Abstract
Background:
This study aimed to evaluate the clinical efficacy of the 2-step procedure used for treating entropion patients: (1) performing a grey line split incision and recessing the anterior lamella; (2) using full-thickness everting sutures of the eyelid to enhance the rotating effect.
Methods:
In total, 31 eyelids of 21 patients were reviewed (male–female ratio = 11:10), with each patient having either upper or lower, or both eyelid entropion due to various causes. All patients underwent the two-step procedure by eyelid splitting and full-thickness everting sutures at the Bundang Cha Hospital from August 2014 until July 2018.
Results:
The mean follow-up duration was 24.3 months (range, 14–107 months). The causes of entropion included involutional entropion (15 eyelids), congenital entropion (10 eyelids), and cicatrical entropion (6 eyelids). Surgery was re-performed on 16 eyelids due to recurrences from previous electrolysis or surgical correction of entropion such as capsulopalpebral fascia repair, full-thickness rotating suture, or folliculectomy. The two-step procedure was performed on all 31 eyelids, and 9 eyelids received additional excision of skin. After the 2-step procedure, patients showed improvement in symptoms, and all were satisfied with the contour of their eyelids. During the follow-up period, there were no recurrences or complications.
Conclusion:
A two-step procedure involving eyelid splitting and full-thickness everting sutures is an effective surgical method to treat entropion due to various causes, when compared with other conventional methods.
INTRODUCTION
Entropion is a malposition resulting in inversion of the eyelid margin. The morbidity of the condition is a result of ocular surface irritation and damage. Successful management of this condition depends on appropriate classification and a procedural choice that adequately addresses the underlying abnormality. Entropion can be divided into the following classes: congenital, acute spastic, involutional, and cicatricial.
Various surgical methods have been used to treat entropion. The Hotz procedure is a method involving excision of the skin and orbicularis oculi muscle in a crescent shape followed by suturing of the skin.1 Capsulopalpebral fascia repair is a method by which a surgeon makes a skin incision beneath the eyelashes, peels the skin and muscles down, and then attaches the lower eyelid retractor to the tarsal plate.2,3 In the Wies operation, a full-thickness eyelid skin incision is made in the horizontal direction of the eyelid margin and a suture passes through the skin from the posterior lamella of the proximal eyelid to the skin. The procedure is determined by the cause, pathology, and degree of entropion.4 We report the results of the smile procedure, which proved to be relatively simple, less invasive, and effective in the correction of entropion, with fewer complications and a lower recurrence rate.
MATERIALS AND METHODS
In this retrospective study, we reviewed case notes and photographs of 21 patients who underwent the smile procedure to correct either upper or lower, or both eyelid entropion between August 2014 and July 2018 at the Bundang CHA Hospital. In total, 31 eyelids of 21 patients were included in this study. Cases with accompanying trichiasis and distichiasis were not included in the study.
Patients’ demographic data, examination findings, surgical procedures, and follow-up results were evaluated retrospectively. Demographic data included age, sex, possible underlying etiology, history of previous treatment, and accompanying eyelid abnormalities. The surgery was performed either when corneal erosion caused by entropion was found during a slit lamp examination in more than 10% of the total cornea, or if patients complained of severe irritation. The patients were observed for at least a year after the operation. All procedures and follow-up monitoring were performed by a single surgeon. The Institutional Review Board (IRB) of the Bundang CHA Hospital approved this retrospective chart review.
Outcomes were assessed based on the review of case notes and comparison of standardized pre-and post-operative clinical photographs assessed by an independent reviewer. Outcome measures include the following: (1) improvement in eyelid margin position and retraction, (2) the direction of the lashes, (3) the corneal status, (4) improvement in symptoms, (5) cosmesis, (6) postoperative complications, and (7) the recurrence rate.
