Abstract
Actively engaging people with lived experience (PWLE) in stroke-related clinical practice guideline development has not been effectively implemented. This pilot project evaluated the feasibility, perceived value, and effectiveness of the Community Consultation and Review Panel (CCRP), a new model to engage PWLE in the writing and review of Canadian Stroke Best Practice Recommendations. Responses to a standardized evaluation tool indicated that participants perceived the CCRP as valued, impactful, effective, and beneficial to stroke care. This project successfully demonstrated that values, experiences, and recommendations of PWLE can be effectively incorporated into guideline content and is applicable to all guideline development processes.
Keywords: stroke, patient engagement, clinical practice guidelines, person-centered care, people with lived experience, rehabilitation, transitions of care, perceptions of care
Introduction
Over the past decade, there has been a concerted international effort to prioritize patient, family member, and informal caregiver engagement at all stages of health-care planning and delivery (1,2). A person-centered approach extends beyond the person experiencing the medical event or condition to include the perspectives and contributions of individuals, caregivers, families, and communities (3). A fundamental aim of person-centered care is the active participation of people with lived experience (PWLE) in the development of clinical practice guidelines (4,5) and the research they are based on. This objective recognizes the value of the unique insights, experiential knowledge, and needs of PWLE with respect to their health condition and its treatment, personal goals and priorities, as well as their ground-level experience navigating the health-care system.
The most recent quality standards for guideline development strongly advocate for public and patient engagement in writing and review (6,7) as there is evidence to suggest that engagement is feasible and generally perceived as a positive experience for the participants involved (8,9). However, determining the best method for this engagement continues to be an avid avenue of study (4,10,11) as criticism has been directed at some approaches deemed too tokenistic (12,13) and lack reliable evaluations.
We developed an inclusive and integrated model of engagement of PWLE for guideline development, named the Community Consultation and Review Panel (CCRP). The aim of this pilot project was to evaluate the feasibility, acceptability, perceived value, and effectiveness of this new engagement model in the update of the 2 components of the Canadian Stroke Best Practice Recommendations (CSBPR) Rehabilitation, Recovery and Community Participation module (14,15).
Method
This pilot study of the feasibility, acceptability, perceived value, and effectiveness of the CCRP model was a nonrandomized mixed methods design, with purposeful recruitment of members. This study adhered to the Standards for Reporting Implementation Studies (Supplementary File 1). The CCRP model was conceived in consultation with several PWLE and was built as a reciprocal and collaborative knowledge sharing process between the CSBPR scientific writing group and a CCRP of PWLE. A review of the literature was conducted to identify and assess other models of engagement in guideline development. People with lived experience helped refine the model throughout the methodology development, implementation of the process, and evaluation. Table 1 describes the critical path and key implementation elements of each phase of the CCRP model with a detailed methodology for replication provided in Supplementary File 2.
Table 1.
Critical Path for a Community Consultation and Review Panel (CCRP).a
| Phase | Goal | Key Elements and Activities |
|---|---|---|

Phase 1 |
Member selection and onboarding |
|

Phase 2 |
Orientation |
|

Phase 3 |
Guideline content review and feedback meetings |
|

Phase 4 |
Integration of information into final documents, review by group |
|

Phase 5 |
Knowledge translation and resource development |
|
Phase 6 |
Evaluation |
|
Abbreviation: CCRP, Community Consultation and Review Panel.
a Detailed methodology for replication of the Heart and Stroke CCRP model in Supplementary File 2.
Results
Participants
The first CCRP (Rehabilitation and Recovery following Stroke) was composed of 5 females (mean age: 41.8 years) and 4 males (mean age: 57.3 years), including among them 7 patients and 2 caregivers from 7 Canadian provinces. A total of 6 teleconferences were held with the group. The second CCRP (Transitions and Community Participation following Stroke) was composed of 5 females (mean age: 41.8 years) and 3 males (mean age: 52.5 years), representing 6 patients and 2 caregivers from 7 provinces. A total of 3 teleconferences were held with this group as there was less content.
