Abstract
Background
The rapidly growing pandemic of coronavirus disease 2019 (COVID-19) has challenged health systems globally. Here we report the first identified infections of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; aetiology of COVID-19) among recent international arrivals to Sudan and their contacts.
Methods
Suspected cases were identified clinically and/or epidemiologically. Samples from suspected cases and their contacts were tested in the National Influenza Centre following World Health Organization protocols. Two real-time reverse transcription quantitative polymerase chain reaction assays were used to detect and confirm SARS-CoV-2 infection.
Results
Seven cases of COVID-19, including two deaths, were confirmed in Sudan between 27 February and 30 March 2020. Suspected cases were identified and tested. As of 30 March, no local transmission was yet reported in the country. Fifty-nine percent of the suspected cases were international travellers coming from areas with current COVID-19 epidemics. Cough and fever were the major symptoms, presented by 65% and 60% of the suspected cases, respectively. By early April, an additional seven cases were confirmed through limited contact tracing that identified the first locally acquired infections in recent contact with imported cases.
Conclusions
The high mortality rate of COVID-19 cases in Sudan might be due to limitations in test and trace and case management services. Unfortunately, infections have spread further into other states and the country has no capacity for mass community screening to better estimate disease prevalence. Therefore external support is urgently needed to improve the healthcare and surveillance systems.
Keywords: coronavirus disease 2019, COVID-19, imported cases, pandemic, SARS-CoV-2, Sudan
Introduction
The coronavirus disease 2019 (COVID-19) pandemic initially emerged in China in December 2019 and quickly spread internationally. The aetiological virus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first isolated from patients with pneumonia of unknown cause. After the virus isolation and characterization using sequencing and transmission electron microscopy, the virus was classified as the seventh member of the coronavirus family that infects humans.1 Initial investigation of the disease has established an association between severe SARS-CoV-2 infection in elderly people and those with pre-existing health conditions, including diabetes, hypertension and cardiovascular diseases. The clinical manifestation of the disease is mainly pneumonia-like signs and symptoms for severe cases, but most patients display fever, cough and myalgia or fatigue.2
Within 3 weeks of the first recognized case on 10 December 2019 in Wuhan, Hubei Province, China, 47 cases of COVID-19 were confirmed in the area and an outbreak was officially declared.3 With cases imported into several countries and local transmission and epidemics growing rapidly, the World Health Organization (WHO) declared COVID-19 a Public Health Emergency of International Concern on 30 January 2020.4,5 The disease was rapidly spreading in China, due in part to uncertainties about modes of transmission, epidemiology and preventive and control measures. By 11 February 2020, 44 672 cases were confirmed in the Wuhan area.6
The COVID-19 pandemic is challenging health systems throughout the world, including well-established ones in wealthy countries, with nearly 27 million cases and >880 000 fatalities worldwide reported by the WHO in the first week of September 2020 from around 200 countries and territories.5 The majority of these cases and deaths are from countries with relatively developed health systems, including China, Italy, Germany, Spain, the UK and the USA.5 Health systems in Africa are typically very weak, underresourced, poorly equipped and constantly struggling with epidemics of several other infectious diseases.7 The health system in Sudan is limited8 and suffers a heavy burden of infectious diseases, including parasitic diseases like malaria, leishmaniasis9 and onchocerciasis,10 and arboviral diseases like Chikungunya virus,11 dengue and rift valley fever,12,13 and their frequent epidemics.14,15 However, with emergency support from the WHO, the capacity of several African countries, including Sudan, to identify, test and isolate COVID-19 cases was somewhat improved.7
In this report we document the first imported cases of COVID-19 in Sudan and describe the epidemiology, epidemic preparedness and public health response in the country.
Materials and methods
This is a cross-sectional descriptive study implemented in Sudan to investigate the importation of SARS-CoV-2 infections and the establishment of the COVID-19 pandemic in the country through international travellers and their contacts between 16 January and 15 April 2020.
Establishing active surveillance
In response to the rapidly growing pandemic of COVID-19, governments worldwide, including Sudan, are struggling to utilize their resources effectively to detect and contain its spread. In Sudan, a federal task force has been assembled to investigate, identify and isolate suspected cases and to provide healthcare to confirmed cases (suspected cases with a positive laboratory test).
