Abstract
Objective
The study sought to assess awareness, perceptions, and value of telehealth in primary care from the perspective of patients.
Materials and Methods
We conducted a cross-sectional, Web-based survey of adults with access to telehealth services who visited healthcare providers for any of the 20 most-commonly seen diagnoses during telehealth visits. Three groups were studied: registered users (RUs) of telehealth had completed a LiveHealth Online (a health plan telehealth service provider) visit, registered nonusers (RNUs) registered for LiveHealth Online but had not conducted a visit, and nonregistered nonusers (NRNUs) completed neither step.
Results
Of 32 831 patients invited, 3219 (9.8%) responded and 766 met eligibility criteria and completed surveys: 390 (51%) RUs, 117 (15%) RNUs, and 259 (34%) NRNUs. RUs were least likely to have a primary care usual source of care (65.6% vs 78.6% for RNUs vs 80.0% for NRNUs; P < .001). Nearly half (46.8%) of RUs were unable to get an appointment with their doctor, and 34.8% indicated that their doctor’s office was closed. Among the 3 groups, RUs were most likely to be employed (89.5% vs 88.9% vs 82.2%; P = .007), have post–high school education (94.4% vs 93.2% vs 86.5%; P = .003), and live in urban areas (81.0% vs 69.2% vs 76.0%; P = .021).
Conclusions
Telehealth users reported that they relied on live video for enhanced access and were less connected to primary care than nonusers were. Telehealth may expand service access but risks further fragmentation of care and undermining of the primary care function absent better coordination and information sharing with usual sources of patients’ care.
Keywords: telemedicine, primary health care, access to health care
BACKGROUND AND SIGNIFICANCE
Primary care, described as a relationship involving first contact, comprehensive, coordinated, and continuous care, has been shown to lead to better health outcomes.1,2 By directing patients to appropriate specialists and tests, interpreting and managing undifferentiated symptoms, and understanding the natural course of disease, primary care allows for the efficient allocation of resources.2 To receive primary care services, patients often seek help from people or facilities that can help with navigating most health care needs, also known as usual sources of care (USCs). In addition to improving reported access, having a USC has been linked to better quality, lower costs, and greater equity.3–5
Telehealth, fueled by an explosion of Internet-connected devices and changing consumer expectations, provides opportunities to increase access for individuals with geographical, transportation, or time constraints.6 Accessing medical care through this medium eliminates many of these historical barriers. The American Telemedicine Association has defined telemedicine as the use of medical information that is exchanged from one site to another through electronic communications to improve a patient’s health and goes on to describe telehealth as encompassing remote health care that does not always involve clinical services.7 Despite decades of use of telehealth in other disciplines and half of all U.S. hospitals employing some type of telehealth, primary care physicians remain early adopters of video visits and other telehealth services.8,9 Kaiser Permanente has reported that a growing percentage of interactions between their physicians and patients are conducted through virtual means,10 leaving many wondering whether the system is an outlier or a harbinger.
Prior research has demonstrated that patients accept telehealth and are satisfied with the services received,11–22 and users consider the quality of visits comparable to in-person visits. However, existing studies demonstrate that patients without exposure to telehealth have concerns regarding the quality of the encounter and whether diagnoses can be made virtually.16,19 These concerns are echoed among providers as some have less confidence in virtual rather than in-person diagnoses.8 The evidence for the impact of telehealth on clinical outcomes is mixed. While most outcomes were similar for telehealth and in-person visits, a few found improvements among patients receiving telehealth.14,23 None of the studies found providing care remotely worsened clinical outcomes.
The relationship between telehealth and costs is similarly mixed, encapsulating the heterogeneity of telehealth uses.13,24,25 Some have demonstrated that telehealth is associated with reduced per-visit spending and fewer diagnostic tests, while others argue that the enhanced access afforded by telehealth leads individuals to seek care for conditions they historically would have monitored on their own.25,26 One strategy for improving access and controlling costs is tighter integration between primary care USCs and telehealth, although this is an approach that needs evaluation. Today, the majority of video visits are for acute, often self-limited conditions, such as upper respiratory infections.25 Given the resources devoted to addressing chronic disease, using telehealth for conditions such as diabetes and depression could more definitively reduce costs although telehealth adoption among primary care physicians would need to increase.8,26,27 To better understand how patients with access to live video visits perceive their USC and telehealth options, and to better understand differences between those who use telehealth and those who do not, we developed an Internet survey to assess the characteristics, attitudes, and use of primary care by individuals with access to LiveHealth Online (LHO), a health plan telehealth service provider and video visit platform consisting of an application and website providing access to U.S. board-certified physicians and licensed therapists via live video visits.
