In a 6-year EHR study of 43 825 patients, we find that many children’s high blood pressure levels resolve over time without intervention.
Abstract
Video Abstract
OBJECTIVES:
To determine the natural history of pediatric hypertension.
METHODS:
We conducted a 72-month retrospective cohort study among 165 primary care sites. Blood pressure measurements from two consecutive 36 month periods were compared.
RESULTS:
Among 398 079 primary care pediatric patients ages 3 to 18, 89 347 had ≥3 blood pressure levels recorded during a 36-month period, and 43 825 children had ≥3 blood pressure levels for 2 consecutive 36-month periods. Among these 43 825 children, 4.3% (1881) met criteria for hypertension (3.5% [1515] stage 1, 0.8% [366] stage 2) and 4.9% (2144) met criteria for elevated blood pressure in the first 36 months. During the second 36 months, 50% (933) of hypertensive patients had no abnormal blood pressure levels, 22% (406) had elevated blood pressure levels or <3 hypertensive blood pressure levels, and 29% (542) had ≥3 hypertensive blood pressure levels. Of 2144 patients with elevated blood pressure in the first 36 months, 70% (1492) had no abnormal blood pressure levels, 18% (378) had persistent elevated blood pressure levels, and 13% (274) developed hypertension in the second 36-months. Among the 7775 patients with abnormal blood pressure levels in the first 36-months, only 52% (4025) had ≥3 blood pressure levels recorded during the second 36-months.
CONCLUSIONS:
In a primary care cohort, most children initially meeting criteria for hypertension or elevated blood pressure had subsequent normal blood pressure levels or did not receive recommended follow-up measurements. These results highlight the need for more nuanced initial blood pressure assessment and systems to promote follow-up of abnormal results.
What’s Known on This Subject:
Pediatric hypertension, currently defined as 3 high blood pressure levels, is known to be underdiagnosed. No studies using routine clinical measurements in primary care show the natural history of pediatric hypertension.
What This Study Adds:
We show that most children and adolescents meeting criteria for hypertension have their abnormal blood pressure levels normalize over several years with repeated measurement. Many children even with stage 2 hypertension do not have routine blood pressure levels measured annually.
Pediatric hypertension has an estimated prevalence of 2% to 5%,1–5 predisposes children to adult hypertension, and is associated with early markers of cardiovascular disease.6–13 Definitions of pediatric hypertension and elevated blood pressure are based on 3 abnormal blood pressure measurements. For children <13 years old, hypertension is defined as diastolic and/or systolic readings ≥95th percentile for age, height, and sex, whereas elevated blood pressure is ≥90th percentile but <95th percentile. For children ≥13 year old, hypertension and elevated blood pressure are defined by absolute blood pressure measures consistent with adult blood pressure guidelines.14,15 Unlike in adults, in whom blood pressure cutoffs are based on morbidity and mortality data, in children, cutoffs are based on SDs from normative blood pressure data and expert opinion.14,15 Pediatric hypertension and elevated blood pressure are underdiagnosed and undertreated.16–18
Because large-scale, longitudinal studies of pediatric hypertension and elevated blood pressure based on routinely collected clinical data generally do not exist, the natural history of abnormal pediatric blood pressure levels obtained through routine clinical care have not been well studied. In this study, we examine longitudinal trajectories of blood pressure levels and the persistence of abnormal blood pressure levels over time as recorded in routine clinical practice. Such information could lead to pediatric hypertension diagnoses definition refinements and more nuanced evaluation and management guidelines.
Methods
The Data Set
We used the American Academy of Pediatrics Comparative Effectiveness Research through Collaborative Electronic Reporting (CER2) Consortium data.18,19 For this study, we extracted data from the electronic health records (EHRs) of 165 pediatric primary care sites among 30 health care systems. This cohort previously demonstrated significant underdiagnosis (only 23.2% of hypertension cases and 10.2% of prehypertension cases were diagnosed) and undertreatment (only 5.6% of patients who should have been prescribed an antihypertensive medication on the basis of pediatric hypertension guidelines were) of pediatric hypertension and so is ideally suited to study the natural history of abnormal blood pressure levels in pediatric populations.18,19 The blood pressure levels and other data in the EHRs used from the 30 different health care systems were not collected for research purposes, and we have no way of determining the methods of how the data were collected. However, all of the data used are actual data collected in pediatric primary care for which standards exist and primary care clinics that care for children have standard protocols and processes for blood pressure measurement.