Identifying suspected cases
Suspected cases were identified according to their clinical presentations and/or epidemiological history (recently visiting epidemic countries and/or having recent contact with suspected or confirmed cases).
Sample collection
Following the identification of suspected cases, nasopharyngeal swab (NPS) samples were collected, preserved in virus transport medium (VTM) and transported to a laboratory according to the WHO guidelines.
RNA extraction
Total RNA was extracted using the QIAamp viral RNA mini kit (Qiagen, Düsseldorf, Germany) according to the manufacturer's instructions.
Molecular tests
Laboratory tests were carried out by a team from the National Influenza Centre (NIC), National Public Health Laboratory. Two consecutive real-time polymerase chain reaction (PCR) assays were used; samples were initially screened with LightMix SarbecoV E-gene plus Equine Arteritis Virus (EAV) (TIB MOLBIOL, Berlin, Germany) that detects sarbecovirus (SARS-CoV and SARS-Cov-2). Positive samples were then confirmed by the LightMix Modular COVID-19 RNA-dependent RNA polymerase (RdRP) gene that detects SARS-Cov-2 only. The samples were also assayed using a detection kit for 2019 novel coronavirus (2019-nCoV) RNA (PCR-fluorescence probing), targeting the N and ORF1b genes.
Results
Identification of suspected cases
On 27 January 2020, the first suspected cases were initially identified and samples were taken. Symptomatic suspected cases were isolated and quarantined in Gabra Hospital, one of the three health facilities designated as the Khartoum Isolation Centre. Demographics of the suspected cases showed that the majority (60%) were young adults 17–37 y of age and only 17% were ≥59 y of age. Males comprised 75% of the suspected cases (Table 1).
Table 1.
Demographics of the suspected cases.
| Occupation | |||||||
|---|---|---|---|---|---|---|---|
| Age group | Male : female | Student | Healthcare provider | Worker | Other | Total | Percentage |
| 17–37 | 3:1 | 33 | 12 | 19 | 26 | 90 | 60 |
| 38–58 | 4:1 | 1 | 2 | 11 | 21 | 35 | 23 |
| 59–72 | 1:1 | – | 1 | 3 | 21 | 25 | 17 |
| Total | 3:1 | 34 | 15 | 33 | 68 | 150 | 100 |
By 30 March, 150 suspected cases were identified and isolated; symptomatic cases were isolated in the governmental isolation centre, while asymptomatic cases were advised to self-isolate in their residences with frequent follow-up calls from the Ministry of Health response team. Based on the travel history to a country with a developing epidemic of COVID-19, contact with suspected cases and presenting symptoms, 150 suspected cases were identified and laboratory tested (Table 2) and NPS samples were taken (Fig. 1).
Table 2.
Representative reasons for selecting the suspected cases to be investigated.
| Potentiality of suspected cases | Number |
|---|---|
| Symptomatic international traveller | 71 |
| Asymptomatic international traveller | 18 |
| Symptomatic companion of suspected case | 40 |
| Asymptomatic companion of suspected case | 21 |
| Suspected cases identified and laboratory tested | 150 |
| Laboratory-confirmed cases among travellers, including two deaths | 7 |
| Laboratory-confirmed cases among non-travellers (locally acquired) | 7 |
Figure 1.
Epicurve shows the suspected and confirmed cases of COVID-19 in Sudan in 2020.
Clinical presentations of suspected cases
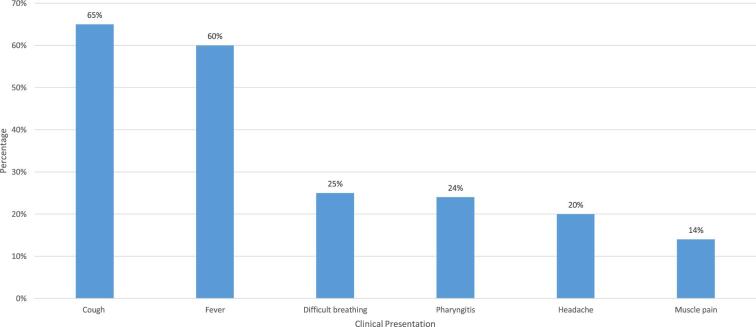
Most of the suspected cases (65%) presented with cough and 60% displayed fever. Difficulty breathing, pharyngitis and headache were experienced by 25%, 24% and 20%, respectively. However, 26% of the suspected cases were asymptomatic but were selected because of their epidemiological risk (Fig. 2).
