Our group uses esophageal manometry routinely to personalize mechanical ventilation in patients with acute respiratory distress syndrome (ARDS) [1, 2]. Esophageal pressures (Pes) allow for differentiation of chest wall, lung and respiratory system mechanics, and we use this for PEEP titration [1, 2], monitoring of parenchymal lung stress, limiting peak end-inspiratory transpulmonary pressures and monitoring for ventilator synchrony [3, 4].
We find that esophageal manometry is straightforward in the majority of patients although proper training and application are important. The initial step is to assure correct placement with insertion of stand-alone catheters or feeding tubes with integrated esophageal balloons which are similar to routine gastric tubes. Typical depth of insertion ranges from 33 to 40 cm, depending on body size and we assure proper placement through functional bedside assessment. First, we look for the presence of cardiac oscillations to assure correct position posterior to the heart. If absent, this suggests the balloon is too deep or shallow and we incrementally adjust while monitoring for these oscillations. Next we perform expiratory breath holds, with changes in Pes, airway (Pao) and transpulmonary pressure (PL = Pao − Pes) monitored during gentle chest pushes. Proper position is confirmed when Pes and Pao increase in equal measure, with no change in the calculated PL. If Pao increases more Pes, this suggests that position is too deep and the balloon is adjusted incrementally with repeat chest pushes. This may be confirmed with gentle abdominal pushes (with Pes increasing more than Pao). (Table 1).
Table 1.
Tricks and troubleshooting
| How we do it | Troubleshooting | |
|---|---|---|
| Proper placement |
(1) Placement depth: Usual depth is 33–40 cm (a good starting point is 37 cm) (2) Balloon inflation: Use a balloon with a consistent working volume. Optimization of volume otherwise will need to be done by measuring the pressure–volume characteristics of the balloon itself which is not always feasible (3) Cardiac oscillations: Cardiac oscillations should be present to confirm placement posterior to the heart above the diaphragm (4) End-Expiratory Hold Chest Pushes: Pes and Pao should increase in equal measures with chest push resulting in no change in PL |
(1) Depth is incrementally adjusted while looking for oscillations and doing chest pushes (2) Depending on body habitus and the unique patient, the amplitude of oscillations may be widely variable (3) If patient is ACTIVELY breathing, expiratory breath holds can still confirm placement. Pao and Pes DECREASES in this case without change in PL |
| PEEP titration |
(1) Measurement of Pes and PL during expiratory holds (2) Adjust PEEP until PL at end –expiration = zero (3) We use in most patients with moderate-severe ARDS (4) Especially useful with obesity or abdominal hypertension |
(1) We no longer use the sliding scale FiO2—PL used in the EPVent studies, targeting PL = zero with acceptable range from -2 to + 2 cmH2O |
| Monitoring cyclic and total lung stress |
(1) Measure end-inspiratory PL: This measurement is obtained when the plateau pressure is measured during an inspiratory breath hold. We keep the end-inspiratory PL < 20cmH2O and ideally aim for < 15cmH2O to provide additional safety (2) Measure ∆PL: Calculated as the end-inspiratory PL minus the end expiratory PL. This provides a more targeted driving pressure measurement than the respiratory system values, and we aim for less than 10–12cmH2O (3) Targeted titration of tidal volume if above target values if allowable with ventilation requirements |
(1) With large cardiac oscillations, use the diastole phase for measurements to be consistent (2) We recommend PEEP titration/optimization to maximize compliance prior to targeted tidal volume reduction |
| Dyssynchrony and neuromuscular blockade |
(1) This is easiest with systems that integrate xy plots (2) This is more advanced level application and beyond routine use as above |
(1) Not recommended for routine use as requires more specialty equipment and training |
Using a balloon with a consistent working range of inflation volume is helpful for obtaining consistent and accurate measurements. While optimal inflation volume can be confirmed based upon the pressure–volume characteristics of the balloon itself [5], this is time-consuming and not required in practice when using a balloon with a known acceptable range. Overinflation results in inaccurately high measured pressures secondary to the compliance of the balloon, while underinflation causes dampening of waveform variation. Visualization and interpretation of data are facilitated by integrated pressure sensors within the ventilator or can be recorded using stand-alone devices as we used in the EPVent and EPVent2 studies [1, 2].
