Abstract
Background:
Managing lower extremity fractures complicated by large soft-tissue defects is challenging for surgeons in low- and middle-income countries, and long-term quality of life (QOL) for these patients is unclear.
Methods:
We examined QOL, surgical complications, and longitudinal outcomes in 10 patients with Gustilo-Anderson Classification Type IIIB open tibia fractures seen at an orthopedic institute in Tanzania, from December 2015 to March 2017. Patients completed follow-up at 2-, 6-, 12-, 26-, and 52-week time points, and returned for qualitative interviews at 2.5 years. The primary outcome was QOL, as measured using EuroQoL-5D scores and qualitative semi-structured interview responses. The secondary outcome was rate of complication, as defined by reoperation for deep infection or nonunion.
Results:
Ten patients enrolled in the study and 7 completed 1-year follow-up. All fractures were caused by road traffic accidents and treated by external fixation. No patients received initial soft-tissue (flap) coverage of the wound. All patients developed an infected nonunion. No patients returned to work at 6 weeks, 3 months, or 6 months. EQ-5D index scores at 1 year were poor (0.71 ± 0.09). Interview themes included ongoing medical complications, loss of employment, reduced income, and difficulty with activities of daily living.
Conclusions:
Patients in low- and middle-income countries with IIIB open tibia fractures not treated with appropriate soft-tissue coverage experience poor QOL, high complication rates, and severe socioeconomic effects as a result of their injuries. These findings illustrate the need for resources and training to build capacity for extremity soft-tissue reconstruction in LMICs.
INTRODUCTION
Musculoskeletal injuries are a major global health problem and contribute to a growing burden of disability and suffering in low- and middle-income countries (LMICs).1 Rates of these injuries are 2–5 times more common in LMICs than in high-income countries, highlighting a serious global healthcare inequity.2,3 Among these injuries, lower extremity fractures are common and are often accompanied by significant soft-tissue injuries.4,5 One of the most severe types of lower extremity fractures is the Gustilo-Anderson Classification Type IIIB open tibial shaft fracture, which is characterized by massive soft-tissue defects, fracture instability, and wound contamination.6–8 The preferred method of treatment for these fractures is bone fixation with external and internal devices, as well as soft-tissue reconstruction, such as rotational flaps and skin grafts. However, the overwhelming majority of orthopedic surgeons in LMICs lack the specialized soft-tissue training required to manage these traumatic defects.5,9–11 Additionally, there remains a significant lack of local plastic surgeons in LMICs, with the necessary training to perform these complex procedures.1,3,12–17 This lack of training contributes to a massive unmet burden of disease in LMICs, with an estimated 66% of surgical disease disability-adjusted life years due to conditions normally treated by plastic surgeons.18,19 Consequently, patients often do not receive adequate soft-tissue coverage for their injuries, leading to short and long-term medical complications such as infection, amputation, chronic disability, or death.6,20,21
Patients who sustain type IIIB open tibia fractures also experience a significant impact on quality of life (QOL) that can lead to devastating socioeconomic consequences, such as financial hardship, job loss, and psychological trauma.21,22 However, reports on the challenge of soft-tissue reconstruction and complications after IIIB open tibia wound coverage do not reflect patient outcomes in an environment where flap coverage is not available, nor do they address long-term quality of life.22–26 This study aimed to examine and define the domains in which IIIB open tibia fractures without appropriate soft-tissue coverage affect QOL among patients in Tanzania.
METHODS
Adult patients (aged 18 years and over) with Gustilo-Anderson Type IIIB tibial shaft fractures unsuitable for primary closure were invited to enroll in a prospective cohort study at an orthopedic institute in Tanzania, from December 2015 to March 2017. The study was reviewed and approved by the University of California, San Francisco (UCSF), and the National Institute for Medical Research in Tanzania. Enrolled patients completed follow-up at 2, 6, 12, 26, and 52-week time points and returned for semi-structured interviews at 2.5 years.
The primary outcome was defined as QOL, as measured using EuroQoL-5D scores and qualitative semi-structured interview responses. The EQ-5D survey assesses QOL in 5 separate categories: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression.27 Five-digit health profiles are subsequently converted into a single summary index ranging from 0 (death) to 1 (full health). The EQ-5D survey also includes a visual analog scale (VAS) component that lets participants self-rate their health, with endpoints ranging from 0 (worst imaginable health state) to 100 (best imaginable health state). All surveys were administered in Swahili. Semi-structured interviews took place in-person at the Tanzanian host institution. Interview questions were developed in an open-ended fashion to determine the long-term impact of injury on the patients’ QOL and emphasized patients’ employment, mobility, emotional well-being, and social relationships as they related to the injury. Interviews were conducted in Swahili, with the assistance of staff translators at the host institution. Responses were transcribed and inductively coded by authors JTH and PDA independently using ATLAS-ti software (ATLAS.ti Scientific Software Development GmbH).
