Abstract
This study compared TRICARE, the health care program of the United States Department of Defense Military Health System, beneficiaries in CenteringPregnancy, an enhanced prenatal care model, to women in individual prenatal care within the same military treatment facility. Maternity patient experience ratings from May 2014 to February 2016 were compiled from the TRICARE Outpatient Satisfaction Survey. Centering patients had 1.91 higher odds of being satisfied with access to care (p < .01, 95% CI = 1.2-3.1) than women in individual care. Specifically, the saw provider within 15 minutes of appointment measure found Centering patients to have 2.00 higher odds of being satisfied than women in individual care (p < .01, 95% CI = 1.2-3.3). There were no other statistically significant differences between cohorts. Qualitative responses indicate most Centering patients surveyed had good experiences, appreciated the structure and communication with others, and would recommend the program. Providers identified command/leadership support, dedicated space, and buy-in from all staff as important factors for successful implementation. Enhanced prenatal care models may improve access to and experiences with care. Program evaluation will be important as the military health system continues to implement such programs.
Keywords: maternal health, CAHPS, military health, access to care
Introduction
Military families face many stressors associated with deployment, frequent moves, and the absence of loved ones (1). This is of particular concern for active duty pregnant service members and pregnant partners of service members because stress has been found to be associated with pregnancy complications, including maternal morbidities, preterm births, decreased patient follow-up, and losses to overall productivity (2 –4). Strong social support may serve as an important mediator on the impact of the stress experienced by service members (5), and military families may benefit from increased social support and services during pregnancy. Assessing military patient’s obstetric (OB) care experiences is important because in recent years, patient satisfaction has become a meaningful and essential indicator for quality of care, assisting health systems in identifying gaps and potential action plans for quality improvement (6). Satisfaction with childbirth experiences is a significant outcome for women’s maternity care, as it impacts their health and relationships with their infants (7).
Prenatal care in the United States typically consists of individual encounters between a single patient and provider. The current recommended practice for traditional prenatal care includes a series of between 7 and 11 visits, typically monthly for the first 28 weeks of gestation, every 2 to 3 weeks between 28 and 36 weeks, and then weekly after 36 weeks (8). Patients typically have a brief encounter with a provider during each prenatal appointment, which limits opportunities for education and dialogue. One alternative to traditional one-on-one prenatal care is a group care model known as CenteringPregnancy (Centering), developed by midwife Sharon Rising (9). Compared to traditional one-on-one care, women participating in Centering are assembled by gestational age for group care. The benefits of Centering extend beyond traditional care to include education on nutrition, exercise, self-care, childbirth, relaxation techniques, breastfeeding and infant care, and as the opportunity to develop social connections to and support from other group members (9,10).
Previous research into the effects of Centering has shown benefits for women in their mental health, prenatal knowledge, level of involvement in their own care, adherence to attending their postpartum visit (11), as well as meeting social support needs and overall care satisfaction (11 –16). Centering’s effects on birth outcomes have been more mixed. Carter et al (17) performed a systematic review and meta-analysis of group prenatal care programs as compared to traditional care and found mixed evidence in outcomes related to low birth weight grouped by study type, and no significant differences in intensive care unit admission or breastfeeding initiation rate (17). However, recent studies published in 2019 have shown decreased risk of preterm birth and low birth rate in larger studies (18,19).
