Highlights
-
•
Early and aggressive resuscitation is the cornerstone of treating BCIS.
-
•
Fluid resuscitation to maintain preload and inotropes to support ventricular contractility are recommended.
-
•
Patients with comorbidities and risk factors should be monitored closely during and after bone cementation.
-
•
A good response time and high-quality cardiopulmonary resuscitation (CPR) also takes a major role in treating BCIS.
-
•
Good coordination among the operation team is needed escpecially for an arthroplasty surgery.
Keywords: Bone cement implantation syndrome (BCIS), Cardiac arrest, Cemented arthroplasty
Abstract
Introduction
Bone Cement Implantation Syndrome (BCIS) is a lethal condition with complex physiological changes after the insertion of Methyl Methacrylate (MMA) cement during intraoperative arthroplasty. Despite the etiology and the pathophysiology of BCIS has not been fully understood, several mechanisms have been discovered. Some clinical manifestations of BCIS are hypotension, hypoxemia, a decrease of consciousness, arrhythmia, pulmonary hypertension, and cardiac arrest.
Presentation of case
A 67 years old woman underwent cemented hemiarthroplasty operation due to intertrochanteric fracture in her right femur. The hemodynamic was stable before and during operation, but suddenly the patient went into cardiac arrest as the cement inserted. Immediate resuscitation was performed successfully and stable hemodynamic was achieved.
Discussion
Several risk factors including underlying cardiovascular disease, advanced age, osteoporosis (enlarged porous cavities increase the risk of emboli generation), fracture type, metastatic bone disease, femoral canal diameter of more than 21 mm, previously non-instrumented femoral canal, and patent foramen ovale (paradoxical embolus). Some studies have shown usage of H1 and H2 antagonists, methylprednisolone, inotropes, vasopressor, and some alterations in surgical technique, can prevent the progression of the BCIS. Communication between the orthopaedic surgeon and anesthesiologist and high-quality cardiopulmonary resuscitation (CPR) will become a good basis in treating BCIS.
Conclusion
Preoperative optimization by increasing oxygen inspiration concentration, usage of inotropes and vasopressor, and avoiding intravascular volume depletion during operation is essential in cemented arthroplasty procedure. Both orthopaedic surgeon and anesthesiologist should recognize the clinical presentation of BCIS and well-prepared for the management of BCIS including any supportive measures.
1. Introduction
The worldwide frequency of hip fractures was 1.6 million in 2000 and estimated to reach 6 million in 2050 [1]. The number of hemiarthroplasties or total hip replacement surgery is increasing concomitantly with patients’ age and severe comorbidities. For several reasons, orthopaedic surgeons prefer cemented hip arthroplasty mainly for older patients to reduce the re-operation rate due to aseptic loosening [2].
Bone cement implantation syndrome (BCIS) is a well-known and potentially fatal complication of orthopaedic surgery involving pressurized bone cement. This syndrome may occur in total hip and knee replacement surgery but frequently is seen in cemented hemiarthroplasty. It is characterized by hypoxia, sudden loss of arterial pressure, pulmonary hypertension, arrhythmias, loss of consciousness, and cardiac arrest [3].
Even though safety guidelines for the reduction of BCIS have been published, BCIS remains a frequent intraoperative complication with an overall incidence up to 28% [2]. In cemented total hip arthroplasty, the incidence of intraoperative death is 0.11% and usually occurs around the time of cementation. In a study including patients with and without hip fractures, the intraoperative mortality for cemented hemiarthroplasty is considerably higher (0.43%) [3].
Although not fully understood, the pathophysiology of BCIS is thought to involve several pathways, including anaphylaxis, pulmonary embolization, complement activation, and histamine release, combining to increase pulmonary vascular resistance, and potentially ventilation/perfusion mismatches with resultant acute hypoxia, right ventricular failure and cardiogenic shock [4].
Certain patient factors are associated with an increased risk of severe cardiovascular events during cemented hemiarthroplasty, in particular, increasing age, male sex, significant cardiopulmonary disease and use of diuretic medication. These factors are also associated with increased 30-day mortality, though the magnitude of the association is far greater for BCIS itself [5]. This study aims to point out that the communication between the orthopaedic surgeon and anesthesiologist and high-quality cardiopulmonary resuscitation (CPR) will become a good basis in treating BCIS.