MATERIALS AND METHODS
Study design and data source
This was a cross-sectional Internet survey of individuals who had access to telehealth services. The data source for the study was the HealthCore Integrated Research Database (HIRD®), a large administrative claims healthcare database that can be linked to inpatient and outpatient medical records, member and provider survey data, and point-of-care clinical data to provide a fully integrated, comprehensive dataset. The HIRD was used as a sampling frame to identify the eligible survey population; in addition, claims from the HIRD were used to determine Deyo-Charlson Comorbidity (DCI) index scores28 and assess the prevalence of 10 common chronic conditions among survey respondents (Supplementary Table S2). The protocol was approved by the American Academy of Family Physicians and New England Institutional Review Boards.
Survey population
The survey population consisted of health plan members who utilized LHO during the most recent 12 months for which usage information was available as well as random samples of members who were eligible for LHO but did not use it. In 2017, there were over 130 000 LHO visits, 89% of which were for adults. The inclusion criteria were: (1) commercially insured adults (aged 18 and older) who (2) were eligible to use LHO, (3) had a valid e-mail address, and (4) had either an in-person physician office visit or video visit conducted between March 2016 and February 2017 for at least 1 of the 20 most common diagnoses seen during LHO visits (Supplementary Table S1). To ensure accurate group categorization, those who agreed to the survey answered 3 screening questions regarding whether they were aware of LHO services, had registered for LHO services, and had used LHO services. These questions included “refused” and “not sure” options, which further limited eligible participants. The survey opened on August 21, 2017, and closed on September 29, 2017, and this sampling methodology has been used in other studies.29 Respondents received $25 upon survey completion. Screening questions allowed respondents to be categorized into 3 groups: registered users (RUs), registered nonusers (RNUs), and nonregistered nonusers (NRNUs). We sought to obtain at least 750 completed surveys, with quotas of 375 RU surveys, 188 RNU surveys, and 187 NRNU surveys. Ultimately, we sought an equivalent number of users and nonusers across the sample.
Survey
We developed our survey instrument based on insights derived from a literature review and informant data extracted from a convening of national experts (Supplementary Appendix). The cross-sectional Internet survey assessed basic demographic information, such as age, sex, race/ethnicity, education level, and employment status. When appropriate, questions from the Telemedicine Satisfaction and Usefulness Questionnaire were adapted and included.28 To identify USCs, we asked if there was a particular doctor’s office, clinic, health center, or other place that respondents usually went for their general health care. We categorized respondents as having a primary care USC if they answered yes to “A family or primary care physician/doctor’s office (eg, family physician/doctor, internal medicine doctor).” The questions pertaining to demographics and use of in-person care were the same for all survey groups; otherwise, questions were tailored to experiences unique to each of the 3 groups.
Analysis
To compare differences across the 3 groups and determine the extent to which respondents and nonrespondents were similar, we used chi-square tests for categorical variables (using Stata 14.0). We considered an alpha <.05 to be statistically significant.
RESULTS
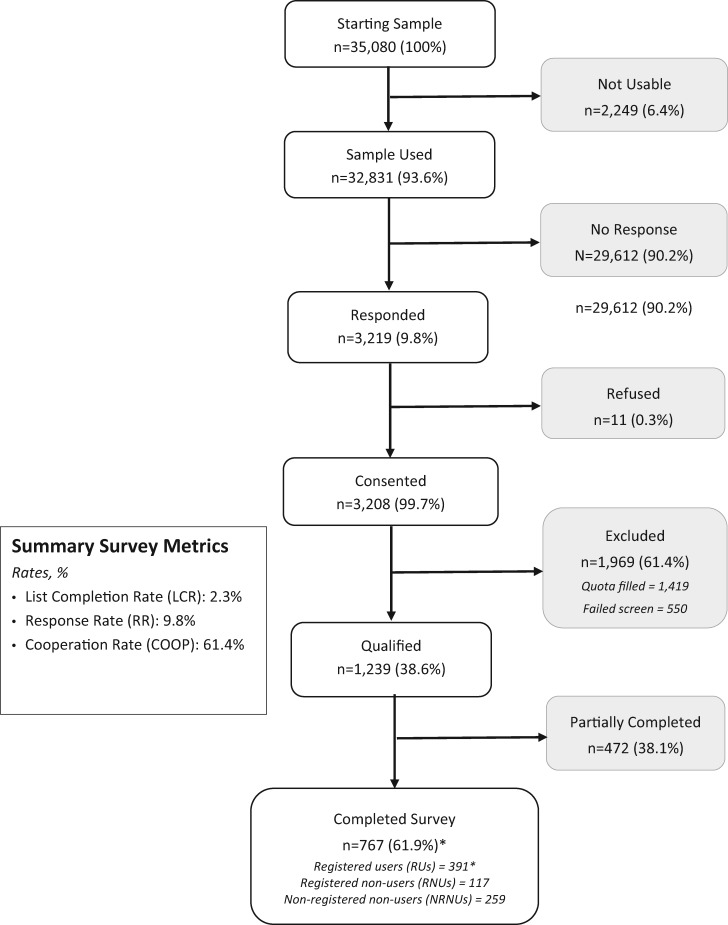
Of the 32 831 individuals who received an e-mail invitation to participate in the survey, 3219 responded (9.8% response rate), 3208 gave electronic consent, 1239 qualified for the survey, and 767 completed the survey (Figure 1 ). However, the analysis was based on 766 completed surveys; 1 RU respondent was excluded because all of their responses were missing. The cooperation rate (the number of completed surveys divided by the difference between the number contacted and number excluded) was 61.4%. Nearly 400 (n = 390, 51%) were RUs, while 117 (15%) were RNUs and 259 (34%) were NRNUs (Table 1). A comparison of respondents and nonrespondents among both telehealth users and nonusers showed that they were similar in age and DCI comorbidity burden but differed in sex and region. Compared with nonrespondents, a greater proportion of respondents were women and lived in the Midwest (Supplementary Tables S3 and S4).
