Summary:
Regional analgesia has been increasing in popularity due to its opioid- sparing analgesic effects and utility in multimodal analgesia strategies. Several regional techniques have been used in plastic surgery; however, there is a lack of consensus on the indications and the comparative efficacy of these blocks. The goal of this review is to provide evidence-based recommendations on the most relevant types of interfascial plane blocks for abdominal and breast surgery. A systematic search of the PUBMED, EMBASE, and Cochrane databases was performed to identify the evidence associated with the different interfascial plane blocks used in plastic surgery. The search included all studies from inception to March 2020. A total of 126 studies were included and used in the synthesis of the information presented in this review. There is strong evidence for using the transversus abdominis plane blocks in both abdominoplasties as well as abdominally-based microvascular breast reconstruction as evidenced by a significant reduction in post-operative pain and opioid consumption. Pectoralis (I and II), serratus anterior, and erector spinae plane blocks all provide good pain control in breast surgeries. Finally, the serratus anterior plane block can be used as primary block or an adjunct to the pectoralis blocks for a wider analgesia coverage of the breast. All the reviewed blocks are safe and easy to administer. Interfascial plane blocks are effective and safe modalities used to reduce pain and opioid consumption after abdominal and breast plastic surgery.
INTRODUCTION
The last several years witnessed a significant increase in opioid-related overdose deaths in the United States.1 Due to the fast, and often effective, analgesic effect of opioids, they are frequently used as method of post-operative pain control.2 Regional/local analgesic techniques are an important component of a multimodal analgesic strategy, with the aim of reducing opioid requirements and opioid-related adverse events.3 This change parallels quality improvement initiatives and the Enhanced Recover After Surgery pathways implemented in many hospitals in North America.4,5
In recent years, there has been an increasing trend toward administration of interfascial plane blocks [eg, transversus abdominis plane (TAP) blocks, pectoralis (PECS I and II) blocks, serratus anterior plane (SAP) blocks, and erector spinae plane blocks (ESPBs)].6 These blocks are purported to be technically easier and safer, and are amenable to be administered by surgeons.7 Due to the broad breadth of plastic surgeries and the wide array of anatomical locations that plastic surgeons operate on, an extensive number of regional analgesic techniques have been investigated within plastic surgery.8,9
To that end, the goal of this practical review is to present clinically-relevant, evidence-based recommendations of the most commonly used regional blocks in abdominal and breast plastic surgery. Specifically, the review will focus on interfascial plane blocks that can be performed directly by plastic surgeons. The review will highlight the technique, indications in plastic surgery, analgesic efficacy, as well as potential complications or challenges associated with these blocks. The ultimate aim of this review is to facilitate their use by plastic surgeons and trainees and gain a widespread use to improve perioperative pain relief, while reducing opioid requirements. Of note, surgical site infiltration techniques are outside the scope of this review.10
Methods
A systematic search of the PUBMED, EMBASE, and Cochrane databases was performed using a combination of keywords and MeSH terms, including “transversus abdominis block,” “pectoral nerve block,” “serratus anterior block,” “erector spinae plane block,” “interfascial plane block,” AND “plastic surgery.” All studies from January 1980 to March 2020 were considered. Inclusion criteria comprised randomized controlled trials, prospective and retrospective cohort studies, as well case series that discussed regional blocks in plastic surgery. Studies assessing the effect of blocks on mastectomies were included, given the significant overlapping relevance to plastic surgery breast procedures. Exclusion criteria included the use of regional analgesia techniques in non-plastic surgery procedures with no overlapping relevance. Studies that included more than 1 block in a group of participants without sub-analyses were excluded. Moreover, clinical studies with less than 10 participants were also excluded. A qualitative analysis of all the included studies was preformed, and recommendations regarding indications, efficacy, and safety were presented.
RESULTS
The primary search yielded a total of 1049 articles, which were assessed for relevance based on their title and abstract. The initial review yielded 376 articles that were then fully read and assessed against the inclusion and exclusion criteria, of which 126 were included and used in the synthesis of the information presented in this review.
Transversus Abdominis Block
Administration Technique
The TAP block was originally described in 2001 by Rafi.11 Although it was first described as a an ultrasound-guided interfascial block, the technique has been modified to allow direct administration by surgeons, typically within the context of abdominal wall reconstruction, but it also has uses in other types of plastic surgical procedures, including abdominoplasty. To successfully administer the TAP block by direct injection in abdominal wall reconstruction (specifically a transversus abdominis release, or “posterior components separation”), the surgeon should separate the posterior rectus sheath from the recuts muscle. The transversus abdominis muscle is released at its insertion point on the posterior rectus sheath. The abdominal wall should be retracted upward by the surgical assistant. The needle is inserted through the transversus abdominis muscle to the plane between the transversus abdominis and the internal oblique. Multiple injections are used to create continuous coverage from the costal margin to the iliac crest bilaterally. A total of 20 cm3 of 0.2% ropivacaine should be injected bilaterally as a single dose, or a 6–8 ml/hour of 0.2% ropivacaine with 2 ml boluses every 20 minutes as a continuous infusion. (See Video 1 [online], which displays the intra operative surgeon administering transversus abdominis plane block.)
Video 1. Video 1 from “Practical Review of Abdominal and Breast Regional Analgesia for Plastic Surgeons: Evidence and Techniques”.
We recommend using ropivacaine as the choice of anesthetic because it is associated with less risk of cardiovascular and central nervous system adverse events compared with other local anesthetics such as bupivacaine. It is also associated will less intense motor blockade, which leads to a faster rate of recovery and patient ambulation.12,13
The TAP block can also be administered under ultrasonography. In a supine position, a linear probe should be placed right above the iliac crest in a cranial-to-caudal orientation. This allows identifying the external oblique, internal oblique, and transversus abdominis muscles in this order, from anterior to posterior. The probe should then be turned 90 degrees while still visualizing all 3 muscles. The needle is then inserted 3–4 cm medially from the probe at a 30-degree angle and advanced until it reaches the plane between the internal oblique and the transversus abdominis muscle. A total of 20 cm3 of 0.2% ropivacaine (or equivalent) should be injected bilaterally11 (Fig. 1).
Fig. 1.
