The Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-Covid-19) pandemic has made the healthcare systems world-wide concentrated on the caring of patients with the infection [1]. However, this has raised questions how to offer the best treatment and care for patients with non-Covid disease [1]. Especially the prognosis for pulmonary embolism (PE) is determined by early diagnostics and proper treatment interventions [2]. On the evening of the 11th of March 2020, the prime minister of Denmark announced the closing of the country's borders, sent all public employees without a critical function home, and urged all private companies to do the same. All non-acute operations and ambulatory appointments were cancelled in an attempt to mitigate the risk that the health care system would be overburdened due to SARS-Covid-19 patients, while general practitioners restricted in-person consultations. In addition, government communication and media reporting discouraged Danes from taking up healthcare resources with (health) issues that could wait until the impending crisis was over. Even though patients might not be contacting the health care system with symptoms, it does not necessarily mean that the symptoms are not present, and will materialize at a later date, perhaps escalating to a more serious degree or postponed to a point where it increases mortality. Government restrictions could have had both a positive and negative impact on the incidence of PE admissions. We therefore sought to investigate the impact of the Danish lockdown on incidence of PE admissions and subsequently risk of mortality.
This study was a retrospective cohort study in which a number of national Danish registries were used [3]. The Danish population was included in the period 1st of January 2018 to 11th of May 2020. To assess the change in incidence of PE admissions before and after the Danish lockdown (week 11), three cohorts were constructed – one for the 18 weeks period starting from the second calendar week every year; 2018 (8th of January), 2019 (7th of January), and 2020 (6th of January). For the three cohorts, the residents were followed until the end of calendar week 19 of the respective year (2018: 14th of May 2019: 13th of May, and 2020: 11th of May), death, or an admission with PE, whichever came first. Each cohort only included residents that were alive and above the age of 18 years on the respective inclusion dates in January of that given year and had no history of pulmonary embolism. When comparing the weeks of 2020 with previous years, 2018 and 2019 were combined (supplementary data shows the analyses when the years are not combined). Crude incidence rates were calculated as number of admissions pr. 1000 person years along with exact Poisson confidence intervals. To investigate the risk of 5-day all-cause mortality following a PE, based on cause-specific Cox regression analyses (adjusted for; sex, age, comorbidities, and use of concomitant medication), it was possible to estimate the directly standardized differences in absolute 5-days risks of all-cause mortality during each week [4].
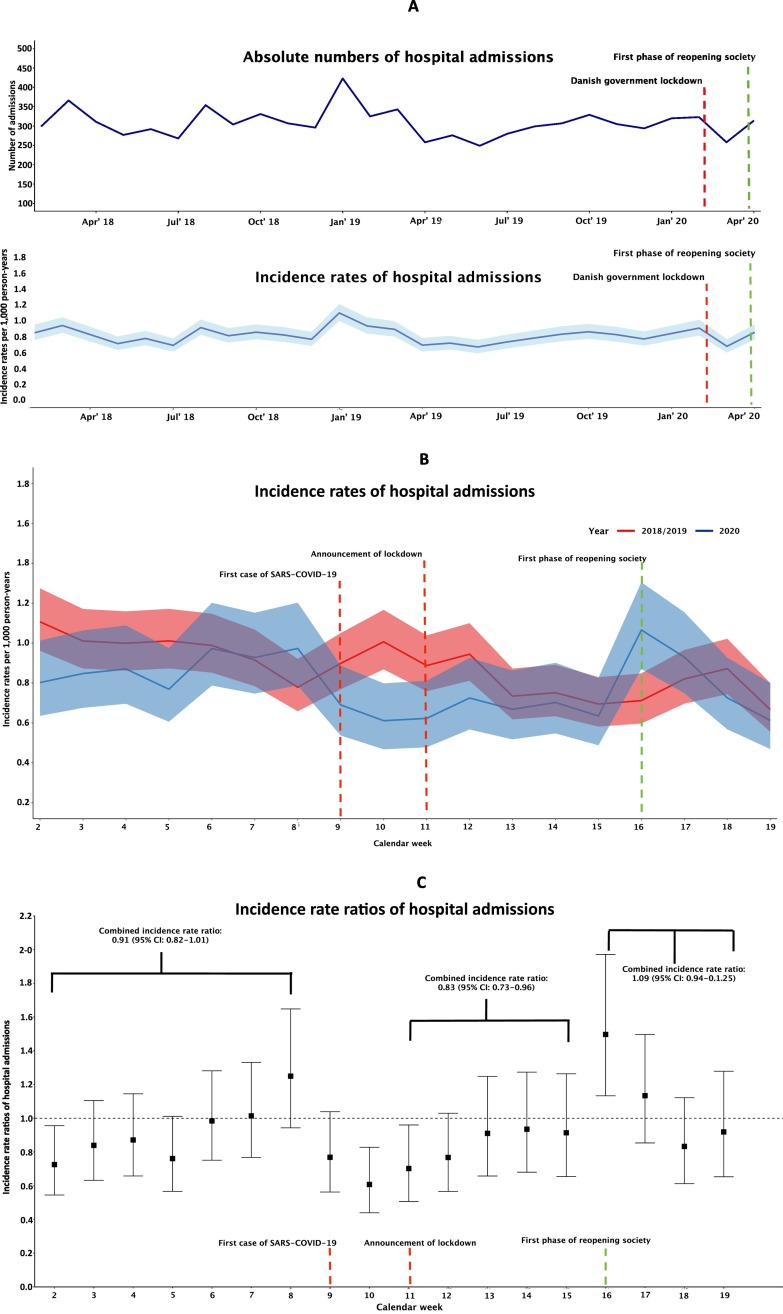
Time trends in incidence of PE admissions are illustrated in Fig. 1A. In the period between 1st of January 2018 and 11th of May 2020, a total number of 4,590,644 Danish residents were identified, with 8212 first-time hospital admissions with PE (incidence rate of 0.80 (95% CI; 0.78–0.82) pr. 1000 person years). Time trends for the periods January to April in 2018/2019 and 2020 are shown in Fig. 1B.
