Abstract
Objective: Lumbar spondylolysis, caused by stress fracture of the pars interarticularis may lead to a bony defect or spondylolisthesis. In adolescents, its surgical treatment employs the smiley face rod method for direct reduction of pseudoarthrotic spondylolysis and spondylolisthesis. Clinical outcomes of this treatment have been occasionally described; however, implant removal has not been discussed previously. We present a patient with lumbar spondylolysis with grade 1 slip at the 5th lumbar vertebra (L5) per the Meyerding classification.
Patient: A 14-year-old boy presented with chronic severe lower back pain. Since conservative therapy did not resolve pain or enable resuming sports activities, the smiley face rod repair was performed 7 months after the initial treatment.
Result: Anterior slippage of the L5 was surgically reduced. The patient wore a brace for 3 months postoperatively, and partial bone fusion was noted 6 months postoperatively. He resumed his sports activity 8 months postoperatively, and absolute bone fusion was confirmed 18 months postoperatively. Implant removal was performed 3 years postoperatively. Grade 1 slip was corrected with absolute bone fusion, and long-term follow-up revealed good results in terms of healing and rehabilitation.
Conclusion: Smiley face rod method that allows for implant removal after bone fusion is suitable for adolescents.
Keywords: lumbar spondylolysis, smiley face rod method, direct reduction, spondylolisthesis, implant removal
Introduction
Spondylolysis is a defect of the pars interarticularis. In pseudoarthrotic spondylolysis where pain is persistent even after conservative therapy, surgical treatment is an effective treatment. Lumbosacral fusion is the most common surgery performed for spondylolysis with a slipped vertebra. We avoid interbody fusion that causes adjacent intervertebral disorders, and prefer repairing the pars defects by using the smiley face rod method to preserve the mobile lumbar segments. Here, we describe the treatment and the bone fusion process, from surgery to implant removal, in a patient with pseudoarthrotic spondylosis who showed reduction of the slipped vertebra and bone fusion on long-term follow-up.
Case presentation
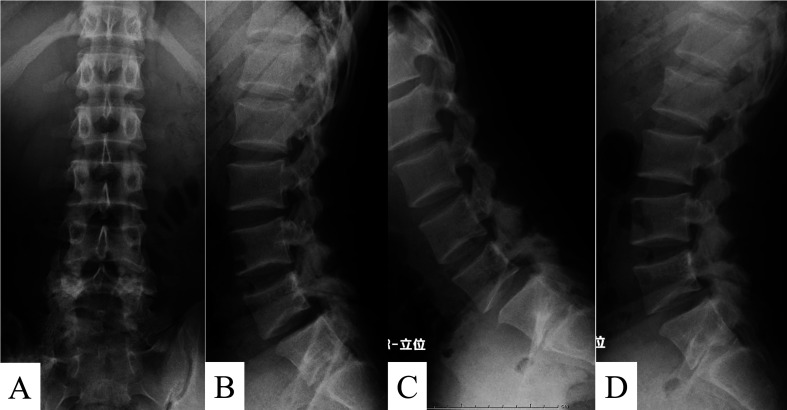
A 14-year-old boy presented with complaints of chronic severe lower back pain during sports activity. Neurological examination at his first visit revealed no muscle weakness or sensory disturbances and normal deep tendon reflexes in both lower limbs. Sciatic nerve tension tests were negative. Plain radiographs of the lumbar spine revealed pars defects at the 5th lumbar vertebra (L5) with grade 1 slip per the Meyerding classification. Anterior translational movement was 6.9 mm and the percentage of slip on the Taillard index was 16.9% (Figure 1). Computed tomography (CT) revealed bilateral pseudoarthrosis of the pars interarticularis at L5. Short tau inversion recovery magnetic resonance images (MRI) showed no signs of bone marrow edema and central or foraminal stenosis (Figure 2). He was diagnosed with pseudoarthrotic spondylolysis, and conservative treatment was started with a brace and physical therapy. However, his pain did not resolve, and the patient was unable to return to his sports activity. The smiley face rod surgical method was advised, and both the patient and his parents consented to its use.