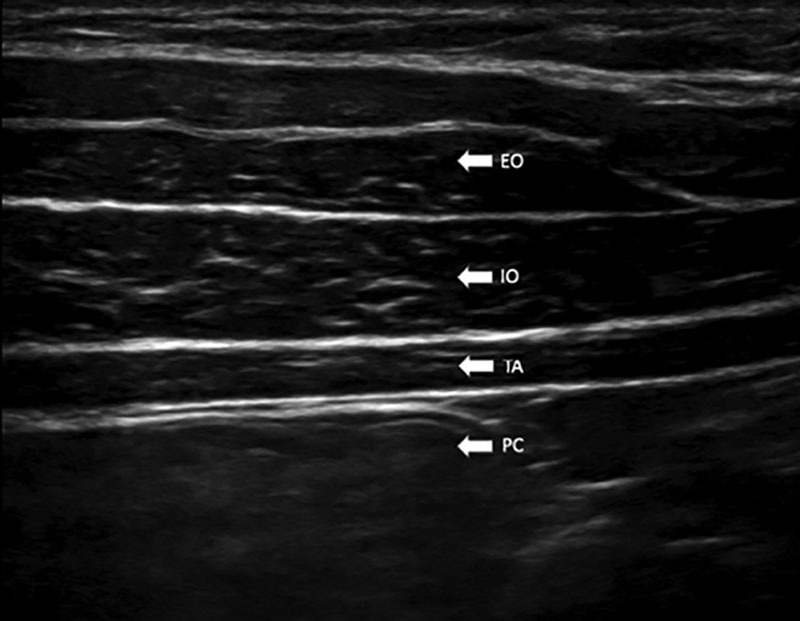
Ultrasound view of the transversus abdominal plane block. EO: external oblique, IO: internal oblique, TA: transversus abdominis, PC: peritoneal cavity.
Indications in Plastic Surgery
The 2 types of plastic surgeries with strong evidence for using the block are microvascular abdominal-based autologous breast reconstruction and abdominoplasty. Two meta-analyses demonstrated that TAP blocks decrease post-operative pain and opioid consumption in patients undergoing the two aforementioned surgeries.14,15 In terms of Level 1 evidence, a total of 5 RCTs assessed the effect of TAP block in plastic surgery, all of which showed a decrease in post-operative pain and/or opioid consumption in patients undergoing abdominally-based autologous breast reconstruction or abdominoplasties when compared with those received general anesthesia (GA) only.16–20 All RCTs used conventional local anesthetic, while only 1 RCT compared conventional and liposomal bupivacaine (prolonged release formulation) in patients undergoing autologous breast reconstruction and found no difference in any outcome between the two types of local anesthesia.20
In terms of non-level 1 evidence, 16 studies assessed the efficacy of the TAP block in the context of plastic surgery. The vast majority of the studies demonstrated a reduction in post-operative pain and/or opioid consumption after abdominally-based autologous breast reconstruction and abdominoplasty. Only 1 retrospective study assessed the effects of the TAP block in patients who had abdominal wall reconstruction and found that it was associated with a significant decrease in post-operative pain and opioid consumption during the first 2 days post-operatively.21 The majority of the studies used a conventional local anesthetic such as bupivacaine, while only 4 studies used liposomal bupivacaine.21–24 Jablonka et al. compared single-dose liposomal bupivacaine and conventional lidocaine infusion TAP blocks in patients undergoing microvascular abdominally-based breast reconstruction.25 They showed that TAP block with either liposomal bupivacaine or conventional lidocaine caused a significant reduction in opioid consumption compared with patients who received GA only. While there was no difference in opioid consumption between the 2 former groups, patients who received liposomal bupivacaine had a significantly shorter hospital stay than those who received the continuous infusion of lidocaine.
Complications
There were no reported complications associated with the TAP block in plastic surgery. However, there has been one reported complication of this block after a caesarian delivery where there was a transient femoral nerve palsy with involvement of the sacral plexus.26 High concentrations/volume of local anesthesia coupled with the increased pressure of the abdominal binder might have increased the risk of this complication. This block is safe to administer under direct visualization or ultrasonography due to the absence of vital structures in the immediate vicinity of the site injection.
Pectoralis (PECS) Block
Administration Technique
The PECS was first described by Blanco in 2011 as an alternative to other regional blocks such as paravertebral and epidural blocks, which have a relatively high rate of complications.27 It was initially used for sub-pectoral implant-based breast reconstruction. The block was initially described as an ultrasound-guided technique but can also be administered under direct visualization by plastic surgeons. After identifying the pectoralis major and minor muscles intraoperatively, the surgeon should inject 20 cm3 of local anesthetic in the plane between the muscles at the level of the third rib. Injection should be performed in a cephalad-to-caudal direction. Once the surgeon is in the right plane, the local anesthetic should spread easily with minimal resistance. Multiple injections could be performed to ensure optimal spread within the plane. (See Video 2 [online], which displays the intra operative surgeon administering pectoralis nerve blocks.)
Video 2. Video 2 from “Practical Review of Abdominal and Breast Regional Analgesia for Plastic Surgeons: Evidence and Techniques”.
The block can also be administered under ultrasonography. A liner probe is placed in a paramedian orientation at the level between the second and the third rib. The probe is then rotated 90 degrees and slid toward the lateral aspect of the chest wall. This view allows identifying the pectoralis major and minor muscle as well as the pectoral branch thoracoacromial artery, which lies between both muscles. The lateral pectoral nerve is reliably located adjacent to that artery. Caution should be taken when advancing the tip of the needle to avoid intra-arterial injection. Color Doppler can be used to help visualize the artery. A total of 20 cm3 of 0.2% ropivacaine (or equivalent) is injected into the interfascial plane, which contains the lateral pectoral nerve. A catheter can also be used for continuous infusions up to 7 days post insertion27 (Fig. 2).
Fig. 2.
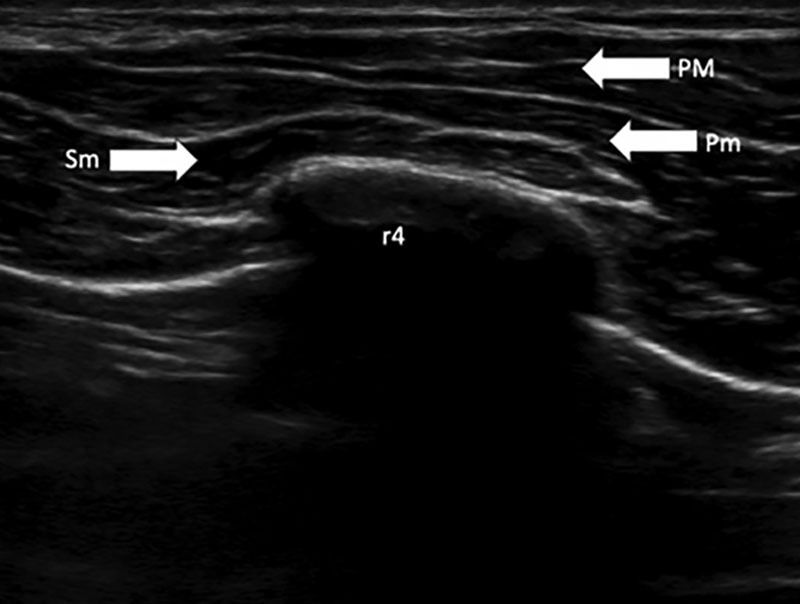
Ultrasound view of pectoral nerve blocks with respect to the fourth rib. SM: serratus anterior muscle, PM: pectoralis major muscle, Pm: pectoralis minor muscle.
