Abstract
Phone calls to patients after discharge from the emergency department (ED) serve as reminders to schedule medical follow-up, support adherence to discharge instructions, and reduce revisits to already-crowded EDs. An existing, nurse-administered, call-back program contacted randomly selected ED patients 24 to 48 hours following discharge. This program did not improve patient follow-up (48.68%) nor reduce the ED revisit rate (6.7% baseline vs 6.0% postimplementation). Plan-Do-Study-Act methodology tested a modification to the existing program consisting of a second, scripted phone call from a trained volunteer at 72 to 96 hours postdischarge. Volunteers utilized a patient list and script, and nurses provided expertise to eliminate identified barriers to follow-up. Follow-up rate and ED revisit were monitored through the electronic medical record. A total of 894 patients participated between October 2017 and June 2018. Follow-up increased from 48.68% to 65.5% (P < .0001) and ED revisit decreased significantly (4.5% vs 8.6%, P < .001). This innovative nurse-led, systematic postdischarge call-back program utilizing hospital volunteers increased patient compliance with post-ED medical follow-up while significantly reducing the rate of patient revisit to the ED within 7 days of discharge.
Keywords: clinician–patient relationship, nursing, patient engagement, patient feedback, quality improvement, transitions of care, communication
Introduction
Utilization of emergency department (ED) services in the United States has sharply increased to a rate faster than that of population growth; at the same time, the total number of EDs in the United States has decreased 3.4% (1,2). This decrease has led to higher patient volumes across EDs, with greater than 90% routinely reporting crowded conditions, impacting capacity to provide quality care (2). In addition to a degraded patient experience, the consequences of ED crowding include poorer patient outcomes; increased medical errors; compromises in patient physical privacy, confidentiality, and communication; and provider moral distress (2). Supporting appropriate ED utilization by reducing preventable revisits is one strategy to alleviate crowding that enhances patient outcomes and improves the overall patient experience.
A revisit to the ED occurs when a patient returns one or more times for emergency care that is clinically related to an index ED visit and within a specified time interval. Approximately 8% of patients have preventable revisits within 3 days of discharge from the ED, although the relative risk of revisit varies widely by state (3). Revisits are potential quality indicators because they may reflect suboptimal clinical care and/or poor coordination of medical services in the immediate postdischarge period. Additionally, revisits contribute to ED operational threats, including overcrowding/capacity challenges, increased costs, and erratic patient flow which may further affect operations throughout the entire hospital (4 -6). Major contributing factors of ED revisit include the patient not knowing whom to contact for follow-up care as well as failure to contact the provider, which frequently leads to fragmented care (4,7,8 -10). When medical issues persist, patients who did not follow-up with their primary or specialty care provider may return to the ED for further assessment and treatment of the same problem.
Problem Overview
Recent evidence from the literature indicates that discharge phone calls can help remind patients to schedule recommended medical follow-up and support compliance with discharge instructions (8,10,11). These interventions are clinically important because increasing patient engagement and commitment to follow-up with medical providers after discharge may also decrease revisits to already crowded EDs (8,10).
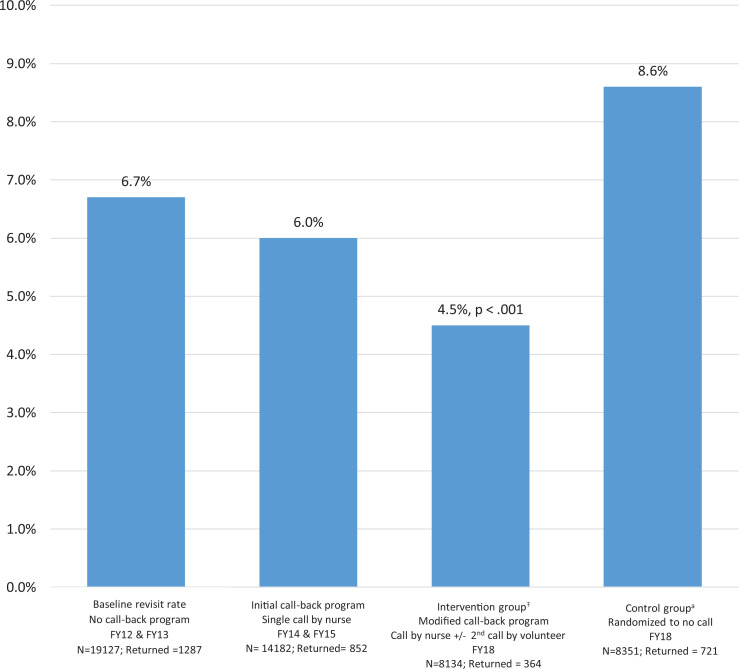
In 2014, we therefore initiated a nurse-administered, patient call-back program that made phone calls to a randomly selected (equal allocation to phone call vs no phone call) roster of ED patients within 24 to 48 hours following their discharge to remind them to follow-up with their primary or specialty care providers (12). In contrast with the literature, the relevant problem was that the call-back program was NOT able to significantly reduce ED revisit rates (6.7% baseline vs 6.0% postimplementation; Figure 1). In fact, analysis of free-text, patient-reported suggestions for improvement recorded by our nurses noted persistent concerns regarding inability to complete the post-ED follow-up, among others (13).