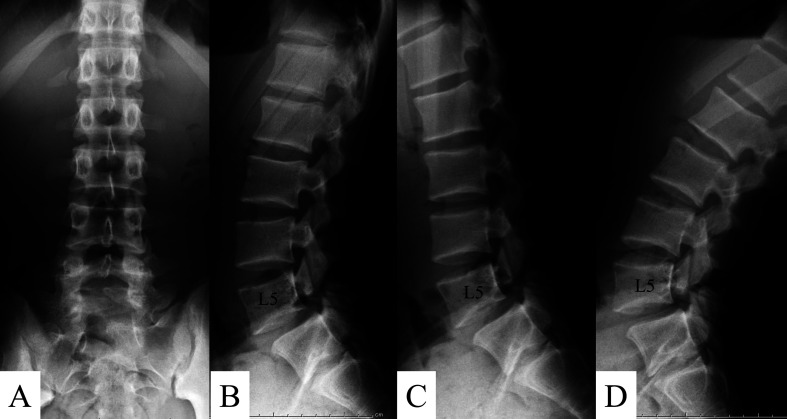
Figure 1.
Preoperative anteroposterior (A) and lateral (B) radiographs of the lumbar spine. The dynamic views are shown in flexion (C) and extension (D). Radiographs revealed pars defects at the 5th lumbar vertebra (L5) with grade 1 slip per the Meyerding classification. The anterior translational movement was 6.9 mm and the Taillard index was 16.9%.
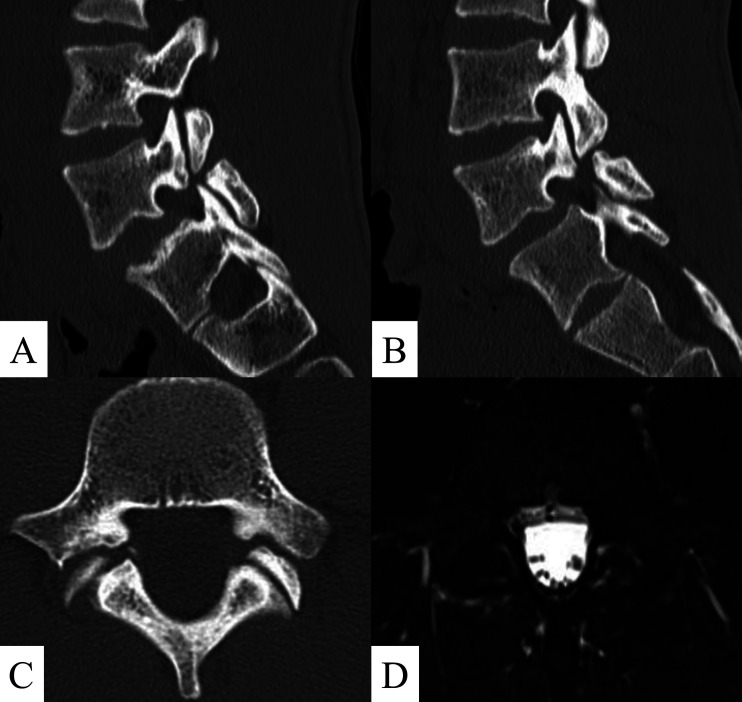
Figure 2.
Preoperative computed tomography (CT) and magnetic resonance imaging (MRI) of L5: Sagittal CT scan of the right (A) and left side (B). The axial CT image (C) of the pars defect. Short tau inversion recovery axial image (D) showing no bone marrow edema.