Defining the Analysis Cohort
We identified all children ages 3 to 18 (age range at study entry was 3.0–13.6 years, and age range at study end was 6.5–18.9 years) with ≥72 months of observation between 1999 and 2016, with ≥3 separate visits with a blood pressure during the first 36-month period (period 1) and ≥3 separate visits with a blood pressure during the second 36-month period (period 2). Because accurate height information is required to interpret pediatric blood pressure measurements, implausible height measurements were excluded,20 and only blood pressure levels on the same day as a valid height were included. With these criteria, each child had the potential to meet hypertension or elevated blood pressure criteria in each of the two 36-month periods and thus could be assessed for persistence of these diagnoses over time. Children were defined as hypertensive if they had ≥3 visits in which either the diastolic blood pressure and/or systolic blood pressure was ≥95th percentile for age, height, and sex.21–23 For selected analyses, we identified the subgroup of children with stage 2 hypertension as having ≥3 blood pressure measurements ≥12 mm Hg above the 95th percentile. Children with ≥3 visits with blood pressure measurements ≥90th percentile but <95th percentile, based on age, height, and sex, were considered to have elevated blood pressure.21–23 (see Supplemental Information for methodology to calculate blood pressure levels in the stage 2 hypertensive range). For children ≥13 years old, we used ≥130/80 as the threshold for abnormal blood pressure. If the child had more than the required 3 blood pressure measurements during the period, only 3 were needed to meet the abnormal blood pressure criteria. Period 1 determined if a child met hypertension or elevated blood pressure criteria, and period 2 assessed whether blood pressure normalized, or diagnoses persisted. If a child had ≥3 abnormal blood pressure levels in period 1 but <3 abnormal blood pressure levels in period 2, they would not be considered to have hypertension or elevated blood pressure during period 2. We used the 2017 American Academy of Pediatrics blood pressure definitions for elevated blood pressure, hypertension, and stage 2 hypertension.15
Analysis
Our goal was to report descriptive statistics, and, for rates of hypertension, 95% confidence intervals. We used multinomial logistic regression (without covariates), with a separate regression for each combination of patient group (eg, by sex) and hypertension level in period 1. Each regression estimated the probabilities, given the period 1 level of hypertension, of 4 outcomes in period 2: normal blood pressure, elevated blood pressure, stage 1 hypertension, or stage 2 hypertension. We then translated the resulting odds to probabilities. Confidence intervals were calculated by using the δ method.24 Finally, statistical models adjusted all confidence bounds to reflect that the data arise from natural clusters formed by patients within clinical practice sites. Because our goal was to calculate variances and confidence intervals properly, our models did not adjust for covariates.
In our results, we deliberately avoid “statistical significance” statements, in keeping with the recent guidance from the American Statistical Association.25 Rather, our results are largely descriptive. The width and location of confidence intervals reflect the power of the analysis and the strength of evidence. In addition, we avoid formal statistical contrasts between subgroups of children defined by sex, age category (<10 and ≥10), and BMI percentile category (<85th percentile, 85th percentile to <95 percentile, ≥95th percentile) because of the multiplicity of possible comparisons and the absence of prespecified contrasts. All comparisons are therefore hypothesis generating.
Secondary Analyses: Follow-up for Patients With <3 Visits in the Second Period
After counting the number of visits in each of the two 36-month periods, we first limited the analysis to those children with ≥3 visits with blood pressure levels and heights per period. Second, we looked at children who had ≥3 visits with blood pressure levels and heights in the first period but <3 visits in the second period.
All statistical analysis was performed with SAS v9.4 (SAS Institute, Inc, Cary, NC) or Stata v15.1 (Stata Corp, College Station, TX) with robust confidence interval estimated by using the program “mlogit” with the “vce” and “cluster” options. The American Academy of Pediatrics Institutional Review Board (IRB) served as the primary IRB and additional local IRBs reviewed and approved this study. The Children’s Hospital of Philadelphia IRB determined that this study was not human subjects research.
Results
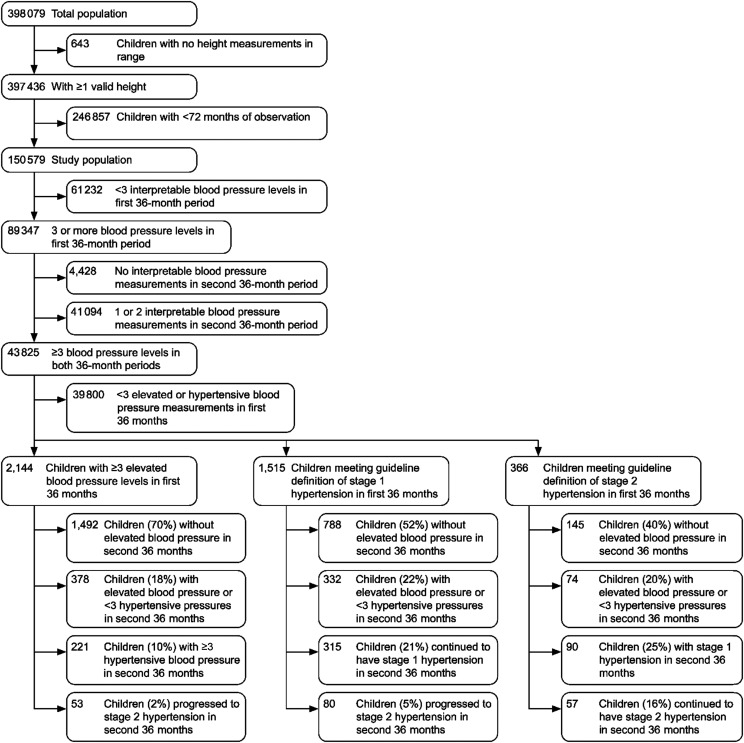
From our initial sample of 398 079 patients, 43 825 patients (11%) met study inclusion criteria (Fig 1). Of this cohort, 4.9% (2144) had elevated blood pressure and 4.3% (1881) were hypertensive (3.5% [1515] stage 1 and 0.8% [366] stage 2), with ≥3 blood pressure measurements during the first 36 months (period 1) (Fig 1). Characteristics of the overall sample compared with those included are described in Table 1. Frequency of included visits ranged from 3 visits per period (77% of all children) to 41 (only 7% of children had >6 visits during the 72 months).
FIGURE 1.
CONSORT (Consolidated Standards Of Reporting Trials) cohort and subsamples population flow diagram.
TABLE 1.
