among hospitalised patients in a tertiary general hospital in China and their attitudes: a cross-sectional survey. BMJ Open. 2019;9:e027736. doi: 10.1136/bmjopen-2018-027736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Corell A, Regueras LM, Verdu E, et al. Effects of competitive learning tools on medical students: a case study. PLoS One. 2018; 13:e0194096. doi: 10.1371/journal.pone.0194096. [DOI] [PMC free article] [PubMed] [Google Scholar]