Figure 1.
Survey sample disposition.
Table 1.
Demographic characteristics, by user group
| User Group |
|||||
|---|---|---|---|---|---|
| Registered User |
Registered Nonuser |
Nonregistered Nonuser |
|||
| n = 390/406a | n = 117/121b | n = 259/267c | |||
| Characteristics | % | % | % | P Value | |
| Age | 18–29 y | 15.1 | 10.3 | 12.0 | .296 |
| 30–44 y | 44.9 | 39.3 | 44.8 | ||
| 45–64 y | 38.7 | 47.9 | 40.2 | ||
| 65 y or more | 1.3 | 2.6 | 3.1 | ||
| Missing | 0.0 | 0.0 | 0.0 | ||
| Sex | Male | 28.5 | 31.6 | 32.4 | .528 |
| Female | 71.5 | 68.4 | 67.6 | ||
| Missing | 0.0 | 0.0 | 0.0 | ||
| Race/Ethnicity | Non-Hispanic White | 88.2 | 88.9 | 91.5 | .694 |
| Non-Hispanic Black | 3.3 | 4.3 | 1.9 | ||
| Non-Hispanic other | 5.4 | 5.1 | 3.5 | ||
| Hispanic | 3.1 | 1.7 | 3.1 | ||
| Missing | 0.0 | 0.0 | 0.0 | ||
| Region | Northeast | 8.5 | 6.8 | 9.7 | .010 |
| South | 36.2 | 37.6 | 42.5 | ||
| Midwest | 25.9 | 38.5 | 28.2 | ||
| West | 29.5 | 17.1 | 19.3 | ||
| Missing | 0.0 | 0.0 | 0.0 | ||
| Employment Status | Employed (full-time and part-time) | 89.5 | 88.9 | 82.2 | .002 |
| Homemaker | 4.1 | 0.9 | 4.6 | ||
| Student | 1.8 | 2.6 | 1.9 | ||
| Disabled | 0.0 | 0.0 | 0.8 | ||
| Retired | 1.3 | 4.3 | 8.1 | ||
| Unemployed | 3.1 | 2.8 | 1.9 | ||
| Missing | 0.3 | 0.9 | 0.4 | ||
| Marital Status | Single | 24.1 | 17.9 | 22.8 | .097 |
| Married | 60.0 | 63.2 | 64.9 | ||
| Domestic partner | 4.9 | 1.7 | 1.2 | ||
| Separated | 1.8 | 0.9 | 0.4 | ||
| Divorced | 6.9 | 12.0 | 6.9 | ||
| Widowed | 1.3 | 3.4 | 2.7 | ||
| Other | 1.0 | 0.9 | 0.8 | ||
| Missing | 0.0 | 0.0 | 0.4 | ||
| Education | Less than high school | 0.0 | 0.0 | 1.2 | .003 |
| Completed high school | 5.6 | 6.8 | 12.4 | ||
| Greater than high school | 94.4 | 93.2 | 86.5 | ||
| Missing | 0.0 | 0.0 | 0.0 | ||
| Household Income | <$25 000 | 3.3 | 23.1 | 5.0 | .229 |
| $25 000-$49 999 | 14.9 | 23.1 | 17.4 | ||
| $50 000-$74 999 | 22.6 | 22.2 | 25.1 | ||
| $75 000-$99 999 | 16.2 | 17.1 | 12.7 | ||
| ≥ $100 000 | 38.5 | 29.1 | 31.7 | ||
| Missing | 4.6 | 6.0 | 8.1 | ||
| Rurality | Rural | 19.0 | 30.8 | 24.0 | .021 |
| Urban | 81.0 | 69.2 | 76.0 | ||
| Missing | 0.0 | 0.0 | 0.0 | ||
| Physical Health | Poor | 1.0 | 0.0 | 0.0 | .490 |
| Fair | 7.4 | 11.1 | 9.7 | ||
| Good | 36.7 | 38.5 | 37.5 | ||
| Very good | 39.5 | 35.0 | 40.5 | ||
| Excellent | 15.4 | 15.4 | 12.4 | ||
| Missing | 0.0 | 0.0 | 0.0 | ||
| Mental Health | Poor | 2.1 | 1.7 | 1.9 | .383 |
| Fair | 10.0 | 6.8 | 11.2 | ||
| Good | 28.7 | 37.6 | 29.0 | ||
| Very good | 39.5 | 34.2 | 32.8 | ||
| Excellent | 19.7 | 19.7 | 25.1 | ||
| Missing | 0.0 | 0.0 | 0.0 | ||
| Adults in Household | 1 | 25.6 | 26.5 | 25.1 | .887 |
| 2 | 57.2 | 59.8 | 58.3 | ||
| 3 | 12.8 | 10.3 | 10.8 | ||
| 4 | 4.1 | 2.6 | 4.2 | ||
| 5 | 0.3 | 0.9 | 1.2 | ||
| Missing | 0.0 | 0.0 | 0.4 | ||
| Children in Household | 0 | 59.0 | 63.2 | 52.9 | .769 |