Indications in Plastic Surgery
The strongest indication for a PECS blocks is in breast cancer surgery such as mastectomies. Two systematic reviews and meta-analysis with over 940 unique participants who underwent mastectomies/breast tumor excision demonstrated a significant decrease in opioid consumption when compared with general anesthesia alone.28,29 A total of 6 level-1 RCTs assessed the efficacy of a PECS block in breast surgery.30–35 Four of these showed a significant decrease in post-operative pain and/or opioid consumption in patients undergoing mastectomies who received a PECS block compared with those who did not.31–33,35 One RCT showed no difference in pain or opioid consumption in patients undergoing a modified radical mastectomy between those who received a PECS block or a paravertebral block (PVB).34 Finally, 1 RCT showed that adding dexmedetomidine to the local anesthetic in the block led to significantly better analgesia in patients undergoing a modified radical mastectomy.30 In terms of non-level 1 clinic studies, all the studies found showed a decrease in post-operative pain and/or opioid consumption in patients post breast surgeries.
Complications
The vast majority of the published literature on PECS blocks in breast surgery have deemed it safe and reliable. One case series of 498 consecutive patients who received the PECS block demonstrated a hematoma incidence rate of 1.6%. No other block-related complications were reported.36
Modified Pectoralis (PECS II) Block
Administration Technique
In 2012, the modified pectoralis block (PECS II) was developed by Blanco et al to include wider breast analgesic coverage.37 In addition to blocking the lateral pectoral nerve, which lies between the pectoralis major and minor muscles (same technique as PECS described above), PECS II includes a second injection of a local anesthetic between the pectoralis minor and the serratus muscles. This block could be injected by plastic surgeons under direct visualization by first performing a PECS I block. This is followed by another injection of 10–20 cm3 of 0.2% ropivacaine (or equivalent) between the pectoralis minor and serratus anterior muscle at the level of the third rib. The goal of the second injection is to block the long thoracic nerve as well as the lateral branches of at least two intercostal nerves (T2–T4). (See Video 2 [online], which displays the intra operative surgeon administering pectoralis nerve blocks.)
Ultrasound-trained plastic surgeons can also administer the PECS II block under ultrasonography. A linear probe is placed under the lateral third of the clavicle. After identifying the subclavian muscle, the axillary artery and vein, the probe is moved distally toward the axilla until the pectoralis minor is found. The serratus anterior should be identified at this location as a muscle that covers the second, third, and fourth ribs. The local anesthetic should be injected in the plane between the serratus anterior and the pectoralis minor muscles37 (Fig. 2).
Indications in Plastic Surgery
The indications for PECS II are similar to PECS; however, it theoretically should provide a wider breast analgesic coverage. Two systematic reviews and meta-analysis with over 800 unique patients demonstrated that PECS II significantly decreases post-operative pain and opioid consumption in patients undergoing breast cancer resection surgeries.38,39 In terms of level-1 evidence, 16 RCTs assessed the efficacy of PECS II on breast cancer surgeries.40–55 All showed significant reduction in post-operative pain and/or opioid consumption following breast surgery. Two RCTs showed that PECS II significantly reduced post-operative pain and opioid consumption in patients undergoing modified radical mastectomy compared to their counterparts who received a PVB block.47,51 Similarly, 2 RCTs comparing PECS II with ESPB showed that the former significantly reduced pain and opioid consumption compared with the latter. Only 1 RCT assessed the efficacy of PECS II in patients undergoing latissimus dorsi breast reconstruction and has found that it led to significant decreases in post-operative pain and opioid consumption compared with controls (GA only). Finally, Schultemaker et al demonstrated that a combination PECS II plus a serratus anterior block (SAB) reduced acute post-operative pain in patients undergoing breast augmentation but did not evidence any change in opioid consumption compared with controls (GA only). However, this study was limited by a small sample size of 30 patients.49
In terms of non-level-1 evidence studies, several cohort studies demonstrated the efficacy of PECS II in reducing post-operative pain and opioid consumption compared to both controls (general anesthesia only), and serratus anterior plane blocks.56–58 Several case reports show that PECS II provided sufficient analgesia without GA in patients undergoing breast conserving surgery.59,60 However, the evidence for using PECS II without GA is sparse and should only be considered as a last resort option.
Complications
None of the aforementioned studies reported any complications with regard to the PECS II block. PECS II block is a relatively safe regional block due to several reasons. The first of which is that the needle is relatively distant from the pleura and epidural space, which decreases the theoretical risk of pneumothorax and epidural hematomas. However, the authors recommend caution when injecting the needle in the specified fascial plane due to its proximity with the thoracoacromial artery, which should be easily identified and avoided using ultrasonography.
Serratus Anterior Plane Block
Administration Technique
The SAP block was first described by Blanco et al in 2013.61 The block was developed after detailed anatomy studies that showed that there are 2 spaces above and below the serratus anterior muscle that PECS and PECS II blocks miss. This block is often added as an adjunct to the PECS II block. To administer the block under direct visualization, the surgeon should identify the serratus anterior and the latissimus dorsi muscle laterally. A total of 20 cm3 of 0.2% ropivacaine (or equivalent) should be injected in the plane between these muscles at the level of the fifth rib. A blunt cannula is used to avoid injuring any important structures.
The SAP block can also be administered under ultrasonography. In a supine position, a linear probe is placed over the mid-clavicular line at the fifth rib in a sagittal plane. At this level, the administrator should identify the latissimus dorsi muscle (superficial and posterior), the serratus anterior muscle (deep and inferior) and the teres minor muscle (superior). Color Doppler can be used to help identify thoracodorsal artery. This artery is used as a landmark to identify the right plane superficial to the serratus anterior muscle. A needle is then inserted in the plane of the ultrasound probe, advanced 1–2 cm (depends on body habitus), and used to inject 20 cm3 of 0.2% ropivacaine (or equivalent) both superficial and deep to the serratus anterior muscle (Fig. 3).
Fig. 3.
