In this article, we integrate findings from the MUSP, a 2-decade longitudinal study assessing outcomes associated with different subtypes of child maltreatment.
Abstract
Video Abstract
Potential long-lasting adverse effects of child maltreatment have been widely reported, although little is known about the distinctive long-term impact of differing types of maltreatment. Our objective for this special article is to integrate findings from the Mater-University of Queensland Study of Pregnancy, a longitudinal prenatal cohort study spanning 2 decades. We compare and contrast the associations of specific types of maltreatment with long-term cognitive, psychological, addiction, sexual health, and physical health outcomes assessed in up to 5200 offspring at 14 and/or 21 years of age. Overall, psychological maltreatment (emotional abuse and/or neglect) was associated with the greatest number of adverse outcomes in almost all areas of assessment. Sexual abuse was associated with early sexual debut and youth pregnancy, attention problems, posttraumatic stress disorder symptoms, and depression, although associations were not specific for sexual abuse. Physical abuse was associated with externalizing behavior problems, delinquency, and drug abuse. Neglect, but not emotional abuse, was associated with having multiple sexual partners, cannabis abuse and/or dependence, and experiencing visual hallucinations. Emotional abuse, but not neglect, revealed increased odds for psychosis, injecting-drug use, experiencing harassment later in life, pregnancy miscarriage, and reporting asthma symptoms. Significant cognitive delays and educational failure were seen for both abuse and neglect during adolescence and adulthood. In conclusion, child maltreatment, particularly emotional abuse and neglect, is associated with a wide range of long-term adverse health and developmental outcomes. A renewed focus on prevention and early intervention strategies, especially related to psychological maltreatment, will be required to address these challenges in the future.
Child maltreatment is a major public health issue worldwide, with serious and often debilitating long-term consequences for psychosocial development as well as physical and mental health.1 In the United States alone, 3.5 million children are reported for suspected maltreatment each year, with an annual substantiated maltreatment rate of 9.1 per 1000 children.2 Some of the long-term adverse outcomes associated with maltreatment include cognitive disability, anxiety and depression, psychosis, teen-aged pregnancy, addiction disorders, obesity, and cardiovascular disease.3 Understanding the distinctive impact of differing types of maltreatment may help medical professionals provide more wholistic care and treatment recommendations as well as identify more specific public health targets for primary prevention.
Unfortunately, however, little is known about the long-term effects of differing types of child maltreatment, which include sexual abuse, physical abuse, emotional abuse, and neglect.4 According to a meta-analysis review,5 research on child maltreatment has predominantly been focused on sexual abuse, with far less attention paid to psychological maltreatment (emotional abuse and/or neglect) and the co-occurrence of different types of maltreatment. In addition, most of the current evidence is derived from cross-sectional studies, which may be subject to recall bias,6–8 in which an outcome status (such as depression) may influence recall of the exposure (ie, previous maltreatment). Few previous studies have adequately controlled for confounding variables, such as perinatal risk, socioeconomic adversity, parental psychopathology, and impaired early childhood development, which may predispose to both child maltreatment and later adverse health outcomes.
Longitudinal studies offer evidence that is more robust, but these studies are relatively few in number and have generally been limited to certain sociodemographic groups9 or to specific types of child maltreatment, such as sexual abuse.1,10 Other longitudinal studies have relied on retrospective recall of maltreatment rather than prospectively collected agency-reported data.11–13 In studies in which prospective data have been collected,7,13–17 only a few have compared different types of child maltreatment.7,16,17
In this special article, we review findings from the Mater-University of Queensland Study of Pregnancy (MUSP), a now 40-year longitudinal prenatal cohort study from Brisbane, Australia, involving >7000 women and their children.18 Unique features of the MUSP include its use of a population-based sample, its use of prospectively substantiated child maltreatment reports, and its consideration of different subtypes of maltreatment. In addition, the study design controlled for a wide range of confounders and covariates, including both maternal and child sociodemographic and mental health variables. This combined body of work, which includes numerous publications over the past decade, has documented a broad range of adverse outcomes associated with child maltreatment, including deficits in cognitive and educational outcomes19–21; mental health problems, such as anxiety, depression, posttraumatic stress disorder (PTSD), psychosis, delinquency, and intimate partner violence (IPV)22–25; substance abuse and addiction26–30; sexual health problems31; physical growth and health deficits32–35; and overall decreased quality of life.36
Our purpose for this special article is to compare the effects of 4 differing types of maltreatment on long-term cognitive, psychological, addiction, and health outcomes assessed in the offspring at ∼14 and/or 21 years of age. Rather than providing a systematic review or meta-analysis of the current literature, which would include diverse study designs and purposes, we report and compare the findings of individual articles that used a common data set and standard methodology to study a broad array of outcomes. We particularly highlight the long-term impact of emotional abuse and neglect, which has received far less attention in the literature.
Methods
Description of the MUSP Cohort
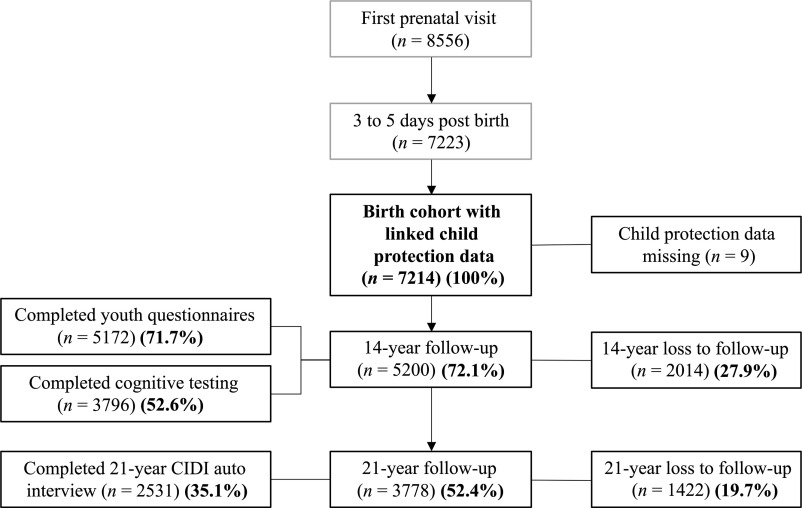
Between 1981 and 1983, 8556 consecutive pregnant women who attended their first prenatal clinic visit at the Mater Mothers’ Hospital in Brisbane, Australia, agreed to participate (Fig 1). After excluding mothers who did not deliver a singleton infant at the Mater Mothers’ Hospital or withdrew consent, the MUSP birth cohort consisted of 7223 mother-infant dyads, who were followed over 2 decades: at 3 to 5 days, 6 months, 5 years, 14 years and 21 years. Midway through the study, this rich data set was anonymously linked to state reports of child abuse and neglect, which identified some form of suspected maltreatment in >10% of cases.37 Notified cases, which had been referred from the community or by general medical practitioners, were investigated by the Queensland government child protection agency. Substantiated maltreatment was determined after a formal investigation when there was “reasonable cause to believe that the child had been, was being, or was likely to be abused or neglected.”38 Substantiated maltreatment occurred when a notified case was confirmed for (1) sexual abuse, “exposing a child to or involving a child in inappropriate sexual activities”; (2) physical abuse, “any non-accidental physical injury inflicted by a person who had care of the child”; (3) emotional abuse, “any act resulting in a child suffering any kind of emotional deprivation or trauma”; or (4) neglect, “failure to provide conditions that were essential for the healthy physical and emotional development of a child,” which encompassed physical, emotional and medical neglect.37
FIGURE 1.
Overview of the MUSP enrollment and testing.