Fig. 1.
(A) Monthly absolute numbers and incidence rates of hospital admissions with PE between 1st of January 2018 and 11th of May 2020. (B) Weekly incidence rates of hospital admissions with PE in the periods of 2nd calendar week up to and including calendar week 19th for the years of 2018/2019, and 2020. (C) Weekly incidence rate ratios for the time periods of 2nd calendar week up to and including calendar week 19th for the years of 2018/2019, and 2020. Years of 2018/2019 are the reference.
A total number of 2778 and 1250 hospital admissions with a PE were observed from the 2nd calendar week to week 19 in 2018/2019 (2018: n = 1400, 2019; n = 1378) and 2020, respectively). The median age was 72 (IQR: 62–80) years for patients in all time periods (Table 1 ), with approximately 50% being male. There were no significant differences in comorbidities or concomitant medication across the years.
Table 1.
Baseline table.
| Cohort 2020 (n = 1250) |
Cohort 2018/2019 (n = 2778) |
Total (n = 4028) |
|
|---|---|---|---|
| Demographics | |||
| Sex (male) | 645 (51.6) | 1396 (50.3) | 2041 (50.7) |
| Age (median [IQR]) | 72 [61, 80] | 72 [62, 80] | 72 [62, 80] |
| Comedication at baseline | |||
| OAC | 83 (6.6) | 216 (7.8) | 299 (7.4) |
| Antiplatelets | 237 (19.0) | 538 (19.4) | 775 (19.2) |
| Non sterodial antiinflammatory drugs | 265 (21.2) | 544 (19.6) | 809 (20.1) |
| Antiadrenergic | 385 (30.8) | 937 (33.7) | 1322 (32.8) |
| Beta-blockers | 222 (17.8) | 636 (22.9) | 858 (21.3) |
| Calcium channel blockers | 298 (23.8) | 703 (25.3) | 1001 (24.9) |
| Renin angiotensin inhibitors | 83 (6.6) | 216 (7.8) | 299 (7.4) |
| Diuretics | 97 (7.8) | 229 (8.2) | 326 (8.1) |
| Statins | 199 (15.9) | 441 (15.9) | 640 (15.9) |
| Comorbidity | |||
| Hypertension | 344 (27.5) | 843 (30.3) | 1187 (29.5) |
| Cancer | 332 (26.6) | 804 (28.9) | 1136 (28.2) |
| Coagulopathies | 13 (1.0) | 48 (1.7) | 61 (1.5) |
| Chronic obstructive pulmonary disease | 181 (14.5) | 473 (17.0) | 654 (16.2) |
| Stroke | 106 (8.5) | 245 (8.8) | 351 (8.7) |
| Acute myocardial infarction | 51 (4.1) | 107 (3.9) | 158 (3.9) |
| Ischemic heart disease | 140 (11.2) | 351 (12.6) | 491 (12.2) |
| Peripheral artery disease | 24 (1.9) | 62 (2.2) | 86 (2.1) |
| Vascular disease | 153 (12.2) | 389 (14.0) | 542 (13.5) |
| Heart failure | 100 (8.0) | 247 (8.9) | 347 (8.6) |
| Chronic kidney disease | 51 (4.1) | 179 (6.4) | 230 (5.7) |
| Liver disease | 27 (2.2) | 86 (3.1) | 113 (2.8) |
It was observed that the crude incidence rates of PE admissions began to decline in the week (calendar week 10) before the announcement of the government lockdown in 2020 compared with the same calendar weeks in 2018/2019 (incidence rate ratio, 0.61, 95% CI: 0.44–0.83) (Fig. 1C). The combined incidence rate ratios for the five weeks (calendar week 11 (lockdown) to week 15 (first phase of the reopening of the society was announced)) showed a significant decline of 17% in the incidence rates for 2020 compared with 2018/2019 (incidence rate ratio; 0.83 (95% CI: 0.73–0.96)). In the weeks following the first phase of reopening there was no significant difference in the incidence of PE compared with 2018/2019 (incidence rate ratio; 1.05 (95% CI: 0.92–1.20)). The standardized absolute risk of 5-day mortality was 2.5% (95% CI: 1.9% to 3.2%) for 2018/2019 and 2.4% (95% CI: 1.0% to 3.1%) in 2020, absolute risk difference 0.4% (95% CI: −0.3% to 1.0%).