The Heart and Stroke Foundation of Canada staff reported spending an average of 3 to 4 hours per week throughout the pilot study for participant recruitment and management, agenda and content preparation, and meeting facilitation. Staff also spent time on notetaking, feedback gathering, and synthesis of materials. The scientific writing group liaison reported spending on average 1 hour per week in preparation and participation on CCRP phone calls. They reported high satisfaction and active engagement with the process.
Evaluation of CCRP Model
At the midway point of the first CCRP, 7 of 9 participants (78%) completed the online survey. They all strongly agreed or agreed on most elements of the evaluation tool. One person rated disagree on having enough information to contribute to the discussion, attributed to the relevance to their experience (eg, they did not receive certain rehabilitation therapies and therefore could not comment on them).
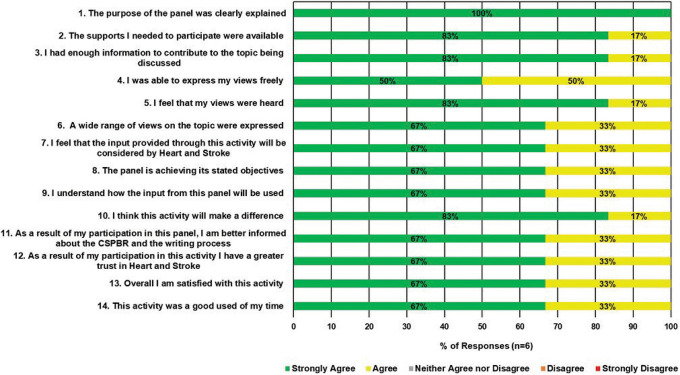
Six of the 7 individual participants who were on both panels responded to the final evaluation of the CCRP model (75% response rate); one individual member and the husband–wife pair were unable to complete the evaluation (n = 3). Figure 1 summarizes the responses of CCRP members to the 14 Likert scale questions from the final evaluation of the CCRP model. All participants who completed the evaluation, agreed or strongly agreed that they were satisfied, felt their participation would make a difference and that the panel achieved its objective. The majority of respondents (n = 5, 83%) strongly agreed that their views were heard, and all of the respondents strongly agreed (n = 3, 50%) or agreed (n = 3, 50%) that they were able to express their views freely.
Figure 1.
Evaluation of the CCRP model. Responses to the Likert scale questionnaire administered to Community Consultation and Review Panel (CCRP) members during the final evaluation of the model.
Subjective feedback was positive, with CCRP members highlighting the value of meeting other PWLE, being able to share their stories in a safe environment and having their experiences benefit others with stroke. Expressed concerns were related to technical quality of the conference calls and the webinar program on their own computer systems, and one member where English was their second language. Inputs from the CCRP were integrated throughout the relevant CSBPR modules, particularly in the Rationale, System Implications, and Performance Measures sections. Supplementary File 3 provides all responses by CCRP members to the open-ended questions from the final evaluation time point (n = 6).
The scientific writing group liaisons and program staff reported that CCRP input was included in as many stages of the process of guideline revision as possible. They rated strongly agree to questions regarding their interest in further training on public and patient engagement; and agreed that as a result of the experience they would be more comfortable in leading public and patient engagement activities in the future, and that the process was a good use of program resources and enhanced decision-making.
Discussion
Engaging PWLE in clinical practice guideline development in a systematic, meaningful, and measurable way has not been previously reported. This pilot project successfully implemented a new engagement model and demonstrated that the values, experiences, and recommendations of PWLE can be effectively incorporated into guideline content and is applicable to all guideline development beyond the scope of stroke.