| 1 | 16.4 | 15.4 | 19.7 | ||
| 2 | 16.4 | 14.5 | 18.1 | ||
| 3 | 4.9 | 5.1 | 5.0 | ||
| 4 | 3.3 | 1.7 | 3.9 | ||
| Missing | 0.0 | 0.0 | 0.4 | ||
| Languages Spoken at Home | English | 98.5 | 97.4 | 98.5 | .952 |
| Spanish | 0.5 | 0.9 | 0.8 | ||
| Other | 0.8 | 0.9 | 0.4 | ||
| Missing | 0.3 | 0.9 | 0.4 | ||
Total N = 794, data missing for n = 28.
aMissing data for n = 15.
bMissing data for n = 4.
cMissing data for n = 8.
RUs were most likely to be employed, have post–high school education, and live in urban areas. Household characteristics were similar across the 3 groups (Table 1). We found that people across the age spectrum are using telehealth with 2 of every 5 users being 45 years of age or older. Compared with both nonuser groups, RUs were more likely to use smartphones, home computers, and work computers and to have Internet access and use e-mail, social media, and video calls (Table 2).
Table 2.
Use of technology and internet access methods, by user group
| User Group |
|||||
|---|---|---|---|---|---|
| Registered User |
Registered Nonuser |
Nonregistered Nonuser |
|||
| n = 390/406a | n = 117/121b | N = 259/267c | |||
| Characteristics | % | % | % | P Value | |
| Use of Technology | |||||
| Has Internet Access | Never | 0.0 | 0.9 | 0.0 | .001 |
| Occasionally | 1.8 | 7.7 | 6.6 | ||
| Frequently | 98.2 | 91.5 | 93.4 | ||
| Missing | 0.0 | 0.0 | 0.0 | ||
| Uses email | Never | 0.3 | 0.9 | 1.2 | .009 |
| Occasionally | 3.6 | 6.0 | 10.0 | ||
| Frequently | 96.2 | 93.2 | 88.8 | ||
| Missing | 0.0 | 0.0 | 0.0 | ||
| Uses social media | Never | 7.4 | 13.7 | 8.9 | .013 |
| Occasionally | 16.2 | 22.2 | 24.3 | ||
| Frequently | 76.4 | 64.1 | 66.8 | ||
| Missing | 0.0 | 0.0 | 0.0 | ||
| Uses video calls | Never | 10.5 | 26.5 | 30.1 | <.001 |
| Occasionally | 56.9 | 47.9 | 49.4 | ||
| Frequently | 32.6 | 25.6 | 20.5 | ||
| Missing | 0.0 | 0.0 | 0.0 | ||
| Type of Internet Access | |||||
| Smartphone | Never | 1.3 | 5.1 | 3.1 | .007 |
| Occasionally | 7.7 | 9.4 | 14.3 | ||
| Frequently | 91.0 | 85.5 | 82.2 | ||
| Missing | 0.0 | 0.0 | 0.4 | ||
| Public Source | Never | 63.3 | 62.4 | 71.0 | .170 |
| Occasionally | 19.2 | 20.5 | 17.4 | ||
| Frequently | 17.4 | 17.1 | 11.2 | ||
| Missing | 0.0 | 0.0 | 0.4 | ||
| Family/Friend’s Computer | Never | 41.5 | 49.6 | 45.6 | 0.487 |
| Occasionally | 35.9 | 29.9 | 35.1 | ||
| Frequently | 22.6 | 20.5 | 18.9 | ||
| Missing | 0.0 | 0.0 | 0.4 | ||
| Home Computer | Never | 1.0 | 6.0 | 3.5 | .017 |
| Occasionally | 10.8 | 12.0 | 14.3 | ||
| Frequently | 88.2 | 82.1 | 82.2 | ||
| Missing | 0.0 | 0.0 | 0.0 | ||
| Work Computer | Never | 11.0 | 14.5 | 22.8 | <.001 |
| Occasionally | 12.6 | 18.8 | 15.4 | ||
| Frequently | 76.4 | 66.7 | 61.4 | ||
| Missing | 0.0 | 0.0 | 0.4 | ||
Total N = 794, data missing for n = 28.
aMissing data for n = 15.
bMissing data for n = 4.
cMissing data for n = 8.
