Abstract
Objective
Electronic health records (EHRs) are routinely used to identify family violence, yet reliable evidence of their validity remains limited. We conducted a systematic review and meta-analysis to evaluate the positive predictive values (PPVs) of coded indicators in EHRs for identifying intimate partner violence (IPV) and child maltreatment (CM), including prenatal neglect.
Methods
We searched 18 electronic databases between January 1980 and May 2020 for studies comparing any coded indicator of IPV or CM including prenatal neglect defined as neonatal abstinence syndrome (NAS) or fetal alcohol syndrome (FAS), against an independent reference standard. We pooled PPVs for each indicator using random effects meta-analyses.
Results
We included 88 studies (3 875 183 individuals) involving 15 indicators for identifying CM in the prenatal period and childhood (0–18 years) and five indicators for IPV among women of reproductive age (12–50 years). Based on the International Classification of Disease system, the pooled PPV was over 80% for NAS (16 studies) but lower for FAS (<40%; seven studies). For young children, primary diagnoses of CM, specific injury presentations (eg, rib fractures and retinal haemorrhages) and assaults showed a high PPV for CM (pooled PPVs: 55.9%–87.8%). Indicators of IPV in women had a high PPV, with primary diagnoses correctly identifying IPV in >85% of cases.
Conclusions
Coded indicators in EHRs have a high likelihood of correctly classifying types of CM and IPV across the life course, providing a useful tool for assessment, support and monitoring of high-risk groups in health services and research.
Keywords: child abuse, health services research, epidemiology, drug withdrawal, data collection
What is already known on this topic?
Electronic health records (EHRs) are readily available and are increasingly used to identify different forms of family violence in practice and public health.
Few studies of EHRs provide comprehensive estimates on the positive predictive values (PPVs) for coded indicators of family violence including child maltreatment, prenatal neglect (neonatal abstinence syndrome or fetal alcohol syndrome) and intimate partner violence.
What this study adds?
This comprehensive meta-analysis provides PPVs of coded indicators in EHRs for different forms of family violence based on external independent reference standards.
We show that routinely coded indicators of family violence have high predictive value for identifying at-risk groups who may benefit from targeted interventions.
Findings emphasise that improving the quality and use of available coded indicators for identifying groups affected by family violence across data systems should be a public health priority.
Introduction
Intimate partner violence (IPV) and child maltreatment (CM) are forms of family violence that often go unnoticed by services,1–3 despite repeated recommendations by the WHO to improve monitoring efforts.4 5 CM and IPV refer to any act of commission or omission that causes biopsychosocial harm to a child, a future child or partner.6 7 Statutory definitions of CM in the UK include fetal alcohol syndrome (FAS) and neonatal abstinence syndrome (NAS) due to neglect or harm during pregnancy.8
Assessing health records for detailed information on family violence is time consuming and expensive. Instead, studies and services are increasingly using routinely coded electronic health records (EHRs) for assessing family violence.9 10 Coded EHRs allow for longitudinal population-based assessments, automated early warning systems and identification of high-risk populations for targeted interventions at relatively low costs.11–13 However, the potential utility of EHRs to support surveillance and clinical decisions is often undermined by reported quality issues and coded conditions are rarely validated externally.14 15 Unable to check the data themselves for accuracy, large-scale studies (eg, Global Burden of Disease Study) and services rely on routinely coded indicators based on the International Classification of Diseases (ICD) with unknown predictive values.10 16 17 The validity of coded indicators are compounded by varying case definitions, ad hoc classifications by coders5 15 18–20 and under-recording due to clinician fears of potential harm or lack of awareness.18 21
To our knowledge, no previous review has estimated the positive predictive values (PPVs) of coded indicators for different forms of family violence including CM, prenatal neglect (NAS or FAS) and IPV based on external independent reference standards (ie, not using other codes in the EHR to validate indicators). This meta-analysis provides a comprehensive summary of PPVs for multiple coded indicators in EHRs aimed at identifying family violence in general healthcare settings, compared with an independent reference standard.
Methods
We followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses for Diagnostic Test Accuracy Studies and the Meta-analysis of Observational Studies in Epidemiology guidelines.22 23 The review protocol was published in the PROSPERO registry (CRD 42019139300),24 with any protocol deviations provided in online supplementary table S1.
archdischild-2020-319027supp001.pdf (922.6KB, pdf)
Search strategy
We searched 18 electronic databases and 20 selected journals for studies published between 1 January 1970 and 24 May 2020 (complete search strategy in online supplementary table S2). Reference lists of eligible full-text articles were hand-searched and 18 frequently cited authors of eligible studies were contacted for article recommendations.
Study eligibility
Three independent reviewers (SS, RA and MS) screened abstracts, full texts and corresponding reference lists of articles using Covidence’s systematic review software.25 Any disagreement over study inclusions between reviewers was resolved by a family violence expert (RG). We included: (1) studies with data to calculate the PPV of a coded EHR indicator for a specific family violence outcome as reported by at least three other eligible studies,26 (2) studies from primary care, paediatric units (including trauma centres) or general hospital settings, (3) studies published in English/Swedish/German and (4) studies distinguishing family violence cases from non-cases (tables 1–2; online supplementary table S3-S4).
Table 1.
Key definitions of electronic health records (EHRs) and family violence
|
EHRs
Routinely collected healthcare data stored and accessible electronically as part of routine care or as part of administrative databases for wider patient, practice and billing management purposes. | |
|
Coded indicators of EHRs
Single or combination of codes aimed at identifying different forms of family violence (table 2). Codes must be based on a recognised classification system (eg, International Classification of Disease system) assigned to patients’ EHRs by a clinician or by a professional coder based on medical records (eg, discharge documentation). | |
|
Family violence outcomes
Any of the below outcomes obtained independently from the coded indicator (ie, not using other codes in the EHR to validate the indicator): | |
|
Child maltreatment (CM) Any act of commission or omission by a parent or caregiver resulting in harm, the potential for harm or threat of harm to a child (0–12 years) or an adolescent (13–19 years) including neglect, psychological, physical, sexual and emotional abuse. Harm does not need to be intended.6–8 6–8 | |
|
Neonatal abstinence syndrome (NAS) or fetal alcohol syndrome (FAS)
Statutory guidelines definition of CM in the UK include any form of maternal omission or commission during pregnancy with potential for significant biopsychosocial harm to the future child such as NAS and FAS.8 This may include compliance with prescribed medication (clinician approved) and/or maternal substance misuse during pregnancy, resulting in drug withdrawal symptoms in newborns and/or harm to the future child's biopsychosocial functioning/appearance. | |
|
Intimate partner violence (IPV) Any incident of threatening behaviour, violence or abuse (psychological, physical, sexual, financial or emotional) between adults who are, or have been, intimate partners or family members.7 In this review, studies are predominately restricted to estimates of women aged 15–50 years. | |
| Eligible methods for obtaining independent reference standards | |
| |
| |
| |
| |
| |
|
Level of certainty for distinguishing cases of family violence from non-cases in the information obtained by the reference standard
Quality ratings correspond to the level of certainty that the reference standard is a true measure of CM, NAS, FAS or IPV. Ratings 1–5 apply to CM, 1–4 apply to NAS and FAS and 1–3 apply to IPV. |
Quality rating |
|
5 (high) |
|
4 |
|
3 |
|
2 |
|
1 (low) |
The criteria for assessing studies of EHRs was adapted from McCormick et al,134 and the quality ratings for the level of certainty of CM in the reference standard were adapted from Kemp et al.29 The complete quality assessment tool is provided in online supplementary table S3.
Table 2.