Figure 2.
The main clinical manifestations of the symptomatic cases.
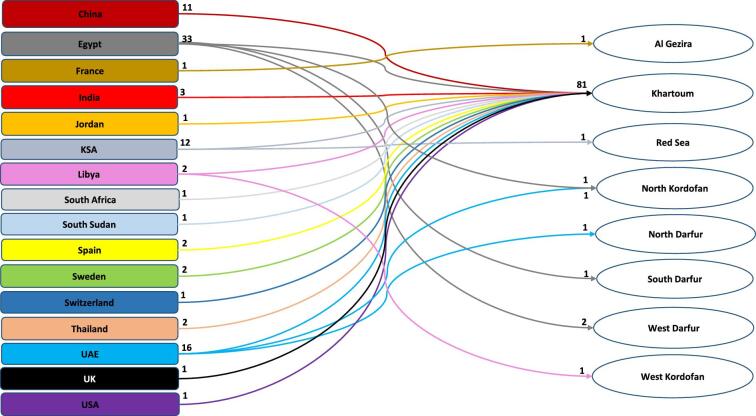
Travel and contact history of the suspected cases
The majority of the suspected cases (59%) were international travellers; most came from Egypt (37%), the United Arab Emirates (UAE; 18%), Saudi Arabia (14%) and China (12%) (Fig. 3). Regardless of their country of travel origination or port of entry into Sudan, the majority (90%) were staying in Khartoum. However, some may have visited more than a single state. An additional 39 asymptomatic but suspected cases were identified from the contacts and companions of the original suspected and confirmed cases and they were advised to self-isolate at home and were closely monitored for clinical signs and symptoms even though they tested negative for COVID-19. In total, we traced and tested 60 individuals who have been in contact with the seven confirmed cases. Only seven of them tested positive for SARS-CoV-2 and all recovered and were released from isolation after the WHO-recommended quarantine period of 14 d. Limited information was available about these contacts.
Figure 3.
The countries from where suspected cases with an international travel history arrived and the states where they were staying in Sudan.
Characteristics and disease outcome among confirmed cases
All of the laboratory-confirmed imported cases of COVID-19 in Sudan so far have been males. The first case was a 50-year-old who arrived in the country on 2 March, coming from the UAE. He experienced cough, fever, headache and difficulty breathing. In <2 weeks, the second case, a 47-year-old, arrived from Spain displaying fever, cough, headache, pharyngitis and difficulty breathing. Soon thereafter, the third and fourth cases, ages 39 and 29 y, arrived from the UAE and presented with cough and fever. Additionally, the third case had headache, muscle pain and diarrhoea. The fifth and sixth cases were 67 and 59 y old, coming from France and the UAE, respectively, and both presented with cough, fever and difficulty breathing. The seventh case was a 65-year-old who arrived from South Africa and was suffering from fever only (Table 3). Unfortunately, the first and sixth cases died due to COVID-19 complications, representing the first two deaths from this disease in Sudan and highlighting the high mortality rate (29%). The other five patients recovered (Table 3).
Table 3.
Characteristics of the COVID-19 confirmed cases.
