Abstract
Background:
Breast reduction, also defined as reduction mammaplasty, is one of the most common procedures performed in aesthetic surgery. Multiple techniques have been proposed throughout the years and several classification systems have been adopted according to: type of incision, pedicle blood supply (cutaneous, glandular, dermoglandular), extent of undermining, excision area, simultaneous or separate tissue excision (fat/gland, skin, or both), and combination of the aforementioned. In the present article, we share our 10 years’ experience with reduction mammaplasty and we describe our personal technique, a modified superior pedicle breast reduction.
Methods:
We performed a retrospective analysis on 823 consecutive patients undergoing either aesthetic or functional reduction mammaplasty at Humanitas Research Hospital between 2009 and 2018. For each patient, we evaluated the mean resection volume and complication rate. We also assessed patients’ satisfaction (VAS scale) and aesthetic outcome (assessed by independent surgeons, scale from 1 to 5).
Results:
The average patient age was 48, ranging from 17 to 77 years. The average operative time was 77 minutes, ranging from 62 to 123 minutes. After a thorough follow-up of these patients, we can conclude that our technique has a low complication rate, patients’ satisfaction is excellent, and the result is stable over time in terms of shape and symmetry (the mean VAS score was 8.1). Postoperative surgeon’s photographs evaluation scores were 4.5 ± 0.5. Average resected volume was 860gr.
Conclusion:
The proposed technique is safe, fast, and simple with a relatively short learning curve, making it didactic and intuitive for young surgeons.
INTRODUCTION
Breast is a symbol of femininity, whose importance is great and widespread. Surgical and psychological aspects, as well as reconstructive and aesthetic problems are involved in reduction mammaplasty. In the early 20th century, almost all the technical possibilities were attempted in a pioneer stage (Hollander 1924,1 Biesenberger 19282), and around 1960 (Wise 1956,3 Arié 1957,4 Strombeck 1960,5 Pitanguy 19606) the debate focused on safety and survival of the nipple–areola complex and skin flaps. Subsequently, different techniques have been proposed to achieve safety and improve aesthetic outcome. A great deal of different surgical approaches has been described, and several classification systems have been proposed according to type of incision, pedicle blood supply (cutaneous, glandular, dermoglandular), extent of undermining, excision area, simultaneous or separate tissue excision (fat/gland, skin or both), and combination of the aforementioned. The recent debate has been focusing on preservation of sensation and breast-feeding function and it has been enhanced by innovations, such as the possibility of inframammary fold repositioning, coating with alloplastic materials, liposuction, periareolar, and, in general, short scars breast reduction.
Vertical, horizontal (Strombeck5), oblique (Skoog,7 Hauben,8 Hall-Findlay9), and central or posterior (Balch,10 Hester,11 Goes12) pedicle designs have been described. Vertical pedicles may be inferiorly (Robbins,13 Courtiss and Goldwyn,14 Hammond15), superiorly (Arié,1 Pitanguy,6 Weiner,16 Lassus,17,18 Marchac,19 Lejour20,21), or bipedicle-based (Strombeck5 and McKissock22). Most techniques produce an inverted-T or anchor-shaped scar (Arié,4 Skoog,7 Pitanguy,6 Weiner,16 Hauben9). Lassus initially proposed a vertical scar without undermining that was subsequently modified with short inframammary scar11,12 similarly to Marchac’s.19 Hinderer 1969,23 Benelli 1989,24 Bustos 1992,25 Toledo 198926 described just periareolar scar, remodeling, and reducing breast volume in different ways.
In the present study, we report our 10 years’ experience with reduction mammaplasty and we describe our personal technique, analyzing pros and cons compared the state of the art. This fast and safe technique, which is a modified superior pedicle breast reduction, allows the authors to simulate and visualize the final result since the very beginning guiding the surgeons in drawings to obtain the initial model.