The significant decline in hospital admissions in March 2020 compared with the preceding years is likely due to several factors. Firstly, many elective procedures were cancelled. Major orthopedic surgery and general surgery is well known to increase the risk of developing venous thromboembolism, e.g. elective hip and knee alloplastic surgery increases the risk [5,6]. Secondly, fewer patients generally contacted the healthcare system because the mitigation strategy from authorities made patients hesitant to seek help in the fear that they would be contributing to an impending collapse of the health care system [7,8]. Thirdly; it is possible that the decline in the incidence of PE admissions were due to the fact that some patients died without proper diagnostics. Nopp et al. found a significant decline in imaging tests performed in an Austrian hospital, which would lead to fewer PEs being detected [7]. However it is not possible in our study to differentiate between whether it was a decrease in diagnostics or a decrease in the disease. Likewise, it was not possible to investigate the number of patients that died from a PE without diagnostics, because the register for causes of death has not been updated with data for 2020.
The incidence of PE seemed to decrease already from week 10, which was the week before the government lockdown, which is explained by the government restrictions regarding the hospitals were already being implemented. Reports from the Danish Health care authorities have shown that the number of hospital admissions (referrals and acute admissions), along with the number of surgeries began to already decline from calendar week 9. During the lock down, in the end of March, news reports came out describing that the hospitals were observing a significant decline in hospital contacts regarding different cardiovascular diseases, which led to many patient organizations urging patients to still contact the healthcare system if they had serious symptoms of disease. This might have mitigated some of the adverse reactions that could have led to an even further decline in the incidence rates. Similar declines in hospital admissions have been seen elsewhere and also for a number of different cardiovascular diseases [[7], [8], [9]]. Specifically for PE a 66% decline in diagnoses during lock down was observed in Austria [7]. Some limitations apply to this study; which includes the lack of data for surgery, fractures, and causes of death. Another limitation is the potential for residual confounding as potential confounders are not available in the dataset such as information on INR, kidney function, liver function, and body weight. Especially the interpretation of the absolute risk relies on an assumption of no unmeasured confounders.
One of the trade-offs during the pandemic has been that between the need to protect caregivers from being exposed to infection and patients' need for procedures and treatment interventions. An important aspect of the diagnostics of PE in relation to SARS-Covid-19, is that both diseases share some overlapping symptoms such as dyspnea. This means that patients with certain symptoms will be suspected of having SARS-Covid-19, and while investigation and diagnostics of this are being performed, the actual cause of symptoms, PE, goes untreated [7]. Thus, it is reassuring that there were no significant differences in mortality between the time periods, because this indicates that the patients that contacted the hospital are receiving the proper diagnostics and treatment interventions.