| Case | Date arrived in Sudan | Coming from | Sex | Age | Symptoms | Clinical outcome |
|---|---|---|---|---|---|---|
| 1 | 2 March 2020 | UAE | Male | 50 | Cough, fever, headache, difficulty breathing | Died |
| 2 | 15 March 2020 | Spain | Male | 47 | Cough, fever, headache, pharyngitis, difficulty breathing | Recovered |
| 3 | 20 March 2020 | UAE | Male | 39 | Cough, fever | Recovered |
| 4 | 21 March 2020 | UAE | Male | 29 | Cough, fever, headache, muscle pain, diarrhoea | Recovered |
| 5 | 21 March 2020 | France | Male | 67 | Cough, fever, headache, muscle pain, difficulty breathing, diarrhoea | Recovered |
| 6 | 19 March 2020 | UAE | Male | 59 | Cough, fever, difficulty breathing | Died |
| 7 | 13 March 2020 | South Africa | Male | 65 | Cough, fever, difficulty breathing | Recovered |
Health system preparedness and capacity
All laboratory-confirmed imported cases who developed COVID-19 were quarantined and received care as needed in the intensive care unit (ICU) of Gabra Hospital for Emergencies in South Khartoum. The quarantine centre is currently composed of three hospitals: Gabra Hospital, with a capacity of 110 beds, including 20 in the ICU; Khartoum Hospital, with a capacity of 106 beds, including 24 ICU beds; and Universal Hospital, with a capacity of 500 beds, including 54 ICU beds. Thus the total capacity for isolation of COVID-19 patients is 716 beds and 98 ICU beds in the Khartoum Isolation Center. In addition to the central isolation centre in Khartoum State, the Sudan Ministry of Health has established an additional five isolation centres to serve other remote regions and entry points into the country. However, these isolation centres have very limited capacities, including 88 beds in Gazira State to serve the southern region, 50 beds in North Kordofan State to support the south-central region, 20 beds in Red Sea State in the east, 10 beds in West Darfur to serve the western region and only 8 beds in River Nile State to support the northern region of the country.
Discussion
Here we report the first 7 laboratory-confirmed imported cases of COVID-19 in Sudan, including 2 deaths among 150 suspected and tested international travellers who arrived in country between 16 January and 30 March. Epidemiological investigations have shown that the first seven locally acquired infections were in recent contact with one or more of the confirmed imported cases of COVID-19. Some of the first locally acquired infections were reported among local healthcare providers without a history of travel but working in facilities that treated one or more of these imported cases. Because of the limited health system in Sudan,8 the country is at high risk of a devastating epidemic. This risk is predicted to be intensified by the lack of data and information sharing in a timely manner, particularly during health emergencies.16,17 Additionally, the Sudanese population was desensitized about the risk of COVID-19 by the statement of the former Minister of Health, ‘We managed to get rid of Omar al-Bashir. How come we cannot get hold of this tiny coronavirus?’, which might have given the wrong impression that the COVID-19 pandemic could be easily managed in Sudan.18 However, the NIC is working in coordination with the WHO country office to routinely update the number of COVID-19 cases and deaths. Interestingly, Sudan was free from the disease up to 2 March and even afterwards experienced a remarkably small number of imported COVID-19 cases. However, this could reflect the limited surveillance system, with additional cases being unidentified.19 The severe clinical presentation of the cases we confirmed suggests that late diagnoses occur because patients ignore their early, mild symptoms.20 Although few patients in our study complained about diarrhoea, this sign should not be eliminated from consideration during the initial case screening at health facilities.21
Sudan's national lockdown (international travel restriction) decision to limit the importation of cases was taken relatively late on 16 March. However, the majority of cases (57%) arrived during the period when the Khartoum International Airport was reopened between the 19 and 21 March to allow Sudanese citizens traveling abroad to return. Unfortunately this was done without adequate preparation and resources to screen all arrivals for signs and symptoms of SARS-CoV-2 infection and to test them to confirm a lack of infection before allowing them into the general, susceptible population. The risk of more imported cases has been reduced by the government's emergency declaration and restrictions on all international travel involving the closure of all air, ground and sea entry points. Changes in control strategies and delays in decision making in other countries such as the USA has led to explosive epidemics including large numbers of cases and deaths.22 The COVID-19 outbreak has grown exponentially from a single case on 19 January to >27 million cases and >880 000 fatalities worldwide by the first week of September 2020.5,20