Patient Characteristics
| Original Sample (N = 397 436), n (%) | Final Cohort (N = 43 825), n (%) | |
|---|---|---|
| Male | 203 221 (51.1) | 23 390 (53.4) |
| Age at start of study,y | ||
| <9 | 279 234 (70.3) | 36 121 (82.4) |
| ≥9 | 118 202 (29.7) | 7704 (17.6) |
| BMI categories | ||
| BMI percentile <85th | 279 823 (70.3) | 31 949 (82.4) |
| BMI percentile ≥85th to <95th | 60 817 (15.3) | 6.484 (14.8) |
| BMI percentile ≥95th | 56 796 (14.3) | 5392 (12.3) |
| Race and ethnicity | ||
| White, not Hispanic | 156 888 (39.5) | 24 411 (55.7) |
| Black or African American, not Hispanic | 100 400 (25.3) | 10 588 (24.2) |
| Hispanic | 29 056 (7.3) | 2470 (5.6) |
| Other not Hispanic | 8220 (2.1) | 976 (2.2) |
| Unknown | 102 872 (25.9) | 5380 (12.3) |
| Percentage meeting criteria for elevated blood pressure | N/A | 2144 (4.9) |
| Hypertension | ||
| Percentage meeting criteria for stage 1 hypertension | N/A | 1515 (3.5) |
| Percentage meeting criteria for stage 2 hypertension | N/A | 366 (0.8) |
N/A, not available.
Of the 1515 children with stage 1 hypertension at the end of period 1, 52% (788) had their blood pressure normalize (ie, had <3 abnormal blood pressure levels), 22% (332) continued to meet criteria for elevated blood pressure but not hypertension, 21% (315) continued to have stage 1 hypertension, and 5% (80) went on to develop stage 2 hypertension by the end of period 2. In those 366 who met criteria for stage 2 hypertension by the end of period 1, persistence of hypertension was more common. Forty percent (145) had their blood pressure normalize, 20% (74) met criteria for elevated blood pressure, 25% (90) met criteria for on stage 1 hypertension, and 16% (57) continued to have stage 2 hypertension by the end of period 2. Among the 2144 children with elevated blood pressure in period 1, 70% (1492) had their blood pressure normalize in period 2 (ie, had <3 blood pressure levels). Another 18% (378) continued to have elevated blood pressure levels, 10% (221) went on to develop stage 1 hypertension and 2% (53) went on to develop stage 2 hypertension by the end of period 2 (Fig 1).
We also investigated patient factors (sex, age category, and BMI category) to describe the association of these factors with persistent blood pressure problems (Tables 2–4). Across groups with elevated blood pressure or stage 1 or stage 2 hypertension in period 1, point estimates for persistence of abnormal blood pressure levels were generally higher among older (≥10 years) versus younger children and among those with overweight or obesity versus normal-weight children. Many sample sizes for subanalyses were small with wide confidence intervals.
TABLE 2.
Among Patients With Stage 2 Hypertension at the End of the First 36 Months, Blood Pressure Diagnoses at the End of the Second 36 Months by Patient Characteristics
| Normal | Elevated | Stage 1 | Stage 2 | |||||
|---|---|---|---|---|---|---|---|---|
| Standardized % (95% CI) | n | Standardized % (95% CI) | n | Standardized % (95% CI) | n | Standardized % (95% CI) | n | |
| Overall | 39.6 (34.1–45.1) | 145 | 20.2 (16.5–23.9) | 74 | 24.6 (16.5–23.9) | 90 | 15.5 (12.6–18.6) | 57 |
| Sex | ||||||||
| Male | 36.9 (29.9–43.9) | 79 | 21.5 (16.8–26.2) | 46 | 25.7 (19.7–31.7) | 55 | 15.9 (10.5–21.3) | 34 |
| Female | 43.4 (36.7–50.1) | 66 | 18.4 (12.6–24.2) | 28 | 23.0 (17.8–28.3) | 35 | 15.1 (10.8–19.4) | 23 |
| Age | ||||||||
| <10 y | 41.9 (35.8–47.9) | 124 | 17.2 (13.7–20.7) | 51 | 26.0 (20.6–31.4) | 77 | 14.9 (10.7–19.0) | 44 |
| ≥10 y | 30 (20.6–39.4) | 21 | 32.9 (22.3–43.4) | 23 | 18.6 (10.7–26.4) | 13 | 18.6 (10.2–27.0) | 13 |
| BMI | ||||||||
| <85% | 45.7 (38.9–52.6) | 75 | 20.1 (15.6–24.7) | 33 | 23.2 (18.3–28.1) | 38 | 11.0 (6.4–15.6) | 18 |
| 85%–95% | 32.7 (18.3–47.1) | 18 | 20.0 (10.2–29.8) | 11 | 20.0 (8.6–31.4) | 11 | 27.3 (14.9–39.7) | 15 |
| >95% | 35.4 (28.4–42.3) | 52 | 20.4 (14.1–26.7) | 30 | 27.9 (22.1–33.7) | 41 | 16.3 (10.4–22.2) | 24 |
CI, confidence interval.
TABLE 4.