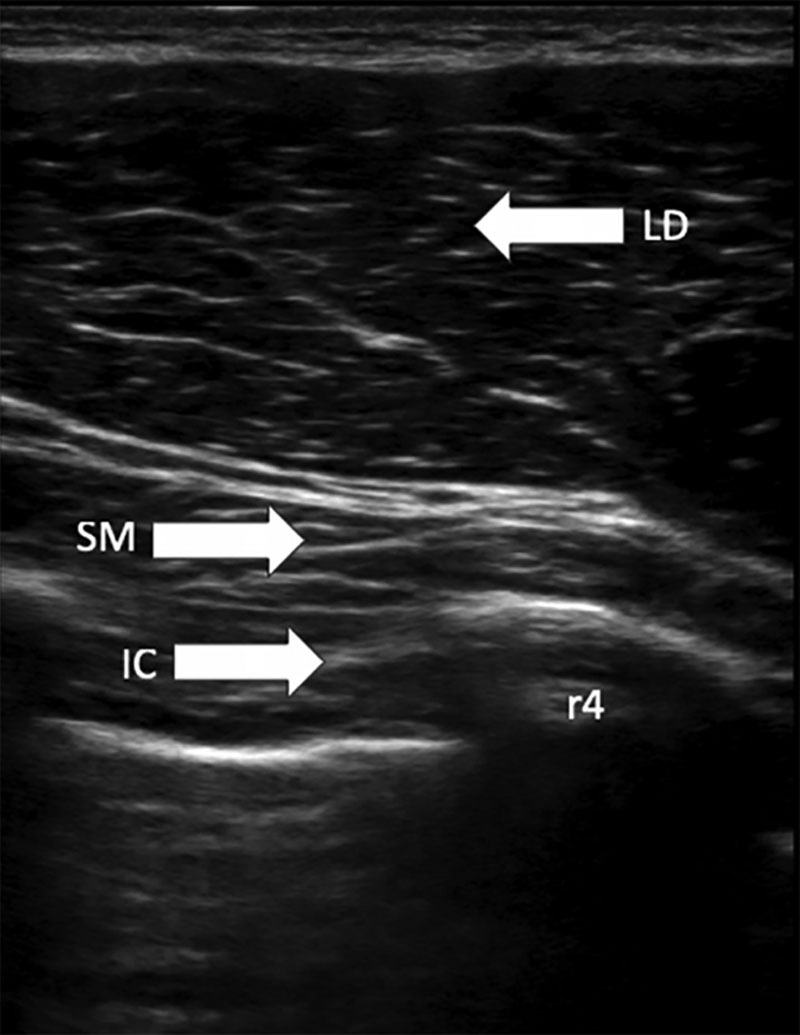
Ultrasound view of the serratus anterior plane block with respect to the fourth rib. SM: serratus anterior muscle; LD: latissimus dorsi muscle; IC: intercostal muscles.
Indications in Plastic Surgery
The indications for using a SAP block are very similar to PECS and PECS II blocks. Three RCTs assessing the effect of SAP blocks in patients who underwent mastectomies found the block significantly lowered post-operative pain and opioid consumption compared with controls.62–64 Two other RCTs assessed the efficacy of varying volumes and concentrations of the local anesthetic used in the SAP block.65,66 They found that increasing the volume of the local anesthetic increases dermatomal anesthesia coverage; however, it does not increase the duration of block or the overall post-operative pain. On the other hand, increasing the concentration of bupivacaine from 0.375% to 0.5% led to significantly lowered pain and longer duration of anesthesia. There was no further effect by increasing the dosage above 0.5%.
All non-level-1 evidence studies concluded that the SAP block provides good analgesia in patients undergoing breast surgeries.9,67–70 Specifically, Homsy et al demonstrated using a case series of 33 patients that a PECS and SAP blocks together provided good pain control post operatively as well as a reduction in opioid consumption in patients undergoing sub-pectoral breast reconstruction and augmentation.9 Similarly, Khemka et al demonstrated that all 11 patients undergoing latissimus dorsi breast reconstruction included in their cases series were pain free up until 9 hours post operatively and none of them used any post-operative opioids during their hospital stay.69
Complications
An infrequent potential complication of the SAP block is pneumothorax. However, because the fascial planes targeted by the SAP blocks are superficial to the ribs, it is very rare. However, due to the seriousness of this complication, it is important to always visualize the pleural line (clearly identifiable on ultrasound) before advancing the needle. Overall, the SAP block is a very safe and relatively easy block to perform.
Erector Spinae Plane Block
Administration Technique
The ESPB was developed in 2016 as a thoracic regional block.71 This block is usually administered by anesthesiologists under ultrasonography in the preoperative setting to avoid repositioning the patient intraoperatively, which can be challenging. It can be administered in a sitting or a lateral position. A linear high frequency ultrasound probe is placed 3 cm lateral to the midline at the level of the T5 spinous process. At this level, one should identify the trapezius, rhomboid major, and erector spinae muscles. All 3 muscles should be superficial to the transverse process (which is hyperechoic on ultrasound). A 8-cm long 22-gauge needle is inserted in a cephalad-to-caudal direction until the needle tip reaches the fascial plane between the rhomboid major and the erector spinae muscle. A total of 20 cm3 of 0.25% bupivacaine (or equivalent) is injected in that fascial plane. This is confirmed by seeing a clear spread of the local anesthetic between the muscles. This block should provide anesthesia from T2 to T9 cephalocaudal and between the midclavicular line to a hypothetical line 3 cm lateral to the midline (thoracic spine)71 (Fig. 4).
Fig. 4.
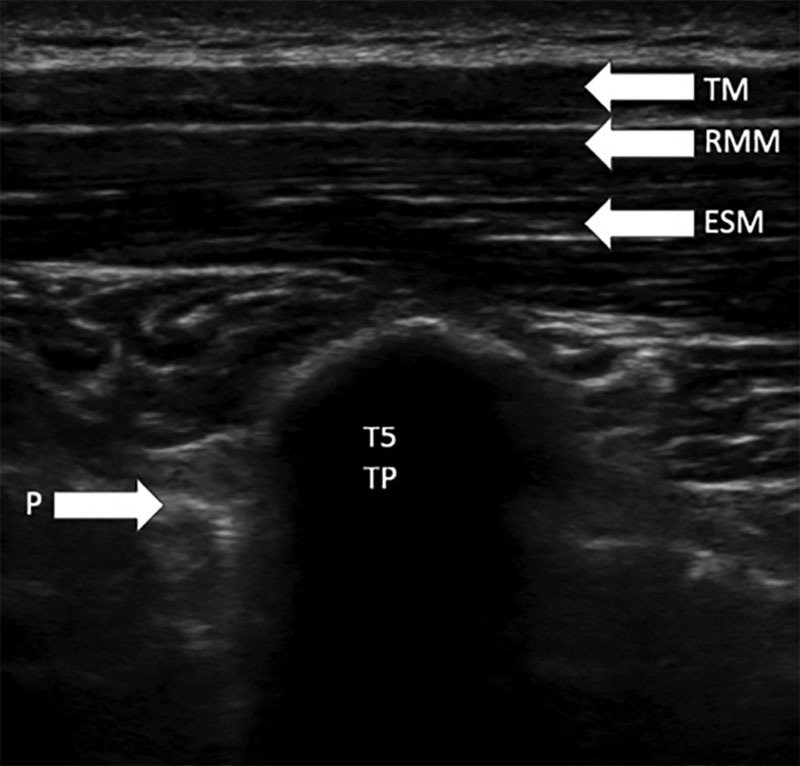
Ultrasound view of erector spinae plane block with resepct to the fifth thoracic transverse process (T5 TP). P: pleura, TM: trapezius muscle, RMM; rhomboid major muscle, ESM: erector spinae muscle.