Several military treatment facilities (MTFs) offer Centering to help improve outcomes and the maternity care experience. Although many MTFs have been offering Centering for several years, Army Medicine implemented a 3-year initiative to start new programs that began in March 2017 (20). There have been a few studies that have examined the effects of implementing Centering at MTFs; however, they have been limited on assessments of patient perception and experience of care. Foster et al (21) revealed multiple advantages for women who participated in Centering within an MTF, including increased continuity of care between women and their providers, the opportunity for women to feel connected to others at the same stage of pregnancy, and decreased anxiety about appointments, since group care sessions were prescheduled (21). Challenges identified included reports of inadequately trained personnel for group care sessions, a transient patient population due to the demands of military life, no access to child care during appointments, poor program continuity and maintenance due to program funding challenges and staff turnover, and low levels of operational support from decision makers. Kennedy et al (22) completed 234 qualitative interviews with women as part of a clinical trial that enrolled 322 women randomized into Centering or traditional prenatal care at MTFs. Researchers performed a narrative and thematic analysis and found that women in Centering groups felt respected, believed they learned a lot about their bodies, felt that they were not alone, and that they had gained power as a health care consumer (22). Tubay et al (23) conducted a randomized controlled study of 129 women in prenatal care in MTFs and found women in Centering were less likely to deliver a small for gestational age or large for gestational age newborn and were more likely to be satisfied with their access to care as compared to women in individual care. They also found that group prenatal care is well received by patients and may positively influence neonatal metabolic status.
Assessing the perception of women who have completed Centering compared to traditional prenatal care is crucial to understanding the full effect of the program. Improving patient care experience has been shown to be a key component of enhanced health outcomes (24 –29). Better patient experience has also been associated with higher levels of adherence to recommended prevention and treatment processes, improved clinical outcomes, healthier patient safety culture, and more efficient health care service utilization (24). The purpose of this study is to understand the experience of care of maternity patients who completed Centering compared to maternity patients who completed traditional prenatal care within the same MTF from the same mix of providers (doctors, nurse practitioners, midwives).
Method
Quantitative Analysis
Sample
This analysis included data from the TRICARE Outpatient Satisfaction Survey (TROSS) supplemented with administrative data from the Comprehensive Ambulatory/Professional Encounter Record (CAPER) data set. The TROSS was a Consumer Assessment of Healthcare Providers and Systems (CAHPS)–based survey that assessed the ambulatory care experiences of MHS beneficiaries with an identified outpatient health care encounter. The TROSS survey was based on the CAHPS C&G 12-month Adult survey, using a 4-point response scale. The TROSS survey was replaced with the Joint Outpatient Experience Survey-CAHPS, which is described on the Defense Health Agency patient experience website (30). This analysis includes the access to care, communication with provider, and satisfaction with staff composite questions from the survey (Figure 1). The TROSS used a stratified random sample consisting of active-duty service members, military retirees, and their families, aged 18 years or older, with a recent ambulatory visit.
Figure 1.
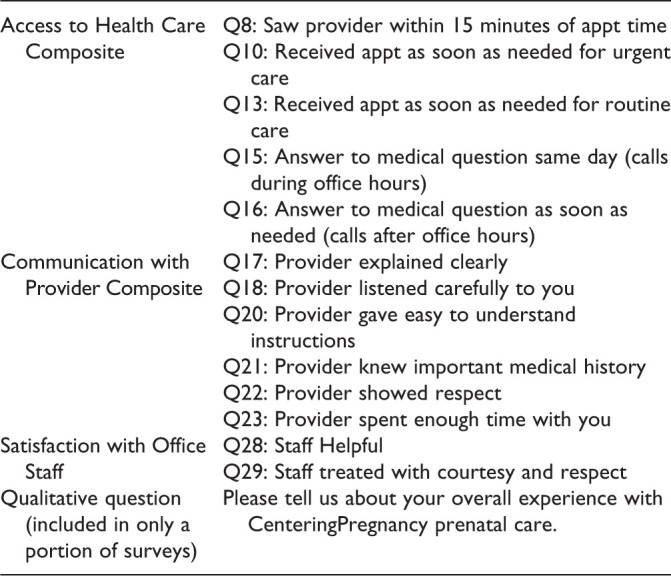
TRICARE Outpatient Satisfaction Survey composite questions included in analysis.