Surgical Technique
A local anesthetic infiltration using 2% lidocaine mixed with epinephrine at a ratio of 1:100,000 was administered subcutaneously in the subciliary skin and palpebral conjunctiva. The locations of where the sutures would be buried were marked about 1 mm below the cilia line (Fig. 1A). After grasping the eyelid with chalazion forceps, a 1- to 2-mm deep split incision was made along the gray line with a No. 15 scalpel blade (Fig. 1B). When the anterior lamella was sufficiently separated, a gap was created between the anterior and posterior lamella. The chalazion forceps were removed and 6-0 nylon suture was passed at previously marked skin stab incision to the palpebral conjunctiva through the inferior border of tarsal plate (Fig. 1C, D) Then it was repassed from the conjunctiva to the skin. This rotating suture strengthens the anterior lamellar recession. The suture was tied at the skin level and 3 more sutures were made at the other previous marks. After slightly pulling the eyelid margin outward, the sutures were buried at the point of the skin incision sites (Fig. 1E). They were placed between subcutaneous tissue and orbicularis muscle.
Fig. 1.
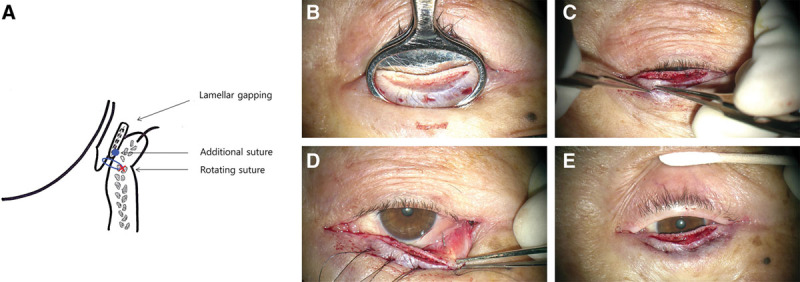
A, Schematic view of the eyelid section after the two-step procedure. B, With chalazion forceps, a split incision is made along the gray line. When anterior lamella was separated sufficiently, there was lamella gapping. C–D, Nylon suture passed from skin to palpebral conjunctiva through the inferior border of tarsal plate: everting suture. E, Adjustment of the position of the notes to make buried sutures.
The MRD2 and Eyelid Contour Analysis
The MRD2 (margin to reflex distance2) was measured from photographs, using Image J software. Each measurement was obtained with the assumption that the corneal diameter was 11.5 mm.5 Eyelid contour was assessed with a custom software developed by MATLAB (MathWorks, Natick, Mass.). The radial mid-pupil eyelid distance lengths were automatically calculated by the software and displayed on a polar plot.6–9 For intuitive understanding, the calculated distances were represented by graphs using an Excel 2010 spreadsheet (Microsoft, Redmond, Wash.).
RESULTS
The study included 31 eyelids (5 upper, 24 lower, and 1 pair of both eyelids) of 21 patients (11 men and 10 women) with a mean age of 53.2 years (range, 6–85 years, 53.2 ± 21.2) (Table 1). There are 4 main categories of entropion and our cases include 17 involutional entropions, 10 congenital entropions, 4 cicatricial entropions, and no spastic entropions.
Table 1.
Demographics and Clinical Characteristics of the Entropion Patients
| Indication | Previous Procedure | Combined Eyelid Condition | Procedure | Symptom Improvement | Lid Position | Recurrence | Complication |
|---|---|---|---|---|---|---|---|
| IV(ULLL:OS) | 20YA, entropion operation (LL:OU) 3YA, UBL (UL:OS) EL(ULLL:OS) EP(ULLL:OS) |
Nil | ALS + RS | FS + T+ US+ I | Everted | Nil | Nil |