The goal of the CCRP model was to facilitate development of specific practice recommendations that are grounded in real-life experience and the unique needs of people with stroke while maintaining scientific rigour, and applicability to those directly impacted by the recommendations—people who have had a stroke, their families and caregivers, as well as the health-care professionals caring for them. The model provided members with opportunities to regularly review and offer feedback on draft recommendations from the scientific writing group, provide context related to their values and preferences in stroke care to help inform what person-centered care meant in the context of their lived experiences. This is a significant advancement from previous models where engagement of PWLE as members of the writing groups was minimal and they were often disengaged, and stated that they felt they had little to contribute during the discussions about the available evidence, it was difficult to speak up during conference calls, and they sometimes felt dismissed by other writing group members when they did comment.
Participation in the CCRP process was perceived as a positive and impactful experience and enabled PWLE to also act as knowledge translation ambassadors through the codevelopment of lay language resources and education tools for PWLE and caregivers. Respondents felt that their feelings and experiences were acknowledged, and they enjoyed the opportunity to connect and hear the experiences of other PWLE to develop stroke recovery strategies and recommendations. The writing group liaison stated it was very meaningful and a privilege to work closely with PWLE and understand the impact of the recommendations from their vantage point. Incorporating feedback from the CCRP helped to highlight areas within the guidelines that were considered to be of high importance and value by PWLE, family members, and caregivers. Health professionals who use these guidelines can utilize this feedback to provide a person-and-family centered approach.
This was a pilot study and the sample size was small. We have now engaged 2 additional CCRP groups in updates of the secondary prevention and acute stroke modules and engagement and feedback has been positive, reinforcing this is an effective model. The CCRP model has been approved for all new and updated modules as part of the Seventh Edition of the CSBPR. We will continue to refine implementation and evaluation of this model.
Conclusions
The overall success of this pilot project established the feasibility and perceived benefit of employing a participatory and collaborative model, the CCRP, to actively engage PWLE in clinical practice guideline development, including all stages from writing to review and dissemination/knowledge translation. The results indicate that the CCRP increases PWLE engagement and provides guideline users with valuable evidence-based recommendations supported by personal experiences, insights, and feedback. This model is pertinent and valuable for all guideline development across disciplines.
Supplemental Material
Supplemental Material, Supplementary_File_1_JPX-20-0037 for People With Lived Experience at the Centre of Canadian Stroke Best Practice Recommendations: A Model for Guideline Developers by M Patrice Lindsay, Natalie Gierman, Jocelyn E Harris, Gavin Arthur, Moira E Teed, Anita Mountain, Gordon Gubitz, Eric E Smith, Dar Dowlatshahi, Andrea de Jong and Leigh C P Botly in Journal of Patient Experience
Supplemental Material, Supplementary_File_2_JPX-20-0037 for People With Lived Experience at the Centre of Canadian Stroke Best Practice Recommendations: A Model for Guideline Developers by M Patrice Lindsay, Natalie Gierman, Jocelyn E Harris, Gavin Arthur, Moira E Teed, Anita Mountain, Gordon Gubitz, Eric E Smith, Dar Dowlatshahi, Andrea de Jong and Leigh C P Botly in Journal of Patient Experience
Supplemental Material, Supplementary_File_3_JPX-20-0037 for People With Lived Experience at the Centre of Canadian Stroke Best Practice Recommendations: A Model for Guideline Developers by M Patrice Lindsay, Natalie Gierman, Jocelyn E Harris, Gavin Arthur, Moira E Teed, Anita Mountain, Gordon Gubitz, Eric E Smith, Dar Dowlatshahi, Andrea de Jong and Leigh C P Botly in Journal of Patient Experience
Acknowledgments
The Heart and Stroke Foundation of Canada (HSFC) is especially grateful to the members of the Community Consultation and Review Panel who reviewed all sections of the modules, shared their personal experiences and insights on what did or would have made their journey optimal. The members of both the Rehabilitation and Recovery following Stroke and Transitions and Community Participation following Stroke CCRPs included: Steven Archer, Rob Claydon (cofacilitated Transitions and Community Participation CCRP), Debbie Chow, Daniel Franco, Amanda Horner, Bruce Hughes, Edith Lambert, Cathy Livingstone, David Livingstone, and Michelle McGroty. The HSFC gratefully acknowledges the members of the CSBPR scientific writing groups for Rehabilitation and Recovery following Stroke and the Transitions and Community Participation following Stroke all of whom have volunteered their time and expertise to the update of these recommendations and participate in the development of the CCRP model and integration of the CCRP feedback into the final module content. We thank the Canadian Stroke Best Practices and Quality Advisory Committee members for their support and input throughout the development and pilot testing of the CCRP model and Anne Simard of the Heart and Stroke Foundation for her leadership during the development of this model. Anne Simard provided leadership during the development and implementtaion of the CCRP model and provided early input into this manuscript.