Coded indicators of specific family violence outcomes as measured by the included studies
| Outcome | Indicator and period* | Descriptions* | No. data sources† | Frequently used codes‡ |
| Prenatal neglect/substance misuse during pregnancy | 20 | |||
| Neonatal abstinence syndrome (NAS) | NAS: primary diagnosis | Diagnosis of substance withdrawal symptoms in newborns, typically within the first few days after birth, resulting from drug use (commonly opioids) during pregnancy.135 | 1336 39–43 45 | ICD-9: 779.5. ICD-10: P96.1. |
| Newborn affected by drugs | Less specific indicator of NAS, defined by the fetus being affected by maternal substances, noxious influences or medications NOS. | 739 43 | ICD-9: 760.72. ICD-10: P04.4x. |
|
| Fetal alcohol syndrome (FAS) | FAS: primary diagnosis | FAS is one type of a spectrum of disorders linked to alcohol exposure during pregnancy. Symptoms include abnormal facial features, deficiencies in growth (including brain/ neurophysiology) and/or neurobehavioural impairment in children (0–19 years, typically diagnosed 2–5 years).136 | 746–52 | ICD-9: 760.71. ICD-10: Q86.0, P04.3. |
| Child maltreatment (CM) among children aged 0–19 years | 50 | |||
| CM | CM primary diagnoses | Any diagnosis of CM including neglect, abandonment, physical, sexual and psychological/emotional abuse (0–18 years). | 1914 55 59 60 62 66 68 71 77 80 82 85 87 96 97 | ICD-9: 995.5x, E967.x, E960.x-968.x. ICD-10: T74.x, Y06.x, Y07.x. |
| Abusive head trauma (AHT) | Skull and/or intracranial injuries due to inflicted blunt impact/penetration and/or violent shaking (0–5 years). Coding clusters include different degrees of certainty: ‘definite or presumptive’ and ‘probable’ AHT. Other common terms are ‘shaking infant syndrome’ or ’whiplash shaking baby syndrome’.137 | 462 80 85 138 | ICD-9: As in CM + 781.0-781.4, 800.x-801.x, 854.0 x, 950.0-950.3. ICD-10: As in CM + S06.0-S06.9, S09.7-S09.8, T90.5. |
|
| Traumatic brain injury (TBI) | Skull and/or intracranial injuries and concussion (<5 years of age) characterised by the level of loss of consciousness or altered mental status, ranging from mild TBI (in most cases a concussion) to severe TBI (patient is comatose, unable to open their eyes and so on).139 | 757 66 69 76 80 84 92 | ICD-9: 800.0-801.9, 803.0-804.9, 850.1-850.5, 850.9, 851.0-854.1, 959.01. ICD-10: S02.0, S02.1x, S02.8, S02.91, S04.02, S04.03.x, S04.04x, S06.x, S07.1, T74.4. |
|
| Skull fractures | A fracture of one or more bones of the cranial vault or skull base. | 1053 57 70 72 73 75 83 88 95 96 | ICD-9: 800.x-804.x ICD-10: S02.x |
|
| Subdural haematoma | A collection of blood between the dura and arachnoid coverings of the brain. In this review, subdural haematoma includes ICD-coded subdural haemorrhages. | 557 76 88 94 96 | ICD-9: 852.2, 432.1. ICD-10: I62.0, S06.57. |
|
| Retinal haemorrhage | Extravasation of blood into the retina, between the retina and the subhyaloid or preretinal or between the retina and the subretina. | 465 81 88 96 | ICD-9: 362.81. ICD-10: H35.6. |
|
| Upper limb fractures | In this review, referred to as fractures of the humerus, radius or the ulna. | 474 86 89 91 96 | ICD-9: 812.x, 813.x ICD-10: S42.2-S42.9, T10. |
|
| Lower limb fractures | In this review, referred to as fractures of the femur, diaphysis, tibia or fibula. | 654 56 63 67 89 96 | ICD-9: 820.x, 821.x. ICD-10: S72.x, S82.x, T12. |
|
| Rib fractures | A break in the rib bone of the thoracic skeleton. | 464 74 88 89 | ICD-9: 807.0-807.1x ICD-10: S22.3, S22.4. |
|
| Multiple burns | Burns and corrosions of multiple and unspecified body regions. | 358 88 96 | ICD-9: 946.0. ICD-10: T29.x-T32.x. |
|
| Assaults | Intentional injuries (sexual, physical, emotional or psychological) inflicted by another person. | 659 77 78 82 88 | ICD-9: E960.0-E969.0, V71.6. ICD-10: X85-Y09. |
|
| Assaults/CM/adversity | Combination of multiple broad codes deemed to meet the threshold for potential child harm including CM, assaults, drug or alcohol intoxication, poisoning of undetermined cause, concerns for psychosocial circumstances, specific fractures and/or sexual diseases in children (0–18 years). | 661 64 82 90 93 | ICD-9: As in CM + V15.4, V61.2, V71.8, E960.1, E967. ICD-10: X85-Y09, Z04.0-Z04.8, Z60.0-Z91.8. |
|
| Intimate partner violence (IPV) among women aged 12–55 years | 18 | |||
| IPV | IPV primary diagnosis | Any diagnosis of partner maltreatment syndromes including neglect, abandonment, physical, sexual and psychological abuse.140 | 3111 114 115 | ICD-9: E967.3, 995.80, 995.81. ICD-10: T74.1, Y06.0, Y07.0. |
| Assaults | Intentional injuries (sexual, physical, emotional or psychological) inflicted by another person. | 10100 102 105 107–109 112–114 116 | ICD-9: E960.0-E969.0, V71.6, V71.5. ICD-10: X85-Y09. |
|
| Head, face and neck injuries | Maxillofacial fractures (mandible fractures, zygomatic complex fractures and intracranial injuries) and crushing injuries of head and neck. | 499 103 107 110 | ICD-9: 802.0-802.9. ICD-10: S02.2, S02.6, S06.x-S07.x. |
|
| Ocular injuries (eg, orbital fractures) |
Ocular injuries such as fractures to the orbital floor and sustained scleral laceration or ruptures. | 499 103 106 117 | ICD-9: 802.6, 871.0, 871.1. ICD-10: S02.3, S05.1, S05.2-S05.3. |
|
| Contusions of upper body | Bruises or contusions of the throat, breast, upper arms/shoulders and eyelids, periocular areas and scalp. | 3101 107 110 | ICD-9: 920.x-924.x. ICD-10: S10.0-S10.9, S20.0, S40.x, S05.1, S00.1, S05.7. |
|
*Indicator definitions represent condensed descriptions for the overall category and are not representative of all ICD code descriptions.
†References represent the number of unique publications per indicator and do not necessarily match the corresponding number of data sources, as one publication can provide estimates for one indicator from several unique data sources. The same reference can also apply to multiple indicators, as one reference can report on estimates for multiple indicators.
‡Complete lists of codes by individual studies and indicators are provided in online supplementary table S8.
“x” indicates any character from fourth through seven.ICD, International Classification of Diseases; NOS, not otherwise specified.
Indicators and outcomes of family violence
An overview of key definitions of indicators and outcomes is provided in tables 1–2. Briefly, indicators were defined as any coded marker or risk factor for family violence, ranging from specific primary diagnostic codes (eg, ‘T74.1 physical abuse’) to injuries (eg, rib fractures and retinal haemorrhages), assaults and combinations of adversity-related codes (table 2). For IPV, we predominately included indicators for women (eg, >80% of study sample were women), as the health consequences for women are higher, and the prevalence among men is significantly lower.27 In terms of family violence, men’s parental status is also more difficult to ascertain than women’s. Outcomes were defined as mutually exclusive categories of family violence according to different life periods: NAS or FAS (representing the prenatal period),8 any form of CM (representing childhood) or IPV (representing women of reproductive age), respectively. Outcomes had to be ascertained and verified by an independent reference standard such as recorded multidisciplinary decisions of family violence extracted from chart reviews (table 1).
Data extraction and quality assessments
Using a piloted standardised extraction form, three reviewers independently extracted relevant study characteristics. If studies reported separate estimates for multiple codes, reference standards or age criteria, we extracted all estimates and prioritised those based on the criterion most frequently used by other studies to increase overall homogeneity. We requested additional information from 25 authors, 6 of whom responded within the 2-month deadline and were included. The risk of bias was assessed by the same three reviewers using a revised version of the Quality Assessment of Diagnostic Accuracy Studies tool (QUADAS-2; online supplementary table S4).28 We rated each study's reference standard according to assessment quality and exclusion criteria based on previous reviews (table 1).29
Data synthesis
The PPVs for each family violence outcome were calculated as the proportion of identified cases by an indicator validated as true cases by an independent reference standard. For studies that reported only sensitivity and specificity, we obtained PPVs using Bayes’ theorem.30 PPVs were pooled using random effects intercept logistic regression models with the logit transformation when at least three studies were available for the same outcome.31 The model accounts for potentially misleading back transformations of PPVs when pooling studies with highly variable sample sizes.31 Where applicable, we also examined documentation quality and coding errors by pooling the proportions of coded medical charts with missing key information (full procedures in online supplementary table S5).
We measured the extent to which the PPVs varied between studies (ie, between-study heterogeneity).32 As the PPV is a measure of proportions, we measured the between-study heterogeneity using the I2 statistic (>75%=indicates substantial heterogeneity),32 standard χ2 tests, prediction intervals (where the PPV is expected for 95% of similar future studies)32 and subgroup analyses when at least four studies were available for each subgroup.24 We used random effects meta-regression to assess for the impact of publication year on the between-study heterogeneity. The influence of individual studies was explored by serially omitting different studies from the overall estimates.