Among Patients With Elevated Blood Pressure at the End of the First 36 Months, Blood Pressure Diagnoses at the End of the Second 36 Months by Patient Characteristics
| Normal | Elevated | Stage 1 | Stage 2 | |||||
|---|---|---|---|---|---|---|---|---|
| Standardized % (95% CI) | n | Standardized % (95% CI) | n | Standardized % (95% CI) | n | Standardized % (95% CI) | n | |
| Overall | 69.6 (66.7–72.5) | 1492 | 17.6 (15.8–19.5) | 378 | 10.3 (8.2–12.4) | 221 | 2.5 (1.8–3.2) | 53 |
| Sex | ||||||||
| Male | 69.8 (66.2–73.4) | 890 | 17.3 (15.2–19.4) | 220 | 10.5 (8.1–12.9) | 134 | 2.4 (1.4–3.4) | 31 |
| Female | 69.3 (66.2–72.3) | 602 | 18.2 (15.4–20.9) | 158 | 10.0 (7.4–12.7) | 87 | 2.5 (1.6–3.4) | 22 |
| Age | ||||||||
| <10 y | 72.4 (69.0–75.9) | 1342 | 15.3 (13.4–17.1) | 283 | 10.1 (7.8–12.5) | 188 | 2.2 (1.5–2.8) | 40 |
| ≥10 y | 51.5 (45.9–57.2) | 150 | 32.6 (27.8–37.5) | 95 | 11.3 (7.2–15.5) | 33 | 4.5 (1.9–7.1) | 13 |
| BMI | ||||||||
| <85% | 74.0 (70.3–77.6) | 963 | 15.1 (12.7–17.6) | 197 | 9.0 (6.7–11.3) | 117 | 1.9 (1.2–2.7) | 25 |
| 85%–95% | 66.0 (61.3–70.8) | 243 | 18.8 (14.9–22.6) | 69 | 12.2 (8.7–15.8) | 45 | 3.0 (1.1–4.9) | 11 |
| >95% | 60.3 (54.7–66.0 | 286 | 23.6 (19.2–28.1) | 112 | 12.4 (9.4–15.5) | 59 | 3.6 (2.2–5.0) | 17 |
CI, confidence interval.
TABLE 3.
Among Patients With Stage 1 Hypertension at the End of the First 36 Months, Blood Pressure Diagnoses at the End of the Second 36 Months by Patient Characteristics
| Normal | Elevated | Stage 1 | Stage 2 | |||||
|---|---|---|---|---|---|---|---|---|
| Standardized % (95% CI) | n | Standardized % (95% CI) | n | Standardized % (95% CI) | n | Standardized % (95% CI) | n | |
| Overall | 52.0 (47.1–56.9) | 788 | 21.9 (20.2–23.6) | 332 | 20.8 (16.4–25.2) | 315 | 5.3 (4.3–6.2) | 80 |
| Sex | ||||||||
| Male | 50.5 (45.2–55.7) | 475 | 22.7 (20.6–24.9) | 214 | 21.1 (16.5–25.8) | 199 | 5.6 (4.1–7.1) | 53 |
| Female | 54.5 (49.2–59.9) | 313 | 20.6 (17.9–23.2) | 118 | 20.2 (15.3–25.1) | 116 | 4.7 (3.1–6.3) | 27 |
| Age | ||||||||
| <10 y | 53.8 (48.6–59.1) | 722 | 21.0 (19.1–22.9) | 282 | 20.2 (15.9–24.6) | 271 | 4.9 (3.9–5.9) | 66 |
| ≥10 y | 37.9 (30.9–44.9) | 66 | 28.7 (21.6–35.8) | 50 | 25.3 (15.7–34.9) | 44 | 8.0 (3.8–12.3) | 14 |
| BMI | ||||||||
| <85% | 54.5 (49.1–59.9) | 463 | 20.7 (17.7–23.8) | 176 | 20.7 (16.1–25.4) | 176 | 4.0 (2.7–5.3) | 34 |
| 85%–95% | 47.8 (39.5–56.1) | 120 | 24.3 (19.0–29.6) | 61 | 22.3 (13.9–30.8) | 56 | 5.6 (2.5–8.6) | 14 |
| >95% | 49.4 (43.7–55.1) | 205 | 22.9 (19.6–26.2) | 95 | 20.0 (15.4–24.6) | 83 | 7.7 (5.3–10.1) | 32 |
CI, confidence interval.
Our results also reveal that for many pediatric patients, even those with abnormal blood pressure levels, follow-up readings were not regularly obtained. Of the 398 079 primary care pediatric patients in our cohort, only 22.4% (89 347) had ≥3 blood pressure levels recorded during a 36-month period, and only 11.0% (43 825) had ≥3 blood pressure levels recorded during 2 consecutive 36-month periods. Patients with blood pressure problems in period 1 were more likely to have additional visits (beyond 2) in period 2 (49% (39 800 of 81 572) of those with normal blood pressure levels versus 52% (4025/7775) of those with elevated blood pressure levels or hypertension) (Table 5). The trend did increase with increasingly abnormal blood pressure category during period 1, with 50% (2144 of 4305) of patients with elevated blood pressure, 54% (1515 of 2821) with stage 1 hypertension, and 56% (366 of 649) with stage 2 hypertension receiving ≥3 blood pressure levels recorded during period 2 to fully assess their blood pressure status during period 2.
TABLE 5.
The Number of Patients With 0, 1, 2, 3, 4, and ≥5 Visits With Blood Pressure Measurements During the Second 36-Month Measurement Period, Among the 89 347 Patients With ≥3 Visits With Blood Pressure Measurement During the First 36-Month Measurement Period, According to the Blood Pressure Stage in the First 36-Month Period
| BP Stagea During the First 36 mo | 0, No. (Row %) | 1, No. (Row %) | 2, No. (Row %) | 3, No. (Row %) | 4, No. (Row %) | 5, or More No. (Row %) | Total Patients |
|---|---|---|---|---|---|---|---|
| Normal | 4053 (5) | 11 719 (14) | 26 000 (32) | 31 168 (38) | 4440 (5) | 4192 (5) | 81 572 |
| Elevated blood pressure | 207 (5) | 686 (16) | 1268 (29) | 1384 (32) | 290 (7) | 470 (11) | 4305 |
| Stage 1 hypertension | 136 (5) | 389 (14) | 781 (28) | 789 (28) | 215 (8) | 511 (18) | 2821 |
| Stage 2 hypertension | 32 (5) | 92 (14) | 159 (24) | 199 (31) | 50 (8) | 117 (18) | 649 |
| Total patients | 4428 | 12 886 | 28 208 | 33 540 | 4995 | 5290 | 89 347 |
BP, blood pressure.