Author Biographies
M Patrice Lindsay is the Director of Health Systems Change at the Heart and Stroke Foundation and leads the development of the of the Canadian Stroke Best Practice guidelines and conceived the CCRP model and was colead on the development of this manuscript.
Natalie Gierman is the Senior Manager of Systems Change at the Heart and Stroke Foundation in Ontario, and co-conceived the CCRP model.
Jocelyn E Harris is is an Associate Professor in the School of Rehabilitation Science and teaches in the MSc (OT) program. She was a member of the CSBPR Rehabilitation scientific writing group and the liaison to the CCRP.
Gavin Arthus was the lead for patient engagement at the Heart and Stroke Foundation at the time of this research.
Moira E Teed is a social worker, and was the liaison for people with lived experience at the Heart and Stroke Foundation at the time of this research.
Anita Mountain is an Assistant professor. Division of Physical Medicine & Rehabilitation, Department of Medicine, chair of the Transitions of Care scientific writing group and co-chair of the CSBPR Advisory Committee She was an active participant in the development and implementation of the CCRP methodology and pilot study.
Gordon Gubitz is a stroke neurologist and senior advisor for the CSBPR Advisory Committee and active participant in the development and implementation of the CCRP methodology and pilot study.
Eric E Smith is a stroke neurologist and co-chair of the CSBPR Advisory Committee and an active participant in the development and implementation of the CCRP methodology and pilot study.
Dar Dowlatshahi is a stroke neurologist and senior advisor for the CSBPR Advisory Committee and active participant in the development and implementation of the CCRP methodology and pilot study.
Andrea de Jong is a nurse educator and participated in the review of this manuscript.
Leigh C P Botly is a scientific writer with the Heart and Stroek Foundation and was colead on the development of this manuscript.
Footnotes
Authors’ Note: Ethics approval was not required for this pilot study. All CCRP participants provided written consent to participate and completed a conflict of interest and confidentiality declaration prior to participation. All members of the CSBPR scientific writing group completed declarations of conflict of interest and confidentiality at the outset of the process.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The development of the CSBPR, including the CCRP model was funded in its entirety by the Heart and Stroke Foundation of Canada.
ORCID iD: M Patrice Lindsay, RN, PhD  https://orcid.org/0000-0002-2584-8580
https://orcid.org/0000-0002-2584-8580
Leigh C P Botly, PhD  https://orcid.org/0000-0002-5979-3899
https://orcid.org/0000-0002-5979-3899
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Ocloo J, Matthews R. From tokenism to empowerment: progressing patient and public involvement in healthcare improvement. BMJ Qual Saf. 2016;25:626–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Brett J, Staniszewska S, Mockford C, Herron-Marx S, Hughes J, Tysall C, et al. Mapping the impact of patient and public involvement on health and social care research: a systematic review. Health Expect. 2014;17:637–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization. WHO | Health Systems Strengthening Glossary [Internet]. WHO; 2019, https://www.who.int/healthsystems/hss_glossary/en/index8.html#2 [Google Scholar]