Publication bias occurs when studies with favourable results (ie, high PPV) are more likely to be published than unfavourable results.33 We explored publication bias by plotting the PPV against the SEs of individual estimates using funnel plots for indicators with at least 10 studies for the same outcome. To test for statistically significant differences in funnel plot asymmetry (ie, publication bias), we used Egger’s test and Begg’s and Mazumdar rank correlation test.33 We used R (V.3.6.1) and the ‘meta’ package with the ‘metaprop’ command to perform the analyses.34 35
Results
Study characteristics
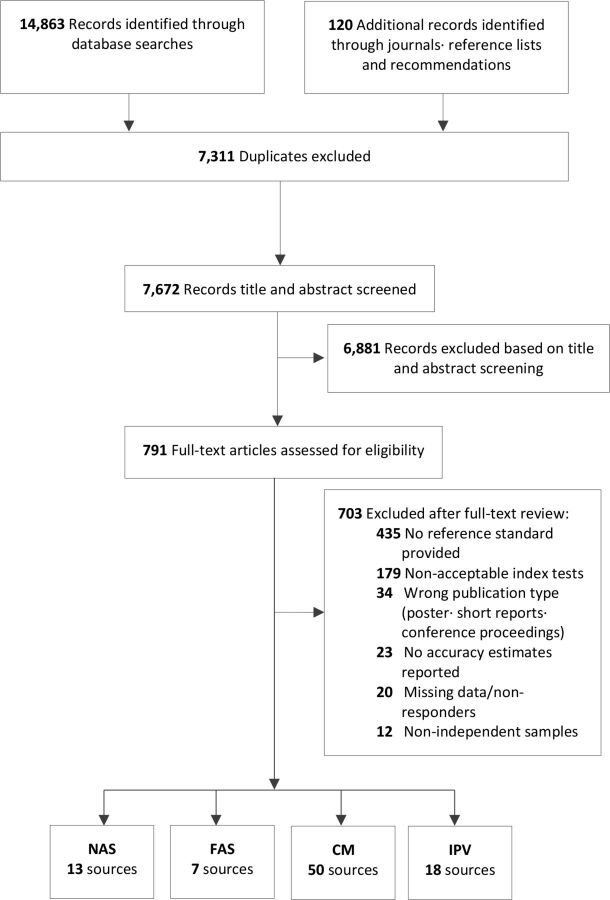
Details of the included study characteristics are provided in online supplementary tables S6–S8 and tables S12–15. In total, 65 cross-sectional and 23 longitudinal studies (81 unique publications), involving 20 indicators and 3 875 183 individuals from 11 different countries met the inclusion criteria (figure 1). Overall, 13 studies provided indicators for NAS,36–45 7 for FAS,46–52 50 for CM (0–18 years)14 53–98 and 18 for IPV among women (12–50 years).99–116 Most studies were from the USA (72 studies, 81%), with a minority from Australia (8 studies, 9%) and Europe (4 studies, 4%). The majority of indicators comprised different ICD-9 coding clusters (64 studies) or modified versions of ICD-10 (14 studies). Chart reviews with predefined family violence criteria were the most frequent type of reference standard for all outcomes (75 studies, median sample size: 301 participants). The smallest study included 38 children,94 involving all ICD-9 coded subdural haematomas (SDH) at one hospital over 10 years. The study was retained as it involved all potential cases presenting to a generic children’s hospital and as SDHs are deemed to be extremely rare in young children and an important indicator for CM.117 We included one unpublished dissertation from 2019,59 specifically assessing ICD codes for CM.
Figure 1.
Flow diagram of the 88 selected studies for this systematic review. CM, child maltreatment; FAS, fetal alcohol syndrome; IPV, intimate partner violence; NAS, neonatal abstinence syndrome.
Study quality assessment
Individual QUADAS-2 scores for studies are provided in online supplementary table S7. Overall, 31 studies (35%) were rated as high risk of bias and lower quality in most domains, and 57 studies (65%) were rated as low risk of bias and higher quality in most domains. The majority of studies were rated lower as they did not mask the outcome when reviewing coded EHRs (95%) or used a lower rated reference standard (42%; a rating <4 for CM; rating <3 for NAS, FAS or IPV).
Pooled estimates of PPVs
Table 3 depicts details for each pooled PPV and between-study heterogeneity by indicator and outcome. Individual forest plots of PPVs and study-specific ICD codes are provided in online supplementary figures S1-S19 and tables S6-S8.
Table 3.
Pooled positive predictive values for NAS, FAS, CM and IPV
| Family violence outcome | Indicator and age cut-off in years | Studies | Ref std. cases/indicator positive | Pooled PPV (95% CI) |
Between-study heterogeneity | |
| (95% prediction interval)* | I2 % | |||||
| Prenatal | ||||||
| NAS | NAS primary diagnosis | 16 | 3030/3796 | 80.9 (71.0 to 87.9) | (32.3–97.4) | 97.4 |
| Newborn affected by drugs | 7 | 384/2202 | 27.2 (16.8 to 40.8) | (6.5–66.7) | 95.0 | |
| FAS | FAS primary diagnosis | 7 | 777/2687 | 39.3 (25.3 to 55.4) | (9.7–79.6) | 97.6 |
| Childhood | ||||||
| CM | CM primary diagnoses ≤18 | 19 | 3090/3717 | 87.8 (83.4 to 91.2) | (63.5–96.8) | 92.1 |
| Abusive head trauma ≤4† | 4 | 437/477 | 91.6 (88.8 to 93.8) | (83.8–96.7) | 36.7 | |
| Traumatic brain injury ≤2 | 7 | 410/1770 | 22.9 (15.3 to 32.9) | (7.0–53.9) | 94.2 | |
| Skull fractures ≤4 | 10 | 603/2872 | 22.1 (18.5 to 26.2) | (13.2–34.7) | 79.7 | |
| Subdural haematoma/haemorrhage ≤3† | 5 | 118/211 | 55.9 (49.2 to 62.5) | (49.2–62.5) | 0.0 | |
| Retinal haemorrhages ≤4† | 4 | 60/74 | 81.1 (70.5 to 88.5) | (70.5–88.5) | 0.0 | |
| Upper limb fractures ≤3 | 4 | 249/298 | 38.5 (11.3 to 75.6) | (1.6–96.1) | 94.9 | |
| Lower limb fractures ≤3 | 6 | 90/272 | 24.0 (12.5 to 41.1) | (4.7–66.8) | 82.0 | |
| Rib fractures ≤4 | 4 | 90/126 | 88.3 (55.2 to 97.9) | (17.7–99.6) | 84.7 | |
| Multiple burns ≤2 | 3 | 70/261 | 22.5 (8.4 to 47.7) | (3.3-.70.9) | 84.3 | |
| Assaults ≤19 | 6 | 218/331 | 77.0 (46.6 to 92.7) | (19.1–97.9) | 97.1 | |
| Assaults/CM/adversity ≤19 | 6 | 1893/4033 | 55.9 (37.0 to 73.3) | (14.4–90.5) | 98.6 | |
| Women predominantly of reproductive age | ||||||
| IPV | IPV primary diagnosis ≤55 | 3 | 1946/2438 | 86.1 (72.2 to 93.6) | (53.0–97.1) | 96.3 |
| Ocular injuries ≤50† | 4 | 22/668 | 3.3 (2.2 to 5.0) | (2.2–5.0) | 0.0 | |
| Facial fractures ≤50 | 4 | 58/1550 | 11.1 (3.0 to 33.9) | (0.6–70.5) | 94.2 | |
| Upper body contusions ≤50 | 3 | 85/325 | 26.5 (18.1 to 37.0) | (13.7–44.9) | 64.9 | |
| Assaults ≤65 | 10 | 6073/20919 | 31.6 (22.3 to 42.7) | (9.2–67.9) | 99.4 | |
Each pooled positive predictive value represents the overall logit transformed estimate by indicator and outcome. Pooled estimates are based on random effects meta-analyses, unless otherwise specified. Individual forest plots are shown in the supplement.
*A 95% prediction interval is a measure of between-study variation and approximates where the PPV is to be expected for 95% of similar future studies.
†Estimates based on a fixed-effects meta-analysis due to lower between-study heterogeneity (ie, I 2 <50%).
CM, child maltreatment; EHR, electronic health record; FAS, fetal alcohol syndrome; IPV, intimate partner violence; NAS, neonatal abstinence syndrome; PPV, positive predictive value; Ref std, reference standard.
Neonatal abstinence syndrome
The pooled PPV of primary ICD diagnoses for NAS was 80.9% (95% CI 71.0% to 87.9%), and the PPV ranged from 31.8% to 98.2%, with substantial between-study heterogeneity. Most studies (54%) used the Finnegan scale (a validated 21-item scale for documented symptom severity) to determine the accuracy of the coded diagnosis,118 with a cut-off score of 8 as a reference standard (except for one study, cut-off score of 4).41 The remaining studies used recorded clinician diagnosis or required pharmacological NAS treatment as reference standards.
Fetal alcohol syndrome
For FAS, we found a low pooled PPV of 39.3% (95% CI 25.3% to 55.4%), and the PPV ranged from 14.0% to 66.9%, with large between-study heterogeneity. All studies used ICD-9 codes to identify cases (eg, alcohol affecting fetus) and required 3–5 prespecified criteria to be met in chart reviews, including facial anomalies, prenatal growth deficiencies and maternal alcohol exposure (online supplementary table S6).
