Abstract
Patient engagement (PE) promotes collaboration between stakeholders (researchers, patients, clinicians, etc). It often faces challenges due to tensions between its ethical/political and scientific underpinnings. This article explores how stakeholders applied the guiding principles of a PE project (“co-build,” “support and mutual respect,” and “inclusiveness”) for an HIV clinical research program initiated in January 2016. Three researchers/clinicians, a PE agent, and 2 patients held 3 meetings (June-October 2018) to discuss challenges faced and how these impacted their approach to PE. Regular stakeholder discussions about PE in clinical research could be documented and help guide PE to better meet stakeholder needs.
Keywords: patient engagement, patient perspectives/narratives, qualitative, methods, Patient Advisory Councils, team communication
Introduction
Patient engagement (PE) seeks to actively involve stakeholders (patients, clinicians, etc) in research, including in governance and knowledge dissemination (1). Patient engagement is theoretically rooted first in ethico-political, if not “ideological,” perspectives promoting empowerment (2 –4), and secondly, in more instrumental or “scientific” views stressing principles of evidence-based medicine. These distinct views can sometimes cause tensions between stakeholders, documented in several fields of medical research (2 –4). These fields include HIV research, despite an historical commitment to empowering affected communities (5). For instance, the Greater Involvement of People Living with HIV principles, formulated in 1994, bolstered the development of community-based participatory research. Still, medical researchers often apply these principles inconsistently, or invoke them strategically (5).
More recently, the Canadian Institutes for Health Research Strategy for Patient-Oriented Research (CIHR/SPOR) defined guiding principles of PE and interactions between stakeholders as: co-build (stakeholders working together), support (emphasizing flexibility, safety, honesty, education, and compensation), mutual respect (acknowledging stakeholders’ respective values and expertise), and inclusiveness (integrating diverse patient perspectives) (1). It is recommended that stakeholders clarify their understanding of the principles guiding their PE initiatives and of the challenges encountered when applying them so as to better understand the impacts of PE and increase its efficiency (2,3). This article presents the results of this reflective exercise for one group of stakeholders involved in PE within an HIV clinical research program.
The PE Project
The I-Score Study (January 2016-present) aims to develop a digital patient-reported outcome measure (PROM) of antiretroviral treatment (ART) adherence barriers and implement it in HIV care (6). Phase 1 (January 2016-September 2017) focused mainly on conducting a synthesis of qualitative research on patient-perceived ART adherence barriers to elaborate the PROM’s conceptual framework (7).
I-Score researchers include an MD (HIV clinician and PhD in theology), and 2 PhDs in public health. In 2015, they appointed a “PE agent” (PhD in anthropology) to form a patient advisory committee (the I-Score Consulting Team, or the Team) and design a PE Project by operationalizing CIHR/SPOR’s Guiding Principles (for details, see Lessard et al (7)). These principles were chosen as “co-build” and “inclusiveness” specifically addressed researchers’ concerns about, respectively, PROM development (the need to ensure the PROM reflected user concerns (6)), and HIV research (the underrepresentation of certain groups, including women (5,8)). In addition, the CIHR has a national network of PE practitioners, which was seen as a potential resource for our project. Table 1 presents how these principles were operationalized in the PE Project.
Table 1.
CIHR Guiding Principles and Their Operationalization in Phase 1 of the I-Score Study.
| Guiding principle | Operationalization | Initial actions |
|---|---|---|
| Co-build | Formation of an advisory committee composed of expected PROM end users Committee consultation at each step of the research Involvement of committee members in knowledge-dissemination activities |
The PE agent recruited 10 HIV patients to compose the advisory committee, renamed the I-Score Consulting Team Twelve committee meetings were organized and facilitated by the PE agent, who also took notes which were transferred to members for validation and presented to researchers Four knowledge-dissemination presentations were organized and given by patients, researchers, and the PE agent to diverse audiences (community members, academics, clinicians, etc) |
| Support and mutual respect | Attention paid to incentives, comfort, and cohesion during meetings | Researchers compensated patients ($50 CAD per meeting), and provided food, and refreshments at each meeting Meetings were held at a community center suggested by committee members and where they felt comfortable Discussions followed a deliberative format: members could spontaneously express themselves and redefine discussion themes based on their interest and concerns |
| Inclusiveness | Recruitment of HIV patients of different genders and ages, from key epidemiological HIV-risk groups in Quebec, and with experience of community organizing and participation in research, to compose the patient advisory committee | The patient committee was composed of 5 men and 5 women of different ages (min.: 27 years old; max.: 69 years old), including men who have sex with men, immigrants from HIV endemic countries, and people with a past of intravenous drug use |
Abbreviations: CIHR, Canadian Institutes of Health Research; PE, patient engagement; PROM, patient-reported outcome measure.