The study population was comprised of female, adult maternity patients of all military beneficiary types, service branch affiliation, education attainment and age, who completed OB care at 1 of 16 clinics identified as having the Centering program. Preliminary analysis of OB respondents indicated that around 10% participated in the Centering program. To achieve a minimum of 80% power with 95% confidence (p < 0.05) in detecting a statistically significant differenence of 15% or greater in satisfaction between the Centering and traditional care groups, the sample included the May 2014 to February 2016 time frame to obtain a minimum of 1100 total nonduplicated respondents. This study employed the existence of the Centering intervention to assess proportion and odds of satisfaction for those who received the program. In cases where an individual was sampled and responded more than once, only the most recent survey response was retained and included in our analysis. Women were categorized as part of the intervention group if their most recent visit was as part of a Centering session. Questions asked of the interview participants can be seen in Figure 2.
Figure 2.
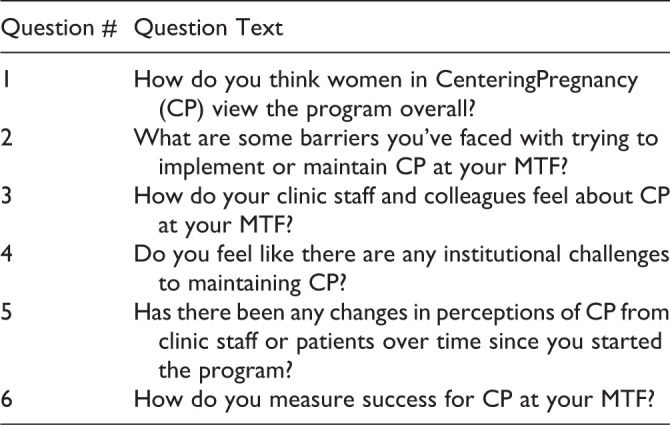
Qualitative Interview Questions.
Dependent variables
Six domains of patient satisfaction were assessed using individual questions from the TROSS. Following CAHPS methodological guidelines, dependent variables were created for the domains of access to care, provider communication, courtesy and respectfulness of office staff, overall provider and health care rating, and overall health care satisfaction. Two rating and 4 composite measures were constructed for patient care measures following CAHPS Clinician and Group Survey version 2.0 guidelines. Rating measures consisted of patient ratings of their provider and their health care on a scale of 0 to 10. For these 2 ratings, patient responses were rescaled to a binary, with scores of 9 or 10 indicating satisfaction. Composite measures combined results for closely related items. Following methods detailed by the Agency for Healthcare Research and Quality for analyzing CAHPS-CG data, questions incorporated into composite measures were top coded and binary indicators were created with the top-rated response representing patient satisfaction.
Analysis
Descriptive statistics illustrated proportion differences of the analytic population who received either traditional individual prenatal care or prenatal care as part of the Centering program. Linear combinations compared proportions of our analytic population that were part of the Centering group to those receiving traditional prenatal care by independent variable to identify significant differences. Logistic regression models were estimated for the analyzed patient experience measures and controlled using covariate variables identified previously. Centering group effects were assessed using a single difference approach, which compared changes in the Centering group to changes in the comparison group. We utilized this design as it was not possible to assess a pretime. We implemented this approach using a multilevel multivariable logistic regression at the service and facility levels to consider the characteristics of the military health system (MHS). Statistical analyses were conducted using Stata SE, version 13.
Qualitative Analysis
There were two qualitative assessments that were included in this study. First, a portion of the TROSS sample included questions specific to the Centering program as well as an open-ended question asking about the patient’s general care experience. Because this question was added to the survey after the program had started, it was only sent to a limited sample of 320 women who had encounters between December 2015 and February 2016. Second, we conducted 45- to 60-minute semistructured interviews with providers and Command Centering directors at 3 facilities (2 navy and 1 army) with current CenteringPregnancy programs to discuss implementation strategies, program successes, and program challenges. These interviews were conducted with 1 or 2 representatives from each facility and provided more in-depth insights on current program challenges, as well as the tools and institutional support necessary for program success.
Qualitative data from the open-ended surveys and the interviews were transcribed and coded by 2 independent coders using Nvivo 10 software. Codes were organized and used to assess for themes across each of the areas assessed.