RUs were the least likely (65.6% compared with 78.6% for RNUs and 80% for NRNUs) to have a primary care USC, a historical mediator of access,5 and to have visited primary care during their last in-person visit (Table 3). Most users conducted 1 LHO visit (Table 4), although 36.6% had 2 or more visits. While 90% of users reported that they chose LHO for their most recent doctor visit because the online visit was more convenient for them, nearly half reported that they could not see their doctor that day either because of a lack of appointments or a closed office (Table 4). Nearly 14% said that they sought the privacy of an online video visit, while only 6% said that they chose the video visit because of transportation issues. More than 95% indicated that the video visit saved them time compared with an in-person visit. Most commonly users indicated that they saved 2 hours by using the video visit (46%), although 20% indicated that they saved 3 or more hours. Nearly 73% reported that they would have seen an in-person provider if they did not complete the video visit, indicating that telehealth video visits are often a substitute for in-person visits.
Table 3.
Care seeking behavior, by user group
| User Group |
|||||
|---|---|---|---|---|---|
| Registered User |
Registered Nonuser |
Nonregistered Nonuser |
|||
| n = 390/406a | n = 117/121b | n = 259/267c | |||
| % | % | % | P Value | ||
| Usual Source of Care | Primary Care | 65.6 | 78.6 | 80.0 | <.001 |
| Other | 34.4 | 21.4 | 15.4 | ||
| Missing | 0.0 | 0.0 | 4.6 | ||
| Last In-Person Visit | Primary Care | 57.9 | 64.1 | 76.8 | <.001 |
| Other | 42.1 | 35.9 | 23.2 | ||
| Missing | 0.0 | 0.0 | 0.0 | ||
Note: Other includes specialist, urgent care, emergency department, retail clinic, online doctor, other, or no usual source of care.
Total N = 794, missing data missing for n = 28.
aMissing data for n = 15.
bMissing data for n = 4.
cMissing data for n = 8.
Table 4.
Use of and attitudes toward telehealth, among users
| Number of LiveHealth Online visits in the past 12 months | % | |
| 0 times | 6.4 | |
| 1 time | 56.9 | |
| 2 times | 25.6 | |
| 3 or more times | 11.0 | |
| Missing | 0.0 | |
| Reasons for using telehealth for the most recent telehealth visit | ||
| The online video visit was more convenient for me | 90.6 | |
| I could not get an appointment to see my doctor that day | 46.8 | |
| I chose not to travel to a doctor’s office, urgent care center or emergency department because of my symptoms | 41.8 | |
| My doctor’s office was closed | 34.8 | |
| I was at work and could not leave | 17.5 | |
| I wanted the privacy of an online video visit | 13.7 | |
| I don’t have a doctor | 12.4 | |
| I had caregiving duties and could not leave | 8.6 | |
| I chose not to travel to a doctor’s office, urgent care center or emergency department because of transportation issues | 6.2 | |
| My doctor told me to use LiveHealth Online | 0.5 | |
| Missing | 0.0 | |
| Do you feel that visiting with a doctor using the video visit saved you time versus an in-person visit? | ||
| Yes | 95.7 | |
| No | 4.3 | |
| Missing | 0.0 | |
| How much time do you feel the video visit saved you versus an in-person visit? | ||
| <1 h | 7.6 | |
| 1 h | 25.7 | |
| 2 h | 46.1 | |
| 3 h | 14.9 | |
| 4 h or more | 5.8 | |
| Missing | 0.0 | |
| If you did not have the video visit, what would you have done? | ||
| Nothing, I would have waited to see if my symptoms improved | 14.3 | |
| Sent an electronic message to my primary care provider | 2.0 | |
| Called my primary care provider | 10.8 | |
| Gone to see my primary care provider | 27.8 | |
| Gone to an urgent care center | 43.1 | |
| Gone to an emergency department | 2.0 | |
| Missing | 0.0 | |
Total N = 406, data missing for n = 16.
DISCUSSION
In this innovative survey, we found that telehealth is an important mediator of access for acute conditions and we gained insight into why people choose video visits. On the patient side, users were less likely to have a primary care USC, indicating a preference for access over continuity. This decision was influenced by in-person availability, with nearly half of users reporting that they could not secure a same day appointment with their doctor and over a third reporting that their doctor’s office was closed.
While we are the first to examine the relationship between telehealth use and having a primary care USC, our other findings are consistent with the existing literature. For example, patients receiving a telemedicine intervention for postoperative visits similarly reported that the video visits saved time.24 Another study found that video visits frequently took place over weekends and holidays, when practices are typically closed.30 By comparison, new patients wait an average of 24 days to see a doctor in-person, spending 2 hours for the encounter and round-trip travel.31–33 Taken together, these findings support the conclusion that users of telehealth are attracted to its convenience.17,18
Our findings also highlight telehealth’s uneven adoption. Within this sample, we found that users were more likely to be educated, employed, and urban based. Not surprisingly, these users possessed the precursors of adoption—Internet access, devices, and technological competence. These findings highlight an inherent challenge in the diffusion of any innovation: ensuring that the new technology is available to those most likely to benefit rather than to only those with resources. As adoption increases, these trends will need to be monitored.
