Abstract
The reduction of intraocular pressure is currently the only known modifiable risk factor for the treatment of Glaucoma, which is the leading cause of irreversible worldwide blindness. This concise review discusses the evidence underpinning the reduction of intraocular pressure in the treatment of glaucoma, the role of target intraocular pressure in clinical practice and appraises clinical data supporting the concept that every mmHg of intraocular pressure reduction is important in reducing the risk of developing glaucoma and the progression of existing disease. Every mmHg in IOP reduction is important, with evidence showing an impact on both functional and structural progression but does not however explain all glaucoma risk.
Keywords: Glaucoma, Intraocular Pressure, Rate of Progression
Glaucoma is the leading cause of irreversible worldwide blindness.[1] It is estimated to be responsible for visual impairment in almost six million people and blindness in three million people across the world.[2] It is also the underlying cause of approximately 10% of those registered as blind within the United States[3] and for almost one-third of sight loss certifications in England.[4]
The reduction of intraocular pressure (IOP) is currently the only known modifiable risk factor that has been borne out by large randomized controlled clinical trials to reduce both the risk of developing glaucoma and the progression of existing disease. Treatment to lower IOP in the ocular hypertension treatment study (OHTS) led to the risk of developing glaucoma at 5 years being reduced by half, from 9.5% to 4.4%.[5] The Collaborative Initial Glaucoma Treatment Study (CIGTS)[6] randomized newly diagnosed glaucoma patients to medical treatment or trabeculectomy and showed that the more aggressive IOP lowering achieved by surgery reduced visual field progression at 8 years in patients presenting with advanced glaucoma. More recently, the United Kingdom Glaucoma Treatment Study (UKGTS)[7] showed that treatment with a prostaglandin analog was effective in both lowering IOP and preserving the visual field in newly diagnosed patients at 2 years. IOP lowering has also been successful in reducing the risk of disease progression in patients with an existing diagnosis of glaucoma as shown by the Collaborative Normal Tension Glaucoma Study (CNTGS)[8] and the Early Manifest Glaucoma Trial (EMGT).[9]
The aim of glaucoma treatment is to prevent the onset and progression of disease in order to maintain visual function and quality of life across an individual patient's lifetime. This should be achieved at a sustainable financial cost to health-care systems and with a risk to benefit ratio acceptable to individual patients with respect to side effects from medication and surgical complications. The target IOP for an individual patient is defined by the European Glaucoma Society as an ”estimate of the mean IOP obtained with treatment that is expected to prevent further glaucomatous damage”[10] and as ”a range of IOP adequate to stop progressive pressure-induced injury” by the American Academy of Ophthalmology.[11] Several factors must be considered when estimating an individual target pressure including the baseline IOP, severity of glaucoma, lifetime risk of visual impairment, and rate of progression.
The landmark trials mentioned earlier unequivocally demonstrate that lowering IOP decreases the risk of both developing glaucoma and its subsequent progression. However, by design, these trials developed a target IOP target based upon a fixed percentage reduction from baseline. Reviewing the various IOP targets adopted by landmark clinical trials can provide some guidance on choosing an optimal target IOP [Table 1]. In ocular hypertensives with no manifest glaucoma, a 20% reduction in IOP may be sufficient.[5] Longer term follow-up of the OHTS cohort showed that the 13-year rate of developing glaucoma after initial randomization was 22% in the observation group compared to 16% in the treatment group.[12] However, the greatest absolute risk reduction was greatest among those participants at the highest baseline risk of developing glaucoma. The EMGT is relevant to cases of newly diagnosed mild–moderate glaucoma.[9] The intervention arm in this trial achieved a 25% reduction of IOP, and in this group, 45% showed evidence of progression at 5 years, compared with 62% of patients in the observation arm. The CNTGS showed that even in normal tension glaucoma, which is characterized by an IOP within normal limits, a further 30% lowering reduced the risk of glaucoma progression to 12% in the study group compared to 35% in the control arm.[8] The CIGTS participants had higher baseline IOPs, and IOP reduction was 40% and 35% in the surgery and medication arms, respectively.[13] In this study, visual field outcomes did not differ between treatment arms suggesting that the additional IOP lowering may not be not beneficial.
Table 1.