This study included a secondary analysis of survey results and included less than 9 human participants for interviews. The Paperwork Reduction Act of 1980, amended in 1995, only requires federal agencies to obtain Office of Management and Budget approval if they intend to collect identical information from more than 9 respondents. Thus, this was excluded from a requirement to obtain approval by an institutional review board approval. In addition, the questions asked on the TROSS instrument were approved by the Survey Licensure and Clearance division, which provides direction, development, implementation, and oversight of survey research for MHS. The department develops policies, strategic plans, and operational guidance for survey research and interfaces with other key Department of Defense activities to ensure appropriate approval and licensing of all MHS surveys.
Results
Table 1 provides summary statistics of the sampled Centering and individual care participants included in this study. Among participants, those participating in the Centering program differed from those in individual care across active duty and active duty family member levels of beneficiary category as well as across age categories. In general, participants in the Centering program were more likely to be active duty and younger as compared to participants who received individual care.
Table 1.
Demographics of Centering Participants and Women in Individual Prenatal Care.
| Category | Centering | Individual care | ||
|---|---|---|---|---|
| N | % | N | % | |
| Total | 100 | 7 | 1241 | 93 |
| Beneficiary category | ||||
| Active dutya | 44 | 44 | 389 | 31 |
| Active duty family memberb | 54 | 54 | 837 | 67 |
| Retiree/retiree family member | 2 | 2 | 17 | 2 |
| Patient service branch affiliation | ||||
| Army | 55 | 55 | 676 | 54 |
| Air force | 12 | 12 | 210 | 17 |
| Marines | 15 | 15 | 134 | 11 |
| Navy | 11 | 11 | 196 | 16 |
| Other/unknown | 7 | 7 | 25 | 2 |
| Education | ||||
| Up to high school graduate | 5 | 5 | 120 | 10 |
| Some college | 40 | 43 | 445 | 37 |
| College graduate | 43 | 52 | 627 | 53 |
| Age (years) | ||||
| 18-24 | 27 | 27 | 230 | 19 |
| 25-34 | 62 | 62 | 794 | 64 |
| 35-44a | 11 | 11 | 217 | 17 |
a p < .05.
b p < .01.
Ratings for the access to care composite were significantly higher for women in Centering than individual care, with women in Centering reporting a 50.5% satisfaction rating compared to 33.8% for individual care, showing women in Centering had 1.91 higher odds of being satisfied with access to care (p < 0.01, 95% CI = 1.2-3.1; Table 2). Specifically, when this composite measure was broken out and examined by individual question, we found that the measure saw provider within 15 minutes of appointment was driving statistical significance in access, with women in Centering having a 2.00 higher odds of being satisfied than women in individual care (p < 0.01, 95% CI = 1.2-3.3; not shown). No other ratings for questions within the composite measure were statistically significantly different between the groups. The odds ratios for the other measures regarding differences between the CenteringPregnancy and individual care groups (Communication with Provider Composite, Office Staff Composite, Overall Satisfaction with Health care, Overall Provider Rating, and Rating of Health Care) ranged from 0.84 to 2.09 but did not achieve statistical significance with a 95% CI. Women in Centering programs and women in individual care showed similar satisfaction ratings for the Communication with Provider and the Office Staff Composites. There were differences in those in Centering programs and individual care for Overall Satisfaction with Health care, Rating of Provider, and Rating of Health Care overall, but these differences were not statistically significant.
Table 2.