The secondary study outcome was rate of complication, as defined by reoperation for deep infection or nonunion. Infections were defined with the use of consensus guidelines on fracture-related infections (FRIs), and were further classified as definite or suggestive infection.28 The presence of a fistula, sinus, or wound breakdown (with communication to the bone or implant) and/or purulent drainage from the wound were regarded as confirmatory signs of definite FRI. Local redness, swelling, increased local temperature, fever (≥38.38°C), or persistent, increasing, or new-onset wound drainage beyond the first few days postoperatively were regarded as confirmatory signs of suggestive FRI.28
RESULTS
Ten patients with IIIB open tibia fractures enrolled in the cohort study, 7 of whom completed 1-year follow-up and were included in our analysis. The average age was 36.1 ± 6.1 years. Four of the patients were women, and the average BMI for all patients was 25.4 ± 3.3. No patients reported additional comorbidities or a history of diabetes. One patient reported tobacco use (Table 1). Road traffic accidents were the primary cause of all fractures, most of which involved motorbike5 or pedestrian2 accidents. Six of the patients presented to the hospital in <6 hours, and 1 patient presented with a delay >24 hours. All 7 patients had Gustilo-Anderson Type IIIB tibial shaft fractures, and 5 patients had wounds ≥10 cm in length. Wounds were further characterized as follows: skin edges do not approximate5; loss of muscle with retained function4; opposable ends or segmental bone loss1; vascular injury with no ischemia2; surface contamination5 (Table 2).
Table 1.
Demographic Characteristics of 7 Patients with Type IIIB Open Tibia Fractures
| Characteristic | |
|---|---|
| Age (mean ± SD) | 36.1 ± 6.1 |
| Male gender | 3 |
| Mechanism of injury | |
| Road traffic injury | 7 |
| Road traffic injury type | |
| Motorbike | 5 |
| Pedestrian | 2 |
| Current smoker | 1 |
| Alcohol use | 4 |
| Body mass index (mean ± SD) | 25.4 ± 3.3 |
| Diabetes | 0 |
Table 2.
Injury Characteristics of 7 Patients with Type IIIB open Tibia Fractures
| Characteristic | |
|---|---|
| Time from injury to hospital | |
| <6-h delay | 5 |
| 6- to 24-h delay | 1 |
| >24-h delay | 1 |
| Time from hospital to surgery (h; mean ± SD) | 10.9 ± 4.6 |
| Delay from hospital to surgery | |
| <6-h delay | 2 |
| 6 to 24-h delay | 5 |
| OTA classification | |
| Type A | 1 |
| Type B | 2 |
| Type C | 3 |
| OTA: open fracture classification | |
| Skin: edges do not approximate | 5 |
| Muscle: loss of muscle with retained function | 4 |
| Bone loss: opposable ends or segmental | 1 |
| Vascular: injury, no ischemia | 2 |
| Contamination: surface contamination | 5 |
| Wound length (cm) | |
| 5–10 cm | 2 |
| ≥10 cm | 5 |
| Time from injury to antibiotics | |
| <6-h delay | 1 |
| 6- to 24-h delay | 5 |
| >24-h delay | 1 |
| Definitive fixation | |
| External fixation | 7 |
The traumatic wounds in all cases were treated with gauze dressing changes, and all patients received a definitive operation with external fixation. No patients received early soft-tissue coverage procedures. Negative pressure wound therapy was not used in any case. One patient underwent a rotational flap 3 weeks post-injury at an outside hospital. Two patients were treated with skin grafting for non-healing wounds. All patients received treatment with antibiotics (Table 2).