Intraocular pressure reduction - lessons from landmark trials
| Trial | Mean baseline IOP (mmHg) | Mean follow-up IOP (mmHg) | IOP reduction (%) | Endpoint at 5 years |
|---|---|---|---|---|
| OHTS[5] | 24.9 | 19.3 | 20 | 4.5% (treatment) |
| 9.5% (observation) | ||||
| EMGT[9] | 20.6 | 15.5 | 25 | 45% (treatment) |
| 62% (observation) | ||||
| CIGTS[6] | 28 | 14.5 (surgery) | 40 (surgery) | No difference |
| 17.5 (medical) | 35 (medical) | |||
| CNTGS[8] | 16.9 | 10.6 | 30 | 12% (treatment) |
| 35% (observation) |
IOP=Intraocular pressure, OHTS=Ocular Hypertension Treatment Study, EMGT=Early manifest glaucoma trial, CIGTS=Collaborative initial glaucoma treatment study, CNTGS=Collaborative Normal tension glaucoma treatment study
There is evidence, however, to support the need for a lower target pressure in advanced glaucoma. Further analysis of the CIGTS data showed that patients with more advanced baseline visual field loss (mean deviation <−10 dB) who underwent surgery showed reduced glaucoma progression at 7 years compared to those who received medical therapy.[6] The Advanced Glaucoma Intervention Study demonstrated that patients who achieved a lower IOP (<14 mmHg) during initial treatment were less likely to develop glaucomatous visual field deterioration, compared to patients with higher levels of IOP.[14] Patients with more severe baseline visual field damage were likely to progress rapidly, with the odds of visual field progression increasing by 11% for every 1dB worsening in mean deviation. These observations confirm that advanced disease at presentation is associated with an increased risk of progression, and therefore, a greater magnitude of IOP lowering will be beneficial to these patients.
The risk of lifetime glaucoma-related visual impairment varies among individuals and is influenced by age and rate of progression [Figure 1]. An older patient, diagnosed later in life with a moderate rate of progression, has a much lower chance of developing severe functional visual impairment in his/her lifetime, compared to a patient diagnosed at a younger age with an identical rate of progression. In contrast to a patient with moderate progression over years, rapidly progressing patients of any age need a considerably lower target IOP and more intensive treatment in order to prevent functional visual impairment.
Figure 1.
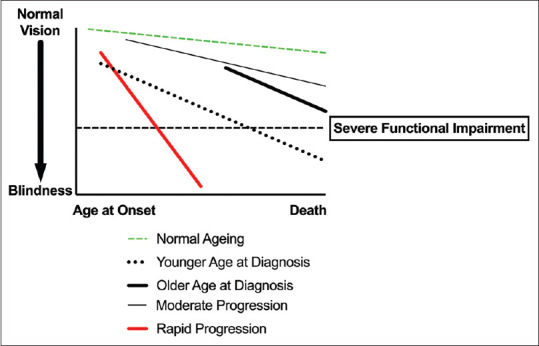
Risk of lifetime visual impairment – the relationship between age at diagnosis and rate of progression. (Adapted from the European Glaucoma Society Guidelines[10])
The rate of glaucoma progression is the major factor that determines the risk of visual impairment during a patient's lifetime. The challenge faced by glaucoma specialists is firstly to differentiate genuine progression from fluctuations in testing performance and normal aging and secondly to differentiate between slow and rapidly progressing patients. The rate of progression is a measurable parameter that can be calculated from serial visual field testing and is modifiable by treatment. Earlier treatment escalation or surgical intervention to lower IOP has the potential to reduce the risk of functional visual impairment in patients with rapidly progressing glaucoma [Figure 2], in particular in those patients of younger age and with more advanced disease at presentation.
Figure 2.
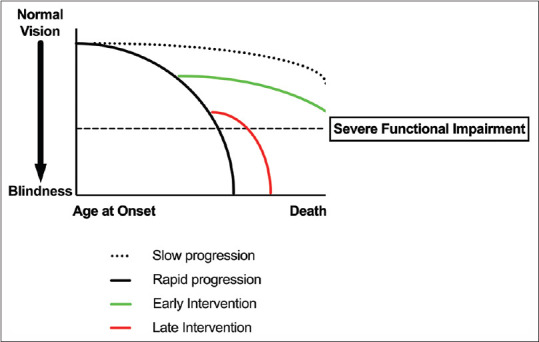
Risk of lifetime visual impairment – the relationship between the rate of progression and time of intervention. (Adapted from Caprioli and Zeyen[15])
The OHTS investigators showed that the risk of conversion from OHT to glaucoma increased by 10% for every 1 mmHg increase in baseline IOP.[16] The EMGT subsequently showed that each initial 1 mmHg reduction of IOP at the first follow-up visit in a cohort of patients with manifest glaucoma (3 months following treatment initiation) decreased the risk of progression by 8%, whereas each 1 mmHg increase in the mean IOP at the first follow-up visit increased the risk of progression by 13%.[17] Each 1 mmHg increase in mean IOP over the follow-up period for patients with a baseline IOP ≥21 mmHg was associated with a 15% increase in the risk of progression and was 13% for patients with a baseline IOP <21 mmHg. The Canadian Glaucoma Study prospectively followed up 258 patients over a median follow-up period of over 5 years.[18] and reported that a higher mean IOP was associated with glaucoma progression, with a 19% increase in risk per mmHg higher IOP. A retrospective study of glaucoma patients with 5 years of follow-up also showed that the odds of glaucoma progression were 13% higher for every mmHg increase in peak IOP.[19]
These concepts were broadly confirmed by the findings of the UKGTS investigators.[7] This double-masked randomized placebo-controlled trial reported a modest 2.9 mmHg IOP reduction at 2 years in the treatment group compared to the placebo. The adjusted hazard ratio of 0.44 for time to visual field deterioration in the treatment group corresponds to a reduction in risk of approximately 19% per mmHg reduction in IOP.