Child maltreatment
The pooled PPV of primary diagnoses for CM was 87.8% (95% CI 83.4% to 91.2%) among children aged 0–18 years across 19 studies, with significant between-study heterogeneity. Individual PPVs from studies ranged from 65.0% to 100.0%.
Overall, 37 studies assessed 11 different indicators of CM (online supplementary figures S3-S14). The pooled PPVs ranged from 88.3% (95% CI 55.2% to 97.9%) for rib fractures to 19.6% (95% CI 8.9% to 37.9%) for multiple burn injuries in children under 5 years. The between-study heterogeneity ranged from small to large (I2 range 0.0%–98.5%). Four studies also assessed the PPV of poisonings (range 7.0%–95.0%),78 88 96 98 but the extreme heterogeneity precluded reliable pooling (prediction interval: 0%–100%). The majority of studies assessing injury indicators of CM actively excluded transport injuries (28 studies, 65%), metabolic bone diseases (10 studies) and birth injuries (9 studies) from the CM group.
Subgroup analyses for NAS, FAS and CM
Details of each subgroup analysis are provided in online supplementary tables S9–S11. For primary diagnoses of CM, we found significantly higher PPVs of CM in studies from inpatient settings (PPV=90.6%) compared with studies from emergency departments (EDs; PPV=80.8%) and in studies that applied a lower rated reference standard (89.4%; a rating <4) relative to a higher rated reference standard (70.8%; a rating ≥4). We found no significant differences when comparing subgroups by coding systems (ICD-9 vs ICD-10), age (younger vs older children) or publication year (p>0.179).
Intimate partner violence
Three studies assessed primary ICD diagnoses of IPV among women presenting to EDs (main age range: 12–55 years), with a pooled PPV of 86.1% (95% CI 72.2% to 93.6%). Individual PPVs from studies ranged from 73.6% to 94.4%. Two studies used the Flitcraft criteria as a reference standard (eg, prespecified IPV criteria) and included both violence by ex and current partners as cases. One study from Hong Kong included only IPV within cohabiting couples as cases and used medical chart reviews to verify that diagnoses matched any documented disclosure of IPV.115
We found 16 studies (10 in EDs/6 inpatient) that assessed four different injury-related presentations of IPV among predominantly women (primary age range: 12–55 years). The pooled PPVs were low, ranging from 31.6% (22.3%–42.7%) for assault-related codes to 3.3% (2.2%–5.0%) for orbital floor fractures. All studies used ICD-9 codes to identify presentations, except for one Finnish study that used ICD-10 codes.108 The between-study heterogeneity ranged from low to substantial across indicators (I 2 range=0.0%–99.4%). For assaults and facial fractures, meta-regressions showed that more recent studies were associated with a lower PPV of IPV (p<0.001). Three studies involved a small proportion of men (4%–17%),108 113 114 as estimates could not be separated from women. No study focused on pregnant or elderly women.
Coding errors for NAS, CM and IPV
The proportion of misclassifications (false positives) due to coding errors were on average 2.1% (95% CI 0.8% to 5.6%) across nine studies on NAS, CM, IPV and assaults (range I 2=97.3%–99.7%; online supplementary figure S20).
Documentation quality of assault indicators for IPV
We found that on average 28.0% (95% CI 14.7% to 46.8%; 18074/31224 charts; six studies) of assault coded cases among women had no recorded perpetrator information in the underlying medical charts (ie, missing data), preventing any classification/coding of IPV (online supplementary figure S21; table S5).
Sensitivity analyses
Serially excluding individual studies revealed that no study significantly impacted the between-study heterogeneity, and it remained substantial across all pooled PPVs (online supplementary tables S9-S10).
Publication bias
The funnel plot of studies reporting on the PPV for primary CM diagnoses was asymmetric (Egger’s test p=0.001, slope=0.999, rank correlation test: p=0.248; online supplementary figure S23), meaning that studies with higher PPVs were potentially more likely to be published. We found no evidence of funnel plot asymmetry for all other indicators with at least 10 or more studies (Egger’s test: p>0.366, rank correlation test: p>0.190; online supplementary figures S22-25).
Discussion
This is the largest meta-analysis to investigate the predictive value of indicators for family violence in EHRs, involving over 3.8 million individuals across 11 countries. Despite the large between-study heterogeneity, the results highlight that EHRs provide consistently high PPV for CM or IPV. We found that more than 8 in 10 coded primary diagnoses were confirmed as cases of NAS, CM and IPV. The findings also indicate that 8 in 10 recorded rib fractures and retinal haemorrhages met criteria for CM, and 1 in 3 assault-related presentations among women met criteria for IPV. Given the consistent recommendations for improved surveillance of violence,119 our findings underscore the utility of using commonly available coded medical data to evaluate services for at-risk groups across the life course. However, estimates varied depending on indicator and outcome, with substantial heterogeneity.
Compared with all other indicators of CM, FAS showed the lowest PPV. This most likely reflects the poor availability of specific ICD-9 codes for FAS, along with the complexity of the diagnosis. All included studies used the ICD-9 code ‘760.71’ focusing on fetuses being affected by alcohol without further description. Yet, the applied reference standard across studies required additional FAS criteria to be met, including facial anomalies and growth deficiencies.46–52 There is also an absence of FAS criteria that are widely recognised by clinicians,120 which may explain a higher underlying rate of misclassifications. Further studies on the accuracy of specific FAS codes using the ICD-10 are needed and may yield higher validity.
The high PPV of coded high-risk injuries of CM aligns with findings from previous reviews based on clinician diagnoses across paediatric healthcare settings. Compared with Kemp et al’s meta-analyses of 32 studies on fractures,29 our results showed higher PPVs for rib fractures (88.3% vs 70.9%) and similar estimates for lower limb fractures but lower estimates for skull (22.1% vs 30.1%) and upper limb fractures (38.5% vs 47.6%). Our PPV for retinal haemorrhages and burn injuries were also consistent with previous reviews of children across settings.121 122 While there are significant methodological differences between this study and previous work (eg, overall age criteria), the consistency between findings suggests that some coded injury patterns could be considered as a broader measure of CM in EHRs to aid identification of high-risk groups.
Coded injury patterns of IPV, such as orbital fractures, provided relatively low PPVs. This is not surprising as the PPV is related to the underlying prevalence of IPV. For example, most studies on IPV were conducted in large populations (eg, EDs) and investigated injury patterns applicable to a wide range of causes. Women are also known to under-report IPV because of safety reasons and stigma.123 124 The under-reporting is consistent with the findings that more than 1 in 4 pooled female assault coded records were missing perpetrator information in the underlying medical charts. Still, broader assault-related presentations and upper body contusions showed higher PPVs of IPV (>25%),125 and their utility in combination with other risk factors might yield comparable predictive accuracy in further studies.
Limitations
This review has important limitations. First, NAS and FAS are not always recognised as forms of prenatal neglect or CM, and the categorisation should be considered with caution to prevent stigma and barriers to help-seeking. Women who misuse substances may be unaware of their pregnancy, and opioids can be prescribed during pregnancy by clinicians for pain or opioid addiction treatment, increasing the risk of NAS.
Second, PPVs were analysed without accounting for study prevalences and within-study correlations of family violence.126 As a result, pooled estimates from studies with higher underlying prevalence estimates will generally lead to higher PPVs. However, we aimed to minimise variation of underlying prevalences by only including studies from general hospitals or paediatric settings.
Third, we were unable to obtain adequate data to reliably pool estimates on specificity and sensitivity. However, these absolute accuracy measures were not the focus of this review. The high volume of eligible patients presenting to healthcare combined with the rare occurrence and under-reporting of all outcomes limits the feasibility to apply a reference standard to non-coded cases to ascertain false negatives. Reliable measures on sensitivity are therefore unlikely to be obtained.
Fourth, the between-study heterogeneity of the pooled PPVs was substantial. As in most large meta-analyses, several factors not examined in the subgroup analyses may have influenced our results. Many estimates were ascertained from lower quality reference standards, prone to circularity bias (ie, using suspicion of CM as a reference standard in the absence of other explanations).127 Still, the consistency of studied ICD codes, combined with the larger samples and the high PPV across indicators, suggests that these estimates are valid and merit further study.
Finally, identifying CM and IPV in practice is complex. Obtaining information is a difficult task, as patients often under-report their experiences or symptoms, and high-risk groups such as infants cannot communicate. Similarly, some symptoms addressed by the reference standard (eg, linkage to social service assessments) may not have been conveyed to the clinician. EHRs may thus lead to potentially missed diagnoses or misclassifications. Estimates of indicators, therefore, reflect the ‘best data’ available and should be viewed in terms of routinely recorded indicators to help inform decisions about the likelihood of abuse, rather than definitive diagnoses.