Patients reported poor EQ-5D index scores at 1-year (0.71 ± 0.09). From pre-injury scores near full health (0.98 ± 0.09), patients’ EQ-5D scores dropped to a low at 2–6 weeks and never returned to pre-injury levels at 52-weeks. EQ-5D VAS scores followed a similar pattern and did not return to pre-health levels at 1 year (71.9 ± 14.5) (Fig. 1) (Table 3). The EQ-5D scores at 52-weeks were below population norms for both the United States and Zimbabwe (the only African-country-specific norm available).27 When compared with disease-specific norms in the US population, EQ-5D scores were comparable to myocardial infarction (0.73) and osteoarthritis (0.70), and were less than those of breast cancer (0.81), prostate cancer (0.77), and chronic obstructive pulmonary disease (COPD) (0.80).29 EQ-5D scores were also less than those of 52-week post-injury scores for femoral shaft fractures requiring re-operation in Tanzania (0.85)30 (Fig. 2).
Fig. 1.
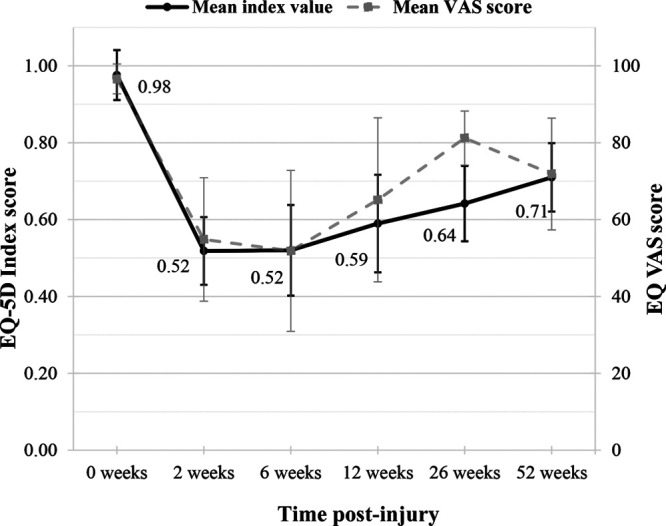
EQ-5D index score and VAS score over 1 year. Mean EuroQoL-5D index scores (0–1) and mean VAS scores (0–100) for 7 patients with Gustilo-Anderson Type IIIB fractures without early soft-tissue coverage procedures are shown over the course of 1 year at 0-, 2-, 6-, 12-, 26-, and 52-week timepoints. Error bars represent SD for sample population.
Table 3.
Study Outcomes
| Primary outcomes | |
| EQ-5D index at 52 weeks | 0.71 ± 0.09 |
| EQ-5D VAS score at 52 weeks | 71.9 ± 14.5 |
| Secondary event (reoperation) | 6 |
| Nonunion or delayed union | 7 |
| Malunion or malalignment | 0 |
| Fracture-related infection (definite) | 5 |
| Fracture-related infection (suggestive) | 2 |
Fig. 2.
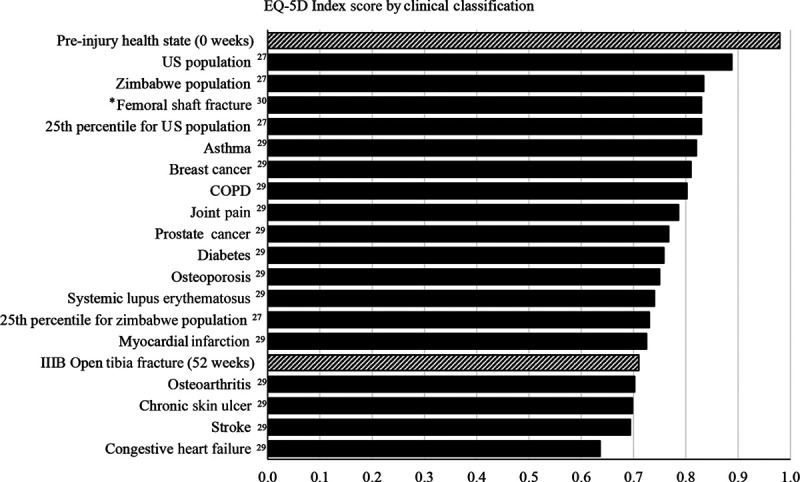
EQ-5D index scores by clinical classification. Mean EQ-5D index scores are shown according to diagnosis. Superscript numbers indicate the reference sources. The striped bars represent mean EQ-5D scores for study patients at both pre-injury health state (0 weeks) and post-injury (52 weeks) time points. Population norms are represented for the US population and Zimbabwe (the only African-country-specific norm available) in black bars, among listed clinical diagnoses. *Femoral shaft fracture represents the mean EQ-5D index score at 1 year for patients who required reoperation for femoral shaft fractures in Tanzania.