| IV(LL:OU) | EP(LL:OU) | Nil | ALS + RS | FS + T | Everted | Nil | Nil |
| IV(LL:OS) | EP(LL:OS) | Nil | ALS + RS | FS + I | Everted | Nil | Nil |
| IV(LL:OD) | 3YA, entropion operation (LL:OD) EL(LL:OS) |
Nil | ALS + RS | FS + T | Everted | Nil | Nil |
| IV(LL:OU) | EL(LL:OU) EP(LL:OU) | Nil | ALS + RS | FS + US+ I | Everted | Nil | Nil |
| CG(LL:OU) | Nil | Nil | ALS + RS | FS | Everted | Nil | Nil |
| CC(LL:OS) | EP(LL:OS) | Tarsal conjunctival scar (LL:OS) | ALS + RS + AMT | FS + US | Everted | Nil | Nil |
| CG(LL:OU) | EP(LL:OU) | Nil | ALS + RS | FS + T+ I + S | Everted | Nil | Nil |
| IV(LL:OD) | 2YA, CPF repair(LL:OD) EP(LL:OD) |
Nil | ALS + RS | FS + T | Everted | Nil | Nil |
| IV(LL:OS) | FC(LL:OS) EL(LL:OS) EP(LL:OS) |
Trichiasis (LL:OS) | ALS + RS | I | Everted | Nil | Nil |
| IV(LL:OD) | Nil | Nil | ALS + RS | FS + I | Everted | Nil | Nil |
| IV(LL:OS) | EP(LL:OS) | Nil | ALS + RS | FS | Everted | Nil | Nil |
| CG(LL:OU) | 3YA, UBL (UL:OU) EP(LL:OU) |
Nil | ALS + RS | FS + I | Everted | Nil | Nil |
| IV(LL:OS) | Nil | Nil | ALS + RS | T | Everted | Nil | Nil |
| IV(LL:OS) | EL(LL:OS) | Nil | ALS + RS | I | Everted | Nil | Nil |
| IV(LL:OD) | Nil | Nil | ALS + RS | T | Everted | Nil | Nil |
| CG(LL:OU) | 3MA,BDTS(UL:OU) RS(LL:OU) EL(LL:OU) |
Nil | ALS + RS + SR + HP | FS + T+ I | Everted | Nil | Nil |
| CG(LL:OU) | Nil | Nil | ALS + RS + SR + HP | I | Everted | Nil | Nil |
| CC(UL:OD) | 40YA, entropion operation (UL:OU) | Dermatochalasis (UL:OU) | ALS + RS + SR + UBL | FS + I | Everted | Nil | Nil |
| CC(UL:OU) | EP(UL:OU) | Blepharoptosis (UL:OU) | ALS + RS + SR + UBL + LC | FS + T+ US | Everted | Nil | Nil |
| IV(UL:OU) | EL(UL:OU) | Dermatochalasis (UL:OU) | ALS + RS + SR + FC | FS + T | Everted | Nil | Nil |
ALS, anterior lamellar splitting; AMT, amniotic membrane transplantation; BDTS, buried double twisted suture; CC, cicatrical entropion; CG, congenital entropion; CPF repair, capsulopalpebral fascia repair; EL, electrolysis; EP, epilation; FC, folliculectomy; FS, foreign body sensation; HP, Hotz procedure; I, itching; IV, involutional entropion; LC, lateral canthoplasty; RS, rotating suture; S, sharp pain; SR, skin resection; T, tearing; UBL, upper blepharoplasty; US, unsatisfying shape.
The chief complaints were most commonly combinations of foreign body sensation, itching, and tearing. There were 25 eyelids (80.6%) with foreign body sensation, 17 eyelids (54.8%) with itching sense, 16 eyelids (51.6%) with tearing, 7 eyelids (22.6%) with unsatisfying shapes, and 2 eyelids (6.5%) with sharp pain. Seventeen eyelids (54.8%) were treated previously with repeated epilation. An estimated 14 eyelids (45.2%) had undergone surgical procedures other than epilation: only electrolysis in 6 eyelids (19.4%), only eyelid surgery in 4 (12.9%), and both electrolysis and eyelid surgery in 4 (12.9%). Six eyelids (19.4%) had additional eyelid abnormalities such as dermatochalasis (3 eyelids, 9.7%), blepharoptosis (2 eyelids, 6.5%), or tarsal conjunctival scars (1 eyelids, 3.2%).