IOP levels have also been shown to be associated with structural progression using optical coherence tomography imaging to detect changes in retinal nerve fiber layer (RNFL) thickness.[20] This study reported a 3-year follow-up of over 500 eyes. Eight percent of eyes showed evidence of visual field progression, with progressing patients showing a greater annual RNFL change compared to those who were stable (−1.02 μm vs. −0.61 μm). The investigators also showed that the risk of additional annual RNFL loss for every 1 mmHg increase in IOP was greater in progressing eyes compared to stable eyes (−0.20 μm vs. −0.04 μm).
A study of treatment escalation showed that a greater IOP reduction was associated with a greater reduction in the rate of visual field progression in patients with primary open-angle glaucoma.[21] Interestingly, the escalation from triple to quadruple topical therapy did not further reduce the rate of progression or IOP lowering indicating that this should be the final threshold for considering surgical intervention.
This wide array of evidence supports the concept that to minimize the risk of patients developing glaucoma-related visual impairment, modulation of the disease early in its course before the onset of significant functional damage is of paramount importance [Figure 2].
The timely and appropriate intensity of treatment can, therefore, save sight. The ”Save Sight Years Engine” was developed by Allergan in conjunction with Professor Anders Heijl to help glaucoma specialists make evidence-based and individualized decisions on the intensity of glaucoma treatment.[22] Its objective is to help preserve vision across a patient's lifetime by maximizing the number of years of saved sight. The software is freely accessible and encourages best practice through frequent monitoring, regular calculation of the rate of progression, and the impact of tailored treatment from a patient's perspective.
It is important to emphasize, however, that a large number of untreated patients in the landmark clinical trials do not demonstrate glaucoma progression.[8,9,18] Although the evidence unequivocally suggests that every mmHg of IOP reduction can influence the risk of developing glaucoma and progression of existing disease, IOP reduction alone clearly does not explain all of the risks. It is also important to balance the risks of IOP reduction with the risk of surgical complications which can also negatively impact patients' vision and quality of life. The relationship between IOP lowering and glaucomatous injury is not necessarily linear, but it is reasonable to infer that a specific threshold exists for an individual eye below which the risk of IOP-induced optic nerve injury is minimal.
In conclusion, the lowering of IOP influences the risk of developing glaucoma and the progression of existing disease. Every mmHg in IOP reduction is important, with evidence showing an impact on both functional and structural progression. However, IOP alone does not explain all the risks, and therefore, future research should focus on addressing this significant unmet need in glaucoma care.
Financial support and sponsorship
The author has received lecture fees/travel expenses from Allergan to present this content in part at the ”Beyond” meeting in Taiwan, June 2019.
Conflicts of interest
The author declares that there are no conflicts of interest of this paper.
Acknowledgments
HJ is employed by Moorfields Eye Hospital NHS Foundation Trust. HJ is supported by the Moorfields Eye Charity. The views expressed in this paper are those of the author and not necessarily those of any funding body or the U.K. Department of Health.