MATERIAL AND METHODS
Clinical Assessment and Patient Selection
We performed a retrospective analysis on 823 consecutive patients undergoing either aesthetic or functional reduction mammaplasty at Humanitas Research Hospital between 2009 and 2018. All patients were evaluated for clinical history and physical examination to assess volume and shape of the breast, identify asymmetries (gland volume, nipple–areola complex [NAC] position, ptosis, breast base asymmetries), quality of tissues, presence of chest wall or spinal deformities, NAC sensibility, comorbidity, and pre-operative patients’ desires. Complete preoperative routine blood workup, ECG, and bilateral breast echotomography were performed in all patients. Bilateral mammography was performed in patients aged over 40 years. Smokers (more than 20 cigarettes per day) and patients with diabetes mellitus, previous mastectomy, lumpectomy, mammaplasty, or mastopexy were excluded from this review. All the remaining patients were selected for this study and treated with our personal technique, described as follows.
The average age was 48 years (ranging between 17 and 77 years). The average preoperative bra cup size was between F and G, ranging from D to H. 73% of the patients treated had asymmetrical breasts. The average notch-NAC distance was 29.7 cm. An estimated 21% of the patients had a Grade II ptosis, 73% a Grade III, and 6% a pseudoptosis (according to Regnault Ptosis Scale). We included in our study monolateral and bilateral breast reduction. The average hospitalization time was 1–2 days.
For each patient, we collected preoperative standards anterior-posterior, oblique and lateral preoperative, short and long term postoperative photographs. We administered perioperative antibiotic prophylaxis with one shot preoperative cefazolin 2000 mg i.v. to all patients (the patients allergic to cephalosporins were administered clindamycin 600 mg i.v.).
For each patient, we evaluated the resection volume and the complication rate (wound dehiscence, cellulitis, rate of partial/complete NAC necrosis, hematoma/seroma, poor scarring, loss of NAC sensibility, breast asymmetries). Furthermore, we administered a 1-year postoperative VAS (0–10) to all patients to assess patients’ satisfaction. Overall feeling about breasts, appearance, shape, symmetry, and volume achieved were assessed.
Finally, examination of preoperative and 1-year postoperative photographs was performed by three independent plastic surgeons with a specific expertise in breast surgery (who did not perform the breast reduction) in a blinded fashion to assess aesthetic outcome. Postoperative photographs were scored from 1 to 5 (1: very poor outcome; 2: poor outcome; 3: acceptable outcome; 4: good outcome; 5: optimal outcome) in terms of symmetry (volume, ptosis, NAC position), shape of the breast, and scar quality.
Surgical Technique
We adopted a modified superior pedicle breast reduction personal technique, which includes the following steps:
Preoperative Markings
Markings in the standing position:
1) The midpoint of the suprasternal notch, the median sternal line, and the existing inframammary fold are marked. Then, measuring tape is placed around the patient’s neck, passing through the two NACs. We draw the two lines that go from the clavicle to the NAC, continuing inferiorly perpendicularly across the inframammary fold. This is the vector that we follow when planning the new position of the NAC (ascent vector). This vector passes close the midclavicular line, usually more medially.
2) The new nipple position is referred normally to the anterior projection of the inframammary fold along the previous medial line. This point can be adjusted depending on the breast type (considering the degree of ptosis or pseudoptosis). In case of stenotic breasts, with a high inframammary fold, the position of the nipple is lower than expected. As a general rule, the new NAC corresponds to the midpoint of the humerus according to the patient’s physical proportions.
Markings when the patient lies supine with open arms:
3) The pinching maneuver displays the final breast shape/cone, with respect to the chest and arms. The position of the new breast apex and the hypothetical areolar circumference is marked along the ideal breast axis, according to the previous fixed points. The length of the new mammary base is highlighted (Fig. 1).
4) Two vertical curved lines are marked below the new areola up to a point usually located in the central breast line, 2–3 cm above the inframammary fold. The distance between the lines points out the amount of tissue to remove; the wider the keyhole is, the tighter the base will be (Fig. 2). Breast is moved medially and laterally to check the 2 vertical lines reaching the central position.
5) The sulcus (horizontal part of the keyhole) will be marked during the surgical procedure.
6) Contralateral breast is planned verifying the distances with a caliper to obtain symmetry respect to the first one.
Fig. 1.
