Abstract Book
3 – 4 December 2020
Disclosure Statement
All content was reviewed and selected by the Irish Thoracic Society Annual Scientific Meeting Faculty which held full responsibility for the abstract selections.
The operational costs of the Irish Thoracic Society Annual Scientific Meeting 2020 are funded with the support of a number of commercial bodies through unrestricted educational grants. These are listed overleaf.
Irish Thoracic Society Annual Scientific Meeting 2020
Wednesday 2nd December
14.00 – 17.00 Irish Thoracic Society Paediatric Forum
Thursday 3rd December
09.00 – 13.00 1. COVID-19Chairs: Dr Marcus Kennedy, Cork University Hospital, Cork
Professor Lorcan McGarvey, Queens University Belfast.
9.00 – 10.15 Poster Discussions
10.15 – 10.30 Break
10.30 – 11.45 Oral Presentations I
1.1.1 Pulmonary Embolism and COVID-19; a single centre review
1.1.2 Persisting Symptoms in COVID-19: A First Look
1.1.3 CoViD-19 at home: A Safety Study for the Remote Home Monitoring of Patients with Novel SARS-CoV-2
1.1.4 Clinical characteristics, disease course and outcome of the first 117 hospitalised patients with COVID-19 pneumonia in a Dublin hospital: a single-centre descriptive study
1.1.5 Evaluating the Outcomes of an Integrated Multidisciplinary COVID-19 Recovery Care Clinic
12.00 – 13.00 Guest Lecture: Management of Acute and Chronic Respiratory Failure due to COVID-19
Professor Stefano Nava, Professor of Respiratory Medicine, University of Bologna
13.00 – 14.00 Break for lunch
14.00 – 18.00 2. Lung Cancer/ILD/CF/Thoracic Surgery and Transplant Chairs: Professor Ross Morgan, Beaumont Hospital Dublin
Professor Karen Redmond, Mater Misericordiae University Hospital Dublin
14.00 – 15.15 Poster Discussions
15.15 – 15.30 Break
15.30 – 16.45 Oral Presentations II
2.1.1 Disease characterisation of people in Ireland with cystic fibrosis heterozygous for the F508del mutation and a minimal function mutation
2.1.2 Interleukin-22 and Neutrophil Proteins as Predictors of Future Disease Severity in Children with Cystic Fibrosis
2.1.3 Real-life Data on the Safety and Tolerability of Pirfenidone versus Nintedanib in Idiopathic Pulmonary Fibrosis (IPF) Patients: A Single-Centre Study
2.1.4 Delay in Primary Lung Cancer detection due to COVID-19 Pandemic
2.1.5 The value of perioperative bronchoalveolar lavage in thoracic surgery- St. Vincent’s University Hospital experience
17.00 – 18.00 Guest Lecture: Skeletal muscle in COPD: now a treatable trait?
Professor Michael Polkey, Royal Brompton Hospital Trust
Friday 4th December
09.00 – 13.00 3. General Respiratory and Sleep Medicine Chairs: Professor Eddie Moloney, Tallaght University Hospital Dublin
Dr Jacqueline Rendall, Belfast City Hospital Belfast
9.00 – 10.15 Poster Discussions
10.15 – 10.30 Break
10.30 – 11.45 Oral Presentations III
3.1.1 A novel high viscosity perfusion solution protects against oedema formation in ex vivo lung perfusion for lung transplant; a preclinical study
3.1.2 A Retrospective Cohort Study, Analysing Factors Which May Influence Adherence to Prescribed Oxygen Therapy
3.1.3 To Develop, Implement and Evaluate an Integrated Care Pathway for Patients Presenting with Pneumothorax
3.1.4 Diagnostic sleep studies and CPAP set-up in the midst of a pandemic
3.1.5 Pilot study to assess the accuracy of Positive Airway Pressure (PAP) derived Apnoea-Hypopnoea Index (AHI) by using an Independent Novel PAP home monitoring device.
11.45 – 12.00 Break
12 .00 – 13.00 Guest Lecture: Sleep Medicine
Professor Atul Malhotra, UC San Diego
13.00 – 14.00 Break for lunch
14.00 – 18.00 4. COPD and Asthma Chairs: Dr Marcus Butler, St Vincent's University Hospital Dublin
Dr Aidan O'Brien, University Hospital Limerick
14.00 – 15.15 Poster Discussions
15.15 – 15.30 Break
15.30 – 16.45 Oral Presentations IV
4.1.1 An Observation of Infection Risks in Severe Asthma Patients on Anti-IL5 Therapy
4.1.2 Is Fractional Exhaled Nitric Oxide measurement relevant in Athletes?
4.1.3 A survey of physiotherapists use of airway clearance techniques for patients experiencing exacerbations of chronic obstructive pulmonary disease in the Republic of Ireland
4.1.4 An Acoustic Method of Determining Dry Powder Inhaler Suitability in Obstructive Lung Disease
4.1.5 Long Term Outcomes in Patients Treated with Non-invasive Ventilation for Hypercarbic
16.45 – 17.00 Break
17.00 – 18.00 Guest Lecture: Immunology and management of severe asthma
Professor Guy Brusselle, University Hospital Ghent
IRISH THORACIC SOCIETY POSTER REVIEW AND DISCUSSION
1. COVID-19
1.1. Mercy University Hospital Covid-19 Management Strategy, Demographics and Outcomes.
Deasy KF1*, Kavanagh G1*, O’Connor B1, McKiernan J1, Unnithan P1, Jackson A2, Curran C1, O’Connor TM1.
1 Department of Respiratory Medicine, Mercy University Hospital
2 Department of Infectious Diseases, Mercy University Hospital
*these authors contributed equally to this work
SARS-CoV2 / Covid-19 is a significant public health dilemma for countries worldwide1. The majority of cases in Ireland evolved over 6 weeks beginning in the latter weeks of March 2020. Parallel approaches emerged to its management in hospitals throughout Ireland.
We developed and managed a streamlined admission process which encompassed 3 streams. A Covid-19 Pathway; broken down into “Covid Resus” / “Covid Pathway” and “Non-Covid”. We created a Covid-19 team and restructured our inpatient services into a 7-day roster with all medical staff, including consultants, assigned to specific hospital areas and groups. A dedicated ED room was converted into a negative pressure resuscitation area. A dedicated ward with negative pressure rooms was assigned exclusively for Covid-19 patients, another was used to isolate patients awaiting swab results.
We performed a retrospective review of definite Covid-19 cases admitted to Mercy University Hospital to our Covid-19 service over approximately a 2-month period beginning March 21st.
| Patient Characteristics (n=36) | No. (% or SD) |
| Age (SD) | 64 (20) |
| Gender, Male (%) | 16 (44) |
| BMI, Mean (SD) | 32 (10.6) |
| Length of Stay, Median (Range) | 7 (1-90) |
| ICU Admission (%) | 6 (16.7) |
| Alive (%) | 33 (91.7) |
| Moderate ARDS | 3 (8.3) |
| Severe ARDS | 7 (19.4) |
| Awake Proning | 4 (11) |
| CPAP / NIPPV | 6 (16.7) |
| Mechanical Ventilation | 7 (19.4) |
| Anti-IL6 Therapy | 2 (5.6) |
No patients died in ICU. MUH suffered no known inpatient Covid-19 transmission. 2 patients died of complications directly attributable to Covid-19. 1 patient recovered from Covid-19 but subsequently died due to an exacerbation of interstitial lung disease. Our in-patient case fatality rate during the examination period was 5.6%.
References
1. Zhu N, Zhang D, Wang W, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. New England Journal of Medicine. 2020;382(8):727-733.
1.2. Audit of the Covid-19 remote patient management programme in Ireland.
1Edwards C, 1Costello E, 2Curley M, 2Smyth L, 3O’Seaghdha C, 3Costello R, 4O’Reilly KMA.
1 patientMpower Ltd., 21 Denzille Lane, Saint Peters, Dublin D02 EY19.
2 HSE Digital Transformation, Dr. Steevens' Hospital, Dublin D08 W2A8.
3 Beaumont Hospital, Beaumont Road, Dublin D09 V2N0.
4 Mater Misericordiae University Hospital, Eccles Street, Dublin D07 R2WY.
Ireland experienced a wave of Covid-19 (SARS-CoV-2) infection starting in February 2020 with 25,462 cases (527/100,000) by 30 June 2020. An important strategy to free up in-hospital capacity was development of capability to remotely manage Covid-19 in lower-risk patients with mild/moderate symptoms.
patientMpower approached the HSE Digital Transformation team and external medical advisers with a design concept for a remote monitoring platform for Covid-19. This consists of a patient-facing app + pulse oximeter (Bluetooth-connected Nonin 3230) enabling patients to record symptoms (e.g. dyspnoea, diarrhoea) & oxygen saturation (SpO2). Patient-recorded data was viewed in real time by their healthcare centre via dedicated monitoring portal. Criteria for remote monitoring included: Covid-19 symptoms, positive for SARS-CoV-2, young age, absence of serious concomitant conditions, need for continued observation post-discharge. Treatment centres emailed app installation instructions to their patients.
Between 13 March and 30 June 2020, 874 patients at 8 primary & 15 secondary care centres had been monitored remotely (median duration: 13 days). 778 patients (89%) gave consent to use of their pseudonymised data for research. Summary statistics from this cohort shown in Table.
Remote monitoring of Covid-19 in appropriate patients can free up in-hospital capacity and provide data to support research.
Summary statistics Covid-19 remote monitoring programme
|
Patients [n (%)] |
Days [median (IQR)] |
|
| Total population | 778 (100%) | |
| Number of days patient used remote monitoring platform | 12 (9-14) | |
| Patients providing ≥1 SpO2 reading | 762 (98%) | |
| Number of days ≥1 SpO2 reading provided | 12 (8-14) | |
| Patients reporting SpO2 94-96% ≥once | 609 (78%) | |
| Patients reporting SpO2 92-93% ≥once | 272 (35%) | |
| Patients reporting SpO2 ≤91% ≥once | 216 (28%) | |
| Patients providing ≥1 dyspnoea score | 733 (94%) | |
| Number of days ≥1 dyspnoea reading provided | 11 (6-13) | |
| Patients reporting ≥1 incidence of diarrhoea | 204 (26%) | |
| Number of days ≥1 incidence of diarrhoea reported | 1 (1-3) | |
| Patients reporting ≥1 co-morbidity | 111 (14%) |
SpO2: oxygen saturation determined by pulse oximetry. IQR: interquartile range.
Conflict of interest statement:
CE and EC are employees and shareholders of patientMpower Ltd.
CO’S is a shareholder of patientMpower Ltd.
RC has received speaking fees for webinars organised by patientMpower Ltd.
1.3. COVID-19 and QTc: Is Hydroxychloroquine worth the risk?
Hydroxychloroquine and Azithromycin Use and QT prolongation in patients hospitalised with COVID-19
C Gill1, A Pollock1,2, R Kumar2, P Devitt2, C Daly2, BD Kent1
Department of Respiratory Medicine 1 & Department of Cardiology 2 , St. James’s Hospital, Dublin, Ireland
1.4. The Effectiveness of Continuous Respiratory Rate Monitoring in Predicting Hypoxic and Pyrexic Events
T. A. McCartan1, A. P. Worrall1, R. Ó Conluain1, F. Alaya1, C. Mulvey1, E. MacHale1, V. Brennan1, L. Lombard1, J. Walsh1, M. Murray1, R. W. Costello1, G. Greene1
1 INCA Group, Royal College of Surgeons in Ireland
Respiratory rate (RR) is a highly useful index of lung function, however objective measurements thereof are rarely taken. In this retrospective cohort study, we compare the distribution of electronically and visually measured RR and test whether continuous electronic RR monitoring can predict oncoming deteriorations in infectious respiratory disease.
34 COVID-19 patients in Beaumont Hospital were analysed, with 3445 observations of visual RR, SpO2 and temperature and 729117 of electronic RR collected. Cox Proportional Hazards Models determined predictive ability for oncoming hypoxic and pyrexic episodes.
Visually measured RR demonstrates bias, toward lower values clustering at 18 and 20 breaths per minute, while electronic RR has a positively skewed gamma distribution (see Figure 1). Raised RR 12 hours prior resulted in a hazard ratio of 1.8 (1.05 to 3.07) for hypoxia and 9.7 (3.8 to 25) for pyrexia. An RR of ≥25 had a sensitivity of 98.4% and a specificity of 91.9% for detecting pyrexia 12 hours in advance.
Electronic, continuous RR removes bias, is a stronger marker of oncoming hypoxia than visual RR and is highly predictive of oncoming pyrexia 12 hours in advance. This could provide an early window to escalate care prior to deterioration, preventing morbidity and mortality.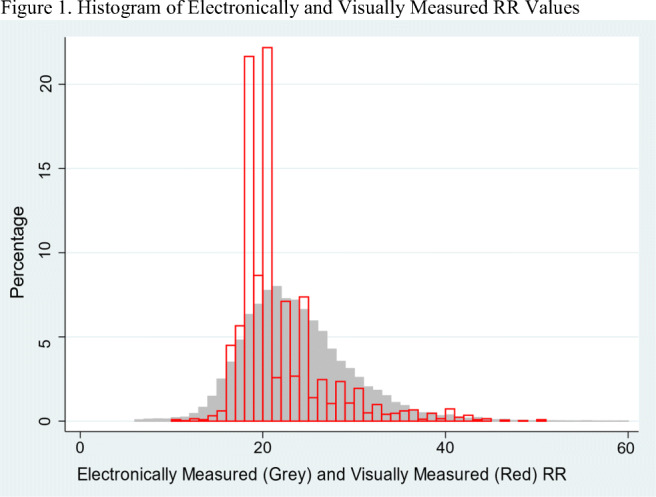
1.5. Increased incidence of ground glass opacification on CT-Thorax during the SARS-CoV-2 pandemic
G. O’Dea1, D. Parfrey1, J. McDonnell1, I. Counihan1, T. Hassan1
1 Respiratory Department, Our Lady of Lourdes (OLOL) Hospital, Drogheda, Co Louth.
Ground glass opacification (GGO) is a radiological sign associated with various lung pathologies, which has recently been described in SARS-CoV-2 respiratory infection1.
We studied the incidence of new GGO on CT-Thorax during a period of the SARS-CoV-2 pandemic in OLOL Hospital between 29 February and 31 July 2020 and examined interval radiology.
During the study period, 64 GGOs were reported on CT-Thorax, compared to 29 in the previous year (increase of 121%, p <0.01). SARS-CoV-2 PCR was detected in 33 cases (51.6%), while 20 cases were highly suspicious for SARS-CoV-2 despite undetectable PCR (31.3%). Remaining cases of GGO included decompensated heart failure (ADHF; 3), pneumocystis pneumonia (PCP; 2), amiodarone-induced pneumonitis (1) and acute interstitial pneumonitis (AIP; 1).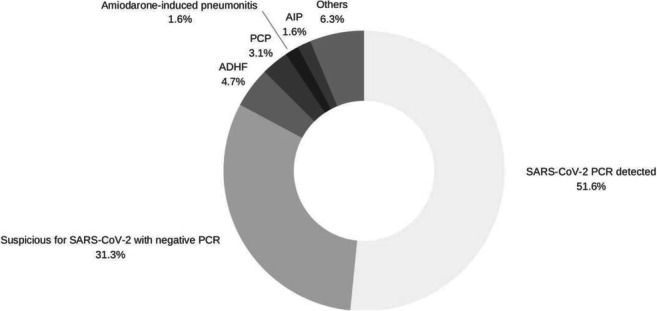
Figure 1. Categorisation of new cases of GGO in the study period.
Although PCR testing is the gold standard in diagnosis of SARS-CoV-2 respiratory infection, CT-thorax findings including GGO are sensitive and are often seen before PCR detection1. Our data shows that the incidence of GGO increased by 3-fold during the pandemic, suggesting that GGO is more sensitive than PCR testing but that other acute respiratory pathologies should be considered.
References
1Fang Y, Zhang H, Xie J, et al. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020;296(2):E115-E117. 10.1148/radiol.2020200432
2Ai T, Yang Z, Hou H, et al. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020;296(2):E32-E40. 10.1148/radiol.2020200642
Potential conflicts of interest: None declared.
1.6. COVID-19 IN SARCOIDOSIS: A REVIEW
A Sarfaraz1, H Rahman1, S Joomye1, A Subramaniam1, SC Donnelly1
1 Medical Professorial Unit, Tallaght University Hospital & Trinity College Dublin
The novel coronavirus pandemic poses challenges to both patients and physicians. COVID-19 is deemed to increase the risk of morbidity and mortality in sarcoidosis despite the limited data at present. We report our experience on the prevalence, clinical features and outcomes of COVID-19 in these patients.
We retrospectively evaluated all sarcoidosis patients attending our specialist ILD service. Data was obtained from telephonic interviews and chart reviews. Parameters including disease manifestation of sarcoidosis, presence of COVID-19 symptoms, viral PCR results and treatment administered were analysed.
Among 175 patients [mean age 58.8 (±14) years, 86 (43.2%) men], 26 (14.8%) were diagnosed with positive COVID-19 infection. Of these, 24 patients (92%) had at least one comorbidity, and 11 (42%) had two or more comorbidities. Comorbidities included hypertension, diabetes, cardiac disease, COPD and malignancy. Hydroxychloroquine was neither associated with the occurrence nor the severity of COVID-19. Four patients [mean age 61 (±11.5) years] required hospital admission and 2 of them died. Hospitalized patients were on higher doses of maintenance corticosteroids than non-hospitalized patients; and all had one or more comorbidity.
In conclusion, our dataset suggests that the prevalence of COVID-19 in sarcoidosis patients is slightly higher than the general population and about 15% present a severe course.
1.7. Awake Proning: Turning the table on COVID-19.
S Toland1, R McGuinness1 , M Casey1, RW Costello1, NG McElvaney1, C Gunaratnam1, P Branagan1, K Hurley1, E O’Brien1, R Morgan1, B McNicholas1, I Sulaiman1
1 Department of Respiratory Medicine, Beaumont Hospital, Dublin 9, Ireland.
One of the few evidence based treatments for Acute Respiratory Distress (ARDS) is prone position ventilation which has proven to reduce mortality in patients receiving mechanical ventilation(MV). It promotes lung homogeneity, improves gas exchange and respiratory mechanics. One of the hallmark features of severe SARS CoV2 is ARDS where patients can be oxygenated by MV or by awake non-invasive ventilation(NIV). It is not clear if awake proning in patients on NIV is as effective in SARS CoV2.
This retrospective multi-centre study assessed all patients admitted with confirmed COVID-19 who were placed in awake prone position. 65 patients were identified across 7 centres. Co-morbidites, medications, vital signs and oxygen requirements on admission were documented. Data was analysed pre and post proning. Outcomes included endotracheal intubation and death.
Of the 65 patients, 44 were male (67.7%) with a median age of 54 (IQR 44-65). Thirty patients (46.1%) were on general wards, 30 (46.1%) in ICU and 5 (7.69%) in HDU. Within the whole cohort only 9 (13.63%) did not tolerate awake proning. The median time spent proning was 4 (IQR 2-8.75) hours. The mean S/F ratio pre-proning was 211, 217 1 hour post proning and 239 post proning. With regards to outcomes, only 19 patients (28.79%) required endotracheal intubation and 4 (6%) patients died.
Awake proning is a non-invasive tool that physiologically promotes gas exchange thus helping avoid intubation and MV in SARS CoV2.
1.8. Non-invasive Respiratory Support Strategies in Covid-19 pneumonia
1L Kingsmore, 1L Davidson, 1C Bradley, 1W Anderson, 1M Drain
1 Respiratory Department, Antrim Area Hospital, Antrim, Northern Ireland
Evidence suggests that the use of continuous positive airway pressure (CPAP) in Covid-19 pneumonitis can avoid intubation in some patients. High flow nasal oxygen (HFNO) use has been contentious.
We retrospectively reviewed the clinical notes for all respiratory patients admitted between March 1st and May 31st 2020 to identify patients with a diagnosis of COVID-19 pneumonitis requiring respiratory support and recorded patient demographics and outcomes.
56 patients who received respiratory support were identified. The median age (IQR) was 65 (54,77 years), 65% were male, and overall mortality was 44%. 3 (5%) patients were intubated without trial of non-invasive ventilation (NIV) and 1 patient received BiPAP (Bilevel positive airway pressure) due to underlying COPD.
The table below demonstrates the results.
| Initial respiratory support | CPAP | HFNO |
| Number of cases | 27 | 25 |
| Median Age (IQR) | 63(54,77) | 70(58,79) |
| Mortality | 43% | 48% |
| Subsequent trial of alternative non-invasive respiratory support | 56%(n=15) | 12%(n=3) |
| Required invasive ventilation | 36%(n=10) | 28%(n=7) |
In conclusion, the mortality in patients with COVID-19 pneumonia who required respiratory support was high, and over half of the patients for full escalation in the event of treatment failure required invasive ventilation. Further studies are clearly required, comparing patient comorbidities and outcomes using different modalities of respiratory support.
1.9. The impact of COVID-19 related healthcare disruption on TB testing and notification
B. Nolan1, P. Lyng2, F. Dennehy3, S. McDermott3, S.L. O’Beirne1,4
1. Department of Respiratory Medicine, St. Vincent’s University Hospital, Elm Park, Dublin 4.
2. Department of Public Health East, Dr Steeven’s Hospital, Dublin 8.
3. Department of Clinical Microbiology, St. Vincent’s University Hospital, Elm Park, Dublin 4.
4. Department of Respiratory Medicine, St. Michael’s Hospital, Dun Laoghaire, Co. Dublin.
The coronavirus disease (COVID)-19 pandemic has impacted all facets of healthcare with dramatic reductions in outpatient clinic and emergency department attendances1. We hypothesised that during the pandemic-related healthcare service disruption, TB testing and diagnosis would be significantly reduced.
In Ireland, COVID-19 cases and healthcare service disruption peaked from March-June. The number of sputa and bronchoalveolar lavage/bronchial washing (BAL/BW) samples submitted to the microbiology laboratory in St. Vincent’s University Hospital (SVUH) for TB testing during this period were evaluated and compared to 2019. Separately, monthly AFB notifications to public health services in counties Dublin, Wicklow and Kildare from March to July 2020 were assessed.
From March-June 2020, 102 BAL/BW and 142 sputum samples were submitted for mycobacterial analysis vs 403 and 239 samples respectively during the same period in 2019, a 62% decrease. The rate of AFB notifications was reduced for March/April/May 2020, however notification rates increased in June/July resulting in similar notifications overall for March-July of both years.
During the height of the COVID-19 pandemic there was a marked reduction in mycobacterial respiratory sample testing at SVUH, and in AFB notifications. However, as restrictions lifted and healthcare services resumed TB notifications increased, remaining overall comparable to same period in 2019.
References
1) Scoping evidence summary for the effectiveness of pathways to enable the resumption of hospital-based care in the context of COVID-19. Ireland; Health Information and Quality Authority, 2020. Available from: https://www.hiqa.ie/sites/default/files/2020-06/Effectiveness-of-pathways-for-the-resumption-of-hospital-care-after-COVID-19.pdf
Conflict of Interest: The authors have no conflict of interest to declare.
1.10 Reduction in hospital admissions for Acute Exacerbations of COPD during COVID-19 pandemic
A Straszewicz, E Jordan, A Nolan, H Mulryan, N Byrne, D Langan, A O’Regan, M McDonnell, M Harrison, R Rutherford, M Brennan.
Department of Respiratory Medicine, Saolta University Health Care Group (SUHCG), University Hospital Galway, Co. Galway
The COVID-19 pandemic led to the rapid introduction of community infection control measures to attenuate viral transmission. Despite patients with COPD being at higher risk of poorer outcomes1 we noticed a reduction in AECOPD and also extremely low COVID-19 infection rates in these patients. We sought to examine this in closer detail.
We performed a retrospective review of hospital admissions with AECOPD to Galway University Hospital during two-month period during the COVID-19 pandemic compared with the same period in 2019. Adult patients with known COPD and a primary diagnosis of AECOPD were included. Data on clinical presentation, laboratory findings, imaging reports, DECAF scores and outcomes was collected using electronic healthcare records.
There was a 31.8% relative reduction in AECOPD hospitalisations during the COVID-19 period, 58 versus 85 patients. There was no difference in premorbid mMRC score, DECAF score, length of stay or mortality between groups indicating similar exacerbation severity.
Our study observed a significant and immediate reduction in AECOPD hospitalisations as a result of community infection control measures instituted to combat the spread of COVID-19. We propose that future COPD management programs could integrate some of these approaches in patients who exacerbate frequently despite optimal management.
The authors have no conflicts of interest to disclose.
References
1. Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, Li YM, Liu XQ, Chen RC, Tang CL, Wang T, Ou CQ. Comorbidity and its impact on 1590 patients with Covid-19 in China: A Nationwide Analysis. European Respiratory Journal. 2020 May 1;55(5).
1.11. Pulmonary Function in Post COVID-19 Symptomatic patients
Stephenson, J., Balicaco, M., Falcao, C., Nyaude, T., O Brien, A
University Hospital Limerick.
Persistent breathlessness following COVID-19 infection is becoming an increasingly observed phenomenon. A recent Italian study noted than over 40% of patients hospitalised with COVID-19 infection had persistent dyspnoea at 60 days after the onset of COVID-19 infection1. We have recently started receiving referrals for such patients. Here we present their Pulmonary Function Data performed at UHL.
7 Patients, (2M/ 5F) aged 34-66, with a Positive Nasal Swab/Throat Swab for COVID -19 between January 2020 and March 2020 were referred for Pulmonary Function due to persistence shortness of breath. Spirometry and DLCO were performed 45-60 days post Covid-19 infection with confirmed negative swab.
6 patients had normal FEV1, FVC and FEV1/FVC ratio. 1 patient had normal FVC and FEV1/FVC% with a mildly reduced FEV1 (ATS 2005). The same patient with low FEV1 has also low transfer factor; the other 6 patients had normal transfer factor.
Most of these patients were very active prior to COVID-19 infection. While most of these patients have normal lung function, there is a significant reduction in their normal activity level due to persistent shortness of breath.
In this study, the persistent shortness of breath in this patient group does not suggest an association with impaired lung function. Further longitudinal lung function measurements in a larger group of symptomatic patients post COVID-19 infection are necessary, as well as further studies to help elucidate the pathophysiology of persistent symptoms despite normal baseline lung function testing.
References
1. Carfi A. JAMA August 11, 2020 Volume 324, Number 6
1.12. A clinical audit to determine the outcome of inpatient exercise rehabilitation on outcomes including functional capacity, dyspnoea and muscle strength in patients diagnosed with COVID-19.
C Barrett, L Pelow
Physiotherapy Department, St Vincent’s University Hospital, Dublin 4
Coronavirus disease 19 (COVID-19), caused by SARS-CoV-2, is an acute viral respiratory disease. Characteristic symptoms include fever, cough, fatigue and dyspnoea1. Exercise is an integral component of physiotherapy in the management of respiratory disorders, with greater benefits for community acquired pneumonia than respiratory physiotherapy alone2. There is limited data on the effects of exercise rehabilitation in COVID-19. This audit aims to analyse the outcome of inpatient exercise rehabilitation on functional outcomes in patients with COVID-19.
A prospective audit was completed, with data collected and analysed using an excel spreadsheet Five patients aged 78±4 received physiotherapy intervention, including exercise rehabilitation, with outcome measures completed at initial assessment and at one week. The primary outcome measure was the two minute walk test (2MWT) to measure functional capacity. The secondary outcomes were muscle strength measured through five times sit-to-stand, and dyspnoea measured by the medical research council (MRC) dyspnoea scale.
Functional outcomes improved in all patients. There was an overall 37% improvement in 2MWT distance, 29% improvement in muscle strength and 47% improvement in dyspnoea.
In conclusion, as has been shown in other respiratory disorders2, one week of inpatient exercise rehabilitation improved functional capacity, muscle strength and dyspnoea in older people with COVID-19.
1Thomas P, Baldwin C, Bissett B, Boden I, Gossenlink R, Granger CL, Hodgson C, Jones A, Kho, M, Moses R, Ntoumenopoulos G, Parry S, Patman S, van der Lee L. Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations, Journal of Physiotherapy. 2020; 66(2)
2Jose A, Dal Corso S. Inpatient rehabilitation improves functional capacity, peripheral muscle strength and quality of life in patients with community-acquired pneumonia: a randomised trial. Journal of Physiotherapy. 2016; 62:96-102
1.13 Review of patient experiences of receiving biologic therapy in Cork University Hospital during COVID19 pandemic.
Maher A1, Casey D1, Sweeney A1, Murphy J1, Plant BJ 1, 2, Murphy DM1,2
1 Department of Respiratory Medicine, Cork University Hospital, Wilton, Cork.
2 Health Research Board, Clinical Research Facility, University College Cork, Cork
We reviewed patients receiving biologic treatment for brittle asthma and assessed their experience of therapy in CUH during COVID-19 using the Hospital Anxiety and Depression Scale (HADS).
56 patients were eligible to take part in this study. They were contacted by the respiratory nurse specialist and asked to complete the HADS questionnaire in July 2020. Patients were asked about their experiences in relation to receiving infusions during COVID-19.
53/56 questionnaires were completed and analysed. 92.4% of patients continued biologic therapy throughout the pandemic. Those that did not attend appointments had safety concerns. 20% of patients exacerbated during COVID-19 and there was one case of COVID-19. 22% of patients reported having a pre-morbid history of anxiety and/or depression. The HADs scale highlighted 32% of people had anxiety while 7.5% of patients had a score in keeping with depression.
Overall, the vast majority of this cohort of patients were happy to date with their care during the COVID-19 pandemic.
1.14. The clinical features and risk factors for death of COVID-19 patients admitted to a model 3 General Hospital
Abbas, Z1., Lee, O1., McErney, T., Hogan, C., Periyakaruppan R1, El Gammal, AI1.
1 Respiratory Dept, Naas General Hospital, Naas, Co Kildare.
Naas General Hospital (NGH) is a model 3 public acute hospital. Kildare to date has the highest incidence rate of COVID-19 outside of the capital Dublin.
Retrospective, single-centre case series of 106 consecutive hospitalised patients with confirmed COVID-19 admitted to NGH between March 8th and May 28th. Demographics, clinical, labarotory, radiological, and treatment data were collected, analysed and compared between survivors and non survivors.
Of 106 patients, the median age was 72 years and 58% were men. The majority of the cases were community acquired (50%). Common symptoms included cough (70%), fever (64%) and Dyspnoea (65%). 70% had infiltrates on CXR. Majority of the patients (83%) received antibacterial therapy, 18% received steroids and five received tocilizumab. Twelve patients were transferred to ICU, of whom 9 received invasive ventilation. ICU mortality rate was 33%. Non survivors were older (median age 79 years vs 65 years), had higher Charlson comorbidity index (median 5.4 vs 3.7), were more lymphopenic with higher DDimers and CRP values.
Overall mortality rate in NGH was 30%. We found that older age, underlying comorbidities, lymphopenia and high levels of CRP and DDimers were risk factors for death of COVID-19 patients which can be helpful to identify patients at higher risk at an early stage.
1.15. Real-time Digital Monitoring and Prediction of Adverse Outcomes in COVID-19
G. Greene1.2, T.A. McCartan1, C. Mulvey1, E. MacHale1, L. Lombard1, J. Walsh1, V. Brennan1, R.W. Costello1
1. INCA Group, Royal College of Surgeons in Ireland
2. School of Mathematics and Statistics, University College Dublin
An accurate, predictive clinical risk score could allow early identification and better treatment of deteriorating COVID-19 patients and estimate future healthcare resource demand.
A 13-point multivariable, clinical early warning index, the COVID Critical Care Index (CCCI) was developed through consensus of a panel of experts, implemented in a digital clinical support tool, and validated in a cohort of 256 patients with COVID-19.
Increase in CCCI was strongly predictive of eventual ICU transfer or death, best predicted by a score of ≥6 at any point during admission (HR=5.6 (3.38 to 9.28)). CCCI was a stronger predictor of death/ICU admission than NEWS score or Ratio of Oxygen Saturation (ROX) index (area under the ROC curve (AUROC) of 0·93 (0·89 to 0·96) for CCCI compared to 0·87 (0·82 to 0·92) for NEWS and 0·79 (0·71 to 0·86) for ROX). CCCI is predictive of death/ICU admission at both ≥6 and ≥24 hours prior (AUROC = 0.9 (0.86 to 0.95) and 0·87 (0·82 to 0·92), respectively).
CCCI predicts which COVID-19 patients are high risk with greater accuracy than established clinical deterioration scores, providing a useful time window to estimate future ICU bed demand, facilitate earlier and more effective treatment, and allow better resource allocation.
1.16. CPAP using the PaO2/FiO2 is a successful first line tool in the treatment of Covid-19 related acute hypoxaemic respiratory failure
Shankar Lal1, Eoin Nolan1, Abdul Qadeer1, Elaine Curran1, Junaid Hashmi1, Ian Counihan1, Tidi Hassan1, Ehtesham Khan1
1 Our Lady’s of Lourdes Hospital, Drogheda, Co Louth.
One of the most important clinical debate for the treatment in of Covid-19 acute respiratory failure includes the role of non-invasive ventilation (NIV) such as continuous positive pressure (CPAP) and the threshold for mechanical ventilation (IMV) (1).
129 laboratory-confirmed Covid-19 patients in Our Lady of Lourdes Hospital were admitted. Twenty-seven patients with acute hypoxic respiratory failure that were not reaching target SaO2 and pO2 received CPAP during inpatient hospital stay with age (mean± SD) of 59 ± 13. Fourteen patients (37%) received at last three session of conscious prone position. Ten subjects subsequently were intubated and ventilated with two deaths. No death was observed in subjects receiving CPAP alone with a 100% success rate. PFR before CPAP initiation was negatively correlated with the maximum pressure to achieve target saturations (rs=-0.61,p=0.009)). PFR at 24 hours after commencement of CPAP was significantly higher (mean± SD) (207±92) compared to before CPAP initiation (p=0.03). The average day for CPAP treatment was (mean± SD) 4.6±4.2 days.
In conclusion, this study urgently and importantly shows that CPAP is a useful first-line treatment for Covid-19 acute respiratory failure in a non-ICU setting. PFR is useful to determine response of CPAP which may avoid mechanical ventilation.
References
1. Arulkumaran N, Brealey D, Howell D, Singer M. Use of non0invasive ventilation for patients with Covid-10; a cause for concern? Lancet Respir Med 2020. 10.1016/S2213-2600(20)30181-8
1.17. A Study of Two Ubiquitous Inexpensive Predictive Markers for SARS-Cov-2 to Guide Testing in Regions of Depleted Resources.
Ruaidhri J. Keane1, Caoimhe McGarvey1, Ahmad Basirat1, Chithra Varghese1
1 Department of Medicine, Tallaght University Hospital & Trinity College Dublin, Ireland
1.18. Spot the clot: Improving VTE prophylaxis prescription among patients admitted to hospital with COVID 19: a quality improvement project.
M Calvo-Gurry1, PJ Kerr1, C Sheil1, A Worrall2, M Rowland3, M Lavin4,5, E deBarra2,6, RK Morgan1 and DJ Ryan1.
1. Respiratory Medicine, Beaumont Hospital, Dublin 9.
2. Infectious Diseases, Beaumont Hospital, Dublin 9.
3. St Paul’s Ward, Beaumont Hospital, Dublin 9.
4. Haematology, Beaumont Hospital, Dublin 9.
5. Irish Centre for Vascular Biology, School of Pharmacy & Biomedical Sciences, Royal College of Surgeons Ireland, Dublin 2.
6. Department of International Health and Tropical Medicine, RCSI, Dublin 2.
SARS-CoV-2/COVID-19 is now recognised as a significant risk factor for the development of venous thromboembolism (VTE) in hospitalised patients1. Correct thromboprophylaxis is vital to decrease associated morbidity and mortality. Our aim was to improve the rate of appropriate VTE prophylaxis in patients admitted to Beaumont hospital with COVID-19.
An audit of initial practice found significant room for improvement in VTE prophylaxis prescription. We assessed this over two time periods to determine if practice improved without intervention. We performed three cycles of audit/QI to improve practice locally.
At baseline, 53% of patients received appropriate VTE prophylaxis. As data emerged that COVID-19 was associated with significant VTE disease, this improved to 58%. An education intervention, a cartoon promoting VTE prophylaxis circulated locally and on social media, and involvement of a CNM-champion to improve weight measurement were chosen as interventions and tested. Weight appropriate VTE prophylaxis improved to 100% following our interventions.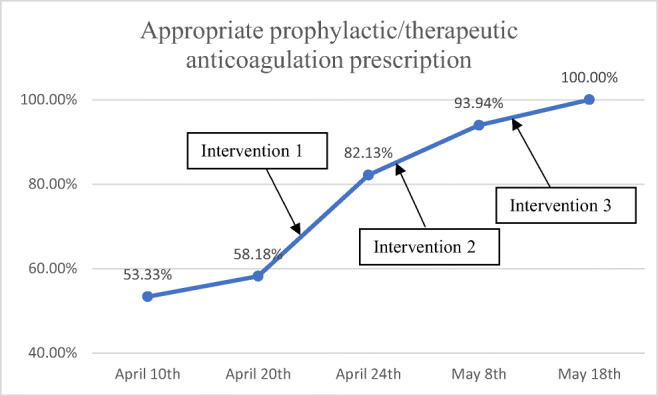
Figure 1. Run chart showing prescription of weight-appropriate thromboprophylaxis/therapeutic anticoagulation where indicated throughout the QI project. Timing of interventions are marked with arrows.
In conclusion, our QI project improved local prescription of VTE thromboprophylaxis during the COVID-19 pandemic. Sustained improvement will require vigilance in the event of a second-peak.
References
1. Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N Engl J Med. 2020 Jul 9;383(2):120–8.
1.19. Pulmonary function in this era of Aerosol generating procedures!
A. Livingstone1, K. Smyth1, M. McCaul1, S. Moan1, E. Hayes1,
1 Department of Respiratory Medicine, Daisy Hill Hospital, Southern Health & Social Care Trust
In 2019, a novel coronavirus was identified and a global pandemic was declared in March 2020. Aerosols generated by medical procedures are one route for the transmission of the COVID-19 virus. Pulmonary function tests (PFTs) are considered an aerosol generating procedure (AGPs) (1) and this has had a significant bearing on service delivery.
Comprehensive needs assessment was undertaken to measure what changes were required to allow the provision of PFTs to continue safely. Retrospective data analysis of waiting times and influence on patient care pre and post introduction of changes has been collected.
The number of air changes per hour required was assessed to be 6. This led to adjustments being made to our extraction and filtration systems. Alterations were also made to PPE recommendations and cleaning procedures. These changes in procedure have reduced the capacity of the PFT laboratory and have led to a significant increase in waiting times.
Improvements to current protocols are allowing us to perform PFTS in a safe manner. This will enable us to provide a comprehensive service to our patients once again. Impact of increased waiting times can be lessened with adjustments to work practices.
References
1. Irish Thoracic Society/IICMS Guidance on Lung Function Testing: SARS COVID-19 Infection. V3
1.20. Clinical characteristics of Coronavirus 2019 positive patients admitted to a district General Hospital.
O. Nic Grianna1, H. McGurk1, M. McCloskey1, R. Sharkey1, M. Kelly1, C. King1 and P. McShane1
1 Respiratory department, Altnagelvin Area Hospital, Derry, Northern Ireland
The aim of this study is to describe clinical characteristics, outcomes and demographics of patients admitted to Altnagelvin Area Hospital with coronavirus 2019 (Covid-19) to help better prepare for second wave.
This is a Retrospective study of 95 adult patients requiring admission between the 16th of March 2020 and 30th of June 2020 and diagnosed with Covid-19. 95 patients had severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection confirmed with polymerase chain reaction testing of nasopharyngeal or sputum samples. Data was collected from electronic medical records and medical notes of the 95 patients.
Clinical features of confirmed covid-19 patients in Altnagelvin Area Hospital
| SEX | |
| Male | 54 |
| Female | 41 |
| AGE | |
| 18-39 | 7 |
| 40-49 | 16 |
| 50-59 | 14 |
| 60-69 | 15 |
| 70-79 | 21 |
| 80-89 | 19 |
| 90-99 | 3 |
| PRESENTING FEATURES | |
| Short of breath (SOB) | 63 |
| Pyrexia | 53 |
| Cough | 61 |
| Other respiratory (Haemoptysis/chest discomfort) | 2 |
| General malaise | 20 |
| Neurological (headache/seizures/reduced GCS/weakness) | 15 |
| Gastrointestinal (Abdominal pain/nausea/vomiting/loose motions) | 12 |
| ENT (anosmia/sore throat/runny nose) | 8 |
| Fall | 7 |
| Other (Haematuria/suicidal/renal failure) | 4 |
64% were hypoxic and of those 38% required greater than 10 litters of oxygen (>10L-O2). 8 patients required continuous positive airway pressure (CPAP), 5 were invasively ventilated and 3 were placed on high flow nasal cannula (HFNC). All except 1 patient requiring >10L-O2 that wasn’t ventilated or placed HFNC died. The mean length of stay (LOS) in days for non-hypoxic patients, 5.9, >2L-O2: 9.6, >10L-O2: 6.4, HFNC: 11, CPAP: 13 and invasive ventilation: 24.
This study showed a prolonged LOS for patients that were invasively ventilated, whilst the need for CPAP had a LOS close to half that of invasive ventilation.
1.21. Clinical characteristics of COVID-19 deaths at Tallaght University Hospital (TUH)
O Omar1, E McCarthy1, K Mullan1, M Kooblall1, S Lane1, E Moloney1
1 Respiratory Department, Tallaght University Hospital
COVID-19 represents a major threat globally. We present the clinical characteristic of patients that died from COVID-19 at TUH.
Out of the 305 patients who were diagnosed with COVID 19, 69(20%) died between March and July 2020.