However, while the consequences for patients suffering from PEs can be dire, many patients suffering from many different diseases are likely to be affected. The SARS-Covid-19 pandemic continues to pose problems for health care systems worldwide, which have finite resources battling a growing demand for their services. There is a general risk that postponement of treatments could have serious, unintended consequences for patients in the long term, for example higher mortality, as well as economic and logistical consequences for the healthcare system and workers, such as the accruement of a large backlog of treatments. These treatments need to be expedited in the wake of the pandemic, where the healthcare systems have perhaps already been overworked. In short, the aftermath of the pandemic is likely to focus on who will pay for rebalancing of healthcare systems, that is, whether governments will have to pay more, healthcare workers will have to work more, or patients will have to lower their expectations of treatment standards and timelines. As such, the discourse in the coming time will be of high interest to all patients and their respective patient organizations. Future research on the subject should be able to supply sound and novel insights to inform these discussion and supply decision makers with the best possible foundation for prioritization of resources.
Ethics
The present study was approved by the data responsible institution, Capital Region. We refer to approval number P-2019-191. In Denmark, retrospective registry-based cohort studies do not require further approval from the Research Ethics Committee System.
CRediT authorship contribution statement
All authors contributed significantly to the conception and design of the study, acquisition of data or analysis and interpretation of the data. CSP, JBO, PB and GG designed the study. CSP, PB, TAG analyzed the data. CSP, PB, JES, MEC produced the Figures. CSP, JBO, PB, TAG, MP, MLH, JHB, JES, MEC, MS, LK, ELF, CTP, GG interpreted the results, CSP, JBO, PB, TAG, MP, MLH, JHB, JES, MEC, MS, LK, ELF, CTP, GG drafted the manuscript. All authors critically reviewed, revised, and approved the final manuscript.
Declaration of competing interest
CSP: None, JBO: None, PB: None, TAG: None, MP: None, MLH None, JHB: None, JES: None, MEC: None, MS: None, LK None, ELF: None, CTP reports grants from Bayer, grants from Novo Nordisk, outside the submitted work, GG: None.
Acknowledgments
Acknowledgement
This study was supported by an unrestricted grant from Læge Sophus Carl Emil Friis og hustru Olga Doris Friis' Legat. The sponsor had no influence on the study design, interpretation of results, or the decision to submit the manuscript for publication.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.thromres.2020.12.025.
Appendix A. Supplementary data
Supplementary material
References
- 1.Rosenbaum L. The untold toll — the pandemic's effects on patients without Covid-19. N. Engl. J. Med. 2020;382:2368–2371. doi: 10.1056/NEJMms2009984. [DOI] [PubMed] [Google Scholar]
- 2.Sindet-Pedersen C., Staerk L., Pallisgaard J.L., et al. Safety and effectiveness of rivaroxaban and apixaban in patients with venous thromboembolism: a nationwide study. Eur. Heart J. Cardiovasc. Pharmacother. 2018;4:220–227. doi: 10.1093/ehjcvp/pvy021. [DOI] [PubMed] [Google Scholar]
- 3.Thygesen L.C., Daasnes C., Thaulow I., Bronnum-Hansen H. Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scandinavian Journal of Public Health. 2011;39:12–16. doi: 10.1177/1403494811399956. [DOI] [PubMed] [Google Scholar]
- 4.Ozenne B.M.H., Scheike T.H., Staerk L., Gerds T.A. On the estimation of average treatment effects with right-censored time to event outcome and competing risks. Biom. J. 2020;62:751–763. doi: 10.1002/bimj.201800298. [DOI] [PubMed] [Google Scholar]
- 5.Goldhaber S.Z., Bounameaux H. Pulmonary embolism and deep vein thrombosis. Lancet. 2012;379:1835–1846. doi: 10.1016/S0140-6736(11)61904-1. [DOI] [PubMed] [Google Scholar]
- 6.Goldhaber S.Z. Pulmonary embolism. Lancet. 2004;363:1295–1305. doi: 10.1016/S0140-6736(04)16004-2. [DOI] [PubMed] [Google Scholar]
- 7.Nopp S., Janata-Schwatczek K., Prosch H., et al. Pulmonary embolism during the COVID-19 pandemic: decline in diagnostic procedures and incidence at a university hospital. Research and Practice in Thrombosis and Haemostasis. 2020;4:835–841. doi: 10.1002/rth2.12391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Butt J.H., Fosbøl E.L., Østergaard L., et al. Effect of COVID-19 on first-time acute stroke and transient ischemic attack admission rates and prognosis in Denmark. Circulation. 2020;142:1227–1229. doi: 10.1161/CIRCULATIONAHA.120.050173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Metzler B., Siostrzonek P., Binder R.K., Bauer A., Reinstadler S.J. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur. Heart J. 2020;41:1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material