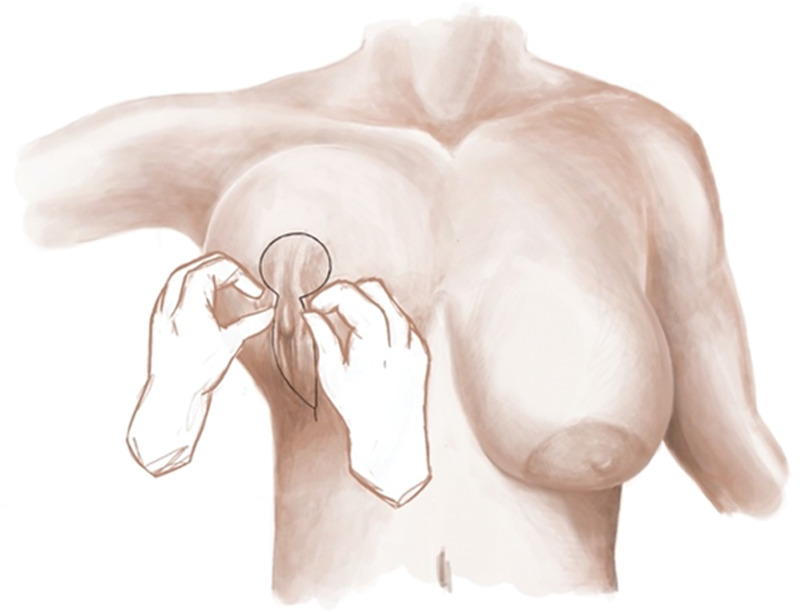
Diagram showing the position of the new NAC with the pinching maneuver and prefiguration of final shape.
Fig. 2.
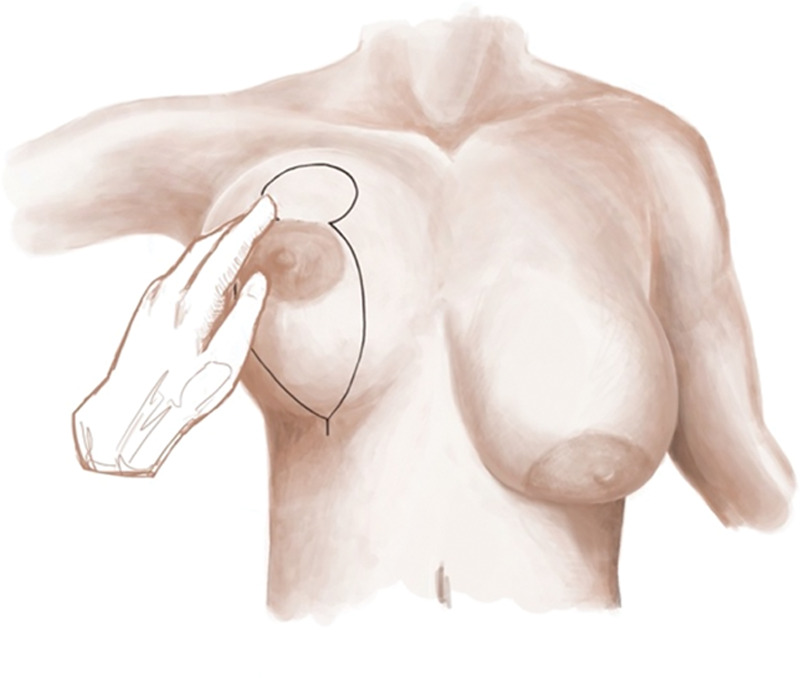
Drawing of the two vertical lines joining 2–3 cm up to the inframammary fold.
Surgical Procedure
1) De-epithelization of the superior pedicle is performed extending it toward the 2 vertical lines medially and laterally, 1 cm lower to the inferior border of the areola.
2) A vertical wedge of skin, gland, and fat is resected below the existing areola, until the pectoralis major fascia, with lateral gland extension (boot-shaped vertical resection). Excessive soft tissue resection at the medial quadrants is avoided.
3) A wide glandular undermining is carried out from the outer pectoralis major fascia, preserving the medial and lateral perforator vessels27,28 (Fig. 3).
4) The central glandular flap supporting the areola (pedicle) is suspended to the pectoralis major fascia at a higher point to obtain more fullness in the upper pole (one or two stitches of non-absorbable suture) and to prevent premature postoperative ptosis.