All 7 patients experienced a complication, with every patient experiencing both a nonunion and FRI (Table 3). Of the FRIs, 5 met definite criteria and 2 met suggestive criteria only. None of the patients returned to work at 6 weeks, 3 months, or 6 months.
Ongoing Medical Complications Related to Injury
The 5 patients who participated in semi-structured QOL interviews at 2.5 years post-injury reported ongoing medical complications related to their injury (Table 4). Four still reported chronic open wounds, 1 of whom reported reoperations related to their injury. Although some patients self-managed the care of these wounds with little concern, others expressed fear of recurrent infections, as reflected by 1 patient:
Table 4.
Themes Reported during 5 Patient QOL Interviews
| Coded Theme | N Reported | Relevant Quote Examples |
|---|---|---|
| Loss of employment | 5 | “Before the injury, I was a farmer and a livestock keeper. I had goats and cows, and I had a farm of vegetables. And I also had a motorcycle for making a business of it. But after the injury, everything has perished out. I have lost everything.” |
| Reduced income | 5 | “It has affected my income very much. Because at that time I was working and I was getting money, and now there is no job and no work. I’m at home. I have no income, unless I get support from my family members.” |
| Transportation difficulty | 4 | “There is a fear of crowds with the bus station and having to fight to get on the bus. With the injury, sometimes I’m scared to enter the bus.” |
| Cannot support family | 4 | “Since (the injury) my children have not had any assistance. Because, since the date of injury up to date, I don’t work anymore for income.” |
| Difficulties with activities of daily living | 4 | “I get assistance from my husband and my daughter with washing clothes and other activities which require assistance.” |
| “I’ve had some problems, especially during the time I’m going to the washroom. I have to go to the washroom with the type of toilet that I can sit on. But not the type where I squat. And most of my activities I have to do while I’m sitting. My daughters and my sons - they helped me to wash. With all the stuff that I need assistance with at home, they help me.” | ||
| Loss of social network and support | 4 | “Some of my friends [initially] gave to me because it seemed like I needed support from them. But now there’s a gap between me and my friends because it seems like I always need support from them.” |
| “My family has isolated me. They say they cannot help me. I have to find one who caused this accident. So that he can help me. That’s why they don’t help me. Instead they have pushed me away.” | ||
| Ongoing pain | 3 | “I feel so painful when I walk from one place to another. I feel embarrassment when I’m using these crutches. And sometimes my legs, I feel pain for sure.” |
| “For sure it has let me down. This injury has caused me a lot of problems. Sometimes I fail to pay the house rent. I don’t have money to eat. So I’m still having trouble. I don’t work sometimes. I cannot work with my injury. I move from one place to another with a lot of pain. This is affecting me a lot.” | ||
| Poor emotional and mental well-being | 3 | “Emotionally it is giving me a lot of pain because I have five kids. And all of them depend on me. I have to help them and I don’t have money. If I get an amount of money, I have to use that money just to come to the hospital. So, I feel like I don’t have anywhere to go now. This injury has affected me a lot emotionally.” |
| Loss of property* | 2 | “I have been affected a lot by this injury. I have lost all of my properties. My family now lives like beggars because I was the key of the family. I am supposed to do work to assist the family. But since the injury, I have not done anything to make money. So it has affected me a lot.” |
*Loss of home, livestock, and/or owned transport.