Two skin incisions were made (4 cm in length) laterally from the midline and the paraspinal musculature was elevated laterally to expose the lamina by the Wiltse’s approach. The defect in the pars was exposed, and the synovium and pseudocapsule of the pars interarticularis were removed. A burr was used to decorticate the hardened pars interarticularis. A pedicle screw was inserted using the Weinstein method. Bone graft was harvested from the iliac crest, placed in the defect, and impacted before insertion of the screw. Thereafter, a rod was contoured in a U shape, placed just caudal to the spinous process, and attached to each pedicle screw. The rod was positioned subcutaneously to penetrate the interspinous ligament to ensure the continuity of the ligament. The reduction tool was used to eliminate the gap in the pars interarticularis and fix the pedicle screw and rod. Bumping the bended rod against the spinous process, the loose lamina was fixed firmly. Final fluoroscopic imaging confirmed the correct position of the screw and rod and the reduction of the slipped vertebra (Figure 3).
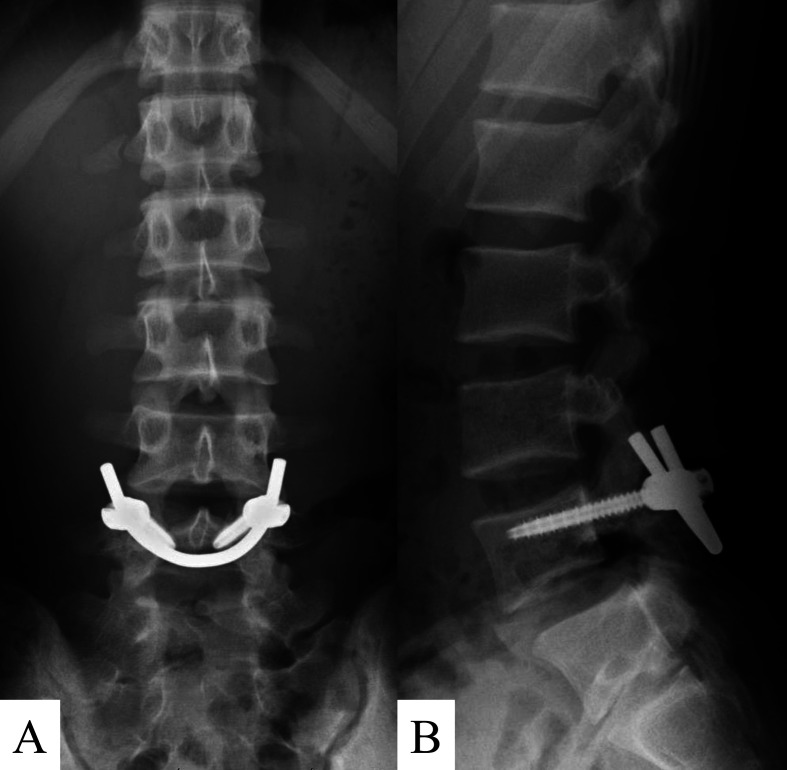
Figure 3.
Postoperative anteroposterior (A) and lateral (B) radiographs
Postoperative treatment
Standing and walking commenced 2 days postoperatively with a semi-rigid brace. Rehabilitation measured that comprised passive and active movements of the lower limbs were initiated immediately. The patient performed isometric exercises for trunk muscles and stretching for tight hamstrings. After 1-month postoperatively, the lower limb muscles were strengthened using static exercises and electro-stimulation; flexion-extension movements of the spine were avoided. He continued to wear the brace for 3 months postoperatively, and healing began from the lateral side as demonstrated on CT. The patient was permitted to start exercises such as jogging and axial rotations. Six months postoperatively, partial fusion was confirmed from the cephalad direction up to both sides in the sagittal section and complete bone fusion was confirmed 18 months postoperatively (Figures 4 and 5). One year postoperatively, the anterior translational movement and percentage of slip were 0 mm and 0%, respectively (Figure 6). Clinical outcome was evaluated pre- and postoperatively using a 100-mm Visual Analog Scale (VAS) with 0 representing no pain and 100 representing maximum pain. One year postoperatively, the VAS score improved from 20 to 0. Implant removal was performed 3 years postoperatively (Figure 7). The patient remained asymptomatic without any repositioning of the slipped vertebra after the implant removal.