Figure 1.
Patient revisit rate to ED* within 7 days of index visit. *Two noncritical, lower-acuity care areas only. ŦIntervention group, PDSA cycles 1 to 3; all patients received at least the baseline, standard call from a nurse at 24 to 48 hours after discharge; eligible patients (n = 894) additionally received a second call at 72 to 96 hours from a hospital volunteer. aThese patients, originating from the same lower-acuity care areas and during the same time frame as the intervention group, did not receive any discharge phone calls. FY indicates fiscal year; ED, emergency department; PDSA, Plan-Do-Study-Act.
Aggregate root cause analysis using a structured team process (14) that included nurses, administrators, patient volunteers, and a physician evaluated trends that led to “patient inability to complete follow-up.” Six contributing factors emerged from these focus groups: knowledge, access, ED discharge procedure, ED process, available resources, and the call-back program itself, specifically:
Knowledge gaps included language barriers, literacy issues, and decreased comprehension due to long waits and eagerness to leave the ED.
Access issues constituted lack of primary care provider, phone, or transportation and inability to reach providers or obtain a timely appointment.
The ED discharge procedure was identified as inconsistent among providers, with high risk for patient noncompliance due to the length/complexity of printed postdischarge instructions and the potential for lost paperwork.
Problems with the structural ED process included failed handoffs, lost electronic referrals, and patients leaving the ED prematurely, before beginning or completing medical evaluation.
Issues identified regarding available resources included provider unfamiliarity with referral options as well as the inability to consult with treating physicians during off-hours.
Challenges with the existing call-back program included a large volume of calls, inadequate staff, small proportion of patients reached, and lack of standardized operating procedures when patients reported difficulty scheduling follow-up care.
Nurses identified “challenges with the existing call-back program” as the most actionable theme to increase patient ability to follow-up with their provider while potentially reducing the ED revisit rate, since it was most consistent with the prior literature in this area (8,10,11), was already operational, fit into the current work flow, was low cost, and potentially had high yield..
Objectives
We therefore modified the existing telephone call-back program in 2017 to include a second, scripted phone call from hospital volunteers at 72 to 96 hours postdischarge and tested its effect on patient follow-up and revisit rates. Our specific aims were to (1) increase the percentage of ED patients who completed recommended follow-up with their medical provider within 7 days of discharge and (2) to decrease the 7-day revisit rate in 2 lower-acuity areas of the ED. This project was undertaken as a quality improvement (QI) initiative and as such was not formally supervised by the Institutional Review Board per their policies.
Methods
Design
Plan-Do-Study-Act (PDSA) methodology utilizing chart review for outcome measures evaluated small tests of change. Plan-Do-Study-Act begins with a plan for the improvement intervention (Plan); a protocol for implementing the improvement intervention with data collection (Do); real-time analysis and interpretation of results (Study); and determination of whether to keep, modify, or reject the intervention (Act). The structured PDSA approach is iterative, whereby data from the initial cycle inform cycles that follow, allowing for testing and modification under realistic conditions.