Yeah I have a problem because of my injury. With this open wound, I can’t do anything. I’m scared to do anything.—Man, age 47
Economic Impact
All interviewed patients reported immediate or long-term employment loss in the aftermath of their injury. Five patients reported a long-term decrease in income, 4 reported inability to support their family, and 2 reported significant loss of property. Loss of employment was directly attributed to ongoing physical disability in all cases. Many patients expressed distress over continued loss of income and the need to rely on family members for financial support, as described by this patient:
It has affected my income very much. Because at that time [of injury] I was working and I was getting money, and now there is no job and no work. I’m at home. I have no income, unless I get support from my family members.—Woman, age 44
Most (4/5) patients were self-employed at the time of injury, and common sources of income included farming, selling produce at the market, or informal jobs. All patients reported a stable income pre-injury regardless of type of employment. In addition to physical disability preventing employment, 2 patients were forced to sell property, including livestock, transportation, or their small business to supplement diminished income. This loss of property, in turn, prevented a return to former employment and a long-term reduction in earning potential. Patients who self-identified as the head of their household also expressed a great deal of emotional distress over not being able to financially provide for their families:
Before the injury, I was a farmer and a livestock keeper. I had goats and cows, and I had a farm of vegetables. And I also had a motorcycle for making a business of it. But after the injury, everything has perished out. I have lost everything... I have been affected a lot by this injury. I have lost all of my properties. My family now lives like beggars because I was the key of the family. I am supposed to do work to assist the family. But since the injury, I have not done anything to make money. So it has affected me a lot.—Man, age 47
Difficulties with Transportation and Activities of Daily Living
Many interviewees (4–5) reported ongoing difficulties with transportation and activities of daily living. Common responses included a fear of using crowded public transportation because of physical disability, not being able to use motorbikes, or difficulty leaving their home without using expensive, private transport. Within the home setting, interviewees reported that they required long-term assistance from family members with daily activities, such as squatting for toilet use, bathing, transferring, and carrying heavy loads:
It [the injury] is affecting me because when I want to squat it is difficult. And I can’t walk as fast as I previously could. And these activities were easier to do before the injury. Like carrying heavy loads, I cannot do now… I get assistance from my husband and my daughter with washing clothes and other activities which require assistance.—Woman, age 41
Loss of Social Support
Although many patients reported receiving financial and emotional support from family members and their community, 3 talked about losing their social network as a result of their injuries. It was common for interviewees to express that their ongoing need for support, both financial and emotional, led to a loss of friendship. Additionally, limited mobility played a significant role in some patients not being able to attend social outings or community activities:
There are some others and friendships that have gone away. This is just because of the Tanzanian mentality. If you have a problem, people leave you away. And I know that they are not true friends. I just put it away instead of letting it get to me… When someone gets a problem, and it’s such a problem, it could be a great one, people will leave you.—Man, age 32
Ongoing Pain
Three patients described ongoing pain related to their injury. One patient described managing the pain with chronic medication use, and a great deal of embarrassment in needing to use crutches to avoid exacerbating the pain. For these patients, ongoing pain played a large role in limiting mobility, which affected many other aspects of their lives. One patient expressed frustration with her pain, and how the pain prevented her return to work and the financial consequences that followed:
This injury has caused me a lot of problems. Sometimes I fail to pay the house rent. I don’t have money to eat. So I’m still having trouble… I cannot work with my injury. I move from one place to another with a lot of pain. This is affecting me a lot.—Woman, age 43
Poor Emotional and Mental Well-being
Three patients expressed significant deterioration of their emotional and mental well-being as a result of the injury. They expressed feelings of hopelessness because of their physical disability and chronic need for medical care. All these patients further identified as the head of their household and related their feelings to an inability to care for their families. As one woman put it:
Emotionally, I feel so bad because I used to fight for my life and for my family. And it was easy because I was strong and I was able to do everything. But now with the type of injury I have, it is not easy. It is not easy to accept. I know that this is God’s will. There is no way. I have to accept, even though it is emotionally disturbing.—Woman, age 44
DISCUSSION
Although treatment delays in neglected open tibia fractures in LMICs can be successfully managed,31 there is general agreement that early closure of open fracture wounds is preferred, and that increased time to soft-tissue reconstruction on IIIB open tibia injuries is a significant predictor of adverse outcomes.24 In our study, none of the patients with an open tibia fracture underwent early coverage with rotational flaps or wound closure, likely contributing to their poor outcomes. One study from the United States reported that the impact of tibial shaft fracture nonunions on physical health was comparable to that of end-stage hip arthrosis, and worse than that of congestive heart failure, highlighting the devastating effects of this outcome.32
In our study, QOL, assessed with the EQ-5D survey, showed some improvement over the course of follow-up, but scores remained low at 1 year compared with those at a pre-injury state near full health. A recent study examining 162 open tibia fractures (Grades I–IIIC) in an Indian population found that EQ-5D scores similarly dropped dramatically at 3 months from a near full health state pre-injury. However, EQ-5D scores in this study’s population at 1 year post-injury were near fully recovered in all groups except those with open infected wounds.33 While this study did not examine EQ-5D scores in IIIB fractures specifically, the high rates of infection in our study may similarly play a role in poor EQ-5D scores at 1 year. Regardless, the 1-year index scores in our study (0.71 ± 0.09) are remarkably poor compared with chronic health conditions in the US population, such as prostate cancer, breast cancer, and COPD.29 While disease-specific norms do not exist for sub-Saharan African populations, the EQ-5D scores were also less than those of both the average and 25th percentile in Zimbabwe,27 as well as less than EQ-5D scores at 1 year following femoral shaft fractures requiring reoperation in Tanzania.30
While the decrement in EQ-5D scores was notable, patients themselves commented on domains in interviews that are not captured by the survey, particularly the economic impact. The most consistent complaint was job loss and reduced income, in addition to the severe negative effects on physical, emotional, and social well-being. These results are consistent with those of previously published work evaluating the socioeconomic impact of traumatic lower leg injuries in Uganda, which identified the financial burden that withdrawal from the workplace has on a recovering patient following their injuries.21 Not only do extremity injuries and associated complications result in significant financial burden on individuals, but the cumulative impact may have broader impact on the economies of their countries.21 Tanzania’s large informal economic sector heavily relies on manual labor; hence, these complications are even more catastrophic to the economic well-being of these patients than in higher resource settings with more sedentary occupations and social safety nets.