Policymakers have indicated that one barrier to more widespread telehealth adoption is its uncertain impact on cost.34 On average, Medicare beneficiaries already see 7 physicians at 4 different practices, leading to duplicate services, conflicting advice, and ultimately inefficiently delivered care.35,36 To enhance access without sacrificing coordination, telehealth will need to share information with primary care and vice versa. Without adequate sharing, errors can occur, and critical information will not be communicated to others. The benefits of the improved access afforded by telehealth risk being tempered by an increase in fragmentation. While many telehealth companies are identifying ways to integrate virtual care with electronic health records, more can be done to enhance data continuity.37–39
To reduce costs, telehealth may need to focus on those that are responsible for the majority of healthcare spending and better integrate with primary care.40 Even though most live video visits are for acute illnesses,25,30 telehealth is increasingly being used for chronic conditions.15,19,41 Primary care physicians are already managing these complex, multimorbid patients, many of whom require frequent visits and have limited physical mobility.42–44 An innovation worthy of further investigation is telehealth as an integrated part of primary care practice for both acute and chronic conditions. Telehealth is potentially an important method for primary care patients to obtain care and for care teams to receive updates. Using technology to broaden access is one of the joint principles of the patient-centered medical home.45 Live video visits are an ideal way to move the patient-centered medical home into the homes of all patients, though our previous work shows this model remains the exception.8,32,46 While our study demonstrates telehealth’s impact on the delivery of timely care, we were unable to assess the remaining dimensions of quality, including safety, effectiveness, patient-centeredness, efficiency, and equity.47 Telehealth can theoretically improve these domains, though additional studies are needed to clarify its impact.
Limitations
There are limitations to consider when interpreting our findings, beginning with their generalizability to broader populations. Our survey respondents were commercially insured adults, 18 years or older; thus, our sample included few respondents over 65 years of age and did not include children. Nonrespondents were more likely than respondents to be women and reside in the Midwest (Supplementary Tables S3 and S4). Among nonusers, respondents tended to have higher DCI comorbidity scores than nonrespondents did. Compared with national figures, our sample was younger and more likely to be a woman, white, and have greater than a high school education.48 Furthermore, we restricted the sample to those with a diagnosis of the top 20 diagnosis codes to create cohorts with similar care-seeking and illness patterns; thus, the generalizability of our results is limited to the population that accesses the healthcare system each year. Second, as with any survey, these results are subject to recall bias. Third, although we attempted to recruit the same number of people for the 2 nonuser groups, we were unable to recruit an adequate number of RNUs as they were difficult to identify from the available data. We compensated by recruiting enough NRNUs to ensure nonusers comprised half of our overall sample. This modification has implications for our findings. For example, RNUs had a higher prevalence across each of the 10 chronic conditions, except for asthma, compared with NRNUs (Supplementary Table S2). Given this difference in morbidity, our results may have differed if we were able to recruit additional RNUs. Finally, many of the differences in demographic characteristics across the groups were not statistically significant, potentially due to the small sample sizes and low power.
CONCLUSION
In summary, we found that users of live video visits were educated, employed, and largely urban based. Compared with nonusers, they were less likely to have a primary care USC, and many unsuccessfully sought to obtain in-person care. Both telehealth and primary care would benefit from tighter integration, though substantial barriers remain and few successful models exist.
FUNDING
This work was supported by Robert Wood Johnson Foundation grant no. 73058.
AUTHOR CONTRIBUTORS
All authors were responsible for study conception and design. AJ, SP, MM, GS, AG, and JJS were responsible for data acquisition. All were responsible for analysis and interpretation of results. All were responsible for drafting and revising the manuscript. All were responsible for final approval.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Conflict of interest statement. GS, AG, and JJS are employed by HealthCore, a wholly owned subsidiary of Anthem, Inc. WA is employed by LiveHealth Online.
Supplementary Material
REFERENCES
- 1. Pandhi N, Schumacher JR, Thorpe CT et al. Cross-sectional study examining whether the extent of first-contact access to primary care differentially benefits those with certain personalities to receive preventive services. BMJ Open 2016; 6 (3): e009738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Starfield B. Primary Care: Balancing Health Needs, Services, and Technology. New York City, NY: Oxford University Press; 1998. [Google Scholar]
- 3. Corbie-Smith G, Flagg EW, Doyle JP et al. Influence of usual source of care on differences by race/ethnicity in receipt of preventive services. J Gen Intern Med 2002; 17 (6): 458–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kim MY, Kim JH, Choi IK et al. Effects of having usual source of care on preventive services and chronic disease control: a systematic review. Korean J Fam Med 2012; 33 (6): 336–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. DeVoe JE, Tillotson CJ, Lesko SE et al. The case for synergy between a usual source of care and health insurance coverage. J Gen Intern Med 2011; 26 (9): 1059–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Weinick RM, Zuekas SH, Drilea S. Research Findings #3: access to health care—sources and barriers, 1996. 2006. https://meps.ahrq.gov/data_files/publications/rf3/rf3.shtml Accessed November 3, 2017.