2. Case report
Sixty-seven years old woman came to the ER with a chief complaint of pain in the right thigh after fell at the bathroom. Patient’s right thigh was swollen and could not move. She has a history of rheumatoid arthritis with routine treatment using Leflunomide 20 mg once daily and hypertension on routine medication. Patient’s plain right femur radiography in Fig. 1 showed a closed intertrochanteric right femoral fracture and she was planned to undergo right hemiarthroplasty with cemented bipolar fixation performed by an orthopaedic surgeon.
Fig. 1.
Intertrochanteric right femoral fracture.
Preoperatively she was noted to be fully conscious, oriented with good cognition and had a pulse rate of 98 beats/minute and her blood pressure was 170/100 mmHg. Her systemic examination was within normal limits. Laboratory examination result showed haemoglobin level was 11 g/dL and all other routine investigations including blood sugar, renal and liver function test, also electrocardiography (ECG) was normal. Her chest X-Ray showed hypertensive heart disease with aorta sclerosis. The case was categorized as ASA 3 and one day before the procedure, the patient got medication of ondansetron, ranitidine, ceftriaxone, and also leflunomide.
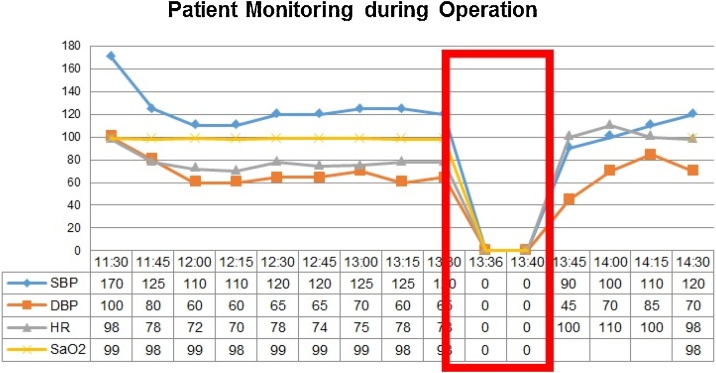
The patient was administered with a 27 G needle in L3L4 space and given 2 mg of bupivacaine intrathecally. After 10 min, she was put in a left lateral position. T5T6 block was achieved. The procedure then conducted with close monitoring of vital signs. Vital signs relatively stable during the procedure until the insertion of MMA cement. Six minutes after the insertion, she went into cardiac arrest. The surgical site was immediately packed and the patient shifted to a supine position. Chest compressions were started and the patient was intubated with an endotracheal tube and ventilated with 100% oxygen. Intravenous adrenaline 1 mg in 10 mL saline was given. Fluids were rushed and cardiac compressions continued. After 2 cycles of high-quality CPR, the patient gained a return of spontaneous circulation and surgery continued, then shifted to ICU. Fig. 2 showed Patient Monitoring during Operation. The red box showed how the patient was in a cardiac arrest condition from the patient’s vital sign monitoring.
Fig. 2.
Cardiac arrest condition during operation after insertion of MMA cement.
After overnight ventilator support, weaning was done and she recovered without any central nervous effects. The patient then transferred to the regular ward and discharged on the tenth day after surgery. In the regular ward, the physiotherapy was performed and the subject satisfied with the operation results. The patient has been informed to avoid combinations of excessive flexion, internal rotation, and adduction or excessive extension, external rotation, and adduction. The patient’s family also has been informed for the subject’s condition and written informed consent was obtained from the patient for publication of this case report and accompanying images after transferred to the regular ward. This study has been carried out in line with SCARE 2018 criteria [6].
3. Discussion
BCIS still has no agreed definition. It is characterized by several clinical features that include hypoxia, hypotension, cardiac arrhythmias, increased pulmonary vascular resistance (PVR), and cardiac arrest. It is commonly associated with hip arthroplasty and usually occurs at one of the five stages in the surgical procedure: femoral reaming, acetabular or femoral cement implantation, insertion of the prosthesis, or joint reduction [7].
BCIS has a wide spectrum of severity. A majority of affected patients develop non-fulminant BCIS which is characterized by a significant, yet transient, reduction in arterial oxygen saturation and systolic blood pressure (SBP) in the peri-cementation period. While a small proportion of patients will develop fulminant BCIS, with profound intraoperative cardiovascular changes, progressing to arrhythmias, shock, or cardiac arrest. Classification of BCIS severity was proposed by Donaldson et al. in 2009 in Table 1 [8].