TROSS Composite Satisfaction Ratings by Type of Prenatal Care, FY14Q3 to FY16Q2 Adjusted Odd Ratios.a
| Category | Access to health care | Communication with provider | Satisfaction with office staff | Rating of provider | Overall satisfaction with health care | Rating of health care | |
|---|---|---|---|---|---|---|---|
| AOR/se | AOR/se | AOR/se | AOR/se | AOR/se | AOR/se | ||
| Number of respondents | 1145 | 1145 | 1143 | 1141 | 1142 | 1271 | |
| CenteringPregnancy | 74 | 77 | 76 | 76 | 77 | 93 | |
| Standard care | 1068 | 1068 | 1067 | 1065 | 1065 | 1178 | |
| CenteringPregnancy | 1.91c | 0.93 | 1.18 | 1.54 | 2.09 | 0.84 | |
| Reference standard care | 0.47 | 0.23 | 0.30 | 0.44 | 1.01 | 0.19 | |
| Age (cont.) | 25-34 years | 0.97 | 1.79c | 1.00 | 1.61c | 1.17 | 1.37 |
| Reference 18-24 years old | 0.18 | 0.31 | 0.18 | 0.29 | 0.30 | 0.23 | |
| 35-44 years | 2.00c | 2.23b | 1.10 | 1.93c | 1.60 | 1.94c | |
| 0.46 | 0.19 | 0.25 | 0.46 | 0.55 | 0.42 | ||
| Education | Some college | 1.20 | 1.08 | 1.02 | 0.63 | 0.84 | 0.69 |
| Reference up to high school graduate | 0.28 | 0.24 | 0.23 | 0.16 | 0.28 | 0.15 | |
| College graduate | 0.84 | 0.81 | 0.77 | 0.47c | 0.75 | 0.51c | |
| 0.21 | 0.09 | 0.18 | 0.12 | 0.26 | 0.12 | ||
| Self-rated health | Good | 0.58c | 0.55b | 0.55b | 0.54b | 0.48c | 0.42b |
| Reference excellent | 0.10 | 0.09 | 0.09 | 0.09 | 0.11 | 0.06 | |
| Fair/poor | 0.37d | 0.21b | 0.55 | 0.28c | 0.13b | 0.25c | |
| 0.18 | 0.09 | 0.22 | 0.11 | 0.05 | 0.10 | ||
| Beneficiary category | Active duty family | 0.92 | 0.82 | 0.46 | 0.76 | 0.59 | 0.80 |
| Reference active duty | 0.52 | 0.44 | 0.25 | 0.42 | 0.39 | 0.43 | |
| Retiree/retiree family | 1.20 | 1.16 | 1.22 | 1.02 | 1.14 | 1.07 | |
| 0.17 | 0.16 | 0.17 | 0.15 | 0.24 | 0.14 |
Abbreviation: TROSS, TRICARE Outpatient Satisfaction Survey.
a Analyses performed using multilevel logistic regression to take into account clustering at the facility level.
b p < 0.001.
c p < 0.01.
d p < 0.05.
Open-Ended Survey Comments
Seventeen women responded with qualitative feedback on the CenteringPregnancy program. The majority (88%) of women who responded indicated that they had positive experiences with the Centering program overall. Patients were happy with the structure of the program, appreciated the opportunity to communicate with other mothers, and indicated that they would recommend the program to others. Comments on the overall experience of Centering included feedback that the program was resourceful and helpful and that the program and format was informative and engaging. One participant commented that it was really helpful as a first-time mom to go through this experience with others at the same time. Program participants indicated that they developed strong connections with each other, as well as bonds with the Centering staff. There was negative feedback present in 4 comments from women, which related to privacy concerns and a lack of individual relationships with doctors and midwives (both regarding lack of one-on-one time and to practitioners’ inability to remember or address patients’ specific, individualized concerns). One woman indicated that certain providers had trouble keeping track of patient details, recalling that their doctor could never remember me or the issues I was having.
Interviews With CenteringPregnancy Providers/Implementers
Providers in the Centering program offered feedback in several areas, including implementation, program successes, and challenges. Two topics that were frequently raised by most providers were the importance of having a dedicated space for the programs within the clinic or hospital and of having support from leadership. Programs without a dedicated space had to perform additional administrative work to continue holding group sessions, as their locations would change, or rooms would become unavailable. One administrator reported this as a significant obstacle for the continuity of their program:
Space [was] very hard to come by—we had a classroom space initially and a lot of work went into getting this classroom as a designated space, but it had to be shared with other educational programs. Eventually we lost the space for Centering to other programs.