Inclusion Criteria for Original Research Publications
We searched PubMed from inception to April 2020 for published MUSP articles in which agency-reported child maltreatment was evaluated as the predictor of a range of outcomes. Studies needed to meet the following criteria for inclusion in the review: (1) notified or substantiated abuse and neglect was listed as a main predictor variable and (2) outcomes included standardized measurements of cognitive, psychological, behavioral, or health functioning. From ∼340 published MUSP studies, we identified 24 articles dealing with child maltreatment, of which 21 included state-reported maltreatment versus self-reported maltreatment data (n = 3). Nineteen of the 21 articles met all inclusion criteria and were evaluated in this review (Fig 2). One study was excluded because it only examined outcomes associated with sexual abuse.8 Another article was excluded because its outcome measures were similar to another included study.29
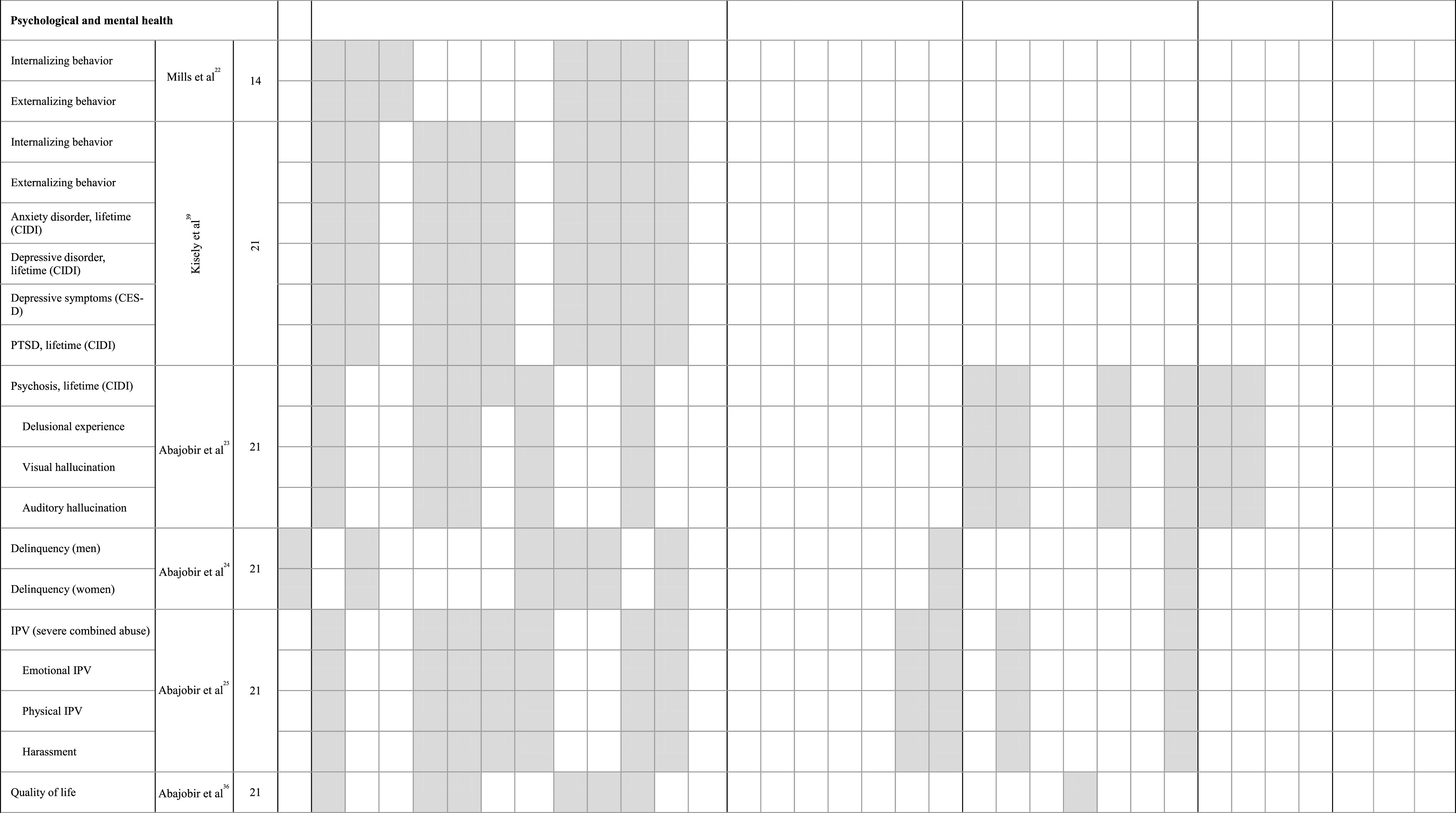
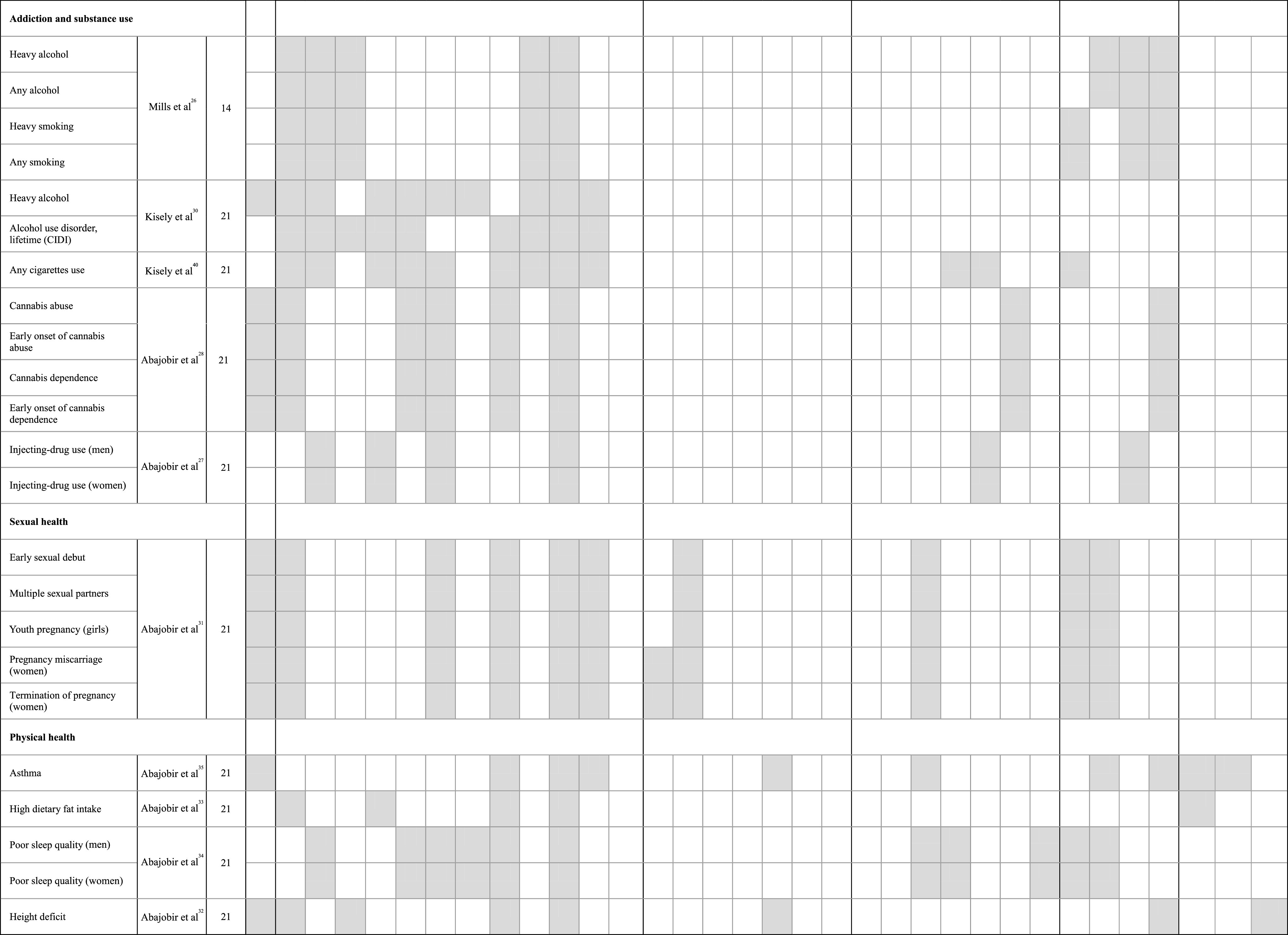
FIGURE 2.