See the text for the definitions of blood pressure staging.
Although this study was not designed to evaluate medication effectiveness, among the 120 hypertensive patients in period 1 prescribed an antihypertensive medication, patterns of blood pressure normalization were similar to the overall cohort. The equivalent analysis (data not shown) using the 2004 pediatric hypertension clinical practice guidelines showed fewer patients meeting criteria for hypertension (1.8%) and prehypertension (2.7%). However, rates of normalization were similar, with only 40% of hypertensive patients in period 1 remaining hypertensive in period 2 and only 10% meeting criteria for prehypertension. This left 50% of hypertensive patients in period 1 not meeting criteria for hypertension or prehypertension in period 2. Among the prehypertensive patients in period 1, 22% became hypertensive, 7% remained prehypertensive, and 71% no longer met criteria for prehypertension or hypertension.
Discussion
In this study, we demonstrate that over several years, most pediatric patients managed in primary care and initially meeting hypertension or elevated blood pressure criteria with 3 routinely collected, in-office blood pressure levels will not continue to meet criteria for hypertension or elevated blood pressure. This pattern of a return to lower blood pressure readings among children with periods of abnormal blood pressure levels has potentially important practice implications. This study also shows that many pediatric patients, even those with abnormal blood pressure levels, do not have follow-up blood pressure levels obtained even on an annual basis, as recommended by current and previous pediatric hypertension guidelines. Blood pressure levels were obtained through practice, not under a strict research protocol. As such, our findings from EHRs raise hypotheses regarding blood pressure measurement and follow-up that could be tested in future prospective studies.
Although we are unaware of previous studies in which researchers examined prevalence of persistent abnormal blood pressure levels in a similarly large primary care pediatric cohort of routinely collected in-office blood pressure levels, several other researchers have investigated aspects of this problem. In 1986, Shear et al26 evaluated persistent abnormal blood pressure levels over 8 years in ∼1500 children in the prospective Bogalusa Heart Study in which auscultated pressures were used. They showed that children with 3 serial blood pressure levels in the top quartile continued to remain in the upper quartile approximately 2/3 of the time and that 97% of children without 3 serial blood pressure levels in the top quartile continued to not have any blood pressure levels in the top quartile. In another study published in 2017 of almost 5600 patients (160 with hypertension) followed over 3 years, Daley et al27 developed a model to predict hypertension based on an initial single elevated blood pressure. The model pointed to systolic blood pressure, previous blood pressure levels, and BMI percentile as significant predictors, but the model did not work well at 2 other sites evaluated in the study, and overall, <20% of children with an initial abnormal blood pressure developed hypertension.27
Authors of several other studies either looking at single “incident” high blood pressure levels or the ≥3 abnormal blood pressure for a true hypertension diagnosis have shown that increasing BMI percentile is highly associated with abnormal blood pressure levels but did not track measures for as long as this study.22,28–31 Authors of the Falkner study, a prospective study in which auscultated pressures were used, showed 31% of boys and 26% of girls continued to exhibit hypertension (compared with our 22%), and 47% of boys and 26% of girls (compared with our 29%) moved from a hypertensive blood pressure level to a blood pressure level in the prehypertensive (Faulkner study) or elevated blood pressure (this study), although this study only had a 2-year follow-up, with a single second blood pressure measurement.22 Fourteen percent of boys and 12% of girls moved from having a single blood pressure level in the prehypertensive range to having a single blood pressure level in the hypertensive range, similar to our 13% moving from elevated blood pressure to hypertension.22 A meta-analysis by Juhola et al32 of 4 longitudinal pediatric blood pressure cohorts followed into adulthood revealed that ∼40% of children with ≥1 visit with an elevated blood pressure level did not have elevated blood pressure levels when measured as an adult (the other 60% did have ≥1 visit with an elevated blood pressure level as an adult or were on antihypertensive medication). Authors of all of these studies support the finding in this study that persistent abnormal blood pressure is hard to predict, and many children with abnormal blood pressure levels do not have persistently high blood pressure measurements.