Implications
More than a billion children and women aged 0–45 years globally reported being victims of abuse in 2014.128 129 Yet, in the UK, studies show that only about 1 in 3 violence-related ED visits for children and adults appear in police records, and self-report studies reveal that 1 in 5 affected women feel reluctant to report abuse to healthcare.3 130 131 In response to WHO’s priorities on addressing gaps in violence prevention, our findings highlight the potential to improve targeted care using routine EHRs to identify, prevent and support high-risk groups of family violence. On a service level, coded indicators of co-occurring family violence have the potential to be incorporated into computerised clinical decision support systems or risk prediction models to flag potential at-risk individuals.132 In the UK, linkage of family members EHRs could also allow for a ‘Think-Family’ approach, where indicators have the potential to identify vulnerable children through mothers or vice versa.133 Despite these potential implications, it remains unknown whether the benefits of using automated EHR systems to identify at-risk individuals outweigh potential harms including stigma, legal consequences, trust and reduced help-seeking.
Acknowledgments
First, we are very grateful to Dr Erin Shriver (University of Iowa Hospitals and Clinics), Professor John Leventhal (Yale School of Medicine), Dr Jennifer N. Lind (Centers for Disease Control and Prevention), Peggy Brozicevic (Vermont Department of Health), Luigi Garcia Saavedra (New Mexico Department of Health), Dr Jane Fornoff (Illinois Department of Public Health), Dr Ulf Höglund (Uppsala University), Björn Tingberg (Linköping University) and Dr Melissa O'Donnell (The University of Western Australia) for responding to additional data requests to complete our analyses. Second, this research benefits from and contributes to the National Institute for Health Research (NIHR) Children and Families Policy Research Unit but was not commissioned by the NIHR Policy Research Programme. The study also benefitted from funding for infrastructure through the NIHR GOSH Biomedical Research Centre and Health Data Research UK. Finally, we express our deepest appreciation to the children and families worldwide for their contribution and participation in interpersonal violence research.
Footnotes
Contributors: Concept: SS and RG. Design: SS. Drafting of the manuscript: SS, RA, RG and LL. Literature search and screening: SS, RA and MS. Acquisition, analysis or interpretation of data: all authors contributed equally. Statistical analysis: SS and LL. Critical revision of the manuscript for important intellectual content: all authors contributed equally. Study supervision: RG and LL.
Funding: The corresponding author had full access to all of the data and had final responsibility to submit for publication.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1. Gilbert R, Kemp A, Thoburn J, et al. Recognising and responding to child maltreatment. The Lancet 2009;373:167–80. 10.1016/S0140-6736(08)61707-9 [DOI] [PubMed] [Google Scholar]
- 2. Jenny C, Hymel KP, Ritzen A, et al. Analysis of missed cases of abusive head trauma. JAMA 1999;281:621–6. 10.1001/jama.281.7.621 [DOI] [PubMed] [Google Scholar]
- 3. Richardson J, Coid J, Petruckevitch A, et al. Identifying domestic violence: cross sectional study in primary care. BMJ 2002;324:274. 10.1136/bmj.324.7332.274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization Global plan of action to strengthen the role of the health system within a national multisectoral response to address interpersonal violence, in particular against women and girls, and against children. Geneva, Switzerland: WHO Document Production Services, 2016. [Google Scholar]
- 5. Mikton CR, Tanaka M, Tomlinson M, et al. Global research priorities for interpersonal violence prevention: a modified Delphi study. Bull World Health Organ 2017;95:36–48. 10.2471/BLT.16.172965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gilbert R, Widom CS, Browne K, et al. Burden and consequences of child maltreatment in high-income countries. The Lancet 2009;373:68–81. 10.1016/S0140-6736(08)61706-7 [DOI] [PubMed] [Google Scholar]
- 7. Krug EG, Mercy JA, Dahlberg LL, et al. The world report on violence and health. The Lancet 2002;360:1083–8. 10.1016/S0140-6736(02)11133-0 [DOI] [PubMed] [Google Scholar]
- 8. HM Goverment. DFE-00195-2018 Working Together to Safeguard Children. A guide to inter-agency working to safeguard and promote the welfare of children. Department for Education; 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/779401/Working_Together_to_Safeguard-Children.pdf [Accessed 20/07/2020]. [Google Scholar]
- 9. Rumball-Smith J, Fromkin J, Rosenthal B, et al. Implementation of routine electronic health record-based child abuse screening in general emergency departments. Child Abuse Negl 2018;85:58–67. 10.1016/j.chiabu.2018.08.008 [DOI] [PubMed] [Google Scholar]
- 10. James SL, Abate D, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. The Lancet 2018;392:1789–858. 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Woodman J, Simon A, Hauari H, et al. A scoping review of ‘think-family’ approaches in healthcare settings. J Public Health 2019;111 10.1093/pubmed/fdy210 [DOI] [PubMed] [Google Scholar]
- 12. Jha AK, DesRoches CM, Campbell EG, et al. Use of electronic health records in U.S. hospitals. N Engl J Med 2009;360:1628–38. 10.1056/NEJMsa0900592 [DOI] [PubMed] [Google Scholar]
- 13. Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med Overseas Ed 2010;363:501–4. 10.1056/NEJMp1006114 [DOI] [PubMed] [Google Scholar]
- 14. McKenzie K, Scott DA. Quantity of documentation of maltreatment risk factors in injury-related paediatric hospitalisations. BMC Public Health 2012;12:563 10.1186/1471-2458-12-563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Scott D, Tonmyr L, Fraser J, et al. The utility and challenges of using ICD codes in child maltreatment research: a review of existing literature. Child Abuse Negl 2009;33:791–808. 10.1016/j.chiabu.2009.08.005 [DOI] [PubMed] [Google Scholar]
- 16. Björkenstam C, Kosidou K, Björkenstam E. Childhood adversity and risk of suicide: cohort study of 548 721 adolescents and young adults in Sweden. BMJ 2017;357:j1334 10.1136/bmj.j1334 [DOI] [PubMed] [Google Scholar]
- 17. Chandan JS, Thomas T, Gokhale KM, et al. The burden of mental ill health associated with childhood maltreatment in the UK, using the health improvement network database: a population-based retrospective cohort study. Lancet Psychiatry 2019;6:926–34. 10.1016/S2215-0366(19)30369-4 [DOI] [PubMed] [Google Scholar]
- 18. Drinkwater J, Stanley N, Szilassy E, et al. Juggling confidentiality and safety: a qualitative study of how general practice clinicians document domestic violence in families with children. Br J Gen Pract 2017;67:e437–44. 10.3399/bjgp17X689353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Herman-Giddens ME, et al. Underascertainment of child abuse mortality in the United States. JAMA 1999;282:463–7. 10.1001/jama.282.5.463 [DOI] [PubMed] [Google Scholar]
- 20. Burns EM, Rigby E, Mamidanna R, et al. Systematic review of discharge coding accuracy. J Public Health 2012;34:138–48. 10.1093/pubmed/fdr054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McKenzie K, Scott DA, Waller GS, et al. Reliability of routinely collected hospital data for child maltreatment surveillance. BMC Public Health 2011;11:8. 10.1186/1471-2458-11-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McInnes MDF, Moher D, Thombs BD, et al. Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: the PRISMA-DTA statement. JAMA 2018;319:388–96. 10.1001/jama.2017.19163 [DOI] [PubMed] [Google Scholar]
- 23. Stroup DF, Berlin JA, Morton SC, et al. Meta-Analysis of observational studies in epidemiology: a proposal for reporting. Jama 2000;283:2008–12. [DOI] [PubMed] [Google Scholar]
- 24. Syed S, Ashwick R, Gonzalez-Izquierdo A, et al. Diagnostic accuracy of interpersonal violence and maltreatment in electronic health records: a systematic review and meta-analysis [CRD42019139300] 2019. [DOI] [PMC free article] [PubMed]
- 25. Covidence systematic review software [program]. Melbourne, Australia 2017.
- 26. Häyrinen K, Saranto K, NYKANEN P, Definition NP. Definition, structure, content, use and impacts of electronic health records: a review of the research literature. Int J Med Inform 2008;77:291–304. 10.1016/j.ijmedinf.2007.09.001 [DOI] [PubMed] [Google Scholar]
- 27. García-Moreno C, Jansen H, Ellsberg M, et al. WHO multi-country study on women’s health and domestic violence against women. 204 Geneva: World Health Organization, 2005: 1–18. [Google Scholar]
- 28. Whiting PF, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011;155:529–36. 10.7326/0003-4819-155-8-201110180-00009 [DOI] [PubMed] [Google Scholar]
- 29. Kemp AM, Dunstan F, Harrison S, et al. Patterns of skeletal fractures in child abuse: systematic review. BMJ 2008;337:a1518 10.1136/bmj.a1518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Carlin JB. Meta-Analysis for 2 X 2 tables: a Bayesian approach. Stat Med 1992;11:141–58. 10.1002/sim.4780110202 [DOI] [PubMed] [Google Scholar]
- 31. Stijnen T, Hamza TH, Özdemir P. Random effects meta-analysis of event outcome in the framework of the generalized linear mixed model with applications in sparse data. Stat Med 2010;29:3046–67. 10.1002/sim.4040 [DOI] [PubMed] [Google Scholar]
- 32. Borenstein M, Higgins JPT, Hedges LV, et al. Basics of meta-analysis: I2 is not an absolute measure of heterogeneity. Res Synth Methods 2017;8:5–18. 10.1002/jrsm.1230 [DOI] [PubMed] [Google Scholar]
- 33. Sterne JA, Egger M, Moher D. Addressing reporting biases. Cochrane handbook for systematic reviews of interventions: Cochrane book series, 2008: 297–333. [Google Scholar]
- 34. Team R Core R: a language and environment for statistical computing 2013.