Improvement Plan
The improvement intervention to the existing patient call-back program consisted of a second, simple, scripted phone call from a trained volunteer at 72 to 96 hours postdischarge, in addition to the initial call by the nurse at 24 to 48 hours postdischarge (the baseline standard). Utilization of unlicensed volunteers was ethically evaluated and carefully vetted before final approval by hospital leadership. All volunteers completed intensive Health Insurance Portability and Accountability Act privacy and security training, and the script of the call was carefully worded to avoid misrepresentation of the volunteer as a licensed clinician:
Hello this is (name). I am a volunteer from the hospital, and we are calling you after your recent discharge from the ED. We are calling to remind you to follow up with your provider. We care about you and want to make sure you receive the best possible care which includes following up with your provider. We do not give any medical advice. Have you contacted your provider?
Two types of experienced hospital volunteers were utilized, categorized internally as “health leads” and “hospital-wide.” Health leads are volunteers who work with 4 specific practice groups (comprised of over 150 providers) at our institution. Health leads have specific training to address factors associated with health disparities, such as transportation issues, difficulty with medication obtainment and purchase, and housing instability. Hospital-wide are a more traditional group of volunteers, receiving a basic orientation to the hospital environment and serving broadly throughout the institution to greet patients, deliver food and books, read to children, and manage play rooms, among other activities. The call-back team initially worked with the health leads because it was a smaller group to train and had higher-level expertise in working with marginalized patients. As the improvement process evolved, hospital-wide volunteers were added to maximally expand the number of postdischarge phone calls.
Volunteers received a daily roster of patients who had already been contacted by a nurse 24 to 48 hours following their discharge from the ED. Volunteers completed the simpler, second reminder phone call at 72 to 96 hours postdischarge, while sitting side-by-side a nurse to allow for real-time triage of obstacles or patient-identified clinical concerns. If patients reported failure to contact providers or barriers obtaining an appointment, the nurse would intervene by contacting the provider’s office, securing the appointment, and troubleshooting logistical issues (eg, transportation, financial, or social service referrals). Anecdotal patient comments about the experience of being called by a volunteer were manually recorded as a direct quote.
Setting and Sample
The modified call-back program was implemented in 2 noncritical, low-acuity care areas of the ED at an urban, tertiary-care, 1000+ bed, teaching hospital. Typical chief complaints evaluated within these areas include chest pain, shortness of breath, abdominal pain, headaches, fractures, injuries from minor motor vehicle crashes, lacerations, and cellulitis. These ED sections were chosen to trial the intervention because they have high patient high volume, representing 52% (57 183) of a total 110 567 annual patient visits to the entire ED, with most patients discharged to home without hospital admission.
Patients eligible to receive the second, volunteer-apportioned, postdischarge telephone call were discharged home, ≥20 years old, and had a hospital-affiliated primary or specialty care provider to enable outcome extrapolation from the common electronic medical record (EMR). Patients who were not eligible still received the baseline standard of a single call by the nurse at 24 to 48 hours postdischarge. Non-English/limited-English speakers were included, using a 3-way calling system with a hospital-approved medical translator. The intervention period was October 7, 2017, to June 9, 2018.
Measurement and Analysis
The outcome measures were (1) percentage of patients with EMR documentation of either (a) communication (email, telephone, or scheduled appointment) with their provider, or (b) a completed visit with their provider within 7 days of discharge from the ED; and (2) the percentage of patients who received at least the baseline standard call and revisited the ED within 7 days of their index visit. Weekly data audits of the enterprise-wide EMR were used to track outcome measures. Data were captured and analyzed using Microsoft Excel (2013). Data mining was limited to clinically licensed nursing staff; hospital volunteers did not access the EMR.