5) After lateral and medial dermal incision of the pedicle, the areola is suspended to the new position.
6) Deep and/or superficial conization resorbable stitches (Polyglactin 1) are placed at different levels at the vertical resection site according to the final shape we aim for. The projection of the final breast and the width of the base are strictly related to the depth of stitches.
7) Intraoperatively the horizontal portion of skin, gland, and fat to be resected in the lower quadrants is defined, between the original inframammary fold (IMF) and a horizontal curved superior line obtained with the pressure of the fingers (Fig. 4). A length between 4.5 and 6 cm of the areola-IMF distance should be proportioned to the patient’s size and breast volume. The new inframammary fold is higher than the original IMF, as previously described in the scientific literature.19 Sometimes performing only skin resection at the IMF leaves 2 superiorly pedicled remaining gland flaps (after dermal release) to be flipped or split as an “auto-implant” behind the new breast cone looking for volume increase in the central pole.
8) The new mammary cone is then fixed at the horizontal resection site. To medialize the breast, the vertical suture is fixed up to 1–2 cm medial to the initial central axis.
9) Hypodermal and subcuticular mattress sutures are placed to close all the incision lines.
10) No drains are requested because of the self-compression of the technique.
11) Sterile tapes are placed on the suture lines and an elastocompressive dressing is positioned, simulating a bra, for 3–4 days; after this, dressing is removed and the patient is suggested to wear a criss-cross-like bra, with the nipple in the center of the cup, so the elastic border can press and fix the new inframammary fold.
Fig. 3.
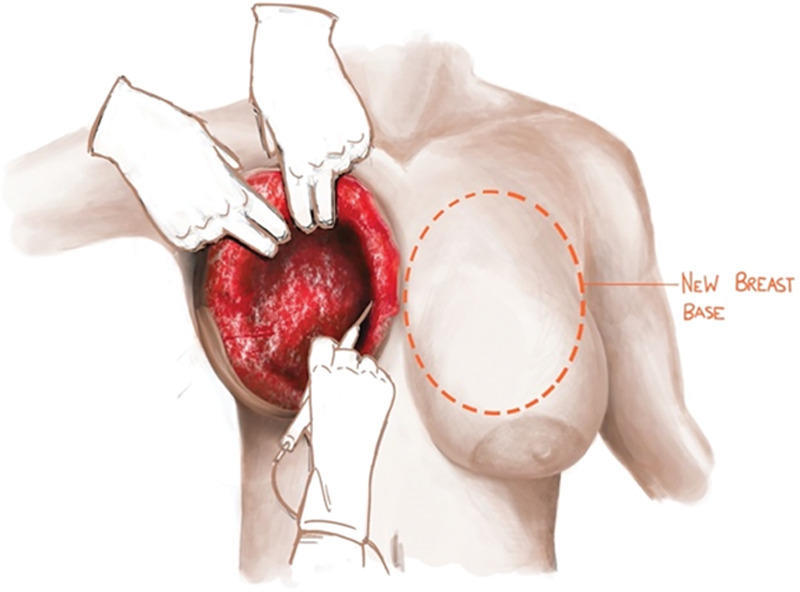
Illustration showing the wide detachment of the gland from the pectoralis major fascia (outlined area).
Fig. 4.
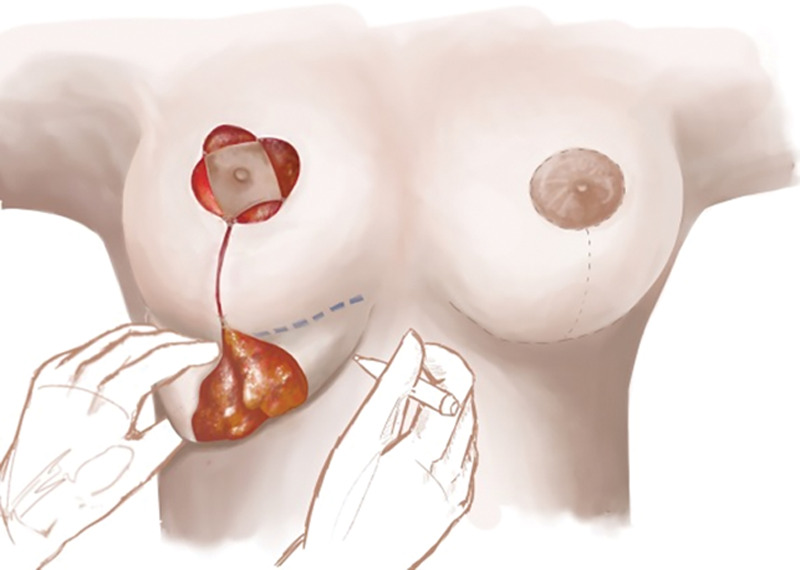
Intraoperative drawing of the horizontal scar.