Buy-in from leadership and other staff was also discussed as an important aspect, as providers indicated it was critical that all staff be supportive and promote the program to continue successfully recruiting participants. Some reported initial challenges with doctors who “Rebuffed [them] because Centering was ‘not a good use of their time,’” whereas more successful programs had multiple staff members from varied staff categories on board including doctors, midwives, and support staff. Speaking of their program success, one administrator reported, “We have command and physician support—we’re the happy unicorn because every MTF isn’t like this.”
Discussion
The military population is unique, with specific social risk factors for family disruption and adverse pregnancy outcomes. In addition, receiving care in MTFs allows for opportunities for a more tailored set of care delivery specific to these beneficiaries. The Centering program offers a model for prenatal care that can be implemented in MTFs and can provide a stable network for women and families. The CenteringPregnancy program has been shown in this study to produce higher patient experience scores among women regarding accessing care in a timely manner compared to women in individual care at the same clinic. Improved access, represented by the measure “saw provider within 15 minutes of appointment,” is a particularly important measure examined within the MHS, because Access to Care has historically had low ratings for military care settings as related to other quality-of-care measures (31,32). This finding indicates a potential area of significant improvement for the MHS in terms of improving patients’ experience of care. Previous studies have shown lower satisfaction with care among patients who experience longer wait times, as well as better treatment adherence and patient outcomes among those who waited shorter periods for care (31,32). Therefore, MHS investments in improving wait times can potentially be beneficial not just for patients but also for physicians in improving patient adherence and outcomes overall.
All other patient experience measures showed no differences between the 2 groups assessed. This may indicate that there are no other differences beyond access to care for women who completed Centering compared to those in individual care. However, because the TROSS instrument was not administered specifically about the Centering program and rather asked questions about a specific outpatient visit additional, more targeted research is needed.
Qualitative responses indicate that most women surveyed in Centering had positive experiences and received interactive learning opportunities, structure, social support, and meaningful communication with other women, and they would recommend the program to others. Providers identified command/leadership support, dedicated program space, and buy-in from staff as important success factors for implementation. These results indicate that Centering programs have had a positive impact on patient experience in military facilities, particularly regarding access to care ratings, and that sustained proper structural and command support is an essential component to successful programs. Assessment of these barriers or facilitators to successful integration is important conduct before implementing the program.
Although previous studies have found an increase in satisfaction with care, our study population showed no significant differences between women in Centering and women in individual care with regard to overall satisfaction as a single measure of care. However, our findings regarding improved patient experience with Access to Care, driven by their ability to see their provider quickly (“saw provider within 15 minutes of appointment”) reflects previous research citing the importance of the amount of time saved waiting for care for women in Centering (22). Similarly, the results of the qualitative analysis are consistent with previous findings reporting improvements in social support for women in Centering programs in military health settings (13,22). Our findings from interviews with providers and implementation staff also reflect those of previous research demonstrating the challenges of finding dedicated program space as well as the importance of support from MTF leadership (21).
Conclusion
This study adds to the literature a mixed-methods analysis of patient experience in CenteringPregnancy unique to the military population in which CenteringPregnancy is expanding. Although our findings are promising, in that they suggest potential for CenteringPregnancy to improve access to care among expectant mothers, there are limitations to the data utilized in this study. Satisfaction questions on TROSS do not fully capture the experience of Centering patients within their specific programs. For example, provider communication questions are specific to satisfaction with provider; however, much of the learning and interaction in the Centering program is with the group facilitator and other women. The sample size used for this study was also small for a few reasons: (1) We retrospectively selected women who completed Centering who happened to be sampled for the TROSS, (2) only a select sample of women received the open-ended question relating to their Centering experience, and (3) we were limited in the number of providers who participated in the interview. Additional qualitative analysis or case studies may be needed to explore in greater depth the effectiveness of particular programs, which vary from facility to facility. Further studies could also be useful in assessing other aspects of the patient experience, prenatal outcomes, and birth outcomes associated with attending Centering compared to individual care.
Acknowledgments
The authors thank the participants of this study and their contributions to this work through their survey responses and interviews.
Author Biographies
Tara Trudnak Fowler is Director at Altarum Institute.