Table 1.
Classification of BCIS severity.
| BCIS Grade | Hypoxia | Hypotension | Loss of Consciousness |
|---|---|---|---|
| Grade I | Moderate: SpO2 <94% | Moderate: Decreased SBP ≥ 20% | None |
| Grade 2 | Severe: SpO2 <88% | Severe: Decreased SBP ≥ 40% | Unexpected Loss of Consciousness |
| Grade 3 | Cardiovascular collapse requiring CPR | ||
Systemic toxicity of unpolymerized methyl methacrylate (MMA) mixed with the MMA polymer or other additives used in cement. It was later shown that maximum MMA monomers concentration in blood during the procedure is 30 times lesser than the required amount to produce cardiovascular and respiratory effects [9].
Immunological mechanisms, type I hypersensitivity/anaphylactic reaction to the acrylic monomer, may have a role in the causation of the acute events [9]. A significant increase in plasma histamine concentration in hypotensive patients undergoing cementation has been demonstrated. It is unclear whether the histamine release is attributable to a direct effect of the cement monomer or through an IgE-mediated process. In a single study, blockade of histamine receptors with clemastine and cimetidine (H1 and H2 antagonists) appeared to impart a protective effect, but these findings have not been reproduced in more recent studies. Contact hypersensitivity (Type 4 hypersensitivity) to MMA has been demonstrated in surgeons and experimental animals. The anaphylatoxins C3a and C5a are potent mediators of vasoconstriction and bronchoconstriction. An increase in C3a and C5a levels, suggesting activation of the complement pathway, has been demonstrated in cemented hemiarthroplasty but not in uncemented hemiarthroplasty. High-dose methylprednisolone (2 g) was demonstrated to attenuate complement activation and hypoxia in a small randomized controlled, double-blinded study of patients undergoing a cemented arthroplasty. Methylprednisolone appeared to prevent the release of anaphylatoxins and the development of oxygen desaturation [7].
Transesophageal echocardiography showed emboli that were named “snow flurry” by Lafont et al. These emboli were seen with both cemented and non-cemented procedures [9]. Embolization occurs as a result of high intramedullary pressures developing during cementation and prosthesis insertion. The cement undergoes an exothermic reaction and expands in the space between the prosthesis and bone, trapping air and medullary contents under pressure so that they are forced into the circulation. The temperature of the cement can increase as high as 96 °C 6 min after mixing the components. When cement is inserted into the femur using a cement gun, the pressures generated are almost double those seen when manual packing is used. The debris from the medulla can embolized to the lungs, heart or paradoxically to the cerebral and coronary circulations. It is thought that showers of pulmonary emboli result in the characteristic hypoxia and right ventricular dysfunction leading to hypotension [7].
The embolic model has become the dominant hypothesis as the causative process in BCIS. However, embolization does not explain all of the observed phenomena. Embolization is not always associated with hemodynamic changes and the degree of embolism correlates poorly with the extent of hypotension or hypoxaemia. Several of the phenomena may have opposing actions and the combined effects of BCIS on hemodynamic variables will depend on the relative magnitude of the changes in PVR, SVR, and myocardial contractility. It is reasonable to assume that the patient’s pre-existing comorbidities may alter the clinical features of BCIS [7].
Several risk factors have been proposed in the development of BCIS, including 1.) Underlying cardiovascular disease: right ventricle (RV) dysfunction, coronary artery disease, and preexisting pulmonary arterial hypertension; 2.) Advanced age; 3.) Osteoporosis (enlarged porous cavities increase the risk of emboli generation); 4.) Fracture diagnosis as an indication for surgery, especially intertrochanteric in type or those associated with underlying malignancy; 5.) Metastatic bone disease; 6.) Femoral canal diameter of more than 21 mm; 7.) Previously non-instrumented femoral canal; 8.) Patent foramen ovale (paradoxical embolus) [9].
Patients with a previously un-instrumented femoral canal may be at higher risk of developing the syndrome than those undergoing revision surgeries. There are two possible mechanisms. First, there is more potentially embolic material present in an un-instrumented femur. Second, once the canal has been instrumented and cemented, the inner surface of the femur becomes smooth and sclerotic, it offers a less permeable surface. The use of a long-stem femoral component increases the likelihood of developing BCIS [7].