Pediatric blood pressure guidelines historically and currently use a “one size fits all” approach for abnormal blood pressure evaluation and follow-up in children ≥3 years old. Our analysis suggests that if the current guidelines were followed and everyone with ≥3 abnormal blood pressure levels were additionally evaluated and managed, significant additional testing and workup would be done in a large cohort of pediatric patients, many of whose blood pressure levels will normalize over time without intervention. Although prospective testing of this hypothesis is warranted, especially with high-risk groups and with research-level measurement, continued routine well-child care or annual blood pressure screening, potentially coupled with standard lifestyle guidance, may be sufficient in many patients. Even larger samples than our own with more complete data are needed to fully evaluate which patients are more likely to have persistent blood pressure problems. Our results also suggest that more nuanced evaluation and management algorithms may be important because the 2017 pediatric hypertension guidelines, although they recommend limiting screening to preventive well-child care visits, also take out children with weight problems from the normative blood pressure tables. This change in the normative blood pressure tables decreases the cutoffs for abnormal blood pressure levels, so significantly more children are identified as having abnormal blood pressure levels.33
Our results also raise the hypothesis that modifying the diagnostic criteria for abnormal blood pressure diagnoses in children may also help in identifying those likely to have persistent abnormalities. Unlike the pediatric definition of hypertension that requires having 3 abnormal blood pressure measurements,15,34 the adult definition of hypertension requires 2 abnormal blood pressure measurements and that the average of blood pressure measurements after the 2 abnormal measurements also be high.35,36 The low rates of persistent hypertension and elevated blood pressure in the current study (which also occurs when the analysis is done by using the 2004 pediatric hypertension clinical practice guidelines) highlights the potential value and need for a more nuanced definition of pediatric hypertension that might include measurement averaging across visits. The adoption of a methodology that averages readings across visits may also be helpful in practice because most pediatric hypertension is undiagnosed and many abnormal and normal blood pressure measurements may exist, especially in younger and shorter children, before any abnormal blood pressure levels are recognized.37
This study has several limitations. First, only ∼10% of our original cohort of almost 400 000 children had enough longitudinal blood pressure measurements to be included in our study. This selection process favored the inclusion of younger children who have more visits. Second, the blood pressure measurements were extracted from many different EHRs with no way to know if they were obtained according to guideline measurement standards. We do not know if multiple blood pressure measurements were made, if any blood pressure averaging was done, if the patient was sitting or standing, or if measurements were oscillometric or auscultatory. In addition, multiple pediatric hypertension guidelines were in place during the study period. However, the overall prevalence of hypertension and abnormal blood pressure (≥90th percentile) measured in this population (4.3% and 4.9% respectively) is only slightly higher than that measured in other studies that more rigorously measure blood pressure, showing hypertension and abnormal blood pressure rates of between 0.3% and 2.1% and 2.8% and 4.5%, respectively, using different abnormal blood pressure definitions that did not take out children with weight problems.1,2,4,5 Also, a recent review and meta-analysis of oscillometric and auscultatory blood pressure measurements showed that systolic oscillometric blood pressure measurements were on average only 2.53 mm Hg higher than auscultatory blood pressure measurements, and diastolic blood pressure measures were statistically the same. The review authors concluded that oscillometric devices may serve as a suitable alternative to auscultation for initial blood pressure screening in pediatric populations.38 Another limitation of this study is that none of the measurements or analysis presented here consider the growing recommendations for an increased role for ambulatory blood pressure measurements in assessment of abnormal blood pressure,39–42 and we cannot determine from our data set if ambulatory blood pressure measurements were ordered or obtained. Additionally, lifestyle changes are incompletely documented in EHRs; therefore, we were unable to assess the impact of lifestyle changes on blood pressure. However, hypertension and elevated blood pressure are underdiagnosed (>80% undiagnosed) in this population18 and generally, so it is unlikely in children with undiagnosed hypertension that specific blood pressure lowering lifestyle interventions are being consistently applied to address an undocumented problem. With respect to the antihypertensive medication analysis, although patterns of blood pressure normalization were similar among children whether they were receiving antihypertensive medication or not, this was a small sample, and this study was not designed to evaluate the effectiveness of these medications. Finally, although we started with hundreds of thousands of pediatrics patients, because of the low prevalence of blood pressure problems, low diagnosis rate, low medications prescriptions,18 and poor long-term follow-up, determining risk factors for persistent abnormal blood pressure levels (including impact of antihypertensive medications) was impossible. Future prospective long-term studies, potentially focused on those at high-risk and followed for longer periods, will be helpful and could be facilitated by the increasing EHR use.
Conclusions
Most children with many blood pressure level measurements who initially meet criteria for hypertension or elevated blood pressure do not continue to meet criteria for hypertension or elevated blood pressure. In our cohort, abnormal blood pressure measurements during a 36-month baseline period were poorly predictive of future hypertension or elevated blood pressure. Additionally, many children, even with stage 2 hypertension, did not have recommended follow-up blood pressure measurements. These hypothesis-generating findings suggest that office-based blood pressure measurements alone may not be sufficient to determine which pediatric patients will have persistently abnormal blood pressure levels. On the basis of these findings, future pediatric hypertension clinical practice guidelines should consider recommending a more nuanced approach to the 3-abnormal-blood-pressures definition of pediatric hypertension, as well as to other approaches to the evaluation and management of these patients. Guidelines should continue to stress the need for routine blood pressure collection, especially in children with some abnormal blood pressure measures. Although many children’s blood pressure will normalize over time, some will not, so it continues to be important that pediatric hypertension clinical practice guidelines be followed. Future prospective studies will be helpful in confirming the findings here and their implications for practice, especially among higher-risk children.
Acknowledgments
We thank additional members of the CER2 Consortium Research Team: Bill Adams and Boston Medical Center, Jennifer Carroll for the American Academy of Family Physicians National Research Network, and Marc Rosenman for Eskenazi Health System for supporting CER2. We would also specifically acknowledge Laura Shone, DrPH MSW and Margaret Wright, PhD for their help with supporting the CER2 Consortium.