Unfortunately, several travellers bypassed clinical screening at the Khartoum International Airport when it was reopened to allow Sudanese travellers to return. Those travellers may have ignored the health screening process at ports of entry because they had no health complaints. Nevertheless, they risked their own health, as well as the establishment of local transmission.23 Regrettably, the Sudan health system is very limited, with poor capacity to provide intensive healthcare. Ministry of Health COVID-19 preparedness and response reports show that the country has only 296 ICU beds throughout the country. Therefore, with the establishment of local transmission, the consequences of caring for severely ill COVID-19 patients could be dire.24 This was highlighted by a WHO report that Sudan is currently ranked the 14th country in Africa based on the number of confirmed cases (13 189), but 7th based on COVID-19 deaths (823).5
In addition, diagnostic capacity for detecting SARS-CoV-2 infections in the country is very limited and is offered only by the NIC, which has extremely limited resources and qualified personnel. However, with support from the WHO, other regional diagnostic centres were established in the Red Sea, Gazira and South Darfur States following intensive training in the NIC. The Ministry of Health is advising people to stay home and is working to raise awareness about SARS-CoV-2 transmission and personal protective measures, including social distancing. Apparently these preventive guidelines are being challenged by some local societal traditions and norms, which resulted from years of neglect regarding health education. In addition, most of Sudanese society cannot adhere to the preventive measures, particularly to stay home, because of their limited financial resources.10 Additional risk is resulting from the abundance of locally displaced persons, refugees and poor people in general.12,14,15 These people rely heavily on daily work to secure their needs of food and other essentials.10 Furthermore, they have poor sanitation and personal hygiene, further increasing their risk of COVID-19.8,17 Nonetheless, the Sudanese government advised residents of Khartoum State to secure their essential needs before the implementation of a 24-h lockdown order issued starting on 18 April. This has now been changed to a 12-h curfew between 06:00 and 18:00 h daily.25
Our study was limited by the lack of sequencing services in Sudan and the restriction of international flights in and out of the country. Therefore we could not fully characterize SARS-CoV-2 samples. The Ministry of Health needs to establish critical diagnostic capabilities locally to generate more robust data for healthcare and research.13
Conclusions
The risk of COVID-19 in Sudan was limited following the initial lockdown of the Khartoum International Airport. However, this risk was significantly increased by the decision to reopen the airport without preparing and applying strict preventive measures and without resources to identify and test all the suspected cases arriving from high-risk areas. Because the country has inadequate resources to contain a local epidemic and a fragile health system, the risk of a major epidemic remains high despite the small number of COVID-19 cases (seven) and deaths (two) initially reported. The high initial mortality rate (29%) suggests a delay or lack of identification of cases, potentially reducing the effectiveness of available healthcare. The limited resources of the country, weak health system and lack of community adherence to personal protection guidelines provided by Ministry of Health suggest that a health disaster due to COVID-19 is inevitable. Enforcement of strict preventive measures, identification and testing of all suspected cases and their contacts, isolation of infected persons and proper care of all COVID-19 patients is urgently needed to avoid this outcome. Furthermore, the Ministry of Health needs to develop well-tailored risk communication messages to raise the awareness of local communities and promote personal protection measures and increase the adherence of the public to the announced health guidelines.
Acknowledgments
We acknowledge all the technical and logistic support from our colleagues in Sudan, the Ministry of Health and the WHO country office.
Contributor Information
Elham R Aljak, National Influenza Centre, National Public Health Laboratory, Sudan Federal Ministry of Health, Khartoum 11111, Sudan.
Mawahib Eldigail, National Influenza Centre, National Public Health Laboratory, Sudan Federal Ministry of Health, Khartoum 11111, Sudan.
Iman Mahmoud, National Influenza Centre, National Public Health Laboratory, Sudan Federal Ministry of Health, Khartoum 11111, Sudan.
Rehab M Elhassan, National Influenza Centre, National Public Health Laboratory, Sudan Federal Ministry of Health, Khartoum 11111, Sudan.
Adel Elduma, National Influenza Centre, National Public Health Laboratory, Sudan Federal Ministry of Health, Khartoum 11111, Sudan.
Abubakr A Ibrahim, Director General, National Public Health Laboratory, Sudan Federal Ministry of Health, Khartoum 11111, Sudan.
Yousif Ali, Directorate of Epidemics and humanitarian settings, Sudan Federal Ministry of Health, Khartoum 11111, Sudan.
Scott C Weaver, World Reference Center for Emerging Viruses and Arboviruses, University of Texas, Medical Branch, Galveston, TX 77550, USA; Institute for Human Infections and Immunity and Department of Microbiology and Immunology, University of Texas Medical Branch, Galveston, TX 77550, USA.
Ayman Ahmed, World Reference Center for Emerging Viruses and Arboviruses, University of Texas, Medical Branch, Galveston, TX 77550, USA; Institute for Human Infections and Immunity and Department of Microbiology and Immunology, University of Texas Medical Branch, Galveston, TX 77550, USA; Institute of Endemic Diseases, University of Khartoum, PO Box 2318 Khartoum 11111, Sudan.