Methods
The PE agent and a team member decided to prepare a panel to present stakeholders’ different experiences of PE for the 2018 CIHR/SPOR Summit (9). They thus invited I-Score researchers and another Team member to 3 preparatory meetings (June 26, September 20, October 30, 2018; 2 hours each). The first Team member facilitated meetings with the PE agent, and the PE agent took notes.
Before meetings, participants filled out a table on challenges faced, solutions envisioned/implemented, and perceived changes in PE. During meetings, they elaborated on these elements. At the panel, each presenter discussed key events that lead to important changes in the PE Project. After the panel, Summit attendees encouraged its publication.
The first author conducted a content analysis for textual documents (10). He associated quotes from participants’ table documents and meeting notes to guiding principles. He then categorized these quotes as challenges, solutions, or results/changes. Considering the content under each principle and category, he identified patterns, the intended outcome of this analysis. To limit biases and ensure trustworthiness (11), David Lessard discussed and validated interpretations with the coauthors.
Results
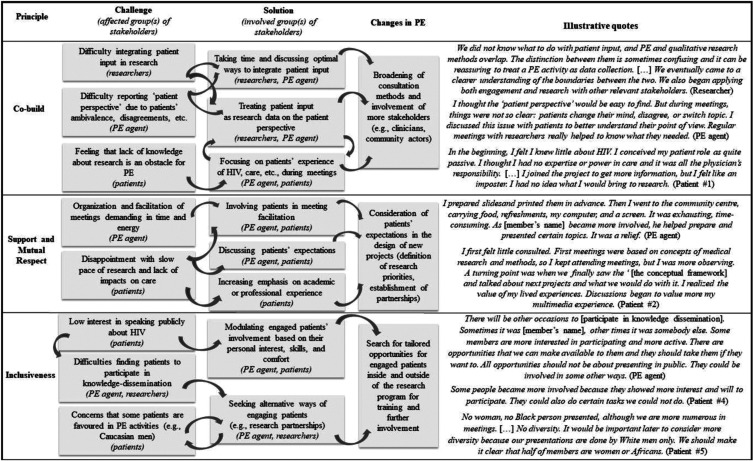
Figure 1 summarizes reported challenges and solutions for each PE principle, and their purported impacts.
Figure 1.
Reported challenges and solutions for each PE principle, purported impacts, and illustrative quotes.
Co-Build
In the initial design of the PE Project, to co-build, it was planned that patients would be consulted at each step of research during team meetings and collaborate in knowledge dissemination. The PE agent would report their feedback to researchers. However, he noted difficulties: patients sometimes shared off-topic comments, disagreed, or changed their minds from one meeting to the next. Patients sometimes felt they did not know enough about research and preferred to leave decisions to researchers. Researchers sought ways to integrate this feedback with the PE agent and decided to explore the patient perspective, treating certain meetings as “focus groups,” qualitatively analyzing transcriptions, and generating findings of general interest to the research program.
Due to the above difficulties, practices associated with “co-building” progressively broadened methodologically, to include a greater variety and number of stakeholders. For instance, when crucial PROM-related decisions had to be made and researchers’ concerns about patient input heightened, researchers added consultation initiatives to the protocol of the I-Score Study with more patients and stakeholder groups (clinicians, community actors, etc). These initiatives draw on both quantitative methods, notably, an online Delphi survey (12) with 96 participants (40 patients and 56 providers), and qualitative methods (eg, focus groups).
Support and Mutual Respect
Initial measures to ensure support and mutual respect incentivised PE (eg, financial compensation) and fostered comfort (eg, choice of room and food) and cohesion (eg, deliberative meeting format). However, the PE agent struggled with the time and energy required. Furthermore, patients’ interest decreased at times due to the slow pace of research, lack of impacts on care, and little interest in the PROM’s conceptual framework in comparison with more relatable topics (eg, HIV-related experiences).
As a solution, the PE agent and team members began discussing expectations and skills that could benefit research, and some team members became more involved in meetings (eg, by cofacilitating discussions). The approach to “support” and “mutual respect” hence became to increasingly account for patients’ expectations and abilities and seek partnerships with individual patients. For instance, they partnered with a team member in the development of the digital platform of the PROM and in the design of a project to generate stakeholder-informed interventions to manage ART adherence barriers.