- 35. Schwarzer G. Meta: an R package for meta-analysis. R news 2007;7:40–5. [Google Scholar]
- 36. Alsaleem M, Berkelhamer SK, Wilding GE, et al. Effects of partially hydrolyzed formula on severity and outcomes of neonatal abstinence syndrome. Am J Perinatol 2019. 10.1055/s-0039-1692684 [DOI] [PubMed] [Google Scholar]
- 37. Chisamore B, Labana S, Blitz S, et al. A comparison of morphine delivery in neonatal opioid withdrawal. Subst Abuse 2016;10:49-54. 10.4137/SART.S34550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Huybrechts KF, Bateman BT, Desai RJ, et al. Risk of neonatal drug withdrawal after intrauterine co-exposure to opioids and psychotropic medications: cohort study. BMJ 2017;358:j3326 10.1136/bmj.j3326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lind JN, Ailes EC, Alter CC, et al. Leveraging Existing Birth Defects Surveillance Infrastructure to Build Neonatal Abstinence Syndrome Surveillance Systems - Illinois, New Mexico, and Vermont, 2015-2016. MMWR Morb Mortal Wkly Rep 2019;68:177–80. 10.15585/mmwr.mm6807a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lind JN, Petersen EE, Lederer PA, et al. Infant and maternal characteristics in neonatal abstinence syndrome--selected hospitals in Florida, 2010-2011. MMWR Morb Mortal Wkly Rep 2015;64:213. [PMC free article] [PubMed] [Google Scholar]
- 41. Maalouf FI, Cooper WO, Stratton SM, et al. Positive predictive value of administrative data for neonatal abstinence syndrome. Pediatrics 2019;143:e20174183 10.1542/peds.2017-4183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Patrick SW, Dudley J, Martin PR, et al. Prescription opioid epidemic and infant outcomes. Pediatrics 2015;135:842–50. 10.1542/peds.2014-3299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Phillips-Bell GS, Holicky A, Lind JN, et al. Assessing the burden of neonatal abstinence syndrome: validation of: ICD-9-CM: data, Florida, 2010-2011. J Public Health Manag Pract 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Umer A, Loudin S, Maxwell S, et al. Capturing the statewide incidence of neonatal abstinence syndrome in real time: the West Virginia experience. Pediatr Res 2019;85:607–11. 10.1038/s41390-018-0172-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Yam P, Lok L, Eastwood J, et al. Validation of hospital discharge coding for neonatal abstinence syndrome. Acta Paediatr 2019;108:1786–92. 10.1111/apa.14803 [DOI] [PubMed] [Google Scholar]
- 46. Allen K, Riley M, Goldfeld S, et al. Estimating the prevalence of fetal alcohol syndrome in Victoria using routinely collected administrative data. Aust N Z J Public Health 2007;31:62–6. 10.1111/j.1753-6405.2007.00012.x [DOI] [PubMed] [Google Scholar]
- 47. Egeland GM, Perham-Hester KA, Gessner BD, et al. Fetal alcohol syndrome in Alaska, 1977 through 1992: an administrative prevalence derived from multiple data sources. Am J Public Health 1998;88:781–6. 10.2105/AJPH.88.5.781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Fox DJ, Druschel CM. Estimating prevalence of fetal alcohol syndrome (Fas): effectiveness of a passive birth defects registry system. Birth Defects Res A Clin Mol Teratol 2003;67:604–8. 10.1002/bdra.10108 [DOI] [PubMed] [Google Scholar]
- 49. Harris KR, Bucens IK. Prevalence of fetal alcohol syndrome in the top end of the Northern Territory. J Paediatr Child Health 2003;39:528–33. 10.1046/j.1440-1754.2003.00208.x [DOI] [PubMed] [Google Scholar]
- 50. Miller L, Tolliver R, Druschel C, et al. Fetal alcohol syndrome--Alaska, Arizona, Colorado, and New York, 1995-1997. MMWR Morb Mortal Wkly Rep 2002;51:433. [PubMed] [Google Scholar]
- 51. Miller LA, Shaikh T, Stanton C, et al. Surveillance for fetal alcohol syndrome in Colorado. Public Health Rep 1995;110:690. [PMC free article] [PubMed] [Google Scholar]
- 52. Welty T, Canfield L, Selva K, et al. Use of international classification of diseases coding to identify fetal alcohol syndrome--Indian Health Service facilities, 1981-1992. MMWR Morb Mortal Wkly Rep 1995;44:253. [PubMed] [Google Scholar]
- 53. Anderst JD. Assessment of factors resulting in abuse evaluations in young children with minor head trauma. Child Abuse Negl 2008;32:405–13. 10.1016/j.chiabu.2007.06.007 [DOI] [PubMed] [Google Scholar]
- 54. Baldwin K, Pandya NK, Wolfgruber H, et al. Femur fractures in the pediatric population: abuse or accidental trauma? Clinical Orthopaedics and Related Research® 2011;469:798–804. 10.1007/s11999-010-1339-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Berger RP, Parks S, Fromkin J, et al. Assessing the accuracy of the International classification of diseases codes to identify abusive head trauma: a feasibility study. Injury Prevention 2015;21:e133–7. 10.1136/injuryprev-2013-040924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Capra L, Levin AV, Howard A, et al. Characteristics of femur fractures in ambulatory young children. Emerg Med J 2013;30:749–53. 10.1136/emermed-2012-201547 [DOI] [PubMed] [Google Scholar]
- 57. Ettaro L, Berger RP, Songer T. Abusive head trauma in young children: characteristics and medical charges in a hospitalized population. Child Abuse Negl 2004;28:1099–111. 10.1016/j.chiabu.2004.06.006 [DOI] [PubMed] [Google Scholar]
- 58. Evasovich M, Klein R, Muakkassa F, et al. The economic effect of child abuse in the burn unit. Burns 1998;24:642–5. 10.1016/S0305-4179(98)00070-9 [DOI] [PubMed] [Google Scholar]
- 59. Garza HH. Diagnostic coding of physical abuse among patients evaluated by a multidisciplinary child protection team in a pediatric level I trauma center 2019.