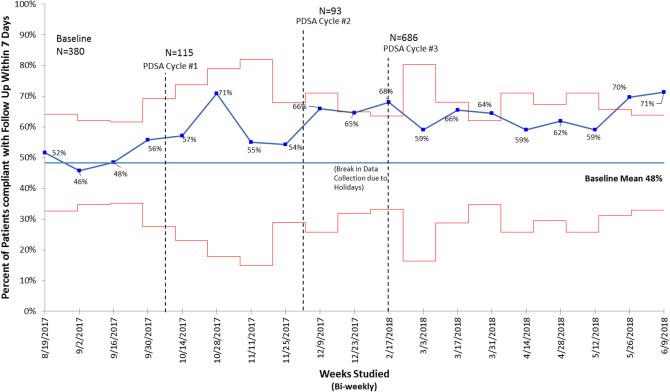
Using the process described by Benneyan et al, a statistical quality control p chart (Figure 2) was utilized to rigorously track the outcome measures in biweekly epochs to efficiently gauge results and make appropriate modifications to subsequent PDSA cycles (15). The advantage of this approach is that it distinguishes between natural variation in outcomes and significant “special cause” variation in order to inform next steps; that is, whether to maintain, adapt, or completely redesign the improvement intervention. Because sample size varied at each data collection time point (due to the overall number of patients discharged to home or number of discharge phone calls completed), the control limits had to be recalculated based on the available sample size. These variable-width control limits, where each observation plots against its own control limits, can be seen in Figure 2 (16). The control chart is displayed with 3 sigma limits and special cause interpretation with standard health care rules. Given 8 data points above the mean positive change was interpreted as significant (15). Postintervention follow-up rates were compared to the baseline rate using Chi-square analysis. A P value < .05 was considered statistically significant.
Figure 2.
Statistical quality control p chart* showing biweekly percentage of patient compliance with post ED discharge follow-up. *Red lines represent the upper and lower control limits within 3-standard deviations of the mean (3-sigma limits); these vary in response to the sample size, with statistically significant data points above the red line. Baseline data: Initial call-back program; single call by nurse at 24 to 48 hours following discharge. PDSA cycle #1: Call by nurse at 24 to 48 hours following discharge with second call at 72 to 96 hours following discharge utilizing “health leads” volunteers; limited to patients established within 4 hospital-based, primary and specialty practice groups. PDSA cycle #2: Call by nurse at 24 to 48 hours following discharge with second call at 72 to 96 hours following discharge utilizing “health leads” and “hospital-wide” volunteers; expanded to also include all hospital-based community clinic patients. PDSA cycle #3: Call by nurse at 24 to 48 hours following discharge with second call at 72 to 96 hours following discharge utilizing hospital-wide volunteers only; full expansion of program to include patients of all enterprise-based providers. ED indicates emergency department; PDSA, Plan-Do-Study-Act.
Results
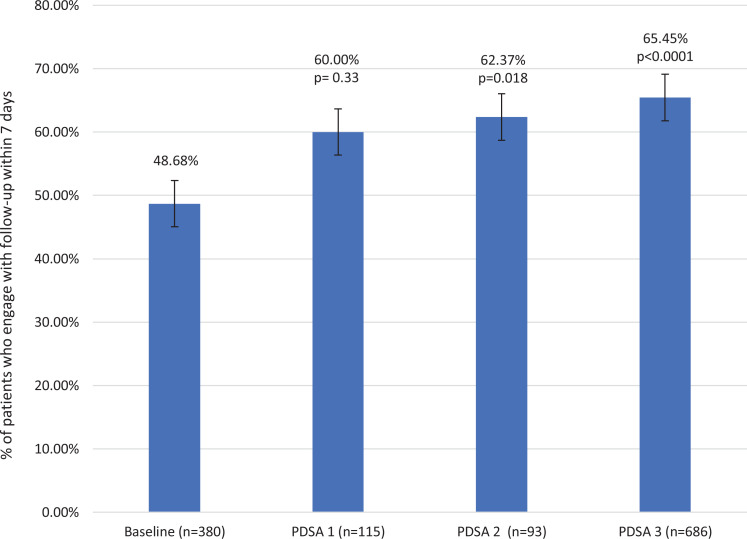
The baseline follow-up rate established during a 1-month observational period utilizing the existing call-back program was 48.6% (Figure 3); these patients (n = 380) are described in Table 1. The intervention sample included 894 patients (PDSA cycles 1-3; Table 1) who received both the standard, initial call from a nurse at 24 to 48 hours discharge and the secondary, volunteer-apportioned call at 72 to 96 hours postdischarge. Plan-Do-Study-Act cycle 1, utilizing “health leads” only and confined to patients within 4 hospital-based practice groups, quickly improved the follow-up rate to 60% (P = .333; Figure 3). Cycle 2 increased the number of volunteers to include hospital-wide” in addition to “health leads” and significantly expanded the number of eligible patients to include all hospital-based community clinic patients, achieving further gains in patient follow-up at 62.4% (P = .018; Figure 3). In cycle 3, hospital-wide volunteers were exclusively utilized to assess whether the effect on follow-up could be maintained with this more conventional type of volunteers while maximally expanding the modified call-back program to include patients of all hospital-affiliated providers, achieving a 65.5% follow-up rate (P < .0001; Figure 3). In addition, we achieved a significant reduction in the rate of patient revisit to the ED within 7 days of an index visit. Patients who received at least the baseline standard phone call had significantly lower ED revisit rates than patients who received no phone call (4.5% vs 8.6%, P < .001; Figure 1).