- 4. Armstrong MJ, Rueda JD, Gronseth GS, Mullins CD. Framework for enhancing clinical practice guidelines through continuous patient engagement. Health Expect. 2017;20:3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Loudon K, Santesso N, Callaghan M, Thornton J, Harbour J, Graham K, et al. Patient and public attitudes to and awareness of clinical practice guidelines: a systematic review with thematic and narrative syntheses. BMC Health Serv Res. 2014;14:321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, et al. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010;182:E839–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. G-I-N PUBLIC Toolkit: patient and public involvement in guidelines—guidelines international network [Internet]. 2012. https://www.g-i-n.net/working-groups/gin-public/toolkit
- 8. Harding E, Brown D, Hayward M, Pettinari CJ. Service user perceptions of involvement in developing NICE mental health guidelines: a grounded theory study. J Ment Health. 2010;19:249–257. [DOI] [PubMed] [Google Scholar]
- 9. Serrano-Aguilar P, Trujillo-Martin M del M, Pérez de la Rosa A, Cuellar-Pompa L, Saavedra-Medina H, Linertova R, et al. Patient participation in a clinical guideline development for systemic lupus erythematosus. Patient Educ Couns. 2015;98:1156–1163. [DOI] [PubMed] [Google Scholar]
- 10. Armstrong MJ, Mullins CD, Gronseth GS, Gagliardi AR. Recommendations for patient engagement in guideline development panels: a qualitative focus group study of guideline-naïve patients. PLoS One. 2017;12:e0174329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Díaz Del Campo P, Gracia J, Blasco JA, Andradas E. A strategy for patient involvement in clinical practice guidelines: methodological approaches. BMJ Qual Saf. 2011;20:779–84. [DOI] [PubMed] [Google Scholar]
- 12. van Wersch A, Eccles M. Involvement of consumers in the development of evidence based clinical guidelines: practical experiences from the North of England evidence based guideline development programme. Qual Health Care. 2001;10:10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hahn DL, Hoffmann AE, Felzien M, LeMaster JW, Xu J, Fagnan LJ. Tokenism in patient engagement. Fam Pract. 2017;34:290–295. [DOI] [PubMed] [Google Scholar]
- 14. Teasell R, Salbach NM, Foley N, Mountain A, Cameron JI, Jong A de, et al. Canadian stroke best practice recommendations: rehabilitation, recovery, and community participation following stroke. Part one: rehabilitation and recovery following stroke, 6th edition. Int J Stroke. Epub ahead of print 27 January 2020 doi: 10.1177/1747493019897843. [DOI] [PubMed] [Google Scholar]
- 15. Mountain A, Patrice Lindsay M, Teasell R, Salbach NM, de Jong A, Foley N, et al. Canadian stroke best practice recommendations: rehabilitation, recovery, and community participation following stroke. Part two: transitions and community participation following stroke. Int J Stroke. Epub ahead of print 27 January 2020 doi: 10.1177/1747493019897847. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, Supplementary_File_1_JPX-20-0037 for People With Lived Experience at the Centre of Canadian Stroke Best Practice Recommendations: A Model for Guideline Developers by M Patrice Lindsay, Natalie Gierman, Jocelyn E Harris, Gavin Arthur, Moira E Teed, Anita Mountain, Gordon Gubitz, Eric E Smith, Dar Dowlatshahi, Andrea de Jong and Leigh C P Botly in Journal of Patient Experience
Supplemental Material, Supplementary_File_2_JPX-20-0037 for People With Lived Experience at the Centre of Canadian Stroke Best Practice Recommendations: A Model for Guideline Developers by M Patrice Lindsay, Natalie Gierman, Jocelyn E Harris, Gavin Arthur, Moira E Teed, Anita Mountain, Gordon Gubitz, Eric E Smith, Dar Dowlatshahi, Andrea de Jong and Leigh C P Botly in Journal of Patient Experience
Supplemental Material, Supplementary_File_3_JPX-20-0037 for People With Lived Experience at the Centre of Canadian Stroke Best Practice Recommendations: A Model for Guideline Developers by M Patrice Lindsay, Natalie Gierman, Jocelyn E Harris, Gavin Arthur, Moira E Teed, Anita Mountain, Gordon Gubitz, Eric E Smith, Dar Dowlatshahi, Andrea de Jong and Leigh C P Botly in Journal of Patient Experience