The median age of the patients who died was 77 years.52.2% were males. 11.6% were admitted to the ICU, 10.1% were ventilated. The most common symptoms were fever and cough. Pneumonia and acute respiratory failure were the direct cause of death in 37 patients, and 25 patients had other causes of death in conjunction with COVID. 61 patients had evidence of infective changes on their admission chest X-ray (CXR). Lymphopenia was present in 72.5% of the patients on admission. D-Dimer done in 53 out of the 69 patients was elevated. Interleukin-6 was only done on 18 patients and was elevated in all of them. Procalcitonin was raised on 34 patients (49.3%).
22.6% of all confirmed COVID-19 cases in TUH died, mostly elderly frail patients, more male than female with severe disease and radiological findings on their CXR and 8 were admitted to ICU.
1.22. Respiratory Multidisciplinary Team Approach to COVID-19 in Our Lady of Lourdes Hospital, Drogheda, Co Louth
Rosaleen Reilly1
Our Lady of Lourdes Hospital, Drogheda, Co Louth 1
The first case of COVID-19 presented to Our Lady of Lourdes Hospital (OLOLH) on 11th March 2020. The 31 bedded Respiratory Ward was designated as the COVID-19 ward receiving patients who were deemed suitable for escalation to ICU.
In total 89 patients (from March to July) who were COVID-19 swab positive or CT positive were treated on the Respiratory Ward. Of these 29% (n26) required CPAP, 7.8%(n7) were treated with Optiflow and 4.49%(n4) BiPAP. Fourteen percent (n13) required ICU and there were 5 deaths (n5.6%).
The Multidisciplinary Respiratory Team merged to manage this caseload including working outside of traditional roles. The team was led by 2 Respiratory Consultants and 1 Infectious Disease Consultant. In addition to a clinical work load one respiratory consultant worked with the senior management team and the other respiratory consultant worked with ICU consultants to lead the Critical Care Response. There were daily morning handovers with the CNM2 to the team which included Consultants, NCHDs, ANPs, CNS, CNM3 and Allied Health professionals. In addition, the physiologist and CNS set up and managed an equipment room in which the NIV/Optiflow/Aerogen equipment was centrally ordered, stored, logged and delivered to requesting wards with details for setup. Remote Monitoring and Virtual Pulmonary rehabilitation was managed by the COPD Outreach physiotherapist and CNS.
1.23. Differential diagnosis of Covid-19 infection in Cork University Hospital: Review of Actual Diagnosis in Covid-19 negative patients.
Walsh LJ1, McElduff E1, Kennedy MP1
1. Department of Respiratory Medicine, Cork University Hospital, Cork
Covid-19 has led to a radical change in the way we practise acute hospital medicine. Suspected COVID-19 cases require isolation and a nasopharyngeal swab which is putting pressure on our hospital systems.
To establish the underlying diagnosis of suspected but ultimately negative COVID-19 cases and if the patient was appropriately placed on the COVID-19 pathway. We aim to better understand non-covid presentations to an acute hospital during a pandemic. A retrospective analysis of all admissions documented as suspected COVID-19 was carried out using Cork University Hospital’s online system to review discharge summaries (n=402). Patient demographics, symptoms, investigations, and length of stay were collected and analysed.
There was an average of 4.37 suspected COVID-19 cases per day. 74.6% of swabs were taken due to respiratory symptoms. 90.8% of patient were correctly placed on the COVID-19 pathway. The average length of stay was 8.7 days. In total, 64.5% of patients had a final diagnosis of a respiratory illness.
Those who are admitted with suspected COVID-19 have a huge impact on inpatient numbers and the availability of isolation rooms. In CUH, there was 283 more respiratory related admissions over a 3-month period in 2020 compared with the same period in 2019.
1.24. Splenic Infarcts and Pulmonary Emboli: The Thromboembolic Potential of Pulmonary Covid-19 Infection
Elkholy K1, Gabr A2, McEvoy N2, Ali O2, O’Keeffe D1, O’Connor M1
1 Respiratory/Hematology/Geriatric/Internal Medicine Departments, University Hospital Limerick, Limerick
2 Clinical Pharmacology Department, St. James’s University Hospital, Dublin 8
We report a case of pulmonary Covid-19 infection unusually presenting with acute splenic infarcts and pulmonary emboli. We believe this is potentially among the first published cases to include contrast-enhanced imaging of splenic infarcts in this condition. There is a growing body of published evidence that complications of Covid-19 are not limited to the pulmonary system. [1,2] To our knowledge, this is the first reported clinical image case of pulmonary Covid-19-related splenic infarcts.
During these unprecedented and overwhelming times of uncertainty of disease manifestations, clinicians of all specialties including our surgical colleagues should be aware of a wide range of thrombotic and disease spectrum manifestations of pulmonary Covid-19 infection to include splenic infarctions in the differential diagnosis of an acute abdomen.
References
1. Zhang Y, Xiao M, Zhang S. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. New England Journal of Medicine 2020;382:e38
2. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with Covid-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–62
1.25. The effect of the COVID-19 pandemic on CTPA use in an academic medical centre
Brian Gaffney1, John Duignan2, Finbarr Conroy1, Peter Conlon1, Evelyn Lynn1, Marcus W. Butler1,3, Michael P Keane1,3, Jonathan D Dodd2, David J Murphy2, Alessandro N Franciosi1, Cormac McCarthy1,3
1 Department of Respiratory Medicine, St. Vincent’s University Hospital, Elm Park, Dublin 4, Ireland
2 Department of Radiology, St. Vincent’s University Hospital, Elm Park, Dublin 4, Ireland
3 School of Medicine, University College Dublin, Dublin 4, Ireland
COVID-19 profoundly affected healthcare services and their utilisation. It has been hypothesised that COVID-19 is associated with increased risk of pulmonary embolism(PE). We assessed how COVID-19 pandemic affected CTPA utilisation and if more PE were diagnosed in COVID-19 positive patients
Data for patients who underwent CTPA between January-May 2020 were analysed, including; age, sex, COVID-19 status, WCC, CRP and D-dimer. COVID-19 status was coded as Non-COVID pathway(NC), SARS-CoV-2 negative(NEG), and SARS-CoV-2 positive(POS). Data was analysed using RStudio.
454 patients were included. More CTPA scans were performed in the second month of the pandemic(n=158) compared to the initial month(n=95). Prevalence of CTPA-defined PE (17.4% vs 14.9% vs 13.6% for POS/NEG/NC respectively, p=ns) and adjusted odds of PE (OR 1.16[95% CI; 0.45-3.0] and 1.21[95% 0.21-7.03] for NEG and POS respectively vs NC] did not differ between groups . Interestingly, SARS-CoV-2 POS patients with negative CTPA had significantly lower D-dimers (median=0.75[0.65,0.97]) compared to NEG or NC patients (median.91[0.42, 1.52] & 1.04[0.69,1.57] respectively, p=0.032).
The purported increased risk of PE in COVID-19 possibly resulted in an increase CTPAs performed as the pandemic evolved. Interestingly there was no increase in PE incidence and paradoxically COVID-19 patients were scanned with lower D-dimers.
1.26. Preference for blended learning approach to non-invasive ventilation education
Healy S1, Hallahan A1, O’Grady M1, Fitzgerald AM1, Murphy DM2, Henry MT2.
1. Physiotherapy Department, Cork University Hospital. 2. Respiratory Department, Cork University Hospital
During the initial stages of COVID-19, an unprecedented number of patients on non-invasive ventilation (NIV) were anticipated. Attendance at NIV class based education sessions in Cork University Hospital (CUH) has traditionally been suboptimal. After action reviews identified lack of knowledge as a risk in operating NIV machines. The anticipated exponential increase in number of patients requiring NIV resulted in novel engagement in education. This pilot project aimed to evaluate the addition of educational NIV videos to traditional class-based sessions.
Class based theory and practical sessions were provided and educational practical videos were developed by physiotherapists. The videos were circulated to all doctors and physiotherapists via WhatsApp groups to enable point of care access to local NIV information. A survey monkey questionnaire evaluated this format of NIV education.
Table 1. Class-based education attendance and questionnaire results
| Demographics | Doctors | Physios | |
| Class attendance | 225 | 39 | |
| Questionnaire response rate | 29 (9%) | 28 (70%) | |
| Education format | Preferred education format (%) |
Class based:93% Videos:22% |
Class based:92% Videos:29% |
| Preferred resource for out of hours |
Videos:74% Laminates: 59% PPG 33% |
Videos :75% Laminates: 78% PPG: 25% |
|
| Knowledge | Confident in NIV set up (Yes/No %) | 59% / 18% | 75% / 14% |
| Aware of NIV storage location | 72% | 100% | |
| Appropriate indications | 100% | 96% | |
| Appropriate initial settings | 80% | 96% |
Despite high attendance at NIV education sessions, the response rate to the questionnaire by doctors was low despite various strategies to improve this. Completing the evaluation at practical classes may yield higher response rates. Class based education was the preferred format of training but videos were the preferred resource for local information out-of-hours. This highlights the value of using technology to supplement the traditional class based approach to NIV education.
1.27. Pulmonary embolism diagnosis during an emerging pandemic: A comparison of pandemic to pre-pandemic practice.
S Garvey1, PJ Kerr1, R Lee1, RK Morgan1, ME O’Brien1.
1. Dept of Respiratory Medicine, Beaumont Hospital, Dublin 9.
Venous thromboembolism and pulmonary embolism (PE) are now recognised complications of SARS-CoV-2 infection in hospitalised patients1. A high clinical suspicion for PE must be maintained due to poor discriminant utility of d-dimer and Well’s score in COVID-19 disease. Our objective was to determine if there was a difference in diagnosis of suspected PE during the early phase of the COVID-19 pandemic in our centre compared to usual practice.
A retrospective audit of CTPA orders and results from 13th March–23rd April 2020 was compared to the same time period in 2019. Data in relation to COVID-19 diagnosis, Well’s score, sPESI score, cardiac biomarkers, presence of right-heart-strain by echocardiogram/CT evaluation were gathered.
During the early pandemic phase, 23 % fewer CTPAs were performed compared to 2019 (103 vs 134). There was no significant difference in positive CTPA studies between study periods (19% vs 16%, P=0.49). CTPA-case positivity in patients with COVID-19 was 39 % (9/24), which may reflect emerging knowledge of the complication.
In conclusion, we noted a significant reduction in CTPAs performed in 2020 compared to 2019. Factors including reduced ED presentations, reduced surgical caseload, and absent preceding knowledge of thromboembolic complications of COVID-19 may be contribute to this finding.
No conflict of interest/financial support disclosure.
References
1. Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N Engl J Med. 2020 Jul 9;383(2):120–8.
1.28. An overview of the establishment and delivery of a Virtual Pulmonary Rehabilitation Programme in Cork University Hospital for patients following COVID 19 infection.
O’Grady M1, Bowen B1, Sadlier C2, Plant BJ1, Kennedy M1, Henry MT1, Murphy D1
1 Department of Respiratory Medicine, Cork University Hospital
2 Department of Infectious Diseases, Cork University Hospital
COVID- 19 survivors can have subsequent deconditioning and chronic lung damage leading to breathlessness. Given the need for social distancing, many services have enhanced clinical management utilising technology. We sought to use technology to implement a virtual pulmonary rehabilitation (VPR) programme for patients hospitalised with COVID-19.
Although evidence for rehabilitation following Covid -19 is limited, PR is established as a key management strategy in the treatment of people with chronic respiratory disease. PR reduces symptoms, increases function and improves QoL in individuals with respiratory disease.
A 6 week exercise and educational programme was designed and provided to 8 participants, who had been hospitalised with COVID -19. Median age was 54 years. Pre and post programme assessments, including 1 min STS, HADS, FSS (Fatigue Severity Scale) and MMRC, were completed. Post programme spirometry was carried out and a programme evaluation form was completed.
To date, 7 participants have completed the course. Although not statistically significant, 86% of participants 1min STS improved by ≥ 3 RPM, FSS score improved in 86%. FEV1 was ≥90% predicted in 71% of participants and 72 % reported that they favoured a virtual over face to face programme. This data demonstrates the feasibility of VPR in this population.
1.29. A Review of the Supported Discharge Service for COVID-19 Patients Following Admission to Cork University Hospital
O’Grady M1, Martin L1, Sweeney AM2, Walsh M2, Plant BJ2, Kennedy M2, Sadlier C3, Henry MT2, Murphy D2
1 Physiotherapy Department, Cork University Hospital
2 Department of Respiratory Medicine, Cork University Hospital
3 Department of Infectious Diseases, Cork University Hospital
A cohort of patients admitted to CUH with COVID-19 were identified as being appropriate for a supported discharge service.
Patients were educated on home pulse oximetry and uploaded SpO2, HR and breathlessness scores onto the PatientMpower application. A physiotherapist reviewed the data daily, phoned the patient and gave advice on exercise, oxygen management, pacing, energy conservation and secretion clearance. A patient satisfaction questionnaire was completed following discharge from the service.
Over 12 weeks, 15 patients had a supported discharge. Readings were monitored 385 times and 176 phone calls were made. Advice was provided on exercise 32 times, oxygen 22 times and secretion clearance 7 times. 58 SpO2 readings were recorded outside the acceptable range and a re-admission was triggered for three patients (20%) for inpatient management. 100% of questionnaire respondents reported that the service met their needs and 90% agreed that the service had a positive effect on their recovery. 88% of the respondents who had received daily phone calls felt that this was more helpful than the objective monitoring aspect of the service.
A supported discharge service including remote monitoring and regular contact with healthcare professionals can facilitate timely, safe and successful discharges of select patient groups.
1.30. A Review of the Respiratory Service in the University Hospital Limerick during a Pandemic
Cullinan, M.1, Ryan, P.1, Ryan, N.1, Kokina, L1., Gleeson, E.1, Julian, N.1, McGrath, C.1, Roche, C.1, O’Brien, A1.
1 Respiratory Department, University Hospital Limerick, Limerick.
Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome is an on-going global health emergency. This pandemic became a reality for UHL in March 2020. Here we discuss the respiratory service and how the respiratory department managed the challenges during a pandemic. Reconfiguration of the respiratory service was central to an ongoing service in challenging times.
The aim of this review is to explore the changes that were made to deal with the pandemic and how this impacted the ongoing respiratory service.
A retrospective review of what was required to manage Covid 19 outbreak within UHL. The respiratory nursing service which consisted of CNS x 3 and RANP x 1 following initial redeployment were given the task of managing educating all healthcare workers with safe practices in managing non-invasive ventilation and oxygen. While ensuring strict infection control guidelines and evolving Covid 19 guidelines. Identification of the safest and highest quality systems for delivering non- invasive ventilation (NIV) which required modification of NIV and AIRVO masks and circuits. This involved investigating and sourcing consumables such as appropriate viral filters to protect the healthcare worker by the respiratory nurse service. Careful consideration of hospital oxygen supply and demand had to be reviewed daily to ensure supply and availability in the system.
820 healthcare workers were upskilled and educated on the practice of non-invasive ventilation and safe administration of high flow oxygen. Clear guidelines were created in conjunction with the ITS guidelines and accessible to all healthcare workers within UHLG on a local platform. Respiratory outpatients continued throughout the pandemic with a lot of the practice on a virtual platform.
Overall, healthcare workers were up skilled and practiced safe administration of non-invasive ventilation and high flow oxygen administration during a pandemic in clinical areas where this practice was unknown. A new and evolving service has being identified to ensure respiratory service continue.
1.31. Patient Demographics & Outcomes in the 1st Wave COVID19 Pandemic within the SHSCT.
Jamie Brannigan1, Conor McCullough1, Orla Thompson1, Debbie Cullen1,Rory Convery1
1 Craigavon Area Hospital, County Armagh, BT63 5QQ.
Craigavon Hospital was the designated Covid19 centre for the Southern Trust in NI (pop. 380,000). A comprehensive database of all admissions was set up by furloughed medical students & we have analysed the figures up until the 30th June.
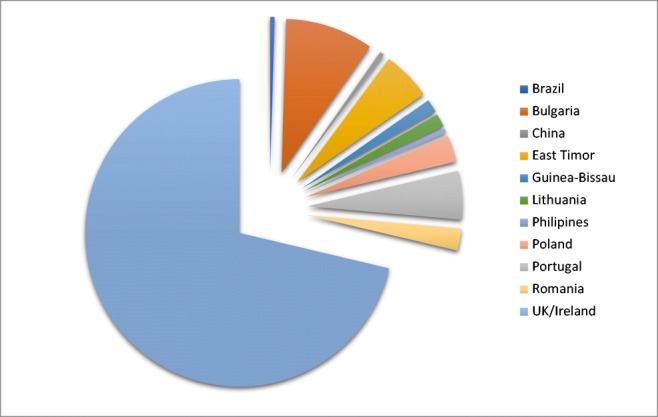
Demographics: 217 patients required inpatient care (122male) with mean age 62.8 (M=F). 63 (29%) of patients were non-NI born with a mean age of 48.4 vs. 68.8 for NI born (p<0.001).
Length of stay was significantly lower for minority groups (8.74 vs 11.9 days) and for females (9.4 vs 12.4). 10 of the minority cohort were diabetic (Type 2) compared to 36 of the NI group (1 minority vs 3 NI T1DM). 25 ICU admissions were documented (10 non-NI born)
Outcomes: 39 (36NI) deaths occurred within 30 days of admission (8 in ICU) with 31 on the Respiratory wards (8 on NIV). Relative mortality for the minority group was 0.048 vs. 0.23 for NI born (0.33 for NI males)
1.32. Factors influencing COVID-19 incidence in the counties of the Republic of Ireland: a population based observational study.
D. O’Malley1, E.F. McKone1
1 Department of Respiratory Medicine, St. Vincent’s University Hospital, Dublin.
The incidence of COVID-19 in counties across Ireland is highly variable. We carried out an observational study looking at the influence of socioeconomic status (SES) and healthcare variables on COVID-19 incidence across counties in the Republic of Ireland.
Outcome was total case rates per county from data.gov.ie over a 128 day time period from February 27th 2020.1 County-level measures of SES were obtained from the 2016 census. Data on numbers of carers, doctors per capita and nursing home beds were obtained from Medical Council and HIQA registries.
Linear regression was used to assess for association. Multivariate analysis identified a statistically significant association between COVID-19 case rates and mean household income (after adjusting for county mean house price), percentage of black/asian ethnicity and number of GPs per 1000.
This study reveals that socioeconomic status and measures of healthcare delivery are associated with a county’s COVID-19 incidence.
1 Rialtas na hÉireann/Government of Ireland. Ireland's COVID-19 Data Hub. https://covid19ireland-geohive.hub.arcgis.com/ (accessed 25th August 2020).
1.33. An audit of sputum culture test in patients admitted to a county hospital with community acquired pneumonia.
MK. Rana1, A Rafi1, M Muzamil1, S. Rizvi1
1 Mayo University Hospital Castlebar.
The British Thoracic society guidelines suggest that microbiological investigations including blood cultures, sputum cultures, pneumococcal urine antigen and pleural fluid microscopy if present, should be performed in patients with moderately severe community acquired pneumonia.
The aim of the audit was to identify whether sputum culture investigation is being performed as per BTS guidelines in Mayo university hospital Castlebar in patients with community acquired pneumonia. Retrospective data was collected for patients admitted with community acquired pneumonia in October 2019.
Out of 57 patients diagnosed with community acquired pneumonia, 47 had radiological confirmed pneumonia. Sputum culture was sent in 11 patients out of which organisms were isolated in 6 patients. 3 patients were positive for E Coli, 1 for both E Coli and Pseudomonas, 1 for Pseudomonas and 1 patient had positive sputum culture for Citrobacter farmer.
This audit showed poor adherence to BTS guidelines for testing of sputum culture in moderate to severe community acquired pneumonia. All medical teams were updated about BTS guidelines for microbiological investigations needed in the management of moderate to severe community acquired pneumonia and re audit should be performed.
IRISH THORACIC SOCIETY ORAL PRESENTATIONS I
1.1.1. Pulmonary Embolism and COVID-19; a single centre review.
AM Farrell1, LJ Walsh1, S Gregg1, A Barry1, BJ Plant1, MT Henry1, MP Kennedy1, JE Eustace2, C Sadlier3, M Crowley4, DM Murphy1,2
1 The Department of Respiratory Medicine, Cork University Hospital, Cork, Ireland
2 The HRB Clinical Research Facility, University College Cork, Cork, Ireland
3 The Department of Infectious Disease Medicine, Cork University Hospital, Cork, Ireland
4 The Department of Haematology, Cork University Hospital, Cork, Ireland
There is increasing concern amongst clinicians of a possible increase in venous thromboembolism (VTE) events in patients with COVID-19 pneumonia. There remains limited data defining the incidence of VTE in this population and thus also a paucity of research examining the impact of targeted treatment in patients with thrombotic complications of COVID-19.
We examined the number of symptomatic VTE events amongst proven COVID-19 pneumonia patients admitted to our institution, a tertiary level academic hospital, over a one month period from 23rd March 2020 to 23rd April 2020. Patient characteristics, admission and discharge inflammatory and coagulation markers were included in the analysis.
61 patients were identified, with a male predominance at 61%. All patients were commenced on thromboprophylaxis on admission. 12/61 (19.6%) of patients admitted with COVID-19 were treated for a suspected PE. Of these patients, 3 patients were discharged on anticoagulation, in the form of apixaban, 3 died and 6 remain inpatients.
COVID positive patients with disease severe enough to have warranted admission to an acute hospital are at increased risk of VTE and that this risk may extend beyond the period of admission. Further research examining the role of extending the duration of anti-coagulation in COVID-19 patients beyond hospital discharge is now warranted.
1.1.2. Persisting Symptoms in COVID-19: A First Look
C Leneghan1, J O’Connor1, G Almadhi1, T Hassan1, I Counihan1
1 Respiratory Department, Our Lady of Lourdes Hospital, Drogheda, Co Louth
Acute symptoms of Coronavirus disease (COVID-19) commonly include cough, fever, dyspnoea, musculoskeletal symptoms (myalgia, joint pain, fatigue), gastrointestinal symptoms, and anosmia/dysgeusia1. However, there is a paucity of data on long-term effects. We assessed persistent symptoms in patients who were discharged from hospital following COVID-19.
72 patients admitted to Our Lady of Lourdes Hospital, Drogheda with COVID-19 were followed up in post-COVID recovery clinic.
81% of patients had complete resolution of their chest radiograph. However 82% of patients reported persisting symptoms including fatigue (73%), shortness of breath (69%), dizziness (42%), palpitations (41%), hair-loss (40%), atypical chest pain (24%), myalgia (21%), insomnia (21%) and headaches (21%). Four patients were referred to the Department of Psychiatry due to possible diagnosis of post-traumatic stress syndrome using Breslau’s Short Screening Scale. Nine pulmonary function tests performed revealed normal spirometric pattern in all cases however, impairment of diffusion capacity was observed in 6 cases with a mean DLCO of 78% (SD). Raised D-dimer after 2 months correlated with persistent symptoms (HR 3.42, 95% CI 2.41-6.57) and >2 symptoms (HR 2.23, 95% CI 1.8-4.12).
This study emphasised the need for integrated multi-disciplinary follow-up of patients after discharge and highlighted the potential long-term health impacts of COVID-19.
References
1. Docherty AB, Harrison EM, Green CA, et al; ISARIC4C Investigators. Features of 20 133 UK patients in hospital with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369:m1985
1.1.3. CoViD-19 at home: A Safety Study for the Remote Home Monitoring of Patients with Novel SARS-CoV-2
S O’Brien1, L Townsend2, C Bannan2, G Courtney2, P Coss3, G Garvan4, AM McLaughlin1, P Nadarajan1
1 Department of Respiratory Medicine, St James’ Hospital, Dublin
2 Department of Infectious Diseases, St James’ Hospital, Dublin
3 Respiratory Laboratory, St James’ Hospital, Dublin
4 IMS Department, St James’ Hospital, Dublin
CoViD-19 is a disease caused by the novel coronavirus SARS-CoV-2 and has a significant impact on healthcare systems worldwide. It places a tremendous burden on hospital bed capacity and in certain countries, has overwhelmed the entire healthcare system, contributing to significant mortality rates from the disease. An early discharge pathway was initiated by HSE with remote monitoring of patients with mild to moderate CoViD-19 disease. We carried out a safety and feasibility evaluation of this supported discharge pathway.
We retrospectively analysed all patients who were enrolled into this pathway. After initial assessment, suitable patients are discharged within 24 hours of presentation to hospital with an oxygen saturation monitor. Oxygen saturation is checked twice daily and this information along with the heart rate is recorded on to the application on the patient's smart phone. This information is then available for review by a remote monitoring team consisting entirely of healthcare staff. A drop in oxygen saturation level below 93% is considered significant and an early indication of deterioration, at which point a text alert is sent to the medical consultant on call. The patient is then contacted by phone and if appropriate, advised to self-present to the Emergency Department for a medical re-evaluation. We evaluated the readmission rate to hospital and the number of unexpected deaths in patients on this pathway.
71 patients were enrolled into the early discharge pathway. Patient demographics are listed in Table 1. Readmission rate to hospital was 4.2%. There were no deaths recorded in this patient group. The average initial length of stay in hospital was 1.9 days and the average number of phone calls made to patients was 1.1 calls per patient.
In conclusion, the early discharge pathway is a safe discharge option that significantly reduces hospital LOS, thus protecting the healthcare system during this pandemic.
Table 1. CoViD-19 Early Discharge Pathway Patient Demographics
| Total patients (n) | 71 |
| Male | 26 (36.6%) |
| Female | 45 (63.4%) |
| Average Age (yrs) | 40.8 |
| Median Age (yrs) | 40 (20-72) |
| Average Age Female (yrs) | 39.7 |
| Average Age Male (yrs) | 42.6 |
| Smoking status | |
| Current | 1 |
| Ex-smoker | 9 |
| Never smoked | 59 |
| Not recorded | 2 |
| Chest X-Ray Result | |
| Normal | 17 |
| Abnormal | 18 |
| Not done | 36 |
| Readmissions | 3/71 (4.2%) |
| Deaths | 0 |
| Average initial LOS in hospital (days) | 1.9 |
| Average no. of phone calls to patient | 1.1 |
n= number of patients; yrs= age in years
Table 2. Inclusion criteria for Early Discharge Pathway
|
• CoViD-19 swab positive • Patient must be able to self-isolate • Age > 18 • Patients must have an email address and a smartphone with data • Patient must be able to communicate in English • Patient must live within the catchment area • Initial oxygen saturations >94% on room air • Initial respiratory rate < 20 breaths per minute |
1.1.4. Clinical characteristics, disease course and outcome of the first 117 hospitalised patients with COVID-19 pneumonia in a Dublin hospital: a single-centre descriptive study
O’Regan, R; Harnedy, F; Reynolds, B; Cormican, L.
Respiratory Department, Connolly Hospital Blanchardstown, RCSI Hospital Group, Dublin
Between 11th March-22nd May 2020, 281 patients were admitted to Connolly Hospital Blanchardstown with confirmed SARS-CoV-2 infection. In this study, we aim to describe the epidemiological, clinical, imaging and laboratory characteristics, treatment course and subsequent outcomes of the first 116 cases presenting to our hospital.
Clinical data on inpatients with COVID-19 pneumonia between March 11th to 22nd May 2020 was collected. The epidemiological characteristics, clinical features, laboratory findings, radiological manifestations, treatment course and clinical outcomes of 116 of these patients were recorded and analysed.
Of 281 inpatients, 201 were discharged (71.5%) and 52 died (18.5%) in hospital at time data collection ceased. Of 116 cases analysed, 100 patients presented from the community, 6 from care homes and 10 were existing inpatients. 54 patients were of a non-Irish White or Black, Asian or minority ethnic (BAME) population (46%). 114 patients reported two or more symptoms at time of diagnosis with 81 (70%) patients having confirmed radiological findings (73%). The majority of patients admitted had one or more co-morbidity. 26 patients (22%) required ICU admission.
The COVID-19 pandemic led to an unprecedented level of hospital admissions to Connolly hospital, at one point accounting for 20% of all Irish ICU admissions. Our hospital’s catchment area serves a wide ranging and diverse population group. Our experience of treating SARS-CoV-2 infection in this cohort was unique when compared to other Irish hospital settings. This work may serve as a reference for decision-making for epidemic prevention and control and guide decision-making for future outbreaks of SARS-COV-2 infection in in similar hospital settings.
1.1.5. Evaluating the Outcomes of an Integrated Multidisciplinary COVID-19 Recovery Care Clinic
Sile Toland1, Manuel Calvo Gurry1, Sean Collins, Helen O’Brien1, Michael J Tracey2, Ciara Ottewill1, Michael E O’Brien1, Ross K Morgan1, Richard W Costello1,3, Cedric Gunaratnam1, Daniel Ryan1, Noel G McElvaney1,3, Samuel J McConkey2,4, Cora McNally2, Gerard F Curley5, Siobhan MacHale6,7, Diane Gillan8, Niall Pender8,9, Helen Barry6,7, Eoghan de Barra2,4, Fiona M Kiernan5, Imran Sulaiman1, Killian Hurley1,3.
1. Department of Respiratory Medicine, Beaumont Hospital, Dublin, Ireland.
2. Department of Infectious Diseases, Beaumont Hospital, Dublin, Ireland.
3. Department of Medicine, Royal College of Surgeons in Ireland, Dublin, Ireland.
4. Department of International Health and Tropical Medicine, Royal College of Surgeons in Ireland, Dublin, Ireland.
5. Department of Anaesthesia and Critical Care, Beaumont Hospital, Dublin, Ireland.
6. Department of Liaison Psychiatry, Beaumont Hospital, Dublin, Ireland.
7. Department of Psychiatry, Royal College of Surgeons in Ireland, Dublin, Ireland.
8. Department of Psychology, Beaumont Hospital, Dublin, Ireland.
9. Department of Psychology, Royal College of Surgeons in Ireland, Dublin, Ireland.
In January 2020, the WHO declared the SARS-CoV-2 outbreak a public health emergency, by March 11th a pandemic was declared. To date in Ireland, over 3,300 patients have been admitted to acute hospitals as a result of infection with COVID-19.
We describe a single centre prospective cohort study which follows patients longitudinally with both virtual and in-person clinic. This clinic established in Beaumont Hospital is a multi-disciplinary service for comprehensive follow up of patients with a hospital diagnosis of COVID-19 pneumonia. This initiative is supported by respiratory, critical care, infectious diseases, psychiatry and psychology services. The comprehensive patient assessment included standardised blood tests, chest x-ray, quality of life scores and a novel mental health assessment tool.
400 patients were assessed with COVID-19, 174 patients discharged from Beaumont Hospital after COVID-19 pneumonia. 67% were male with a median age (IQR) of 66.5 (51-97). 22% were admitted to the ICU for mechanical ventilation, 11% had non-invasive ventilation or high-flow oxygen and 67% did not have specialist respiratory support. Early data suggested that 48% of these patients will require medium to long-term specialist follow-up.
Longitudinal follow up has predominantly revealed radiographic improvement of pneumonia, and in many cases complete resolution of bilateral infiltrates. However, cases of persistent infiltrates, myocarditis and ongoing physical and psychological sequelae of COVID-19 were identified.
IRISH THORACIC SOCIETY POSTER REVIEW AND DISCUSSION
2. Lung Cancer/ILD/CF/Thoracic Surgery and Transplant
2.1. The efficacy of Elexacaftor/Tezacaftor/Ivacaftor in patients with cystic fibrosis and advanced lung disease
O.M. O’Carroll1, K.M. O’Shea 1, C. Carroll1, B. Grogan1, A. Connolly1, L. O’Shaughnessy1, T. Nicholson1, C.G. Gallagher1,2, E.F. McKone1,2.
1 National Referral Centre for Adult Cystic Fibrosis, St. Vincent’s University Hospital, Dublin 4, Ireland.
2 School of Medicine, University College Dublin, Dublin 4, Ireland.
Elexacaftor/tezacaftor/ivacaftor (ELX/TEZ/IVA) has delivered transformative improvements to the lives of people with mild to moderate cystic fibrosis with at least one Phe508del mutation (1, 2). The effects of this drug combination are not yet well understood in patients with severe disease.
We conducted a single-centre observational study with a cohort of patients who received (ELX/TEZ/IVA) as part of a managed access programme if they had either severe lung disease (ppFEV1<40%) or were awaiting lung transplantation. Multiple outcomes were measured and compared with baseline data. Paired student T-test was used and a two-sided p-value of <0.05 was considered to be significant.
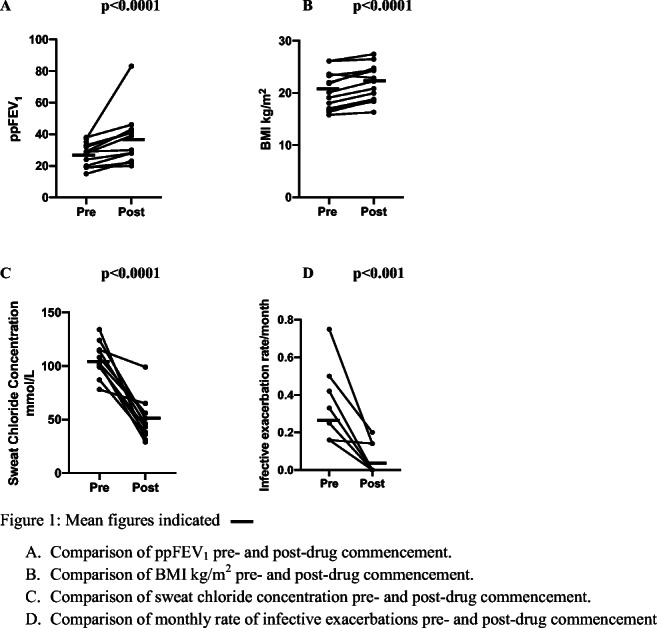
14 patients were included in this analysis. After treatment with ELX/TEX/IVA was initiated, ppFEV1 improved (27.3±7.3% vs 36.3± 16.5%, p<0.0001, n=14). BMI also improved (20.7±3.6 vs 22.1±3.4 kg/m2, p<0.0001) as did sweat chloride concentration (105.7±15.9 vs 50±19.8 mmol/l, p<0.0001). Infective exacerbations requiring hospitalisation reduced in frequency (0.28 ± 0.17 exacerbations per month vs 0.04 ± 0.07 exacerbations per month, p<0.001) (Figure 1).
This therapy is expected to greatly improve the disease trajectory for many CF patients with at least one Phe508del mutation and this expectation should also apply to those groups with more advanced disease.
References
1. Heijerman HGM, McKone EF, Downey DG, Van Braeckel E, Rowe SM, Tullis E, et al. Efficacy and safety of the elexacaftor plus tezacaftor plus ivacaftor combination regimen in people with cystic fibrosis homozygous for the F508del mutation: a double-blind, randomised, phase 3 trial. Lancet. 2019;394(10212):1940-8.
2. Middleton PG, Mall MA, Drevinek P, Lands LC, McKone EF, Polineni D, et al. Elexacaftor-Tezacaftor-Ivacaftor for Cystic Fibrosis with a Single Phe508del Allele. N Engl J Med. 2019;381(19):1809-19.
Figure 1: Comparison of outcome measures pre- and post- initiation of ELX/TEZ/IVA
2.2. Impact of the Covid-19 pandemic on pulmonary fibrosis patients, carers and healthcare professionals.
Cassidy N1, Fox L2, Brown L3, Galvin L1, O’Reilly K2.
1 The Irish Lung Fibrosis Association, Dublin, Ireland,
2 Mater Misericordiae University Hospital, Dublin, Ireland.,
3 St Vincent’s University Hospital, Dublin, Ireland.
The Irish Lung Fibrosis Association (ILFA) conducted an online/telephone survey from 16 April-5 May 2020 to determine Covid-19’s impact on Interstitial Lung Disease (ILD) stakeholders.
111 pulmonary fibrosis patients (43% female), 59 carers (86% female) and 49 healthcare professionals (HCP) (71% female) responded. 17% patients were diagnosed <1-year, 64% diagnosed 2 to 5-years and 19% diagnosed >5-years. 51% patients lived with a spouse/partner, 36% used oxygen and 66% took anti-fibrotics. 33% patients had a telephone consultation with their medical team since Covid-19 restrictions, 43% had tests postponed and 39% had results delayed. 83% patients and 88% carers were concerned about a patient’s ability to access urgent hospital care. 47% patients exercised less, 15% patients and 42% carers were financially worse off. 58% of carers, 23% patients and 29% HCP had poorer sleep quality. 42% carers were "extremely worried” compared to patients (32%) and HCP (6%). The mean level of worry for patients, carers and HCP was 7.4/10, 8.1/10 and 6.5/10 respectively. Patient and carer scores were significantly higher than for the general public (6.6/10)1. The advocacy priorities for stakeholders were having an ILD clinical care programme, improved pulmonary rehabilitation access and greater awareness.
Carers and patients experienced significant Covid-19 worry and may benefit from psychological support.
1 https://assets.gov.ie/73911/25d65090b992459783120064745187c6.pdf
2.3. Fungal Exposure and Sarcoidosis
G. Doran1; M. Nugdallah1; L. Davidson1; E Murtagh1; SC Donnelly2; P Minnis1
1Interstitial Lung Disease Service, Respiratory Medicine, Antrim Area Hospital, Bush Road 2Department of Medicine, Trinity Centre for Health Sciences, Tallaght Hospital, Tallaght, Dublin, Ireland
Possible initiation triggers of pulmonary sarcoidosis are intriguing. Particular attention has previously focused on M. tuberculosis and P. acnes.1+2There is limited literature in the role of fungi in the development of sarcoidosis, however it often complicates fibrotic disease. We examined cohorts of well-characterised patients from Leinster and Ulster. Both cohorts were similar in terms of demographics, mode of presentation, physiological impairment and need for treatment.
The Leinster cohort consisted of 338 individuals identified from a historical database and those attending clinic and managed by a single physician. 47 patients were enrolled prospectively, at the time of assessment, after undergoing skin prick testing (SPT) and were followed up for a median of 40 months. Of the patients who were positive 74% reacted to Grass, 48% to D Pteronyssinus and 26% to Aspergillus or mould mix. Positive SPTs had reduced uptake of standard therapy OR 0.21 (0.07-0.62), p =0.0051.
The Ulster cohort consisted of 242 patients attending a single specialised clinic. Serum aspergillus titres were available for 72. There was no significant difference in titre level when stratified for CXR stage (Figure 1). Initial analysis documented no significant correlation between systemic inflammation as measured by ESR and aspergillus titre (Rho -0.073).
There was no signal from this large group of individuals with sarcoidosis to suggest that Aspergillus drives sarcoidosis in terms of radiological disease severity or systemic inflammation but a suggestion that it may correlate to reduced treatment need.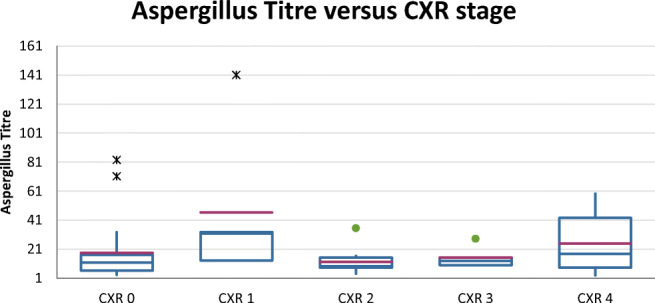
References
1. Gupta D, Agarwal R et al. Molecular evidence for the role of mycobacteria in sarcoidosis: a meta-analysis. Eur Respir J. (2007) 30:508-16.
2. Eishi Y. Etiologic aspect of sarcoidosis as an allergic endogenous infection caused by Propionibacterium acnes. Biomed Res Int. (2013) 93:52-89.
2.4. Patient characteristics of lymphangioleiomyomatosis in an Irish population.
E Lynn1, L Browne1, J Morrow2, A Sahadevan1,4, A Kelly1, A Fabre3,4, J.D. Dodd2, M P. Keane1,4, D.J. Murphy2, C McCarthy1,4
1 Department of Respiratory Medicine, St. Vincent’s University Hospital, Elm Park, Dublin 4, Ireland
2 Department of Radiology, St. Vincent’s University Hospital, Elm Park, Dublin 4, Ireland
3 Department of Pathology, St. Vincent’s University Hospital, Elm Park, Dublin 4, Ireland
4 School of Medicine, University College Dublin, Dublin 4, Ireland
Lymphangioleiomyomatosis (LAM) is a metastasizing neoplasm resulting in parenchymal destruction and cystic lung disease1. It has an estimated prevalence of 3-8 cases per million women2.
Data on patients with LAM attending our cystic lung disease clinic was analysed to characterise this cohort. Age, history of pneumothorax, mode of diagnosis, VEGF-D levels, PFTs, CT cyst scores and mTOR treatment was assessed.
Twenty seven females with LAM were included, 63% diagnosed radiologically, 22% with VEGF-D levels meeting diagnostic criteria and 15% with confirmed tissue diagnosis. Mean age was 50.52 years (range 27–81). 93%(n=25) were sporadic LAM, 67% were pre-menopausal. 26% (n=7) were treated with mTOR inhibitors. 30% had a history of pneumothorax, 14% chylothorax and 33% angiomyolipoma. 15% required long term oxygen. Mean VEGF-D level was 626pg/ml (+/-599.48). Mean DLCO and FEV1 were 64.52% (+/-27.35) and 85.7% (+/-16.05) respectively. VEGF-D inversely correlated with both DLCO (R2=0.4468, p=0.0034) and FEV1% (R2=0.3281,p=0.013)
LAM is a rare disease2, however correct diagnosis is important as it has implications for lifestyle modification and there is effective therapy available. With at least 27 patients identified in Ireland, this represents a prevalence of 11.2 per million women, and is likely higher than this both in Ireland and worldwide.
References
1. McCormack FX, Travis WD, Colby TV, Henske EP, Moss J. Lymphangioleiomyomatosis: calling it what it is: a low-grade, destructive, metastasizing neoplasm. Am J Respir Crit Care Med 2012: 186(12): 1210-1212.