Glossary
- CER2
Comparative Effectiveness Research through Collaborative Electronic Reporting
- EHR
electronic health record
- IRB
Institutional Review Board
Footnotes
Dr Kaelber conceptualized and designed the study, assisted in obtaining data, drafted the initial manuscript, and reviewed the manuscript; Dr Localio helped design the study, led and helped conduct data analyses, helped draft the initial manuscript, and reviewed the manuscript; Dr Ross helped design the study, helped conduct data analyses, and reviewed the manuscript; Ms Leon helped design the study, assisted in obtaining data, drafted the initial manuscript, and reviewed the manuscript; Dr Pace helped design the study, assisted in obtaining data, and reviewed the manuscript; Dr Wasserman helped conceptualize and design the study, assisted in obtaining data, and reviewed the manuscript; Dr Grundmeier helped conceptualize and design the study, assisted in obtaining data, and reviewed the manuscript; Ms Steffes assisted in obtaining the data, and reviewed the manuscript; Dr Fiks helped conceptualize and design the study, assisted in obtaining data, drafting the initial manuscript, and reviewed the manuscript; The Comparative Effectiveness Research through Collaborative Electronic Reporting Consortium reviewed the study design and coordinated and supervised data collection at each Collaborative Electronic Reporting site; and all authors revised and approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: Dr Fiks received an Independent Research Grant from Pfizer for work unrelated to this project. He received no personal salary support.
FUNDING: Supported by the Health Resources and Services Administration of the US Department of Health and Human Services under grant R40MC24943: “Primary Care Drug Therapeutics CER in a Pediatric EHR Network,” and grant UB5MC20286: “Pediatric Primary Care Electronic Health Record (EHR) Network for Comparative Effectiveness Research (CER).” Further support was provided by the Agency for Healthcare Research and Quality under grant P30HS021645:”National Center for Pediatric Practice Based Research and Learning.” Funding was also provided by the Eunice Kennedy Shriver National Institute of Child Health and Human Development under the Best Pharmaceuticals for Children Act. Additional infrastructure funding was provided by the American Academy of Pediatrics. This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by the American Academy of Pediatrics, Agency for Healthcare Research and Quality, Health and Human Services, Health Resources and Services Administration, National Institute of Child Health and Human Development or the US Government. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2020-018481.
References
- 1.Moore WE, Stephens A, Wilson T, Wilson W, Eichner JE. Body mass index and blood pressure screening in a rural public school system: the Healthy Kids Project. Prev Chronic Dis. 2006;3(4):A114. [PMC free article] [PubMed] [Google Scholar]
- 2.Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ. Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics. 2004;113(3, pt 1):475–482 [DOI] [PubMed] [Google Scholar]
- 3.Ford ES, Mokdad AH, Ajani UA. Trends in risk factors for cardiovascular disease among children and adolescents in the United States. Pediatrics. 2004;114(6):1534–1544 [DOI] [PubMed] [Google Scholar]
- 4.Koebnick C, Black MH, Wu J, et al. The prevalence of primary pediatric prehypertension and hypertension in a real-world managed care system. J Clin Hypertens (Greenwich). 2013;15(11):784–792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lo JC, Sinaiko A, Chandra M, et al. Prehypertension and hypertension in community-based pediatric practice. Pediatrics. 2013;131(2). Available at: www.pediatrics.org/cgi/content/full/131/2/e415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berenson GS, Srinivasan SR, Bao W, Newman WP III, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med. 1998;338(23):1650–1656 [DOI] [PubMed] [Google Scholar]
- 7.Arnett DK, Glasser SP, McVeigh G, et al. Blood pressure and arterial compliance in young adults: the Minnesota Children’s Blood Pressure Study. Am J Hypertens. 2001;14(3):200–205 [DOI] [PubMed] [Google Scholar]
- 8.Burke GL, Arcilla RA, Culpepper WS, Webber LS, Chiang YK, Berenson GS. Blood pressure and echocardiographic measures in children: the Bogalusa Heart Study. Circulation. 1987;75(1):106–114 [DOI] [PubMed] [Google Scholar]
- 9.Johnson MC, Bergersen LJ, Beck A, Dick G, Cole BR. Diastolic function and tachycardia in hypertensive children. Am J Hypertens. 1999;12(10 pt 1):1009–1014 [DOI] [PubMed] [Google Scholar]
- 10.Knoflach M, Kiechl S, Kind M, et al. Cardiovascular risk factors and atherosclerosis in young males: ARMY study (Atherosclerosis Risk-Factors in Male Youngsters). Circulation. 2003;108(9):1064–1069 [DOI] [PubMed] [Google Scholar]
- 11.Hanevold C, Waller J, Daniels S, Portman R, Sorof J; International Pediatric Hypertension Association . The effects of obesity, gender, and ethnic group on left ventricular hypertrophy and geometry in hypertensive children: a collaborative study of the International Pediatric Hypertension Association [published correction appears in Pediatrics 2005;115(4):1118]. Pediatrics. 2004;113(2):328–333 [DOI] [PubMed] [Google Scholar]
- 12.Theodore RF, Broadbent J, Nagin D, et al. Childhood to early-midlife systolic blood pressure trajectories: early-life predictors, effect modifiers, and adult cardiovascular outcomes. Hypertension. 2015;66(6):1108–1115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008;117(25):3171–3180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.U.S. Preventive Services Task Force. Final recommendation statement: blood pressure in children and adolescents (hypertension): screenling. 2016. Available at: https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/blood-pressure-in-children-and-adolescents-hypertension-screening. Accessed April 28, 2018