These findings indicate that better training and resource allocation for managing soft-tissue injuries may improve outcomes for patients with IIIB open fractures in LMICs. However, the literature suggests that many LMICs lack access to plastic surgeons, particularly in Sub-Saharan Africa.18,19,34,35 Sustainable methods that emphasize soft-tissue training for both orthopedic and plastic surgeons have been proposed to address this unmet burden.36–38 One such example is the Surgical Management and Reconstructive Training (SMART) Course, which focuses on teaching the principles and lower rungs of the reconstructive ladder to non-plastic surgeons through a 2-day interactive course.5,12,39 Despite the reported success of training courses like these, surgeons continue to face significant barriers in resource allocation when performing soft-tissue reconstruction procedures.9 As such, policy-makers should focus on increasing plastic surgeons, providing sustainable training courses to non-plastic surgeons, and improving resource allocation in LMICs to improve outcomes for patients with devastating soft-tissue injuries.
This study had several potential limitations. First, the sample size was small because IIIB injuries are not common. Over the same time period, the host institution enrolled 270 patients with open tibia fractures, but only 10 were identified as type IIIB. The combination of quantitative and qualitative results is nonetheless effective in illustrating the poor outcomes for patients whose fractures are treated without flap coverage. Second, a longer follow-up period may identify if the generally negative effects of IIIB tibial injury can be considered permanent. A study of 23,653 patients in Canada suggested that QOL index scores did not return to pre-fracture levels for at least 3 years following a low-energy trauma.40 Patients’ QOL following traumatic injuries like IIIB tibial fractures may take just as long to recover, if not longer. Finally, there was no control group of patients who had early flap coverage to compare and measure the effect of soft-tissue reconstruction. Nonetheless, the 100% rate of complications in this cohort of patients is higher than other reported series of IIIB open tibia fractures, where flap procedures are often commonplace. A retrospective analysis of 120 patients with IIIB open tibia fractures in Singapore found that infection rates were near 30% and nonunion rates near 40% for patients who all received flap coverage within 1 week of injury.41 Furthermore, a systematic review examining 20 years of the literature estimated the infection rate for IIIB open tibia fractures treated with external fixation to be 13%–36%, which is significantly less than that reported in our study findings.42
In conclusion, this study demonstrates that patients in Tanzania with IIIB open tibia fractures experience high rates of infection and nonunion without the appropriate soft-tissue coverage, and poor long-term QOL. Managing IIIB open tibia injuries can be challenging for surgeons in all settings, but even more so when resources to perform soft-tissue reconstruction are not available.22,43 Opportunities to improve care by expanding access to plastic and reconstructive training are evident.5,10,11,44,45 The absence of resources to perform extremity soft-tissue reconstruction is not unique to Tanzania, having been reported in other LMICs across sub-Saharan Africa, Asia, and Latin America.9,10 This study further supports the clear need for training and allocation of resources for soft-tissue procedures for both plastic and orthopedic surgeons in LMICs.