Nine patients underwent bilateral surgeries: 7 had surgery to the left eye, and 5 to the right eye (one patient had surgery on both upper and lower lids of the left eye). All 31 eyelids underwent the smile procedure, and 9 eyelids received additional skin excisions. The mean duration of follow-up was 24.3 months (range, 14–107 months). Successful postoperative results were defined by improvement in eyelid margin position, which meant no lashes touching the globe, the resolution of symptoms, and satisfactory cosmesis. After the smile procedure, the symptoms of all patients had improved and all were satisfied with the shape of their eyelids. The lid contour was repaired to its original contour (Fig. 2). The MRD2 of 25 eyes of 18 patients who underwent the smile procedure on the lower eyelid increased from 5.4 ± 0.7 to 5.5 ± 0.7. The MRD2 of 10 eyes of congenital entropion patients increased from 5.3 ± 0.7 to 5.7 ± 0.9, and the MRD2 of 1 eye of cicatricial entropion patient decreased from 5.4 to 5.3. The MRD2 of 14 eyes of involutional entropion patients decreased from 5.5 ± 0.8 to 5.4 ± 0.6. They had no statistical significance (Fig. 3). During follow-up monitoring, there were no recurrences or complications such as ectropion, eyelid retraction, lagophthalmos, or epiphora.
Fig. 2.
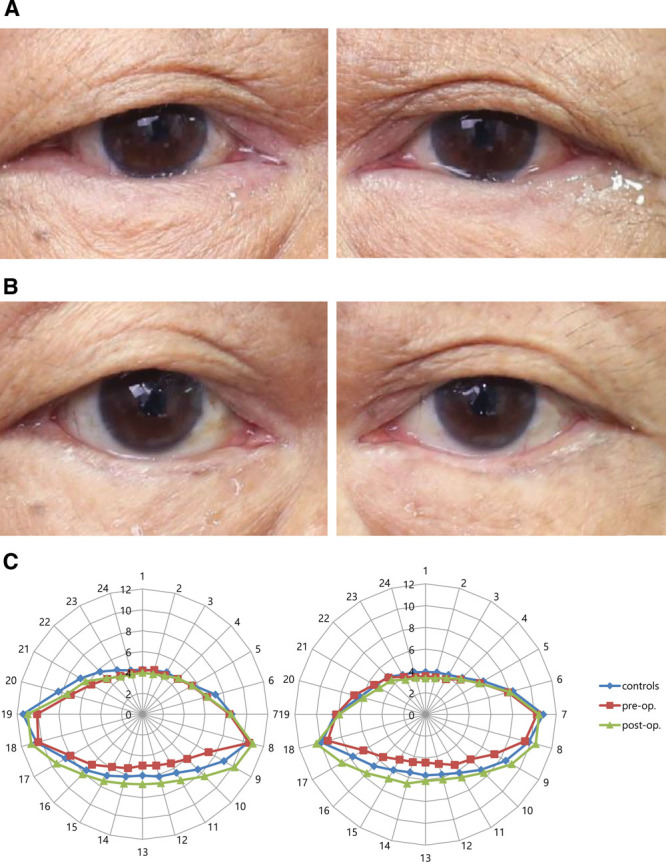
Clinical photographs of the eyelids with the diagnosis of entropion in a 79-year-old male. Both eyes with involutional lower lid entropion presented (A) preoperatively and (B) postoperatively. (C) Compared with the normal eyelid contour (blue lines), the contour was nearly normalized after the smile procedure.
Fig. 3.
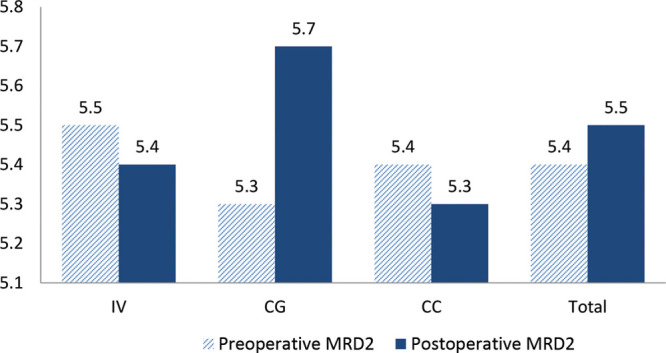
Comparison between preoperative and postoperative of MRD2 according to the type of entropion. IV, involutional entropion; CG, congenital entropion; CC, cicatrical entropion.