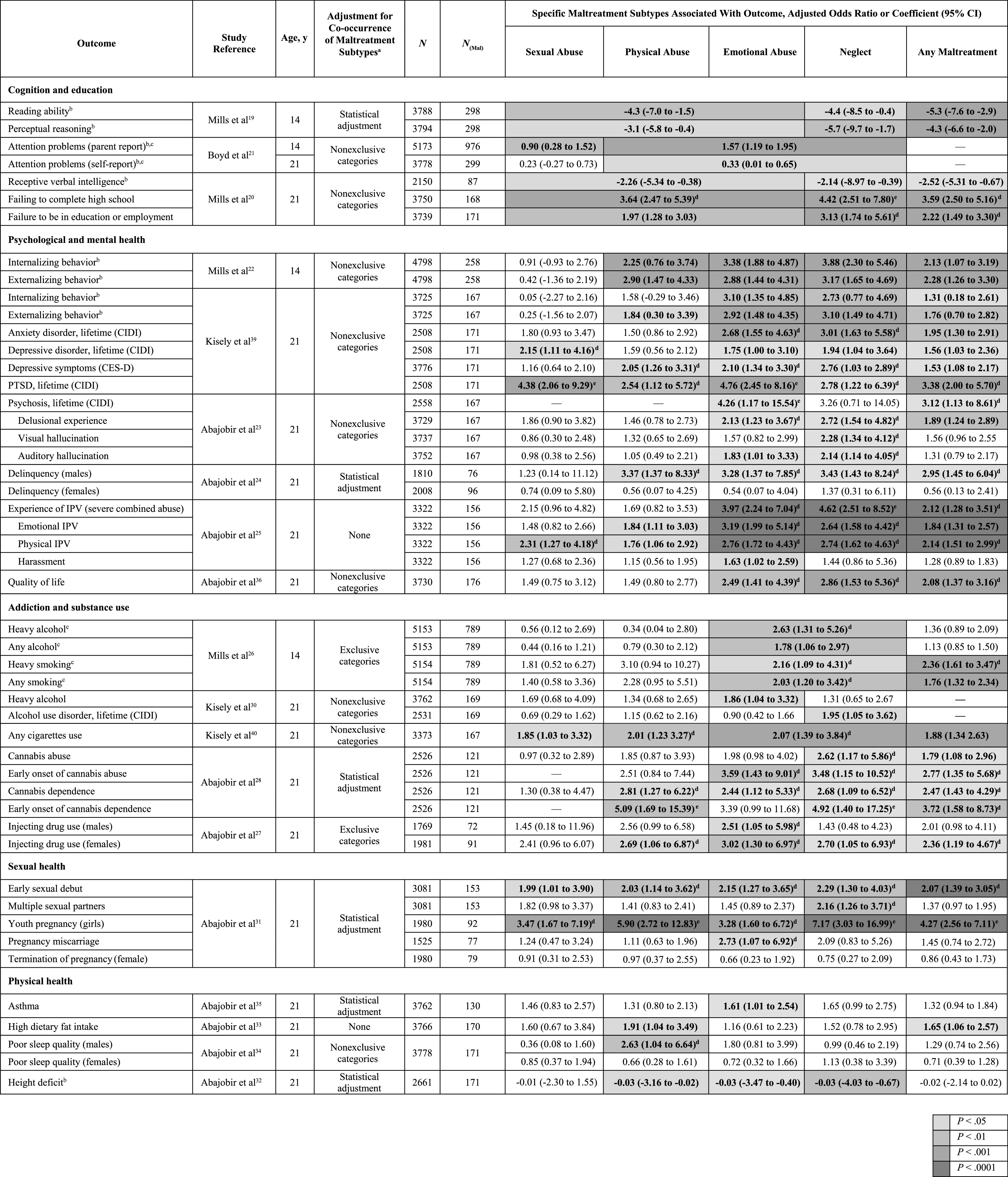
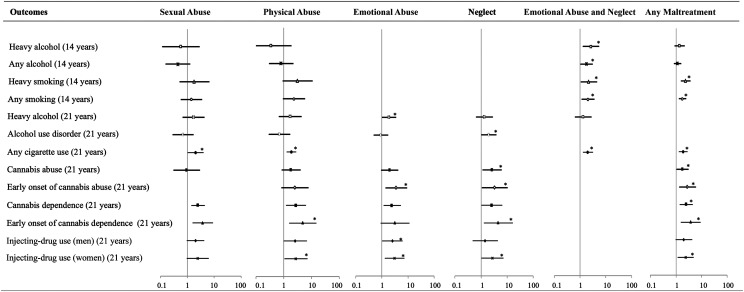
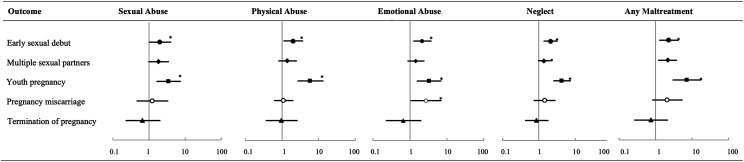
Published studies from the Mater-University of Queensland Study of Pregnancy, linking long-term outcomes with specific maltreatment subtypes (adjusted coefficients or odds ratios ± 95% confidence intervals). CES-D, Center for Epidemiologic Studies–Depression Scale; CI, confidence interval; N, number of offspring in sample; N(Mal), number of offspring who experienced maltreatment. aIn different articles adjusting for co-occurrence of maltreatment subtypes was handled in different ways: (1) statistical adjustment: each maltreatment subtype predictor was statistically adjusted for the other maltreatment subtypes (eg, neglect was adjusted for the occurrence of physical, sexual, and emotional abuse) and is reflected in the table’s odds ratios and coefficients; (2) exclusive categories: different combinations of maltreatment types are included in mutually exclusive groups (eg, physical abuse only, physical abuse and emotional abuse only, physical and emotional abuse and neglect [without sexual abuse], etc; see Table 1); (3) nonexclusive categories: maltreatment categories may overlap with other categories (eg, any substantiated abuse [sexual, physical, or emotional] versus any substantiated neglect); and (4) none: no statistical adjustments or combined categories were presented for co-occurring maltreatment subtypes. bAdjusted coefficients (95% CI) were reported as statistical association measures rather than adjusted odds ratios. cCases of notified (rather than substantiated) maltreatment. In the study by Mills et al,26 a sensitivity analysis was performed after exclusion of unsubstantiated cases of maltreatment. The associations between any maltreatment and substance use were similar to those seen in the original analysis after full adjustment. dMedium effect size, based on magnitude of the adjusted odds ratio (2 ≤ odds ratio ≤ 4). eLarge effect size, based on magnitude of the adjusted odds ratio (odds ratio > 4).
Quality of Supporting Literature
Each of the reviewed articles followed Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for the conduct of cohort studies.41 The quality of the studies was also evaluated by using a modified version of the Newcastle-Ottawa Scale, which is used to assess the following domains: sample representativeness and size, comparability between respondents and nonrespondents, ascertainment of outcomes, and statistical quality.42 On the basis of this assessment, all of the MUSP studies were determined to be of low risk of bias, with a score of 4 out of 5 points (Supplemental Information).
Predictors: Maltreatment Types
In all but 2 studies (which used notified maltreatment21,26) events were dichotomized and coded as substantiated maltreatment versus no substantiated maltreatment. According to a validated classification of maltreatment types,43 specific categories and co-occurring forms of childhood maltreatment44 were used to predict outcomes. In 2 studies,19,20 all types of abuse were combined into 1 category and compared to neglect, whereas in another study, sexual abuse was compared to any combination of nonsexual maltreatment.21 In 2 other studies,26,40 emotional abuse and neglect (examples of psychological maltreatment) were combined, partly because of overlapping definitional constructs from the government child protection agency (emotional abuse included “emotional deprivation,” and neglect included the failure to provide for “healthy…emotional development”). In all but 2 of the included articles,25,33 co-occurrence of different types of maltreatment was considered, either by examining specific combinations of maltreatment types (in exclusive or nonexclusive overlapping categories) or by statistically adjusting for all remaining types of maltreatment (Fig 2).
Covariates
All of the odds ratios, mean differences, or coefficients were adjusted for potential confounding variables (Fig 3). All articles adjusted for a variety of sociodemographic variables, such as age, race, education, income, and marital status. Perinatal and/or childhood factors, such as birth weight, gestational age, and breastfeeding status, were used as covariates, particularly in articles in which cognitive and educational outcomes were examined. Psychological and mental health variables (such as internalizing and externalizing behavior problems, maternal depression, chronic stress, or exposure to violence) were primarily included as covariates in mental health outcome studies, especially for psychosis. Addiction studies adjusted for youth and maternal alcohol or tobacco use, among other covariates, and physical health outcome studies adjusted for relevant covariates (such as BMI in a study of dietary fat intake and parental height when studying offspring height). In selected articles, maltreatment subtypes were also statistically adjusted for the other types of maltreatment to determine independent effects.
FIGURE 3.