Optional steps include:
– Liposuction of the lateral quadrants or the innermost central region of the mammary gland to further remodel the lateral edge of the breast and to reduce the density of the mammary tissue.
– Periareolar purse string non-absorbable suture to reduce the new areolar circumference and/or modify the length of the vertical scar.
RESULTS
The average patient age was 48, ranging from 17 to 77 years. The average operative time was 77 minutes, ranging from 62 to 123 minutes. Patients were discharged mostly after 1 or 2 days, even though in specific cases we were able to perform this surgical procedure in a day-hospital setting. Average resected volume was 860gr per breast.
Overall complication rate was 35% (Table 1). Transient areolar hypoesthesia was quite common (30% of the patients), and permanent hypoesthesia at 1 year after surgery occurred in less than 1%; we did not have any case of complete loss of areolar sensation (excluding complete NAC necrosis). Partial NAC necrosis occurred in 3% of our patients, while total NAC necrosis occurred in 0.48%. Infection was seen in 0.97%, and hematoma occurred in 0,48% (we had only early hematomas, no cases of late ones): only half of them needed to be drained in the operating room. Seroma was a complication for 2% of our patients. The incidence of poor scarring was 4%, wound dehiscence (all <2 cm) was a complication in 5.1% of the patients.
Table 1.
Complication Rate
| Complication | No. Patients | Percentage |
| Seroma | 17 | 2 |
| Hematoma | 4 | 0.48 |
| Infection | 8 | 0.97 |
| Wound dehiscence | 42 | 5.1 |
| NAC necrosis | Partial: 25 | 3 |
| Complete: 4 | 0.48 | |
| Loss of NAC sensibility | Transient: 247 | 30 |
| Permanent: 6 | 0.72 | |
| Poor scarring | 33 | 4 |
Aesthetic outcome in terms of shape and symmetry was satisfying and stable over time. We achieved a breast natural appearance with high patients’ satisfaction (mean VAS score 8.1). Postoperative surgeon’s photographs evaluation scores were 4.5±0.5. Postoperative follow-up was made at 1, 3, 6, and 12 months after surgery. We had no patients lost to follow up (Figs. 5, 6, and 7).
Fig. 5.
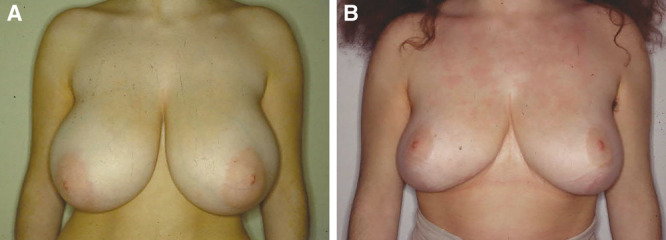
Case 1. A, Patient with hypertrophic bilateral breast. B, Same patient after 1 year from the breast reduction.
Fig. 6.
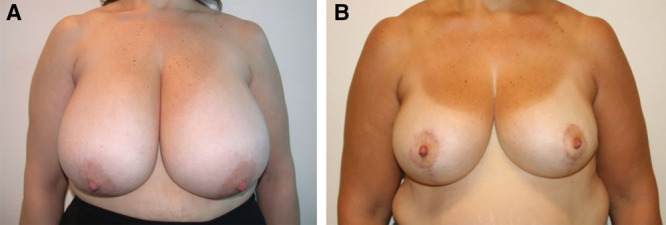
Case 2. A, Patient with bilateral gigantomastia. B, Same patient after 1 year from the breast reduction.