Figure 3.
Percentage of patients completing post-ED follow-up care, by PDSA cycle. Error bars indicate standard error. Baseline data: Initial call-back program; single call by nurse at 24 to 48 hours following discharge. PDSA cycle #1: Call by nurse at 24 to 48 hours following discharge with second call at 72 to 96 hours following discharge utilizing “health leads” volunteers; limited to patients established within 4 hospital-based, primary and specialty practice groups. PDSA cycle #2: Call by nurse at 24 to 48 hours following discharge with second call at 72 to 96 hours following discharge utilizing “health leads” and “hospital-wide” volunteers; expanded to also include all hospital-based community clinic patients. PDSA cycle #3: Call by nurse at 24 to 48 hours following discharge with second call at 72 to 96 hours following discharge utilizing hospital-wide volunteers only; full expansion of program to include patients of all enterprise-based providers. ED indicates emergency department; PDSA, Plan-Do-Study-Act.
Table 1.
Demographic Profile of ED Patients.
| Existing call-back program observational period N = 380 |
Modified call-back program PDSA cycle 1, 2, 3a N = 879b |
|
|---|---|---|
| N (%) | N (%) | |
| Mean age, years (range) | 54 (20-95) | 54 (19-101) |
| Female sex | 216 (57) | 536 (61) |
| Race | ||
| White | 279 (73) | 618 (70) |
| Black | 37 (10) | 92 (10) |
| Other | 64 (17) | 169 (20) |
| Ethnicity | ||
| Hispanic | 40 (11) | 118 (13) |
| Primary language | ||
| English | 360 (95) | 807 (92) |
| Spanish | 7 (2) | 43 (5) |
| Othera | 13 (3) | 29 (3) |
| Insurance | ||
| Medicaid | 29 (8) | 125 (14) |
| Medicare only | 155 (41) | 263 (30) |
| Private insurance | 196 (51) | 491 (56) |
| Education | ||
| Eighth grade or less | 13 (3) | 28 (3) |
| High school, some high school, GED, vocational/technical, other | 151 (40) | 352 (40) |
| College or some college | 148 (39) | 324 (37) |
| Graduate school and above | 60 (16) | 152 (17) |
| Missing data | 8 (2) | 23 (3) |
Abbreviations: ED, emergency department; GED, general equivalency diploma; PDSA, Plan-Do-Study-Act.
a In order of highest-lowest frequency: Haitian-Creole, Arabic, Italian, Portuguese, Khmer, Portuguese-Creole, Chinese-Mandarin, French, Somali.
b Data missing for 15 patients.
Discussion
With the initial call-back program, less than half of patients (48.68% ± 2.56%, n = 380) initiated or completed ED-recommended follow-up within 7 days of discharge (Figure 3). Plan-Do-Study-Act cycle 1 served as a proof-of-principle test to verify that patient follow-up rates could be increased with a second reminder call by highly trained volunteers and extralogistical support from nurses. In 2 subsequent PDSA cycles that tested incremental expansion across provider clinics while also phasing out the higher-level expertise of the “health leads,” statistically significant increase in follow-up was achieved (65% vs 48%, P < .0001; Figure 3). For patients who received at least the baseline standard phone call, this translated into a clinically significant and operationally relevant reduction in patient revisit to the ED (4.5% vs 8.6%, P < .001; Figure 1).