- 7. American Telemedicine Association. Telemedicine glossary. http://thesource.americantelemed.org/resources/telemedicine-glossary Accessed November 1, 2017.
- 8. Moore MA, Coffman M, Jetty A et al. Family physicians report considerable interest in, but limited use of, telehealth services. J Am Board Fam Med 2017; 30 (3): 320–30. [DOI] [PubMed] [Google Scholar]
- 9. The Healthcare Information and Management Systems Society (HIMSS). 2016 Telemedicine Study. 2016. http://www.himssanalytics.org/research/essentials-brief-telemedicine-study Accessed November 3, 2017.
- 10. Advisory Board. A milestone: Kaiser now interacts more with patients virtually than in-person. 2016. https://www.advisory.com/daily-briefing/2016/10/13/kaiser-telehealth Accessed November 1, 2017.
- 11. Polinski JM, Barker T, Gagliano N et al. Patients’ satisfaction with and preference for telehealth visits. J Gen Intern Med 2016; 31 (3): 269–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lilholt PH, Heiden S, Hejlesen OK. User satisfaction and experience with a telehealth system for the Danish TeleCare North trial: a think-aloud study. Stud Health Techology Inform 2014; 205: 900–4. [PubMed] [Google Scholar]
- 13. Livingstone J, Solomon J. An assessment of the cost-effectiveness, safety of referral and patient satisfaction of a general practice teledermatology service. Lond J Prim Care 2015; 7 (2): 31–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lee T-T, Huang T-Y, Chang C-P et al. The evaluation of diabetic patients’ use of a telehealth program. CIN Comput Inform Nurs 2014; 32 (12): 569–77. [DOI] [PubMed] [Google Scholar]
- 15. Odeh B, Kayyali R, Nabhani-Gebara S et al. Evaluation of a telehealth service for COPD and HF patients: clinical outcome and patients’ perceptions. J Telemed Telecare 2015; 21 (5): 292–7. [DOI] [PubMed] [Google Scholar]
- 16. Jenkins-Guarnieri MA, Pruitt LD, Luxton DD et al. Patient perceptions of telemental health: systematic review of direct comparisons to in-person psychotherapeutic treatments. Telemed J E Health 2015; 21 (8): 652–60. [DOI] [PubMed] [Google Scholar]
- 17. McIntosh S, Cirillo D, Wood N et al. Patient evaluation of an acute care pediatric telemedicine service in urban neighborhoods. Telemed J E Health 2014; 20 (12): 1121–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Robinson M, Branham A, Locklear A et al. Measuring satisfaction and usability of facetime for virtual visits in patients with uncontrolled diabetes. Telemed J E Health 2016; 22 (2): 138–43. [DOI] [PubMed] [Google Scholar]
- 19. Fatehi F, Martin-Khan M, Smith AC et al. Patient satisfaction with video teleconsultation in a virtual diabetes outreach clinic. Diabetes Technol Ther 2015; 17 (1): 43–8. [DOI] [PubMed] [Google Scholar]
- 20. Young LB, Foster L, Silander A et al. Home telehealth: patient satisfaction, program functions, and challenges for the care coordinator. J Gerontol Nurs 2011; 37 (11): 38–46. [DOI] [PubMed] [Google Scholar]
- 21. López C, Valenzuela JI, Calderón JE et al. A telephone survey of patient satisfaction with realtime telemedicine in a rural community in Colombia. J Telemed Telecare 2011; 17 (2): 83–7. [DOI] [PubMed] [Google Scholar]
- 22. McCrossan BA, Sands AJ, Kileen T et al. A fetal telecardiology service: patient preference and socio-economic factors: A fetal telecardiology service: patient preference and socio-economic factors. Prenat Diagn 2012; 32(9): 883–7. doi:10.1002/pd.3926. [DOI] [PubMed] [Google Scholar]
- 23. Marquis N, Larivée P, Saey D et al. In-home pulmonary telerehabilitation for patients with chronic obstructive pulmonary disease: a pre-experimental study on effectiveness, satisfaction, and adherence. Telemed J E Health 2015; 21 (11): 870–9. [DOI] [PubMed] [Google Scholar]
- 24. Stypulkowski K, Uppaluri S, Waisbren S. Telemedicine for postoperative visits at the Minneapolis VA Medical Center. Minn Med 2015; 98 (2): 34–6. [PubMed] [Google Scholar]
- 25. Gordon AS, Adamson WC, DeVries AR. Virtual visits for acute, nonurgent care: a claims analysis of episode-level utilization. J Med Internet Res 2017; 19 (2): e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ashwood JS, Mehrotra A, Cowling D et al. Direct-to-consumer telehealth may increase access to care but does not decrease spending. Health Aff (Millwood) 2017; 36 (3): 485–91. [DOI] [PubMed] [Google Scholar]
- 27. Bauer UE, Briss PA, Goodman RA et al. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. Lancet 2014; 384 (9937): 45–52. [DOI] [PubMed] [Google Scholar]