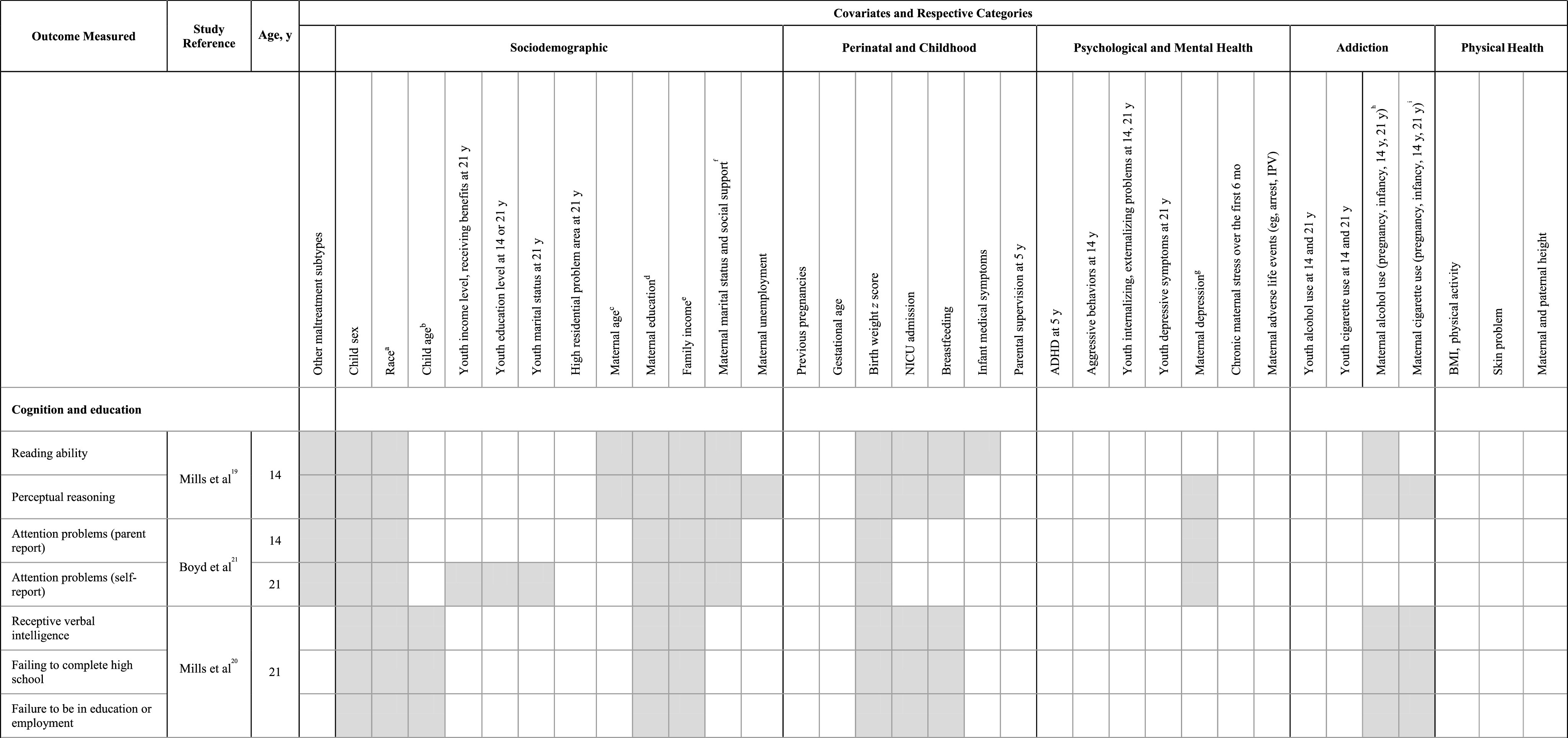
Covariates used in published articles from the MUSP to adjust for possible confounding. a Race: child’s race, parental race, and maternal or paternal racial origin at pregnancy. b Child age: child age and gestational age. c Maternal age: maternal age at the first visit clinic or at pregnancy. d Maternal education: maternal education (prenatal or at birth). e Family income: annual family income, familial income over the first 5 years or family poverty before birth or over the first 5 years of life, family income before birth, and annual family income. f Maternal marital status and social support: same partner at birth and 14 years and social support at 5 years. g Maternal depression: maternal depression during pregnancy, 3- to 6-month follow-up, or 21-year follow-up; chronic maternal depression. h Maternal alcohol use: maternal alcohol use at 3- to 6-month or 14-year follow-up and binge drinking. i Maternal cigarette use: cigarette use during pregnancy, 6 months postpartum, or at 14-year follow-up. ADHD, attention-deficit/hyperactivity disorder; CES-D, Center for Epidemiologic Studies–Depression Scale; IPV, intimate partner violence. Covariates used in published articles from the MUSP to adjust for possible confounding.
Outcomes
A total of 46 outcomes were assessed at 14 years (n = 5200) and/or 21 years (n = 3778) (Fig 1) and were grouped into 5 domains (Fig 2):
Cognition and education outcomes included reading ability and perceptual reasoning measured in adolescence, and, at age 21, receptive verbal intelligence and failure to complete high school or be either enrolled in school or employed; attention problems were measured at both time points.
Psychological and mental health outcomes at 21 years included internalizing and externalizing behavior problems (which were also assessed at 14 years), lifetime anxiety disorder, depressive disorder and symptoms, PTSD, lifetime psychosis diagnosis, psychotic symptoms (such as delusional experience or visual and/or auditory hallucinations), delinquency, experience of IPV or harassment, and overall quality of life.
Addiction and substance use, measured at both time points, included alcohol and cigarette use at 14 and 21 years, and cannabis abuse and/or dependence (including early onset) and injecting-drug use at the 21-year follow-up.
Sexual health was investigated at age 21 in terms of early initiation of sexual experience, having multiple sexual partners, youth pregnancy, and miscarriage or termination.
Physical health outcomes measured at 21 years included symptoms of asthma, high dietary fat intake, poor sleep quality, and height deficits.
The 14-year assessments included a youth questionnaire (n = 5172) and in-person cognitive testing (n = 3796). The 21-year visit included an in-person assessment of mental health diagnoses in a subset of the cohort (n = 2531) with the World Health Organization Composite International Diagnostic Interview (CIDI), which is based on Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria45 (Fig 1). All of the questionnaire and interview measures were validated, except for reported frequencies of specific events (ie, pregnancy, number of cigarettes, etc).
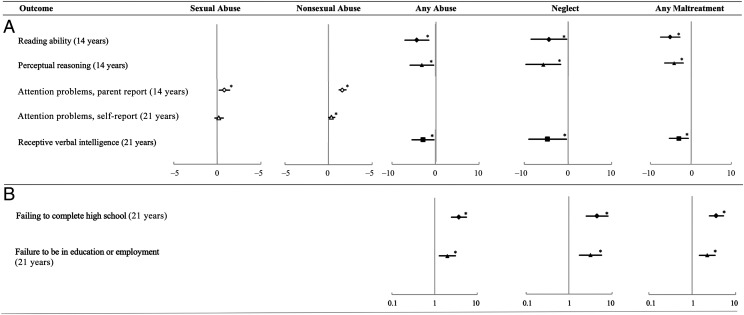
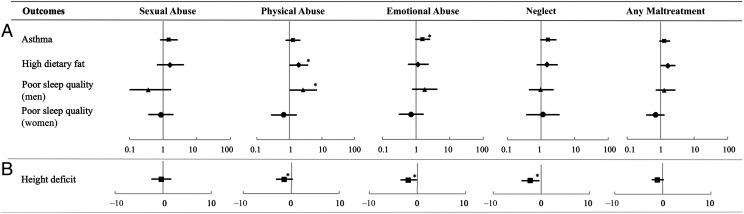
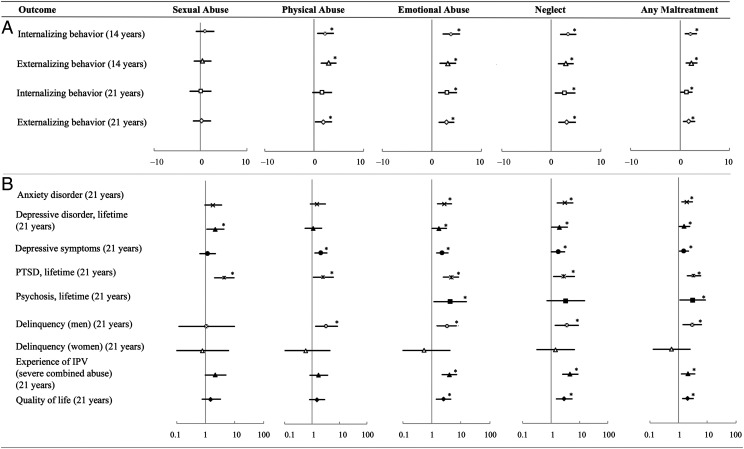
Associations were described by using either adjusted odds ratios or mean differences and coefficients, along with the corresponding 95% confidence intervals, and were plotted to visualize and compare the statistical significance of each association across specific outcome categories and types of maltreatment (Figs 4–8).
FIGURE 4.
Child maltreatment and cognition and educational outcomes at 14 and 21 years. A, Adjusted coefficients ± 95% confidence intervals. B, Odds ratios ± 95% confidence intervals. * P < .05.
FIGURE 8.
Child maltreatment and physical health outcomes at 21 years. A, Adjusted odds ratio ± 95% confidence interval. B, Adjusted coefficients ± 95% confidence interval. * P < .05.
Ethical Approval
The MUSP was approved by the Human Ethics Review Committee of The University of Queensland and the Mater Misericordiae Children’s Hospital. Ethical approval was obtained separately from the Human Ethics Review Committee of The University of Queensland for linking substantiated child maltreatment data to the 21-year follow-up data.