Fig. 7.
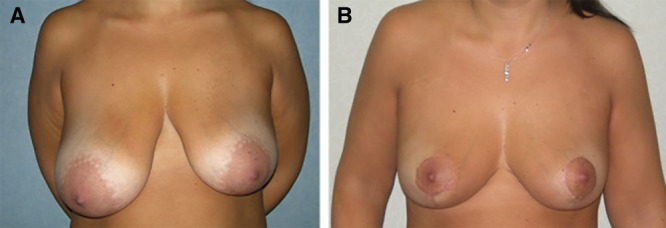
Case 3. A, Patient with bilateral asymmetric hypertrophic breast (right > left). B, Same patient after 1 year from the breast reduction, with a good symmetry between the two breasts.
DISCUSSION
The correct approach to treat mammary hypertrophy and ptosis should evaluate local anatomy, breast composition, systemic and local conditions, psychosocial aspects, and most importantly the entire body proportions. The ideal procedure has been defined by Goldwyn as “safe, simple, speedy, bloodless and relatively scarless, to achieve exquisite, unchanging and normal results with respect to sensation, function, and palpation.”14,29 Hauben added: “size, symmetry, suitable, sexy-shaped breasts, as well as sine sanguine.”30 Each technique may provide excellent results and has both advantages and drawbacks, and no single technique is suitable for all types of breast hypertrophy.
In the present study, we describe a personally modified superior pedicle technique for breast reduction. The key aim characterizing our approach is to obtain a new aesthetically appealing breast cone, different from the initial preoperative shape, instead of a simply reduced breast.
We do not refer to rigid measurements to identify the new nipple position because we always refer to patient’s body proportions and planned breast volume. Thus, we usually place the new nipple at the midlevel of humerus and/or at the level of the anterior projection of the inframammary fold corresponding to the apex of the breast cone displayed by pinching maneuver. In addition, we usually shift the vertical axis of the new breast medially to the mid clavicular point to minimize the lateral displacement of the cone.
The true innovative concept of our technique is the initial pre-representation of the desired breast shape, that can be easily displayed through the pinching maneuver marking preoperatively the upper part of the “keyhole” representing the new areolar position along the breast axis previously determined.
The lower part of the “keyhole” marking, defining the vertical wedge resection, is planned in a curved fashion, extending from the inferior edges of the new areolar circumference converging to a point located 2–3 cm above the inframammary fold. We can plan and adjust the vertical skin and glandular wedge resection to modify breast volume and breast base as desired, thus obtaining a new breast cone. Again, we do not need rigid measurements to determine the resection width that can be adjusted according to the modification of the breast base and volume that we want to obtain. The same maneuvers are reproduced on the contralateral breast.
We always perform a wide glandular detachment from the outer pectoralis major fascia. The wide undermining allows an effective repositioning and complete reshaping of the gland necessary for the creation of the new breast cone. Intra- and postoperative bleeding is minimized due to the wide glandular detachment, allowing a fast and easy hemostasis. Concerning safety and vascularization, our results show a low incidence of postoperative flaps and NAC necrosis. The wide superior dermoglandular pedicle ensures a reliable vascularization to the NAC. The vertical inferior wedge resection associated with a wide retromammary dissection allows preserving the main vascular and lymphatic systems located within the medial and lateral walls of the gland rising mainly from the perforator branches of the internal mammary artery and lateral thoracic artery.27,28 Marcus described significant variations in periareolar subcutaneous plexuses: in 70%–75% of cases, a complete periareolar ring is formed by perforating branches of the lateral thoracic artery, internal mammary artery, and intercostal arteries; in 20% of cases, branches of the lateral thoracic artery predominate and form a loop around the areola; in 5% of cases, a radial pattern without anastomotic ring is found. In our experience, skin and parenchymal wedge resection just below the areola allows preserving periareolar vascular plexus and sensation.
Medial and lateral wide dermal pedicle releasing incisions are usually performed to decrease tension forces at the new areolar site, thus favoring a tension-free pedicle inset. We usually place one or two suspension stitches anchoring the gland to the outer pectoralis fascia. The suspension sutures are placed to restore the upper pole fullness without flattening the gland and they contribute to the stability of the new breast shape, although there is a physiological reduction of upper pole convexity due to the gravity at 1 year.