- 60. Gessner BD, Moore M, Hamilton B, et al. The incidence of infant physical abuse in Alaska. Child Abuse Negl 2004;28:9–23. 10.1016/j.chiabu.2003.03.002 [DOI] [PubMed] [Google Scholar]
- 61. Gonzalez-Izquierdo A, Ward A, Smith P, et al. Notifications for child Safeguarding from an acute hospital in response to presentations to healthcare by parents. Child Care Health Dev 2015;41:186–93. 10.1111/cch.12134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Gumbs GR, Keenan HT, Sevick CJ, et al. Infant abusive head trauma in a military cohort. Pediatrics 2013;132:668–76. 10.1542/peds.2013-0168 [DOI] [PubMed] [Google Scholar]
- 63. Hansoti B, Beattie TF. Limb fractures and nonaccidental injury in children less than 24 months of age. Eur J Emerg Med 2008;15:63–6. 10.1097/MEJ.0b013e3282f08d1c [DOI] [PubMed] [Google Scholar]
- 64. Högberg U, Sennerstam R, Wester K, et al. Medical diagnoses among infants at entry in out-of-home care: a Swedish population-register study. Health Sci Rep 2019;2:e133 10.1002/hsr2.133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Hooft A, Ronda J, Schaeffer P, et al. Identification of physical abuse cases in hospitalized children: accuracy of international classification of diseases codes. J Pediatr 2013;162:80–5. 10.1016/j.jpeds.2012.06.037 [DOI] [PubMed] [Google Scholar]
- 66. Hooft AM, Asnes AG, Livingston N, et al. The accuracy of ICD codes: identifying physical abuse in 4 children's hospitals. Acad Pediatr 2015;15:444–50. 10.1016/j.acap.2015.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Hui C, Joughin E, Goldstein S, et al. Femoral fractures in children younger than three years: the role of nonaccidental injury. J Pediatr Orthop 2008;28:297–302. 10.1097/BPO.0b013e3181653bf9 [DOI] [PubMed] [Google Scholar]
- 68. Karatekin C, Almy B, Mason SM, et al. Health-Care utilization patterns of Maltreated youth. J Pediatr Psychol 2018;43:654–65. 10.1093/jpepsy/jsy004 [DOI] [PubMed] [Google Scholar]
- 69. Keenan HT, Marshall SW, Nocera MA, et al. Increased incidence of inflicted traumatic brain injury in children after a natural disaster. Am J Prev Med 2004;26:189–93. 10.1016/j.amepre.2003.10.023 [DOI] [PubMed] [Google Scholar]
- 70. Kim PT, McCagg J, Dundon A, et al. Consistent screening of admitted infants with head injuries reveals high rate of nonaccidental trauma. J Pediatr Surg 2017;52:1827–30. 10.1016/j.jpedsurg.2017.02.014 [DOI] [PubMed] [Google Scholar]
- 71. Krawiec C, Gerard S, Iriana S, et al. What we can learn from failure: an EHR-based child protection alert system. Child maltreatment 2019;1077559519848845. [DOI] [PubMed] [Google Scholar]
- 72. Lane WG, Rubin DM, Monteith R, et al. Racial differences in the evaluation of pediatric fractures for physical abuse. JAMA 2002;288:1603–9. 10.1001/jama.288.13.1603 [DOI] [PubMed] [Google Scholar]
- 73. Laskey AL, Stump TE, Hicks RA, et al. Yield of Skeletal Surveys in Children ≤18 Months of Age Presenting with Isolated Skull Fractures. J Pediatr 2013;162:86–9. 10.1016/j.jpeds.2012.06.038 [DOI] [PubMed] [Google Scholar]
- 74. Lavin LR, Penrod CH, Estrada CM, et al. Fractures in the pediatric emergency department: are we considering abuse? Clin Pediatr 2018;57:1161–7. 10.1177/0009922818759319 [DOI] [PubMed] [Google Scholar]
- 75. Lyons TW, Stack AM, Monuteaux MC, et al. A Qi initiative to reduce hospitalization for children with isolated skull fractures. Pediatrics 2016;137:e20153370 10.1542/peds.2015-3370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Myhre MC, Grøgaard JB, Dyb GA, et al. Traumatic head injury in infants and toddlers. Acta Paediatr 2007;96:1159–63. 10.1111/j.1651-2227.2007.00356.x [DOI] [PubMed] [Google Scholar]
- 77. O'Donnell M, Nassar N, Jacoby P, et al. Western Australian emergency department presentations related to child maltreatment and intentional injury: population level study utilising linked health and child protection data. J Paediatr Child Health 2012;48:57–65. 10.1111/j.1440-1754.2011.02189.x [DOI] [PubMed] [Google Scholar]
- 78. O'Donnell M, Nassar N, Leonard H, et al. Rates and types of hospitalisations for children who have subsequent contact with the child protection system: a population based case-control study. J Epidemiol Community Health 2010;64:784–8. 10.1136/jech.2009.093393 [DOI] [PubMed] [Google Scholar]
- 79. Paroskie A, Carpenter SL, Lowen DE, et al. A two-center retrospective review of the hematologic evaluation and laboratory abnormalities in suspected victims of non-accidental injury. Child Abuse Negl 2014;38:1794–800. 10.1016/j.chiabu.2014.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Parrish J, Baldwin-Johnson C, Volz M, et al. Abusive head trauma among children in Alaska: a population-based assessment. Int J Circumpolar Health 2013;72:21216. 10.3402/ijch.v72i0.21216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Payne BS, Kutz TJ, Di Maio A, et al. Prevalence of retinal hemorrhages in infants presenting with isolated long bone fractures and evaluation for abuse. J Emerg Med 2016;51:365–9. 10.1016/j.jemermed.2016.05.043 [DOI] [PubMed] [Google Scholar]
- 82. Raghavan R, Brown DS, Allaire BT, et al. Challenges in using Medicaid claims to ascertain child maltreatment. Child Maltreat 2015;20:83–91. 10.1177/1077559514548316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Rangel EL, Cook BS, Bennett BL, et al. Eliminating disparity in evaluation for abuse in infants with head injury: use of a screening guideline. J Pediatr Surg 2009;44:1229–35. 10.1016/j.jpedsurg.2009.02.044 [DOI] [PubMed] [Google Scholar]
- 84. Ricci L, Giantris A, Merriam P, et al. Abusive head trauma in Maine infants: medical, child protective, and law enforcement analysis. Child Abuse Negl 2003;27:271–83. 10.1016/S0145-2134(03)00006-1 [DOI] [PubMed] [Google Scholar]
- 85. Risen SR, Suskauer SJ, Dematt EJ, et al. Functional outcomes in children with abusive head trauma receiving inpatient rehabilitation compared with children with nonabusive head trauma. J Pediatr 2014;164:613–9. 10.1016/j.jpeds.2013.10.075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Ryznar E, Rosado N, Flaherty EG. Understanding forearm fractures in young children: abuse or not abuse? Child Abuse Negl 2015;47:132–9. 10.1016/j.chiabu.2015.02.008 [DOI] [PubMed] [Google Scholar]
- 87. Schnitzer PG, Slusher P, Van Tuinen M. Child maltreatment in Missouri: combining data for public health surveillance. Am J Prev Med 2004;27:379–84. 10.1016/j.amepre.2004.08.007 [DOI] [PubMed] [Google Scholar]
- 88. Schnitzer PG, Slusher PL, Kruse RL, et al. Identification of ICD codes suggestive of child maltreatment. Child Abuse Negl 2011;35:3–17. 10.1016/j.chiabu.2010.06.008 [DOI] [PubMed] [Google Scholar]
- 89. Sharkey MS, Buesser KE, Gaither JR, et al. Abusive fracture incidence over three decades at a level 1 pediatric trauma center. Child Abuse Negl 2018;76:364–71. 10.1016/j.chiabu.2017.11.008 [DOI] [PubMed] [Google Scholar]
- 90. Somji Z, Plint A, McGahern C, et al. Diagnostic coding of abuse related fractures at two children's emergency departments. Child Abuse Negl 2011;35:905–14. 10.1016/j.chiabu.2011.05.016 [DOI] [PubMed] [Google Scholar]
- 91. Strait RT, Siegel RM, Shapiro RA. Humeral fractures without obvious etiologies in children less than 3 years of age: when is it abuse? Pediatrics 1995;96:667–71. [PubMed] [Google Scholar]
- 92. Thyen U, Leventhal JM, Yazdgerdi SR, et al. Concerns about child maltreatment in hospitalized children. Child Abuse Negl 1997;21:187–98. 10.1016/S0145-2134(96)00144-5 [DOI] [PubMed] [Google Scholar]
- 93. Tingberg B. Child abuse-clinical investigation, management and nursing approach 2010.