Results
Prevalence and Co-occurrence of Maltreatment Subtypes
In this cohort of 7214 children (Fig 1), 7.1% (n = 511 children) experienced at least 1 episode of substantiated maltreatment. Substantiated sexual abuse was reported in 2.0% (n = 147), physical abuse in 4.0% (n = 287), emotional abuse in 3.7% (n = 267), and neglect in 3.7% of cases (n = 269) (Table 1). Almost 60% of the children with substantiated maltreatment had multiple substantiated episodes (293 children; range: 2–14 episodes per child; median: 3 episodes per child37). Of the 3778 young adults included in the 21-year follow-up, 4.5% (n = 171) had a history of substantiated maltreatment,39 including sexual abuse (n = 53), physical abuse (n = 60), emotional abuse (n = 71), and neglect (n = 89).
TABLE 1.
Nonexclusive and Exclusive Categorization of Child Maltreatment Subtypes (Single and in Combination) Within the MUSP Cohort
| Combinations of Substantiated Maltreatment | n | % of Cohort (N = 7214) |
|---|---|---|
| Nonexclusive categories of maltreatment | ||
| Any sexual abuse | 147 | 2.0 |
| Any physical abuse | 287 | 4.0 |
| Any emotional abuse | 267 | 3.7 |
| Any neglect | 269 | 3.7 |
| Exclusive categories of maltreatment | ||
| None | 6703 | 92.9 |
| Sexual abuse only | 63 | 0.87 |
| Physical abuse only | 60 | 0.83 |
| Emotional abuse only | 24 | 0.33 |
| Neglect only | 71 | 0.98 |
| Sexual and physical abuse only | 10 | 0.14 |
| Sexual and emotional abuse only | 6 | 0.08 |
| Sexual abuse and neglect only | 12 | 0.17 |
| Physical and emotional abuse only | 74 | 1.03 |
| Physical abuse and neglect only | 23 | 0.32 |
| Emotional abuse and neglect only | 37 | 0.51 |
| Sexual, physical, and emotional abuse only | 5 | 0.07 |
| Sexual and physical abuse and neglect only | 5 | 0.07 |
| Sexual and emotional abuse and neglect only | 11 | 0.15 |
| Physical and emotional abuse and neglect only | 75 | 1.04 |
| Sexual, physical, and emotional abuse and neglect | 35 | 0.49 |
| Total with any substantiated maltreatment | 511 | 7.1 |
More than half of the children who experienced substantiated maltreatment were reported for ≥2 co-occurring maltreatment types (Table 1). Of the substantiated sexual abuse cases, 57.1% of the children experienced ≥1 additional maltreatment types (84 of 147); for physical abuse, this proportion was 79.1% (227 of 287); for emotional abuse, 83.5% (223 of 267); and for neglect, 73.6% (198 of 269). In particular, emotional abuse and neglect co-occurred, with or without other types of maltreatment, in ∼59% of cases.46
Cognition and Education Outcomes
Abuse (a combined category) and neglect were both associated with significantly lower cognitive scores at both 14 and 21 years, as well as with negative long-term educational and employment outcomes in young adulthood.19,20 This was after adjusting for factors such as the child’s race, sex, birth weight, breastfeeding exposure, and age; family income; and maternal education and alcohol and/or tobacco use (Fig 3). Specifically, proxy measures of IQ, such as reading ability and perceptual reasoning, at age 14 years were adversely associated with both substantiated abuse and neglect.19 Sexual abuse was associated with attention problems in adolescence, whereas nonsexual maltreatment was associated with attention problems at both time points.21 Young adults who experienced substantiated child maltreatment had reduced scores on the Peabody Vocabulary Test at 21 years. In terms of educational outcomes in young adulthood, both abuse and neglect manifested a threefold to fourfold increase in odds of failing to complete high school and a twofold to threefold increase in the likelihood of being unemployed at age 21 years20 (Figs 2 and 4).
Psychological and Mental Health Outcomes
During adolescence, physical abuse, emotional abuse, and neglect were all significantly associated with both internalizing and externalizing behavior problems, although this was not the case for physical abuse notifications without co-occurring emotional abuse or neglect.22 After adjustment for relevant sociodemographic variables, the associations with emotional abuse and neglect remained significant at 21 years.39 No statistically significant association was found between sexual abuse and these behavior problems at either time point.
Psychological maltreatment in childhood was associated with all of the other 15 psychological and mental health outcomes in young adulthood, except for delinquency in women. This was true after adjustment for sociodemographic variables and psychological and mental health problems (such as attention-deficit/hyperactivity disorder, aggressive behavior problems, and maternal depression or adverse life events, in the case of psychosis and/or IPV exposure outcomes) (Fig 3). Specifically, both emotional abuse and neglect were significantly associated at 21 years with all of the following outcomes: anxiety, depression, PTSD, psychosis (with some exceptions), delinquency in men, and experiencing IPV and harassment (except for neglect).22–25,39 Emotional abuse and neglect were the only maltreatment subtypes associated with a significant decrease in quality-of-life scores.36
The only mental health outcomes associated with sexual abuse were clinical depression, lifetime PTSD, and experiencing physical IPV.8,25,39 Physical abuse was associated with externalizing behavior problems and delinquency (in men), internalizing behavior problems and depressive symptoms, experience of IPV, and PTSD22,24,25,39 (Figs 2 and 5).
FIGURE 5.
Child maltreatment and psychological and mental health outcomes at 14 and 21 years. A, Adjusted coefficients ± 95% confidence intervals. B, Odds ratios ± 95% confidence intervals. * P < .05.
Addiction and Substance Use Outcomes
Overall, emotional abuse and/or neglect were associated with all categories of substance use and addiction at both 14 and 21 years, whereas physical and sexual abuse were associated with surprisingly few substance abuse outcomes. Specifically, childhood emotional abuse and neglect were associated with adolescent substance use at age 14, including alcohol use and smoking.26 This was after adjustment for sociodemographic factors and youth and maternal drug use. The association with cigarette and alcohol use persisted from adolescence to adulthood. The category of "any cigarette use" was the only addiction outcome associated with all 4 types of maltreatment.40 At 21 years, emotional abuse and neglect were both associated with the early onset of cannabis abuse after adjustment for maternal stress and cigarette use. Additionally, physical abuse, emotional abuse, and neglect all revealed increased odds of cannabis dependence at age 21, with early onset associated with physical abuse and neglect.28 In contrast, only emotional abuse significantly predicted injecting-drug use in young adult men, after adjustment for maternal alcohol use and depression, whereas all types of substantiated childhood maltreatment were associated with injecting-drug use in women.27 Sexual abuse was not associated with any addiction or substance use outcome except for cigarette use at 21 years (Figs 2 and 6).
FIGURE 6.
Child maltreatment and addiction and substance use outcomes at 14 and 21 years (adjusted odds ratio ± 95% confidence interval). * P < .05.
Sexual Health Outcomes
All forms of maltreatment were significantly associated, at 21 years, with early onset of sexual activity and subsequent youth pregnancy. This was after adjustment for factors such as gestational age, youth psychopathology, and drug use. Neglect was the only type of maltreatment associated with having multiple sexual partners and was the maltreatment type most strongly associated with most other sexual health outcomes, especially youth pregnancy. Pregnancy miscarriage was modestly associated with emotional abuse, whereas termination of pregnancy was not associated with any maltreatment subtype31 (Figs 2 and 7).
FIGURE 7.
Child maltreatment and sexual health outcomes at 21 years (adjusted odds ratio ± 95% confidence interval). * P < .05.
Physical Health
Reduced adult height at 21 years, adjusted for parental height, was associated with all maltreatment subtypes except sexual abuse (which was not associated with any of the physical health outcomes). At 21 years, physical abuse was also associated with high dietary fat intake, a risk factor for obesity (adjusted for BMI), and poor sleep quality in men (adjusted for psychopathology and drug use). Asthma at 21 years revealed a modest association with emotional abuse. The combined category of any maltreatment was also associated with high dietary fat intake (Figs 2 and 8).
Magnitude of Effects
To estimate the magnitude of potential effects of child maltreatment on long-term outcomes, other studies have used a number of statistical techniques. In one Australian study that used the MUSP and other data sets, the population attributable risk of child maltreatment causing anxiety disorders in men and women, was estimated to be 21% and 31%, respectively, and 16% and 23% for depressive disorders.46 Similarly, in the MUSP study on cognitive and educational outcomes of maltreated youth, the population attributable risk of child maltreatment leading to “failure to complete high school” was 13%, and 14% for “failure to be in either education or employment at 21 years.”20
Based on one published metric of effect size using the magnitude of the adjusted odds ratio,47 77% of the statistically significant associations in this review were considered to have a medium to large effect size (odds ratio ≥2), including 10% with a large effect size (odds ratio >4) (Fig 2).