One of our primary applications of esophageal manometry is for titration of positive end-expiratory pressure (PEEP). Critically ill patients frequently exhibit increased chest wall weight and elevated basal end-expiratory pleural pressures secondary to edema, effusions, abdominal hypertension and other causes that may lead to derecruitment, increased lung elastance and hypoxemia. We measure Pes as a surrogate for pleural pressure [6] and if the pleural pressure is larger than the measured airway/alveolar pressure (PL = Pao − Pes), these collapsing pressures can be countered with the application of PEEP. Our EPVent [2] and EPvent2 [1] studies investigated the use of esophageal manometry to titrate PEEP and while the latter study did not show clear benefit compared with empiric high-PEEP, further analysis suggested a benefit when end-expiratory PL were maintained in a tight physiological range of − 2 to + 2cmH2O with PEEP adjustment (publication under review) which is how we practice clinically. We aim for an end-expiratory PL of zero regardless of the FiO2 which is distinct from the original sliding-scale protocols [1, 2] and is in part secondary to the slight benefit gained from mediastinal artifact in the “actual” vs. measured PL [7].
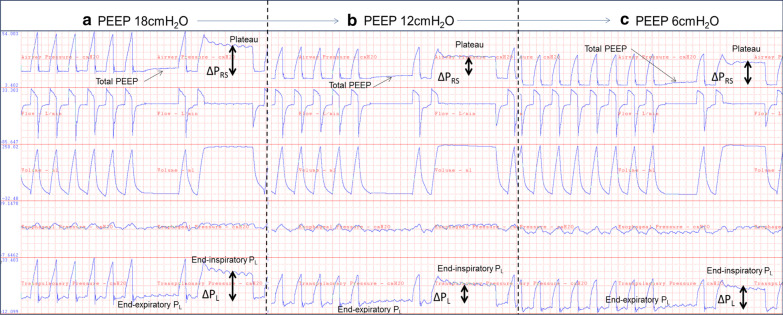
We find esophageal manometry particularly useful with morbid obesity and ARDS [8, 9], allowing for measurement of elevated pleural pressures and safe application of high PEEP levels (~ 20–30cmH2O) to offload the weight of the chest wall. Conversely, esophageal manometry is also useful in determining when applied PEEP is too high allowing for targeted titration to lower PEEP which may prevent the harmful effects of overdistension (Fig. 1).
Figure 1.
This figure represents positive end-expiratory pressure (PEEP) titration in a mildly obese woman with moderate-severe acute respiratory distress syndrome (ARDS) secondary to ascites and TRALI, with increased chest wall stiffness and mildly elevated basal pleural pressures. Patient was on Vt 250 cc (close to 5 cc/kg IBW), RR 34 and FiO2 0.6. This example illustrates the use in PEEP titration and monitoring of cyclic and total lung stress levels and how esophageal manometry can be used to titrate PEEP not only to HIGH levels, but also be used to titrate downwards to an optimal mid-range. PEEP (airway pressure—Pao) was adjusted to match the measured esophageal pressure (Pes) to calculate the transpulmonary pressure (PL = Pao – Pes) and target a PL equal to zero. a Empiric PEEP of 18cmH2O (equivalent to using empiric high PEEP ARDSnet tables) was utilized initially on this patient. On these initial settings, the total PEEP was 20cmH2O, plateau pressure was 40cmH2O, respiratory system driving pressure (∆PRS) was 20cmH2O, and respiratory system compliance was 12.5 ml/cmH2O. The end-expiratory transpulmonary pressure (PL) was + 5cmH2O, and end-inspiratory PL 20cmH2O with a transpulmonary driving pressure (∆PL) of 15cmH2O with a lung compliance of 15 ml/cmH2O. These numbers suggested PEEP application was too high and could be resulting in overdistension as measured by the cyclic and total lung stress. b Lowering PEEP to 12cmH2O resulted in finding optimized mechanics at a PEEP of 12cmH2O. This resulted in a total PEEP of 14.5cmH2O, plateau pressure of 29.5cmH2O, ∆PRS of 15cmH2O, respiratory system compliance of 18 ml/cmH2O, end-expiratory PL of + 0.5cmH2O, end-inspiratory PL of 11cmH2O, ∆PL of 10.5 ml/cmH2O and lung compliance of 24 ml/cmH2O. c Dropping PEEP further to 6cmH2O resulted in apparent derecruitment with worsened mechanics. Total PEEP was 8.5cmH2O, plateau pressure 26.5cmH2O, ∆PRS 18cmH2O, respiratory system compliance 13.9 ml/cmH2O, end-expiratory PL was − 5.8cmH2O, end-inspiratory PL was 9cmH2O, ∆PL 14.8cmH2O, lung compliance 16.8 ml/cmH2O