Kimberley Marshall Aiyelawo is chief of patient experience measurement at the Defense Health Agency.
Chantell Frazier is manager and senior researcher at Altarum Institute.
Craig Holden is a senior researcher at Altarum Institute.
Joseph Dorris is senior health care economist at Altarum Institute.
Authors’ Note: The contents of this presentation are the sole responsibility of the authors and do not represent the official views of The Defense Health Agency, Department of Defense.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was performed under a contract with the Defense Health Agency and Altarum Institute, Contract number: HHSP233201500031I_HHSP23337003T.
ORCID iD: Tara Trudnak Fowler  https://orcid.org/0000-0001-7722-0501
https://orcid.org/0000-0001-7722-0501
References
- 1. Green S, Nurius P, Lester P. Spouse psychological well-being: a keystone to military family health. J Hum Behav Soc Environ. 2013;23:753–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McNeary A, Lomenick T. Military duty: risk factor for preterm labor? A review. Mil Med. 2000;165:612–5. [PubMed] [Google Scholar]
- 3. Shaw J, Nelson D, Shaw K, Woolaway-Bickel K, Phibbs CS, Kurina LM. Deployment and preterm birth among US army soldiers. Am J Epidemiol. 2018;187:687–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Stinson J, Lee K. Premature labor and birth: influence of rank and perception of fatigue in active duty military women. Mil Med. 2003;168:385–90. [PubMed] [Google Scholar]
- 5. Ozbay F, Fitterling H, Charney D, Southwick S. Social support and resilience to stress across the life span: a neurobiologic framework. Curr Psychiatry Rep. 2008;10:304–10. [DOI] [PubMed] [Google Scholar]
- 6. Al-Abri R, Al-Balushi A. Patient satisfaction survey as a tool towards quality improvement. Oman Med J. 2014;29:3–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ferrer M, Jordana M, Meseguer C, Carrillo García C, Martínez Roche ME. Comparative study analysing women’s childbirth satisfaction and obstetric outcomes across two different models of maternity care. BMJ Open. 2016;6:e011362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kilpatrick S, Papile L, Macones G. Guidelines for Perinatal Care. 8th ed American Academy of Pediatrics and American College of Obstetrics and Gynecology; 2017. [Google Scholar]
- 9. Rising S. CenteringPregnancy an interdisciplinary model of empowerment. J Nurse Midwifery. 1998;43:46–54. [DOI] [PubMed] [Google Scholar]
- 10. Tanner-Smith E, Steinka-Fry K, Gesell S. Comparative effectiveness of group and individual prenatal care on gestational weight gain. Maternal Child Health J. 2013;18:1711–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Trudnak T, Arboleda E, Kirby R, Perrin K. Outcomes of Latina women in centering pregnancy group prenatal care compared with individual prenatal care. J Midwifery Womens Health. 2013;58:396–403. [DOI] [PubMed] [Google Scholar]
- 12. Benediktsson I, McDonald S, Vekved M, McNeil D, Dolan S, Tough S. Comparing centering pregnancy® to standard prenatal care plus prenatal education. BMC Pregnancy Childbirth. 2013;13:S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chae S, Chae M, Kandula S, Winter RO. Promoting improved social support and quality of life with the CenteringPregnancy® group model of prenatal care. Arch Womens Ment Health. 2016;20:209–20. [DOI] [PubMed] [Google Scholar]
- 14. Homer CSE, Ryan C, Leap N, Foureur M, Teate A, Catling-Paull CJ. Group versus conventional antenatal care for women. Cochrane Data Syst Rev. 2012:CD007622. [DOI] [PubMed] [Google Scholar]
- 15. Ickovics JR, Kershaw TS, Westdahl C, Magriples U, Massey Z, Reynolds H, et al. Group prenatal care and perinatal outcomes: a randomized controlled trial. Obstetrics Gynecol. 2007;110:330–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ruiz-Mirazo E, Lopez-Yarto M, McDonald S. Group prenatal care versus individual prenatal care: a systematic review and meta-analyses. J Obstet Gynaecol Can. 2012;34:223–9. [DOI] [PubMed] [Google Scholar]
- 17. Carter E, Temming L, Akin J, Fowler S, Macones G, Colditz G, et al. Group prenatal care compared with traditional prenatal care. Obstet Gynecol. 2016;128:551–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Crockett AH, Heberlein EC, Smith JC, Ozluk P, Covington-Kolb S, Willis C. Effects of a multi-site expansion of group prenatal care on birth outcomes. Matern Child Health J. 2019;23:1424–33. [DOI] [PubMed] [Google Scholar]
- 19. Abshire C, Mcdowell M, Crockett AH, Fleischer NL. The impact of centeringpregnancy group prenatal care on birth outcomes in Medicaid eligible women. J Womens Health (Larchmt). 2019;28:919–28. [DOI] [PubMed] [Google Scholar]
- 20. Elliott W. Centering prenatal care around you. 2016. Retrieved August 28, 2018, from: https://www.army.mil/article/178532/centering_prenatal_care_around_you.