There is an absence of clinical trials comparing different management approaches to BCIS, so current recommendations are empiric and guided by case reports as well as basic physiological principles. Cardiovascular collapse, in the context of BCIS, should be viewed and treated as right ventricular (RV) failure. In general, early and aggressive resuscitation is the cornerstone of treating BCIS. Administration of 100% inspired oxygen is a first-line therapy. Invasive hemodynamic monitoring should be established. In severe BCIS, regular advanced cardiopulmonary life support (ACLS) algorithms and procedures should be followed. Fluid resuscitation to maintain RV preload and inotropes to support ventricular contractility is recommended. Vasopressors (such as phenylephrine and noradrenaline) primarily cause peripheral vasoconstriction, increase aortic blood pressure, which in turn supports coronary artery blood flow, and thus improves myocardial perfusion and contractility. The use of vasopressors and inotropes should be continued into the postoperative period as necessary, under the management of the intensive care unit (ICU) [8].
Alterations in surgical technique consist of changes to minimize the likelihood of cement embolization, including consideration of using uncemented prosthesis in high-risk patients. A recent experimental study using sheep models also explored the role of inferior vena cava (IVC) filters in preventing pulmonary embolization and subsequent BCIS. The clinical impact of an IVC filter is yet to be determined. As anaesthetic management of BCIS is mainly supportive, once the decision has been made to proceed with the operation, surgical modifications are the only alterations which will affect the occurrence of BCIS and has been shown in Table 2 [8].
Table 2.
Surgical techniques to minimize the risk of BCIS.
| Surgical techniques addressing BCIS |
|---|
| Lavage of the femoral canal before cement insertion |
| High pressure, high-volume, pulsatile lavage |
| Brushing and drying of the intramedullary canal of the femoral shaft before cementation |
| Use of a suction catheter to depressurise the intramedullary canal |
| Utilizing a bone-vacuum technique (mixing cement in a vacuum and using a retrograde cement introduction) |
The patient illustrated in our case was diagnosed with severe or grade 3 bone cement implantation syndrome. Although the etiology is still unclear, our patient has several comorbidities that increased the risk of BCIS, including advanced ages and intertrochanteric femur fracture. Although the further examination is needed, the patient also suspected with heart failure related to hypertensive heart disease and osteoporosis due to the history of rheumatoid arthritis, advanced ages, and her pathological fracture.
Despite its high mortality rate, which is 2% and 95% of patients who died within 48 h had BCIS grade 2 or 3 during surgery based on a retrospective study conducted by Olsen et al. 2014 [3], this patient successfully resuscitated following ACLS algorithm and giving the mechanical ventilation. She was then discharged nine days after the procedure with a stable condition.
The limitation of this study is the difficulty to follow up on the patient post discharged. It is because some Indonesian has a habit to change their phone number frequently especially if they live on the border region or the outskirt of Indonesia. The other problem is the distance from the patient’s home to the hospital that causing the patient to be reluctant to undergo follow up under the same surgeon. They usually choose to go to the nearest hospital for the next follow up and for the wound control. These issues hinder the author to follow up the patient for the general condition after the BCIS and the underlying risk factor that can contribute to the BCIS incidence.
Despite the rarity of the BCIS, the high mortality rate still becomes a concern in orthopaedic. Communication between the orthopaedic surgeon and anesthesiologist will become a good basis for a perioperative preparation. A good response time and high-quality cardiopulmonary resuscitation (CPR) also takes a major role in a BCIS critical condition.
4. Conclusion
BCIS is a rare complication of bone cementation in orthopaedic procedures. Patients with comorbidities and risk factors should be monitored closely during and after bone cementation. Both orthopaedic surgeon and anesthesiologist should recognize the clinical presentation of BCIS and well-prepared for the management of BCIS including supportive measures along with ACLS guidelines. Preoperative optimization by increasing oxygen inspiration concentration and avoiding intravascular volume depletion during operation is essential in cemented arthroplasty procedure.
Declaration of Competing Interest
The author has no conflict of interest to declare.
Funding
Author’s personal funding.
Ethical approval
This study has been reviewed by the authors’ Institutional Review Board, and the patient had given a written consent.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Registration of research studies
Not applicable.
Guarantor
Respatih S. Dradjat, MD, PhD.