Indications
ESPB was originally described as a block for neuropathic pain of the thorax.71 However, due to its ease of administration, it quickly evolved to be used across many other domains. Within plastic surgery, ESPB is indicated for breast surgeries.8 Although the evidence shows that it is quite effective in reducing post-operative pain and opioid consumption compared with controls (GA only), comparative studies present mixed evidence. A total of 12 level-1 evidence RCTs assessed the efficacy of ESPB on breast surgeries. Specifically, 5 RCTs demonstrated that ESPB significantly reduced post-operative pain and/or opioid consumption in patients undergoing mastectomies compared with controls (GA only).72–76 Similarly, one RCT showed that patients undergoing breast reduction who received an ESPB block had a significantly lower post-operative pain and opioid consumption compared with those who received tumescent anesthesia.77 When comparing ESPB with PVB, 3 RCTs demonstrated no significant differences in the aforementioned outcomes between the 2 blocks,73,78,79 while only 1 RCT concluded that PVB is associated with significantly less pain and opioid consumption compared with ESPB.80 However, when ESPB was compared with a PECS block, all RCTs demonstrated that the latter led to significantly lower post-operative pain and opioid consumption compared with the former block.41,45,52 Finally, only 1 RCT showed that increasing the concertation of bupivacaine from 0.25% to 0.375% led to a further decrease in pain and opioid consumption within the first 24 hours post-surgery.
In terms of non-level-1 evidence, 1 retrospective cohort study showed that ESPB significantly reduced post-operative pain and opioid consumption in patients undergoing total mastectomies.81 More interestingly, Malawat et al conducted a case series of 30 patients undergoing modified radical mastectomies with an ESPB block only (with no GA). They showed that all 30 patients achieved good pain control and none of them required conversion to GA.82 Several smaller case reports/series demonstrate the efficacy of ESPB on both autologous and implant-based breast reconstruction.83,84
Complications
The ease of identification of the ultrasound landmarks coupled with the absence of vital structures in the immediate vicinity of the site of injection makes ESPB a relativity safe and simple block to administer. ElHawary et al reviewed all cases of ESPB in the literature and showed that only 3 of 319 cases presented with complications. Two of these were considered minor (inadequate intraoperative analgesia), while the third was a pneumothorax that developed 3 minutes after ESPB administration.8
SUMMARY AND CONCLUSIONS
Several effective, evidence-based regional blocks are indicated for abdominal and breast plastic surgery. There is strong evidence for the use of TAP blocks in abdominal-based flap reconstruction and abdominoplasties. TAP blocks should also be used in abdominal wall reconstruction surgeries; however, the supporting evidence is limited (only 1 retrospective study). For breast surgeries, the authors would recommend using PECS and/or PECS II as their primary choice of regional block. Moreover, there is strong evidence for the use of SAP blocks in breast surgeries. The SAP block could be as a primary block or as an adjunct to the PECs blocks. Finally, there is strong evidence that ESPB blocks are effective in reducing post-operative pain and opioid consumption; however, preliminary evidence shows that it is inferior to the PECS II block (Table 1). While any medical procedure has its risks, these plane blocks are relatively safe due to the absence of vital structures in the immediate vicinity. It is important not to exceed the recommended dosage of anesthetic to avoid any anesthetic-related toxicity. We recommend using ropivacaine as the choice of anesthetic. All these blocks can be administered a single dose or as a continuous infusion. For continuous infusions, the authors recommend not exceeding 6–8 ml/hour of 0.2% ropivacaine with 2 ml boluses every 20 minutes, if needed. Furthermore, while previous studies have demonstrated the benefits of liposomal bupivacaine, the current review shows no significant differences in opioid consumption when compared with conventional local anesthetics. Therefore, we recommend future studies to compare the efficacy of liposomal bupivacaine and ropivacaine in the aforementioned plane blocks.
Table 1.
Summary of Recommendations for Plastic Surgeons
| Block | Administration | Indication | Evidence† |
|---|---|---|---|
| Transversus abdominis plane blocks | Local anesthetic between the internal oblique and transversus abdominis muscle | Abdominoplasty | Strong |
| Abdominal-based flap reconstruction (ie, TRAM flap) | Strong | ||
| Abdominal wall reconstruction | Limited | ||
| Pectoralis blocks | Local anesthetic between the pectoral major and minor muscles | Breast surgery* | Strong |
| Modified pectoralis blocks | Local anesthetic between the pectoralis major and minor muscles and between the pectoralis minor and serratus anterior muscles | Breast surgery* | Strong |
| Serratus anterior plane blocks | Local anesthetic between superficial and deep to the serratus anterior muscle | Breast surgery* | Strong |
| Erector spinae plane blocks† | Local anesthetic between rhomboid major and erector spinae muscles | Breast surgeries* | Strong |
*Breast surgeries include mastectomies, breast reconstructions, and reduction mammoplasties; however, majority of the evidence is with regard to mastectomies.
†Evidence strength is based on the number of RCTS and non-level 1 studies—strong: the majority of the RCTs and level-1 evidence supports its use; limited: few level-1 evidence and/or majority of non-level 1 evidence support its use.
It is important for plastic surgeons to familiarize themselves with evidence-based regional blocks and the important ultrasound landmarks associated with them. This will help them gain the necessary knowledge to administer these blocks themselves (intraoperatively) and ultimately help provide the best post-operative care possible for their patients. Although it is not expected for plastic surgeons to administer ultrasound guided techniques themselves, we believe it is important for them to recognize their efficacy, ease of administration, and safety profile so that they can advocate for their use in their practice/institution. In a quickly evolving field such as plastic surgery, there is a constant drive to provide our patients with the best available care. All the previous blocks are deemed very safe with minimal risk of complications; therefore, we recommend plastic surgeons to perform the block they are most comfortable with, as the evidence shows marginal differences between them in terms of efficacy. Although this article provides practical evidence-based recommendations for a wide variety of regional blocks that could be used by plastic surgeons, it is not an exhaustive list. There are minor differences in technique administration for different surgeries (ex. abdominoplasty versus DEIP flap breast reconstruction), which were not described in this review. Moreover, future studies should compare surgical site infiltration techniques to regional plane block techniques to provide plastic surgeons with evidence regarding their comparative efficacy. Finally, as the domain of pain management continues to evolve, novel blocks such as quadratus lumborum, which demonstrated preliminary evidence of efficacy in abdominoplasties, should be further studied before recommending them to plastic surgeons. Moreover, future studies should compare the efficacy of surgical site infiltration.
To maintain patient safety, communication between surgeons and anesthesiologists is essential. There should be discussion regarding the type of regional block that will performed as well as the maximum local anesthetic dose specific for the patient that would prevent local anesthetic systemic toxicity. In addition, identification and management of potential local anesthetic technique must also be planned.85 Finally, to attain the maximum analgesic benefits, it is critical that regional analgesia is combined with other non-opioid analgesics (eg, acetaminophen and non-steroidal anti-inflammatory drugs or cyclo-oxygenase (COX)-2 specific inhibitors), unless there are contraindication. These drugs should be administered as scheduled (ie, round the clock). It is necessary to counsel patients regarding the need for non-opioid analgesics to avoid severe pain after block resolution (rebound pain).
Footnotes
Published online 17 December 2020.