DISCUSSION
Eyelid margin malpositions include entropion, trichiasis, distichiasis, and epiblepharon. These diseases tend to be mentioned together because they have similar symptoms and overlapping treatments. However, they are distinguished from one another because their pathophysiologies are different. Therefore, accurate diagnosis is necessary for proper treatment. It is also important to make an accurate diagnosis for entropion through close examination because treatments are aimed specifically at the particular causes of the condition.
First, the physician should pay close attention to the position of the eyelid margin to evaluate if there is inward turning of the eyelids. If a patient is diagnosed with entropion, it is important to see whether the entropion is cicatrical or not. If it is not cicatrical, most of it is involutional. Therefore, doctors need to confirm this using an eyelid distraction test and a snap back test. Furthermore, it is also necessary to determine whether the entropion is congenital or spastic.
Most entropion patients commonly have eyelashes touching the cornea, causing conjunctiva and corneal scarring as well as corneal irritation symptoms. Therefore, turning the direction of the inwardly curved eyelashes outward can be a common treatment.
The authors designed the smile procedure, which involves performing a grey line split incision to recess the anterior lamella and a full-thickness everting suture to enhance the rotating effect, with or without skin excision. This procedure differs from other surgical procedures in that an entropion can be corrected without skin incision. Therefore, the procedure is less invasive and can make fewer scars because of the lack of a skin incision. Depending on the presence or absence of sagging eyelids, skin excision can be added. Because the gap between the anterior and posterior lamella after surgery looked similar to a smile, the procedure was named the smile procedure.
In terms of the lower eyelid position, we predicted that the smile procedure could increase the MRD2 by turning the lower lid outward. However, in this study, MRD2 was increased in 11 eyelids, decreased in 12 eyelids, and showed no change of value in 2 eye following the smile procedure. The reason why did not all the MRD2 of eyelids increase after surgery is probably due to the laxity of the eyelid as well as the elasticity of the capsulopalpebral fascia (CPF). MRD2 changes may be different according to the tension of the CPF. Regarding eyelids with partial or complete detachment of tarsal-capsulopalpebral fascia attachment, full-thickness rotating sutures may play a role in CPF repair by reinforcing cutaneous-capsulopalpebral fascia attachment and consequently decreasing MRD2.
Pandey et al10 used an approach of repositioning the levator-recession and anterior lamella through a grey-line approach for upper eyelid cicatrical margin entropion patients. This surgery is similar to our surgery in that it corrects entropion without a skin crease incision. However, it is only for cicatrical patients with lid retraction due to posterior lamellar contraction. The authors recessed not only anterior lamella but also the levator and posterior lamella, which can be invasive, especially after opening the orbital septum. This procedure is far more complex, time-consuming, and limited only to upper eyelid cicatrical margin entropion patients.
Bouazza et al11 used an approach of anterior lamellar resection with lid margin splitting of the upper eyelid in the treatment of cicatrical trachomatous entropion. Like the smile operation, this procedure tries to maintain the original anatomy of the upper eyelid as much as possible. However, this procedure does not recess the anterior lamella and only resects it after incision of the upper eyelid margin.
Ahmed and Abdelbaky12 used a technique to reposition the anterior lamellar by simple splitting of the lid margin in treating trachomatous trichiasis. This procedure also added excision of dysplastic lashes. After 6 months, 14.9% of the eyelids showed recurrence, while 66.1% were completely cured. However, residual eyelid entropion persisted in 2.66%, and 12.9% required another surgery. In the smile operation, full-thickness everting sutures reinforce rotating effects and also reduce the risk of recurrence.
Hwang et al13 used a technique of splitting the lid margin and excising the redundant skin and muscle during the surgical correction of epiblepharon. This method differs from our procedure in that it involves skin incision without rotating sutures, but it is similar in that it does not disturb the posterior lamella.
Choi et al14 reported that 30 eyelids of 22 marginal entropion patients underwent eyelid margin splitting and anterior lamellar repositioning via skin incision. The overall success rate was 90% with only 3 eyelids with recurrent trichiasis. There were no significant complications such as secondary ectropion or eyelid retraction and only 2 cases with minor complications of exposure of the buried 8-0 nylon suture knot. This method is also essential for excision of redundant tissue and tarsal fixation suture as in other surgical procedures.