Footnotes
Published online 21 December 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380:2197–2223. [DOI] [PubMed] [Google Scholar]
- 2.Mock C, Cherian MN. The global burden of musculoskeletal injuries: challenges and solutions. Clin Orthop Relat Res. 2008;466:2306–2316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gosselin RA, Spiegel DA, Coughlin R, et al. Injuries: the neglected burden in developing countries. Bull World Health Organ. 2009;87:246–246a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chalya PL, Dass RM, Mchembe MD, et al. Citywide trauma experience in Mwanza, Tanzania: a need for urgent intervention. J Trauma Manag Outcomes. 2013;7:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu HH, Patel KR, Caldwell AM, et al. Surgical Management and Reconstruction Training (SMART) course for international orthopedic surgeons. Ann Glob Health. 2016;82:652–658. [DOI] [PubMed] [Google Scholar]
- 6.Court-Brown CM, Bugler KE, Clement ND, et al. The epidemiology of open fractures in adults. A 15-year review. Injury. 2012;43:891–897. [DOI] [PubMed] [Google Scholar]
- 7.Kim PH, Leopold SS. In brief: Gustilo-Anderson classification. [corrected]. Clin Orthop Relat Res. 2012;470:3270–3274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bach O. Musculo skeletal trauma in an East African public hospital. Injury. 2004;35:401–406. [DOI] [PubMed] [Google Scholar]
- 9.Holler JT, Albright P, Challa S, et al. Barriers to performing soft tissue reconstruction procedures among orthopedic surgeons in low- and middle-income countries: results of a surgical skills training course. Plast Reconstr Surg Glob Open. 2019;7:e2420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Albright PD, Mackechnie MC, Jackson JH, et al. Knowledge deficits and barriers to performing soft-tissue coverage procedures: an analysis of participants in an orthopaedic surgical skills training course in Mexico. OTA International. 2019;2:e044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Hara NN, O’Brien PJ, Blachut PA. Developing orthopaedic trauma capacity in uganda: considerations from the Uganda sustainable trauma orthopaedic program. J Orthop Trauma. 2015;29Suppl 10S20–S22. [DOI] [PubMed] [Google Scholar]
- 12.Carey JN, Caldwell AM, Coughlin RR, et al. Building orthopaedic trauma capacity: IGOT international SMART course. J Orthop Trauma. 2015;29(Suppl 10S17–S19. [DOI] [PubMed] [Google Scholar]
- 13.Ikem IC, Oginni LM, Bamgboye EA. Open fractures of the lower limb in Nigeria. Int Orthop. 2001;25:386–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Conway DJ, Coughlin R, Caldwell A, et al. The institute for global orthopedics and traumatology: a model for academic collaboration in orthopedic surgery. Front Public Health. 2017;5:146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grimes CE, Bowman KG, Dodgion CM, et al. Systematic review of barriers to surgical care in low-income and middle-income countries. World J Surg. 2011;35:941–950. [DOI] [PubMed] [Google Scholar]
- 16.Ngcelwane M. Expanding the orthopaedic training programme to improve the management of lower extremity trauma. SA Orthopaedic J. 2015;14:14–15. [Google Scholar]
- 17.Corlew DS. Perspectives on plastic surgery and global health. Ann Plast Surg. 2009;62:473–477. [DOI] [PubMed] [Google Scholar]
- 18.Ozgediz D, Jamison D, Cherian M, et al. The burden of surgical conditions and access to surgical care in low- and middle-income countries. Bull World Health Organ. 2008;86:646–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Borrelli MR. What is the role of plastic surgery in global health? A review. World J Plast Surg. 2018;7:275–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Melvin JS, Dombroski DG, Torbert JT, et al. Open tibial shaft fractures: I. Evaluation and initial wound management. J Am Acad Orthop Surg. 2010;18:10–19. [DOI] [PubMed] [Google Scholar]
- 21.O’Hara NN, Mugarura R, Slobogean GP, et al. The orthopaedic trauma patient experience: a qualitative case study of orthopaedic trauma patients in Uganda. PLoS One. 2014;9:e110940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mathieu L, Potier L, Niang CD, et al. Type III open tibia fractures in low-resource setting. Part 2: soft-tissue coverage with simple, reliable and replicable pedicle flaps. Med Sante Trop. 2018;28:230–236. [DOI] [PubMed] [Google Scholar]
- 23.Pollak AN, McCarthy ML, Burgess AR. Short-term wound complications after application of flaps for coverage of traumatic soft-tissue defects about the tibia. The Lower Extremity Assessment Project (LEAP) study group. J Bone Joint Surg Am. 2000;82:1681–1691. [PubMed] [Google Scholar]