2. Harknett EC, Chang WY, Byrnes S, Johnson J, Lazor R, Cohen MM, Gray B, Geiling S, Telford H, Tattersfield AE, Hubbard RB, Johnson SR. Use of variability in national and regional data to estimate the prevalence of lymphangioleiomyomatosis. QJM 2011: 104(11): 971-979
2.5. Defining the “F” in Fibroblast: a definitive identification of mesenchymal populations in the healthy and fibrotic lung
Simon C. Rowan1,2*, Xue Liu2*, Jiurong Liang2 Yizhou Wang3, Paul W. Noble2*, Dianhua Jiang2,3*
1 UCD School of Medicine, Conway Institute, University College Dublin, Belfield, Ireland.
2 Department of Medicine and Women’s Guild Lung Institute, Cedars-Sinai Medical Center, Los Angeles, CA 90048, USA.
3 Genomics Core, Cedars-Sinai Medical Center, Los Angeles, CA 90048, USA. and
3 Department of Biomedical Sciences, Cedars-Sinai Medical Center, Los Angeles, CA 90048, USA.
*These authors contributed equally.
Pulmonary mesenchymal cells are critical players in the pathogenesis of fibrotic lung diseases like Idiopathic Pulmonary Fibrosis. They are increasingly recognized as highly heterogeneous but a consensus on the subpopulations present in the lung, and discriminative for each subtype, remains elusive.
We completed scRNA-seq analysis, and re-analysis of publicly available datasets, of mesenchymal cells from the post-natal, adult and the aged fibrotic lungs of humans. We delineated the transcriptome of lipofibroblasts, myofibroblasts, pericytes, mesothelial cells, smooth muscle cells, and a novel population delineated by Ebf1 expression. Comparative analysis of murine and human lung mesenchymal cells revealed homologous subpopulations with conserved transcriptomic signatures.
We demonstrated that all mesenchymal sub-populations, not solely myofibroblasts, contributed to the expression of extracellular matrix genes in fibrosis. We did not observe evidence of transdifferentiation between fibroblast subtypes in fibrosis. Rather these data suggest that mesenchymal fate decision occur during embryonic development and the identified subtypes remain distinct into adulthood and in the aged healthy and fibrotic lung.
This analysis challenges long held beliefs on the contribution of fibroblast subtypes to fibrotic lung disease and provides a basis for definitive identification of the different mesenchymal populations in development, heath and disease.
2.6. Thoracic Surgical Oncology – Maintaining a High-Volume High-Quality Surgical Programme in Ireland during the Coronavirus Pandemic
R Weedle1, A Daly1, VK Young1, RJ Ryan1, GJ Fitzmaurice1
Department of Cardiothoracic Surgery, St James’s Hospital & The Blackrock Clinic, Dublin
Coronavirus caused unprecedented disruption to the delivery of healthcare services worldwide. Within Ireland, existing resources were realigned to primarily manage Covid-19 patients and consequently novel solutions were urgently required to maintain treatment strategies for time-sensitive non-Covid illnesses, including thoracic malignancies. The purpose of this study was to review the delivery of our thoracic surgical service during this pandemic.
A retrospective review was performed of a prospectively-maintained database of all cases performed between 25th March and 29th June 2020, when our elective surgical caseload transferred to the Blackrock Clinic. Patient demographics, operative details, and outcomes were collected. Qualitative analysis was performed using Microsoft Excel.
During this 13-week time period, 97 operative procedures were performed. Results are shown in table 1.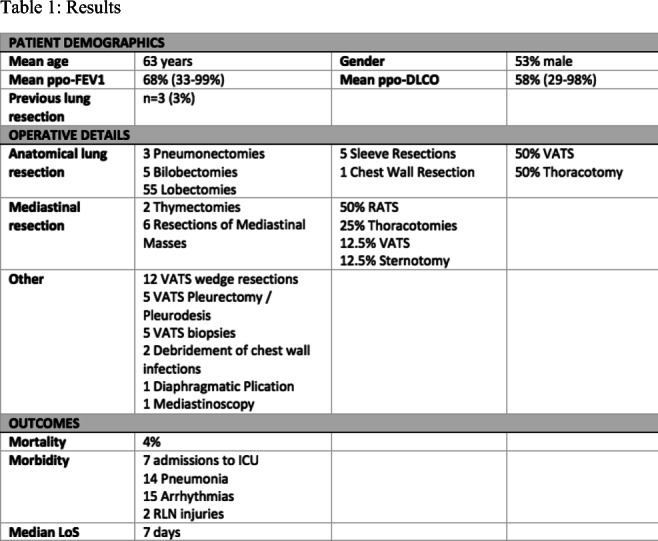
We instituted a strict admission pathway with the aim of establishing and maintaining a Covid-free environment. A rigorous anaesthetic and intra-operative protocol was established to limit aerosolisation risk. Post-operative management was based in individual patient rooms with a standardised recovery pathway. Overall case volume and mix was maintained with stable morbidity and mortality. This approach facilitated the maintenance of a ‘Covid-free’ high volume high quality thoracic surgical oncology programme during a time of unprecendented disruption to the Irish health service.
2.7. Complications of bronchoscopy in a major teaching centre.
W. Mahmood1, U. Khan1, O. Rahman1, MK. Rana1, A. O’Brien1
1 Respiratory Department, University Hospital Limerick, Limerick.
To evaluate frequency of complications associated with flexible fiberoptic bronchoscopy in a teaching center.
It’s a retrospective study.500 patients underwent flexible fiberoptic bronchoscopy with different pulmonary pathologies at University Hospital Limerick in last 6 months. There were 227 females and 273 males(mean age 55+/- 11). Bronchoscopies included 95 transbronchial biopsies (19%), 113 transbronchial needle aspirations (22.6%), 281 bronchoalveolar lavage (56.2%), 29 brushings (5.8%), 21 trans-tracheal biopsies (4.2%).
Total 13 patients suffered bronchoscopic complications (2.8%). Incidence of major complications secondary to transbronchial biopsy was 8 (1.6%), (including 6 pneumothoraces (1.2%), 2 with significant bleeding (0.4%)), 5 patient had complications secondary to endobronchial biopsies (0.8%) (3 pneumothoraces (0.6%), 2 with significant bleeding (0.4%)). Only 3 patients with pneumothoraces needed chest drain placement, the remainder were managed conservatively; bleeding complications were treated with cold saline +/- adrenaline during the procedure. All the patients who suffered pneumothoraces required hospital admission, duration of stay was 2 (+/-1) days and mortality rate was 0%.
This study shows that bronchoscopy is a safe method with low to moderate incidence of complications and mortality. We believe that preparation, experience and continuous training of trainees and nursing team play a fundamental role in reducing the incidence of complications.
Conflict of interest: None to Declare.
2.8. Uniportal Thoracoscopy linked to an Enhanced Recovery Programmeis Superior to Traditional Approaches in Management of Pleural Empyema
M Aladaileh1, M Ni Fhlatharta1, J Olaniyil1, R Brown1, KC Redmond1
1 Thoracic Surgery Department, Mater Misericordiae University Hospital, Dublin, Ireland
In recent years, there has been a paradigm shift in the management of patients presenting with pleural empyema towards minimally invasive modalities. Till today, few reports advocate uniportal-video assisted thoracic surgery (U-VATS) for decortication.
This is a single-centre retrospective analysis of 120 consecutive patients who underwent U-VATS decortication from Janaury 2015 to June 2019. The patients were divided into ERAS and non-ERAS groups.
The literature review demonstrated that a U-VATS approach was superior in outcomes to either a M-VATS or open thoracotomy approach.
In this study, the mean age of patients was 56 (range) years, 67% were males. Complete decortication was obtained in all patients through a U-VATS approach. Fifty patients (41.6%) presented with stage II and 70 patients (58.3%) stage III empyema. The mean length of hospital stay for all patients of 5.4±3.9 days, and the post-operative chest tube duration noted to be 5.1±3.6 days. Length of stay was significantly shorter in the ERAS group compared with the non-ERAS group (P-value 0.005).
U-VATS decortication should be the preferred initial approach to the treatment of stages II and III empyema. When U-VATS decorticationis aligned to an ERAS programme, outcomes are superior to all other treatment approaches.
Keywords: Enhanced recovery after surgery (ERAS); Uniportal video-assisted thoracic surgery (U-VATS); pleural empyema; decortication.
2.9. Audit: Retrospective Review of Time to Treatment Decision for Lung Cancer in the Saolta Group Over a 6 Month Period.
P. Ridge1; L. O’Loughlin1; D. Breen1
1Interventional Respiratory Unit, Galway University Hospital (GUH), Galway
Prompt diagnosis and staging of lung cancer is essential for improved patient outcomes1,2. Staging should be achieved with the least and most minimally invasive investigation1. The Lung-BOOST trial confirmed that the upfront use of EBUS for suspected lung cancer confined to the thorax reduced the time-to-treatment decision by half and was associated with increased survival compared with previous conventional diagnosis and staging2.
All cases of lung cancer are discussed through our lung MDM in GUH. This allowed us to audit if individual units were achieving the key performance indicator of time-to-treatment decision within 14 days of initial CT. This is a standard established by the Lung-BOOST trial and now recommended by the NHS National Optimal Lung Cancer Pathway.
A retrospective review of all the lung cancer cases discussed at our lung MDM from January to June 2018 was performed. All data was recorded and analysed using an anonymised and encrypted Microsoft Excel database.
Results:
| Site |
Time from index CT* to first Investigations (Days) |
Time Index CT to EBUS** (Days) |
Time from index CT to MDM*** (Days) |
Number of total Investigations (No.) |
|
GUH N=56 |
8.69 | 13.44 | 24.86 | 2.09 |
|
Hospital A N=3 |
21.33 | 18.5 | 29.67 | 1 |
|
Hospital B N=15 |
24.33 | 44.2 | 52.8 | 2.4 |
|
Hospital C N=19 |
22.05 | 26.25 | 40.37 | 1.69 |
|
Hospital D N=4 |
31.5 | 13 | 36.25 | 1.5 |
|
Other N=2 |
32.5 | 45 | 40.5 | 2 |
|
Saolta Group N=99 |
15.4 | 20.88 | 32.99 | 2.02 |
*CT: Computed Tomography
** Endobronchial Ultrasound
*** Multi-Disciplinary Meeting
GUH had a shorter mean time-to-treatment decision than other units. However no unit achieved the target of 14 days. This audit indicates a need for greater access to EBUS across the Saolta Group and a need for shortening the delay between index CT and EBUS.
References
1. BMJ, 2019. Lung cancer: diagnosis and management: summary of updated NICE guidance. p.l1514.
2. Navani N, Nankivell M, Lawrence D, Lock S, Makker H, Baldwin D et al. Lung cancer diagnosis and staging with endobronchial ultrasound-guided transbronchial needle aspiration compared with conventional approaches: an open-label, pragmatic, randomised controlled trial. The Lancet Respiratory Medicine. 2015;3(4):282-289.
Conflict of Interests:
None
2.10. Nindetanib and Pirfenidone, experience of a tertiary referral centre in the Republic of the Ireland
PK Coghlan1, E. Lim Man Yu1, MF Iftikhar1, L Al Haddah1, A O’Brien1
1Respiratory Department, University Hospital Limerick, Dooradoyle, Limerick
Idiopathic pulmonary fibrosis has a median survival time after diagnosis of 2–5 years. Pirfenidone and nintedanib are well established as first-line therapy in idiopathic pulmonary fibrosis (IPF). The purpose of our study was to look at objective data available to us for our IPF patients who had been started on targeted anti-fibrotic therapy and compare the experience.
We reviewed the charts and records of all IPF patients (162) who were treated with anti-fibrotic medication during the period between 1 December 2012 and 30 April 2020 and whose clinical and pulmonary function records were complete for at least a 12-month period.
After 1 year, lung function test parameters of patients treated with pirfenidone and nintedanib had remained stable from baseline with no significant differences in FVC, TLC and DLCO. Nindetanib outperformed pirfenidone in terms of exacerbation rate, radiological progression of disease and adverse drug events over the course of the treatment course evaluated.
This study emphasizes that both nindetanib and pirfenidone remain good therapeutic choices in slowing lung function decline albeit in the context of a disease with enduring mortality.
| Nindetanib (58 patients) | Pirfenidone | |
| FVC at 12 months | -3.77% (n=22) | -4.21% (n=54) |
| DLCO at 12 months | -4.9% (n=19) | -6.6% (n=51) |
| TLC at 12 months | -2.22% (n=18) | -6.2% (n=41) |
| Exacerbations per patient per 12 months | 0.93 (n=58) | 1.42 (n=97) |
| Radiological progression of disease | 31% (n=17) | 56% (n=35) |
| Mortality | 44% (since March 2016) | 58% (n=104) |
| Drug cessation | 13.8% (n=58) | 28% (n=104) |
| ADEs | 6.9% (n=58) | 14.4% (n=104) |
2.11. Pneumocystis Pneumonia in an Irish University Hospital Setting: A Five Year Review 2015-2020
Shinners, O1., Holmes, O1., Tyrrell, R1., Shahsavari, S1., Scott, A1., Khan, U1., Teoh, T.2, Powell, J.2 and O’Brien, A.1
1 Department of Respiratory Medicine, University Hospital Limerick, Dooradoyle, Limerick.
2 Department of Microbiology, University Hospital Limerick, Dooradoyle, Limerick.
Pneumocystis Pneumonia (PCP), an opportunistic infection, is caused by the atypical fungus Pneumocystis jirovecii. PCP is seen in patients with underlying immunodeficiency, cancer patients receiving treatment, transplant recipients and those on medications such as steroids and other immunosuppressants[1}.
This study aims to investigate the incidence of PCP over a 5 year period in a University Hospital and to identify the method of diagnosis and associated patient demographics.
PCP positive cases were extracted via the Laboratory Information Management System outlining patient age and method of diagnosis. A retrospective chart review was carried out on positive PCP cases examining; immunosuppressant status and type, relevant background history, prophylaxis status, treatment and associated mortality.
51 of 274 samples analysed were positive (18.61%). Method of diagnosis included; bronchial washings (62.75%), sputum (35.29%) and nasopharyngeal swab (1.96%). Of 46 patient charts subsequently reviewed; no patient was on prophylaxis at time of diagnosis, 50% were on immunosuppressing agents, 73.91% received treatment with Trimethoprim/sulfamethoxazole and a mortality of 26.08% was recorded. Most common underlying conditions included; malignancy (41.3%), respiratory disease (33.6%) and HIV (10.87%).
Over 5 years, an average of 10 PCP positive samples were identified per annum. Patients with underlying malignancy represent the largest cohort of cases.
References
1. Patterson, L., Coyle, P., Curran, T., Verlander, N.Q. and Johnston, J. Changing epidemiology of Pneumocystis pneumonia, Northern Ireland, UK and implications for prevention, 1 July 2011–31 July 2012. Journal of Medical Microbiology, 2017, 66;11
2.12. Trends in Empyema Requiring Decortication in the West of Ireland
A White, R Weedle, A Soo
Department of Cardiothoracic Surgery, University Hospital Galway
2.13. Biopsychological, physical activity and sedentary behaviour profile of adults with Cystic Fibrosis in Ireland
Curran, M.1,3, Tierney, AC.1,3,4, Collins, L.2, Kennedy, L.2, McDonnell, C.2, Jurascheck, A.J.1, Sheikhi, A.3., Button, B.4, Casserly, B.2, Cahalan, R.1,3.
1 School of Allied Health, University of Limerick, Limerick, Ireland
2 University Hospital Limerick, Limerick, Ireland
3 Health Research Institute, University of Limerick, Limerick, Ireland
4 Department of Dietetics, Nutrition and Sport, La Trobe University, Melbourne, Australia
5 Cystic Fibrosis Service, Alfred Health, Melbourne, Vic 3004
Sleep, wellbeing, and quality of life (QOL) are important considerations in Cystic Fibrosis (CF) management. Furthermore, physical activity (PA) should be optimised as it can improve patient health.
This observational study assessed sleep, wellbeing, QOL, and PA levels in adults with CF at University Hospital Limerick. Wellbeing was assessed by the Alfred Wellness Score (AWE), sleep quality by the Pittsburgh Sleep Quality Index (PSQI) and QOL using the CF Questionnaire-Revised (CFQ-R). PA and sedentary behaviour were assessed using an ActivPAL accelerometer which was worn for seven days.
33 participants (13M/20F; 26.2 ± 7.1 years) were recruited. Results indicated very good self-reported levels of wellbeing and QOL. Mean daily step count was 7788 (± 3583 SD). Over 75% of participants did not reach recommended PA targets (>10,000 steps/day), with females being 25% less active than males. The PSQI revealed 48.5% of participants scored >5, indicating poor sleep quality. Pearson correlation co-efficients highlighted that sleep quality was significantly negatively correlated with low step counts (-0.713, p = 0.0005) and positively correlated with higher sedentary time (0.681, p=0.0005).
Most participants did not meet PA guidelines. PA and sedentary behaviour levels correlate to self-reported sleep quality which should be considered in PA interventions.
Keywords: Cystic fibrosis, physical activity, sleep, wellbeing
2.14. Audit of compliance with updating a Cystic Fibrosis electronic record in a Cystic Fibrosis speciality unit
Toland, S1. Krajewski1, D. Kerr1, O. Gunaratnam, C1.
1 Department of Respiratory Medicine, Beaumont Hospital, Dublin 9.
A Cystic Fibrosis Electronic Record (CF ER) has been in use in Beaumont Hospital since 2011. The CF ER contains patient demographics as well as pulmonary function tests (PFTs), laboratory investigations, US abdomen and DEXA results, which must be updated manually. It is an efficient way to see all results pertaining to each patient, ensuring annual investigations have been completed, as well as allowing for monitoring trends.
We compared the data of 140 patients on the CF ER to the most recent investigations these patients had performed in Beaumont Hospital, assessing our compliance with data input. Parameters assessed were PFTs, diabetic status, US abdomen and DEXA scans
132 (94%) had their most recent PFT results, 50 patients (36%) had their most recent HbA1c/OGTT results, 111 (79%) had their DEXA results, 66 (47%) had their US abdomen results updated.
The results highlight that the majority of patients had their PFTs inputted however this was not the case for the other investigations. This may represent a reduced focus on the extrapulmonary effects of Cystic Fibrosis. In order to combat this we are providing education sessions to highlight the importance of the multi-systemic effects of CF. We plan to re-audit in 3 months.
2.15. Pulmonary Rehabilitation Outcomes in a Non-COPD Cohort
Khan J.1,2, Tonge P.1, O’Beirne S.L.1,2
1 Department of Respiratory Medicine, St Michael’s Hospital, Dun Laoghaire, Dublin.
2 Department of Respiratory Medicine, St Vincent’s University Hospital, Elm Park, Dublin 4.
Pulmonary rehabilitation (PR) plays a crucial role in the management of symptomatic patients with chronic obstructive pulmonary disease (COPD), improving exercise tolerance and quality of life (QOL) and reducing exacerbation frequency. However, it’s place in the management of other chronic respiratory diseases including interstitial lung disease (ILD) is less well studied.
To address this, we retrospectively analysed outcome data from our cohort of non-COPD patients (n=39) undertaking a PR programme between September 2016 and February 2020.
Of the 39 patients included, the majority (74%, n=29) had ILD, 17% (n=5) were female and 83% (n=24) were male with a mean age of 71±13 years and BMI of 27.4±4.7 kg/m2. Twenty-eight patients underwent pre and post PR incremental shuttle walk testing with average walk distance improving by 23.4±63.5 m post PR. Eleven patients were assessed pre and post PR with a six-minute walk test with a mean improvement of 28.6±36.1 m. There were no significant changes in the Hospital Anxiety and Depression Scale or Chronic Respiratory Disease Questionnaire scores pre/post PR.
These data indicate that in our of patients with chronic respiratory diseases other than COPD, general PR leads to modest improvement in functional exercise capacity without a significant change in QOL.
Conflict of Interest: The authors have no conflict of interest to declare.
2.16. Bone Health in Sarcoidosis
L Kingsmore1; T Scullion1; E Murtagh1; J Burns2; P Minnis1
Interstitial Lung Disease Service, Antrim Area Hospital, Bush Road
1Respiratory Medicine 2Rheumatology
The mainstay treatment of sarcoidosis is corticosteroid therapy, which often complicates bone health. We examined all patients attending the ILD clinic with sarcoidosis within 1 year for radiological involvement and axial bone health.
Baseline data was collated from 184 patients. 9 patients (5%) had reported evidence of appendicular involvement on imaging. 14% were treated with hydroxychloroquine. Treatment naïve patients tended to osteopenia BMD 0.952 g/cm2 (Ts -1.27), in comparison to treated patients lumbar BMD 1.061 g/cm2 (Ts -0.8). BMD were similar between those treated with low dose prednisolone and combination agents. Stratification by CXR stage indicated similarities between stage 0 and 4 in terms of treatment rates 89% versus 79% and BMD 1.021 g/cm2 (Ts -0.73) versus 1.06 g/cm2 (Ts -0.77). Inflammatory CXR stages 1-3 had a lower treatment rate (53%) and lower BMD 1.00 g/cm2 (T score -1.19). The majority of patients were sufficient in Vitamin D (64%) at time of testing.
There appears to be mechanisms outside corticosteroid induced net bone loss at play in patients with sarcoidosis. This data suggests a link between bone health and active pulmonary sarcoidosis that could not be explained by treatment or vitamin D deficiency.
2.17. LIVING WITH IPF: A PATIENT’S PERSPECTIVE
A Sarfaraz1, H Rahman1, M Poland1, C Varghese1, A Subramaniam1, SC Donnelly1
1 Medical Professorial Unit, Tallaght University Hospital & Trinity College Dublin
Idiopathic pulmonary fibrosis (IPF) is an irreversible, fatal lung disease with a major impact on patients' quality of life (QOL). Apart from curative lung transplantation, antifibrotics can slow disease progression. We aimed to study patients’ perspective about IPF and their treatment experience.
A qualitative descriptive study was conducted on 30 IPF patients on antifibrotics (22 Pirfenidone, 8 Nintedanib), attending our specialist ILD service. Telephonic interviews were conducted and structured patient reported outcomes (PRO) were obtained assessing 5 domains; patients’ understanding, impact on HRQOL, psychosocial aspects of the disease, patient/carer support from ILD specialist nurse as well as antifibrotics experience and side effects.
The framework method was used for qualitative analysis. Key outcome was patients challenged by having an “unknown” (n=12) and “invisible” (n=9) disease. Patient experiences and satisfaction with antifibrotics were fairly positive, and similar for both drugs. Self-reported impact on QOL was the main factor associated with overall medication satisfaction. Hospital Anxiety and Depression scoring was slightly higher in Pirfenidone (3.9) than Nintedanib users (3). Majority of patients stated that a specialist nurse was their main clinical contact for healthcare.
In conclusion, our study provides an overview of the most used PRO measures in IPF to integrate patients’ perspective into clinical practice, thus enhancing personalized medicine.
2.18. Clinical characteristics of a Diffuse Idiopathic Pulmonary Neuroendocrine Cell Hyperplasia Cohort
M. Gleeson1, A. Fabre1, D. O’ Toole1, R. Crowley1, D. Murphy1, C. Mc Carthy1
1 Rare Lung Disease Clinic, St. Vincent’s University Hospital, Elm Park, Dublin 4
Diffuse Idiopathic Pulmonary Neuroendocrine Cell Hyperplasia (DIPNECH) is a rare disease typically of middle aged non smoking women, with few cases described. After first recognitition in 1992, the WHO described it as a precursor to pulmonary carcinoid tumours. Currently there is no consensus on radiological and/or pathological criteria for diagnosis. Herein we aim to describe our experience of DIPNECH in St. Vincent’s University Hospital.
A retrospective analysis of 15 cases was performed. Data collected included: Age, gender, smoking status, CT findings, PFTs, treatment and assocaited neuroendocrine tumours.
All patients were female with a mean age of 60.2years. 9 patients had respiratory symptoms at diagnosis. 10 patients had lung function tested with an obstructive pattern seen in 40%. CT findings included a dominant nodule(n=7), associated nodules(n=13) and mosaicism(n=5). 13 cases were associated with a pulmonary carcinoid. Treatment included somatostatin analogues and inhaled corticosteroids in 5 and 5 patients respectively.
This is amongst the largest studies evaluating DIPNECH patients in a single centre. DIPNECH is a histological diagnosis, often asymptomatic and therefore underdiagnosed. Obstructive symptoms and lung function were most commonly seen. Given its rarity and current lack of evidence based guidelines a specialist centre is most appropraite for managing such patients.
2.19. Indications for cessation and/or dose reduction for adverse events from Nintedanib for the treatment for Idiopathic Pulmonary Fibrosis
S. Green1, K.M.A. O’Reilly1 and L. Fox1
1 Respiratory Department, Mater Misericordiae University Hospital, Dublin
Nintedanib has been shown in both clinical trials and real world experience to be a well-tolerated treatment that slows the rate of progression in Idiopathic Pulmonary Fibrosis (IPF). The most common adverse event reported is diarrhoea, occurring in 50-65%1. Experts report that approximately one third of patients discontinue antifibrotic therapies because of side effects.
In order to better understand our patients’ experience and potentially identify factors that might improve tolerability, we reviewed 26 patients (19M, 7F,) with IPF receiving Nintedanib at our institution between 2015 to 2020.
They had a median age of 69.50 years and 80.7% (n=21) had at least one comorbidity: 65.3% reported at least one adverse event; diarrhoea 34.6% (n=9), weight loss 30.7% (n=8), nausea 19.2% (n=5), deranged liver enzymes 7.6% (n=2), anorexia 3.8% (n=1), gout 3.8% (n=1). Twelve patients (46.1%) had at least one interruption to treatment, 5 patients (19.2%) continue on a reduced dose and 2 patients (7.6%) stopped treatment completely due to deranged LFTs and diarrhoea.
Therefore in our experience the majority of patients who experience a side effect related to Nintedanib therapy benefit from a temporary cessation of treatment, followed by recommencement of treatment at full or reduced dose.
References
1. Rivera-Ortega P, Hayton C, Blaikley J, Leonard C, Chaudhuri N. Nintedanib in the management of idiopathic pulmonary fibrosis: clinical trial evidence and real-world experience. Ther Adv Respir Dis. 2018;12:1753466618800618. 10.1177/1753466618800618
2.20. Thoracic Surgeons Performing Bronchoalveolar Lavage After Intubation Supports Best Practice Antibiotic Guidelines for Lung Resection
H Jones1, M AlAdaileh1, D O’Callaghan2, B Lynch3, KC Redmond1
1. Department of Thoracic Surgery, Mater Misericordiae University Hospital, Dublin, Ireland
2. Department of Respiratory Medicine, Mater Misericordiae University Hospital, Dublin, Ireland
3. Department of Microbiology, Mater Misericordiae University Hospital, Dublin, Ireland
2.21. Complications of CT-guided lung biopsies in the over 70s – a 10 year institutional review
H Dolphin1, L Greene2, M.P. Rogan1, M.A. Farrell2, S.C. Foley1
1. Department of Respiratory Medicine, University Hospital Waterford
2. Department of Radiology, University Hospital Waterford
Lung cancer occurs frequently in older patients. Previous studies suggest that older patients are less likely to undergo invasive diagnostic testing compared to younger patients1. CT-guided lung biopsy is the investigation of choice for peripheral lung nodules to determine pathology and to guide management. The purpose of our study was to investigate the rate of complication post CT-guided lung biopsy in patients aged 70 years and above and compare data to the published literature.
Incidence of complications following CT-guided lung biopsies between 2010 and 2020 was retrospectively reviewed for all patients aged 70 and over in our institution. Via accession number on National Integrated Medical Imaging System (NIMIS), the incidence of post- biopsy pneumothorax, pneumothorax requiring intervention and perilesional haemorrhage was obtained.
223 procedures were performed on patients aged 70 years and above. 33(14.7%) patients developed a pneumothorax at 2 hours post procedure of which 10(4.4%) required narrow bore chest drain insertion. Perilesional haemorrhage was noted at time of biopsy in 28(12.5%) patients, one requiring intervention. All incidences are lower than published international complication rates2.
Compared to international data, our rate of major and minor complications post CT-guided lung biopsy in older patients is low.
References
1. Cassidy, R.J., et al. (2018), Health care disparities among octogenarians and nonagenarians with stage III lung cancer. Cancer, 124: 775-784.
2. Heerink WJ, et al Complication rates of CT-guided transthoracic lung biopsy: meta-analysis. Eur Radiol. 2017 Jan;27(1):138-148.
2.22. Audit on the impact of the COVID 19 pandemic on the functioning, effectiveness and efficiency of the Rapid Access Lung Clinic (RALC) pathway
C Farrell2, A Scott2, D McGrath1, B Casserly1, A O’Brien1
1. Respiratory Department, University Hospital Limerick, Limerick
2. Respiratory Department, St John’s Hospital, Limerick
The COVID 19 pandemic is having a significant effect on the functioning of the Rapid Access Lung Clinic (RALC), this has not yet been fully quantified.
This is a retrospective audit of all patients referred to University Hospital Limerick (UHL) RALC in April and May 2019 and 2020.
Since the onset of the pandemic there has been a significant reduction in Lung Cancer diagnosed in Stages 1 and 2. See table. 12 (32.5% of total) in April and May 2019 compared to 5 (17.2% of total) in the same period 2020. Total referrals were 40% lower 210 in 2019, compared to 128 in 2020. Direct GP referrals were 67% lower, 103 in 2019 and 34 in 2020. The average time from referral to review was 15.6 days in 2019 compared to 14.1 days in 2020. The percentage of total referrals diagnosed with lung cancer was 15.2% in 2019 and 23% in 2020.
| Lung cancer diagnosis breakdown by stage | ||||||
| April 2019 | May 2019 | Total April and May 2019 | April 2020 | May 2020 | Total April and May 2020 | |
| Stage 1 | 3 | 4 | 7 | 0 | 2 | 2 |
| Stage 2 | 4 | 1 | 5 | 2 | 1 | 3 |
| Stage 3 | 1 | 3 | 4 | 1 | 2 | 3 |
| Stage 4 | 8 | 8 | 16 | 11 | 10 | 21 |
| Total | 16 | 16 | 32 | 14 | 15 | 29 |
The reduced number of direct GP referrals secondary to a delay in presentation to GP may at least partly account for the lower number diagnosed with Stage 1 or 2 lung cancer. This is likely to result in a delay in lung cancer diagnosis for many, diagnosis occurring at a later stage, greater burden placed on the healthcare system and ultimately more deaths.
2.23. Audit on the efficiency of the Rapid Access Lung Clinic (RALC) pathway and how this has been affected by the COVID 19 pandemic
C Farrell1, A Scott1, D McGrath1, B Casserly1, A O’Brien1
1 Respiratory Department, University Hospital Limerick
The COVID 19 pandemic is having a significant effect on the functioning of the Rapid Access Lung Clinic (RALC), this has not yet been fully quantified.
This is a retrospective audit of all patients referred to University Hospital Limerick (UHL) RALC in April and May 2019 and 2020. Initial referral, receipt of referral, clinic review, CT Thorax and bronchoscopy dates are all recorded.
210 patients were referred to the RALC in April and May 2019 compared to 128 in April and May 2020. Of these 107 were referrals direct from GP in 2019 compared 34 in 2020. The average time from referral to review was 15 days in 2019 compared to 13.5 days in 2020.
There has been a 40% reduction in the total numbers referred to the RALC and 68% reduction in direct GP referrals to the RALC in April and May 2020. This is likely to result in a delay in lung cancer diagnosis, diagnosis occurring at a later stage, greater burden placed on the healthcare system and ultimately more deaths.
2.24. Pulmonary mucosa-associated lymphoid tissue lymphoma- A single center review of the diagnostic approach.
Farrell AM1, Farrell SA1, Kennedy MP1, Henry MT1.
1. Department of Respiratory Medicine and Regional Lung Cancer service, Cork University Hospital, Cork, Republic of Ireland
Pulmonary mucosa-associated lymphoid tissue (MALT) lymphoma is a rare disease and diagnosis is difficult, often requiring multiple attempts at tissue sampling. The aim of this review was to evaluate the diagnostic pathway.
A retrospective review was preformed of patients diagnosed with pulmonary MALT lymphoma in a tertiary referral lung cancer center over 9 years. Ten patients were identified and each diagnostic and treatment approach was analyzed.
30% were diagnosed via transbronchial biopsy, two with the assistance of radial probe ultrasound guidance and one with transbronchial lung cryobiopsy of a predetermined CT-guided targeted segment. 70% were diagnosed following surgical biopsy. 40% had localized disease.
Diagnosis was not successfully achieved until a large sized tissue specimen was obtained. The implementation of novel bronchoscopy techniques can assist in reducing the number of invasive surgical procedures required to obtain a diagnosis. All cases should be discussed in a multidisciplinary setting prior to diagnostic attempts.
2.25. Manipulation of the retinoic acid axis to circumvent cisplatin resistance in NSCLC
L. MacDonagh1, C. Mulvey2, S. Toland2, SG. Gray1, E. Breen3, SP. Finn4, S. Cuffe5, KJ. O’Byrne1,6, MP. Barr1.
1. Thoracic Oncology Research Group, Trinity Translational Medicine Institute, Trinity College Dublin, School of Clinical Medicine, St. James's Hospital, Dublin 8.
2. Department of Respiratory Medicine, Beaumont Hospital, Dublin 9.
3. Flow Cytometry Core Facility, Trinity Translational Medicine Institute, Trinity College Dublin, School of Clinical Medicine, St. James's Hospital, Dublin 8.
4. Department of Pathology, St. James's Hospital, Dublin 8.
5. Department of Oncology, HOPE Directorate, St. James's Hospital, Dublin 8.
6. Cancer and Ageing Research Program, Queensland University of Technology, Queensland, Brisbane, Australia.
Pan-resistance to platinum agents remains a major clinical challenge in NSCLC. Due to the lengthy process of drug design and trial attention has turned to the repurposing of approved drugs within therapeutic resistance. Cancer stem cells (CSCs) have been hypothesised to be the initiating cells of resistance. All-trans retinoic acid (ATRA) is a well-established chemotherapeutic agent in the treatment of acute promyelocytic leukaemia; it induces terminal differentiation of immature cells. We hypothesise that exploitation of the retinoic acid pathway will deplete the CSC population thereby restoring cisplatin sensitivity.
The presence of an ALDH1-positive CSC subpopulation within cisplatin resistant (CisR) sublines was confirmed by flow cytometry. Cells were treated with retinol or ATRA and the presence of CSCs reassessed. The functional parameters of proliferation, clonogenic survival and apoptosis were also assessed.
Retinol and ATRA significantly depleted CSCs. Retinol and ATRA used in combination with cisplatin significantly reduced proliferation and survival of CisR sublines while increasing apoptosis compared to cisplatin alone.
Exploitation of the vitamin A/retinoic acid pathway re-sensitised sublines to the cytotoxic effects of cisplatin. These data suggest vitamin A supplementation or the addition of FDA-approved ATRA to cisplatin-based regimens may be of clinical benefit in overcoming recurrence and cisplatin resistance.
2.26. miR-34a a micromanager of cancer stemness and resistance in NSCLC
L. MacDonagh1, S. Toland2, SG. Gray1, M. Gallagher3, B. Ffrench3, C. Gasch3, M. Reidy4, S. Finn1,4, S. Cuffe5, K. O’Byrne1,6, MP. Barr1.
1. Thoracic Oncology Research Group, Trinity Translational Medicine Institute, Trinity College Dublin, School of Clinical Medicine, St. James's Hospital, Dublin 8.
2. Department of Respiratory Medicine, Beaumont Hospital, Dublin 9.
3. Histopathology and Oncology Research Group, Trinity College Dublin, Coombe Women and Infants University Hospital, Dublin 8.
4. Department of Pathology, St. James's Hospital, Dublin 8.
5. Department of Oncology, HOPE Directorate, St. James's Hospital, Dublin 8.
6. Cancer and Ageing Research Program, Queensland University of Technology, Queensland, Brisbane, Australia.
Disruption of Dicer-1, a crucial component of microRNA biogenesis depletes the stem cell pool, indicating a role for microRNAs in the maintenance of stem cells. MicroRNAs play a role in cancer stem cell (CSC) self-renewal, differentiation, resistance and metastasis. MicroRNAs associated with cisplatin resistance and CSC maintenance may be key in targeting the CSC root of resistance.
miRNAs associated with resistance were validated by qPCR. An ALDH1-positive CSC subpopulation was isolated using FACS. Expression of the miRNA panel was investigated within CSC populations. Altered miRNAs were inhibited using antagomiRs and stemness reassessed. Expression of the miRNA panel was investigated in FFPE tumour tissue of a xenograft model of CSCs.
A 5-miR signature associated with cisplatin resistance was identified across NSCLC histologies. The ALDH1-positive subpopulation was confirmed as CSCs, within this population miR-34a-5p was shown to be up-regulated. This result was mirrored within FFPE tissue. Inhibition of miR-34a-5p with antagomiRs did not deplete the CSC population however it significantly reduced the clonogenic capacity of cell lines.
These data suggest that miR-34a-5p, while significantly up-regulated within the CSC population, may not play a regulatory role in expression of CSC markers, however it may play a functional role in the survivability of CSCs.
2.27. Timing And Accuracy Of Clinical Staging of Non-Small Cell Lung Cancer in a Tertiary Lung Cancer Referral Centre
S O Brien1, B Dalton1, L Edwards2, S Nicholson3, R Ryan4, V Young4, G Fitzmaurice4, F O’Connell1, P Nadarajan1
1 Department of Respiratory Medicine, St. James’ Hospital, Dublin
2 School of Medicine, Trinity College Dublin, Dublin
3 Department of Histopathology, St. James’ Hospital, Dublin
4 Department of Cardiothoracic Surgery, St. James’ Hospital, Dublin
The accuracy of clinical staging of non-small cell lung cancer (NSCLC) is crucial in the establishment of both prognosis and treatment pathways for patients. There can be significant discrepancies between clinical and pathological stages (1). We assessed whether the agreement of clinical and pathological stages in a real world context was similar to that of the data collected from randomised control trials (1). Delays in patient flow through diagnostic imaging can result in an increase in tumour size and stage, so we also assessed whether delays impacted the accuracy of staging of patients in our cohort. (2)
We retrospectively collected data on 103 patients who had surgery for NSCLC in 2019. We assessed the difference between overall clinical staging and pathological staging as well as clinical and pathological T and N stages. We then constructed a timeline for each individual patient by analysing the time in days from their diagnosis to their surgery including duration between important timepoints such as PET scan and date of biopsy and EBUS.
Results are summarised in figure 1. There is agreement in the overall clinical and pathological stage in 56.7% (n=51) and disagreement in 43.3% (n=39). Median time between date of diagnosis and date of surgery was 50 and 55 days in the agreement and disagreement groups respectively. Median time between PET scan and surgery was 50 days in the agreement group and 65 days in the disagreement group.
In conclusion, the level of agreement in our centre is similar to that of data from randomised controlled trials. Duration between PET scan and surgery may influence the accuracy of clinical staging however we did not identify any other significant delays that contributed.
References
1. Navani N, Fisher DJ, Tierney JF, et al. The accuracy of clinical staging of stage I-IIIa non-small cell lung cancer: An analysis based on individual participant data. Chest 2019;155:502-9. 10.1016/j.chest.2018.10.020
2. Byrne SC, Barrett B, Bhatia R. The impact of diagnostic imaging wait times on the prognosis of lung cancer. Can Assoc Radiol J. 2015;66(1):53-57. 10.1016/j.carj.2014.01.003
2.28. A study of usefulness bronchoalveolar washing cytology in diagnostic of lung cancer
Qsous G1, Tolan M1, Healy DG1
1 Cardiothoracic Surgery Department – St. Vincent’s University Hospital – Dublin
A regular collection of cytology specimens from bronchoalveolar washing is expected to increase the ability of bronchoscopy to diagnose lung cancer. However, we aimed to study the sensitivity of cytology washing tests for diagnosing malignant lung lesions.
This is a retrospective study including 68 patients who underwent different thoracic surgeries for lung cancer in St. Vincent University Hospital from June 2018 to March 2020. The results of all cytology specimens from bronchoalveolar washing were reviewed from the patients' files.
Out of 68 patients, the predominant type of lung cancer was adenocarcinoma (54.4%) and squamous cell carcinoma (22.2%). Most of the patients were in stage I (67.6%). The positive cytology result as malignant cells was shown in 5 patients (7.4%). Also, another 5 patients (7.4%) had atypical cells.
The value of cytology specimens from bronchoalveolar washing in this study was not significant. This may be due to increasing the incidence of adenocarcinomas. Eliminating this technique could be considered in centers with similar experiences.
2.29. EBUS via the oesophagus for poorly accessible lesions: A Case Series
Quigley D1, O Connell F1, Nadajaran P1
1 Respiratory Department, Saint James Hospital, Dublin
EBUS has long been a common diagnostic tool used in the diagnosis of pulmonary pathologies. In the last decade increased interest has been shown in its usage via the oesophagus for sampling lesions inaccessible via the airways known as EUS-B-NA (1).
Our centre conducted 6 cases in which we used this modality to biopsy lesions after failing to do so with traditional EBUS due to poor visualisation/unsafe access (Case-figure1). CT guided biopsy was also not a safe option in any of our cases.
The key outcome was the high diagnostic yield of our cases of 100% with no adverse events reported in any case. No patient received sedation above the standard of regular bronchoscopy. Coughing and desaturation seemed less of an issue subjectively during the procedure.
We recommend that respiratory specialist training encompasses this modality in Ireland and the UK. This requires an increased number of cases when appropriate to be done in specialised centres as well as stimulated teaching courses. A combined procedure can be carried out in one simple session. All cases were conducted in the COVID pandemic and a reduction in gastroenterology referrals means reduced further delays in diagnosis/treatments for our patients.