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
Respati Suryanto Dradjat: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing - original draft, Writing - review & editing. Ananto Satya Pradana: Project administration, Conceptualization, Formal analysis, Investigation, Methodology, Writing - original draft, Writing - review & editing. Domy Pradana Putra: Conceptualization, Formal analysis, Investigation, Methodology, Software, Writing - original draft, Writing - review & editing. Ray Asaf Hexa Pandiangan: Writing - review & editing. Felix Cendikiawan: Writing - review & editing. Edi Mustamsir: Conceptualization, Data curation, Formal analysis, Project administration, Resources.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Contributor Information
Respati Suryanto Dradjat, Email: respatisdradjat@ub.ac.id.
Ananto Satya Pradana, Email: satyapradana88@gmail.com.
Domy Pradana Putra, Email: domypradanaputra@gmail.com.
Ray Asaf Hexa Pandiangan, Email: ray.asaf@gmail.com.
Felix Cendikiawan, Email: md.felix.c@gmail.com.
Edi Mustamsir, Email: edimustamsir@ub.ac.id.
References
- 1.Barışhan F.C., Akesen B., Atıcı T., Durak K., Bilgen M.S. Comparison of hemiarthroplasty and total hip arthroplasty in elderly patients with displaced femoral neck fractures. J. Int. Med. Res. 2018;46:2717–2730. doi: 10.1177/0300060518770354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaufmann K.B., Baar W., Rexer J., Loeffler T., Heinrich S., Konstantinidis L., Buerkle H., Goebel U. Evaluation of hemodynamic goal-directed therapy to reduce the incidence of bone cement implantation syndrome in patients undergoing cemented hip arthroplasty - a randomized parallel-arm trial. BMC Anesthesiol. 2018 doi: 10.1186/s12871-018-0526-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Olsen F., Kotyra M., Houltz E., Ricksten S.E. Bone cement implantation syndrome in cemented hemiarthroplasty for femoral neck fracture: incidence, risk factors, and effect on outcome. Br. J. Anaesth. 2014 doi: 10.1093/bja/aeu226. [DOI] [PubMed] [Google Scholar]
- 4.Baig M.N., Curtin W., Callaghan M.A., Murphy C.G. Catastrophic cement reaction following cementation for megaprosthesis for proximal femoral fracture. BMJ Case Rep. 2017 doi: 10.1136/bcr-2017-220158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Griffiths R., White S.M., Moppett I.K., Parker M.J., Chesser T.J.S., Costa M.L., Johansen A., Wilson H., Timperley A.J. Safety guideline: reducing the risk from cemented hemiarthroplasty for hip fracture 2015: Association of Anaesthetists of Great Britain and Ireland British Orthopaedic Association British Geriatric Society. Anaesthesia. 2015 doi: 10.1111/anae.13036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A.J., Orgill D.P., Zhu H., Alsawadi A., Noureldin A., Rao A., Enam A., Thoma A., Bashashati M., Vasudevan B., Beamish A., Challacombe B., De Wilde R.L., Machado-Aranda D., Laskin D., Muzumdar D., D’cruz A., Manning T., Healy D., Pagano D., Goel P., Ranganathan P., Pai P.S., Raja S., Ather M.H., kadioäžlu H., Nixon I., Mukherjee I., Gómez Rivas J., Raveendran K., Derbyshire L., Valmasoni M., Chalkoo M., Raison N., Muensterer O., Bradley P., Roberto C., Afifi R., Rosin D., Klappenbach R., Wynn R., Giordano S., Basu S., Surani S., Suman P., Thorat M., Kasi V. The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018 doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 7.Donaldson A.J., Thomson H.E., Harper N.J., Kenny N.W. Bone cement implantation syndrome. Br. J. Anaesth. 2009 doi: 10.1093/bja/aen328. [DOI] [PubMed] [Google Scholar]
- 8.So D., Yu C., Doane M.A. Bone Cement Implantation Syndrome; 2017. Subscribe to ATOTW Tutorials by Visiting; pp. 1–6.www.wfsahq.org/resources/anaesthesia-tutorial-of-the-week [Google Scholar]
- 9.Kalra A., Sharma A., Palaniswamy C., El-Oshar S., Desai P., Yazbeck M., Zanotti-Cavazzoni S.L. Diagnosis and management of bone cement implantation syndrome: case report and brief review. Am. J. Ther. 2013 doi: 10.1097/MJT.0b013e31820b3de3. [DOI] [PubMed] [Google Scholar]