- 21. Foster G, Alviar A, Neumeier R, Wootten A. A tri-service perspective on the implementation of a centering pregnancy model in the military. J Obstet, Gynecol Neonatal Nurs. 2012;41:315–21. [DOI] [PubMed] [Google Scholar]
- 22. Kennedy H, Farrell T, Paden R, Hill S, Jolivet R, Willetts J, et al. “I Wasn’t Alone” – a study of group prenatal care in the military. J Midwifery Womens Health. 2009;54:176–83. [DOI] [PubMed] [Google Scholar]
- 23. Tubay AT, Mansalis KA, Simpson MJ, Armitage NH, Briscoe G, Potts V. The effects of group prenatal care on infant birthweight and maternal well-being: a randomized controlled trial. Mil Med. 2019;184:e440–6. [DOI] [PubMed] [Google Scholar]
- 24. Anhang Price R, Elliott M, Zaslavsky A, Hays RD, Lehrman WG, Rybowski L, et al. Examining the role of patient experience surveys in measuring health care quality. Med Care Res Rev. 2014;71:522–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Browne K, Roseman D, Shaller D, Edgman-Levitan S. Measuring patient experience as a strategy for improving primary care. Health Affairs. 2010;29:921–5. [DOI] [PubMed] [Google Scholar]
- 26. Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3:e001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Robert Wood Johnson Foundation. Forces driving implementation of the CAHPS Clinician & Group Survey. 2013. Retrieved August 29, 2018, from: https://www.rwjf.org/content/dam/farm/reports/issue_briefs/2013/rwjf72668.
- 28. Greenfield S, Kaplan S, Ware J. Expanding patient involvement in care. Ann Inter Med. 1985;102:520. [DOI] [PubMed] [Google Scholar]
- 29. Stewart M. Effective physician-patient communication and health outcomes: a review. Can Med Assoc J. 1995;152:1423–33. [PMC free article] [PubMed] [Google Scholar]
- 30. Military Health System. MHS Patient Satisfaction Surveys. [online]. 2019. Retrieved December 16, 2019, from: https://www.health.mil/Military-Health-Topics/Access-Cost-Quality-and-Safety/Health-Care-Program-Evaluation/MHS-Patient-Satisfaction-Surveys.
- 31. Defense Health Agency (DHA), Decision support division office of the assistant secretary of defense (Health Affairs) (OASD [HA]). Evaluation of the TRICARE Program: Fiscal Year 2018 Report to Congress. Access, cost, and quality data through fiscal year 2017. 2018. Retrieved August 29, 2018, from: https://www.health.mil/Military-Health-Topics/Access-Cost-Quality-and-Safety/Health-Care-Program-Evaluation/Annual-Evaluation-of-the-TRICARE-Program.
- 32. Final Report to the Secretary of Defense: Military Health System Review. Health.mil. 2014. Retrieved August 23, 2018, from: https://www.health.mil/Military-Health-Topics/Access-Cost-Quality-and-Safety/MHS-Review.