References
1. F.J. Herth, M. Krasnik, N. Kahn et al. Combined endoscopic-endobronchial ultrasound-guided fine-needle aspiration of mediastinal lymph nodes through a single bronchoscope in 150 patients with suspected lung cancer. Chest, 138 (2010), pp. 790-794
2.30. Audit of Endobronchial Ultrasound-Guided Transbronchial Needle Aspirates (EBUS-TBNA) in St Vincent’s University Hospital for 2019.
Nancy Morsi1, Aurelie Fabre1
1 Department of Histopathology, St Vincent’s University Hospital, Dublin.
This is a retrospective yearly audit of EBUS performed in 2019 in a large teaching hospital, to assess diagnostic yield, adequacy, and use of rapid on-site evaluation (R.O.S.E.).
Overall, 158 patients underwent EBUS procedure (187 lymph nodes, 44.9% women) with a mean age of 60.92yrs .
The overall inadequacy rate was 9.49% . ROSE was performed in 84.8% with a positive yield in 91.8%.
80.21% were ATS N2 stations (2, 4, 7). In 19% cases (30/158), 2 nodes or more where sampled.
Overall, 61.39% showed benign cytology, of which granulomas were identified in 26.58% .
Sarcoidosis suspected in 43 patients (49 lymph nodes) with a yield for granulomas of 79.1%..
Of the 111 EBUS performed for suspected malignancy, 38.74% were positive for pulmonary and extrapulmonary malignancies; 52.25% were benign; 7 showed granulomas (6.31%).
Metastatic small cell carcinoma was diagnosed in in 27.9%, pulmonary adenocarcinoma in 23.26% , squamous cell carcinoma in 11.6%, extrapulmonary malignancy in 32%; metastatic breast carcinoma was the commonest.
EBUS is a good tool for the diagnosis of both malignant and non-malignant hilar and mediastinal lymphadenopathy, with 79.1% yield for sarcoidosis and overall inadequacy rate of 9.49%. These samples can be used to assess for molecular targets.
2.31. The of impact of a new diagnostic needle implementation on quality of sampling in EBUS-TBNA
Lucy Power¹, Tomas McHugh¹, Catriona Higgins², Ross K. Morgan¹, M. Emmet O’Brien¹
¹Department of Respiratory Medicine, Beaumont Hospital
²Cancer Data Department, Beaumont Hospital, Dublin 9
Endobronchial ultrasound-transbronchial needle aspiration (EBUS-TBNA) is indicated for sampling of thoracic lymph nodes and lung masses located near central airways. New Olympus® FNA needles were introduced in Beaumont Hospital in January 2020, replacing Cook® FNA needles. We examined periods before and after introduction of the new needles to assess for tissue adequacy, need for repeat procedures, and tissue adequacy for molecular studies.
This study was registered as a clinical audit. Data was examined for all patients undergoing EBUS from September to December 2019 (Cook® EchoTip® Needle; n=54) and March to June 2020 (Olympus® Vizishot 2®; n=59). Tissue adequacy was determined from pathology reports.
Lung mass was the most frequent indication for EBUS, 57/113 (50.44%). 6/51 (11.1%) Cook® TBNA samples were deemed inadequate vs 11/59 (18.6%) Olympus® TBNA samples, P=0.43. In the Cook® group there were 7 (12.9%) repeat EBUS procedures and 3 repeat procedures (5.08%) in the Olympus® group, P=0.19. Multiple regression analysis was performed to rule out operator-dependent variation.
In conclusion, adoption of Olympus® needle resulted in non-inferior pathologic outcomes to Cook® needle, with a non-significant reduction in repeat EBUS procedures.
2.32. CT Scanning of Cardiothoracic Patients preoperatively for COVID-19 in a single centre
M O’Dwyer1, J Fish1, JB McLoughlin1, D Doyle2, T N Dhonnchu1
1. Department of Cardiothoracic Surgery, Cork University Hospital, Wilton, Cork, Ireland
2. Department of Radiology, Cork University Hospital, Wilton, Cork, Ireland
COVID-19 poses a significant risk to patients and staff involved in Cardiothoracic Surgery(CTS).(1)
In CUH, planned pre-operative CTS patients underwent COVID-19 screening using polymerase chain reaction tests on nasopharyngeal swabs and more sensitive Computed Tomography(CT) of the chest as recommended by governing medical organisations.(1-2)
Our study assessed the impact of CT scanning these patients over a two month period, evaluating findings, upstaging of malignancy or changes to operative planning.
Sixty-six patients underwent cardiothoracic procedures in CUH in April and May 2020. 43% were thoracic operations and 57% were cardiac operations. Mean age of patients was 63.6 years(Range 21-82). All patients had a negative COVID-19 swab within 72 hours of surgery. Fifty-three CT’s were performed, on average 2.4 days(Range 0-19) before surgery. 35.8%(19/53) of CTs were performed outside of normal working hours. No CT revealed COVID-19 in this group. 13% had incidental CT findings which required follow up. No patient had upstaging to their disease. No patient had their surgical strategy changed based on screening scan findings.
This small study, at the outset of an evolving pandemic, demonstrated that CT scanning provided additional reassurance. There was no disparity between laboratory viral screening and radiology screening, suggesting a lack of adjunctive benefit.
References
1. SCTS Current Recommendations Regarding Screening for COVID-19 in Patients undergoing Cardiothoracic Surgery (22nd April 2020) [Internet]. Scts.org. 2020 [cited 31 August 2020]. Available from: https://scts.org/wp-content/uploads/2020/04/SCTS-Current-Recommendations-Regarding-Screening-for-COVID-19-in-Patients-Undergoing-Cardiothoracic-Surgery-22nd-April-2020.pdf
2. Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W et al. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020;296(2):E32-E40.
2.33. Lung cancer diagnoses during the SARS-CoV-2 pandemic
D. Parfr1ey, G. O’Dea1, G. Coogan1, J. McDonnell1, T. Hassan1, I. Counihan1
1 Respiratory Department, Our Lady of Lourdes (OLOL) Hospital, Drogheda
Lung cancer is the leading case of cancer-related deaths in the Republic of Ireland. Common presenting symptoms of cough and dyspnoea are non-specific and widespread screening is not in place; unfortunately, most lung cancer is diagnosed at an advanced stage. The OLOL Rapid Access Lung Cancer Service continues to operate and accept referrals during the SARS-CoV-2 pandemic.
We observed the incidence of new diagnoses of lung cancer in OLOL Hospital during the SARS-CoV-2 pandemic between 1 March and 30 June 2020, compared with the same period in the year before.
During the study period, 39 cases of lung cancer were diagnosed in OLOL Hospital. This compares to 23 cases in the same time period in the year before, representing an increase of 69.6%.
There have been concerns that reduced scheduled care could lead to delayed cancer diagnosis during the pandemic, and overseas health services have reported decreased cancer diagnosis during this time1. However, we have observed an increased incidence of lung cancer diagnosis during the pandemic, which may be due to patients seeking medical attention for symptoms of SARS-CoV-2, which overlap with those of lung cancer, and undergoing thoracic imaging, which often involves CT-Thorax for radiological diagnosis of SARS-CoV-22.
Potential conflicts of interest: None declared.
References
1. Dinmohamed AG, Visser O, Verhoeven RH, Louwman MW, van Nederveen FH, Willems SM, Merkx MA, Lemmens VE, Nagtegaal ID, Siesling S. Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. The Lancet Oncology. 2020 Jun 1;21(6):750-1.
2. Xu X, Yu C, Qu J, Zhang L, Jiang S, Huang D, Chen B, Zhang Z, Guan W, Ling Z, Jiang R. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. European journal of nuclear medicine and molecular imaging. 2020 Feb 28:1-6.
2.34. Video-Assisted Thoracic Surgery (VATS) thymectomy Versus Median Sternotomy: A retrospective comparison
D Alsaadi1, M Forde1, A White1, N O’Halloran1, A Soo1
1 Department of Cardiothoracic Surgery, University Hospital Galway, Galway.
Thymoma is the leading cause of mediastinal neoplasms in adults. Until recently an open approach via median sternotomy has been the mainstay surgical approach. Over the last decades the use of minimally invasive VATS has emerged. Such procedures enable smaller incisions, faster recovery and shorter in-patient hospital stays. The aim of this study was to compare surgical techniques.
This comparative retrospective study included all cases of thymectomies performed in University Hospital Galway between 2015 and 2020.
A total of 16 patients were included in this 5-year study period. 75% were male (n=12). 75% were smokers. 87.5% presented as incidental findings, 12.5% as myasthenia gravis. 6 patients (38%) underwent VATS (starting in 2017) with a 0% conversion rate. The remaining patients (62%) underwent open surgery. Histopathology confirmed benign thymomas in 57% of the VATS cases and 40% of the open surgical cases. The average length of stay was 4 and 6 days for VATS and open surgery, respectively.
This study highlights a low morbidity rate of VATs thymectomy despite early learning experience. A shorter in hospital stay for VATs procedures is noted when compared to standard open techniques with a consequent potential for reduced overall cost.
2.35. An Audit on the Prevalence of Chronic Kidney Disease (CKD) in Post Lung Transplant Patients
A. Asis1, S Winard1, S Towell1, I Lawrie1, J Egan1, N. Ronan1, M Murray1
1 Heart and Lung Transplant Unit, Mater Misericordiae University Hospital, Dublin
CKD in post-lung-transplant is defined as estimated glomerular filtration rate (eGFR) of <60 mL/min/1.73m2 in at least 1-month post-transplant, which corresponds to the National Kidney Foundation Kidney Disease Outcome Quality Initiative (KDOQI) guidelines1
We analysed fifty transplant recipients through electronic records. Data on eGFR at baseline and post lung transplant and few independent risk factors such as age, gender, and indications and types of transplants we collected and analysed in Microsoft excel. We used a multiple variable association modelling to interpret our findings.
The results demonstrate that the prevalence of CKD is higher in elderly patients aged >65 with an absolute difference of 12.9%, male gender with 3.8%, COPD as indications of lung transplant with 6.5%, and single lung transplant with 4.3%
| Recipient Characteristics on the Day of Transplant | Prevalence of CKD Post Transplant |
| Age | |
| <65 | 80.6% |
| >65 | 92.9% |
| Gender | |
| Male | 85.7% |
| Female | 81.9% |
| Indications for Transplant | |
| CF | 88.2% |
| IPF | 81.0% |
| COPD | 87.5% |
| Type of Transplant | |
| Double | 82.1% |
| Single | 86.4% |
Table 1
CKD is common in post-transplant patients, particularly in elderly, male populations, with a COPD related single lung transplant. This finding is significant as more study needed to identify the association between these risk factors development of CKD.
Conflict of Interest: None.
References
1. 2002 National Kidney Foundation clinical practice guidelines for chronic kidney disease: evaluation, classification and stratification. National Kidney Foundation website. http://www.kidney.org/professionals/KDOQI/guidelines_ckd/p4_class_g1.htm. Accessed September 14, 2011
2.36. Breathlessness and respiratory disability post renal transplantation.
Farrell AM1, Baqer N1, Kant S2, Farrelly S1, Hunt E1, Clarkson MR2, Henry MT1, Kennedy MP1, Plant WD2, Plant B.J1,3, Eustace J2,3, Murphy DM1,3.
1 The Department of Respiratory Medicine, Cork University Hospital, Cork, Ireland
2 Department of Renal Medicine, Cork University Hospital, and College of Medicine, University College Cork, Cork, Ireland
3 The HRB funded Clinical Research Facility, University College Cork, Cork, Ireland.
Dyspnea is a common complaint in patients with end stage kidney disease being treated with dialysis. Symptoms often persist post renal transplant. The aim of this study was to assess a cohort of renal allograft recipients for potential respiratory compromise, hence identifying a potential target for therapeutic intervention.
Renal transplant patients under active follow-up in a single tertiary referral center, were asked to partake in this cross-sectional study at time of clinic follow up. Patients who consented completed the Medical Research Council (MRC) Dyspnea Score and performed basic spirometry. An MRC score ≥2 and/or a forced expiratory volume in one second <90% prompted formal clinical assessment by a Respiratory Physician. 103 patients were enrolled in this study.
35% of all patients reported breathlessness and, with the combined evaluation, 56% of all patients warranted formal respiratory medicine review. Following completion of their investigations, 33 patients were found to have an underlying condition accounting for their symptoms.
We recommend that structured evaluation utilising the MRC Dyspnea Score and spirometry be incorporated into the routine follow-up of renal transplant recipients, as this study has indicated a substantial burden of disease that is not ascertained by non-systematic clinical review. Furthermore, it may be prudent to consider this in potential renal transplant recipients prior to transplantation.
2.37. To assess safety and rate of complications of transbronchial biopsies: A single centre experience.
W. Mahmood1, U. Khan1, O. Rahman1, K. Rana1, A. O’Brien1.
1 Respiratory Department, University Hospital Limerick.
Bronchoscopy with/without fluoroscopy is employed in diagnosis of variety of lung diseases such as peripheral lung masses, focal/diffuse lung infiltrates, suspected fungal/mycobacterial lung infections. Complications include penumothoraces, bleeding and infections. Whether use of fluoroscopy decreases rate is unclear1.At UHL, all transbronchial biopsies are performed without fluoroscopy due to lack of access. we aim to assess safety and rate of complications of transbronchial biopsies without fluoroscopy.
In this retrospective study,95 patients underwent flexible fiberoptic bronchoscopy with transbronchial biopsy, for different pulmonary pathologies in last 6 months.44 were male and 51were female. Average age 70 years (+/-11).Of these,51 had transbronchial needle aspirations (53%),57 bronchoalveolar lavage(60%),13 brush biopsies(13.6%).
8(8.4%)patients suffered complications secondary to transbronchial biopsies:6(6.3%)were pneumothoraces,2(2.1%)were significant bleeding.One patient required chest drain insertion while remainder of patients with pneumothoraces were managed conservatively.Patients with bleeding were managed with cold saline +/- adrenaline.Patients who suffered pneumothoraces required hospital admission and mean duration of stay was 2 days(+/-1).There were no deaths.Our results were consistent with a recent meta-analysis showing rate of pneumothorax ranges between 0.4-5.8% in studies with use of fluoroscopy,and 1.5-20.2% without the use of fluorosocpy1.
Our study shows transbronchial biopsies without fluorosopy are relatively safe procedure,and fluoroscopy may not reduce the complication risk.Experience and training play fundamental role in reducing complication rates.
Conflict of interest: None to Declare.
References
1) María José Bernabé Barrios., et al. “Transbronchial Biopsy With or Without Fluoroscopy?”. EC Pulmonology and Respiratory Medicine 8.4 (2019): 345-355.
2.38. The utility of intra-operative bronchoalveolar lavage in thoracic surgery
Qsous G MD 1, Healy DG MD1
1 Cardiothoracic Surgery Department – St. Vincent’s University Hospital - Dublin
Chest infection is one of the most common complications after thoracic surgery, we aim to investigate the usefulness of intra-operative bronchoalveolar washing to help decrease the rate of postoperative chest infection and predict the causative microorganism.
This is a retrospective study including 100 patients who underwent different thoracic surgeries in St. Vincent University Hospital from June 2016 to March 2020. All patients underwent intra-operative bronchoalveolar lavage before beginning the surgery. Also, a bronchial washing sample was sent for microbiological analysis.
One hundred patients were included in our study. Out of 100 surgery, there were 16 cases performed by open thoracotomy, 13 robotic-assisted thoracoscopic surgery and 71 cases with video-assisted thoracoscopic surgery. Additionally, there were 53 cases as primary lung cancer, 16 cases as secondary lung cancer (metastasis) and 31 benign cases. Chest infection was noticed in 12 patients (12%). Out of these 12 patients, there were 7 patients (58.3%)have a positive culture from the bronchoalveolar washing. The mean duration of postoperative hospital stay was 6.1 days.
Adopting the intra-operative bronchoalveolar lavage in thoracic surgery can decrease the rate of chest infection and predict the causative microorganism. Consequently, that leads to a decrease in the length of hospital stay.
2.39. The use of a 3D printed ultrasound needle guide to aid trainees in developing skills for bedside ultrasound guided fine needle aspiration and core biopsy of phanthom lymph nodes.
S. Shahsavari1, C. Farrell1, K. O’Sullivan1, A. Scott1
1 St. Johns Hospital Limerick, University Hospital Limerick Working Group.
Rapid Innovation Unit, University Limerick
In the COVID era access to aerosol generating procedures for diagnostics is limited. It has been shown that ultrasound guided fine needle aspiration and core needle biopsy of neck lymph nodes performed by respiratory physicians is safe and accurate to diagnose and stage cancer. A well formed knowledge of neck anatomy and ultrasound is required in order to train physicians to perform this procedure to an accurate and safe level. In order to correctly guide a needle into a lymph node it is necessary to develop hand-eye co-ordination and use knowledge of in-plane or out of plane ultrasound needling in order to hit the target.
The Rapid Innovation Unit of University Limerick has 3D printed a first of their kind device specific needle guides for our portable handheld ultrasound systems. This has allowed us to assess the skills of respiratory trainees in performing this procedure on a simulated ultrasound phanthom and then gauge if they found it easier to use the sterile and autoclavable 3D printed needle guide to improve accuracy and safety in performing FNA and core biopsies.
None of our trainees had any previous experience in performing this procedure free style or with a 3D printed needle guide.
2.40. Rapid access lung cancer clinic deferral letter audit
R. Tyrrell1, O. Shinners1, J. Lowry1, A. Scott1, S. Shabsavuri1, U. Khan1, A. O’Brien1
1 Respiratory Department, University Hospital Limerick.
2.41. Lung Cancer in young patients: A Review of the MidWest Lung Cancer data.
O. Rahman1, M.K. Rana1, W. Mahmood1, A. O’Brien1
1Respiratory department, University Hospital Limerick
We performed a retrospective review of our lung cancer database for young patients presenting with a new diagnosis of lung cancer in the last 5 years (2015 to 2019). We looked at gender distribution, smoking history, types of cancer and treatment options, and molecular studies. We also compared these results to all lung cancer patients in the national lung cancer registry.
There were 16 patients below the age of 50 years diagnosed with lung cancer during that period. The mean age of the group was 43. 50% were male. Adenocarcinoma was present in 56% of our patients, 6.2% had squamous cell carcinoma, carcinoid 18.7%, small cell carcinoma was 12.5% and NSCL-NOS was 6.2%. 68.7% were either current or ex-smokers. 68.7% of patients diagnosed had stage 4 lung cancer. 31.2% of patients had surgical resection, 43.7% had chemotherapy, 6.2% had radiotherapy, while 18.7% did not receive any treatment.
When compared to national data of all lung cancer patients, the major differences noted included: prevalence of adenocarcinoma - 56% in younger group vs 34% in the national data; squamous cell carcinoma 6.2% vs 25%. The other difference was the stage of diagnosis- 68.7% were diagnosed at stage 4 in younger population vs 37% in the national data.
Conclusion: Young lung cancer patients have a higher prevalence of adenocarcinoma, lower prevalence of squamous cell carcinoma and present at a more advanced stage than older patients.
2.42. Experience of stereotactic ablative body radiotherapy for radically treatable lung cancer in a District General Hospital
Dr O Ni Griannna1, CNS H Mc Cormick1, Dr MG Kelly1, Dr C King1, Dr R Sharkey1, Dr M Mc Closkey1
1 Department of Respiratory medicine Altnagelvin Area Hospital, Glenshane Road, Londonderry.
Stereotactic ablative body radiotherapy (SABR) was introduced as a treatment for radically treatable Non-Small Cell Lung Cancer (NSCLC) in Northern Ireland in 2017. The treatment is given in the regional Cancer centre in Belfast (NICC), 70 miles from this District General Hospital (DGH). The aim of this study was to assess patient outcomes and experience since the service was introduced.
All patients who attended the oncology unit from 2017 to 2019 at this DGH were assessed. The number of patients diagnosed with lung cancer, numbers treated radically with surgical resection and numbers of those treated with SABR were recorded. Demographic profile and outcome of those treated with SABR was recorded and compared with those who had surgical resection. Patient experience was audited by a Patient Satisfaction Survey.
Over the three year period, 115 patients had surgery for potentially curative NSCLC. Eighteen patients underwent SABR in NICC. Mean age for patients who had surgery was 67.1 (range 40-84) Mean age of patients who had SABR was 75.5(range 60-86). Outcome over the 3 year period was similar in both groups. Patient tolerance of SABR was good, follow up arrangements post SABR were difficult because patients had to travel large distances for outpatient clinics.
SABR has been well tolerated in this DGH since introduced regionally. Patient tolerance has been good but difficulties remain as regards follow up post treatment.
2.43. Regional variation in lung cancer presentation, tumor type and tumor burden
Waheed Shah1,5, Qsous Ghaith2, Aurelie Fabre,1,4, Brian Canavan3, Cormac McCarthy1,5, David Healy2, Michael P. Keane.1,5
1 Department of Respiratory Medicine, St. Vincent’s University Hospital, Elm Park, Dublin 4.
2 Department of Cardiothoracic Surgery, St. Vincent’s University Hospital, Elm Park, D4.
3 St Luke’s Hospital Kilkenny.
4 Department of Pathology, St. Vincent’s University Hospital, Elm Park, D4.
5 School of Medicine, University College Dublin, D4.
Lung cancer is a leading cause of death worldwide. As regional variation in cancer outcomes is undesirable, understanding the reasons for such is essential to improve care.
A retrospective analysis was performed of 584 patients diagnosed with primary lung cancer at the NCCP MDT at St Vincent's University Hospital from 2016-2020. Stage at diagnosis, lymph nodes status, tumour size post resection and outcomes were evaluated and comparisons between patients referred directly through Model-4 Hospital and Model-2/3 Hospitals were analysed.
Patients referred via Model-2/3 had more advanced stage and increased nodal burden compared to Model-4 referrals ((Stage 4 = 53% vs 30%). There were a higher proportion of squamous cell (33%), and small cell carcinomas (13%) in Model-2/3 patients compared to Model 4 (27% &,8%).Out of 249 surgical resections, patients from Model-2/3 (n=152) had larger median tumour size compared to Model-4 (n=97)( (31.72mm vs. 24.74mm, p=0.026) and more advanced nodal stage (N1:14.5%,N2:9.1%vs N1:9.2%, N2:4.2%)(p=0.249).
This study revealed both variation in stage at presentation between regions but also interestingly in patients undergoing surgery for similar stage following PET-CT imaging, post-operative pathology revealed higher tumour and nodal burden. Further research is warranted to determine if this is due to environmental, epigenetic or other factors.
2.44. Incidence and Clinical Outcomes of Post-Transplant Lymphoproliferative Disorder (PTLD) in Lung Transplant Recipients
Boyle N1, Winward S1, Lawrie I1, Towell S1, Egan J1, Ronan N1, Murray M1
1 The National Heart and Lung Transplant Centre, Mater Misericordiae University Hospital, Dublin.
PTLD is a complication of transplantation with significant morbidity and mortality1. Incidence varies with age, transplant type and immunosuppression2. We aimed to examine the incidence and PTLD outcomes in lung transplant recipients.
A retrospective review of lung transplant recipients in the National Lung Transplant Unit between 2005 and 2020 was undertaken to identify patients with PTLD.
From 297 recipients, 8 (7 males, 1 female) were diagnosed with PTLD (2.69%). Indications for transplant were cystic fibrosis (n=5, 62%), sarcoid (n=2, 25%) and emphysema (n=1, 12.5%). Median age at transplant was 30. Median time from transplant to PTLD was 10.53 months. Median age at diagnosis was 35. All were on immunosuppression at the time of diagnosis. The majority had monomorphic PTLD (n=5 Diffuse Large B-Cell, n=1 Burkitt, n=2 polymorphic). 37.5% had bone marrow involvement. 25% had central nervous system involvement. Immunosuppression was reduced in all. 75% received rituximab, 37% received chemotherapy (n=1 R-epoch, n=2 R-chop), 12% received radiotherapy and 1 died prior to treatment. One-year survival was 62.5%. One experienced recurrence at 21-months.
This highlights the incidence and outcomes of PTLD in lung transplant recipients in Ireland which are in keeping with international studies1,2.
References
1. Parker, A., Bowles, K., Bradley, J., Emery, V., Featherstone, C., Gupte, G., Marcus, R., Parameshwar, J., Ramsay, A. and Newstead, C., 2010. Management of post-transplant lymphoproliferative disorder in adult solid organ transplant recipients - BCSH and BTS Guidelines. British Journal of Haematology, 149(5), pp.693-705.
2. Zaffiri, L., Long, A., Neely, M., Cherikh, W., Chambers, D. and Snyder, L., 2020. Incidence and outcome of post-transplant lymphoproliferative disorders in lung transplant patients: Analysis of ISHLT Registry. The Journal of Heart and Lung Transplantation.
IRISH THORACIC SOCIETY ORAL PRESENTATIONS II
2.1.1. Disease characterisation of people in Ireland with cystic fibrosis heterozygous for the F508del mutation and a minimal function mutation
E McKone,1 P Mondejar-Lopez,2 S Naehrig,3 D Salvatore,4 K Bresnick,5 C DeSouza,5 E Arteaga-Solis,5 L Kirwan6
1Department of Medicine, St. Vincent’s University Hospital, Dublin, Ireland; 2Hospital Clínico Universitario Virgen de la Arrixaca, Murcia, Spain; 3Med. Klinik V, LMU Klinikum der Universität München, Munich, Germany; 4Hospital San Carlo, Potenza, Italy; 5Vertex Pharmaceuticals Incorporated, Boston, MA, USA; 6Cystic Fibrosis Registry of Ireland, UCD Belfield, Ireland
2.1.2. Interleukin-22 and Neutrophil Proteins as Predictors of Future Disease Severity in Children with Cystic Fibrosis
E. Reece1§, J. Renwick 1§, J Walsh2, R Walsh2, T Persaud2, C O’Leary2, S. C. Donnelly3 † and P. Greally 2 †
1.Clinical Microbiology, Trinity College Dublin, Ireland.
2 Children’s Health Ireland and Tallaght University Hospital, Dublin, Ireland.
3 Department of Medicine, Tallaght University Hospital and Trinity College Dublin, Ireland.
§ These authors contributed equally to this manuscript
† Joint senior authors
2.1.3. Real-life Data on the Safety and Tolerability of Pirfenidone versus Nintedanib in Idiopathic Pulmonary Fibrosis (IPF) Patients: A Single-Centre Study
Thong L1, Bowen B1, Henry MT1.
1 Department of Respiratory Medicine, Cork University Hospital
In the last decade, the management of IPF has changed drastically with the licensing of 2 disease modifying agents. We aim to study the real-life experience of our IPF patients on Pirfenidone versus Nintedanib.
All IPF patients commenced on Pirfenidone and Nintedanib from January 2017 to January 2020(3 years) were recruited. 108 patients were included in the study. Patient demographics, date of treatment initiation, side-effects(SE), dosages and pulmonary function test pre-treatment and 6 months post-treatment were collected.
Mean age of patients in our study is 75.1 years. Male to female ratio 2.6. Exactly 50% of patients experience SEs from Pirfenidone versus 28.6% in the Nintedanib group (See Table 1). Dose reduction/termination of treatment were higher in the Pirfenidone group.
In the Pirfenidone group, the 6-month mean % reduction of FVC and DLCO in the full dose vs reduced dose was FVC-2.5%, DLCO-0.1% versus FVC -0.7%, DLCO -3.4%. In the Nintedanib group, the % reduction was FVC -6.2%, DLCO -3.3% vs FVC -1.5%, DLCO -11.6% full and reduced dose respectively.
The Nintedanib group appears to experience less side effects. Dose reduction in Nintedanib appears to impact 6-month follow-up PFTs negatively more than Pirfenidone. There are limitations to our study due to relatively low numbers.
2.1.4. Delay in Primary Lung Cancer detection due to COVID-19 Pandemic
D Halim, CD Campbell, C Higgins, F Colhon, D Burnell, RK Morgan, ME O’Brien.(1)
(1) Respiratory Department, Beaumont Hospital, Dublin 9.
Lung cancer is the leading cause of cancer related deaths worldwide and late diagnosis is a key contributor to poor outcomes. There is considerable international concern on the effect of the COVID-19 pandemic on cancer services. Our objective was to determine any delay in lung cancer referrals to the Rapid Access Lung Cancer Clinic (RALC) due to COVID-19 pandemic.
We compared referrals to the RALC service at Beaumont Hospital and subsequent diagnosis of lung malignancy in the six-month periods January-June across 2018, 2019 and 2020.
In 2020, there was 20% reduction in outpatient referrals (165 to 129). Average number of cancer detected per month since 2018 is 10 cases but this number dropped to 1, 5 and 6 in April, May and June 2020 respectively, coinciding with the peak of COVID-19 pandemic. Simultaneously, 30 inpatient cases were diagnosed in 2020 compared to 12 and 7 cases in 2019 and 2018 respectively. Of the new outpatient diagnosis, 8/11(70%) were stage IV, compared to 14/33(42%) and 9/36(25%) in the period April to June 2019 and 2018 respectively. These differences were statistically significant (p<0.0141 and p<0.0094 respectively). Questionnaire data obtained shows that 30% of patients reported delay in presentation due to COVID-19, related to delay in visiting GP, delay in receiving hospital appointment or cocooning.
The COVID-19 pandemic has led to a significant delay of lung cancer diagnosis in some patients. The proportion of inpatient lung cancer presentations increased during the COVID-19 pandemic with symptomatic Stage IV disease accounting for this finding.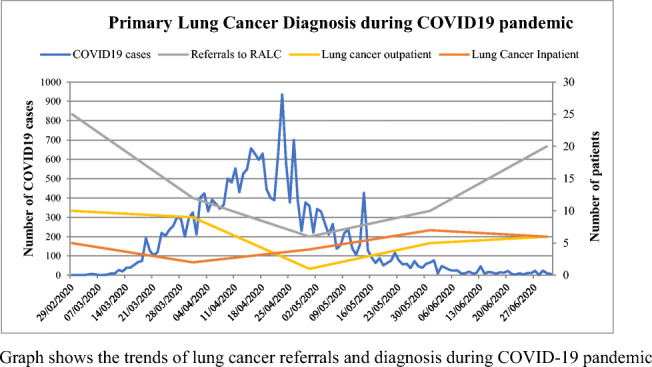
2.1.5. The value of perioperative bronchoalveolar lavage in thoracic surgery- St. Vincent’s University Hospital experience
Qsous G1, Tolan M1, Healy DG1
1Cardiothoracic Surgery Department - St. Vincent’s University Hospital – Dublin
Lung infection after thoracic surgeries are one of the most common complications that can lead to an increase in the length of hospital stay. We aimed to explore whether perioperative bronchoalveolar lavage can reduce postoperative chest infection.
This is a retrospective study including 194 patients who underwent different thoracic surgeries in St. Vincent University Hospital from June 2013 to March 2020. Patients were divided into two groups. The first group is the standard group included 94 patients, while the second group included 100 patients who had perioperative bronchoalveolar lavage.
The bronchoalveolar lavage group (n=100) had a significantly lower incidence of postoperative lung infection (11%) compared to the standard group (22.3%) P value = 0.033. Also, the length of hospital stay was significantly shorter in the bronchoalveolar lavage (5.6 days) compared to the standard group (9.4 days) P value = 0.000. Moreover, the bronchoalveolar lavage showed a useful diagnostic side when (73%) of patients who developed chest infection had a positive culture from the bronchial washing.
As conclusion bronchoalveolar lavage decreases the risk of post-operative chest infection and decrease the length of hospital stay. Also, it can use as diagnostic methods to treat patients with a chest infection.
IRISH THORACIC SOCIETY POSTER REVIEW AND DISCUSSION
3. General Respiratory and Sleep Medicine
3.1. An audit of documentation using wells score and d-dimer for CTPA requests in the MMUH
Jehangir Khan1, Killian Armstrong1, Prof. Sean Gaine1
1Mater Misericordiae University Hospital, Dublin.
Wells score is an important indicator of probability of having a PE, D-Dimers is a very good negative predictive value for PE (Pulmonary Embolism)(3). We performed an audit on CTPA performed in the first week of January 2020 by reviewing their request retrospectively.
Standards: This is per local and HSE guidelines for patient needing a CTPA need both D-Dimer and Wells score documented.
Retrospective review of CTPA (Computerised Topography Pulmonary Angiogram) request on NIMIS (National integrated Medical imaging system), from January 1 to January 7th 2020. To see for the documentation for D-dimers and Well’s scores. We also analysed the outcome of the CTPA based on the documentation and whether they were present in the order. We also analysed whether the orders were from the ED or the wards and whether they differed.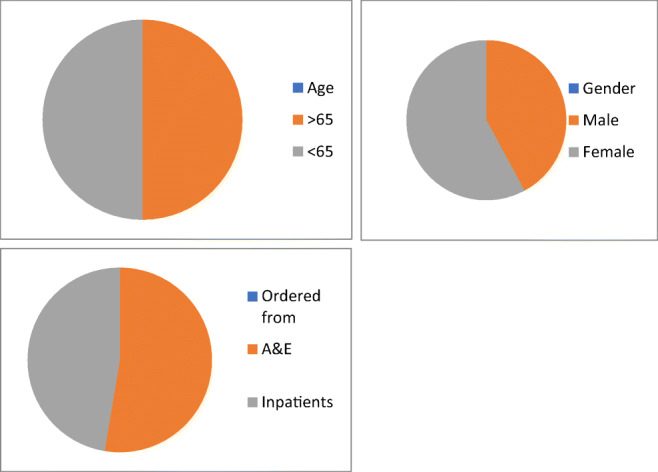
Results: Over the 7 day period, 38 CTPAs were performed on 38 patients with an even split of 19 for both over 65 and under 65 with an uneven split of 16 for male (42%) and 22 for female (58%). A&E had a slight increase of 20 (52%) & 18 for inpatients (48%). However the alarming results of this audit showed that only 6 patients had a documented Well’s scores when ordering the scan (15%), with 9 positive d-dimers used (24%). Of the 38 no order had both D-dimer and wells score in the order. Of the 38 scans ordered there are only 2 positive results (5.2%), both of which did not use the required D-dimer or wells score.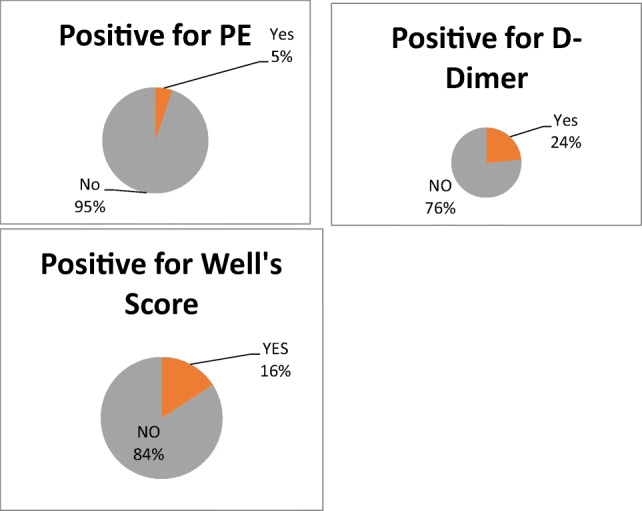
Retrospective reviews of CTPA, there were 38 Scans ordered in a 7 day period with 2 Positive results for PE, a 5.2% positive result. The documentation of both Well’s score and D-Dimer are both needs to be improved with less than a quarter for D-dimer documentation and a 15% documentation of the required Well’s scoring System.
Recommendations: There is significant room to improve in the ordering of CTPA scans. Based on the clinical situation all patients should have a Well’s score documented and/or a D-Dimer done. We are planning to re-audit in the coming months.
References
1. Booker M, Johnson J, Optimizing CT Pulmonary Angiogram Utilization in a Community Emergency Department: A Pre- and Post-intervention Study: J Am Coll Radiol 2017;14:65-71.
2. Singh B, Mommer SK, Erwin PJ, et al Pulmonary embolism rule-out criteria (PERC) in pulmonary embolism—revisited: A systematic review and meta-analysisEmergency Medicine Journal 2013;30:701-706.
3. Stein PD, Hull RD, Patel KC, et al. d-Dimer for the Exclusion of Acute Venous Thrombosis and Pulmonary Embolism : A Systematic Review. Ann Intern Med. 2004;140:589–602.
3.2. A Comparative Study of the European Coal and Steel Community (ERS 1993) and the Global Lung Initiative (2017) Reference Equations used for Diffusion Capacity Testing in an Irish Population
A. Bukhari1, O. McGuinness1, A. McGowan1, L. Cormican1,
1 Respiratory and Sleep Diagnostics Department, Connolly Hospital Blanchardstown, Dublin, Ireland
This study compares two reference equations used for Single breath diffusing capacity (DLCO) testing; the 1993 update of (ECSC) and the 2017 (GLI). Data was retrospectively collected from 240 patient DLCO tests, half of which were females, carried out in Connolly Hospital.
Both reference values for each patient were analyzed using both reference equation sets and the average percentage difference between the two was calculated. The impact on clinical classification of the severity of DLCO was also investigated.
An average difference of 12.23% between reference values was found in females, and 5.42% in males. This demonstrates that the ECSC percentage predicted values were lower than the GLI, with potential for over diagnosis. These results were clinically significant as the difference is greater than 5%. Hence, an average of 23% of females and 8% males were misclassified based on their severity of DLCO.
In conclusion, a clinically significant difference exists between the ECSC and GLI reference equations. Respiratory departments should strongly consider changing to GLI (2017) to avoid misdiagnosis.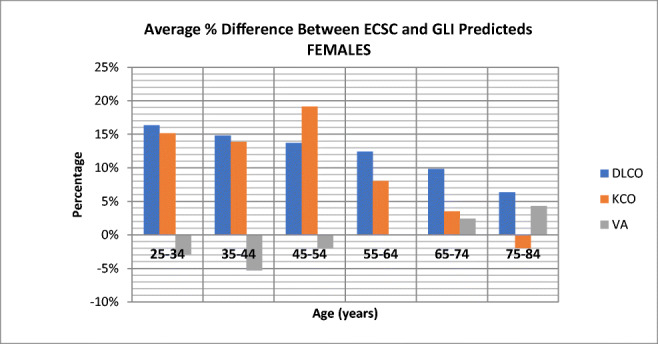
References
1. Oostveen, E., Derom, E., Vints, A. and Liistro, G. (2019). Comparison of ERS′93 to the newly published GLI′17 reference values for carbon monoxide transfer factor. Respiratory Medicine, 146, pp.113-115.
2. Stanojevic, S, Graham, B, Cooper, B, Thompson, B, Carter, K, Francis, R, and Hall, G. (2017) Official ERS technical standards: Global Lung Function Initiative reference values for the carbon monoxide transfer factor for Caucasians. European Respiratory Journal 2017; 50: 1700010
3.3. Worrying changes in adolescent e-cigarette use 2014-2019: A secondary analysis of five Irish health datasets
J Hanafin1, S Sunday1, S Keogan1, L Clancy1
1 TobaccoFree Research Institute Ireland (TFRI), TU Dublin, Dublin 8.
E-cigarette use is increasing worldwide. Concerns about adolescent use include harms (known and unknown), nicotine addiction, and as a “gateway” drug.
Secondary analysis was carried out on five Irish health datasets, with questions on adolescent e-cigarette, all stratified random samples in school-based settings: ECIGS-TFRI 2014 (N=817), ESPAD-TFRI 2015 (N=1508), SILNE-R-TFRI 2016 (N=2051), GUI 2017 (N=6216), ESPAD-TFRI 2019 (N=3556). We report on 16 and 17 year olds.
Descriptive statistical techniques were used to estimate changes in prevalence, reasons for trying e-cigarettes, and relationship with tobacco at first use.
Prevalence of ever-use increased from 23% in 2014 to 39% in 2019, representing a rapid increase, particularly since 2016. Curiosity (66%) and friends (29%) are now the two main reasons adolescents use e-cigarettes. Those saying they had never used tobacco when they first tried e-cigarettes increased from 32% in 2015 to 68% in 2019.