- 94. Tzioumi D, Oates RK. Subdural hematomas in children under 2 years. accidental or inflicted? A 10-year experience. Child Abuse Negl 1998;22:1105–12. 10.1016/S0145-2134(98)00093-3 [DOI] [PubMed] [Google Scholar]
- 95. Wood JN, Christian CW, Adams CM, et al. Skeletal surveys in infants with isolated skull fractures. Pediatrics 2009;123:e247–52. 10.1542/peds.2008-2467 [DOI] [PubMed] [Google Scholar]
- 96. M-F W, T-H L, Lin C-J, et al. Risk factors and physical signs of child abuse in hospitalized children in Taiwan. Children and Youth Services Review 2015;58:137–41. [Google Scholar]
- 97. Durand MB, McLaughlin CM, Imagawa KK, et al. Identifying targets to improve coding of child physical abuse at a pediatric trauma center. Journal of Trauma Nursing 2019;26:239–42. 10.1097/JTN.0000000000000461 [DOI] [PubMed] [Google Scholar]
- 98. Wood JN, Pecker LH, Russo ME, et al. Evaluation and referral for child maltreatment in pediatric poisoning victims. Child Abuse Negl 2012;36:362–9. 10.1016/j.chiabu.2012.01.001 [DOI] [PubMed] [Google Scholar]
- 99. Arosarena OA, Fritsch TA, Hsueh Y, et al. Maxillofacial injuries and violence against women. Arch Facial Plast Surg 2009;11:48–52. 10.1001/archfacial.2008.507 [DOI] [PubMed] [Google Scholar]
- 100. Biroscak BJ, Smith PK, Roznowski H, et al. Intimate partner violence against women: findings from one state's ED surveillance system. J Emerg Nurs 2006;32:12–16. 10.1016/j.jen.2005.11.002 [DOI] [PubMed] [Google Scholar]
- 101. Bonomi AE, et al. Medical and psychosocial diagnoses in women with a history of intimate partner violence. Arch Intern Med 2009;169:1692–7. 10.1001/archinternmed.2009.292 [DOI] [PubMed] [Google Scholar]
- 102. Brown S, Malcoe L, Carson E, et al. Intimate partner violence injuries--Oklahoma, 2002. MMWR Morb Mortal Wkly Rep 2005;54:1041–5. [PubMed] [Google Scholar]
- 103. Clark TJ, Renner LM, Sobel RK, et al. Intimate partner violence: an underappreciated etiology of orbital floor fractures. Ophthalmic Plast Reconstr Surg 2014;30:508–11. 10.1097/IOP.0000000000000165 [DOI] [PubMed] [Google Scholar]
- 104. Cohen AR, Clark TJE, Renner LM, et al. Intimate partner violence as a mechanism of traumatic ocular injury in women. Can J Ophthalmol 2019;54:355–8. 10.1016/j.jcjo.2018.05.017 [DOI] [PubMed] [Google Scholar]
- 105. Fanslow JL, Norton RN, Spinola CG. Indicators of assault-related injuries among women presenting to the emergency department. Ann Emerg Med 1998;32:341–8. 10.1016/S0196-0644(98)70011-3 [DOI] [PubMed] [Google Scholar]
- 106. Goldberg SH, McRill CM, Bruno CR, et al. Orbital fractures due to domestic violence: an epidemiologic study. Orbit 2000;19:143–54. 10.1076/orbi.19.3.143.2659 [DOI] [PubMed] [Google Scholar]
- 107. Kernic MA, Wolf ME, Holt VL. Rates and relative risk of hospital admission among women in violent intimate partner relationships. Am J Public Health 2000;90:1416. 10.2105/ajph.90.9.1416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Kivelä S, Leppäkoski T, Ruohoniemi J, et al. The documentation and characteristics of hospitalized IPV patients using electronic medical records data: a follow-up descriptive study. J Fam Violence 2019;34:611–9. 10.1007/s10896-019-00081-z [DOI] [Google Scholar]
- 109. Lipsky S, Caetano R, Roy-Byrne P. Racial and ethnic disparities in police-reported intimate partner violence and risk of hospitalization among women. Women's Health Issues 2009;19:109–18. 10.1016/j.whi.2008.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Muelleman RL, Lenaghan PA, Pakieser RA. Battered women: injury locations and types. Ann Emerg Med 1996;28:486–92. 10.1016/S0196-0644(96)70110-5 [DOI] [PubMed] [Google Scholar]
- 111. Muelleman RL, Liewer JD. How often do women in the emergency department without intimate violence injuries return with such injuries? Acad Emerg Med 1998;5:982–5. 10.1111/j.1553-2712.1998.tb02775.x [DOI] [PubMed] [Google Scholar]
- 112. Ranney ML, Mello MJ. A comparison of female and male adolescent victims of violence seen in the emergency department. J Emerg Med 2011;41:701–6. 10.1016/j.jemermed.2011.03.025 [DOI] [PubMed] [Google Scholar]
- 113. Saltzman LE, Mahendra RR, Ikeda RM, et al. Utility of hospital emergency department data for studying intimate partner violence. J Marriage Fam 2005;67:960–70. 10.1111/j.1741-3737.2005.00187.x [DOI] [Google Scholar]
- 114. Schafer SD, Drach LL, Hedberg K, et al. Using diagnostic codes to screen for intimate partner violence in Oregon emergency departments and hospitals. Public Health Rep 2008;123:628–35. 10.1177/003335490812300513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Wong JY-H, Choi AW-M, Fong DY-T, et al. A comparison of intimate partner violence and associated physical injuries between cohabitating and married women: a 5-year medical chart review. BMC Public Health 2016;16:1207. 10.1186/s12889-016-3879-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Yau RK, Stayton CD, Davidson LL. Indicators of intimate partner violence: identification in emergency departments. J Emerg Med 2013;45:441–9. 10.1016/j.jemermed.2013.05.005 [DOI] [PubMed] [Google Scholar]
- 117. Yang W, Huang J. Chronic subdural hematoma: epidemiology and natural history. Neurosurg Clin N Am 2017;28:205–10. 10.1016/j.nec.2016.11.002 [DOI] [PubMed] [Google Scholar]
- 118. Finnegan LP, Connaughton JF, Kron RE, et al. Neonatal abstinence syndrome: assessment and management. Addict Dis 1975;2:141–58. [PubMed] [Google Scholar]
- 119. Butchart A, Mikton C, Krug E. Governments must do more to address interpersonal violence. The Lancet 2014;384:2183–5. 10.1016/S0140-6736(14)62124-3 [DOI] [PubMed] [Google Scholar]
- 120. Coles CD, Gailey AR, Mulle JG, et al. A comparison among 5 methods for the clinical diagnosis of fetal alcohol spectrum disorders. Alcohol Clin Exp Res 2016;40:1000–9. 10.1111/acer.13032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Maguire SA, Watts PO, Shaw AD, et al. Retinal haemorrhages and related findings in abusive and non-abusive head trauma: a systematic review. Eye 2013;27:28–36. 10.1038/eye.2012.213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Maguire S, Moynihan S, Mann M, et al. A systematic review of the features that indicate intentional scalds in children. Burns 2008;34:1072–81. 10.1016/j.burns.2008.02.011 [DOI] [PubMed] [Google Scholar]
- 123. Tjaden PG, Thoennes N. Full report of the prevalence, incidence, and consequences of violence against women: findings from the National violence against women survey: US department of justice, office of justice programs. National Institute of Justice 2000. [Google Scholar]
- 124. Feder GS, Hutson M, Ramsay J, et al. Women exposed to intimate partner violence: expectations and experiences when they encounter health care professionals: a meta-analysis of qualitative studies. Arch Intern Med 2006;166:22–37. 10.1001/archinte.166.1.22 [DOI] [PubMed] [Google Scholar]
- 125. Wu V, Huff H, Bhandari M. Pattern of physical injury associated with intimate partner violence in women presenting to the emergency department: a systematic review and meta-analysis. Trauma Violence Abuse 2010;11:71–82. 10.1177/1524838010367503 [DOI] [PubMed] [Google Scholar]
- 126. Riley RD, Jackson D, Salanti G, et al. Multivariate and network meta-analysis of multiple outcomes and multiple treatments: rationale, concepts, and examples. BMJ 2017;358:j3932. 10.1136/bmj.j3932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Colville-Ebeling B, et al. Circularity bias in abusive head trauma studies could be diminished with a new ranking scale. Egypt J Forensic Sci 2016;6:6–10. [Google Scholar]
- 128. Hillis S, Mercy J, Amobi A, et al. Global prevalence of past-year violence against children: a systematic review and minimum estimates. Pediatrics 2016;137:e20154079. 10.1542/peds.2015-4079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Organization WH Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. World Health Organization, 2013. [Google Scholar]
- 130. Sutherland I, Sivarajasingam V, Shepherd JP. Recording of community violence by medical and police services. Inj Prev 2002;8:246–7. 10.1136/ip.8.3.246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. MacMillan HL, Wathen CN, Jamieson E, et al. Approaches to screening for intimate partner violence in health care settings: a randomized trial. JAMA 2006;296:530–6. 10.1001/jama.296.5.530 [DOI] [PubMed] [Google Scholar]
- 132. Suresh S, Saladino RA, Fromkin J, et al. Integration of physical abuse clinical decision support into the electronic health record at a tertiary care children's Hospital. J Am Med Inform Assoc 2018;25:833–40. 10.1093/jamia/ocy025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Excellence SCIf Think child, think parent. Think Family: Social Care Institute for Excellence 2009. [Google Scholar]
- 134. McCormick N, Lacaille D, Bhole V, et al. Validity of myocardial infarction diagnoses in administrative databases: a systematic review. PLoS One 2014;9:e92286. 10.1371/journal.pone.0092286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Hudak ML, Tan RC, et al. , COMMITTEE ON DRUGS . Neonatal drug withdrawal. Pediatrics 2012;129:e540–60. 10.1542/peds.2011-3212 [DOI] [PubMed] [Google Scholar]
- 136. Chudley AE, Conry J, Cook JL, et al. Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. CMAJ 2005;172:S1–21. 10.1503/cmaj.1040302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Parks SE, Annest JL, Hill HA, et al. Pediatric abusive head trauma: recommended definitions for public health surveillance and research 2012.
- 138. Berger RP, Parks S, Fromkin J, et al. Assessing the accuracy of the International classification of diseases codes to identify abusive head trauma: a feasibility study. Inj Prev 2015;21:e133–7. 10.1136/injuryprev-2013-040924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Faul M, Xu L, Wald MM, et al. Traumatic brain injury in the United States: national estimates of prevalence and incidence, 2002-2006. Injury Prevention 2010;16:A268 10.1136/ip.2010.029215.951 [DOI] [Google Scholar]
- 140. Breiding M, Basile KC, Smith SG, et al. Intimate partner violence surveillance: uniform definitions and recommended data elements. version 2.0 2015.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
archdischild-2020-319027supp001.pdf (922.6KB, pdf)