Disclosure: Dr. Janis receives royalties from Thieme and Springer Publishing. Dr. Joshi has received honoraria from Baxter Pharmaceuticals and Pacira, for this study.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Demsey D, Carr NJ, Clarke H, et al. Managing opioid addiction risk in plastic surgery during the perioperative period. Plast Reconstr Surg. 2017;140:613e–619e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alexander JC, Patel B, Joshi GP. Perioperative use of opioids: current controversies and concerns. Best Pract Res Clin Anaesthesiol. 2019;33:341–351. [DOI] [PubMed] [Google Scholar]
- 3.Joshi GP, Kehlet H. Postoperative pain management in the era of ERAS: an overview. Best Pract Res Clin Anaesthesiol. 2019;33:259–267. [DOI] [PubMed] [Google Scholar]
- 4.Jogerst K, Pockaj B. ASO author reflections: enhanced recovery after surgery (ERAS) principles extend beyond abdominal surgery. Ann Surg Oncol. 2020;27:3446–3447. [DOI] [PubMed] [Google Scholar]
- 5.Joshi GP, Kehlet H. Enhanced recovery pathways: looking into the future. Anesth Analg. 2019;128:5–7. [DOI] [PubMed] [Google Scholar]
- 6.Machi A, Joshi GP. Interfascial plane blocks. Best Pract Res Clin Anaesthesiol. 2019;33:303–315. [DOI] [PubMed] [Google Scholar]
- 7.Joshi GP, Kehlet H, Rawal N. Surgeon-administered regional analgesia to replace anaesthetist-administered regional analgesia: need for communication and collaboration. Br J Anaesth. 2019;123:707–709. [DOI] [PubMed] [Google Scholar]
- 8.ElHawary H, Abdelhamid K, Meng F, et al. Erector spinae plane block decreases pain and opioid consumption in breast surgery: systematic review. Plast Reconstr Surg Glob Open. 2019;7:e2525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Homsy C, Lindsey JT. Regional anesthetic blocks in plastic surgery using portable ultrasound: a simplified approach. Ann Plast Surg. 2019;82(6S Suppl 5):S374–S379. [DOI] [PubMed] [Google Scholar]
- 10.Joshi GP, Machi A. Surgical site infiltration: a neuroanatomical approach. Best Pract Res Clin Anaesthesiol. 2019;33:317–324. [DOI] [PubMed] [Google Scholar]
- 11.Rafi AN. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia. 2001;56:1024–1026. [DOI] [PubMed] [Google Scholar]
- 12.Araco A, Pooney J, Araco F, et al. Transversus abdominis plane block reduces the analgesic requirements after abdominoplasty with flank liposuction. Ann Plast Surg. 2010;65:385–388. [DOI] [PubMed] [Google Scholar]
- 13.Wheble GA, Tan EK, Turner M, et al. Surgeon-administered, intra-operative transversus abdominis plane block in autologous breast reconstruction: a UK hospital experience. J Plast Reconstr Aesthet Surg. 2013;66:1665–1670. [DOI] [PubMed] [Google Scholar]
- 14.Abdou SA, Daar DA, Wilson SC, et al. Transversus abdominis plane blocks in microsurgical breast reconstruction: a systematic review and meta-analysis. J Reconstr Microsurg. 2020;36:353–361. [DOI] [PubMed] [Google Scholar]
- 15.Vonu PM, Campbell P, Prince N, et al. Analgesic efficacy of nerve blocks after abdominoplasty: a systematic review. Aesthet Surg J. 2020;40:1208–1215. [DOI] [PubMed] [Google Scholar]
- 16.Abo-Zeid MA, Al-Refaey AK, Zeina AM. Surgically-assisted abdominal wall blocks for analgesia after abdominoplasty: a prospective randomized trial. Saudi J Anaesth. 2018;12:593–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Salama ER. Post-operative bilateral continuous ultrasound-guided transversus abdominis plane block versus continuous local anaesthetic wound infusion in patients undergoing abdominoplasty. Indian J Anaesth. 2018;62:449–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sforza M, Andjelkov K, Zaccheddu R, et al. Transversus abdominis plane block anesthesia in abdominoplasties. Plast Reconstr Surg. 2011;128:529–535. [DOI] [PubMed] [Google Scholar]
- 19.Zhong T, Ojha M, Bagher S, et al. Transversus abdominis plane block reduces morphine consumption in the early postoperative period following microsurgical abdominal tissue breast reconstruction: a double-blind, placebo-controlled, randomized trial. Plast Reconstr Surg. 2014;134:870–878. [DOI] [PubMed] [Google Scholar]
- 20.Ha AY, Keane G, Parikh R, et al. The analgesic effects of liposomal bupivacaine versus bupivacaine hydrochloride administered as a transversus abdominis plane block after abdominally based autologous microvascular breast reconstruction: a prospective, single-blind, randomized, controlled trial. Plast Reconstr Surg. 2019;144:35–44. [DOI] [PubMed] [Google Scholar]
- 21.Fayezizadeh M, Majumder A, Neupane R, et al. Efficacy of transversus abdominis plane block with liposomal bupivacaine during open abdominal wall reconstruction. Am J Surg. 2016;212:399–405. [DOI] [PubMed] [Google Scholar]
- 22.Momeni A, Ramesh NK, Wan D, et al. Postoperative analgesia after microsurgical breast reconstruction using liposomal bupivacaine (Exparel). Breast J. 2019;25:903–907. [DOI] [PubMed] [Google Scholar]
- 23.Oppenheimer AJ, Fiala TGS, Oppenheimer DC. Direct transversus abdominis plane blocks with exparel during abdominoplasty. Ann Plast Surg. 2016;77:499–500. [DOI] [PubMed] [Google Scholar]
- 24.Salibian AA, Frey JD, Thanik VD, et al. Transversus abdominis plane blocks in microsurgical breast reconstruction: analysis of pain, narcotic consumption, length of stay, and cost. Plast Reconstr Surg. 2018;142:252e–263e. [DOI] [PubMed] [Google Scholar]
- 25.Jablonka EM, Lamelas AM, Kim JN, et al. Transversus abdominis plane blocks with single-dose liposomal bupivacaine in conjunction with a nonnarcotic pain regimen help reduce length of stay following abdominally based microsurgical breast reconstruction. Plast Reconstr Surg. 2017;140:240–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Salaria ON, Kannan M, Kerner B, et al. A rare complication of a TAP block performed after caesarean delivery. Case Rep Anesthesiol. 2017;2017:1072576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blanco R. The ‘pecs block’: a novel technique for providing analgesia after breast surgery. Anaesthesia. 2011;66:847–848. [DOI] [PubMed] [Google Scholar]
- 28.Singh PM, Borle A, Kaur M, et al. Opioid-sparing effects of the thoracic interfascial plane blocks: a meta-analysis of randomized controlled trials. Saudi J Anaesth. 2018;12:103–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sun Q, Liu S, Wu H, et al. Clinical analgesic efficacy of pectoral nerve block in patients undergoing breast cancer surgery: a systematic review and meta-analysis. Medicine (Baltimore). 2020;99:e19614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bakr MA, Mohamed SA, Mohamad MF, et al. Effect of dexmedetomidine added to modified pectoral block on postoperative pain and stress response in patient undergoing modified radical mastectomy. Pain Physician. 2018;21:E87–E96. [PubMed] [Google Scholar]