E-cigarette use has risen rapidly among adolescents in Ireland since 2014. E-cigarettes are not used by adolescents for smoking cessation. The majority of adolescents who use e-cigarettes were not smokers when they started using e-cigarettes, pointing to a worrying new route into nicotine addiction. Current tobacco control regulations for young people should be extended to include e-cigarettes.
| Changes in |
16 year olds n (%) |
17 year olds n (%) |
| Prevalence of e-cigarette ever-use | ||
| ESPAD-TFRI 2019 | 754 (38.8) | 279 (37.5) |
| GUI 2017 | 1564 (31.3) | |
| SILNE-R-TFRI 2016 | 148 (31.8) | 85 (50.0) |
| ESPAD-TFRI 2015 | 252 (24.2) | 98 (26.3) |
| ECIGS-TFRI 2014 | 77 (25.7) | 101 (23.0) |
| Reasons for trying e-cigarettes | ||
| ESPAD-TFRI 2019 | ||
|
To quit smoking Because friends were using it Out of curiosity |
16 (3.4) 137 (28.8) 315 (66.3) |
14 (5.0) 83 (29.8) 187 (67.0) |
| ESPAD-TFRI 2015 | ||
|
To quit smoking As an alternative to tobacco smoking Because friends were using it Out of curiosity |
48 (19.2) 27 (10.8) 57 (22.8) 151 (60.4) |
15 (15.5) 9 (9.3) 25 (25.8) 64 (66.0) |
| Relationship with Tobacco when first tried e-cigarettes | ||
| ESPAD-TFRI 2019 | ||
|
I have never smoked tobacco I smoked tobacco occasionally I smoke tobacco regularly |
461 (66.7) 168 (24.3) 57 (8.9) |
149 (58.7) 83 (32.7) 22 (8.7) |
| SILNE-R-TFRI 2016 | ||
|
I have never smoked tobacco I have tried tobacco but don’t use it regularly I smoked tobacco occasionally/regularly |
10 (19.6) 0 (0.0) - |
0 (0.0) 0 (0.0) |
| ESPAD-TFRI 2015 | ||
|
I have never smoked tobacco I smoked tobacco occasionally I smoke tobacco regularly |
76 (32.2) 123 (52.1) 37 (15.7) |
31 (34.1) 42 (46.1) 18 (19.8) |
Table 1. Changes among Irish 16 and 17 year olds between 2014 and 2019 in prevalence of e-cigarette ever-use, reasons for trying e-cigarettes, and relationship with tobacco when first trying e-cigarettes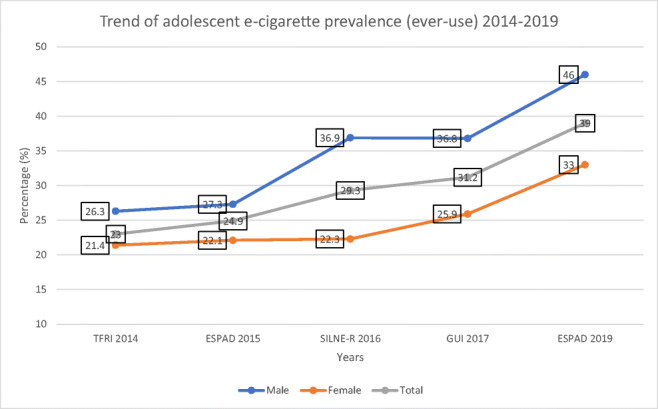
Figure 1: Trend of e-cigarette prevalence between 2014 and 2019
Conflicts of interest: None
References
1. Electronic cigarette use among Irish youth: A cross sectional study of prevalence and associated factors. Babineau K, Taylor K, Clancy L (2015). PLoS ONE 10(5): e0126419. 10.1371/journal.pone.0126419
2. E-cigarettes: effective cessation tools or public health threat?
Clancy L and Babineau K (2016). QJM: An International Journal of Medicine, 109(2):
3.4. Atypical CT Appearance of Thoracic Sarcoid: Case Series
H Dolphin1, M Bolger2, M.P. Rogan1, M.A. Farrell2, S.C. Foley1
1 Department of Respiratory Medicine, University Hospital Waterford
2 Department of Radiology, University Hospital Waterford
The characteristic imaging features of thoracic sarcoid are well recognised and include bihilar and mediastinal lymphadenopathy, perilymphatic pulmonary micronodules and pulmonary fibrosis. However, atypical features occur on CT imaging in up to 30% of cases1. We present a case series of nine patients with atypical CT appearances of thoracic sarcoid from the respiratory chest conference at a tertiary referral centre. Histological confirmation of the diagnosis was made in all cases.
Unilateral hilar adenopathy was an incidental finding in two cases of thoracic sarcoid without respiratory symptoms. Large pulmonary nodules were seen in three patients, two of whom presented asymptomatically. Biopsy of these nodules subsequently confirmed pulmonary sarcoid. Wedge-shaped and patchy ground glass airspace opacifications were imaged in four patients who presented variably with dry cough and dyspnoea and had ultimate histological confirmation of sarcoidosis.
The imaging features of bilateral hilar and mediastinal adenopathy with/without pulmonary parenchymal micronodularity are characteristic for the disease and present in approximately 70% of patients2. However sarcoidosis is coined “the great mimicker” due to its many ambiguous forms of atypical imaging features as described. Recognition of the atypical CT appearances of the disease is relevant for treating physicians and radiologists.
References
1. E Cariado et al. Pulmonary Sarcoidosis: Typical and Atypical Manifestations at High-Resolution CT with Pathologic Correlation. Radiograhics. 2010 Oct;30(6):1567-86
2. Miller BH, Rosado-de-Christenson ML, McAdams HP, Fishback NF. Thoracic sarcoidosis: radiologic pathologic correlation. RadioGraphics 1995;15(2): 421–437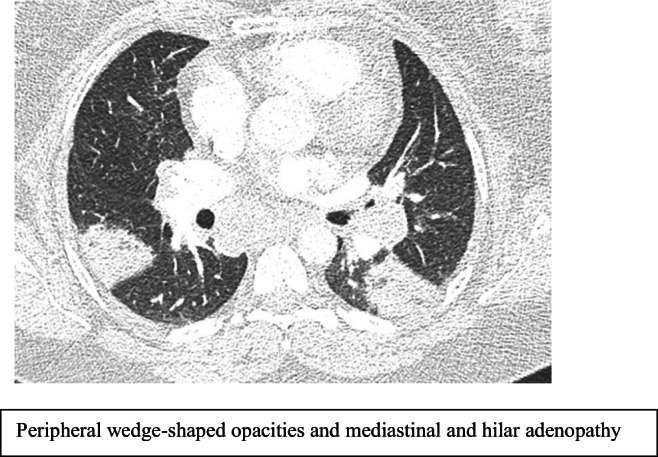
3.5. Is there a role for tracheobronchoplasty in patients with severe debilitating airway obstruction?
JB Mc Loughlin1, D Rice1 and K Redmond1
1 Department of Thoracic Surgery, Mater Misericordiae University Hospital, Dublin
Tracheobronchomalacia (TBM) is a condition characterised by a pathologic collapse of the posterior membrane of the upper airways. This produces a dynamic outflow obstruction leading to an array of respiratory symptoms. The management of these patients is complex with therapeutic interventions carrying significant risks.
We describe three patients with severe TBM that have undergone a trial of carinal stenting to assess for suitability for tracheobronchoplasty (TBP).
| Patient | Age | Gender | Duration of Stent | ECMO for Stent Insertion |
| 1. | 68 | Male | 13 months | No |
| 2. | 67 | Male | 3 months | Yes |
| 3. | 64 | Female | 2 months | No |
In all cases a trial period of carinal stenting was performed successfully. Extracorporeal membrane oxygenation (ECMO) was used electively in one case. Each patient enjoyed symptomatic improvement demonstrating the suitability of these patients for surgical airway stabilisation. Carinal stenting is not a long term solution for these patients given the associated iatrogenic symptoms.
TBP is an invasive procedure involving the plication of the redundant posterior membranous wall using a polypropylene mesh through a thoracotomy incision. It requires thorough pre-operative work-up, careful patient selection, optimisation of any overlap conditions. International experience has demonstrated good long term results including; symptom improvement, prolonged airway patency and improved quality of life. There is a cohort of Irish patients that warrants work-up for consideration of TBP.
3.6. Clinical characteristics of Birt-Hogg-Dube Syndrome in an Irish Cohort
O’Carroll OM1, Gaffney B1, Cullen J2, Murphy D.J.3, Dodd J.D.3,5, Fabre A4,5, Keane M.P.1,5, McCarthy C1,5
1 Department of Respiratory Medicine, St. Vincent’s University Hospital, Elm Park, Dublin 4
2 Department of Respiratory Medicine, Tallaght University Hospital, Dublin 24
3 Department of Radiology, St Vincent’s University Hospital, Elm Park, Dublin 4
4 Department of Histopathology, St. Vincent’s University Hospital, Elm Park, Dublin 4
5 Department of Medicine, University College Dublin, Dublin 4
Birt-Hogg-Dube Syndrome (BHD) is a rare autosomal dominant disorder resulting from mutations in the FLCN gene. It is characterised by pulmonary cysts, fibrofolliculomas of the skin, and increased risk of spontaneous pneumothorax and renal malignancy. The clinical presentation of this disease is variable, even within families.
The clinical and genetic characteristics of a cohort of patients attending a single referral centre in Ireland were assessed.
16 patients, 11 of which came from 3 families, were included for analysis. 10 patients were female (62.5%). Median age was 50.5 years (range:19-86). 2 were current smokers (12.5%), 4 ex-smokers (25%), and 10 never smokers (62.5%). All had FLCN mutations confirmed, the most common mutation was C.17_21delCTCTC. 9 patients (56.25%) had had at least one spontaneous pneumothorax and one patient had suffered spontaneous pneumomediastinum. Most patients had pneumothorax aged 30-35. 8 patients (50%) had fibrofolliculomas. No patient had any renal tumour.
BHD is a rare condition which can result in variable clinical presentation, even in families with the same genetic mutation. Studies such as this add to the understanding of the complexity of this rare disease. We aim to define the natural history in a larger cohort.
3.7. Use of non-invasive ventilation in Motor Neuron Disease – a retrospective cohort analysis
Walsh LJ1, Deasy KF1, Ryan A2, Murphy DM1,3
1. Department of Respiratory Medicine, Cork University Hospital, Cork, Ireland.
2. Department of Neurology, Cork University Hospital, Cork, Ireland.
3. Health Research Board, Clinical Research Facility, University College Cork, Cork.
Motor neuron disease (MND) is a neurodegenerative disorder which leads to progressive muscle weakness including respiratory muscle function decline. The introduction of non-invasive ventilation (NIV) has been shown to improve quality of life, survival and slow the rate of pulmonary function decline.
A retrospective chart analysis of patients who attended the MND clinic from 2009 -2019 in Cork University Hospital, Ireland, was carried out to evaluate if NIV and greater compliance with NIV improved survival. Information regarding NIV use, compliance, pulmonary function tests (PFTs) and basic patient demographics was collected. In total 111 patients were included in the study.
The mean age at diagnosis was 63.8 years and 61.3% were males. 45.2% used NIV for more than 4 hours per night and 66.7% were compliant. There was a statistically significant longer survival in the bulbar group who used and were compliant with NIV compared to those who did not use NIV (p=0.02). Bulbar onset MND had worse SNIP and peak cough flow at diagnosis.
We found a significantly longer survival with the use of NIV in those with bulbar onset MND but this was not reflected in the patient cohort as a whole.
3.8. Improving Internal Medicine Trainee’s Experience: Introduction of a Pleural Skills Lab
Cullen D1, Hagan C1, Polley L1, John A1, Green A1, Chapman N1, Convery R1, McNicholl D1
1 Department of Respiratory Medicine, Craigavon Area Hospital, 68 Lurgan Road, Portadown BT63 5QQ
Introduction: The Internal Medicine curriculum states IMT trainees should be competent in pleural procedures including pleural aspiration and chest drain insertion
Aim: To introduce a pleural skills lab to cover the objectives set out by JRCPTB in the Internal Medicine Trainee (IMT) curriculum. We aimed to cover pleural aspiration and chest drain insertion for fluid and pneumothorax. This is part of our wider aim to improve the overall Internal Medicine Trainee experience.
Methods: We designed and sent out a survey to trainees within our hospital. The survey had an 80% response rate with all respondents registering interest. One trainee had skills lab training previously and similarly, one trainee had a previous DOPS for pleural procedures. As expected, trainees who had no previous exposure to Respiratory Medicine found sign off challenging.
We designed a 90 minute teaching session based on the IMT curriculum and using British Thoracic Society guidelines delivered an initial didactic teaching session, moving onto interactive teaching with the assistance of the Blue Phantom training model led by senior respiratory physicians.
Results: 80% of Internal medical trainees attended the session and all achieved skills lab competence fulfilling curriculum requirements and with positive feedback to educators.
Conclusion: A pleural procedure skills lab can be delivered in a general district hospital with limited resources, improving junior doctor’s skills and educational experience.
3.9. To lyse or not lyse that is the question?
Murray A1, Deshpande R1, Donaghy C1, Hayes E1,
1 Department of Medicine, Daisy Hill Hospital, Southern Health & Social Care Trust.
Pulmonary embolism (PE) is a significant cause of death and morbidity, 5% of all hospital deaths are attributable to PE. Prompt recognition and treatment are essential for minimizing the mortality and morbidity associated with PE.
Lysis decisions remain challenging for physicians. In massive PE, with haemodynamic collapse, the robust evidence base for the administration of fibrinolysis is well defined. However, there has been considerable debate on the benefits of lysis in sub-massive PE as evidenced by the Peitho trial (1)
We are nearing completion of a comprehensive trust wide protocol to help guide these decisions whilst still allowing an individualized approach to patient care. This protocol involved evidenced based analysis and inter-departmental collaboration. An extensive teaching programme on the protocol has been implemented prior to its trust-wide roll out.
Our work on this project has highlighted the complexity surrounding decision making in critically ill patients who are being considered for lysis. Our protocol sets out comprehensive guidance which is evidence based to help standardize patient care.
References
(1) Fibrinolysis for patients with intermediate-risk Pulmonary embolism Meyer G, et al. N Engl J Med. 2014 Apr 10;370 (15):1402-11
3.10. Proteomic analysis reveals different responses to hypoxia in male and female human pulmonary microvascular endothelial cells
Daria Kostyunina1, Eugene Dillon2, Keith Rochfort3, Philip Cummins3, Paul McLoughlin1
1) School of Medicine, Conway Institute, University College Dublin;
2) Conway Institute, University College Dublin;
3) School of Biotechnology and National Institute for Cellular Biotechnology, Dublin City University.
Pulmonary arterial hypertension (PAH) is a severe pulmonary disease which is more common in women. Sex hormone independent mechanisms were recently shown to contribute to the higher incidence in females but the specific mechanisms are unknown. Pulmonary endothelial cell abnormalities are central in the development of PAH and hypoxia is one of the stimuli that leads to these abnormalities. The aim of this study was to test the hypothesis that female predominance in PAH is due to different endothelial cell responses to hypoxia compared to males, which are independent of sex hormones.
Human pulmonary microvascular endothelial cells (HPMEC) from 3 male and 3 female age matched donors were placed either in normoxia or hypoxia (1%O2, 24/48 hours).
Proteomic data analysis revealed pathways that were enriched in females compared to males in hypoxia: “hypoxia”, “KRAS signalingDn”, “glycolysis”, “MYC targetsV2”, and “spermatogenesis”. Proteins that showed sex-dependent responses included thymosin-β 4 and glucose-6-phosphate-1-dehydrogenase, which X-chromosome linked, and previously implicated in PAH.
Proteomic analysis revealed that 1) hypoxic responses of female and male HPMEC are different 2) X chromosome linked proteins may play a role in the sex-dependent differences of HPMEC responses to hypoxia. These factors may contribute to the female predominance in PAH.
3.11. Gender difference results in increase in adolescent smoking in 2019 in Ireland- European trend analysis of current smoking prevalence 1995-2019
J Hanafin1, S Sunday1, S Keogan1, Luke Clancy1
1 TobaccoFree Research Institute Ireland (TFRI), TU Dublin, Dublin 8
We examine trends in 30-day smoking among adolescents in Ireland and Europe, 1995-2020.
Ireland has participated in seven data collection waves of ESPAD (European Schools Project for Alcohol and Other Drugs) between 1995 and 2019, during which time more than 500,000 students have completed questionnaires on substance use, including cigarettes.
In 2019, some 100,000 students participated in ESPAD. In Ireland, 1967 students, born in 2003, were surveyed from a stratified random sample of 50 Irish schools.
We compared prevalence and gender differences in the Irish and European samples at different time points from 1995 to 2019.
In Ireland and across Europe, total prevalence of 30-day smoking decreased significantly between 1995 and 2019. Ireland’s decrease (from 41% to 14%) was more dramatic than the European average (32% to 20%). Ireland’s current prevalence is lower than the European average. However, while there was a decline of 5% in the European average between 2015 and 2019, Ireland’s decreasing trend reversed, accounted for by an increase in male smoking from 13% to 16%.
In Ireland, smoking prevalence in 15-16-year-olds has increased for the first time in 25 years. Further focused action is urgently needed to achieve a prevalence of 5% by 2025.
Conflicts of interest: None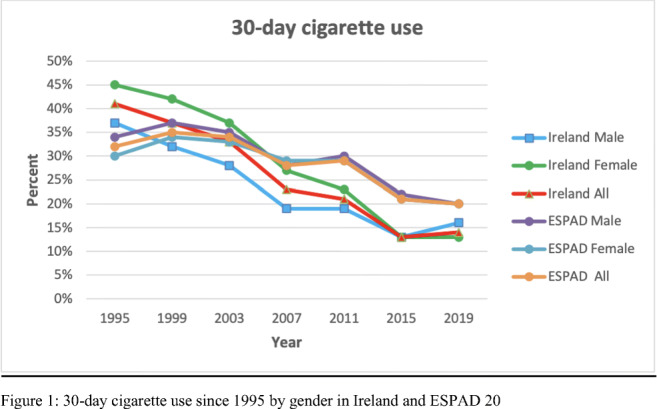
3.12. Standardising the Delivery of High Flow Nasal Oxygen on a Respiratory Ward
N Ferguson1, D Comer1, D Moore1, T Craig1.
1 Mater Hospital, Belfast, UK
High flow nasal oxygen (HFNO) is used to treat patients with hypoxic respiratory failure.(1,2) HFNO use must be accompanied by forward planning in terms of whether escalation to critical care is appropriate.(1) HFNO is usually initiated by junior doctors, and we had observed that in this patient group, less than 50% of had an escalation plan determined within 24 hours.
Our aim was to promote HFNO awareness, provide educational sessions, design a proforma with emphasis on escalation planning, and collate medical staff and patient feedback.We therefore designed a HFNO proforma which included indication, initiation and weaning, and to include an escalation plan timely countersigned by a respiratory consultant.
We achieved over 80% compliance in terms of use of our proforma indicating escalation planning was both established early and consultant led. This was discussed with the patient at the time. Feedback from the medical staff was positive. Although the majority of patients regarded HFNO comfortable, they were often unclear of its indication.
Promoting HFNO awareness and providing educational sessions resulted in a positive and sustained uptake of the proforma. This resulted in both earlier consultant led escalation planning and discussion with the patients and families. Feedback from educational sessions was positive.
References
1) O’Neill et al. 2017 ‘High Flow Nasal Oxygen (HFNO): Use and management for adult inpatients in secondary care’. BHSCT policy v1.0
2) Roca O, Riera J, Torres F, Masclans JR (2010) High-flow oxygen therapy in respiratory failure Respiratory Care;55(4), 408-413
3.13. Gallbladder polyps in patients receiving subcutaneous treprostinil therapy for Pulmonary Arterial Hypertension.
Cullivan S1, Boyle N1, Mc Cullagh B1, Gaine SP1
1. National Pulmonary Hypertension Unit, Mater Misericordiae University Hospital, Ireland
Idiopathic pulmonary arterial hypertension (IPAH) is a devastating illness characterised by progressive pulmonary vascular remodelling, proliferation and obliteration. Prostacyclin therapy is a core component of treatment, as it exerts beneficial pulmonary vasodilatory, antiproliferative, anti-inflammatory and antiplatelet properties. Interestingly prostacyclin analogues are not specific for the prostacyclin (IP) receptor and bind additional prostanoid receptors; this is exemplified by treprostinil, which mediates its physiological effects via a combination of IP, prostaglandin E2 (EP2) and prostaglandin D1 receptors (1). Outside of the pulmonary vasculature, prostacyclin has diverse functions including a recognised role in gallbladder physiology (2).
In our centre, a total of 50 patients are currently prescribed exogenous prostacyclin therapy for pulmonary hypertension and 8 have recent gallbladder imaging. Gallbladder polyps were identified in 3 of these 8 cases (37.5%) and all of these received prolonged treprostinil (Remodulin) therapy (Table 1). These results are higher than anticipated, as studies have reported gallbladder polyp prevalence between 1.4 - 12% in the general population.
We describe three cases of incidental gallbladder polyps in patients with IPAH and hypothesize that treprostinil may be implicated in the formation of these gallbladder polyps, due to its specific effects on IP and EP2 receptors and the established role of prostanoids in gallbladder health and disease.
Conflicts of interest: None
Table 1
Clinical characteristics of three cases of asymptomatic gallbladder polyps in patients prescribed prostacyclin analogues for IPAH. *The patient in Case 3 was transitioned from subcutaneous treprostinil to IV epoprostenol in August 2019
| Case 1 | Case 2 | Case 3 | |
| Patient characteristics | |||
| Age | 60 | 47 | 48 |
| Gender | Female | Male | Female |
| BMI | 22 | 25 | 20 |
| Duration of IPAH (years) | 17 | 18 | 16 |
| NYHA | II | III | II |
| PH therapy |
Sildenafil Macitentan Treprostinil |
Sildenafil Macitentan Treprostinil |
Sildenafil Ambrisentan Treprostinil/ Epoprostenol* |
| Treprostinil dose (ng/kg/min) | 30 | 60 | N/A |
| Treprostinil duration (years) | 15 | 12 | 8 |
| Treprostinil route | S/C | S/C | S/C |
| additional medications |
Burinex, Aldactone, Gabapentin Prednisolone |
Pantoprazole, Furosemide Gabapentin |
Frumil Singulair Venlafaxine Warfarin |
| Biochemistry | |||
| Bilirubin | 32 | 10 | 13 |
| Alkaline phosphatase | 45 | 80 | 83 |
| yGT | 18 | 19 | 50 |
| Total cholesterol | 5.1 | 4.7 | 5.1 |
| Fasting triglycerides | 1.05 | 1.26 | 2.03 |
| HDL | 1.2 | 1.06 | 1.09 |
| LDL | 3.4 | 3.1 | 3.4 |
| Non HDL cholesterol | 3.9 | 3.6 | 4 |
| Gallbladder imaging | |||
| Indication for ultrasound | Transplant assessment | Transplant assessment | Transplant assessment |
| Symptomatic gallbladder disease | No | No | No |
| Largest polyp size (mm) | 7 | 5 | 9.5 |
| Total polyp count | >1 | 3 | >10 |
References
1. Whittle BJ, Silverstein AM, Mottola DM, Clapp LH. Binding and activity of the prostacyclin receptor (IP) agonists, treprostinil and iloprost, at human prostanoid receptors: treprostinil is a potent DP1 and EP2 agonist. Biochem Pharmacol. 2012;84(1):68-75. 10.1016/j.bcp.2012.03.012
2. Myers SI, Bartula L. Human cholecystitis is associated with increased gallbladder prostaglandin I2 and prostaglandin E2 synthesis. Hepatology. 1992;16(5):1176-1179
3.14. Incorporating Virtual Telehealth into the Oxygen Clinic in Tallaght University Hospital (TUH).
Cunneen S.1, Baily-Scanlan M1., Cullen J1.
1 Physiotherapy and Respiratory Departments, Tallaght University Hospital.
The implementation of telemedicine services was necessitated internationally due to Covid-19 restrictions. A guidance document1 was published on the incorporation of virtual telehealth into oxygen clinics and TUH piloted the first virtual oxygen clinic in Ireland.
Patients on the waiting list were triaged, prioritised and further categorised based on their suitability for a virtual assessment (VA) 1. VAs took place over the phone and patientMpower SpO2 monitors were used for remote monitoring. The one minute sit-to-stand test was used in place of the six minute walk test2.
The pilot ran over a 3-month period and 66 patients attended the oxygen clinic during this time; 50% of attendances were VAs. Only patients who required an intervention that had to be completed face-to-face attended the hospital. Of the 33 VAs, the requirement for a subsequent face-to-face appointment was low (n=2), highlighting the efficacy of the triage system. Patients who received a VA reported they had no preference regarding virtual or face to-face appointments (n=10) or that they preferred VA (n=23).
The incorporation of VAs improved access to the oxygen clinic during Covid-19 and has resulted in a change in practice. Prioritisation, categorisation and VAs will continue to be a vital aspect of waiting list management going forward, with patients only attending for face-to-face appointments if they cannot be assessed virtually.
References
1. Murphy, D., Curtis, S., Cunneen, S., Cribbin, E. National Clinical Programme for Respiratory (COPD & Asthma) Guidance for the process of incorporating Virtual Teleheath into existing Oxygen Clinics. (2020).
2. Bohannon RW, Crouch R. 1-minute Sit to stand Test: Systematic Review of Procedures, Performance, and Clininetric Properties. Journal of Cardiopulmonary Rehabilitation and Prevention 2019; 39(1): 2-8.
3.15. Pulmonary Embolism assessment why are we still getting it wrong!
C. Donaghy1, A Murray1, T. Byrne1, H. Kennedy1, R. Kerr1, L. McConville1, G. McCurdy1, A. Mclean1, D. Rafferty1, C. Sharkey1, E Hayes1
1 Dept of Respiratory Medicine, Daisy Hill Hospital, Southern Health and Social Care Trust
In haemodynamically stable patients a systematic approach to assessment should be undertaken to avoid unnecessary investigations. Whenever Pulmonary Embolism (PE) is suspected the pretest probability should be assessed. Meta-analyses suggest that probability scores may have higher specificity and increase the diagnostic yield of CTPA (1). Despite this they are used incorrectly in up to 80 percent of patients. (2)
We retrospectively audited patients who underwent CT pulmonary angiogram (CTPA) for a possible PE diagnosis in our hospital. Data was collected on each patients Wells score, D-dimer, bed days, Investigations and Pulmonary Embolism Severity Index Score (PESI.)
Results showed that PE detection percentage was in the range of 14% which is considered below the accepted standards set by clinical radiology. D-Dimers were performed inappropriately in 33% of patients. 70% of patients were found not to have had basic investigations completed. 55.5% of patients admitted to hospital had a PESI score of class 2 or less.
Patients continue to have incomplete assessments done prior to CTPA. Pre-test probability scoring has been shown to significantly improve detection rates of PE but continues to be underutilized in clinicians. Furthermore with the use of the PESI score a significant proportion of patients could be managed in the ambulatory setting.
References
(1) Wang RC, Bent S, Weber E, et al. The Impact of Clinical Decision Rules on Computed Tomography Use and Yield for Pulmonary Embolism: A Systematic Review and Meta-analysis. Ann Emerg Med 2016; 67:693.
(2) Newnham M, Stone H, Summerfield R, Mustfa N. Performance of algorithms and pre-test probability scores is often overlooked in the diagnosis of pulmonary embolism. BMJ 2013; 346:f1557
3.16. Evaluation of a Multidisciplinary Breathlessness Support Service for individuals with chronic refractory breathlessness.
Julie Goss,1 Amanda Drury,2, 3 Jide Afolabi, 1 Gillian Mc Hugh, 1Norma O’Leary,1 & Anne-Marie Brady3
1 Our Lady’s Hospice & Care Services. Harold’s Cross, Dublin D6W, RY72
2 School of Nursing, Midwifery and Health Systems, College of Health and Agricultural Sciences, University College Dublin, Belfield, Dublin 4.
3 School of Nursing & Midwifery, Faculty of Health Sciences, Trinity College Dublin, 24 D'Olier Street, Dublin 2, Ireland, D02 T283.
Chronic refractory breathlessness is defined as breathlessness at rest or with minimal exertion that persists despite optimal treatment of the underlying cause. 1 It is a frightening symptom that decreases physical, mental and social functioning with wider implications for the individual, caregivers and health systems. The Multidisciplinary Breathlessness Support Service (MBSS) provides a brief intervention to support the management of refractory breathlessness in an outpatient palliative care setting.
A longitudinal mixed methods study was conducted. Service users (n=10) completed questionnaire including Chronic Respiratory Questionnaires [CRQ]), (Dyspnoea-12 [D-12]; and healthcare experience at T1 (at admission) and T2 (after discharge). A subsample of service users (n=8), referrers (n=2) and carers (n-1) were interviewed after T2 to discuss their experiences of using the service.
CRQ subscales demonstrated enhanced mastery (p=0.013), emotional function (p=0.014) and reduced fatigue (p=0.012). Statistically non – significant effects noted on [D-12]; and [CRQ] dyspnoea subscale. Interviewees, uniformly described positive impacts on their functional and emotional well-being.
The results of this study suggest that a multidisciplinary intervention which reflects service users individualised goals is feasible and positively affects emotional well-being, fatigue and mastery of this difficult symptom. Further exploration is needed to examine duration of effect of the intervention.
References
1. Currow D. and Johnson M.(2016) Distilling the essence of breathlessness: the first vital symptom. European Respiratory Journal 45, 1526-1528.
3.17. Oxygen Prescription & Administration to Inpatients at Midland Regional Hospital Tullamore – An Audit
Aneet Kumar1, Hidayat Ullah1, Hashim Khan1, Youssef Guirguis1,
1 Midlands Regional Hospital Tullamore
Oxygen is one of the most common drugs used in the acute care of patients. The aim of this audit was to evaluate if oxygen was prescribed as per Irish Thoracic Society guidelines at Midlands Regional Hospital Tullamore showing oxygen prescription, SpO2, flow rate, target SpO2, delivery system, duration period/review date, continuous or as required (PRN) in the drug Kardex.
Inpatients data was collected on 4 medical, 1 surgical and 1 orthopaedic wards on the 15th of June 2020. Demographics, comorbidities, indication and prescription for oxygen therapy, SpO2 and target levels & mechanism of oxygen delivery were obtained.
Out of total 135 inpatients, 22(16.30%) received oxygen but none (0%) of these patients had oxygen prescribed on the dedicated oxygen prescription section in the drug Kardex. 17/22 (77.27%) patients received oxygen via nasal prongs. 3/22 (13.64%) via Airvo & 1 (4.54%) patient via tracheostomy. 6 (27.27%) patients had no clear indications for supplemental oxygen therapy, though 6(37.5%) patients had known COPD, 3 (18.75%) ILD, 3 (18.75%) Pulmonary Oedema & 2 (12.5%) had Pneumonia.
Our results have been alarming regarding oxygen prescription & documentation. A targeted intervention can effectively improve compliance with oxygen prescription through educating prescribers, nurses, physiotherapists, pharmacists, and requiring nurse’s signature for Oxygen therapy at each drug round.
References
1. Irish Thoracic Society. Irish Guidelines on the Administration of Oxygen Therapy in the Acute Clinical Setting in Adults 2017. 1–38 (2017).
2. O’Donnell, C., Davis, P. & McDonnell, T. Oxygen Therapy in Ireland: A Nationwide Review of Delivery, Monitoring and Cost Implications. Ir. Med. J. 112, 933 (2019).
3.18. An audit of the documentation of well’s score and or D-Dimers for CTPA requests in the Mater x Hospital.
D McMorrough1, J Khan1, S Gaine1.
1Mater Misercordiae University Hospital, Eccles Street, Dublin 7.
HSE & Mater Misercordiae University Hospital (MMUH) guidelines state a patient requiring a CTPA should have both D-Dimer and Wells score documented on the order.
This study aimed to review CTPA orders made over 2 discreet 7-day periods in January (n=38) and May 2020 (n=33) in cases where Pulmonary Embolus was suspected. There orders were examined to evaluate the proportion of CTPA orders that took D-Dimer, Well’s Score or both into account, in accordance with the agreed standard of care.
While no CTPA ordered during the study period took both metrics into account, there was a significant increase in the proportion of orders that mentioned D-Dimer levels from 24% in January to 58% of orders made in May. The proportion of orders that included a Well’s score fell from 15% to 3% from January to May.
While there was an increase in the proportion of orders that recorded D-Dimers, there is still significant room for improvement the ordering of CTPA scans. In particular, when coupled with the negative predictive value of D-Dimer levels, the inclusion of a Wells score could help reduce the burden of unnecessary scans on both patients and the radiology departments across the HSE.
References
Rajagopalan P, Digby JW, Lee C, Barker RD. Does Wells score documentation really prevent excessive CTPA requests in a teaching hospital? A retrospective study in 800 patients. European Respiratory Journal. 2014 Sep 1;44(Suppl 58).
3.19. Pneumothorax; Collapse or compliance? An audit of the management of pneumothorax in an Irish tertiary teaching centre.
E McNally1, L Gleeson1
1 Department of Respiratory Medicine, St James Hospital, Dublin, Ireland
Pneumothorax (PTX) commonly presents to hospital however approach to management varies. We compared our management of PTX with most recent guidelines by The British Thoracic Society (BTS).
We conducted a retrospective review of admitted patients with PTX recorded as the primary diagnosis, excluding those electively admitted or transferred for advanced management of a persistent PTX under cardiothoracic surgery (CTS). We included 28 patients(n=28). 12(43%) primary spontaneous PTX, 16(57%) secondary spontaneous PTX. 4(14%) were admitted under CTS, 1(3%) oncology, 15(54%) pulmonology and 8(29%) general medicine.
The size measured at hilum ranged from 0.7cm– 11cm. 8(29%) cases were classified as ‘small’ ie <2cm. 3 proceeded immediately to placement of an intercostal drain. 1 required pleural aspiration followed by drainage. 4 underwent observation with 2 ultimately requiring drain placement for extension of PTX and 2 requiring no further intervention. Average length of stay among this subgroup was 2.5 days.
There was inconsistency across documentation. In 13(46%) cases, suction was applied however the timing was ambiguous in 4(14%). In 8(29%) instances, the type and size of drain was unclear. There was no documentation of safety advice for 10(36%). Overall, we showed compliance with guidelines but highlighted scope to manage a select group with PTX <2cm as outpatients.
3.20. An Overview of Minimally Invasive Pectus Excavatum Repairs available in Ireland
D Rice1, S Barrett1, J McLoughlin1, R Fleck1, KC Redmond1
1 Department of Thoracic Surgery, Mater Misercordiae University Hospital, Dublin Ireland
Pectus excavatum (PE) is the most common congenital deformity of the thoracic wall, characterised by an inwards turned sternum, resulting in a concave “funnel-like” chest. PE is associated with a wide spectrum of clinical presentations with questionable cardiopulmonary effects and psychosocial concerns re aesthetics.
PE is traditionally managed by two main surgical techniques; the open “Ravitch” method and the less invasive “Nuss” method. Due to the potential for major complications and internal organ damage, further less invasive techniques have been developed with a view to reducing post-operative morbidity, decreasing operative times and hospital stay length, and primarily focus on improving cosmesis.
Pectus Up is an innovative, minimally invasive set of implants and tools, centred around a new procedure called taulinoplastia, which involves elevating the sternum before securing it with a bioinert plate.
Alternatively, a custom made implant, offered by Anatomik modelling, can be inserted superficial to the patient’s sternum. Silicone implants are specifically engineered using computer assisted design (CAD), tailored to a patient’s unique anatomy based on imaging, and implanted with a superficial, straightforward procedure.
A series of patients, following the lifting of Covid19 public health restrictions are undergoing minimally invasive corrective surgery for PE. A review of the evidence base and available techniques including operative videos will be presented.
3.21. Burden of Nasal Symptoms in Motor Neuron Disease patients
M Talty1, F Gargoum1, R Rutherford1.
1 Respiratory Dept, Galway University Hospital.
There is a lot of attention given to serially assessing the strength of the inspiratory1,2 and expiratory muscles in MND patients to try and predict impending respiratory and sputum clearance failure. To our knowledge, there have been no studies looking at the effect of weak respiratory muscles on the patient’s ability to clear their upper airway. This can be a distressing symptom for patients and reduce the efficacy of non-invasive ventilation.
We, therefore, surveyed our patients by questionnaire to assess their burden of nasal symptomatology. 21 out of 30 (70%) patients responded and consented. 14 (66%), described regular nasal and/or sinus symptoms, occurring ≥ a few times a week. 11 (52%) reported a moderate or greater impact on QoL. 16 (63%) reported difficulty with nasal congestion and an inability to adequately clear their nose, 9 (56%) of whom felt it was due to an inability to generate enough expiratory force. 9 (45%) patients employed NIV, none of whom reported an impact on its use.
In this small study we identified a significant burden of nasal symptomatology in our MND population. Topical medications, breath stacking and single nostril expulsion technique could all play an important role in ameliorating this symptom.
References
1. Chaudri MB, Liu C, Watson L, Jefferson D, Kinnear WJ. Sniff nasal inspiratory pressure as a marker of respiratory function in motor neuron disease. European Respiratory Journal. 2000 Mar 1;15(3):539-42.
2. Janssens JP, Adler D, Ferfoglia RI, Poncet A, Graf LG, Leuchter I, Imhof ME, Barras AC. Assessing Inspiratory Muscle Strength for Early Detection of Respiratory Failure in Motor Neuron Disease: Should We Use MIP, SNIP, or Both?. Respiration. 2019;98(2):114-24.
3.22. Compliance of CXR follow up- An Audit, Beaumont Hospital
S. Toland1, S. Collins1, P. Branagan1.
1 Department of Respiratory Medicine, Beaumont Hospital, Dublin 9, Ireland.
Pneumonia affects around 8 in 1,000 adults each year in Ireland.1 British Thoracic Society (BTS) Guidelines state that all patients admitted to hospital with community acquired pneumonia (CAP) should have a follow up chest x-ray (CXR) within 6 weeks of being discharged from hospital.2
The aim of this retrospective audit is to evaluate whether follow-up CXRs were performed on patients admitted with radiologically confirmed pneumonia within the correct time frame as outlined in the BTS guidelines. We randomly selected 100 patients who were admitted via the emergency department in Beaumont Hospital between October 1st and November 31ST 2019 with a consolidation evident on their admission CXR.
100 patients were identified, 52% were female 48% male with a median age of 64.5 years. 45% did not have any follow up imaging. 55% did have follow up imaging, of which 45% had their CXR within 6 weeks of discharge, 32.7% within 6-12 weeks, 12 21.8% greater than 12 weeks. 72.7% had full resolution.
55 patients had follow-up chest imaging, with 25 fulfilling the BTS guidelines. This means that potential lung cancer diagnoses/other respiratory conditions may be delayed. Our plan is to educate the importance of follow up CXRs and we plan to re-audit in 3 months.
References
1. Pneumonia - Overview [Internet]. Www2.hse.ie. 2020 [cited 30 August 2020]. Available from: https://www.2.hse.ie/conditions/pneumonia/pneumonia-overview.html#:~:text=Pneumonia%20affects%20around%208%20in,very%20young%20or%20the%20elderly.
2. British Thoracic Society Guidance on Respiratory Follow Up of Patients with a Clinico-Radiological Diagnosis of COVID-19 Pneumonia [Internet]. British Thoracic Society; 2020 [cited 30 August 2020]. Available from: https://www.brit-thoracic.org.uk/about-us/covid-19-information-for-the-respiratory-community/
3.23. Creating a High Flow Nasal Cannula (HFNC) AirvoTM Protocol in Beaumont Hospital
S Toland1, CD Campbell1, P Branagan1.
1 Department of Respiratory Medicine, Beaumont Hospital, Dublin 9, Ireland.
HFNC oxygen therapy (AirvoTM) delivers humidified and heated air at flows up to 60litres/minute and FiO2 from 21% to 100%. Its use in critically unwell patients with respiratory failure has been increasing rapidly. HFNC reduces the anatomical dead space, provides a mild positive end-expiratory pressure, maintains consistent FiO2 and humidification. HFNC has been shown to be efficacious in hypoxic and hypercapnic respiratory failure, weaning from NIV and reducing the need for reintubation in the ICU.
We conducted an NCHD wide survey assessing their knowledge of HFNC particularly looking at indications/contraindications as well as their overall confidence in initiating HFNC prior to implementing a hospital wide policy.
59 NCHDs from all disciplines completed the survey. 26 (44.07%) had previously commenced a patient on HFNC, 33 (59.03%) had not. 12 ( 20.34%) reported they felt confident in initiating a patient on HFNC ,16 ( 27.12%) reported knowledge of the required settings. 57 (96.6%) of respondents reported they would feel more confident initiating HFNC if there was a policy available.
Based on the results of our study, a hospital wide policy on the use of HFNC was
implemented, including clear indications/contraindications, infection control measures, appropriate settings and a flow diagram outlining monitoring and escalation of care. We will re-audit in three months time.
3.24. Optimum viscosity of a perfusion solution reduces oedema formation in the isolated mouse lung.
D Walsh1, J F Boylan2, P McLoughlin1
1. School of Medicine and Conway Institute, University College Dublin.
2. Department of Anaesthesia and Critical Care Medicine, St. Vincent’s University Hospital, Dublin.
Intravenous fluid therapy is a cornerstone in the resuscitation of acute hypotensive states. However, resuscitation strategies can cause marked haemodilution, reducing plasma protein concentration, plasma oncotic pressure, and blood viscosity, with subsequent interstitial and pulmonary oedema formation (1). We have recently reported that perfusing isolated murine lungs with a solution with a relative viscosity (RV) of 2.5, adjusted with a biocompatible macromolecule, reduced the rate of oedema formation when compared to a solution with a viscosity lower than blood (RV1.5) (2). We now report work identifying the optimum viscosity of perfusing solutions and demonstrate that the beneficial effect of optimum viscosity solutions is independent of the macromolecules used to increase RV.
Mouse lungs were isolated and perfused ex vivo until oedema developed or 180 minutes had elapsed. Perfusion solution with low viscosity (RV 1.5) was compared to higher viscosity solutions (RV 2.0, 2.25, 2.5). RV1.5 comprised Dulbecco’s Modified Eagle Medium with Ficoll PM (40g/l) added. Higher viscosities solutions were prepared by adding one of the following high molecular weight polymers: Ficoll PM400, or Dextrans of different molecular weights (>300kDa) at concentrations sufficient to achieve the target RV. Oedema formation was assessed using Wet:Dry weight ratios(W:D).
Using Ficoll 400kDa, lungs perfused with solution RV2.5 had significantly lower (P<0.05) W:D than RV2.0. Perfusate with RV2.25 was similar to RV2.5. When perfusates with RV2.5 were prepared using two different high molecular Dextran solutions (>300kDa), W:D was also significantly lower (P<0.05) compared to RV1.5.
Perfusion solutions exhibiting an optimum viscosity (RV2.5) reduced interstitial oedema formation in isolated lungs. This effect is independent of the exact concentrations or chemical structures of the biocompatible macromolecules used to alter viscosity. Further work exploring the potential impact of reduced blood viscosity caused by haemodilution during standard resuscitation protocols is needed.
Acknowledgments
1. British Journal of Anaesthesia/ Royal College of Anaesthesia - WKR0-2019-0074 Project Grant.
2. St Vincent’s Anaesthesia Foundation.
References
1. Maiden MJ, Finnis ME, Peake S, McRae S, Delaney A, Bailey M, et al. Haemoglobin concentration and volume of intravenous fluids in septic shock in the ARISE trial. Critical Care. 2018;22:118.
2. Rowan SC, Rochfort KD, Piouceau L, Cummins PM, O’Rourke M, McLoughlin P. Pulmonary endothelial permeability and tissue fluid balance depend on the viscosity of the perfusion solution. American Journal of Physiology-Lung Cellular and Molecular Physiology. 2018;315:L476-L84.