Authors’ contributions
ERA, ME, IM, RME, AE, AIA, SCW and AA conceived and designed the study. ERA, ME, IM, RME, AE, YA and AA were responsible for study implementation. ERA, AE and AA were responsible for formal analysis and interpretation of data. AA was responsible for writing the original draft. ERA, ME, IM, RME, AE, AIA, YA, SCW and AA were responsible for review and editing of the article. All authors have read and agreed to the published version of the article. ERA and AA are guarantors of the paper.
Funding
None.
Competing interests
None declared.
Ethical approval
Not required. All data included in this article is collected by a surveillance system investigating the COVID-19 pandemic and all patients were treated in accordance with Declaration of Helsinki and their privacy rights were observed. This research was approved by the Sudan National Public Health Laboratory.
Data availability
The data underlying this article are available in this published article.
References
- 1. Zhu N, Zhang D, Wang W et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Huang C, Wang Y, Li X et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Li Q, Guan X, Wu P et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382(13):1199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sohrabi C, Alsafi Z, O'Neill N et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020;76:71–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. World Health Organization Novel coronavirus (2019-nCoV) situation reports. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports [accessed 5 September 2020]. [Google Scholar]
- 6. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 Cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–42. [DOI] [PubMed] [Google Scholar]
- 7. Makoni M. Africa prepares for coronavirus. Lancet. 2020;395(10223):483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wharton G, Ali OE, Khalil S et al. Rebuilding Sudan's health system: opportunities and challenges. Lancet. 2020;395(10219):171–3. [DOI] [PubMed] [Google Scholar]
- 9. Mohamed NS, Osman HA, Muneer MS et al. Identifying asymptomatic Leishmania infections in non-endemic villages in Gedaref state, Sudan. BMC Res Notes. 2019;12(1):566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ahmed A, Elbashir A, Mohamed AA et al. Socioeconomic impacts of elimination of onchocerciasis in Abu-Hamed focus, northern Sudan: lessons after elimination. BMC Res Notes. 2020;13(1):256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ahmed A, Ali Y, Mohamed NS. Arboviral diseases: the emergence of a major yet ignored public health threat in Africa. The Lancet Planetary Health. 2020;4(12):e555. [DOI] [PubMed] [Google Scholar]
- 12. Ahmed A, Ali Y, Elmagboul B et al. Dengue fever in the Darfur Area, Western Sudan. Emerging Infect Dis. 2019;25(11):2126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ahmed A, Dietrich I, LaBeaud AD et al. Risks and challenges of arboviral diseases in Sudan: the urgent need for actions. Viruses. 2020;12(1):81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ahmed A, Ali Y, Elduma A et al. Unusual outbreak of Rift Valley fever in Sudan, 2019. Emerg Infect Dis. 2020;26(12):3030–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ahmed A, Elduma A, Magboul B et al. The first outbreak of dengue fever in Greater Darfur, Western Sudan. Trop Med Infect Dis. 2019;4(1):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ahmed A. Urgent call for a global enforcement of the public sharing of health emergencies data: lesson learned from serious arboviral disease epidemics in Sudan. Int Health. 2020;12(4):238–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Charani E, Cunnington AJ, Yousif AHA et al. In transition: current health challenges and priorities in Sudan. BMJ Glob Health. 2019;4(4):e001723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. BBC Coronavirus in Sudan exposes new leaders. Available from: https://www.bbc.com/news/world-africa-52735520 [accessed 16 October 2020]. [Google Scholar]
- 19. Lau H, Khosrawipour V, Kocbach P et al. Internationally lost COVID-19 cases. J Microbiol Immunol Infect. 2020;53(3):454–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Holshue ML, DeBolt C, Lindquist S et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Parodi SM, Liu VX. From containment to mitigation of COVID-19 in the US. JAMA. 2020;323(15):1441–2. [DOI] [PubMed] [Google Scholar]
- 23. Bai Y, Yao L, Wei T et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323(14):1406–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395(10231):1225–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Overseas Security Advisory Council Health alert: Sudan, government announces lockdown In Khartoum effective April 18. Available from: https://www.osac.gov/Content/Report/1c445abc-3b41-4784-8491-18717e93b48b [accessed 17 April 2020]. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article are available in this published article.