- 24.Clegg DJ, Rosenbaum PF, Harley BJ. The effects of timing of soft tissue coverage on outcomes after reconstruction of type IIIB open tibia fractures. Orthopedics. 2019;42:260–266. [DOI] [PubMed] [Google Scholar]
- 25.Saddawi-Konefka D, Kim HM, Chung KC. A systematic review of outcomes and complications of reconstruction and amputation for type IIIB and IIIC fractures of the tibia. Plast Reconstr Surg. 2008;122:1796–1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xu YQ, Lin YQ, Li J, et al. Repair and reconstruction of severe leg injuries: retrospective review of eighty-five patients. Chin J Traumatol. 2006;9:131–137. [PubMed] [Google Scholar]
- 27.Szende A, Janssen B, Cabases J, eds. Self-Reported Population Health: An International Perspective Based on EQ-5D. 2014Netherlands: Springer; [PubMed] [Google Scholar]
- 28.Govaert GAM, Kuehl R, Atkins BL, et al. Fracture-Related Infection (FRI) Consensus Group. Diagnosing fracture-related infection: current concepts and recommendations. J Orthop Trauma. 2020;34:8–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nyman JA, Barleen NA, Dowd BE, et al. Quality-of-life weights for the US population: self-reported health status and priority health conditions, by demographic characteristics. Med Care. 2007;45:618–628. [DOI] [PubMed] [Google Scholar]
- 30.Eliezer EN, Haonga BT, Morshed S, et al. Predictors of reoperation for adult femoral shaft fractures managed operatively in a sub-Saharan country. J Bone Joint Surg Am. 2017;99:388–395. [DOI] [PubMed] [Google Scholar]
- 31.Mathieu L, Mottier F, Bertani A, et al. Management of neglected open extremity fractures in low-resource settings: experience of the French army medical service in chad. Orthop Traumatol Surg Res. 2014;100:815–820. [DOI] [PubMed] [Google Scholar]
- 32.Brinker MR, Hanus BD, Sen M, et al. The devastating effects of tibial nonunion on health-related quality of life. J Bone Joint Surg Am. 2013;95:2170–2176. [DOI] [PubMed] [Google Scholar]
- 33.Doshi P, Gopalan H, Sprague S, et al. Incidence of infection following internal fixation of open and closed tibia fractures in India (INFINITI): a multi-centre observational cohort study. BMC Musculoskelet Disord. 2017;18:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Semer NB, Sullivan SR, Meara JG. Plastic surgery and global health: how plastic surgery impacts the global burden of surgical disease. J Plast Reconstr Aesthet Surg. 2010;63:1244–1248. [DOI] [PubMed] [Google Scholar]
- 35.Nangole WF, Khainga S, Aswani J, et al. Free flaps in a resource constrained environment: a five-year experience-outcomes and lessons learned. Plast Surg Int. 2015;2015:194174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Levin LS. The reconstructive ladder. An orthoplastic approach. Orthop Clin North Am. 1993;24:393–409. [PubMed] [Google Scholar]
- 37.Fernandez MA, Wallis K, Venus M, et al. The impact of a dedicated orthoplastic operating list on time to soft tissue coverage of open lower limb fractures. Ann R Coll Surg Engl. 2015;97:456–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jordan DJ, Malahias M, Khan W, et al. The ortho-plastic approach to soft tissue management in trauma. Open Orthop J. 2014;8:399–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Challa S, Conway D, Wu HH, et al. Can a 2-day course teach orthopaedic surgeons rotational flap procedures? An evaluation of data from the Nepal SMART course over 2 years. J Orthop Trauma. 2018;32Suppl 7S38–S42. [DOI] [PubMed] [Google Scholar]
- 40.Tarride JE, Burke N, Leslie WD, et al. Loss of health related quality of life following low-trauma fractures in the elderly. BMC Geriatr. 2016;16:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Singh A, Jiong Hao JT, Wei DT, et al. Gustilo IIIB open tibial fractures: an analysis of infection and nonunion rates. Indian J Orthop. 2018;52:406–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Papakostidis C, Kanakaris NK, Pretel J, et al. Prevalence of complications of open tibial shaft fractures stratified as per the Gustilo-Anderson classification. Injury. 2011;42:1408–1415. [DOI] [PubMed] [Google Scholar]
- 43.Chandran A, Hyder AA, Peek-Asa C. The global burden of unintentional injuries and an agenda for progress. Epidemiol Rev. 2010;32:110–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bhandari M, Tornetta P, III, Sprague S, et al. Predictors of reoperation following operative management of fractures of the tibial shaft. J Orthop Trauma. 2003;17:353–361. [DOI] [PubMed] [Google Scholar]
- 45.Clelland SJ, Chauhan P, Mandari FN. The epidemiology and management of tibia and fibula fractures at Kilimanjaro Christian Medical Centre (KCMC) in Northern Tanzania. Pan Afr Med J. 2016;25:51. [DOI] [PMC free article] [PubMed] [Google Scholar]