It was important that this improvement intervention was nurse-led, but volunteer apportioned, to enable broader capture of patients. Many patients simply required a second “nudge” to initiate their recommended follow-up, and the call from the volunteer was effective for this purpose. Reserving nursing expertise to help patients who reported difficulty securing follow-up allowed for the synchronous completion of many more calls by the volunteer. An all-nurse call back team would have been exceedingly costly and limited in call capacity. Volunteers were committed, enthusiastic, and largely enjoyed working collaboratively with the nurses. Nurses were able to provide volunteers with supportive coaching, guidance, and mentorship. Collaboration became a substantial part of the process with communication extending to providers, social workers, patient navigators, and case management. Additional resources that were helpful included use of a 3-way calling system for interpreter services and a predetermined script for the volunteer calls.
Attentive consideration of local context, culture, and resources additionally supported the success and sustainability of the program. Importantly, the need for this improvement project was identified through thematic content analyses of patient recommendations for improved experience in the ED (13); this data driven approach to identifying and prioritizing performance improvement initiatives ensured that the project would resonate with patients and staff. The use of a rigorous methodology that included root cause analysis facilitated development of an intervention that fit into the current workflow was low cost and patient-centric. Leveraging fully screened and HIPAA-trained volunteers allowed the call-back program to be highly sustainable and economically feasible. While there were some concerns initially about volunteers making the calls to patients, no safety or privacy issues were identified, and patients reported no adverse effects from receiving a call from a volunteer.
Both patient and volunteer comments were consistently positive. Examples of patient comments recorded by volunteers were “You must really care about me,” and “This is such a nice service provided by the ED.” Noted in the EMR were patient comments to the follow-up provider that demonstrated personal accountability and understanding of the importance of follow-up (eg, “I was told to follow-up within seven days” and “I was told it was important to see you after my ED visit”). Based on these successes, the program is now a standard component of ED nursing care.
Limitations and Conclusion
Results may not translate to other EDs as the sample reflects the larger demographics of our service area which is mostly white, English-speaking, and privately insured; data on socioeconomic status while not collected are presumably higher than other areas of the United States, given the insurance status and educational level reported by our sample (Table 1). Our hospital is part of a larger health care enterprise consisting of 12 hospitals, multiple primary and specialty care practices, a managed care organization, specialty care facilities, community health centers, and other health-related entities, most sharing a common EMR that allowed for extensive tracking of follow-up care across thousands of providers. Nevertheless, patients of nonenterprise providers or those who revisited EDs within other hospital networks may not have been captured. Other EDs looking to replicate this program may be limited in outcomes measurement by lack of a common EMR. Additionally, our hospital has a roster of over 1400 regular volunteers who undergo rigorous HIPAA training with required annual reeducation; the scope and availability of dedicated, seasoned volunteers was a major factor in the success of this project and may be difficult to replicate elsewhere.
This QI project demonstrated that improvements in patient compliance with provider follow-up instructions and significant reduction in ED revisit rates can be achieved by making minor modifications to an established call-back program. While providing ED discharge calls by experienced nurses can be key to a patient’s success in connecting with primary or specialty providers, we were only able to demonstrate a statistically significant increase in follow-up compliance rates when a simple, second call by highly trained volunteers was added to our existing process, reserving nursing expertise for troubleshooting. When issues with appointment access were encountered, the nurse could provide expert assessment, knowledge, collaboration, and coordination with external resources, while the trained volunteer could continue making calls to other patients on the roster. Patients receiving the call frequently described feeling supported, cared for, and valued. This novel, nurse-led, systematic postdischarge patient call-back program utilizing hospital volunteers may be an efficient and feasible hybrid model for other EDs seeking to improve patient experience, follow-up, and reduce the number of revisits to the ED after discharge. Other barriers impacting patient follow-up, including transportation, insurance status, financial issues, and relationship with primary or specialty care providers, require further study. A cost-benefit analysis is underway.
Author Biographies
Ines Luciani-McGillivray, BSN RN CEN is a registered nurse at Massachusets General Hospital Department of Emergency Medicine.
Julie Cushing, BSN RN is a registered nurse at Massachusetts General Hospital Department of Emergency Medicine.
Rebecca Klug, MPH BSN RN is a registered nurse at Lowell General Hospital in Regulatory Compliance.
Hang Lee, PhD is an associate investigator at the Biostatistics Center, Massachusetts General Hospital and associate professor of Medicine at Harvard Medical School.