- 31.Cros J, Sengès P, Kaprelian S, et al. Pectoral I block does not improve postoperative analgesia after breast cancer surgery: a randomized, double-blind, dual-centered controlled trial. Reg Anesth Pain Med. 2018;43:596–604. [DOI] [PubMed] [Google Scholar]
- 32.Kamiya Y, Hasegawa M, Yoshida T, et al. Impact of pectoral nerve block on postoperative pain and quality of recovery in patients undergoing breast cancer surgery: a randomised controlled trial. Eur J Anaesthesiol. 2018;35:215–223. [DOI] [PubMed] [Google Scholar]
- 33.Kumar S, Goel D, Sharma SK, et al. A randomised controlled study of the post-operative analgesic efficacy of ultrasound-guided pectoral nerve block in the first 24 h after modified radical mastectomy. Indian J Anaesth. 2018;62:436–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tripathy S, Mandal I, Rao PB, et al. Opioid-free anesthesia for breast cancer surgery: a comparison of ultrasound guided paravertebral and pectoral nerve blocks. A randomized controlled trial. J Anaesthesiol Clin Pharmacol. 2019;35:475–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang W, Song W, Yang C, et al. Ultrasound-guided pectoral nerve block I and serratus-intercostal plane block alleviate postoperative pain in patients undergoing modified radical mastectomy. Pain Physician. 2019;22:E315–E323. [PubMed] [Google Scholar]
- 36.Ueshima H, Otake H. Ultrasound-guided pectoral nerves (PECS) block: complications observed in 498 consecutive cases. J Clin Anesth. 2017;42:46. [DOI] [PubMed] [Google Scholar]
- 37.Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of Pecs II (modified Pecs I): a novel approach to breast surgery. Rev Esp Anestesiol Reanim. 2012;59:470–475. [DOI] [PubMed] [Google Scholar]
- 38.Hussain N, Brull R, McCartney CJL, et al. Pectoralis-II myofascial block and analgesia in breast cancer surgery: a systematic review and meta-analysis. Anesthesiology. 2019;131:630–648. [DOI] [PubMed] [Google Scholar]
- 39.Versyck B, van Geffen GJ, Chin KJ. Analgesic efficacy of the Pecs II block: a systematic review and meta-analysis. Anaesthesia. 2019;74:663–673. [DOI] [PubMed] [Google Scholar]
- 40.Al Ja’bari A, Robertson M, El-Boghdadly K, et al. A randomised controlled trial of the pectoral nerves-2 (PECS-2) block for radical mastectomy. Anaesthesia. 2019;74:1277–1281. [DOI] [PubMed] [Google Scholar]
- 41.Altiparmak B, Korkmaz Toker M, Uysal Aİ, et al. Comparison of the effects of modified pectoral nerve block and erector spinae plane block on postoperative opioid consumption and pain scores of patients after radical mastectomy surgery: A prospective, randomized, controlled trial. J Clin Anesth. 2019;54:61–65. [DOI] [PubMed] [Google Scholar]
- 42.Choi JJ, Jo YY, Kim SH, et al. Remifentanil-sparing effect of pectoral nerve block type II in breast surgery under surgical pleth index-guided analgesia during total intravenous anesthesia. J Clin Med. 2019;8:1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cui X, Zhu X, Chen H, et al. Effect of pectoral nerve block type II under general anesthesia on the immune function of patients with breast cancer. Am J Surg. 2020;220:938–944. [DOI] [PubMed] [Google Scholar]
- 44.Fujii T, Shibata Y, Akane A, et al. A randomised controlled trial of pectoral nerve-2 (PECS 2) block vs. serratus plane block for chronic pain after mastectomy. Anaesthesia. 2019;74:1558–1562. [DOI] [PubMed] [Google Scholar]
- 45.Gad M, Abdelwahab K, Abdallah A, et al. Ultrasound-guided erector spinae plane block compared to modified pectoral plane block for modified radical mastectomy operations. Anesth Essays Res. 2019;13:334–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim DH, Kim S, Kim CS, et al. Efficacy of pectoral nerve block type II for breast-conserving surgery and sentinel lymph node biopsy: a prospective randomized controlled study. Pain Res Manag. 2018;2018:4315931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kulhari S, Bharti N, Bala I, et al. Efficacy of pectoral nerve block versus thoracic paravertebral block for postoperative analgesia after radical mastectomy: a randomized controlled trial. Br J Anaesth. 2016;117:382–386. [DOI] [PubMed] [Google Scholar]
- 48.Othman AH, El-Rahman AM, El Sherif F. Efficacy and safety of ketamine added to local anesthetic in modified pectoral block for management of postoperative pain in patients undergoing modified radical mastectomy. Pain Physician. 2016;19:485–494. [PubMed] [Google Scholar]
- 49.Schuitemaker RJ, Sala-Blanch X, Sánchez Cohen AP, et al. Analgesic efficacy of modified pectoral block plus serratus plane block in breast augmentation surgery: a randomised, controlled, triple-blind clinical trial. Rev Esp Anestesiol Reanim. 2019;66:62–71. [DOI] [PubMed] [Google Scholar]
- 50.Senapathi TGA, Widnyana IMG, Aribawa IGNM, et al. Combined ultrasound-guided Pecs II block and general anesthesia are effective for reducing pain from modified radical mastectomy. J Pain Res. 2019;12:1353–1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Siddeshwara A, Singariya G, Kamal M, et al. Comparison of efficacy of ultrasound-guided pectoral nerve block versus thoracic paravertebral block using levobupivacaine and dexamethasone for postoperative analgesia after modified radical mastectomy: a randomized controlled trial. Saudi J Anaesth. 2019;13:325–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sinha C, Kumar A, Kumar A, et al. Pectoral nerve versus erector spinae block for breast surgeries: a randomised controlled trial. Indian J Anaesth. 2019;63:617–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Thomas M, Philip FA, Mathew AP, et al. Intraoperative pectoral nerve block (Pec) for breast cancer surgery: a randomized controlled trial. J Anaesthesiol Clin Pharmacol. 2018;34:318–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Versyck B, van Geffen GJ, Van Houwe P. Prospective double blind randomized placebo-controlled clinical trial of the pectoral nerves (Pecs) block type II. J Clin Anesth. 2017;40:46–50. [DOI] [PubMed] [Google Scholar]
- 55.Wang K, Zhang X, Zhang T, et al. The efficacy of ultrasound-guided type II pectoral nerve blocks in perioperative pain management for immediate reconstruction after modified radical mastectomy: a prospective, randomized study. Clin J Pain. 2018;34:231–236. [DOI] [PubMed] [Google Scholar]