3.25. The Pilot of an Acute Respiratory Assessment Unit significantly improved outcomes for the respiratory patient.
T Byrne1, A Granitsas1, H Mc Loughlin1
1 HSE- Portiuncula Hospital
Burden of respiratory disease is challenging. Only 1/3 to 1/2 of individuals with airflow obstruction have a formal diagnosis1
Often respiratory diseases are managed in primary care, without access to diagnostics. Early diagnosis and pharmacological intervention are essential in achieving better clinical outcomes for patients.
The pilot of an RAU. The unit facilitated early review of patients with suspected respiratory disease and those who frequently exacerbated. The RANP facilitated a full clinical examination with access to diagnostics required. Where possible patients received an accurate diagnosis, education, health promotion and commenced on appropriate medication.
46.5% (n=20) were diagnosed with COPD and commenced inhaled therapy.
14 % (n=6) were diagnosed with asthma and commenced inhaled therapy.
39.5% (n=17) were referred with other respiratory concerns such as;
Lung Nodules,
OSA,
Cough
Haemoptysis
11% (n=5) required admission
88% (n=38) were discharged
The RAU had significant positives for both patient and institution. Studies suggest pharmacologic intervention in early respiratory disease have beneficial effects on ameliorating the decline in lung function 2. The RAU not only improves a patient’s QOL but also potentially reduces the need for an emergency hospital admission.
A permanent RAU would;
Improve patient outcomes/experience
Reduced waiting lists.
Reduce ED presentations/Hospital Admissions.
References
1. Labaki, W.W &Han, ML. (2018) Improving early detection of chronic obstructive pulmonary disease. Annals ATS .15(4) pp243-248
2. Sun, Y. & Zhou, J. (2019). New insights into early intervention of chronic obstructive pulmonary disease with mild airflow limitation. International Journal of Chronic Obstructive Pulmonary Disease :14 1119–1125
3.26. Two-week audit investigating timelines of patient flow from Tallaght University Hospital to Peamount Healthcare Respiratory Unit
E Cribbin1, B McNamara1, C Lynch1, K Anyakudo1, A Bradley1, C Slattery1, M Fitzgerald1, S Lane1,2, E Moloney1,2, M Kooblall1,2
1 Peamount Healthcare, Dublin
2 Tallaght University Hospital, Dublin
Peamount Healthcare Respiratory Unit offers inpatient rehabilitation for respiratory patients requiring ongoing intervention following their acute stay in Tallaght University Hospital. In 2019, the bed occupancy for the unit was 76%. The purpose of this two-week audit was to review timelines of patient flow from TUH to the unit to identify ways of improving efficiency of transfer and maximising bed capacity.
A two-week service audit was carried out identifying number of referrals to the unit, time from receipt of referral to registrar review, acceptance and admission to the unit, and number of communications between sites prior to patient being admitted.
Over the two-week period, 9 patients were referred to the unit, 8 were accepted. The time from receipt of referral to review was 0.88 days, from review to acceptance 1.75 days, and from acceptance to admission to the unit 0.5 days. Additional medical information was requested for 5 out of the 9 referrals, and an average of 6.4 additional communications between sites occurred to obtain all relevant information.
The results indicate improvements could be made in ensuring all relevant information is being sent on initial referral to minimise the number of communications and resulting delay in patients being accepted to the unit. Data collection and quality improvement projects are ongoing aiming to maximise bed capacity and improve respiratory care pathways between acute and subacute hospital sector.
3.27. “The Breath Factor”- a pilot study of singing for lung health as part of pulmonary rehabilitation
E. Liston1, K. Devenney2, C. Gleeson2, C. Gray2, E. O’Shea1
1Physiotherapy Department, St. James’s Hospital. 2Respiratory Assessment Unit, St. James’s Hospital.
“Singing for Lung Health” (SLH) 1 when used as an adjunct to managing symptoms in chronic respiratory conditions has the potential to improve health related quality of life and anxiety. This pilot study sought to examine the effects of SLH incorporated into a local standard pulmonary rehabilitation programme (PRP).
All participants attending an 8-week PRP between November and December 2019 were invited to partake in an optional once weekly 30-minute SLH session. It was conducted over 5 weeks immediately after their exercise training sessions. The SLH session was led by a physiotherapist with a musical background and comprised of warm- up/breath control exercises followed by well-known popular songs. A post intervention participant survey and focus group (n=11) were completed, facilitated by a physiotherapist not involved in the intervention.
Thematic analysis of the results demonstrated improvements in mood, well-being, symptom control & confidence. The participants also reported the experience was fun, enjoyable and social.
SLH has the potential to deliver health, psychological and social benefits to people with chronic respiratory conditions and preliminary data from this pilot study supports this. However robust research is required before it can be adopted as an intervention offered routinely to people with respiratory disease.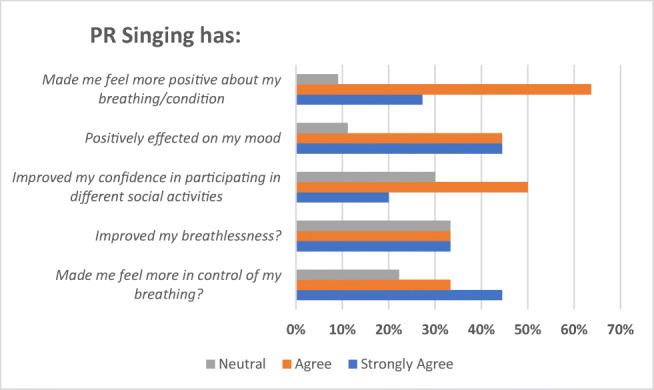
References
1. Lewis, A., Cave, P., Stern, M., Welch, L., Taylor, K., Russell, J., Doyle, A.M., Russell, A.M., McKee, H., Clift, S. and Bott, J., 2016. Singing for Lung Health—a systematic review of the literature and consensus statement. NPJ primary care respiratory medicine, 26(1), pp.1-8.
3.29. An audit of a nurse-led clinic for follow-up of inpatients newly commenced home oxygen
A. O’Keeffe1, M. O’Donnell1, A. Devi1, N. Dhondt1, E. Drudy1, W. Binalialsharabi1, K. Breathnach1, C. Gleeson1, C. Gray1, P Nadarajan1
1 St. James’s Hospital, James’s Street, Dublin 8.
Patients newly commenced on ambulatory oxygen therapy (AOT) and long-term oxygen therapy (LTOT) are often not followed up to assess appropriateness/necessity of initial prescription [1]. The aim of this audit was to assess the effectiveness and outcomes of a nurse-led clinic at ensuring follow-up of all patients who were newly commenced on LTOT and/or AO following a hospital admission.
The audit examined all inpatient home oxygen requests sent between November 2019 - March 2020. Data in relation to follow up attendance and modification of prescription was captured on Excel.
Fifteen patients newly commenced LTOT and/or AOT as an inpatient over the study period and were eligible for inclusion in the audit. Only six patients attended the first follow up at six weeks (DNA n= 5; CNA due to COVID n=4). Twelve patients attended a further follow up review at six months. Six persons attended twice and only two had no follow-up. Over the two visits, LTOT was stopped in 4 persons and modified in two, while AOT was also stopped in four persons and modified in two.
Nurse-led care allowed for high follow-up rates of patients prescribed home oxygen following a hospital admission and ensured appropriate changes were made.
References
1. Ringbaek T, Lange P, Viskum K. Are patients on long-term oxygen therapy followed up properly? Data from the Danish Oxygen Register. Journal of Internal Medicine. 2001;250(2):131-136.
3.30. Audit of the appropriate prescribing of Low Molecular Weight Heparin in a busy Regional Hospital
A Rafi1, HY Li, NKB Abidin1, MK Rana1, M Muzammil1, S Rizvi1
1 Medical Department, Mayo University Hospital, Castlebar
Low molecular weight heparin (LMWH) is a class of anticoagulants that is frequently prescribed in hospitals. Its various indications include Thromboprophylaxis, treatment of DVT/PE, A.Fib and ACS. This audit aimed to assess whether LMWH is prescribed appropriately in this hospital based on Age, Weight and Creatinine Clearance, and according to HSE LMWH prescribing guidelines.
All patients admitted in the surgical and medical wards of Mayo University hospital between 8th-10th June 2020 were included. Their drug charts were reviewed, documented weights collected and their Creatinine Clearance (CrCl) was calculated according to the Cockcroft-Gault equation.
Out of 128 patients, 67 (52%) patients were on LMWH. Among them, 94% were on Clexane and 6% were on Innohep. 49 (73.1%) patients were appropriately prescribed LMWH and 18 (26.9%) patients were not. Out of those 18 patients, 10 (55.6%) patients were under prescribed and 8 (44.4%) patients were overprescribed. (7 (38.9%) patients were not prescribed according to weight, 3 (16.7%) patients were not prescribed according to CrCl and the remaining 8 (44.4%) patients were prescribed incorrect dose)
These results demonstrate that the majority (73.1%) of patients were prescribed LMWH appropriately. But to achieve maximum compliance and minimise the risk of complications/side effects, on-going education should be provided to NCHDs. Inclusion of the VTE prophylaxis Protocol and specified page for anticoagulation prescription in the hospital’s drug chart would be a useful and safe practice.
3.31. Ensuring patients attending the Oxygen Therapy Clinic receive the right care at the right place, at the right time – a review of the Oxygen Therapy Clinic in Louth County Hospital, Dundalk
M. O’Reilly1 and R. Reilly2
1. Dept. of Respiratory Medicine, Our Lady of Lourdes Hospital, Drogheda
2. Department of Physiotherapy, Our Lady of Lourdes Hospital, Drogheda
The Oxygen Therapy Clinic (OTC) was established in Louth County Hospital (LCH) in April 2019. Prior to this, patients from North Co. Louth and Co. Monaghan travelled to the OTC in Our Lady of Lourdes Hospital (OLOLH), Drogheda. Being aware of the burden and cost of travel for these patients, we established the OTC in LCH to alleviate this.
An anonymous patient satisfaction survey was carried out in March 2020 on the 61 patients who had attended in the year prior. The response rate was 66%.
100% of patients reported increased convenience to have their appointment in LCH rather than OLOLH and would prefer future OTC appointments in LCH. 100% of patients reported that the directions and information in their appointment letter were clear, they had a comfortable, clean area to wait and the nurse/physiotherapist listened to them/their carer. 93% of patients reported their appointment was on time. 98% were satisfied with the treatment/advice. A total of 1932km and over 20 hours travel time was saved for patients by facilitating their appointment in LCH rather than OLOLH
Patients from North Co. Louth and Co. Monaghan report preference to attending OTC appointments in LCH saving travel cost and time.
3.32. Bronchiolitis
RM Rutherford1, D Doyle1, J Ryan1
Respiratory Department, Galway University Hospital
We examined the adult population of patients with bronchiolitis in GUH to determine common aetiologies and their responses to treatment. There is scant literature outlining the management of bronchiolitis so our data may shed some light on this uncommon disease.
Our patient electronic system was interrogated with the search term “bronchiolitis” and 75 patients were reviewed. In a number of cases, bronchiolitis was not specifically reported by a radiologist, but instead found to be a feature present on imaging by a pulmonologist.
Two thirds of our patients were female and the mean age at diagnosis was 63. Half of the patients had obstructive pattern on spirometry. Bronchiectasis, obstructive airway disease and reflux/aspiration were the commonest causes of adult bronchiolitis in our cohort. H influenzae was the most common pathogen, followed by P aeruginosa then S pneumoniae.
Two thirds of our cohort had repeat imaging and, of these, three quarters showed improvement. The chart below displays which treatment strategies were used and their outcomes. This study was conducted outside a lung transplant centre, so it should be mentioned that lung transplant is a recognised cause of bronchiolitis but not one that was included in our dataset.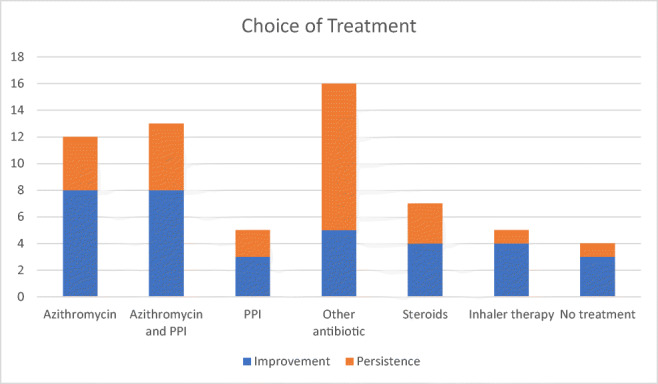
3.33. An Investigation into the Utility of Serum Bicarbonate as a predictor of Obstructive Sleep Apnoea in a Sleep Clinic Population.
Campbell, C D.[1] Doherty, M[1] Baker, L[1] Finan, K[1]
[1] Respiratory Department, Sligo University Hospital, Sligo.
3.34. Improving the efficiency and accuracy of OSA diagnostics
C Gill1, P Coss1, O Gavin1, A Martin1, R McLoughlin1, T Matthews1, AM McLaughlin1, B Kennedy1, BD Kent1
1 Department of Respiratory Medicine, St James’ Hospital, Dublin 8
Polysomnography (PSG) is the gold standard test for obstructive sleep apnoea (OSA), but is resource intensive. Nocturnal oximetry is often used as an initial diagnostic tool in suspected OSA because of its convenience and low cost, but it lacks sensitivity, with consequent long PSG waiting lists. We conducted a quality improvement project to expedite OSA diagnosis, using a novel sleep diagnostic device, the WatchPAT.
To gauge the impact of OSA undiagnosed by oximetry on PSG waiting lists, we initially assessed consecutive PSGs undertaken in our centre in the preceding year. Thereafter, patients awaiting PSG for suspected OSA underwent home sleep testing (HST) using WatchPAT devices, to quantify the proportion of patients that could be spared PSG by the use of more advanced HST.
PSG identified a significant burden of OSA not diagnosed by oximetry: 84% of PSG patients an AHI >5 events/hour, with 64% having at least moderately severe disease. 16 subsequent patients with non-diagnostic oximetry had HST: mean AHI was 20.3±16.5 events/hour, 14 (87.5%) were identified as having OSA, with 8 (50%) having an AHI>15.
These data highlight the impact of OSA on PSG waiting lists, along with the role of emerging technologies in expediting OSA diagnosis and treatment.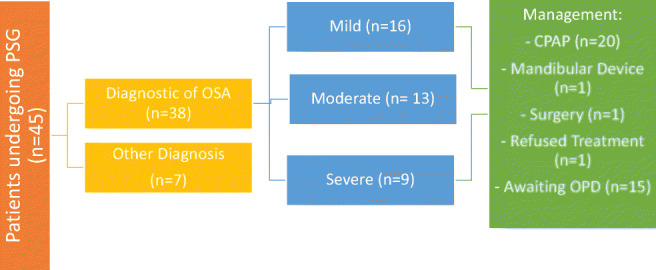
3.35. Primary human macrophages from healthy individuals show differential susceptibility and inflammatory response to Mycobacterium avium
TD Shaw1, AD Krasnodembskaya1, GN Schroeder1, CM O’Kane1
1Wellcome-Wolfson Institute for Experimental Medicine, Queen’s University Belfast
Non-tuberculous mycobacterial pulmonary disease (NTM-PD) is increasingly reported in patients with no identifiable risk factors. We sought to characterise the susceptibility of primary macrophages from healthy individuals to Mycobacterium avium (M. avium).
Primary monocyte-derived macrophages (MDMs) from 22 healthy volunteers were infected with M. avium (Chester reference laboratory strain) at multiplicity of infection of 0.1-1 for 4 hours, before washing. Supernatant was collected, and cells lysed in 0.2% saponin, to determine extracellular and cell-associated colony counts at baseline and 24-hour intervals. Supernatant cytokines were quantified by ELISA. Statistical analysis was performed using the Kruskal-Wallis test.
There was diversity between donors in the proportion of viable bacteria that was cell-associated at baseline (median 25.4% IQR 15.5-37.8%). Bacterial proliferation was observed in all donor MDMs, with inter-donor variability in growth (Fig. 1) and secretion of IL-6 (median 1306pg/ml, IQR 550-4576pg/ml) and IL-8 (median 9156pg/ml, IQR 5814-17713pg/ml). There was an inverse relationship between IL-6/IL-8 secretion and bacterial growth but this was not significant. Similar findings were observed in two clinical isolates of M. avium.
In conclusion, primary macrophages from healthy donors show differential susceptibility and inflammatory responses to M. avium. Further investigation is warranted to elicit host factors to predict susceptibility to NTM-PD.
3.36. Home-based Virtual Pulmonary Rehabilitation Programme (VPR) for patients with Chronic Obstructive Pulmonary Disease (COPD), Interstitial Pulmonary Fibrosis (IPF) and Asthma.
M. O’Reilly1, C. Gillen1 and J. Smith1.
1Department of Respiratory Medicine, Our Lady of Lourdes Hospital, Drogheda, Co. Louth
Physiotherapy Department, Our Lady of Lourdes Hospital, Drogheda, Co. Louth
VPR is an evidence-based live physiotherapy led exercise and education programme for patients with IPF, Asthma and COPD. It utilises technology to deliver twice weekly classes for seven weeks; eliminating both the cost and inconvenience of travel often reported as barriers in attending traditional programmes.1,2
Prior to the COVID-19 pandemic patients attended the hospital for their pre and post assessments, which included exercise tolerance, quality of life(QOL) and falls assessments, patients also received on-going technology training. Due to the COVID 19 restrictions modifications were made to allow assessments to be completed virtually therefore reducing unnecessary presentation of high-risk patients to the hospital.
Preliminary results from three programmes (20 participants) have demonstrated significant clinical improvements in both exercise capacity and QOL status comparable to traditional PR programmes. Since beginning VPR, patients saved 15,731km and 302 hours in travel. High levels of acceptability (93.7%) and self-efficacy improving confidence to exercise at home (98%) were reported.
VPR allowed high-risk patients safe access to a PR programme throughout the COVID-19 Pandemic. This alternative model is the first of its kind nationally and through collaboration with the National Clinical Programme for Respiratory formed the basis for the national guidelines on VPR during COVID-19.
References
1. Almadana V, Romero C, Valido A, Gómez-Bastero A, Sánchez J, Montemayor T. Profile of Patients Who Drop out of a Pulmonary Rehabilitation Program. Chest. 2014;145(3):370A.
2. Keating A, Lee A, Holland A. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chronic Respiratory Disease. 2011;8(2):89-99.
3.37. Waiting to Move
M. O’Reilly1
1Physiotherapy Department, Our Lady of Lourdes Hospital (OLOLH), Drogheda, Co. Louth
BTS Quality Standards for Pulmonary Rehabilitation (PR)1 states that patients accepted to enrol in PR should commence their programme within 3 months of receipt of referral. The aim of the study was to reduce PR waiting list in OLOLH from 13 months to 3 months.
Analysis of existing service identified a number of inefficiencies: 1) inappropriate referrals 2) patients not attending assessment, 3) patients dropping out. To improve the standard of referral the Respiratory team was educated on referral criteria and the PR program. A new referral form and patient information leaflet was introduced. To improve uptake and completion rate a compulsory information talk was introduced for patients.
Waiting list times reduced to 10 weeks. Completion rate increased from 56% to 77%. Improvements were noted in exercise tolerance (89%), dyspnoea (44%), Chronic Obstructive Pulmonary Disease (COPD) health status(95%) and confidence levels in self-management of their disease(96%).
The new referral form was effective in reducing inappropriate referrals while ensuring appropriate patient uptake and completion of PR. Patients continued to yield improvements in their exercise tolerance, symptoms and knowledge of their chronic lung disease. The PR waiting list in OLOLH is in line with BTS PR Quality Standards 2014.
References:
1. Bolton C, Blakey J, Morgan M. The British Thoracic Society guideline on pulmonary rehabilitation in adults: your opinion is noted. Thorax. 2014;69(4):388-389.
IRISH THORACIC SOCIETY ORAL PRESENTATIONS III
3.1.1. A novel high viscosity perfusion solution protects against oedema formation in ex vivo lung perfusion for lung transplant; a preclinical study.
E McCormack1,2, P Geoghegan3, G Curley3, K Redmond2, P McLoughlin1
1 Conway Institute, School of Medicine, University College Dublin, Dublin, Ireland
2 Department of Cardiothoracic Surgery, Mater Misericordiae University Hospital, Dublin, Ireland.
3 Department of Anaesthesiology, Royal College of Surgeons Ireland, Dublin, Ireland
3.1.2. A Retrospective Cohort Study, Analysing Factors Which May Influence Adherence to Prescribed Oxygen Therapy
C Ottewill1, O Buzdygan1, S Cunneen2, J Cullen3, M Kooblall1, A Subramaniam1 S Donnelly1, E Moloney1, S Lane1,
1. Department of Respiratory Medicine, Tallaght University Hospital
2. Department of Physiotherapy, Tallaght University Hospital
3. Acute Medical Unit, Tallaght Hospital
Adherence to oxygen therapy is complex and multifactorial, with previous studies highlighting issues including perceived benefit, physical difficulty using oxygen, self-consciousness and social stigma contributing to poor adherence.(1) Despite evidence showing a survival benefit to Long Term Oxygen Therapy (LTOT), in hypoxaemic Respiratory Failure in Chronic Obstructive Pulmonary Disease (COPD), studies estimate adherence to therapy at anywhere between 50% and 80%. (2)
This retrospective cohort study analysed patient-reported compliance to prescribed oxygen therapy. All return patients on prescribed oxygen therapy, attending Oxygen Clinic, over a one-year period were assessed. Factors including age, gender and level of socioeconomic deprivation were analysed to assess whether they affected adherence to prescribed therapy. Adherence to LTOT and Ambulatory Oxygen Therapy (AOT) were analysed separately.
104 return patients attended the Oxygen Clinic over a 12-month period. Amongst this cohort, 54 (52%) were male, with a median age of 72 years. 59 patients (56.7%) had a diagnosis of COPD. Notably three patients had a new oxygen requirement post-COVID-19 infection.
This project seeks to assess factors affecting adherence to prescribed oxygen therapy in an Irish cohort, focussing on age, gender, underlying lung disease. It shall analyse whether socioeconomic deprivation affects patient compliance.
References
1. Earnest MA. Explaining adherence to supplemental oxygen therapy. J Gen Intern Med. 2002 Oct 1;17(10):749–55.
2. Ringbaek T, Lange P, Viskum K. Compliance with LTOT and consumption of mobile oxygen. Respir Med. 1999;93(5):333-337. 10.1016/s0954-6111(99)90314-1
3.1.3. To Develop, Implement and Evaluate an Integrated Care Pathway for Patients Presenting with Pneumothorax
Ben Shanahan1, Jan Sorenson1, Tomas Breslin1, Donna Eaton1, Karen Redmond1
1 Mater Misericordiae University Hospital, Royal College of Surgeons in Ireland, Dublin, Ireland.
Pneumothorax is a common presentation to acute healthcare services in Ireland, accounting for 7,045 inpatient bed days in Ireland in 2017. There is robust evidence to demonstrate that ambulatory management of pneumothorax is feasible and safe.
This project developed, implemented and evaluated an Integrated Care Pathway (ICP) for patients with pneumothorax that maximised ambulatory management for suitable patients. The ICP was evaluated using a prospective multi-site observational study. At the centre of the study design was an extensive economic analysis of ambulatory management for pneumothorax. Such an economic analysis of the effect of ambulatory management for pneumothorax has not been presented elsewhere in the literature.
Thirty two patients were recruited over an eleven month period. Implementation of the Pneumothorax ICP resulted in a statistically significant reduction in inpatient length of stay of 2.84 days from 7.4 to 4.56 days (p=0.001), and thus a per-patient cost saving of 2314 euro.
This project has demonstrated that standardisation of care for pneumothorax patients, with a focus on ambulatory management, is economically beneficial for the healthcare service. It is thus anticipated that this work will be used to inform healthcare policy at a national level in Ireland.
3.1.4. Diagnostic sleep studies and CPAP set-up in the midst of a pandemic.
M. McCall1, K. Smyth1, A Livingstone1, S. Moan1, E. Hayes1,
Department of Respiratory Medicine, Daisy Hill Hospital, Newry, Southern Health & Social Care Trust
Sleep disordered breathing and obstructive sleep apnoea are conditions with a high burden of patient morbidity and can have long term consequences for a patient’s physical health leading to higher rates of coronary artery and cerebrovascular disease. (1)
However in late 2019 with the outbreak of the SARS-CoV2 pandemic and the realisation that spread was predominantly by aerosol a number of major modifications were made to how many procedures were performed. In particular any procedure expected to generate an Aerosol (AGP).
This had a profound effect on the diagnostic and therapeutic sleep services within the Southern Trust. In particular continuous positive airway pressure (CPAP). As a result of this there has been a significant change in waiting times for diagnostic sleep studies and for CPAP initiation. This is due to a number of factors; the redeployment of staff, the need for increased sterilisation between procedures and patients and also the advice given to many large groups of patients to “shield” and only leave their homes for emergencies or essential reasons. (2)
Improvements to current protocols and work practices have allowed us to re-establish the sleep service maximising efficiency whilst at the same time maintaining staff and patient safety.
References
1. ARTP (association for respiratory technology and physiology): standards of care in sleep apnoea.
2. ARTP (association for respiratory technology and physiology): Respiratory function testing and sleep services during endemic COVID-19. Aug 2020
3.1.5. Pilot study to assess the accuracy of Positive Airway Pressure (PAP) derived Apnoea-Hypopnoea Index (AHI) by using an Independent Novel PAP home monitoring device.
M Herron1, L Stewart1, K McEvoy1, A McGowan1, L Cormican1.
1 Department of Respiratory Medicine, Connolly Hospital Blanchardstown, Dublin 15, Ireland.
Conflict of interest: None declared.
To assess the accuracy of the AHI reported by multiple commercially available PAP devices using the Dynomed device. Both AHI values from PAP and Dynomed were compared to Physiologist scored AHI from a simultaneously recorded limited sleep study (LSS).
Eighteen PAP compliant patients with a previous diagnosis of Obstructive Sleep Apnoea (OSA) underwent a single night limited home sleep study whilst using PAP accompanied by Dynomed. Three patients were excluded for technical reasons. The sleep studies were manually scored to AASM standard. Time-matched AHIs were analysed with Wilcoxon paired signed ranks tests, Spearman correlation and Bland-Altman plots.
There was no significant difference between AHI values measured via LSS and Dynomed (p=0.29), however, there was a significant difference in AHI when LSS was compared with PAP values (p=0.02) (Figure 1), with an overall underestimation when comparing AHI ratios (p=0.005). Dynomed and LSS absolute AHIs correlated significantly (r=0.88, p=0.00005). In contrast, there was no statistically significant correlation between LSS and NIV (r=0.34, p=0.22).
Our results indicate that Dynomed reports AHI accurately via remote monitoring as it correlates significantly with limited sleep study. This study altered the clinical management in 7 of our patients.
IRISH THORACIC SOCIETY POSTER REVIEW AND DISCUSSION
4. COPD and ASTHMA
4.1. Asthma Biological Treatment: Review of patient outcomes with severe brittle asthma in Cork University Hospital.
Casey D1, Farrell A1, O’ Sullivan G1, Murphy J1, Plant BJ 1, 2, Murphy DM1,2
1 Department of Respiratory Medicine, Cork University Hospital, Wilton, Cork.
2 Health Research Board, Clinical Research Facility, University College Cork, Cork.
A retrospective review was performed of patients with severe asthma on biologic therapy (Omalizumab, Mepolizumab, Resilizumab or Benralizumab) in our centre 45 patients were identified and their outcomes prior to and one year post biologic therapy commencement were analysed.
73 patients had been initially commenced on monoclonal therapies in our institution. 45 have continued therapy for over 12 months.
We recorded the ACQ score, number of exacerbations, hospital and ITU admissions in the 12 months before and 1 year after commencement of therapy. Antibiotic and steroid use was examined in relation to both exacerbation treatment and prophylaxis.
An 80% reduction in exacerbations and a 75% reduction in hospital admissions, with a subsequent reduction of 403 bed days, which was significant (p= 0.04). There has been a 100% reduction in ICU admissions. ACQ was calculated at a mean score of 3.3 pre biologic therapy. A reduction in ACQ to 1.5 a year post biologics (P=0.005).
There was a 50% reduction in the use of maintenance steroids and an 80% discontinuation rate of prophylactic antibiotics (P=0.004)
Thus biologic therapy significantly improves patient outcomes and should be considered for suitable patients with severe asthma.
4.2. Asthma exacerbations requiring ICU: patients more likely to have prior history of smoking and prior ICU admission.
C. Hayes1, D. Long1, RW Costello1,2, DM Ryan1,2
1 Respiratory Department, Beaumont Hospital, Dublin 9
2 Royal College of Surgeons in Ireland
Asthma is a common condition affecting 1 in 12 people in Ireland.[1] Asthma exacerbation requiring ICU admission (AE-ICU) is associated with increased risk for asthma death.[2]
Our aim was to audit pre-ICU management of patients with AE-ICU at Beaumont Hospital (BH) and identify areas for improvement. Medical records for AE-ICU to BH during 2014-2019 were reviewed regarding presentation and clinical course, timing and choice of treatments and imaging results. Patient care was compared to recognised standard of care (SOC) National Clinical Effectiveness Committee (2015) asthma guidelines.[1]
There were 468 asthma admissions to BH with 15 (3.2%) AE-ICU. 11/15 (73%) were female. Mean age was 45.4 years (SD ±17.2). 9/15 (60%) had history of smoking and 10/15 (67%) prior AE-ICU. 5/15 (33%) required mechanical ventilation. There were no asthma deaths. Median time to first nebuliser was 24 minutes (range 6-94) and to first steroid 25 minutes (range 6-553). Undocumented/inaccurate assessment of exacerbation severity (12/15) and inappropriate corticosteroid dose (12/15) were common.
We conclude that AE-ICUs are infrequent at BH. Consistent with literature, we found prior smoking and AE-ICU history increase risk for future AE-ICU. Patients received early nebulisation but little PEFR monitoring. Excessive steroid dosing was common.
Table 2. Main Results
| Age | Mean 45.4 years (SD ± 17.2) |
| Sex | 73% Female, 27% Male |
| BMI | Mean 29.8 (SD ± 7.1) |
| Smoking History | Yes 60%, No 40% |
| No. of other co-morbidities | Mean 1.64 (Range 0-5) |
| Asthma-related admission in last 12 months? | Yes 67%, No 33% (Mean 3.3) |
| Prior ICU Admission | Yes 67%, No 33% |
| Time to ED Review | Median 17min (Range 2-149) |
| Time to 1st Nebuliser | Median 24min (Range 6-94) |
| Time to 1st Steroid | Median 25min (Range 6-553) |
| Corticosteroid Given? | Yes 100% (93% IV, 7% PO) |
| Steroid Dose Appropriate | Yes 20%, No 80% |
| Over-oxygenated (SpO2 >98%) | Yes 47%, No 53% |
| CXR Performed | Yes 100% |
| CXR Abnormal? | Yes 33% (80% hyperinflation) |
| Antibiotics Given? | Yes 100% |
| Antibiotics Indicated? | Yes 67%, No 33% |
| MgSO4 given | Yes 83%, No 17% |
| PEFR Performed | Yes 60%, No 40% |
| Time to 1st PEFR | 43.1min (Mean) |
| PEFR measurement interval | 253.6min (Mean) |
| Total documented PEFR | 2.5 (Mean) |
| Time to ICU Admission | Median 500min (Range 210-4247) |
References
1. Department of Health. Management of an Acute Asthma Attack in Adults (NCEC National Clinical Guideline No. 14). Dublin: Department of Health, 2015.
2. Royal College of Physicians. Why asthma still kills: the National Review of Asthma Deaths (NRAD) Confidential Enquiry report. London: RCP, 2014.
4.3. Characteristics of Chronic Rhinosinusitis in Severe Asthma Cohort.
1M. Talty, 2H. Mulryan, 3M. Thornton, 4 M. Harrison, 5A. O’Regan,
1245 Respiratory Department, Galway University Hospital (GUH)
3 ENT Department, Galway University Hospital.
Chronic rhinosinusitis (CRS) is an important cause of poor asthma control, yet there is little prospective data on risk factors and impact of CRS treatment. We established a prospective study utilising a combined asthma-ENT clinic to assess this patient group. We report the characteristics of the first 40 patients in this study.
Patients recruited from the Asthma clinic in GUH were assessed and managed in a standardised manner using a multidisciplinary team approach. 40 asthmatics (mean age 57 +/- & 21 male) were studied with evidence of CRS (Lund MacKay Score 11+7). By RAST testing (22/39) 56% were atopic (HDM 1; Grass 12; Tree 3; Dog 5; Cat 6) Aspergillus sensitization was seen in 7(17%). 30/39 (76%) had eosinophilia including 12/17 of the non-atopic cases. Other results included ANCA (2); ANA (4); Low immunoglobulins (3) and alpha 1 antitrypsin deficiency (2); aspirin exacerbated (2).
Compared to general asthmatic populations, atopy, while common, is less prevalent in this cohort of CRS in asthma. The strong association with eosinophilia and aspergillus sensitization is noteworthy. Further studies relating to risk factors and management are ongoing in this prospective cohort.
4.4. The Impact of Biofeedback on Self-efficacy in Adults with Asthma.
J. Walsh1, Z. Moore1, B. Murray1,
1 School of Nursing and Midwifery, Royal College Surgeons, Dublin.
To examine self-efficacy among adults with asthma, following a nurse led educational intervention using biofeedback of treatment use.
Participants (n=88) who had completed a larger RCT (INCA Sun) took part in this study. Participants were randomised into a control (best practice education) or intervention (best practice education, enhanced with personalised biofeedback) group in the RCT. Biofeedback on inhaler treatment use was generated using inhaler adherence technology, attempted and actual adherence was recorded. An adapted version of the Asthma Self-Efficacy Questionnaire was completed by all participants once.
Both study groups had highest mean attempted and actual adherence in month 1 and lowest in month 8. Control group felt most confident in communicating with their healthcare provider, intervention group felt most confident about the use of their inhalers. The highest mean level of overall self-efficacy was reported by the control group; despite this they showed a statistically significant (p=0.003) decline in mean actual adherence between month 1 and month 8.
A high level of perceived self-efficacy did not reflect actual behaviour when compared to objective measures of self-management such as inhaler adherence. Biofeedback when incorporated into asthma self-management strategies results in a more accurate assessment of self-efficacy, representative of actual behaviour. This information can be used to deliver personalised asthma and self-management education, ensuring effective asthma management.
4.5. Prevalence of Osteoporosis in Patients with Asthma Requiring Biological Treatment: A Single-Centre Study
L Thong1, D Casey1, J Murphy1, BJ Plant1, DM Murphy1
1 The Department of Respiratory Medicine, Cork University Hospital
Prolonged use of steroids is an associated risk factor for osteoporosis. Many patients with severe asthma require multiple courses or even continuous maintenance steroids to manage their asthma.
We screened 49 patients were on or awaiting monoclonal treatment for their asthma for osteoporosis 43 were included in the analysis (6 did not have full results). Data collected include patient demographics, body mass index (BMI), Z-score, T-scare, FRAX score and other risk factors for osteoporosis.
7.0% of patients were osteoporotic (n=3) and 44.2% osteopenic (n=19). 46.5% of all patients had previous fracture, the highest being in the normal group, 55.0% (n=11) followed by the osteopenic group, 45.0% (n=9). None of the osteoporotic patients had previous fractures. Patients in the obese group had the highest percentage of normal BMD at 61.1% (n=11), followed by the overweight group, 41.2% (n= 7).
Consistent with previous studies, the proportion of osteopenic and osteoporotic patients were lower in the overweight groups. Interestingly, patients with normal BMD appear more likely to have had previous fractures. Further studies are required to confirm or refute these findings as this has an important implication of whether asthmatic patients who meet the criteria for biological treatment will require prophylactic treatment for osteoporosis regardless of their BMD.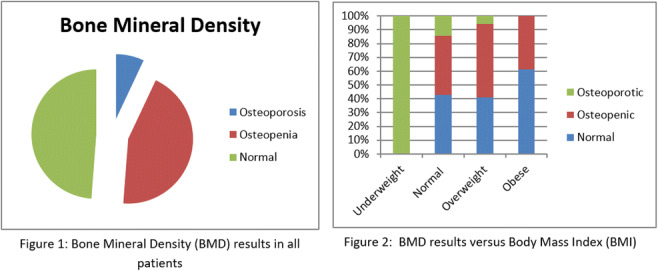
4.6. Efficacy of supervised maintenance exercise in peer support groups to maintain gains following pulmonary rehabilitation: A quasi-experimental study
B. Murphy1, A. Holmes1,2, B. Fitzgibbon2.
(1). School of Allied Health, University of Limerick
(2). St. Luke’s Hospital, Kilkenny
Although the short-term benefits of pulmonary rehabilitation (PR) are well established in chronic obstructive pulmonary disease (COPD), long-term benefits remain unclear.
This study aimed to examine i) if those who participated in community-based exercise in a peer support group (SG) were more likely to maintain exercise capacity and health status at 12 month follow-up and ii) perceived barriers and facilitators to participation.
Participants presented with COPD and previously completed an 8-week PR programme. Participants were encouraged to participate in SG following PR. Pre-PR, post-PR and 12-months outcomes included the ISWT, CAT and secondary measures of anxiety, depression, lower limb functional capacity and gait speed. Benefits and barriers to participation in SG were assessed using a questionnaire.
Participants (n=19) endorsed the benefits of the SG. Barriers included accessibility, transport and timing of sessions. Mean changes at 12 months showed significant, clinically relevant between-group differences in favour of SG for exercise capacity, gait speed and anxiety (all p < 0.05).
SG are endorsed by participants with COPD, and can offer a potentially innovative and efficient model for maintaining exercise capacity and health-related quality of life gains following PR. A larger, multicentre, randomized controlled trial is warranted to further explore the promising results of this study.
4.7. Association between oxygen therapy and adverse events in hypercapnic COPD patients
S Joomye1, A Betts1, J Joomye1, D O’Sullivan1, A Subramaniam1, M Khooblall1
1 Tallaght University Hospital.
Chronic obstructive pulmonary disease (COPD) is a leading cause of mortality worldwide. Oxygen therapy is an essential component in the acute management of COPD exacerbations but there is a risk of triggering hypercapnic respiratory failure. Oxygen should be prescribed to achieve target saturations (Sp02) of 88-92% to prevent adverse outcomes1.
To investigate in-hospital adverse events related to excess supplemental oxygen in COPD patients with chronic hypercapnia (PaC02 > 6.0kPa).
A study of 50 hypercapnic COPD patients admitted to hospital between September 2019 and January 2020. Data including demographics, blood gases, Sp02, and in-hospital adverse events were collected retrospectively from medical records. Patients on LTOT were excluded. Adverse outcomes included decompensated type 2 respiratory failure (T2RF) requiring BIPAP and intensive care unit admission.
21(42%) were male and 29(58%) were female. Mean age was 68.7 years. 40(80%) patients had their target Sp02 range charted. Out of these, 23(57%) received over-oxygenation and 7 (30%) required BIPAP and 4(17%) were escalated to ICU. Out of the 10(20%) who did not have parameters charted, 6 (60%) received over-oxygenation without any adverse events.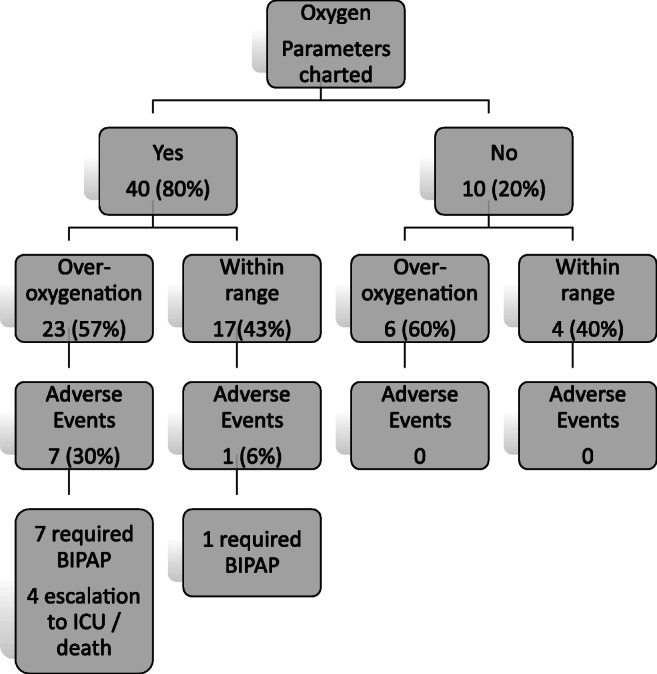
Adherence to guidelines on Oxygen therapy in COPD patients remain suboptimal. Education programme directed at healthcare staffs is required to meet standardised practice.
Reference
O’Driscoll BR, Howard LS, Earis J, et al. British Thoracic Society Guideline for oxygen use in adults in healthcare and emergency settings . BMJ Open Resp Res 2017;4: e000170. 10.1136/bmjresp-2016-000170
4.8. Real life uptake of Virtual Pulmonary Rehabilitation (VPR) in chronic lung disease
Authors: O’Mahony AM1,2, Tonge P1, Kelly C1,2, O’Beirne SL1,2
1 Department of Respiratory Medicine, St Michaels Hospital, Dun Laoghaire, Dublin
2 Department of Respiratory Medicine, St Vincent’s University Hospital, Elm Park, Dublin 4
4.9. Evaluating Palliative Care Referral and Mortality Rates in St Michael’s COPD Outreach Service
Kuda, D.1, O’ Sullivan, K.1, Gregan, P.2 O’Beirne, S.L.1,3.
1 Department of Respiratory Medicine, St. Michael’s Hospital, Dun Laoghaire, Co. Dublin.
2 Palliative Care Service, Blackrock Hospice, Blackrock, Co Dublin
3 Department of Respiratory Medicine, St. Vincent’s University Hospital, Elm Park, Dublin
Despite the important role of palliative care (PC) in the management of patients with chronic obstructive pulmonary disease (COPD), it is frequently under-utilised and is not offered to the majority of patients with advanced disease1,2.