Although the follow-up duration of our study is not long, it is noteworthy that there were no recurrences or side effects during follow-up monitoring. A possible side effect, however, could be the exposure of the buried sutures knots.
In conclusion, compared with other conventional methods, the smile procedure is a fast and simple surgical procedure that can help surgeons treat entropion with or without skin excision and has fewer numbers of recurrences and complications. The procedure has 2 steps: creating a gap between the anterior and posterior lamella, recessing the anterior lamella and reinforcing rotating effect by using full-thickness everting sutures. In terms of eyelids with laxity, the full-thickness rotating sutures can make the cutaneous-capsulopalpebral fascia attachment stronger and laxity can be improved secondarily. In addition, regardless of what surgical method, undercorrections, or recurrences the patient might have had, this procedure can still be used afterward.
Footnotes
Published online 9 December 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
REFERENCES
- 1.Ding J, Chen F, Zhai W, et al. Orbicularis oculi muscle transposition for repairing involutional lower eyelid entropion. Graefes Arch Clin Exp Ophthalmol. 2014; 252:1315–1318. [DOI] [PubMed] [Google Scholar]
- 2.Jones LT. The anatomy of the lower eyelid and its relation to the cause and cure of entropion. Am J Ophthalmol. 1960;49:29–36. [PubMed] [Google Scholar]
- 3.Kreis AJ, Shafi F, Madge SN. Transconjunctival entropion repair – the backdoor approach. Orbit. 2013;32:271–274. [DOI] [PubMed] [Google Scholar]
- 4.Serin D, Buttanri IB, Karslioglu S, et al. The efficacy of the combined procedure in involutional entropion surgery: a comparative study. Korean J Ophthalmol. 2013;27:405–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mashige KP. A review of corneal diameter, curvature and thickness values and influencing factors. South African Optometrist. 2013;72:185–194. [Google Scholar]
- 6.Sung Y, Park JS, Lew H. Clinical outcomes of frontalis sling using silicone rod with two-point brow incisions in blepharoptosis. J Pediatr Ophthalmol Strabismus. 2016;53:224–232. [DOI] [PubMed] [Google Scholar]
- 7.Kang D, Lee J, Park J, et al. Analysis of lid contour in thyroid eye disease with upper and lower eyelid retraction using multiple radial midpupil lid distances. J Craniofac Surg. 2016;27:134–136. [DOI] [PubMed] [Google Scholar]
- 8.Milbratz GH, Garcia DM, Guimarães FC, et al. Multiple radial midpupil lid distances: a simple method for lid contour analysis. Ophthalmology. 2012;119:625–628. [DOI] [PubMed] [Google Scholar]
- 9.Ribeiro SF, Milbratz GH, Garcia DM, et al. Lateral and medial upper eyelid contour abnormalities in graves orbitopathy: the influence of the degree of retraction. Ophthalmic Plast Reconstr Surg. 2013;29:40–43. [DOI] [PubMed] [Google Scholar]
- 10.Pandey N, Jayaprakasam A, Feldman I, et al. Upper eyelid levator-recession and anterior lamella repositioning through the grey-line: Avoiding a skin-crease incision. Indian J Ophthalmol. 2018;66:273–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bouazza M, Elbelhadji M, Cherkaoui S, et al. [Anterior lamellar resection with lid margin split of the upper eyelid in the treatment of trachomatous entropion]. J Fr Ophtalmol. 2017;40:453–459. [DOI] [PubMed] [Google Scholar]
- 12.Ahmed RA, Abdelbaky SH. Short term outcome of anterior lamellar reposition in treating trachomatous trichiasis. J Ophthalmol. 2015;2015:568363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hwang SW, Khwarg SI, Kim JH, et al. Lid margin split in the surgical correction of epiblepharon. Acta Ophthalmol. 2008;86:87–90. [DOI] [PubMed] [Google Scholar]
- 14.Choi YJ, Jin HC, Choi JH, et al. Correction of lower eyelid marginal entropion by eyelid margin splitting and anterior lamellar repositioning. Ophthalmic Plast Reconstr Surg. 2014;30:51–56. [DOI] [PubMed] [Google Scholar]