The level of conization stitches is an additional versatile tool to modify breast projection and breast base, substantially affecting the final breast shape. The deeper we place the suture, the more projection and breast base narrowing we obtain. At this point modifying breast shape is still possible.
The horizontal resection at the inframammary fold is planned to obtain a final vertical scar length between 4.5 and 6 cm according to the patient’s body proportions. We do not extend the vertical scar length beyond 6 cm to avoid bottoming out deformity and upward areolar malpositioning. In addition, the inferior resection and the consequent horizontal scar allow us a possible medial advancement of the entire new mammary cone. The horizontal resection can be limited to the skin, while using superior pedicle glandular flaps to increase projection and fullness of the central pole.
We do not place drains for the self-compression produced in a minimal cavity.
Furthermore, the operative time is relatively short if compared with other techniques, as originally described by their authors. Operating time normally does not exceed 80–90 minutes.
This approach has some of the typical limitations associated with the classical superior pedicle techniques: it can be difficult to apply in severe ptosis (distance NAC-sternal notch > 30 cm), where inferior pedicle or bipedicle might be more suitable, for a matter of ptosis, not of volume. Liposuction sometimes allows shorter lateral scar and volume reduction at the lateral breast. Vertical and horizontal scars are normally inconspicuous, especially the horizontal one, which is pressed on by the corner of the bra, definitely leaving to the quality of the periareolar one. However, the technique described is very adaptable and adequate in different kinds of breasts in terms of volume, shape, and composition, with results that are fast and safe and furthermore useful to learn to young surgeons.
CONCLUSIONS
The variability and adaptability of the initial steps of the procedure make it suitable for different types of breasts. No rigid and strict preoperative or intraoperative markings are needed because the result can be easily predetermined with the pinching maneuver. Upper pole and final shape are aesthetically satisfying and quite attractive, respecting the body proportions. The proposed technique is safe, fast, and simple with a relatively short learning curve, making it didactic and intuitive for young surgeons.
Footnotes
Published online 2 December 2020.
Disclosure: No financial support or benefits have been received by any author. We do not have any relationship with any commercial source related directly or indirectly to this article. The principles outlined in the Declaration of Helsinki have been followed in this study.
REFERENCES
- 1.Holländer E. Die Operation der Mammahypertrophie und der Haengebrust. Dtsch Med – Wochenschr. 1924;41:1400. [Google Scholar]
- 2.Biesenberger H. Eine neue Methode der Mammaplastik. Zentralbl Chir. 1928;55:2382. [Google Scholar]
- 3.Wise RJ. A preliminary report on a method of planning the mammaplasty. Plast Reconstr Surg (1946). 1956;17:367–375. [DOI] [PubMed] [Google Scholar]
- 4.Arié G. Una nueva téchnica de mastoplasia. Rev Lat Am Cir Plast. 1957;3:22. [Google Scholar]
- 5.Strombeck JO. Mammaplasty: report of a new technique based on the two-pedicle procedure. Br J Plast Surg. 1960;13:79–90. [DOI] [PubMed] [Google Scholar]
- 6.Pitanguy I. Breast ipertrofy. 1960:In: Transactions of International Society of Plastic Surgeons. Second Congress, London, 1959 Edinburgh, Scotland: Livingstone; 509. [Google Scholar]
- 7.Skoog T. A technique of breast reduction; transposition of the nipple on a cutaneous vascular pedicle. Acta Chir Scand. 1963;126:453–465. [PubMed] [Google Scholar]