To examine the utilisation of PC services in the cohort of patients supported by the COPD Outreach Service in St Michael’s Hospital, a retrospective analysis of the service from July 2019 to July 2020 was performed. The majority of patients had attended the emergency department and/or been hospitalised with a COPD exacerbation in the preceding year, markers of poor prognosis.
A total of 168 patients engaged with the service during this period, with ten deaths occurring (5.9% mortality rate) half of which were attributed to COPD. Chart review of deceased patients’ medical records revealed 50% had severe disease based on spirometric criteria and overall 70% of them had been referred to PC services.
This finding is encouraging, given the low overall PC referral rates reported1,2. This and the low mortality rate in the cohort may be related at least in part to the involvement of a COPD outreach team providing support and continuity of care for individuals with advanced COPD in the community.
References
1. Bloom CI, et al. Low uptake of palliative care for COPD patients within primary care in the UK. Eur Respir J. 2018;51:1701879
2. Gershon AS, et al. End of life strategies among patients with advanced chronic obstructive pulmonary disease (COPD). AJRCCM Artic Press. 2018: 03–592. 10.1164/rccm.201803-0592OC.7.
Conflict of Interest: The authors have no conflict of interest to declare.
4.10. Tele Pulmonary Rehabilitation in the COVID-19 pandemic, the new normal for COPD patients.
Leitermann, M1. Murray, B2.
1 Mayo University Hospital, Castlebar, Co Mayo
2 Royal College of Surgeons in Ireland, Dublin
Global best practice guidelines recommend access to a pulmonary rehabilitation programme, as it provides long-term benefits for COPD patient’s, their quality of life and the overall functional abilities. In addition, there is a proven reduction in hospital admission rates (GOLD 2020, HSE 2019, Kjaergaard et al 2020, McDonnell et al 2019). The current COVID-19 pandemic has focused greater attention on the need to have virtual telerehabilitation/telehealth as part of standard practice and provide “business as usual” (Hollander et al 2020, HPSC 2020).
A literature review was undertaken following a comprehensive, and structured search strategy which yielded five studies suitable for review (n = 602) (Bhatt et al 2019, Broadbent et al 2018, Dinesen et al 2012, Rosenbeck Minet et al 2015, Vasilopulou et al 2017).
The data analysis indicates that tele-pulmonary rehabilitation appears to provide a reduction in hospital admission rates of COPD patients. In addition, the studies indicate a positive impact on reducing hospital costs and increasing functional/physical assessment scores and medication/inhaler adherence.
The current COVID-19 pandemic has focused greater attention on the need to have virtual tele-pulmonary rehabilitation as part of standard practice in the provision of “business as usual”. More studies are necessary to further substantiate these findings prior to the development of standardised, evidence based virtual tele-pulmonary rehabilitation systems.
4.11. An Audit of Asthma Deaths at Beaumont Hospital Dublin
O’Connor A1, Hayes C1, Long D1, Costello RW1,2, Ryan DM1,2.
(1) Respiratory Service, Beaumont Hospital, Dublin
(2) Royal College of Surgeons in Ireland, Dublin.
Asthma is common, affecting 1 in 13 people in Ireland (1). 60-70% is uncontrolled, with an associated increased risk for death (2). In Beaumont Hospital (BH), we recently audited asthma standards of care (SOC) for ward and ICU admissions. We now proceed to an audit of asthma deaths.
Asthma deaths occurring between January 2010 and February 2020 were identified using the Hospital In-Patient Enquiry (HIPE) system. An audit pro-forma was designed evaluating asthma SOC, against National Clinical Effectiveness Committee Guidelines (2015).
HIPE confirmed approximately 80 asthma admissions per year (3% ICU) to BH and four in-patient asthma deaths during 2010-2020 (0.5%). Median age 63 (34-86) years, 3/4 (75%) female, 3/4 (75%) non-smokers, 1/4 (25%) prior ICU admission, 3/4 (75%) multiple co-morbidities, 1/4 (25%) intubated and died in ICU. Median time to death 3 (2-13) days. Disappointingly, there was no peak flow (PEFR) monitoring performed (100%) and steroid dosing was inappropriate (75% exceeded, 25% below guidelines) (see Table).
Asthma death following admission to Beaumont Hospital is rare. Asthma deterioration was early, similar to our ICU cohort. There were no differences in standard of care between patients who survived or died following asthma exacerbation.
| Table of Results | ||||
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | |
| Age | 86 | 34 | 72 | 53 |
| Gender | F | F | F | M |
| Smoker | N | Y | N | N |
| Time of presentation | 04:44 | 19:53 | 12.06 | 00:58 |
| Triage priority | Orange | Red | Yellow | Red |
| Time to triage | 00:24 | 0 | 00:04 | 00:22 |
| Time to ED review | 01:16 | 0 | 01:20 | 00:10 |
| Initial PEFR recorded | N | N | N | N |
| Severity of exacerbation | Life-threatening | Near-Fatal | Mild | Severe |
| Severity documented | N | Y (life-threatening) | N | N |
| Nebulisation | Y | Y | Y | Y |
| Time to first steroid | 03:16 | 00:47 | 01:54 | 00:47 |
| Steroid dosing compared to guidelines | Exceeded | Exceeded | Below | Exceeded |
| Antibiotics if appropriate | Y | Y | Y | Y |
| Magnesium sulphate | N | Y |
Y (8 days post-admission) |
N |
| Under respiratory team | N | Y | Y | Y |
| On respiratory ward/ICU | N | Y | Y | Y |
| PEFR chart during admission | N | N | N | N |
| On sole SABA PRN therapy | Y | Y | N | N |
| On ICS or ICS/LABA | N | N | Y | Y |
| Maintenance steroid | N | N | Y | Y |
| Biologic therapy | N | N | N | In past |
| Time of death | 05:35 | 16:05 | 09:45 | 07:52 |
| Location of death | Ward | ICU | Ward | Ward |
| Season | Spring | Summer | Spring | Spring |
| Day of week | Saturday | Thursday | Friday | Thursday |
References
1. The Asthma Society of Ireland; Dublin, Ireland. Asthma Facts and Figures. Available online: https://www.asthma.ie/get-help/resources/facts-figures-asthma. Accessed on 30/08/20.
2. Royal College of Physicians. Why Asthma Still Kills: the National Review of Asthma Deaths (NRAD) Confidential Enquiry Report. London, RCP, 2014.
4.12. Aspirin Desensitization for NSAID - Exacerbated Respiratory Disease – A Single Centre Experience
C Ottewill1, J Maxwell1, S Varghese1, S O’Brien1, S Lane1
1 Tallaght University Hospital, Dublin.
Aspirin sensitivity is one of the hallmarks of Samter’s triad, and is present in up to 14% of patients with severe asthma.(1) NSAID-exacerbated respiratory disease (N-ERD) is a chronic, eosinophilic inflammatory condition, occurring in those with asthma, chronic rhino-sinusitis, nasal polyps and symptom exacerbation associated with NSAID use. Aspirin challenge has been established with the aims of both confirming aspirin hypersensitivity in asthma, while aspirin desensitization has been shown to have a role with regard to treatment. (2)
A one-day aspirin challenge and desensitization programme was established in TUH in 2018. Since establishment, this programme has treated 15 patients with an aspirin change and, if successful, subsequent aspirin desensitization. This retrospective cohort study assesses for improvement in symptoms, exacerbation rate, and need for rescue medications following desensitization.
Aspirin desensitization in N-ERD has shown promise as a safe method to reduce symptom burden and glucocorticoid prescription. Initial data from our service, presented at this conference last year showed that 80% of those assessed had a positive aspirin challenge, with 37.5% having clear symptom benefit thereafter.(3) This project seeks to build on previous data, aiming to show that aspirin desensitization reduces symptoms and exacerbation rate in our patient cohort.
References
1. Laidlaw TM, Boyce JA. Aspirin-Exacerbated Respiratory Disease — New Prime Suspects. Longo DL, editor. N Engl J Med. 2016 Feb 4;374(5):484–8.
2. Kowalski ML, Agache I, Bavbek S, Bakirtas A, Blanca M, Bochenek G, et al. Diagnosis and management of NSAID-Exacerbated Respiratory Disease (N-ERD)—a EAACI position paper. Allergy. 2019;74(1):28–39.
3. O’Brien S, Breathnach C, Burke S, Lane S. NSAID exacerbated respiratory disease; one day protocol for challenging and desensitising patients using 45 minute intervals. In: IRISH JOURNAL OF MEDICAL SCIENCE. SPRINGER LONDON LTD 236 GRAYS INN RD, 6TH FLOOR, LONDON WC1X 8HL, ENGLAND; 2019. p. 264–265.
4.13. Implementation of a Novel Innovative Digital Health Study in Border Regions between the Republic of Ireland and Northern Ireland.
J. Walsh1, E. MacHale1, L. Lombard1, C. Mulvey1, T McCartan1, V. Brennan1, G. Green1, RW. Costello1
1 Royal College of Surgeons, Clinical Research Centre, Dublin.
In Ireland and the UK, most clinical research is conducted in large specialist services in academic teaching hospitals. Staff and patients in these centres have the opportunity to be involved in trials. This is not the case for those living in border regions between the Republic of Ireland and Northern Ireland. The CHITIN project is a collaborative project between the RCSI and the Cross-border Healthcare Intervention Trials in Ireland Network (CHITIN).
A clinical trial of a novel innovative digital health study (INCA Sun Study) was deployed to four border region hospitals; Altnagelvin Area Hospital, Craigavon Hospital, Cavan General Hospital and Our Lady of Lourdes Hospital, Drogheda. A post test analysis survey was conducted with staff from each site (n=19).
All staff reported having appropriate training/education for this role, 84% stated their guidance and training was adequate for the supporting structure. Barriers to implementing this study were; ethical approval process and significant delays from GDPR (26%), difficulty executing contracts (42%) and patient recruitment due to time constraints (52%).
In conclusion, while the results of this survey state that staff members in border regions were well trained, future studies in border regions can benefit from; practical knowledge of the different jurisdictions involved, early and well-tailored ethical committee applications and suitable time frame to facilitate patient recruitment.
4.14. The contribution of inhaled corticosteroid exposure to adrenal insufficiency in a severe asthma cohort monitored with an INCA device
V. Brennan1, J. Martin-Grace2, C. Mulvey1, G. Greene1, G. Collier3, T. McCartan1, L. Lombard1, J. Walsh1, S. Plunkett1, E. Mac Hale1, M. Sherlock2, RW. Costello1
1. Royal College of Surgeons, Ireland – Department of Respiratory Medicine
2. Royal College of Surgeons, Ireland – Department of Endocrinology
3. Beaumont Hospital, Department of Clinical Biochemistry
Inhaled corticosteroids (ICS) are reported to cause adrenal insufficiency (AI) 1. The prevalence is unknown and published studies are confounded by oral corticosteroids (OCS) and selection bias. This study aims to establish the relative contribution of OCS and ICS to adrenal suppression in a severe asthma cohort.
Morning cortisol samples were collected on completion of the INCA-SUN RCT and analysed using the Roche-Elecsys Cortisol-II assay. Results were classed suppressed (<100nmol/l), indeterminate (101-314nmol/l) or normal (>315nmol/l), based on published data predicting short Synacthen test outcomes using morning cortisol.
20% (13/65) of participants had a morning cortisol <100 nmol/l, suggesting AI. 13.8% of participants received maintenance OCS and 63% received at least one course of OCS during the study. The predicted prevalence of AI in patients without OCS exposure in the preceding week was 11%. Serum cortisol was strongly predicted by cumulative glucocorticoid exposure. Linear regression of serum cortisol versus mean daily ICS exposure showed a reduction in serum cortisol of -120nmol/L [-224, -22] per milligram increase in fluticasone propionate exposure (p=0.02). When adjusted for cumulative OCS exposure, this relationship remained significant with an effect size of -90nmol/L [ -13, -175]. 20% of patients with severe asthma may have undiagnosed AI. Our analysis shows a strong association between cumulative ICS exposure and the risk of AI, independent of OCS use.
References
1. Broersen LH, Pereira AM, Jorgensen JO, et al. Adrenal Insufficiency in Corticosteroids Use: Systematic Review and Meta-Analysis. J Clin Endocrinol Metab 2015; 100: 2171-2180. 2015/04/07. 10.1210/jc.2015-1218.
2. Dineen R, Mohamed A, Gunness A, et al. Outcomes of the short Synacthen test: what is the role of the 60 min sample in clinical practice? Postgrad Med J 2019 2019/09/27. 10.1136/postgradmedj-2019-136669.
4.15. Asthma inhalers and devices Poster 2020: “which one is it?”
Carrig C.1, Mc Donald M. 1, Devitt M. 1, Kilcullen N. 1, El Nazir B1.
1 Paediatric Respiratory Department, CHI @ Tallaght, Dublin 24.
The wide range of asthma medication can be confusing to both the patient and the physician. The asthma inhaler poster helps patients, physicians and healthcare professional identify the correct asthma inhalers. This poster assists you to identify the name of the inhaler, the strength of the inhaler as well as spacer devices. It can be an excellent tool for patients attending an outpatient appointment and scheduled or unscheduled healthcare visit. The poster can assist the health care professional identify the correct medication dosages and aiding decision making on stepping up and down of the inhaled medication to ensure optimum asthma control.
This is the 4th edition of the poster and is a collaboration between colleagues in Tallaght University Hospital working across Adult and Children Respiratory, Pharmacy and Medical photography.
4.16. Development of a combined hospital and home service for patients on Mepolizumab treatment.
Michele Cuddihy1, Olivia Flattery1 Prof. Liam Cormican1James Carr1
1 Connolly Hospital, Blanchardstown. Dublin 15.
Anti IL5 therapy is now an established therapy for the treatment of uncontrolled severe asthma. Currently 14 GINA 51 patients at are receiving Mepolizumab therapy in Connolly Hospital, Blanchardstown.
Mepolizumab, a humanized monoclonal antibody against interleukin-5, selectively inhibits eosinophilic inflammation and reduces the number of eosinophils in both sputum and blood, resulting in a reduction in exacerbations and in the need for treatment with systemic glucocorticoids.
Prior to COVID 19 restrictions patients attended the clinical nurse specialist led clinic monthly for Mepolizumab injections. In March 2020 COVID 19 restrictions came in to play and affected our ability to provide the anti IL5 treatment service in hospital.
A service was developed to enable the medication to be given at the patient’s home using the auto injector pen2 avoiding hospital visits. A policy and an SOP have been developed with agreement from pharmacy, nursing practice development and the Respiratory Consultant, to continue this service for patients. The patients now attend the hospital three monthly for assessment and collection of their next two doses of Mepolizumab. The patients were all given education on how to use the auto injector pen, consent was gained from each patient and any concerns or anxieties around injections were addressed. A questionnaire was sent to each patient to gain information on the patient experience of this new service in Connolly hospital. The results will be used to help improve the quality of the service.
References
1. Global Initiative for Asthma Guidelines (GINA), Global strategy for Asthma Management 2019. Available from: https://ginasthma.org (Accessed 8th August 2019).
2. https://www.ncpe.ie/drugs/Mepolizumab-nucala/
4.17. ASTHMA AUDIT
Dominic Doyle1, Robert Rutherford1, John O’Donnell1, Martin Doris1, Owais Rahman1, Maeve Brassil1
1 Respiratory and Emergency Departments, Galway University Hospital
With effective inhalers, we are observing fewer acute asthma presentations to GUH. Accordingly, the expertise in managing these presentations has probably deteriorated. Therefore, we audited this critical phase of emergency management in our ED.
A retrospective list of asthma presentations between January 2019 and May 2020 was generated. Paediatric and obvious non-asthma patients were excluded. A sample size of 20 patients was selected. The records of their investigation and treatment were examined and compared with standard care outlined by the BTS guidelines 2019.
Among our results we found that only 11 of 20 patients received nebulised salbutamol 5mg as first line therapy. The mean time from review to administration of nebuliser was 21 minutes. Only 6 of 20 patients had their severity scored. 11 of 20 patients had their PEFR scored. 2 patients with SpO2 ≤92% did not have an ABG.
Our audit identified areas for improvement, in particular with respect to the recommended first choice of nebuliser. Severity should be calculated because it is a useful guide to management. We aim to plan simulated training for ED and medical staff as well as create a management algorithm before re-auditing.
4.18 Experience of retaining patients in a randomised control trial translated into clinical practice
L. Lombard1, E. MacHale1, V. Brennan1, J. Walsh1, S. Plunkett1, C. Mulvey1, G. Greene1, T. McCarten1, M. Mokoka1, RW. Costello1.
1Clinical Research Centre, RCSI, Dublin
There is a higher non-attendance rate seen in patients with uncontrolled asthma compared to other respiratory conditions (32.6% versus 23.7%) 1. Continuity of care in this cohort is essential. Similarly in medical research, high attrition may threaten the validity of study findings. Retention strategies should be addressed during the study design phase as attrition rates for asthma RCTs can be up to 40%2. These strategies can translate into clinical practice.
We report the attrition rates from an eight month, prospective RCT (INCASUN). Patients were randomized into two groups; group one personalized biofeedback, group two standard care. Patients attended the research facility monthly. Various retention strategies were implemented in this study such as; building rapport with the study team, no waiting times, telephone reminders and paid parking.
Four sites had an attrition rate of 0%. 20 patients withdrew from the six remaining, with an overall attrition rate of 9%. Between site difference was observed, suggesting strategies implemented reduce attrition rates. The lowest attrition rate was seen in the biofeedback group (25%) demonstrating that patient engagement in their own care is an important factor.
Lessons learnt can be translated into clinical practice. The NHS estimates an economic cost of £600m/year due to non-attendance at clinics. Implementing these strategies would be cost effective and improve patient outcomes.
References
1 McDonough B, Mault S. Non-attendance at a difficult-asthma clinic. Nursing Times. 2013; 109 (16): 12-14.
2 Frampton GK, Shepherd J, Pickett K, Griffiths G, Wyatt JC. Digital tools for the recruitment and retention of participants in randomised controlled trials: a systematic map. Trials. 2020; 21 (478).
4.19. Establishment of a Combined Respiratory-ENT Clinic at GUH
1H. Mulryan, 2M. Thornton, 3D. Langan, 4A O'Regan
134 Respiratory Department Galway University Hospital.
2 ENT Department, Galway University Hospital.
Chronic rhinosinusitis is increasingly common with a high proportion of referrals to respiratory clinics. Access to ENT input is hampered by long waiting lists. We established a combined clinic in GUH to provide improved and multidisciplinary patient care.
This was a prospective nurse led study with REC approval. 65 new patients were seen in the 18 months (age 57+12; 30 male). 66% were asthmatic with 2 sarcoidosis. There was only 1 smoker and a variety of occupations (4 med-tech, 4 farmers, 4 HCW). 50% had been on systemic steroids in the last year. 85% were on nasal steroids. 27% had has prior sinus surgery. SNOT -22 was elevated at 52+24 with Lund MacKay sinus score 12+7. Assessments were carried out in a single visit and patient satisfaction was high
A nurse led combined respiratory-ENT clinic is feasible and efficient with good patient satisfaction. Prospective data will be collected on outcomes and SNOT-22 scores over time.
4.20. Body mass index affects asthma control test questionnaire scores
C. Mulvey1, G. Greene1, T. McCartan1, V. Brennan1, E. MacHale1, L. Lombard1, J. Walsh1, M. Quinn1, R. Costello1
(1) Department of Medicine, Royal College of Surgeons in Ireland
Asthma control is often assessed with the use of questionnaires. With levels of obesity rising globally, it is likely that associated comorbid conditions and deconditioning in baseline fitness may occur within asthma populations. This may lead to confusion between the effects of raised body mass index (BMI) and asthma symptoms. We hypothesised that asthma control test (ACT) scores are significantly impacted by BMI.
Analysis of a systematic review of clinical trials assessing additional therapies to ICS/LABA combinations yielded a significant result indicating BMI is reducing over time (coefficient -0.195, p 0.008, C.I. -0.335 - -0.054). This significance is lost when country of recruitment is accounted for.
Analysis of a combined dataset of two adherence randomised control trials (NCT01529697 and NCT02307669) to assess the relationship between ACT scores and BMI yielded a significant relationship indicating raised BMI results in lower ACT scores (coefficient -0.134, p 0.001, C.I. -0.214 – -0.054).
BMI has a significant effect on ACT scores which may lead clinicians to misinterpret asthma control. Clinical trials are increasingly conducted in countries with lower BMIs, therefore trial results may not apply to patient groups in clinical practice elsewhere, whose asthma may be complicated by raised BMI.
4.21. An in vitro investigation of aerosolised Budesonide delivery in simulated adult and paediatric spontaneous breathing models using a vibrating mesh nebuliser
P. J. Naughton1, B. Murphy1, A. O’Sullivan1, M. Mac Giolla Eain1, M. Joyce1, R. MacLoughlin1.
1 Aerogen Ltd, IDA Business Park, Dangan, Galway, Ireland.
Aerosolised corticosteroids are commonly used in the treatment and prevention of airway inflammation associated with asthma and other respiratory illnesses.1 The aim of this study was to assess aerosol delivery performance of Budesonide during simulated adult and paediatric spontaneous breathing.
A standard 2 mL dose of Budesonide (Pulmicort 0.5 mg/2 mL, Astra Zeneca, UK) was aerosolised using the Aerogen Solo (Aerogen, Ireland) in combination with the Aerogen Ultra aerosol chamber and facemask, with 2 litres per minute supplemental gas flow. A breathing simulator (Copley Scientific, UK) in combination with appropriate head models was used to generate both adult (Vt 500mL, 15 BPM, I:E 1:1) and paediatric (Vt 155 mL, 25 BPM, I:E I:2) breaths as per International Standard ISO27427.2 The mass of drug delivered to the level of the trachea was determined using UV spectrophotometry (241 nm). Five replicates were performed for each test.
Following test, the recorded tracheal doses were adult (23.36 ± 1.35 %), and paediatric (15.14 ± 1.15 %). This study confirms that high levels of Budesonide can be delivered using a vibrating mesh nebuliser. This information should inform clinicians in their approach to clinical aerosol therapy.
Conflicts of Interest: All authors are employees of Aerogen.
References
1. Hvizdos K, Jarvis B. Budesonide inhalation suspension: a review of its use in infants, children and adults with inflammatory respiratory disorders. Drugs [Internet]. 2012 Sep 17 [cited 2020 Aug 31];60(5):1141-1178. Available from: 10.2165/00003495-200060050-00010
2. ISO - ISO 27427:2019 - Anaesthetic and respiratory equipment — Nebulizing systems and components
4.22. A Review of the Use of Omalizumab in a Tertiary Referral Centre
C. Gill1, S. Roche1, L. Dolan1, P. Nadarajan1
1 Department of Respiratory Medicine, St James’ Hospital, Dublin 8
Asthma is a chronic inflammatory condition resulting in episodes of reversible airway obstruction. Severe asthma accounts for 10% of all disease (1), and poses a significant therapeutic challenge. In recent years, a number of biological therapies have been approved for treatment of steroid refractory asthma.
We reviewed the use of Omalizumab in patients commenced on the drug over a ten year period using electronic patient records. We compared pre and post treatment spirometry, frequency of exacerbations per year and mean daily steroid intake.
We identified 14 patients (50% male; mean age 59.07 years) commenced on Omalizumab during this period. Mean daily steroid use decreased from 10mg Prednisolone per day to 5mg per day while on Omalizumab. Most patients (86%) had reduced rates of exacerbations while on the drug. 75% of patients also had improved spirometry results on treatment, with an average improvement of 10% in forced expiratory volume.
This review highlights the beneficial effects of Omalizumab in a small patient population in a tertiary referral centre. A further review of patients who failed to improve on Omalizumab could be worthwhile to elucidate any common patient characteristics that might indicate poor response to therapy.
References
1. Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J 2014; 43: 343–373.
4.23. Experience of Benralizumab (Fesenra) at St. Luke Hospital, Kilkenny [ SLK] – Carlow.
Zaheer M.S. 1, Shahzad Q1, Helly F1, Walsh J1, Canavan B1.
1 Department of Respiratory Medicine St. Luke’s General Hospital, Kilkenny
Benralizumab (Fasenra) is a HSE approved monoclonal antibody, directed against the alpha-chain of IL-5 receptor, for the treatment of severe eosinophilic asthma and has been shown to improve asthma control in this cohort1. In January 2020, 6 patients in St Luke’s General Hospital, Co. Kilkenny, commenced Benralizumab treatment. Here we present the results of patients having completed 5 (n=2) and 7 (n=4) months of treatment.
The study population comprised 66.66% females (n=4) with a mean age of 64.67 years and a mean eosinophil count of 0.55 x10^9/L. All were steroid dependant with average prednisolone intake of 189.16mg/week. Benralizumab 30mg was administered subcutaneously 4 weekly for 3 months, and 8 weekly thereafter.
With Benralizumab, prednisolone use reduced to 17.5mg/week, with an overall 90.74% reduction in the steroid use [p =0.0002]. 66.66% of participants were able to completely stop steroids after 3 months. Exacerbation’s, hospital and GP visits were reduced from 8.1 per patient to 0.166, representing a 100% reduction in GP visits. ACT score improved 50.79% from 12.6 to 19 [p=0.029]; while AQLQ[s] score improved 27.3%. No significant side effects were reported.
This study demonstrates that Benralizumab improves control in severe eosinophilic asthma, reducing exacerbations, steroid dependency and doctor visits.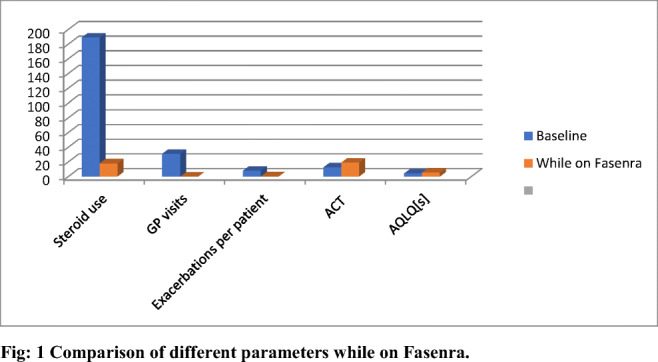
References
1. Casey D, Walsh LJ, Murphy J, Plant BJ, Murphy DM; Cork University Hospital patient experiences on Fasenra; Ir J Med Sci (2019) S268 188 (Suppl 10):S255–S320
4.24. Mepolizumab: Real life experience of IL-5 inhibitor’s use in severe Eosinophilic Asthma at St Luke General Hospital, Kilkenny
Shahzad Q,1 Zaheer M.S. 1, Helly F1, Reidy1, N, Canavan B1.
1 Department of Respiratory Medicine St. Luke’s General Hospital, Kilkenny
Mepolizumab (Nucala®), a monoclonal antibody specific for IL-5, has been shown to reduce hospitilisation rate’s for those with severe eosinophilic asthma by half when compared to placebo1. At St. Luke’s General Hospital, Co. Kilkenny (SLK) a cohort of patients (n=8) began Mepolizumab treatment for severe eosinophilic asthma. Here a retrospective study to assess efficacy of Mepolizumab in this cohort is presented.
On average patients have received of 16.50 months of treatment, with 50% (n=4) completing >18months of treatment. Post induction, the average steroid dose required has reduced by 73.77% from 22.5mg/day to 5.9mg /day [p=0.002]. Steroid dependency has decreased with 62% patients (n=5) now steroid free for 8 months. Mean eosinophil count reduced from 0.522 x10^9/L to 0.15 x10^9/L, an 81.99% reduction [p=0.0002]. Mean AQLQ scores improved by 87%, from 3.37 to 6.30 [p=0.0001]. Mean GP visits have reduced from 59 to 21 [64.40%, p=0.0006]. Participants saw an average FEV1 increase from 2.33L to 2.65L [10%, p =0.16].
Our centre’s experience is comparable to studies published by other centres in Ireland2,3, and internationally4, showing Mepolizumab is an effective treatment for severe eosinophilic asthma, reducing exacerbation frequency & steroid treatment, decreasing GP and hospital presentations and improving overall quality of life.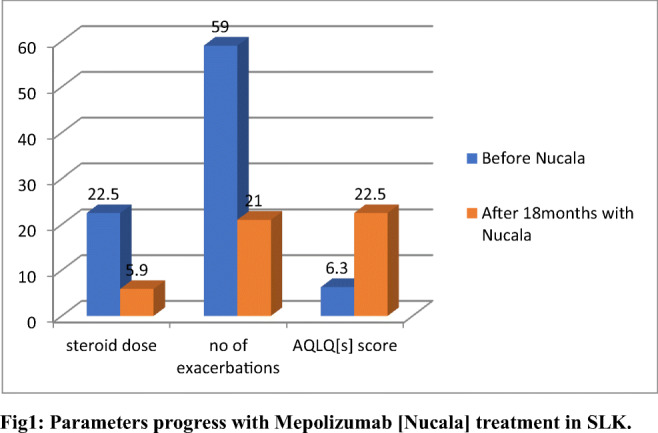
References
1. Yancey SW, Ortega HG, Keene ON, et al. Meta-analysis of asthma-related hospitalization in mepolizumab studies of severe eosinophilic asthma. J Allergy Clin Immunol. 2017;139(4):1167-1175.e2. 10.1016/j.jaci.2016.08.008
2. B. O’Connor, DR Curran, TM O’Connor, An audit of anti-IL5 therapy in a severe asthma clinic at Mercy University Hospital (MUH), Cork; Ir J Med Sci (2019) 188 (Suppl 10):S255–S320
3. Casey D, Ibrahim H, Murphy J, Plant BJ, Murphy DM; Cork University Hospital experience of Mepolizumab, one year review. Respiratory Department-Cork University Hospital; Ir J Med Sci (2019) 188 (Suppl 10):S266–S267
4. Ortega, H., Liu, M., Pavord, I., Brusselle, G., FitzGerald, J., Chetta, A., Humbert, M., Katz, L., Keene, O., Yancey, S. and Chanez, P. (2014). Mepolizumab Treatment in Patients with Severe Eosinophilic Asthma. New England Journal of Medicine, 371(13), pp.1198-1207.
4.25. The role of a Specialist Physiotherapist in Respiratory Pathways in Tallaght University Hospital (TUH).
Cunneen S. 1, Cullen J1.
1 Physiotherapy and Respiratory Departments, Tallaght University Hospital.
In January 2019 a six-month 0.5 WTE Physiotherapy post was established with the aim of reducing length of stay (LOS) and improving quality of care for respiratory patients. Funding to further progress this post was resumed in January 2020.
Data was collected and analysed from January to July 2020. The Physiotherapist screened respiratory patients on their first weekday of admission (n=351). Discharge planning commenced and 215 discharges were accelerated. Patients were discharged to Peamount Healthcare Respiratory Rehabilitation Unit (PHRRU) (n=66) if appropriate. Patients who were discharged home accessed services such as COPD Outreach (n=94), Pulmonary Rehabilitation (n=30) and Oxygen clinic (n=46) if required.
The LOS of COPD patients reduced by 1.3 days. There was a 68% increase in transfers to PHRRU and 55% of patients transferred within 24 hours of referral. TUH patients spent a cumulative of 1,491 bed days in PHRRU indicating the number of bed days saved in the acute setting. A patient satisfaction survey was conducted; 108 patients were contacted via phonecall and 49 agreed to participate. The following results were reported: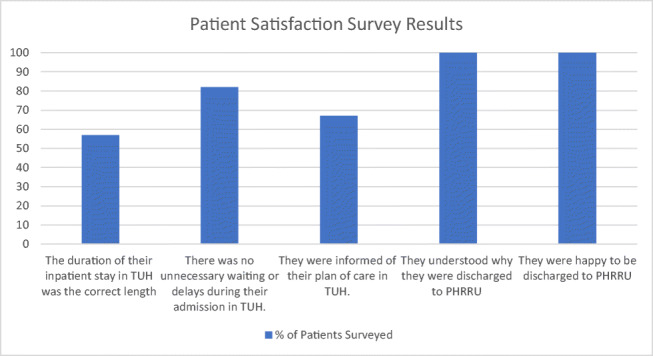
The Specialist Physiotherapist in Respiratory Pathways improved the efficiency of transfers to PHRRU. This had a positive impact on LOS for COPD patients in TUH. Patients had an early discharge from hospital with appropriate follow up and were satisfied with the service.
4.26. Utilization of specialist palliative care in the management of advanced Chronic Obstructive Pulmonary Disease (COPD) in St John’s Hospital
C Farrell1, A Scott1
1 Respiratory Department, St John’s Hospital, Limerick
Chronic Obstructive Pulmoonary Disease (COPD) is currently the fourth leading cause of death worldwide. In patients with advanced/GOLD stage D COPD the provision of specialist palliative care is an important component leading to better symptom control and more frequent use of advance care planning.
This is a retrospective review of GOLD stage D COPD patients selected from the pulmonary rehabilitation database in St John’s Hospital of Limerick. A review of charts and Inpatient Management System (IPMS) was used to record data and determine if palliative care reviewed.
45 patients with COPD were referred for pulmonary rehabilitation in the last two years. Using the combined COPD assessment 23 patients are in group D with palliative care reviewing and following up only 1 (4.3%) of these patients. 5 (22%) of group D patients had a hospital re-admission within 90 days.
An integrated approach is required with specialist palliative care and end stage pulmonary disease as this leads to better symptom management and more frequent use of advanced care planning.
4.27. Causes and Impact of Stigma in Chronic Obstructive Pulmonary Disease: A Qualitative Meta-Synthesis
Healy, A. 1, Cahalan, R. 1
1 Physiotherapy Department, School of Allied Health, University of Limerick, Castletroy, Co. Limerick
Chronic Obstructive Pulmonary Disease (COPD) is a leading cause of morbidity and mortality internationally. The number of people with COPD (pwCOPD) is growing, causing an increase in the socioeconomic burden of the disease. [1] Stigmatisation negatively impacts healthcare utilisation and quality of life for pwCOPD.
Although COPD-associated stigma has been explored in small-scale studies, evidence on its causes and implications has not been synthesised. This study aims to explore the phenomenon of stigma in COPD through its causes and impact on pwCOPD.
A qualitative meta-synthesis was conducted and reported in line with the Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ) statement. Studies were identified by systematic searching of four databases and hand-checking reference lists of relevant articles. The CASP tool was used for quality appraisal. NVivo Plus software facilitated use of Braun and Clarke’s thematic analysis framework for data synthesis. [2]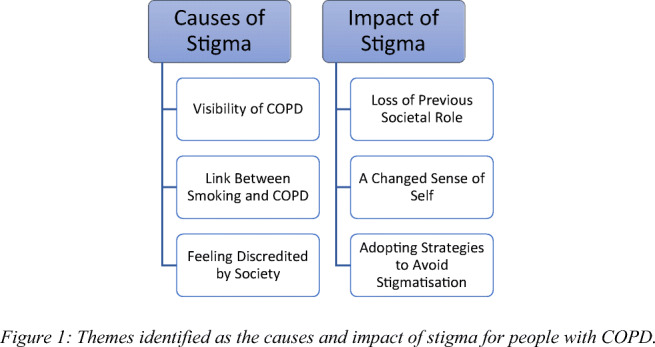
Nine high-quality studies were included in the synthesis. As per Figure 1, three themes were identified as causes of COPD-related stigma and three themes described the impact of stigma on pwCOPD. Stigmatisation of COPD stems from society’s negative perceptions of the disease and people with the disease, resulting in adverse psychosocial and lifestyle implications for pwCOPD.
References
1. Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease: 2020 Report. USA: GOLD; 2020.
2. Braun V, Clarke V. Using thematic analysis in psychology. Qualitative research in psychology. 2006;3(2):77-101.
4.28. Impact of Direct Access to a Respiratory Advanced Nurse Practitioner Service in the Emergency Department
B. Magimairaj1, P. O’Toole1, M. Ward1, A. Deegan1, S.L. O’Beirne1,2.
1 Department of Respiratory Medicine, St. Michael’s Hospital, Dun Laoghaire, Co. Dublin.
2 Department of Respiratory Medicine, St. Vincent University Hospital, Elm Park, Dublin-4.
A direct access respiratory advanced nurse practitioner (ANP) service was developed in 2018 to support St. Michael’s Hospital Emergency Department (ED) by providing evidenced-based care and timely access to patients presenting with symptoms related to asthma and/or chronic obstructive pulmonary disease (COPD).
A retrospective review of 50 care episodes between October-December 2019 was performed to evaluate interventions provided by ANPs related to care delivery and patient follow-up, with questionnaires prepared using national guidelines for asthma1 and COPD management2.
All patients received standardised, evidence-based assessment and treatment. Additional ANP initiated interventions included: respiratory inhaler management (58%), treatment of upper respiratory (36%) and gastrointestinal (6%) symptoms and smoking cessation (36%). Non-pharmacological management included: initiation of high flow oxygen (4%) and provision of health-related education e.g. trigger avoidance, peak flow diary and vaccinations. Disposition decisions included: medical referral (34%), ED review for non-respiratory symptoms (10%) and discharge (56%). Discharge follow-up included: COPD outreach service (48%), ANP-led review (16%), respiratory clinic (34%) and GP (32%). Consultation referrals included cardiology, palliative care, orthopaedics and physiotherapy.
A direct access ANP service in the ED for asthma and COPD assists evidence-based evaluation and treatment, supplements standard care by promoting patient-centred management and links patients to specialist services.
References
1. Department of Health - Management of an Acute Asthma Attack in adults, National Clinical Guideline No. 14, November 2015. Management of acute adult asthma in ED, AMU and in hospitals. Accessed at https://assets.gov.ie/11579/f2dc69b4f5c64baa927c79dcd11e4b3a.pdf accessed on 20.08.2019
2. National Clinical COPD programme, 2012, COPD Acute management bundle. accessed at http://copd.ie/wp-content/uploads/2014/10/copd-bundle.pdf accessed on 10.08.2019
Conflict of Interest: The authors have no conflict of interest to declare.
4.29. Respiratory Advanced Nurse Practitioner Led Screening Service in an at Risk Population Attending an Emergency Department
P. O’Toole.1, B. Magimairaj1., A. Deegan1., T.J. McDonnell1,2., N. Salter3., N. Ramphul3., S.L. O’Beirne1,2.
1. Department of Respiratory Medicine, St. Michael’s Hospital, Dun Laoghaire, Co. Dublin.
2. Department of Respiratory Medicine, St. Vincent University Hospital, Elm Park, Dublin 4
3. Deparment of Emergency Medicine, St. Michael’s Hospital, Dun Laoghaire, Co. Dublin.
Symptoms of chronic obstructive pulmonary disease (COPD) such as dyspnoea, cough and recurrent chest infections can be non-specific, contributing to diagnostic delays despite patient presentations to healthcare settings1. Screening at risk populations results in earlier diagnosis and treatment2. Our aim was to target an at risk population, screening them for pulmonary disease.
A retrospective chart review of at risk patients, defined as those with respiratory symptoms and >20 pack-year smoking history, referred by Emergency Department (ED) clinicians for Advanced Nurse Practitioner (ANP) assessment was performed.
Over 24 months n=61 referrals were received, 54% of which had no previous diagnosis of pulmonary disease. Among those without a prior diagnosis (n=33), n=3 (9%) had no significant disease, n=10 (30%) had normal spirometry but impairment to DLCO attributed to emphysema, n=2 (6%) had very severe COPD, n=2 (6%) severe COPD, n=3 (9%) moderate COPD, n=3 (9%) mild COPD and n=12 (36%) were diagnosed with asthma. Of those with a pre-existing respiratory disease (n=28), n=9 (28%) had a diagnosis change. ANP interventions included initiation of pharmacotherapy and crucial educational/preventative measures such as smoking cessation.
ANP-led ED COPD screening targeting symptomatic, at risk individuals has the potential to increase COPD diagnosis and improve patient care.
References
1. Lippiett K, Gillett K, Longstaff J, et al. Identifying undiagnosed COPD through searches of UK routine primarycare databases. European Respiratory Journal 2015; 46: Suppl. 59, PA338.
2. Kaplan A, Thomas M. Screening for COPD: the gap between logic and evidence. Eur Respir Rev 2017; 26: 160113
Conflict of Interest: The authors have no conflict of interest to declare.
4.30. Why this inhaler?
P. Hallahan1, L. McLeod1, C. Sheridan1, L. Fox1, C. Buckley1, C. O’Grady1
1 Department of Respiratory Medicine, Mater Misericordiae University Hospital, Dublin.
All authors contributed equally to this work.
In February 2020 the Respiratory Clinical nurse specialist (CNSp) service undertook a four week audit of COPD patients. Included were patients from both the inpatient and outpatient setting as well as nurse-led clinics. The aim of the audit was to assess if the patient’s inhaled therapy was in line with the recommendations as per GOLD Guidelines and the ABCD assessment tool (GOLD 2020).
Respiratory nurse specialists follow guidelines in order to ensure patients receive the most appropriate therapy for their disease stage. We wished to investigate, by means of audit, that we were adhering to these guidelines and that the appropriate therapy was prescribed.
A number of reasons for changing inhaled therapy were identified. These included inappropriate therapy, increased exacerbation rates, inhaler technique optimisation and up-titration of treatment. Additional reasons for changes to patients inhaled therapies were unintentional non-adherence and prescribing errors.
It was noted during the audit that 65% of the patients seen required a change of therapy, highlighting the importance of the role of the respiratory CNSp in the optimisation of inhaled therapy for COPD patients. Unfortunately due to the Covid-19 pandemic we were obliged to cut the audit short. We intend to revisit this audit when feasible.
References
1. GOLD (2020) Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Pulmonary Disease. https://goldcopd.org/wp-content/uploads/2019/11/GOLD-2020-REPORT-ver1.0wms.pdf
4.31. High need for Community care to support earlier discharge in Low DECAF scores for patients admitted with Acute Exacerbation of COPD in a level 3 hospital.