Inclusiveness
“Inclusiveness” was initially applied to team composition, by recruiting patients of different genders, ages, and epidemiological HIV-risk groups. Challenges arose when the PE agent sought the team’s collaboration in knowledge dissemination: members were little interested in speaking publicly about HIV. Stakeholders hence agreed to modulate participation based on individual interest and comfort. The team, nevertheless, noticed that the 3 members included in knowledge dissemination were all Caucasian men. There was no representation of women or racialized members. These concerns were further fueled when researchers approached 2 Caucasian male patients to establish partnerships base on their professional expertise (ie, statistics, information technologies).
After phase 1, the approach to inclusiveness evolved to include notions of equity and accessibility. The PE agent sought out tailored opportunities for the active engagement of more individual members. For example, one female patient of African origin cosigned a letter supporting a funding proposal, and 2 female and immigrant patients piloted I-Score-related questionnaires.
Discussion
This article explored stakeholders’ experiences of PE guiding principles in an HIV research program. Challenges were not fully resolved, but as suggested in a recent commentary (3), clarifying stakeholders’ perspectives can lead to improvement and better balance ethico-political and scientific considerations in PE. For instance, in the PE Project, adjustments in “co-building” toward greater methodological and stakeholder diversification, brought more voices to the table and improved the quality of evidence generated by PE. Changes in the approach to “support and mutual respect” and “inclusiveness” generated individual engagement opportunities, including partnerships, that were more tailored to patients (eg, expertise, preference).
Combining PE and research while engaging different stakeholders (eg, clinicians, community actors) carries the risk of sidestepping patient input or assigning patients roles that “fit” their skillset (13). This concern is relevant when practicing PE with patients with HIV, who often face barriers related to stigma, mental health, or quality of life (5,14). However, with time, engaged patients can reduce these barriers by supporting or learning coping strategies from each other (5,8,14). Furthermore, if all stakeholders agree to make PE an integral part of research, a more productive PE/research synergy can emerge (4). In the present PE Project, research is conducted with the close and active involvement of a growing and diverse group of patients. In fact, new research initiatives have created PE opportunities more sensitive to individual interests, limits, and learning capacities. Likewise, several new studies were instigated based on patient feedback (eg, the project to generate interventions to manage ART adherence barriers). Cultivating these opportunities has become a vital component of a CIHR/SPOR Mentorship Chair (awarded to the last author in February 2018), that ensured PE’s continuity in subsequent phases of the research program.
Limitations
Few patients participated in this article. Nevertheless, an earlier publication discussed patient perspectives (7), and in this article, we sought to present a variety of stakeholder accounts. Participants may have favored groupthink, although stakeholders held diverging opinions, including within groups. Organizational aspects of PE were not systematically addressed in this article. These include time, spatial, and human resources specifically dedicated to selecting, preparing, and involving patients, and a supportive and accountable leadership (15). This study focussed on issues raised by select key stakeholders, with mention of some organizational aspects (eg, time, location, incentives for PE). Their importance could be analyzed in greater depth in another study. Finally, the retrospective nature of the data, and the fact that one person took and analyzed notes without audio recordings or transcriptions, may have induced biases. However, all participants approved the results.
In conclusion, this article highlights some of the “growing pains” of a PE project affiliated with an HIV research program. Regular stakeholder discussions could help individuals to meet their respective objectives, needs, and concerns, thus improving accountability and showcasing PE’s evolving nature.
Acknowledgments
The authors thank AIDS Community Care Montreal (ACCM), Portail VIH/sida du Québec, Maison Plein Coeur, Projet PluriELLES, and the McGill University Health Centre (MUHC) Chronic and Viral Illness Service (CVIS) staff for their help initiating the patient engagement Project. The authors also thank Laurianne Senécal for revisions of this paper. Our Patient Engagement Project received support from the CIHR/SPOR Mentorship Chair in Innovative Clinical Trials in HIV, and from an unrestrictive grant from Gilead Sciences Canada Inc. The opinions expressed in this manuscript are those of the authors and do not necessarily represent those of Merck Canada Inc., Gilead Sciences Canada Inc., or their affiliates or related companies.
Author Biographies
David Lessard, PhD (Social Anthropology), is a research assistant at the Centre for Outcome Research and Evaluation (CORE) at the Research Institute of the McGill University Health Centre (RI-MUHC). His work focusses on the conduct of patient-oriented research and patient & stakeholder engagement initiatives within an HIV, COVID-19, and oncology clinical research program.
Kim Engler, PhD (Public Health), is a research associate at CORE, RI-MUHC. Her current work centers on medication adherence and patient-reported outcome measure development and implementation for research and care, especially in the field of HIV.
Serge Vicente, PhDc (Statistics), is a lecturer for undergraduate courses of mathematics and statistics at University of Montréal and a statistician collaborating with the Research Institute of the McGill University Health Centre as a research trainee. He acts as a co-author for several patient-oriented research projects with his statistical expertise and works on the development of innovative clinical trials such as platform trials.