As a more specific measure of lung stress, we routinely monitor the cyclic distending pressures across the lungs (transpulmonary driving pressure [∆PL]) [10]. While the respiratory system driving pressure correlated with mortality in patients with ARDS [11], we believe it is inadequate due to the inherent variability and heterogeneity of the chest wall which we can directly measure using Pes. We target a ∆PL of less than 10–12cmH2O due to lung inhomogeneity and local stress raisers [12], which could prevent lung injury [13] and is in agreement with our retrospective mortality data [10]. ∆PL is easily measured as the end-inspiratory PL (plateau pressure equivalent) minus the end-expiratory PL (total PEEP equivalent).
In addition to the cyclic lung stress, we use Pes to measure the total lung stress (end-inspiratory PL) in addition to plateau pressure. A plateau pressure < 30cmH2O represents a widely varying level of lung stress depending on the chest wall mechanics. While safe levels have not been clearly defined, we have extrapolated thresholds from our understanding of the relationship between stress, strain and specific elastance, and data suggesting high ∆PL and end-inspiratory PL can bring the lung to total lung capacity and lead to lethal ventilator induced lung injury [14]. As such, our practice is to limit end-inspiratory PL to less than 20cmH2O (and ideally even lower, to < 15cmH2O), to decrease overdistension and improve the margin of safety.
If we identify a patient with elevated ∆PL or total end-inspiratory PL, this data is used to facilitate targeted tidal volume reduction, to bring these values within safer limits. We recognize that further prospective investigation of these limits is warranted to better clarify targets, but we synthesize these data with other clinical data to help inform our bedside care. Importantly, with widely variable chest wall pressures and elastance, we cannot predict if we are reaching these thresholds of cyclic and total stress without the use of an esophageal balloon.
We also use esophageal manometry in the bedside assessment of patient–ventilator synchrony using the chest wall pressure volume loops for identification of passive ventilator delivered breaths, spontaneous breaths, dyssynchrony [3, 4], for titration of neuromuscular blockade [6] and for direct measurement of work of breathing, inspiratory muscle efforts and lung-directed mechanical power to assess when levels of effort may be harmful [15]. In conclusion, esophageal balloon catheters are easily placed and interpreted. Measured esophageal pressures and calculation of transpulmonary pressures have broad applications for personalized care of mechanically ventilated patients with PEEP titration, measurement of lung stress and assessment for ventilator synchrony.
Authors’ contributions
Article was written and edited by both authors.
Funding
Dr Baedorf Kassis’ work was conducted with the support of a KL2 award (an appointed KL2 award) from Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award KL2 TR002542). The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, or the National Institutes of Health.
Availability of data and material
Not applicable. If your manuscript does not contain any data, please state not applicable in this section.
Consent for publication
Not applicable. No consent needed for this editorial.
Ethics approval and consent to participate
Not applicable. There was no ethics approval needed for this editorial.