E.Burke1, A.Yunes1, H.McLoughlin1
1 Respiratory Department, Portiuncula Hospital, Ballinasloe.
Dyspnoea, Eosinopenia, Consolidation, Academia and Atrial Fibrillation (DECAF) Score is a clinical prediction tool used in patients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD). The scores reflect in-hospital mortality risk. Scores of 0-1; low risk, 2; intermediate risk and 3-6; high risk. A prolonged hospital stay during an episode of AECOPD increases the risk of associated medical complications. Using the DECAF can guide appropriate early discharge from hospital to community follow up. Hospital admissions for exacerbation of COPD are a major cost to health services. Reducing length of stay (LOS) will reduce cost. The European COPD audit (ERJ,2013) calculated the mean LOS at 8.7days. The National Institute for Health and Clinical excellence (NICE) guidelines suggest that early discharge to appropriate community care can reduce the cost burden.
A retrospective study of patients admitted with AECOPD from June to December 2019 were examined. The DECAF score and LOS was calculated on each. A prolonged LOS was defined as greater than 5 days.
A total of 47 patients were included in this study. The average LOS calculated for this group was 5.92 days. Thirty nine of this group had a DECAF score of 0-1. The average LOS for low risk patients was 5.439 days. 38.4% scoring a DECAF of 0-1 showed a prolonged length of hospital stay.
More than one third of patients could have been discharged earlier if there was suitable services in our community.
4.32. A review of the feasibility of a smartphone application (app) supporting a self- management programme among Chronic Obstructive Pulmonary Disease (COPD) patients.
L Glynn1, E Moloney1, M Klooblall1, C McCabe1, M Mc Cann1
1 Respiratory Department, Tallaght University Hospital, Tallaght, Dublin 24.
COPD has a significant impact on respiratory morbidity and mortality resulting in frequent exacerbations that often require hospital admissions. Studies have proven that self-management programmes among COPD patients result in improved self -management decisions leading to an improved quality of life. The use of a smartphone app has the potential to support the delivery of a self-management programme, thereby improving the quality of life in patients with COPD.
To evaluate the literature pertaining the use of a smartphone app in supporting a self-management programme among COPD patients.
Systematic searches of bibliographic databases such as MEDLINE, CINAHL, AMED, CENTRAL and PubMed pertaining to smartphone apps relating to self-management programmes used in COPD patients. Initial search generated 1709 articles, after screening of articles and reference lists, ten studies met the inclusion criteria for this review.
A self-management programme via a smartphone app is feasible among COPD patients. Moreover, there should be a focus on simplicity of structure and ease of use for data capture. As limited research exists, further randomised control trials are required.
References
1. Hermosa JLR Gomila AF, Maestu LP, et al. Compliance and Utility of a smartphone App for the detection of Exacerbations in Patients with Chronic Obstructive Pulmonary Disease: Cohort Study. JMIR Mhealth Uhealth. 2020;8(3):15699.
2. Park SK, Bang CH, Lee SH. Evaluating the effect of a smartphone app-based self-management program for people with COPD: A randomized controlled trial. Applied Nursing Research. 2020; 52, 1-11.
4.33. Virtually Exercising
A Review of Virtual Exercising in the University Hospital Limerick during a Pandemic
Julian, N. 1, Cullinan, M. 1, Ryan, P. 1, Ryan, N. 1, Kokina, L1., Gleeson, E1., O’Brien, A. 1
1 Respiratory Department, University Hospital Limerick, Limerick.
Pulmonary Rehabilitation (PR) as we know it ended in UHL on March 6th 2020. Uncertainty and indecision followed- lots of phone reviews and reassurance. UL MSc physiotherapy students came onboard to lend a hand. Together we endeavoured to help our current participants to finish out the course- both online and over the phone.
With a guidance document from the National Clinical Care Program in COPD & Asthma on Virtual PR released in April we set about recruiting participants for the first Virtual Pulmonary Rehabilitation Program (VPR) in the Mid West.
45% of those surveyed off the waiting list were interested in participating and felt they would have the relevant technology to participate. The Attend Anywhere platform was the chosen interface for virtual clinician-patient contact in UHL.
10 participants were assessed for the program. Assessment included- review of diagnosis via medical chart, PFTs, imaging and bloods, COPD Assessment Test, Hospital Anxiety Depression Scale, Modified Falls Efficacy Scale and 1 minute Sit to Stand.
9 completed the 8 week program- one drop out due to technological difficulties. Low uptake rates, low attendance rates and high drop out rates are common problems for PR programs. We finished our program with a 75% attendance and a 90% pass rate- with the traditional PR model we would have had up to 40% drop out rate.
Both subjective and objectives outcomes measures were very positive. The group have continued to meet to exercise via another virtual platform since completing the program. Long term compliance with the lifestyle modification from VPR will be interesting to follow up.
The group that engaged in the program and had the relevant technology and skill set to utilise the technology showed significant benefits- in keeping with face to face pulmonary rehabilitation. The fact that an independent exercise class has continued may suggest a more sustained benefit.
4.34. Chronic Obstructive Pulmonary Disease (COPD) Outreach at Tallaght University Hospital (TUH) – a 5 year activity analysis of COPD Assessment Tool (CAT) scores, average length of stay and acceptance rates onto the COPD Outreach programme.
M Ní Chléirigh1, M Kooblall1, E Moloney1, S Lane1
1 COPD Outreach Department, Tallaght University Hospital, Tallaght, Dublin 24, Éire
COPD Outreach (COPDOR) provides early supported discharge to hospital presenting patients with an acute exacerbation of COPD. The national target is to accept 20% of all COPD patients and to reduce overall hospital length of stay (LOS).
The purpose of this report was to analyse data from 2016-2020 using Microsoft Excel to review 1) CAT scores at Week 1 and Week 6 and 2) the percentage of COPD patients accepted by COPDOR and their average LOS. Data was collated from the COPD Outreach and TUH HIPE databases to analyse this activity.
CAT scores reported at week 1 showed no statistical difference from 2016-2020. The average percentage improvement from week 1 to week 6 was 36%, and was consistent from 2016-2020.
The target of accepting 20% of all COPD patients was achieved only in 2019 (21%) and will in 2020 (42% at end of August). However, these figures may be disingenuous due to substantially lower admissions rates secondary to COVID-19. Average LOS (Table 1) is at its lowest this year for patients accepted on the COPDOR Programme potentially due to a notable shift towards earlier supported discharge pathways (LOS 0-3 days) and away from supported discharges (LOS 4+ days).
References
1. Health Service Executive. National clinical programme for respiratory: end to end COPD model of care; 2019.
2. Health Service Executive. COPD outreach programme model of care, national COPD quality in clinical care programme; 2011.
4.35. An overview of the establishment and implementation of a Virtual Pulmonary Rehabilitation Programme for COPD and Asthma patients in Cork University during a global pandemic.
O’Grady M1, Bowen B1, Plant BJ1, Kennedy M1, Henry MT1, Murphy D1
1 Department of Respiratory Medicine, Cork University Hospital.
In a time of unprecedented requirement to adhere to HSE guidance on infection control and public health guidance on social distancing, there has been a necessity to turn to technology to enhance and optimise patient management.
A virtual pulmonary rehabilitation (VPR) programme was established in CUH for patients on the waiting list for conventional PR. 13 patients were contacted, 6 accepted enrolment and 4 completed the first VPR programme which comprised of a 7 week group exercise and education programme using the WebEx Platform.
1min STS test was used to assess functional exercise capacity. The HADS, CAT and MMRC were completed pre and post programme. Results were analysed using a t-test. Mean age of participants was 68 years. (75% COPD, 25% ACOS). Mean improvement in 1min STS = 8.75 repetitions (P 0.067). Each patient improved by >7 reps with an improvement ≥3 showing clinical significance. There were non significant improvements in CAT.
In this small pilot study, a VPR programme has shown to be an effective way of improving exercise capacity at a time when it is not feasible to run conventional PR programmes.
4.36. Satisfaction among patients accepted onto Chronic Obstructive Pulmonary Disease (COPD) Outreach in Tallaght University Hospital (TUH) during the nationwide lockdown period as compared to patients accepted pre COVID19
C Scallan1, A Armstrong1, M Kooblall2, A Subramanian2, E Moloney2, S Lane2
1COPD Outreach, Tallaght University Hospital, Dublin 24.
2 Respiratory Department, Tallaght University Hospital, Dublin 24.
This study looked at the satisfaction of patients accepted onto the COPD Outreach programme in TUH during the nationwide lockdown period (March to May 2020) as compared to patients accepted pre COVID19.
The COVID19 pandemic has caused major disruption across the health service in Ireland – COPD Outreach in TUH included. The usual programme of home visits to patients following discharge with an acute exacerbation of COPD was interrupted. As a result, all patient contact during the lockdown period was completed over the phone. This was not ideal and it was decided to assess patients’ satisfaction with the quality of the care received during this period.
Satisfaction questionnaires are routinely posted out to patients following their discharge from COPD Outreach. Eighteen patients were accepted onto the COPD Outreach programme during the lockdown period. These received telecontact questionnaires by the unbiased hospital administration team. Eighteen questionnaires from 2019 were randomly selected and the responses were compared to those from the lockdown period.
Both groups were “very satisfied” with the overall care and service they received from the COPD Outreach team. This is very positive as it may allow the service to expand to those outside our traditional catchment area in the future.
4.37. Do Patients Continue to Exercise After Completion of a Pulmonary Rehabilitation Programme?
P. Tonge1 & S.L. O’Beirne1,2
1 Department of Respiratory Medicine, St. Michael’s Hospital, Dun Laoghaire, Co. Dublin.
2 Department of Respiratory Medicine, St. Vincent’s University Hospital, Elm Park, Dublin 4.
Pulmonary Rehabilitation (PR) is recommended for patients with chronic obstructive pulmonary disease (COPD) to improve quality of life, and to reduce exacerbation frequency and hospitalisations1,2. However, the benefits of PR appear to decline over time if participants do not continue maintenance exercise2. As a result, PR participants should be encouraged to continue exercising, including through community exercise groups, to maintain benefits.
This study aimed to ascertain if patients who completed PR remained compliant with exercise afterwards, and whether they joined a community COPD exercise group. Patients who completed PR including a post-PR assessment between January 2019–January 2020 (n=83) were contacted by telephone and responded to a questionnaire.
77% (n=64) of patients completed the telephone questionnaire. Of these, 27 (42%) were female and 37 (58%) male, with a mean age of 70±11 years. The majority (80%, n=51) had a diagnosis of COPD. Overall 81% (n=52) of patients reported continuing to exercise after PR completion with no significant difference in age or sex between groups. Of these, only 29% (n=15) reported joining a community COPD exercise group.
These data suggest that most patients continue to exercise upon completion of PR but do so independently without joining community COPD exercise groups.
References
1. Global Initiative for Chronic Obstructive Lung Disease (2019) Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease 2019 Report.
2. Bolton, C., Bevan-Smith, E., Blakey, J., Crowe, P., Elkin, S., Garrod, R., Greening, N., Heslop, K., Hull, J., Man, W., Morgan, M., Proud, D., Roberts, C., Sewell, L., Singh, S., Walker, P. & Walmsley, S. (2013) British Thoracic Society guideline on pulmonary rehabilitation in adults: accredited by NICE. Thorax, 68(2), ii1-ii30.
Conflict of Interest: The authors have no conflict of interest to declare.
4.38. The National Alpha-1 Antitrypsin Deficiency Targeted Detection Programme
T.P. Carroll, O. Cahalane1, E. Howard1, E. Pentony1, I. Ferrarotti2, S. Ottaviani2, G. Kelly and N.G. McElvaney.
Alpha-1 Foundation Ireland, RCSI Education & Research Centre, Beaumont Hospital, Dublin 9. 1Department of Biochemistry, Beaumont Hospital, Dublin 9. 2Department of Biochemistry and Clinical Genetics, University of Pavia, Italy.
4.39. Clinical Features of SS Alpha-1 Antitrypsin Deficiency – A Risk Genotype?
D Fraughen1, P Hawkins1, T Carroll1, G Kelly1, C Gunaratnam1, NG McElvaney1.
1 Irish Centre for Genetic Lung Disease, RCSI Education and Research Centre, Beaumont Hospital.
Alpha-1 antitrypsin deficiency (AATD) is a genetic disorder that can cause lung, liver, and rarely skin disease. Guidelines advocate screening all COPD, poorly-controlled asthma, and cryptogenic liver disease patients, as well as first degree relatives of known AATD patients. The most common harmful mutation is Z (1 in 25 Irish people are carriers) which leads to a severe plasma deficiency if AAT. 1 in 10 Irish individuals carry the less harmful S mutation (Glu264Val, rs17580), one of the highest allele frequencies in Europe. However, the true clinical significance of the S mutation remains poorly understood (1).
We evaluated the clinical characteristics of individuals homozygous for the S mutation enrolled on the National AATD Registry through chart reviews.
23 individuals with the SS genotype were included in our analysis. Basic demographics, smoking status with pack-year, asthma diagnosis, Lung findings on CT and presence of liver disease were analysed.
Our study revealed that the prevalence of lung disease in this cohort of SS individuals remains low but larger study is needed to confirm this AAT genotype as low risk. The Alpha-1 Registry is an essential resource to collate data and answer this question.
Reference
1. Carroll TP, O'Connor CA, Floyd O, McPartlin J, Kelleher DP, O'Brien G, et al. The prevalence of alpha-1 antitrypsin deficiency in Ireland. Respir Res. 2011;12(1):91.
4.40. Patients and Doctors Satisfaction with Virtual Clinic in a Respiratory Department
D Halim1, S Toland1, RW Costello1, NG McElvaney1, C Gunaratnam1, P Branagan1, K Hurley1, E O’Brien1, R Morgan1, I Sulaiman1
1 Respiratory Department, Beaumont Hospital
In light of the COVID19 pandemic and need for social distancing, many out-patient services have opted for phone call consultation or virtual clinic (VC). We aimed to establish if VC is a viable alternative to face-to-face clinic (F2FC) in a respiratory department.
One-Hundred participants were asked to fill out patient satisfaction questionnaires via phone call. Eighteen physicians within the department were also asked to fill out questionnaires.
The majority of patients (94%) were satisfied with VC and agreed that VC was convenient (n=90), information was relayed clearly (n=96) and covered everything that patients wanted to discuss (n=92). VC was deemed comparable to F2FC by 83 patients. However, 44 (44%) patients preferred F2FC in the future. From the physician perspective, 10 (56%) were satisfied with VC and 8 (45%) felt that it was comparable to F2FC. Interestingly, 11 (61%) physicians had no specific clinic preferences. Through Chi-square test, we found significant difference where patients had higher mean score as compared to physicians for all studied variables.
Virtual clinics, by phone call, is a feasible medium to continue running a respiratory out patient service while adhering to social distancing with good patient satisfaction. In addition we have identified ways to improve this service.
4.41. COPD and Asthma Patient Preferences - Virtual versus Standard Respiratory Nurse-Led Clinics
M. Ward1, P. O’Toole1, B. Magimairaj1, A. Deegan1 & S.L. O’Beirne1,2.
1 Department of Respiratory Medicine, St. Michael’s Hospital, Dun Laoghaire, Co. Dublin.
2 Department of Respiratory Medicine, St. Vincent’s University Hospital, Dublin 4.
During the COVID-19 pandemic virtual clinics (VC) were utilised in many outpatient settings in place of standard outpatient visits, with some centres continuing this following the lockdown period. This study aimed to ascertain whether, if given the option, existing respiratory nurse-led clinic (NLC) patients with chronic obstructive pulmonary disease (COPD) and/or asthma, would prefer a VC over a standard outpatient clinic visit.
35 current respiratory NLC patients were surveyed by phone regarding their preferences related to virtual vs standard outpatient clinics, and digital literacy and access.
The mean age of participants was 56 years, 27 (77%) were female and 8 (23%) were male. 18 (51%) had COPD, 12 (34%) had asthma and 5 (15%) had asthma-COPD overlap syndrome. The majority of patients (n=20, 57%) preferred to attend a standard outpatient clinic. Of the 15 (43%) who preferred to be reviewed virtually, only 3 (20%) would utilise this option if they felt their condition was unstable, with the remaining 12 (80%), preferring to attend an outpatient clinic if unwell.
This study demonstrates that, while VC have a role, particularly during a lockdown period, the majority of patients within this service would rather attend the outpatient clinic as normal, particularly when unwell.
Conflict of Interest: The authors have no conflict of interest to declare.
IRISH THORACIC SOCIETY ORAL PRESENTATIONS IV
4.1.1. An Observation of Infection Risks in Severe Asthma Patients on Anti-IL5 Therapy
A Basirat1, J Maxwell1, J Joseph1, A Bradley1, E Moloney1, A Subramaniam1, S Lane1
1 Department of Respiratory Medicine, Tallaght University Hospital/ Peamount Healthcare, Dublin
Monoclonal antibody against interleukin-5, is approved as an add-on treatment for adult patients with severe eosinophilic asthma (SEA). Current literature suggests immunosuppressive conditions and medications predispose to an increased risk of opportunistic infections. We aimed to evaluate the incidence of opportunistic infections on SEA patients receiving anti IL-5 therapy.
A retrospective telephonic survey was conducted on all SEA patients treated with Reslizumab, Mepolizumab and Benralizumab in Tallaght and Peamount Hospital. Key parameters assessed included annual exacerbation rate, corticosteroid therapy, incidence of opportunistic infection; namely varicella and herpes zoster, parasitic and COVID-19 infections as well as vaccination history.
Thirty-six patients (mean age: 57.3 years, 56% female) were included. Mean duration of therapy was 23.9 months, and 50% of patients were on oral corticosteroids. The mean annual exacerbation rate was 2.7. Twenty-four patients reported prior varicella infection or vaccination, and none received herpes zoster vaccination. Two patients (5%) receiving Mepolizumab experienced on-treatment herpes zoster infection, while there was no parasitic or COVID-19 infections reported.
In conclusion, SEA patients on anti IL-5 therapy do not seem to present a higher risk of opportunistic infections and this result appears similar to clinical trials.
4.1.2. Is Fractional Exhaled Nitric Oxide measurement relevant in Athletes?
J. Oliveira1, H. Dias1, M. Nagle1, S. Navarro1, A. Mulgrew1, A. Jahangir1
1 Respiratory Department, Bon Secours Hospital, Tralee, Co Kerry.
The Fractional Exhaled Nitric Oxide (FENO) is a non-invasive tool of measuring eosinophilic airway inflammation and assessing airways disease. In sports, the presence of asthma and related diseases is frequent, therefore FENO may be a helpful marker evaluating those cases.
We performed a cross-sectional study aiming to evaluate the FENO levels in Elite Gaelic Athletes and its correlation with spirometry and presence of airway symptoms (upper or lower). The study group consisted of 43 male athletes aged 21 to 32. On December 2019, we performed spirometry and FENO measurements on all subjects and collected their background clinical history and respiratory symptoms.
A weak negative correlation was found between FENO and Forced Expiratory Volume (FEV1) values (r=-0,2639; p=0,087). We verified that the presence of airway symptoms in athletes with history of asthma was 67% while without was 35%, however not significantly different (p=0,133).
Significant difference was found in values for FENO between 25 athletes without and 18 with airway symptoms (p=0,0348). Analysing the type of symptoms, mean FENO was higher in upper airway symptoms (mean=66,40) compared to lower airway symptoms (mean=50,63), even though not significantly different (p=0,4940). Thus FENO seems to correlate with airway symptoms but not with a drop in FEV1.
4.1.3. A survey of physiotherapists use of airway clearance techniques for patients experiencing exacerbations of chronic obstructive pulmonary disease in the Republic of Ireland
C. Hanrahan1, Pedlow, K2, Osadnik, C3.
1. Discipline of Physiotherapy, School of Clinical Therapies, College of Medicine and Health, University College Cork, Cork, Ireland
2. School of Health Sciences, Jordanstown Campus, Shore Road, Newtownabbey, Co. Antrim, BT37 OQB
3. Discipline of Physiotherapy, School of Primary and Allied Health Care, Monash University, Building G, Level 3, McMahons Road, Frankston Victoria 3199, Australia
The purpose of this study was to explore current practices of physiotherapists’ use of airway clearance techniques (ACTs) for patients experiencing exacerbations of chronic obstructive pulmonary disease (ECOPD) in the Republic of Ireland (ROI).
A cross-sectional online survey using multiple-choice questions and Likert scales was distributed to 202 participants directly via email and via the Irish Society of Chartered Physiotherapists (ISCP).
Seventy of 202 responses (35%) were received. Physiotherapists in ROI use ACTs physical exercise (PE) (n=93%) and breathing exercises (n=90%) most frequently for ECOPD. Sputum management (n=94%) is the most commonly reported indicator for use of ACTs. The majority of physiotherapists (n=60%) reported being unsure of the literature or finding the literature conflicting/non-existent in relation to ACTs.
Despite lack of evidence to support the use of ACTs, physiotherapists continue to use them in their management of ECOPD, consistent with similar international findings (1,2). In order to reduce the disease burden of COPD and improve patients’ quality of life, future studies are required to determine the efficacy of PE and the combination of PE with other ACTs. The clear translation of research findings to physiotherapists must be prioritised in order to disseminate clinically useful strategies for the management of ECOPD.
References
1. Osadnik CR, McDonald, CF, Holland AE. Airway clearance techniques in acute exacerbations of COPD: a survey of Australian physiotherapy practice. Physiotherapy. 2013;99: 101-106
2. Westerdahl E, Osadnik, C, Emtner M. Airway clearance techniques for patients with acute exacerbations of chronic obstructive pulmonary disease; Physical therapy practice in Sweden. Journal Chronic respiratory disease. 2019;16:1-8
4.1.4. An Acoustic Method of Determining Dry Powder Inhaler Suitability in Obstructive Lung Disease
T. A. McCartan1, G. Greene1, C. Mulvey1, E. MacHale1, V. Brennan1, L. Lombard1, J. Walsh1, R. W. Costello1
1 INCA Group, Royal College of Surgeons in Ireland
Dry powder inhalers (DPIs) are an effective method of medication delivery, however, if a patient cannot provide sufficient inspiratory flow, inadequate medication reaches distal airways. We describe the development of a cost-effective acoustic device that can accurately determine whether a patient is suitable for a DPI.
A small, T-shaped, hand-held acoustic device with a mouthpiece, inflow aperture and a resonance chamber was designed. Upon inhalation through the mouthpiece, air flows in through the inflow aperture and is directed into the resonance chamber by a labium. The device was specially designed to favour different ratios of fundamental and harmonic acoustic resonance at different airflows.
The device’s acoustic transition point, the inspiratory flow rate above which the device acoustics change to mark sufficient airflow, was tailored to account for the resistance and required airflow of common DPIs. A simple audio analysis program that can be employed on smartphones was used to analyse acoustics via a Fast Fourier Transform. The current device version detects sufficient airflow with 95.2% sensitivity and 100% specificity.
In conclusion, we developed a small, extremely cheap acoustic device suitable for biodegradable materials (PLA) that determines DPI suitability, and therefore whether an aerosolised or nebulised medication is more appropriate.
4.1.5. Long Term Outcomes in Patients Treated with Non-invasive Ventilation for Hypercarbic Respiratory Failure
S O Brien1, C Gill1, N Cograve2, RJ Fahy1
1 Department of Respiratory Medicine, St. James’ Hospital, Dublin
2 School of Medicine, Trinity College Dublin, Dublin
Chronic Obstructive Lung Disease (COPD) remains a major cause of morbidity and mortality across the world. (1) We evaluated survival at 1,2 and 5 years in a cohort of patients with COPD requiring acute inpatient non-invasive ventilation. We analysed prognostic indices to evaluate if they were predictive of mortality.
We performed a retrospective chart review of all patients who were admitted to St. James’s Hospital respiratory ward with acute hypercarbic respiratory failure who required non-invasive ventilation (NIV) over a 12 month period and followed their outcomes over 5 years.
99 patients were identified over a 12 month period from January to December 2011. Survival at 1, 2 and 5 years was 65% (n= 64), 42% (n=42) and 25% (n=25) respectively. Increasing age (p<0.001) and a lower serum albumin (p <0.005) were predictive of worse survival. There was a trend towards improved five year survival in the group who had pre-existing home NIV prior to admission compared to no NIV therapy at home but this did not reach statistical significance (Figure 1, p value< 0.088).
This study highlights the high mortality in patients with COPD admitted with hypercarbic respiratory failure requiring NIV. Home NIV may be protective however this did not reach statistical significance. This adds to our knowledge of the protective benefits already known in relation to home NIV in COPD. (2)
References
1. Müllerova H, Maselli DJ, Locantore N, et al. Hospitalized exacerbations of COPD: risk factors and outcomes in the ECLIPSE cohort. Chest. 2015;147(4):999-1007. 10.1378/chest.14-0655.
2. Murphy PB, Rehal S, Arbane G, et al. Effect of Home Noninvasive Ventilation With Oxygen Therapy vs Oxygen Therapy Alone on Hospital Readmission or Death After an Acute COPD Exacerbation: A Randomized Clinical Trial. JAMA. 2017;317(21):2177–2186. 10.1001/jama.2017.4451.
5. Irish Thoracic Society Paediatric Forum
5.1. Interlobar IL-8 variation in pre-school children with CF. Interim findings of the Study to Evaluate the Additional Gains of Upper and Lower Lobe Sampling in Children with CF (SEAGULLS).
Butler D1,3, Montague T2, O’Sullivan N2, Cox D1,2, McNally P1,2,3.
1 National Children’s Research Centre, Crumlin, Dublin, Ireland.
2 Children’s Health Ireland at Crumlin, Crumlin, Dublin, Ireland.
3 RCSI Department of Paediatrics, RCSI, Dublin, Ireland.
Six lobe Bronchoalveolar lavage (BAL) during bronchoscopy in children has been reported to be safe and confer a higher microbiological yield. Regional variability in CF lung disease is well described clinically but the etiology remains incompletely understood. The aim of our study is to assess the safety of a standardised six lobe BAL collection technique using 2x1ml/kg/lobe and to evaluate the factors contributing to regional variability in infection and inflammation. Samples were processed into individual lobar, two (RML & lingula) and six lobe pooled aliquots. In this interim analysis, IL-8 was measured in BAL supernatant using a commercially available kit.
Samples from Five subjects were included with mean age 3.4yrs (range 2-5yrs). Log10IL-8 values per lobe (mean, 95% CI) showed RML (1.88, 0.67-3.09), RLL (2.56, 1.35-3.78), RUL (2.21, 1.13-3.29), lingula (2.39, 1.22-3.56), LUL (2.06, 0.75-3.37), LLL (2.45, 1.34-3.55), pooled RML & Lingula (2.35, 1.34-3.55) and six lobes (2.98, 2.52-3.45). Assessing for interlobar variation using a t-test demonstrated the RML has significantly lower IL-8 when compared the six lobes pooled in this cohort (p=0.047).
This interim analysis demonstrated variable IL-8 concentrations across anatomically separated lung regions. Further analysis with larger numbers is underway to assess this lobar variability more comprehensively.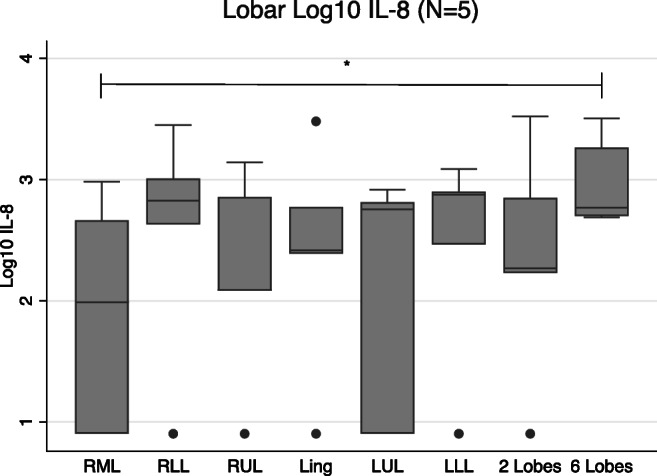
5.2. Gender difference results in increase in adolescent smoking in 2019 in Ireland- European trend analysis of current smoking prevalence 1995-2019
J Hanafin1, S Sunday1, S Keogan1, Luke Clancy1
1TobaccoFree Research Institute Ireland (TFRI), TU Dublin, Dublin 8
We examine trends in 30-day smoking among adolescents in Ireland and Europe, 1995-2020.
Ireland has participated in seven data collection waves of ESPAD (European Schools Project for Alcohol and Other Drugs) between 1995 and 2019, during which time more than 500,000 students have completed questionnaires on substance use, including cigarettes.
In 2019, some 100,000 students participated in ESPAD. In Ireland, 1967 students, born in 2003, were surveyed from a stratified random sample of 50 Irish schools.
We compared prevalence and gender differences in the Irish and European samples at different time points from 1995 to 2019.
In Ireland and across Europe, total prevalence of 30-day smoking decreased significantly between 1995 and 2019. Ireland’s decrease (from 41% to 14%) was more dramatic than the European average (32% to 20%). Ireland’s current prevalence is lower than the European average. However, while there was a decline of 5% in the European average between 2015 and 2019, Ireland’s decreasing trend reversed, accounted for by an increase in male smoking from 13% to 14%.
In Ireland, smoking prevalence in 15-16-year-olds has increased for the first time in 25 years. Further focused action is urgently needed to achieve a prevalence of 5% by 2025.
Conflicts of interest: None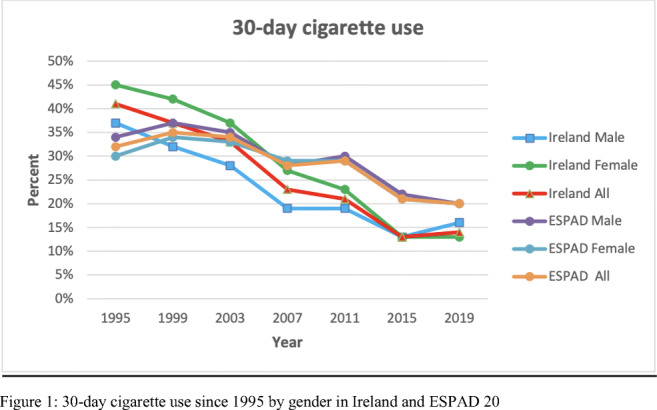
5.3. Worrying changes in adolescent e-cigarette use 2014-2019: A secondary analysis of five Irish health datasets
J Hanafin1, S Sunday1, S Keogan1, Luke Clancy1
1TobaccoFree Research Institute Ireland (TFRI), TU Dublin, Dublin 8
E-cigarette use is increasing worldwide. Concerns about adolescent use include harms (known and unknown), nicotine addiction, and as a “gateway” drug.
Secondary analysis was carried out on five Irish health datasets, with questions on adolescent e-cigarette, all stratified random samples in school-based settings: ECIGS-TFRI 2014 (N=817), ESPAD-TFRI 2015 (N=1508), SILNE-R-TFRI 2016 (N=2051), GUI 2017 (N=6216), ESPAD-TFRI 2019 (N=3556). We report on 16 and 17 year olds.
Descriptive statistical techniques were used to estimate changes in prevalence, reasons for trying e-cigarettes, and relationship with tobacco at first use.
Prevalence of ever-use increased from 23% in 2014 to 39% in 2019, representing a rapid increase, particularly since 2016. Curiosity (66%) and friends (29%) are now the two main reasons adolescents use e-cigarettes. Those saying they had never used tobacco when they first tried e-cigarettes increased from 32% in 2015 to 68% in 2019.
E-cigarette use has risen rapidly among adolescents in Ireland since 2014. E-cigarettes are not used by adolescents for smoking cessation. The majority of adolescents who use e-cigarettes were not smokers when they started using e-cigarettes, pointing to a worrying new route into nicotine addiction. Current tobacco control regulations for young people should be extended to include e-cigarettes.
| Changes in |
16 year olds n (%) |
17 year olds n (%) |
| Prevalence of e-cigarette ever-use | ||
| ESPAD-TFRI 2019 | 754 (38.8) | 279 (37.5) |
| GUI 2017 | 1564 (31.3) | |
| SILNE-R-TFRI 2016 | 148 (31.8) | 85 (50.0) |
| ESPAD-TFRI 2015 | 252 (24.2) | 98 (26.3) |
| ECIGS-TFRI 2014 | 77 (25.7) | 101 (23.0) |
| Reasons for trying e-cigarettes | ||
| ESPAD-TFRI 2019 | ||
|
To quit smoking Because friends were using it Out of curiosity |
16 (3.4) 137 (28.8) 315 (66.3) |
14 (5.0) 83 (29.8) 187 (67.0) |
| ESPAD-TFRI 2015 | ||
|
To quit smoking As an alternative to tobacco smoking Because friends were using it Out of curiosity |
48 (19.2) 27 (10.8) 57 (22.8) 151 (60.4) |
15 (15.5) 9 (9.3) 25 (25.8) 64 (66.0) |
| Relationship with Tobacco when first tried e-cigarettes | ||
| ESPAD-TFRI 2019 | ||
|
I have never smoked tobacco I smoked tobacco occasionally I smoke tobacco regularly |
461 (66.7) 168 (24.3) 57 (8.9) |
149 (58.7) 83 (32.7) 22 (8.7) |
| SILNE-R-TFRI 2016 | ||
|
I have never smoked tobacco I have tried tobacco but don’t use it regularly I smoked tobacco occasionally/regularly |
10 (19.6) 0 (0.0) - |
0 (0.0) 0 (0.0) |
| ESPAD-TFRI 2015 | ||
|
I have never smoked tobacco I smoked tobacco occasionally I smoke tobacco regularly |
76 (32.2) 123 (52.1) 37 (15.7) |
31 (34.1) 42 (46.1) 18 (19.8) |
Table 1. Changes among Irish 16 and 17 year olds between 2014 and 2019 in prevalence of e-cigarette ever-use, reasons for trying e-cigarettes, and relationship with tobacco when first trying e-cigarettes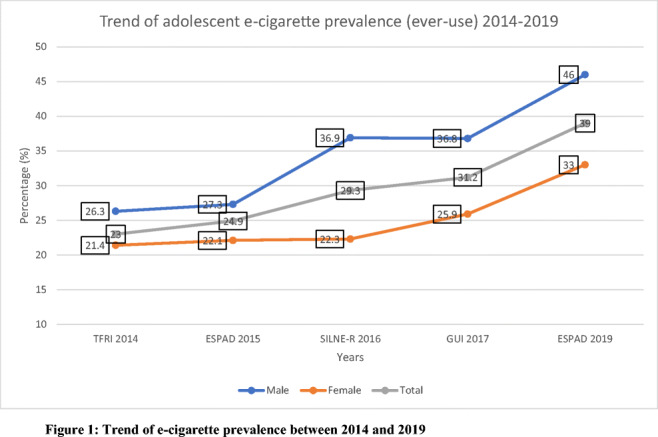
Conflicts of interest: None
References
1. Electronic cigarette use among Irish youth: A cross sectional study of prevalence and associated factors. Babineau K, Taylor K, Clancy L (2015). PLoS ONE 10(5): e0126419. 10.1371/journal.pone.0126419
2. E-cigarettes: effective cessation tools or public health threat? Clancy L and Babineau K (2016). QJM: An International Journal of Medicine, 109(2):
5.4. Aerosol Delivery Characterisation during Simulated Mechanical Ventilation of a Neonate
L. Gallagher1, M. Joyce1, E. Fernández Fernández1, & R. MacLoughlin1
1Aerogen, IDA Business Park, Dangan, Galway, Ireland.
Aerosol therapy is commonly prescribed during mechanical ventilation within the neonatal intensive care setting. The objective of this study was to characterise aerosol delivery using a vibrating mesh nebuliser (VMN) and jet nebuliser (JN) at two circuit positions during simulated neonatal mechanical ventilation in an infant incubator.
A VMN (Aerogen Solo, Aerogen, Ireland) and JN (Cirrus™2, Intersurgical, UK) were placed at the dry side and 30 cm before the wye within a humidified circuit (Fisher & Paykel, New Zealand) connected to a Servo-U Ventilator (Getinge, Germany)(Vt12mL, 60BPM, I:E 1:2). A 3.0mm endotracheal tube (ETT) was attached to a test lung and placed within an isolette (Dräger Air-Shields C2000, Germany) at 37°C. 2000 μg salbutamol was nebulised, and aerosol was captured distal to the ETT(n=5). Lung dose was quantified using UV-spectrophotometry (276nm).
| Lung Dose (μg) | |||
| Nebuliser | 30 cm before the wye | Dry Side | P-Value |
| Aerogen Solo | 155.45 ± 9.71 | 40.00 ± 8.20 | <0.001 |
| Cirrus™2 JN | 31.21 ± 4.37 | 33.94 ± 6.83 | 0.48 |
| P-Value | <0.001 | 0.25 | |
Results indicate that nebuliser type and circuit position significantly impact aerosol delivery in a simulated mechanically ventilated neonate, with the VMN being the most efficient device when located outside the isolette, 30 cm before the wye.
Conflicts of Interest:
All authors are employees of Aerogen.
5.5. Compliance and efficacy of non-invasive ventilation in children with Down syndrome
L. MacDonagh1, L. Farrell2, R. O'Reilly2, P. McNally2, S. Javadpour2, DW. Cox1,2
1. School of Medicine, University College Dublin, Dublin 4.
2. Respiratory Department, Children's Health Ireland, Crumlin, Dublin 12.
Children with Down syndrome (DS) have increased prevalence of obstructive sleep apnoea (OSA), for which non-invasive ventilation (NIV) is a cornerstone of management. Compliance has previously been described as a major issue in the therapeutic efficacy of NIV within the DS population. This study aimed to measure adherence and delivery of NIV within a paediatric DS cohort.
This retrospective cohort study involved 106 children with confirmed OSA and home NIV with downloadable data. Children were divided into DS (n=44) and non-DS cohorts (n=62). Adherence and clinical outcomes, such as apnoea-hypopnoea index (AHI), delivery and system leakage were recorded and compared between DS and non-DS cohorts and within the DS cohort based on age and surgical history.
Significantly greater NIV usage, in the form of percentage days used, was observed in the DS cohort relative to non-DS counterparts (p=0.031). However, children with DS displayed significantly greater system leakage (p=0.022) and increased AHI (p=0.0493). Surprisingly, those with DS with prior cardiothoracic surgery showed significantly reduced compliance.
These data confirm that satisfactory NIV adherence is achievable in children with DS. However, we have identified excessive system leak at the machine-patient interface as a factor, which could undermine NIV efficacy in children with DS.
5.6. Interleukin-22 and Neutrophil Proteins as Predictors of Future Disease Severity in Children with Cystic Fibrosis
E. Reece1§, J. Renwick 1§, J Walsh2, R Walsh2, T Persaud2, C O’Leary2, S. C. Donnelly3 † and P. Greally 2 †
1.Clinical Microbiology, Trinity College Dublin, Ireland. 2 Children’s Health Ireland and Tallaght
University Hospital, Dublin, Ireland. 3 Department of Medicine, Tallaght University Hospital and Trinity College Dublin, Ireland.
§ These authors contributed equally to this manuscript
† Joint senior authors
5.7. Impact of Carers’ Smoking Status on Childhood Obesity in the Growing up in Ireland Cohort Study
S. Sunday1, K.Zubair1
1School of Public Health, University College Cork
5.8. An in vitro investigation of aerosolised Budesonide delivery in simulated adult and paediatric spontaneous breathing models using a vibrating mesh nebuliser
P. J. Naughton1, B. Murphy1, A. O’Sullivan1, M. Mac Giolla Eain1, M. Joyce1, R. MacLoughlin1.
1Aerogen Ltd, IDA Business Park, Dangan, Galway, Ireland.
Aerosolised corticosteroids are commonly used in the treatment and prevention of airway inflammation associated with asthma and other respiratory illnesses.1 The aim of this study was to assess aerosol delivery performance of Budesonide during simulated adult and paediatric spontaneous breathing.
A standard 2 mL dose of Budesonide (Pulmicort 0.5 mg/2 mL, Astra Zeneca, UK) was aerosolised using the Aerogen Solo (Aerogen, Ireland) in combination with the Aerogen Ultra aerosol chamber and facemask, with 2 litres per minute supplemental gas flow. A breathing simulator (Copley Scientific, UK) in combination with appropriate head models was used to generate both adult (Vt 500mL, 15 BPM, I:E 1:1) and paediatric (Vt 155 mL, 25 BPM, I:E I:2) breaths as per International Standard ISO27427.2 The mass of drug delivered to the level of the trachea was determined using UV spectrophotometry (241 nm). Five replicates were performed for each test.
Following test, the recorded tracheal doses were adult (23.36 ± 1.35 %), and paediatric (15.14 ± 1.15 %). This study confirms that high levels of Budesonide can be delivered using a vibrating mesh nebuliser. This information should inform clinicians in their approach to clinical aerosol therapy.
Conflicts of Interest:
All authors are employees of Aerogen.
References
1. Hvizdos K, Jarvis B. Budesonide inhalation suspension: a review of its use in infants, children and adults with inflammatory respiratory disorders. Drugs [Internet].
2012 Sep 17 [cited 2020 Aug 31];60(5):1141-1178. Available from: 10.2165/00003495-200060050-00010
2. ISO - ISO 27427:2019 - Anaesthetic and respiratory equipment — Nebulizing systems and components
5.9. Dexamethasone for acute asthma exacerbations and viral induced wheeze: quality improvement in a Paediatric Emergency Department
Ruddell, J.1, Trouton, M.1, Davison, G.1,2, McDonald, R.2, O’Neill, V.1, McCann, J.2, Kennedy, B.2, Mullen, S.2
1Centre for Medical Education, Queen’s University Belfast, Mulhouse Building, Mulhouse Road, Belfast, BT12 6DP, Northern Ireland
2Children’s Emergency Department, Royal Belfast Hospital for Sick Children, 274 Grosvenor Road, Belfast, BT12 6BA, Northern Ireland
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.