- 28. Bakken S, Grullon-Figueroa L, Izquierdo R et al. Development, validation, and use of English and Spanish Versions of the telemedicine satisfaction and usefulness questionnaire. J Am Med Inform Assoc 2006; 13 (6): 660–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Stephenson JJ, Raval AD, Kern DM et al. Non-adherence to basal insulin among patients with type 2 diabetes in a US managed care population: results from a patient survey. Diabetes Obes Metab 2018; 20 (11): 2700–4. [DOI] [PubMed] [Google Scholar]
- 30. Uscher-Pines L, Mehrotra A. Analysis of teladoc use seems to indicate expanded access to care for patients without prior connection to a provider. Health Aff (Millwood) 2014; 33 (2): 258–64. [DOI] [PubMed] [Google Scholar]
- 31. Ray KN, Chari AV, Engberg J et al. Disparities in time spent seeking medical care in the United States. JAMA Intern Med 2015; 175 (12): 1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dorsey ER, Topol EJ. State of telehealth. N Engl J Med 2016; 375 (2): 154–61. [DOI] [PubMed] [Google Scholar]
- 33. Merritt Hawkins. Survey of physician appointment wait times. 2017. https://www.merritthawkins.com/news-and-insights/thought-leadership/survey/survey-of-physician-appointment-wait-times/ Accessed November 3, 2017.
- 34. U.S. Senate Committee on Finance. Bipartisan chronic care working group policy options document. 2015. https://www.finance.senate.gov/download/ccwg-policy-options-paper Accessed November 3, 2017. [Google Scholar]
- 35. Pham HH, O’Malley AS, Bach PB et al. Primary care physicians’ links to other physicians through medicare patients: the scope of care coordination. Ann Intern Med 2009; 150 (4): 236–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Institute of Medicine, Comittee on the Learning Health Care System in America, Smith M, Saunders R, Stuckhardt L, McGinnis JM, eds. Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, DC: National Academies Press; 2012. [PubMed] [Google Scholar]
- 37. Office of the National Coordinator. Connecting health and care for the nation: a shared nationwide interoperability roadmap. 2015. https://www.healthit.gov/sites/default/files/hie-interoperability/nationwide-interoperability-roadmap-final-version-1.0.pdf Accessed November 2, 2017.
- 38. American Hospital Association. Achieving interoperability that supports care transformation. 2015. https://www.aha.org/guidesreports/2015-07-19-achieving-interoperability-supports-care-transformation Accessed November 2, 2017. [Google Scholar]
- 39. Healthcare IT. News. Comparing 11 top telehealth platforms: company execs tout quality, safety, EHR integrations. Healthc. IT News. 2017. http://www.healthcareitnews.com/news/comparing-11-top-telehealth-platforms-company-execs-tout-quality-safety-ehr-integrations Accessed November 2, 2017.
- 40. Stanton MW, Rutherford MK. The high concentration of US health care expenditures. agency for healthcare research and quality 2005. https://meps.ahrq.gov/data_files/publications/ra19/ra19.pdf Accessed November 3, 2017. [Google Scholar]
- 41. Osenbach JE, O’Brien KM, Mishkind M et al. Synchronous telehealth technologies in psychotherapy for depression: a meta-analysis. Depress Anxiety 2013; 30 (11): 1058–67. [DOI] [PubMed] [Google Scholar]
- 42. Moore M, Gibbons C, Cheng N et al. Complexity of ambulatory care visits of patients with diabetes as reflected by diagnoses per visit. Prim Care Diabetes 2016; 10 (4): 281–6. doi:10.1016/j.pcd.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 43. Bernard D, Selden T, Yeh S. Financial burdens and barriers to care among nonelderly adults: the role of functional limitations and chronic conditions. Disabil Health J 2016; 9 (2): 256–64. [DOI] [PubMed] [Google Scholar]
- 44. Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health 2013; 38 (5): 976–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Patient-Centered Primary Care Collaborative. Joint Principles of the Patient-Centered Medical Home. 2007. https://www.pcpcc.org/about/medical-home Accessed November 3, 2017. [Google Scholar]
- 46. Herendeen N, Deshpande P. Telemedicine and the patient-centered medical home. Pediatr Ann 2014; 43 (2): e28–32. [DOI] [PubMed] [Google Scholar]
- 47. Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 48. U.S. Census Bureau. U.S. Census Bureau Quick Facts. 2017. https://www.census.gov/quickfacts/fact/table/US/PST045217 Accessed November 5, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.