References
- 1.Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: A systematic review and meta-analysis. Ophthalmology. 2014;121:2081–90. doi: 10.1016/j.ophtha.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 2.Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96:614–8. doi: 10.1136/bjophthalmol-2011-300539. [DOI] [PubMed] [Google Scholar]
- 3.Quigley HA, Vitale S. Models of open-angle glaucoma prevalence and incidence in the United States. Invest Ophthalmol Vis Sci. 1997;38:83–91. [PubMed] [Google Scholar]
- 4.Rahman F, Zekite A, Bunce C, Jayaram H, Flanagan D. Recent trends in vision impairment certifications in England and Wales. Eye (Lond) 2020;34:1271–8. doi: 10.1038/s41433-020-0864-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP, et al. The ocular hypertension treatment study: A randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120:701–13. doi: 10.1001/archopht.120.6.701. [DOI] [PubMed] [Google Scholar]
- 6.Musch DC, Gillespie BW, Lichter PR, Niziol LM, Janz NK. CIGTS Study Investigators. Visual field progression in the collaborative initial glaucoma treatment study the impact of treatment and other baseline factors. Ophthalmology. 2009;116:200–7. doi: 10.1016/j.ophtha.2008.08.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garway-Heath DF, Crabb DP, Bunce C, Lascaratos G, Amalfitano F, Anand N, et al. Latanoprost for open-angle glaucoma (UKGTS): A randomised, multicentre, placebo-controlled trial. Lancet. 2015;385:1295–304. doi: 10.1016/S0140-6736(14)62111-5. [DOI] [PubMed] [Google Scholar]
- 8.Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Collaborative normal-tension glaucoma study group. Am J Ophthalmol. 1998;126:487–97. doi: 10.1016/s0002-9394(98)00223-2. [DOI] [PubMed] [Google Scholar]
- 9.Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M, et al. Reduction of intraocular pressure and glaucoma progression: Results from the early manifest glaucoma trial. Arch Ophthalmol. 2002;120:1268–79. doi: 10.1001/archopht.120.10.1268. [DOI] [PubMed] [Google Scholar]
- 10.European Glaucoma Society Terminology and Guidelines for Glaucoma. 4th Edition-Chapter 3: Treatment principles and options Supported by the EGS Foundation: Part 1: Foreword; Introduction; Glossary; Chapter 3 Treatment principles and options. Br J Ophthalmol. 2017;101:130–95. doi: 10.1136/bjophthalmol-2016-EGSguideline.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prum BE, Jr, Rosenberg LF, Gedde SJ, Mansberger SL, Stein JD, Moroi SE, et al. Primary open-angle glaucoma preferred practice pattern(®) guidelines. Ophthalmology. 2016;123:P41–111. doi: 10.1016/j.ophtha.2015.10.053. [DOI] [PubMed] [Google Scholar]
- 12.Kass MA, Gordon MO, Gao F, Heuer DK, Higginbotham EJ, Johnson CA, et al. Delaying treatment of ocular hypertension: The ocular hypertension treatment study. Arch Ophthalmol. 2010;128:276–87. doi: 10.1001/archophthalmol.2010.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lichter PR, Musch DC, Gillespie BW, Guire KE, Janz NK, Wren PA, et al. Interim clinical outcomes in the collaborative initial glaucoma treatment study comparing initial treatment randomized to medications or surgery. Ophthalmology. 2001;108:1943–53. doi: 10.1016/s0161-6420(01)00873-9. [DOI] [PubMed] [Google Scholar]
- 14.The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. The AGIS Investigators. Am J Ophthalmol. 2000;130:429–40. doi: 10.1016/s0002-9394(00)00538-9. [DOI] [PubMed] [Google Scholar]
- 15.Caprioli J, Zeyen T. A critical discussion of the rates of progression and causes of optic nerve damage in glaucoma: International glaucoma think tank II: July 25-26, 2008, Florence, Italy. J Glaucoma. 2009;18:S1–21. doi: 10.1097/IJG.0b013e3181aff461. [DOI] [PubMed] [Google Scholar]
- 16.Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA, et al. The ocular hypertension treatment study: Baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120:714–20. doi: 10.1001/archopht.120.6.714. [DOI] [PubMed] [Google Scholar]
- 17.Leske MC, Heijl A, Hyman L, Bengtsson B, Dong L, Yang Z, et al. Predictors of long-term progression in the early manifest glaucoma trial. Ophthalmology. 2007;114:1965–72. doi: 10.1016/j.ophtha.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 18.Chauhan BC, Mikelberg FS, Balaszi AG, LeBlanc RP, Lesk MR, Trope GE, et al. Canadian glaucoma study: 2. Risk factors for the progression of open-angle glaucoma. Arch Ophthalmol. 2008;126:1030–6. doi: 10.1001/archopht.126.8.1030. [DOI] [PubMed] [Google Scholar]
- 19.De Moraes CV, Hill V, Tello C, Liebmann JM, Ritch R. Lower corneal hysteresis is associated with more rapid glaucomatous visual field progression. J Glaucoma. 2012;21:209–13. doi: 10.1097/IJG.0b013e3182071b92. [DOI] [PubMed] [Google Scholar]
- 20.Diniz-Filho A, Abe RY, Zangwill LM, Gracitelli CP, Weinreb RN, Girkin CA, et al. Association between Intraocular Pressure and Rates of Retinal Nerve Fiber Layer Loss Measured by Optical Coherence Tomography. Ophthalmology. 2016;123:2058–65. doi: 10.1016/j.ophtha.2016.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aptel F, Bron AM, Lachkar Y, Schweitzer C. Change in Visual Field Progression Following Treatment Escalation in Primary Open-angle Glaucoma. J Glaucoma. 2017;26:875–80. doi: 10.1097/IJG.0000000000000748. [DOI] [PubMed] [Google Scholar]
- 22.Allergan Save Sight Years Engine. [Last accessed on 2020 Oct 12]. Available from: https://ssyenginecom .