- 8.Hauben DJ. Experience and refinements with the supero-medial dermal pedicle for nipple-areola transposition in reduction mammaplasty. Aesth Plast Surg. 1984;8:189. [DOI] [PubMed] [Google Scholar]
- 9.Hall-Findlay EJ. A simplified vertical reduction mammaplasty: shortening the learning curve. Plast Reconstr Surg. 1999;104:748–759; discussion 760. [PubMed] [Google Scholar]
- 10.Balch CR. The central mound technique for reduction mammaplasty. Plast Reconstr Surg. 1981;67:305–311. [DOI] [PubMed] [Google Scholar]
- 11.Hester TR, Jr, Bostwick J, III, Miller L, et al. Breast reduction utilizing the maximally vascularized central breast pedicle. Plast Reconstr Surg. 1985;76:890–900. [DOI] [PubMed] [Google Scholar]
- 12.Goes JCS. Periareolar mammaplasty: double skin technique. Rev Bras Cir Plast. 1989;4:55. [Google Scholar]
- 13.Robbins TH. A reduction mammaplasty with the areola-nipple based on an inferior dermal pedicle. Plast Reconstr Surg. 1977;59:64–67. [DOI] [PubMed] [Google Scholar]
- 14.Courtiss EH, Goldwyn RM. Reduction mammaplasty by the inferior pedicle technique. An alternative to free nipple and areola grafting for severe macromastia or extreme ptosis. Plast Reconstr Surg. 1977;59:500–507. [PubMed] [Google Scholar]
- 15.Hammond Hammond DC. Short scar periareolar inferior pedicle reduction (SPAIR) mammaplasty. Plast Reconstr Surg. 1999;103:890–901. [DOI] [PubMed] [Google Scholar]
- 16.Weiner DL, Aiache AE, Silver L, et al. A single dermal pedicle for nipple transposition in subcutaneous mastectomy, reduction mammaplasty, or mastopexy. Plast Reconstr Surg. 1973;51:115–120. [DOI] [PubMed] [Google Scholar]
- 17.Lassus C. A technique for breast reduction. Int Surg. 1970;53:69–72. [PubMed] [Google Scholar]
- 18.Lassus C. Breast reduction: evolution of a technique. A single vertical scar. Aesthet Plast Surg. 1987;11:107. [DOI] [PubMed] [Google Scholar]
- 19.Marchac D, de Olarte G. Reduction mammaplasty and correction of ptosis with a short infra mammary scar. Plast Reconstr Surg. 1982;69:45. [PubMed] [Google Scholar]
- 20.Lejour M, Abboud M. Vertical mammaplasty without inframammary scar and with breast liposuction. Perspect Plast Surg. 1990;4:67. [Google Scholar]
- 21.Lejour M. Vertical mammaplasty and liposuction of the breast. Plast Reconstr Surg. 1994;94:100–114. [DOI] [PubMed] [Google Scholar]
- 22.McKissock PK. Reduction mammaplasty with a vertical dermal flap. Plast Reconstr Surg. 1972;49:245–252. [DOI] [PubMed] [Google Scholar]
- 23.Hinderer U. Primera experiencia con una nueva tecnica de mastoplastia para ptosis ligeres. Presented at the Sixth National Reunion of Spanish Society of Plastic and Reparative Surgery; October 29–31, 1969; Madrid. [Google Scholar]
- 24.Benelli L. A new periareolar mammoplasty: the “round block” technique. Aesth Plast Surg. 1990;14:93. [DOI] [PubMed] [Google Scholar]
- 25.Bustos RA. Periareolar mammaplasty with silicone supporting lamina. Plast Reconstr Surg. 1992;89:646–657; discussion 658. [PubMed] [Google Scholar]
- 26.Toledo LS, Matt Sudo PKR. Mammoplasty using liposuction and periareolar incision. Aesth Plast Surg. 1989;13:9. [DOI] [PubMed] [Google Scholar]
- 27.Marcus GH. Untersuchungen uber die arterielle Blutversorgung der Mamilla. Archiv fur klinische. Langenbecks Arch Klin Chir. 1934;179:361–369. [Google Scholar]
- 28.Maliniac JW. Arterial blood supply of the breast: revised anatomic data relating to reconstructive surgery. Arch Surg. 1943;47:329. [Google Scholar]
- 29.Goldwyn RM, ed. Complications and unfavorable results of reduction mammaplasty. In: Reduction Mammaplasty. 1990:Toronto: Little, Brown; 561–578. [Google Scholar]
- 30.Hauben DJ. Superomedial pedicle technique of reduction mammaplasty (discussion). Plast Reconstr Surg. 1989;83:479. [DOI] [PubMed] [Google Scholar]