- 15.Flynn JT, Kaelber DC, Baker-Smith CM, et al. ; Subcommittee on Screening and Management of High Blood Pressure in Children . Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140(3):e20171904. [DOI] [PubMed] [Google Scholar]
- 16.Brady TM, Solomon BS, Neu AM, Siberry GK, Parekh RS. Patient-, provider-, and clinic-level predictors of unrecognized elevated blood pressure in children. Pediatrics. 2010;125(6). Available at: www.pediatrics.org/cgi/content/full/125/6/e1286 [DOI] [PubMed] [Google Scholar]
- 17.Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. JAMA. 2007;298(8):874–879 [DOI] [PubMed] [Google Scholar]
- 18.Kaelber DC, Liu W, Ross M, et al. ; Comparative Effectiveness Research Through Collaborative Electronic Reporting (CER2) Consortium . Diagnosis and medication treatment of pediatric hypertension: a retrospective cohort study. Pediatrics. 2016;138(6):e20162195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fiks AG, Grundmeier RW, Steffes J, et al. ; Comparative Effectiveness Research Through Collaborative Electronic Reporting (CER2) Consortium. Comparative effectiveness research through a collaborative electronic reporting consortium. Pediatrics. 2015;136(1). Available at: www.pediatrics.org/cgi/content/full/136/1/e215 [DOI] [PubMed] [Google Scholar]
- 20.Daymont C, Ross ME, Russell Localio A, Fiks AG, Wasserman RC, Grundmeier RW. Automated identification of implausible values in growth data from pediatric electronic health records. J Am Med Inform Assoc. 2017;24(6):1080–1087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.BernardRosner. Pediatric blood pressure. Available at: https://sites.google.com/a/channing.harvard.edu/bernardrosner/pediatric-blood-press. Accessed June 26, 2019
- 22.Falkner B, Gidding SS, Portman R, Rosner B. Blood pressure variability and classification of prehypertension and hypertension in adolescence. Pediatrics. 2008;122(2):238–242 [DOI] [PubMed] [Google Scholar]
- 23.Rosner B, Cook N, Portman R, Daniels S, Falkner B. Determination of blood pressure percentiles in normal-weight children: some methodological issues. Am J Epidemiol. 2008;167(6):653–666 [DOI] [PubMed] [Google Scholar]
- 24.Oehlert GW. A note on the Delta Method. The American Statistician. 1992;46(1):27–29 [Google Scholar]
- 25.Wasserstein RL, Schirm AL, Lazar NA. Moving to a world beyond “p < 0.05”. Am Stat. 2019;73(sup1):1–19 [Google Scholar]
- 26.Shear CL, Burke GL, Freedman DS, Berenson GS. Value of childhood blood pressure measurements and family history in predicting future blood pressure status: results from 8 years of follow-up in the Bogalusa Heart Study. Pediatrics. 1986;77(6):862–869 [PubMed] [Google Scholar]
- 27.Daley MF, Reifler LM, Johnson ES, et al. Predicting hypertension among children with incident elevated blood pressure. Acad Pediatr. 2017;17(3):275–282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Daley MF, Sinaiko AR, Reifler LM, et al. Patterns of care and persistence after incident elevated blood pressure. Pediatrics. 2013;132(2). Available at: www.pediatrics.org/cgi/content/full/132/2/e349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lo JC, Chandra M, Sinaiko A, et al. Severe obesity in children: prevalence, persistence and relation to hypertension. Int J Pediatr Endocrinol. 2014;2014(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maring B, Greenspan LC, Chandra M, et al. Comparing US paediatric and adult weight classification at the transition from late teenage to young adulthood. Pediatr Obes. 2015;10(5):371–379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parker ED, Sinaiko AR, Kharbanda EO, et al. Change in weight status and development of hypertension. Pediatrics. 2016;137(3):e20151662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Juhola J, Magnussen CG, Berenson GS, et al. Combined effects of child and adult elevated blood pressure on subclinical atherosclerosis: the International Childhood Cardiovascular Cohort Consortium. Circulation. 2013;128(3):217–224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sharma AK, Metzger DL, Rodd CJ. Prevalence and severity of high blood pressure among children based on the 2017 American Academy of Pediatrics Guidelines. JAMA Pediatr. 2018;172(6):557–565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2, suppl 4th report):555–576 [PubMed] [Google Scholar]
- 35.Chobanian AV, Bakris GL, Black HR, et al. ; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee . The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572 [DOI] [PubMed] [Google Scholar]
- 36.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–520 [DOI] [PubMed] [Google Scholar]
- 37.van Schalkwyk JM, Turner MJ. Diagnosing hypertension in children and adolescents. JAMA. 2008;299(2):168; author reply 168-169 [DOI] [PubMed] [Google Scholar]
- 38.Duncombe SL, Voss C, Harris KC. Oscillometric and auscultatory blood pressure measurement methods in children: a systematic review and meta-analysis. J Hypertens. 2017;35(2):213–224 [DOI] [PubMed] [Google Scholar]
- 39.Flynn JT, Daniels SR, Hayman LL, et al. ; American Heart Association Atherosclerosis, Hypertension and Obesity in Youth Committee of the Council on Cardiovascular Disease in the Young . Update: ambulatory blood pressure monitoring in children and adolescents: a scientific statement from the American Heart Association. Hypertension. 2014;63(5):1116–1135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lurbe E, Agabiti-Rosei E, Cruickshank JK, et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens. 2016;34(10):1887–1920 [DOI] [PubMed] [Google Scholar]
- 41.Salice P, Ardissino G, Zanchetti A, et al. Age-dependent differences in office (OBP) vs ambulatory blood pressure monitoring (ABPM) in hypertensive children and adolescents: 8C.03. J Hypertens. 2010;28:e423–e424 [Google Scholar]
- 42.Stergiou GS, Alamara CV, Salgami EV, Vaindirlis IN, Dacou-Voutetakis C, Mountokalakis TD. Reproducibility of home and ambulatory blood pressure in children and adolescents. Blood Press Monit. 2005;10(3):143–147 [DOI] [PubMed] [Google Scholar]