Discussion
In summary, over the past decade, the MUSP has revealed that child maltreatment is associated with a broad array of adverse outcomes during adolescence and young adulthood, including the following:
deficits in cognitive development, attention, educational attainment, and employment;
serious mental health problems, including anxiety, depression, PTSD, and psychosis, as well as delinquency and the experience of IPV;
substance use and addiction problems;
sexual health problems; and
physical health limitations and risk.
These results were seen after adjustment for a broad range of relevant sociodemographic, perinatal, psychological, and other risk factors (Fig 3). Many of the studies also adjusted for the other subtypes of child maltreatment and demonstrated that specific maltreatment types were closely associated with particular outcomes.
Abuse, Neglect, and Cognitive Development
Significant cognitive delays and educational failure were seen for both abuse and neglect across adolescence and adulthood. In another study, the authors concluded that preexisting cognitive impairments at 3 or 5 years may explain this association, rather than maltreatment per se.16 However, other research has revealed that children neglected over the first 4 years of life show a progressive decline in cognitive functioning, which is associated with a significantly reduced head circumference at 2 and 4 years of age.48 In rodent models, contingent maternal behavior is linked with infant cognitive development, and possible mechanisms include increases in synaptic connections within the hippocampus49 and reduced apoptotic cell loss.50 Prolonged maternal separation, in contrast, is associated with impaired cognitive development in rodent and primate models.51,52
Psychological Maltreatment: Emotional Abuse and/or Neglect
One of the most striking conclusions from this review was the broad association between emotional abuse and/or neglect and adverse outcomes in almost all areas of assessment (Fig 2). In stark contrast, physical abuse and sexual abuse were associated with far fewer adverse outcomes. Overall, quality of life was lower for those who had experienced emotional abuse and neglect but not for those who had experienced physical or sexual abuse. Although emotional abuse and neglect often co-occur with other types of maltreatment,46 the associated outcomes were generally robust even after statistical adjustment or separation into differing maltreatment categories (Fig 2).
Emotional abuse and neglect in early childhood may lead to psychopathology via insecure attachment,53,54 which has been associated with externalizing behavior problems55 and impaired social competence.56,57 Emotional neglect, in particular, may lead to deficits in emotion recognition and regulation, as well as insensitivity to reward,3 potentially influencing social and emotional development. Neglected children are less able to discriminate facial expressions and emotions,58 whereas youth who have been emotionally neglected show blunted development of the brain’s reward area, the ventral striatum.59 Reduced reward activation may predict risk for depression,59 addiction,60 and other psychopathologies.61
Neglect was also associated with the early onset of sexual activity, multiple sexual partners, and youth pregnancy, even after adjustment for other maltreatment subtypes. This suggests that neglect may result in compensatory efforts to obtain sexual intimacy, consistent with other studies revealing higher rates of unprotected sex62 and adolescent pregnancy in neglected children.63 In the animal literature, female rodents that experience maternal deprivation tend to have an earlier onset of puberty and increased sexual receptivity, leading to elevated reproductive activity to help offset an environment of higher offspring risk.64,65
Sexual Abuse
As observed elsewhere,66 sexual abuse was associated with early sexual experimentation and youth pregnancy as well as symptoms of PTSD and depression. Risky sexual behaviors were independent of other types of maltreatment but were not specific for sexual abuse. An additional MUSP study comparing self-reported and agency-notified child sexual abuse revealed consistent associations with major depressive disorder, anxiety disorders, and PTSD.8 The absence of associations with other adverse outcomes, however, may be, in part, due to the lower prevalence of substantiated sexual abuse, especially at the 21-year follow-up.
Physical Abuse
Outcomes associated with physical abuse differed from those associated with sexual abuse, with increased odds of externalizing behavior problems, and delinquency in men. Jaffee3 suggests that physical abuse, in particular, may lead to a hypervigilance response to threat, including negative attentional bias, disproportionate to relatively mild threat cues. Studies have revealed that physically abused children show selective attention to anger cues,67 have difficulty disengaging from them,58,68 and are more likely to misinterpret facial cues as being angry or fearful.69
Limitations
Although these studies demonstrated significant associations between maltreatment and a range of long-term outcomes, association does not equal causality. The causal mechanisms proposed above are tentative and may relate to multiple types of maltreatment.
Other limitations should also be considered. Firstly, selective attrition of socioeconomically disadvantaged and maltreated young people was evident in the MUSP cohort (Supplemental Information). However, based on multiple imputation calculations and inverse probability weighting of MUSP data,18,70 differences in the rate of loss to follow-up, for both dependent and independent variables, made little difference to either the estimates or their precision, mirroring findings from other longitudinal studies.71 In addition, the findings were mostly unchanged when using propensity analysis, which is used to assess the effects of nonrandom sampling variation by analyzing the probability of assignment to a particular category within an observational study given the observed covariates.72 Specifically, the sample was weighted so that it better resembled sociodemographic characteristics at baseline to minimize bias from differential attrition in those with greater socioeconomic disadvantage.
Secondly, differences in the prevalence of specific maltreatment subtypes might have influenced the statistical power to detect true effects, particularly regarding sexual abuse (Table 1).
Finally, the co-occurrence of different types of maltreatment may have impacted the ability to accurately predict the associations between specific types of maltreatment and outcomes. Other studies have revealed that emotional abuse and neglect, in particular, are more likely to co-occur with each other and with other types of maltreatment.73 However, even in those articles that statistically adjusted for other co-occurring maltreatment subtypes, the associated outcomes linked with emotional abuse and/or neglect were generally robust. In articles that did not adjust for these co-occurrences, some of the strongest associations were still observed for emotional abuse and/or neglect.
Conclusions
Child maltreatment, particularly psychological maltreatment, is associated with a broad range of negative long-term health and developmental outcomes extending into adolescence and young adulthood. Although these data do not establish causality, neurodevelopmental pathways are likely influenced by stress and early social experience through epigenetic mechanisms, which may affect gene expression and regulation and, ultimately, behavior and development.3,74
Understanding the developmental roots of these adverse outcomes may motivate physicians to more systematically inquire about early-life trauma and refer patients to more appropriate treatment services.75,76 Even more importantly, early intervention and prevention programs, such as prenatal and infancy nurse home visiting,77 have demonstrated, in randomized clinical trials, diminished rates of child abuse and neglect.78,79 Long-term benefits to the offspring include decreased childhood internalizing problems,80 reduced antisocial behavior and substance abuse in adolescence,81 and improved cognitive skills extending into young adulthood.80,82 Supporting at-risk parents and young children should thus be an urgent priority.