Martin Bilodeau has been implicated with the HIV community as project manager, board administrator and peer advisory committee member. His professional focus is on technological platforms, education and online learning empowering people living with HIV.
Bertrand Lebouché, MD, PhD, is a clinician researcher specialized in primary care for people living with HIV and / or hepatitis C at the Chronic Viral Illness Service of the MUHC. He is also an associate professor in the Department of Family Medicine at McGill University. With his team, he is currently developing new e-health solutions to promote HIV self-management.
Authors’ Note: The PE Project was submitted to the Research Ethics Board of the Research Institute of the MUHC which approved it on September 8, 2015. Written informed consent was obtained from patients.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: B.L. is supported by a Research Scholar award of the FRQS (Quebec Health Research Funds) and is the recipient of a Canadian Institutes for Health Research Strategy for Patient-Oriented Research (CIHR/SPOR) Mentorship Chair in Innovative Clinical Trials in HIV. The I-Score Study is supported by CIHR’s HIV Clinical Trials Network (CTN 283) and by a research grant from the Investigator Initiated Studies Program of Merck Canada (IISP-53538).
ORCID iD: David Lessard  https://orcid.org/0000-0002-1151-3763
https://orcid.org/0000-0002-1151-3763
References
- 1. SPOR Patient Engagement Consultation Workshop. Strategy for Patient-Oriented Research: Patient Engagement Framework: Canadian Institutes of Health Research Strategy for Patient Oriented Research; 2014.
- 2. Staley K. ‘Is it worth doing?’ Measuring the impact of patient and public involvement in research. Res Involv Engagem. 2015;1:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Boivin A. From craft to reflective art and science comment on “metrics and evaluation tools for patient engagement in healthcare organization- and system-level decision-making: a systematic review”. Int J Health Policy Manage. 2019;8:124–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Edelman N, Barron D. Evaluation of public involvement in research: time for a major re-think? J Health Serv Res Policy. 2016;21:209–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Karris MY, Dubé K, Moore AA. What lessons it might teach us? Community engagement in HIV research. Curr Opin HIV AIDS. 2020;15:142–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Engler K, Lessard D, Toupin I, Lènàrt AS, Lebouché B Engaging stakeholders into an electronic patient-reported outcome development study: On making an HIV-specific e-PRO patient-centered. Health Policy Technol. 2017;6:59–66. [Google Scholar]
- 7. Lessard D, Engler K, Toupin I, Routy JP, Lebouche B. Evaluation of a project to engage patients in the development of a patient-reported measure for HIV care (the I-Score Study). Health Expect. 2019;22:209–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Largent EA, Lynch HF, McCoy MS. Patient-engaged research: choosing the “right” patients to avoid pitfalls. Hastings Center Rep. 2018;48:26–34. [DOI] [PubMed] [Google Scholar]
- 9. Lessard D, Vicente S, Toupin I, Laurent M, Engler K, Lebouche B, eds. “I never thought it would take me here”: Investigators’ and people living with HIV’s evolving experiences and perspectives on patient engagement working on a clincial study (the I-Score Study). Strategy for Patient-Oriented-Research Summit - Mapping the Progress of Patient-Oriented Research in Canada; 2018. [Google Scholar]
- 10. Hodder I. The interpretation of documents and material culture In: Denzin NK, Lincoln YS, eds. The Handbook of qualitative research: Sage Publications; 1994. 393–402. [Google Scholar]
- 11. Noble H, Smith J. Issues of validity and reliability in qualitative research. Evid Based Nurs Evidence Based Nurs. 2015;18:34. [DOI] [PubMed] [Google Scholar]
- 12. Engler K, Ahmed S, Lessard D, Vicente S, Lebouché B. Assessing the content validity, actionability, and cross-cultural equivalence of a new patient-reported outcome measure of barriers to antiretroviral therapy adherence for electronic administration in routine HIV care: protocol for an online Delphi study. J Med Int Res. 2018;8:e12836 In print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rowland P, McMillan S, McGillicuddy P, Richards J. What is “the patient perspective” in patient engagement programs? Implicit logics and parallels to feminist theories. Health. 2017;21:76–92. [DOI] [PubMed] [Google Scholar]
- 14. Varni SE, Miller CT, McCuin T, Solomon S. Disengagement and engagement soping with HIV/AIDS stigma and psychological well-being of people with HIV/AIDS. J Soc Clini Psychol. 2012;31:123–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Baker GR, Judd M, Fancott C, Maika C. Creating “engagement-capable environments” in healthcare. Patient Engag Catalyz Improv Innovat Healthc. 2016;12:11–34. [Google Scholar]