Competing interests
The authors declare that there are no competing interests regarding publication of this editorial. Of note both Dr Baedorf Kassis and Dr Talmor receive educational speaking fees from Hamilton Medical for unrelated work.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Beitler JR, Sarge T, Banner-Goodspeed V, Gong MN, Cook DJ, Novack V, et al. Lung mechanics to guide positive end-expiratory pressure in acute respiratory distress syndrome: The EPVent-2 Randomized Clinical Trial. 2019. [DOI] [PMC free article] [PubMed]
- 2.Talmor D, Sarge T, Malhotra A, O’Donnell CR, Ritz R, Lisbon A, et al. Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med. 2008;359:2095–2104. doi: 10.1056/NEJMoa0708638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baedorf Kassis E, Su HK, Graham AR, Novack V, Loring SH, Talmor DS. Reverse trigger phenotypes in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2020; [DOI] [PMC free article] [PubMed]
- 4.Baedorf Kassis E, Loring SH, Talmor D. Lung volumes and transpulmonary pressure are decreased with expiratory effort and restored with passive breathing in ARDS: a reapplication of the traditional Campbell diagram. Intensive Care Med. 2018;44. [DOI] [PubMed]
- 5.Mojoli F, Iotti GA, Torriglia F, Pozzi M, Volta CA, Bianzina S, et al. In vivo calibration of esophageal pressure in the mechanically ventilated patient makes measurements reliable. Crit Care. 2016. [DOI] [PMC free article] [PubMed]
- 6.Baedorf Kassis E, Train S, MacNeil B, Loring SH, Talmor D. Monitoring of neuromuscular blockade: a comparison of train-of-four and the Campbell diagram. Intensive Care Med. 2018;44:2305–2306. doi: 10.1007/s00134-018-5420-5. [DOI] [PubMed] [Google Scholar]
- 7.Baedorf Kassis E, Loring SH, Talmor D, Terragni P, Mascia L, Ranieri VM. A fixed correction of absolute transpulmonary pressure may not be ideal for clinical use: discussion on “Accuracy of esophageal pressure to assess transpulmonary pressure during mechanical ventilation.” Intensive Care Med. 2017;43. [DOI] [PubMed]
- 8.De Santis Santiago R, Teggia Droghi M, Fumagalli J, Marrazzo F, Florio G, Grassi LG, et al. High pleural pressure prevents alveolar overdistension and hemodynamic collapse in ARDS with Class III obesity. Am J Respir Crit Care Med. 2020. [DOI] [PMC free article] [PubMed]
- 9.Fumagalli J, Santiago RRS, Teggia Droghi M, Zhang C, Fintelmann FJ, Troschel FM, et al. Lung recruitment in obese patients with acute respiratory distress syndrome. anesthesiology. 2019. [DOI] [PubMed]
- 10.Baedorf Kassis E, Loring SH, Talmor D. Mortality and pulmonary mechanics in relation to respiratory system and transpulmonary driving pressures in ARDS. Intensive Care Med. 2016. [DOI] [PubMed]
- 11.Amato MBP, Meade MO, Slutsky AS, Brochard L, Costa ELV, Schoenfeld DA, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015. [DOI] [PubMed]
- 12.Cressoni M, Amini M, Cadringher P, Chiurazzi C, Febres D, Gallazzi E, et al. Quantification of stress raisers in ARDS. Crit Care. BioMed Central; 2013;17:P105.
- 13.Mauri T, Yoshida T, Bellani G, Goligher EC, Carteaux G, Rittayamai N, et al. Esophageal and transpulmonary pressure in the clinical setting: meaning, usefulness and perspectives. Intensive Care Med. 2016. [DOI] [PubMed]
- 14.Protti A, Cressoni M, Santini A, Langer T, Mietto C, Febres D, et al. Lung stress and strain during mechanical ventilation: Any safe threshold? Am J Respir Crit Care Med. 2011. [DOI] [PubMed]
- 15.Schaefer M, Loring SH, Talmor D, Baedorf Kassis E. Comparison of mechanical power estimations in mechanically ventilated patients with the acute respiratory distress syndrome: a secondary data analysis from the EPVent study. Intensive Care Med. 2020;Under Revi. [DOI] [PubMed]