Glossary
- CIDI
Composite International Diagnostic Interview
- IPV
intimate partner violence
- MUSP
Mater-University of Queensland Study of Pregnancy
- PTSD
posttraumatic stress disorder
Footnotes
Dr Strathearn conceptualized and designed the original study linking the Mater-University of Queensland Study of Pregnancy data set with substantiated reports of child maltreatment, drafted the special article, and reviewed and revised the manuscript; Dr Giannotti assisted in drafting the manuscript and prepared all tables and figures; Drs Mills, Kisely, and Abajobir conceptualized and wrote the original research articles summarized in this article; Dr Najman was the original principal investigator of the Mater-University of Queensland Study of Pregnancy; and all authors critically reviewed the manuscript for important intellectual content and approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Partially supported by the US National Institute on Drug Abuse (R01DA026437). The content is solely the responsibility of the authors and does not necessarily represent the official views of this institute or the National Institutes of Health. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373(9657):68–81 [DOI] [PubMed] [Google Scholar]
- 2.US Department of Health and Human Services; Administration for Children and Families; Administration on Children, Youth and Families; Children’s Bureau . Child Maltreatment 2017. Washington, DC: US Government Printing Office; 2019 [Google Scholar]
- 3.Jaffee SR. Child maltreatment and risk for psychopathology in childhood and adulthood. Annu Rev Clin Psychol. 2017;13:525–551 [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization Report of the Consultation on Child Abuse Prevention, 29–31 March, 1999. Geneva, Switzerland: World Health Organization; 1999 [Google Scholar]
- 5.Stoltenborgh M, Bakermans-Kranenburg MJ, Alink LRA, IJzendoorn MH. The prevalence of child maltreatment across the globe: review of a series of meta-analyses. Child Abuse Rev. 2015;24(1):37–50 [Google Scholar]
- 6.Dube SR, Williamson DF, Thompson T, Felitti VJ, Anda RF. Assessing the reliability of retrospective reports of adverse childhood experiences among adult HMO members attending a primary care clinic. Child Abuse Negl. 2004;28(7):729–737 [DOI] [PubMed] [Google Scholar]
- 7.Newbury JB, Arseneault L, Moffitt TE, et al. . Measuring childhood maltreatment to predict early-adult psychopathology: comparison of prospective informant-reports and retrospective self-reports. J Psychiatr Res. 2018;96:57–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mills R, Kisely S, Alati R, Strathearn L, Najman J. Self-reported and agency-notified child sexual abuse in a population-based birth cohort. J Psychiatr Res. 2016;74:87–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trickett PK, Noll JG, Putnam FW. The impact of sexual abuse on female development: lessons from a multigenerational, longitudinal research study. Dev Psychopathol. 2011;23(2):453–476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spataro J, Mullen PE, Burgess PM, Wells DL, Moss SA. Impact of child sexual abuse on mental health: prospective study in males and females. Br J Psychiatry. 2004;184(5):416–421 [DOI] [PubMed] [Google Scholar]
- 11.Doidge JC, Higgins DJ, Delfabbro P, Segal L. Risk factors for child maltreatment in an Australian population-based birth cohort. Child Abuse Negl. 2017;64:47–60 [DOI] [PubMed] [Google Scholar]
- 12.Springer KW, Sheridan J, Kuo D, Carnes M. Long-term physical and mental health consequences of childhood physical abuse: results from a large population-based sample of men and women. Child Abuse Negl. 2007;31(5):517–530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Breslau N, Koenen KC, Luo Z, et al. . Childhood maltreatment, juvenile disorders and adult post-traumatic stress disorder: a prospective investigation. Psychol Med. 2014;44(9):1937–1945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sidebotham P, Heron J; ALSPAC Study Team . Child maltreatment in the “children of the nineties”: a cohort study of risk factors. Child Abuse Negl. 2006;30(5):497–522 [DOI] [PubMed] [Google Scholar]
- 15.Scott KM, Smith DR, Ellis PM. Prospectively ascertained child maltreatment and its association with DSM-IV mental disorders in young adults. Arch Gen Psychiatry. 2010;67(7):712–719 [DOI] [PubMed] [Google Scholar]
- 16.Danese A, Moffitt TE, Arseneault L, et al. . The origins of cognitive deficits in victimized children: implications for neuroscientists and clinicians. Am J Psychiatry. 2017;174(4):349–361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Croft J, Heron J, Teufel C, et al. . Association of trauma type, age of exposure, and frequency in childhood and adolescence with psychotic experiences in early adulthood. JAMA Psychiatry. 2019;76(1):79–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Najman JM, Alati R, Bor W, et al. . Cohort profile update: the Mater-University of Queensland Study of Pregnancy (MUSP). Int J Epidemiol. 2015;44(1):78–78f [DOI] [PubMed] [Google Scholar]
- 19.Mills R, Alati R, O’Callaghan M, et al. . Child abuse and neglect and cognitive function at 14 years of age: findings from a birth cohort. Pediatrics. 2011;127(1):4–10 [DOI] [PubMed] [Google Scholar]
- 20.Mills R, Kisely S, Alati R, Strathearn L, Najman JM. Cognitive and educational outcomes of maltreated and non-maltreated youth: a birth cohort study. Aust N Z J Psychiatry. 2019;53(3):248–255 [DOI] [PubMed] [Google Scholar]
- 21.Boyd M, Kisely S, Najman J, Mills R. Child maltreatment and attentional problems: a longitudinal birth cohort study. Child Abuse Negl. 2019;98:104170. [DOI] [PubMed] [Google Scholar]
- 22.Mills R, Scott J, Alati R, O’Callaghan M, Najman JM, Strathearn L. Child maltreatment and adolescent mental health problems in a large birth cohort. Child Abuse Negl. 2013;37(5):292–302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abajobir AA, Kisely S, Scott JG, et al. . Childhood maltreatment and young adulthood hallucinations, delusional experiences, and psychosis: a longitudinal study. Schizophr Bull. 2017;43(5):1045–1055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abajobir AA, Kisely S, Williams G, Strathearn L, Clavarino A, Najman JM. Gender differences in delinquency at 21 years following childhood maltreatment: a birth cohort study. Pers Individ Dif. 2017;106:95–103 [Google Scholar]
- 25.Abajobir AA, Kisely S, Williams GM, Clavarino AM, Najman JM. Substantiated childhood maltreatment and intimate partner violence victimization in young adulthood: a birth cohort study. J Youth Adolesc. 2017;46(1):165–179 [DOI] [PubMed] [Google Scholar]
- 26.Mills R, Alati R, Strathearn L, Najman JM. Alcohol and tobacco use among maltreated and non-maltreated adolescents in a birth cohort. Addiction. 2014;109(4):672–680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abajobir AA, Kisely S, Williams G, Clavarino A, Strathearn L, Najman JM. Gender-based differences in injecting drug use by young adults who experienced maltreatment in childhood: findings from an Australian birth cohort study. Drug Alcohol Depend. 2017;173:163–169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abajobir AA, Najman JM, Williams G, Strathearn L, Clavarino A, Kisely S. Substantiated childhood maltreatment and young adulthood cannabis use disorders: a pre-birth cohort study. Psychiatry Res. 2017;256:21–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mills R, Kisely S, Alati R, Strathearn L, Najman JM. Child maltreatment and cannabis use in young adulthood: a birth cohort study. Addiction. 2017;112(3):494–501 [DOI] [PubMed] [Google Scholar]
- 30.Kisely S, Mills R, Strathearn L, Najman JM. Does child maltreatment predict alcohol use disorders in young adulthood? A cohort study of linked notifications and survey data. Addiction. 2020;115(1):61–68 [DOI] [PubMed] [Google Scholar]
- 31.Abajobir AA, Kisely S, Williams G, Strathearn L, Najman JM. Risky sexual behaviors and pregnancy outcomes in young adulthood following substantiated childhood maltreatment: findings from a prospective birth cohort study. J Sex Res. 2018;55(1):106–119 [DOI] [PubMed] [Google Scholar]
- 32.Abajobir AA, Kisely S, Williams G, Strathearn L, Najman JM. Height deficit in early adulthood following substantiated childhood maltreatment: a birth cohort study. Child Abuse Negl. 2017;64:71–78 [DOI] [PubMed] [Google Scholar]
- 33.Abajobir AA, Kisely S, Williams G, Strathearn L, Najman JM. Childhood maltreatment and high dietary fat intake behaviors in adulthood: a birth cohort study. Child Abuse Negl. 2017;72:147–153 [DOI] [PubMed] [Google Scholar]
- 34.Abajobir AA, Kisely S, Williams G, Strathearn L, Najman JM. Childhood maltreatment and adulthood poor sleep quality: a longitudinal study. Intern Med J. 2017;47(8):879–888 [DOI] [PubMed] [Google Scholar]
- 35.Abajobir AA, Kisely S, Williams G, Strathearn L, Suresh S, Najman JM. The association between substantiated childhood maltreatment, asthma and lung function: a prospective investigation. J Psychosom Res. 2017;101:58–65 [DOI] [PubMed] [Google Scholar]
- 36.Abajobir AA, Kisely S, Williams G, Strathearn L, Clavarino A, Najman JM. Does substantiated childhood maltreatment lead to poor quality of life in young adulthood? Evidence from an Australian birth cohort study. Qual Life Res. 2017;26(7):1697–1702 [DOI] [PubMed] [Google Scholar]
- 37.Strathearn L, Mamun AA, Najman JM, O’Callaghan MJ. Does breastfeeding protect against substantiated child abuse and neglect? A 15-year cohort study. Pediatrics. 2009;123(2):483–493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Steering Committee for the Review of Commonwealth/State Service Provision Report on government services 2000. Available at: https://www.pc.gov.au/research/ongoing/report-on-government-services/2000/2000. Accessed August 1, 2019.