Jennifer E Cahll, PhD RN is a nurse scientist at the Yvonne L. Munn Center for Nursing Research at Massachusetts General Hospital.
Footnotes
Authors’ Note: This project was undertaken as quality improvement research and did not meet the requirements to obtain informed consent from study participants.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported in kind by the Department of Nursing at Massachusetts General Hospital with additional services for manuscript preparation provided by the Yvonne L. Munn Center for Nursing Research.
ORCID iDs: Ines Luciani-McGillivray, BSN, RN, CEN  https://orcid.org/0000-0003-2202-0849
https://orcid.org/0000-0003-2202-0849
Jennifer E Cahill, PhD, RN  https://orcid.org/0000-0003-2879-8395
https://orcid.org/0000-0003-2879-8395
References
- 1. Hooker EA, Mallow PJ, Oglesby MM. Characteristics and trends of emergency department visits in the United States (2010-2014). J Emerg Med. 2019;56:344–351. [DOI] [PubMed] [Google Scholar]
- 2. Moskop JC, Geiderman JM, Marshall KD, McGreevy J, Derse AR, Bookman K, et al. Another look at the persistent moral problem of emergency department crowding. Ann Emerg Med. 2019;74:357–364. [DOI] [PubMed] [Google Scholar]
- 3. Duseja R, Bardach NS, Lin GA, Yazdany J, Dean ML, Clay TH, et al. Revisit rates and associated costs after an emergency department encounter: a multistate analysis. Ann Intern Med. 2015;162:750–756. [DOI] [PubMed] [Google Scholar]
- 4. Crocker JB, Crocker JT, Greenwald JL. Telephone follow-up as a primary care intervention for postdischarge outcomes improvement: a systematic review. Am J Med. 2012;125:915–921. [DOI] [PubMed] [Google Scholar]
- 5. Leppin AL, Gionfriddo MR, Kessler M, Brito JP, Mair FS, Gallacher K, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174:1095–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Thompson R. Reducing Readmissions-Local and National Perspectives. In: Presented for Case Management Week, 3 October 2017, Massachusetts General Hospital. [Google Scholar]
- 7. Tang N, Fujimoto J, Karliner L. Evaluation of a primary care-based post-discharge phone call program: keeping the primary care practice at the center of post-hospitalization care transition. J Gen Intern Med. 2014;29:1513–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Biese K, LaMantia M, Shofer F, McCall B, Roberts E, Stearns S, et al. A randomized trial exploring the effect of a telephone call follow-up on care plan compliance among older adults discharged home from the emergency department. Acad Emerg Med. 2014;21:188–195. [DOI] [PubMed] [Google Scholar]
- 9. Auerbach A, Kripalani S, Vasilevskis E, Sehgal N, Lindenauer P, Metlay J, et al. Preventability and causes of readmissions in a national cohort of general medicine patients. JAMA Intern Med. 2016;176:484–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Carmel AS, Steel P, Tanouye R, Novikov A, Clark S, Sinha S, et al. Rapid primary care follow-up from the ED to reduce avoidable hospital admissions. West J Emerg Med. 2017;18:870–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Samuels-Kalow ME, Stack AM, Porter SC. Effective discharge communication in the ED. Ann Emerg Med. 2012;60:152–159. [DOI] [PubMed] [Google Scholar]
- 12. Luciani-Mcgillivray I. Emergency department post discharge phone calls lessons learned. J Emerg Nurs. 2017;43:581–583. [DOI] [PubMed] [Google Scholar]
- 13. Natsui S, Aaronson EL, Joseph TA, Goldsmith AJ, Sonis JD, Raja AS, et al. Calling on the patient’s perspective in emergency medicine: analysis of 1 year of a patient callback program. J Patient Exp. 2018;6(4)318–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Neily J, Ogrinc G, Mills P, Williams R, Stalhandske E, Bagian J, et al. Using aggregate root cause analysis to improve patient safety. Jt Comm J Qual Saf. 2003;29:434–439. [DOI] [PubMed] [Google Scholar]
- 15. Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12:458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Montgomery D. Statistical Quality Control. 6th ed John Wiley & Sons; 2009. [Google Scholar]