- 56.Bell A, Ali O, Robinson A, et al. The role of pectoral nerve blocks in a day-case mastectomy service: a prospective cohort study. Ann Med Surg (Lond). 2019;48:65–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.De Cassai A, Bonanno C, Sandei L, et al. PECS II block is associated with lower incidence of chronic pain after breast surgery. Korean J Pain. 2019;32:286–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kubodera K, Fujii T, Akane A, et al. <Editors’ Choice> Efficacy of pectoral nerve block type-2 (Pecs II block) versus serratus plane block for postoperative analgesia in breast cancer surgery: a retrospective study. Nagoya J Med Sci. 2020;82:93–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hong B, Yoon SH, Youn AM, et al. Thoracic interfascial nerve block for breast surgery in a pregnant woman: a case report. Korean J Anesthesiol. 2017;70:209–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moon EJ, Kim SB, Chung JY, et al. Pectoral nerve block (pecs block) with sedation for breast conserving surgery without general anesthesia. Ann Surg Treat Res. 2017;93:166–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Blanco R, Parras T, McDonnell JG, et al. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013;68:1107–1113. [DOI] [PubMed] [Google Scholar]
- 62.Matsumoto M, Flores EM, Kimachi PP, et al. Benefits in radical mastectomy protocol: a randomized trial evaluating the use of regional anesthesia. Sci Rep. 2018;8:7815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rahimzadeh P, Imani F, Faiz SHR, et al. Impact of the ultrasound-guided serratus anterior plane block on post-mastectomy pain: a randomised clinical study. Turk J Anaesthesiol Reanim. 2018;46:388–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang HJ, Liu Y, Ge WW, et al. [Comparison of ultrasound-guided serratus anterior plane block and erector spinae plane blockperioperatively in radical mastectomy]. Zhonghua Yi Xue Za Zhi. 2019;99:1809–1813. [DOI] [PubMed] [Google Scholar]
- 65.Huang L, Zheng L, Wu B, et al. Effects of ropivacaine concentration on analgesia after ultrasound-guided serratus anterior plane block: a randomized double-blind trial. J Pain Res. 2020;13:57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kunigo T, Murouchi T, Yamamoto S, et al. Injection volume and anesthetic effect in serratus plane block. Reg Anesth Pain Med. 2017;42:737–740. [DOI] [PubMed] [Google Scholar]
- 67.Abdallah FW, MacLean D, Madjdpour C, et al. Pectoralis and serratus fascial plane blocks each provide early analgesic benefits following ambulatory breast cancer surgery: a retrospective propensity-matched cohort study. Anesth Analg. 2017;125:294–302. [DOI] [PubMed] [Google Scholar]
- 68.Hards M, Harada A, Neville I, et al. The effect of serratus plane block performed under direct vision on postoperative pain in breast surgery. J Clin Anesth. 2016;34:427–431. [DOI] [PubMed] [Google Scholar]
- 69.Khemka R, Chakraborty A. Ultrasound-guided modified serratus anterior plane block for perioperative analgesia in breast oncoplastic surgery: a case series. Indian J Anaesth. 2019;63:231–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Khemka R, Chakraborty A, Ahmed R, et al. Ultrasound-guided serratus anterior plane block in breast reconstruction surgery. A A xz Rep. 2016;6:280–282. [DOI] [PubMed] [Google Scholar]
- 71.Forero M, Adhikary SD, Lopez H, et al. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 201641:621–627. [DOI] [PubMed] [Google Scholar]
- 72.Aksu C, Kuş A, Yörükoğlu HU, et al. Analgesic effect of the bi-level injection erector spinae plane block after breast surgery: a randomized controlled trial. Agri. 201931:132–137. [DOI] [PubMed] [Google Scholar]
- 73.Gürkan Y, Aksu C, Kuş A, et al. Erector spinae plane block and thoracic paravertebral block for breast surgery compared to IV-morphine: a randomized controlled trial. J Clin Anesth. 2020;59:84–88. [DOI] [PubMed] [Google Scholar]
- 74.Gürkan Y, Aksu C, Kuş A, et al. Ultrasound guided erector spinae plane block reduces postoperative opioid consumption following breast surgery: a randomized controlled study. J Clin Anesth. 2018;50:65–68. [DOI] [PubMed] [Google Scholar]
- 75.He W, Wu Z, Zu L, et al. Application of erector spinae plane block guided by ultrasound for postoperative analgesia in breast cancer surgery: a randomized controlled trial. Cancer Commun (Lond). 2020;40:122–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Singh S, Kumar G, Akhileshwar Ultrasound-guided erector spinae plane block for postoperative analgesia in modified radical mastectomy: A randomised control study. Indian J Anaesth. 2019;63:200–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Oksuz G, Bilgen F, Arslan M, et al. Ultrasound-guided bilateral erector spinae block versus tumescent anesthesia for postoperative analgesia in patients undergoing reduction mammoplasty: a randomized controlled study. Aesthetic Plast Surg. 2019;43:291–296. [DOI] [PubMed] [Google Scholar]
- 78.El Ghamry MR, Amer AF. Role of erector spinae plane block versus paravertebral block in pain control after modified radical mastectomy. A prospective randomised trial. Indian J Anaesth. 2019;63:1008–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Moustafa MA, Alabd AS, Ahmed AMM, et al. Erector spinae versus paravertebral plane blocks in modified radical mastectomy: randomised comparative study of the technique success rate among novice anaesthesiologists. Indian J Anaesth. 2020;64:49–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Swisher MW, Wallace AM, Sztain JF, et al. Erector spinae plane versus paravertebral nerve blocks for postoperative analgesia after breast surgery: a randomized clinical trial. Reg Anesth Pain Med. 2020;45:260–266. [DOI] [PubMed] [Google Scholar]
- 81.Hong B, Bang S, Chung W, et al. Multimodal analgesia with multiple intermittent doses of erector spinae plane block through a catheter after total mastectomy: a retrospective observational study. Korean J Pain. 2019;32:206–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Malawat A, Verma K, Jethava D, et al. Erector spinae plane block for complete surgical anaesthesia and postoperative analgesia for breast surgeries: a prospective feasibility study of 30 cases. Indian J Anaesth. 2020;64:118–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Santonastaso DP, De Chiara A, Pizzilli G, et al. Ultrasound-guided erector spinae plane block for breast reconstruction surgery with latissimus dorsi muscle flap. Minerva Anestesiol. 2019;85:443–444. [DOI] [PubMed] [Google Scholar]
- 84.Ohgoshi Y, Ikeda T, Kurahashi K. Continuous erector spinae plane block provides effective perioperative analgesia for breast reconstruction using tissue expanders: a report of two cases. J Clin Anesth. 2018;44:1–2. [DOI] [PubMed] [Google Scholar]
- 85.Neal JM, Bernards CM, Butterworth JF, IV, et al. ASRA practice advisory on local anesthetic systemic toxicity. Reg Anesth Pain Med. 2010;35:152–161. [DOI] [PubMed] [Google Scholar]