- 39.Kisely S, Abajobir AA, Mills R, Strathearn L, Clavarino A, Najman JM. Child maltreatment and mental health problems in adulthood: birth cohort study. Br J Psychiatry. 2018;213(6):698–703 [DOI] [PubMed] [Google Scholar]
- 40.Kisely S, Abajobir AA, Mills R, et al. . Child maltreatment and persistent smoking from adolescence into adulthood: a birth cohort study. Nicotine Tob Res. 2020;22(1):66–73 [DOI] [PubMed] [Google Scholar]
- 41.Nicholls SG, Quach P, von Elm E, et al. . The Reporting of Studies Conducted Using Observational Routinely-Collected Health Data (RECORD) statement: methods for arriving at consensus and developing reporting guidelines. PLoS One. 2015;10(5):e0125620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mata DA, Ramos MA, Bansal N, et al. . Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA. 2015;314(22):2373–2383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lau AS, Leeb RT, English D, et al. . What’s in a name? A comparison of methods for classifying predominant type of maltreatment. Child Abuse Negl. 2005;29(5):533–551 [DOI] [PubMed] [Google Scholar]
- 44.Senn TE, Carey MP, Vanable PA. Childhood and adolescent sexual abuse and subsequent sexual risk behavior: evidence from controlled studies, methodological critique, and suggestions for research. Clin Psychol Rev. 2008;28(5):711–735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Robins LN, Wing J, Wittchen HU, et al. . The Composite International Diagnostic Interview. An epidemiologic instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiatry. 1988;45(12):1069–1077 [DOI] [PubMed] [Google Scholar]
- 46.Moore SE, Scott JG, Ferrari AJ, et al. . Burden attributable to child maltreatment in Australia. Child Abuse Negl. 2015;48:208–220 [DOI] [PubMed] [Google Scholar]
- 47.Rosenthal JA. Qualitative descriptors of strength of association and effect size. J Soc Sci Res. 1996;21(4):37–59 [Google Scholar]
- 48.Strathearn L, Gray PH, O’Callaghan MJ, Wood DO. Childhood neglect and cognitive development in extremely low birth weight infants: a prospective study. Pediatrics. 2001;108(1):142–151 [DOI] [PubMed] [Google Scholar]
- 49.Liu D, Diorio J, Day JC, Francis DD, Meaney MJ. Maternal care, hippocampal synaptogenesis and cognitive development in rats. Nat Neurosci. 2000;3(8):799–806 [DOI] [PubMed] [Google Scholar]
- 50.Weaver IC, Grant RJ, Meaney MJ. Maternal behavior regulates long-term hippocampal expression of BAX and apoptosis in the offspring. J Neurochem. 2002;82(4):998–1002 [DOI] [PubMed] [Google Scholar]
- 51.Dettling AC, Feldon J, Pryce CR. Repeated parental deprivation in the infant common marmoset (Callithrix jacchus, primates) and analysis of its effects on early development. Biol Psychiatry. 2002;52(11):1037–1046 [DOI] [PubMed] [Google Scholar]
- 52.Huot RL, Plotsky PM, Lenox RH, McNamara RK. Neonatal maternal separation reduces hippocampal mossy fiber density in adult Long Evans rats. Brain Res. 2002;950(1–2):52–63 [DOI] [PubMed] [Google Scholar]
- 53.Strathearn L. Maternal neglect: oxytocin, dopamine and the neurobiology of attachment. J Neuroendocrinol. 2011;23(11):1054–1065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cyr C, Euser EM, Bakermans-Kranenburg MJ, Van Ijzendoorn MH. Attachment security and disorganization in maltreating and high-risk families: a series of meta-analyses. Dev Psychopathol. 2010;22(1):87–108 [DOI] [PubMed] [Google Scholar]
- 55.Fearon RP, Bakermans-Kranenburg MJ, van Ijzendoorn MH, Lapsley AM, Roisman GI. The significance of insecure attachment and disorganization in the development of children’s externalizing behavior: a meta-analytic study. Child Dev. 2010;81(2):435–456 [DOI] [PubMed] [Google Scholar]
- 56.Fearon RMP, Roisman GI. Attachment theory: progress and future directions. Curr Opin Psychol. 2017;15:131–136 [DOI] [PubMed] [Google Scholar]
- 57.Groh AM, Fearon RP, Bakermans-Kranenburg MJ, van Ijzendoorn MH, Steele RD, Roisman GI. The significance of attachment security for children’s social competence with peers: a meta-analytic study. Attach Hum Dev. 2014;16(2):103–136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pollak SD, Cicchetti D, Hornung K, Reed A. Recognizing emotion in faces: developmental effects of child abuse and neglect. Dev Psychol. 2000;36(5):679–688 [DOI] [PubMed] [Google Scholar]
- 59.Hanson JL, Hariri AR, Williamson DE. Blunted ventral striatum development in adolescence reflects emotional neglect and predicts depressive symptoms. Biol Psychiatry. 2015;78(9):598–605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kim S, Iyengar U, Mayes LC, Potenza MN, Rutherford HJV, Strathearn L. Mothers with substance addictions show reduced reward responses when viewing their own infant’s face. Hum Brain Mapp. 2017;38(11):5421–5439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Koob GF, Le Moal M. Addiction and the brain antireward system. Annu Rev Psychol. 2008;59:29–53 [DOI] [PubMed] [Google Scholar]
- 62.Thompson R, Lewis T, Neilson EC, et al. . Child maltreatment and risky sexual behavior. Child Maltreat. 2017;22(1):69–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Negriff S, Schneiderman JU, Trickett PK. Child maltreatment and sexual risk behavior: maltreatment types and gender differences. J Dev Behav Pediatr. 2015;36(9):708–716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cameron N, Del Corpo A, Diorio J, McAllister K, Sharma S, Meaney MJ. Maternal programming of sexual behavior and hypothalamic-pituitary-gonadal function in the female rat. PLoS One. 2008;3(5):e2210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Champagne FA. Epigenetic legacy of parental experiences: dynamic and interactive pathways to inheritance. Dev Psychopathol. 2016;28(4, pt 2):1219–1228 [DOI] [PubMed] [Google Scholar]
- 66.Stevens-Simon C, Reichert S. Sexual abuse, adolescent pregnancy, and child abuse. A developmental approach to an intergenerational cycle. Arch Pediatr Adolesc Med. 1994;148(1):23–27 [DOI] [PubMed] [Google Scholar]
- 67.Pollak SD, Tolley-Schell SA. Selective attention to facial emotion in physically abused children. J Abnorm Psychol. 2003;112(3):323–338 [DOI] [PubMed] [Google Scholar]
- 68.Curtis WJ, Cicchetti D. Affective facial expression processing in young children who have experienced maltreatment during the first year of life: an event-related potential study. Dev Psychopathol. 2011;23(2):373–395 [DOI] [PubMed] [Google Scholar]
- 69.Gibb BE, Schofield CA, Coles ME. Reported history of childhood abuse and young adults’ information-processing biases for facial displays of emotion. Child Maltreat. 2009;14(2):148–156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Saiepour N, Najman JM, Ware R, Baker P, Clavarino AM, Williams GM. Does attrition affect estimates of association: a longitudinal study. J Psychiatr Res. 2019;110:127–142 [DOI] [PubMed] [Google Scholar]
- 71.Wolke D, Waylen A, Samara M, et al. . Selective drop-out in longitudinal studies and non-biased prediction of behaviour disorders. Br J Psychiatry. 2009;195(3):249–256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Goodman JS, Blum TC. Assessing the non-random sampling effects of subject attrition in longitudinal research. J Manage. 1996;22(4):627–652 [Google Scholar]
- 73.Kim K, Mennen FE, Trickett PK. Patterns and correlates of co-occurrence among multiple types of child maltreatment. Child Fam Soc Work. 2017;22(1):492–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jaffee SR, Price TS, Reyes TM. Behavior genetics: past, present, future. Dev Psychopathol. 2013;25(4, pt 2):1225–1242 [DOI] [PubMed] [Google Scholar]
- 75.Allen B. The use and abuse of attachment theory in clinical practice with maltreated children, part II: treatment. Trauma Violence Abuse. 2011;12(1):13–22 [DOI] [PubMed] [Google Scholar]
- 76.Nemeroff CB, Heim CM, Thase ME, et al. . Differential responses to psychotherapy versus pharmacotherapy in patients with chronic forms of major depression and childhood trauma. Proc Natl Acad Sci U S A. 2003;100(24):14293–14296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Olds DL, Kitzman H, Anson E, et al. . Prenatal and infancy nurse home visiting effects on mothers: 18-year follow-up of a randomized trial. Pediatrics. 2019;144(6):e20183889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Olds DL, Eckenrode J, Henderson CR Jr., et al. . Long-term effects of home visitation on maternal life course and child abuse and neglect. Fifteen-year follow-up of a randomized trial. JAMA. 1997;278(8):637–643 [PubMed] [Google Scholar]
- 79.Kitzman H, Olds DL, Henderson CR Jr., et al. . Effect of prenatal and infancy home visitation by nurses on pregnancy outcomes, childhood injuries, and repeated childbearing. A randomized controlled trial. JAMA. 1997;278(8):644–652 [PubMed] [Google Scholar]
- 80.Kitzman HJ, Olds DL, Cole RE, et al. . Enduring effects of prenatal and infancy home visiting by nurses on children: follow-up of a randomized trial among children at age 12 years. Arch Pediatr Adolesc Med. 2010;164(5):412–418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Olds D, Henderson CR Jr., Cole R, et al. . Long-term effects of nurse home visitation on children’s criminal and antisocial behavior: 15-year follow-up of a randomized controlled trial. JAMA. 1998;280(14):1238–1244 [DOI] [PubMed] [Google Scholar]
- 82.Kitzman H, Olds DL, Knudtson MD, et al. . Prenatal and infancy nurse home visiting and 18-year outcomes of a randomized trial. Pediatrics. 2019;144(6):e20183876. [DOI] [PMC free article] [PubMed] [Google Scholar]