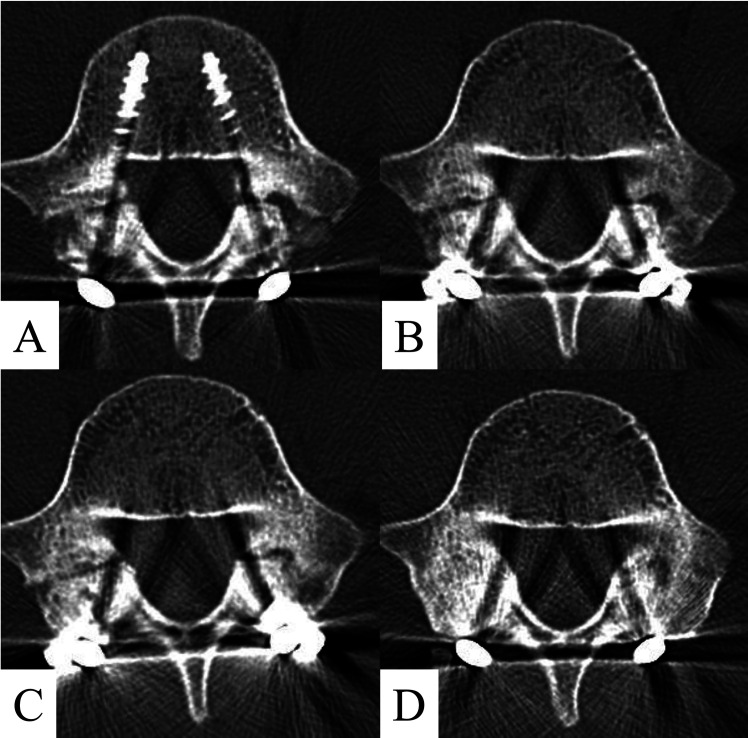
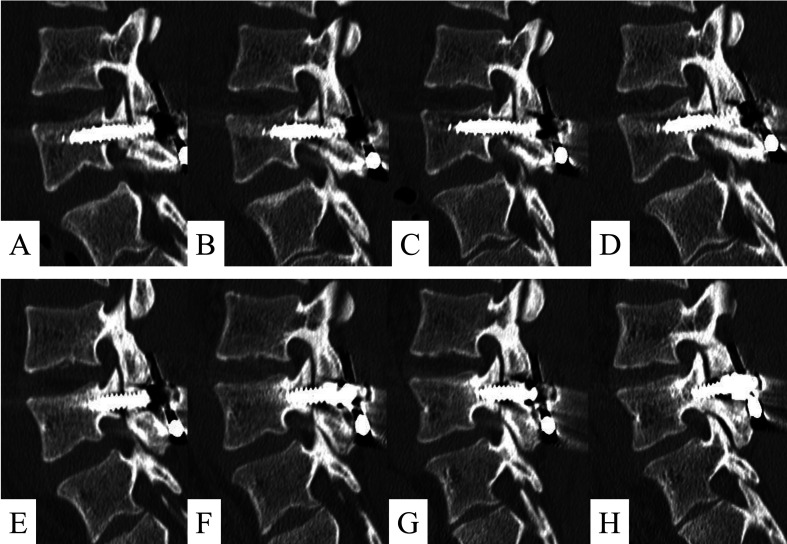
Figure 4.
Postoperative axial computed tomography (CT) scan showing compression over the pars defect (A). CT scans demonstrate fracture healing 3 months postoperatively (B) and partial bone union 6 months postoperatively (C). Eighteen months postoperatively, the CT scan indicates the union of the pars defect (D).
Figure 5.
Follow-up computed tomography (CT) images of the lumbar spine on the right side (A–D), postoperative CT scan at 3 months, 6 months, and 18 months postoperatively, and of the left side (E–H).
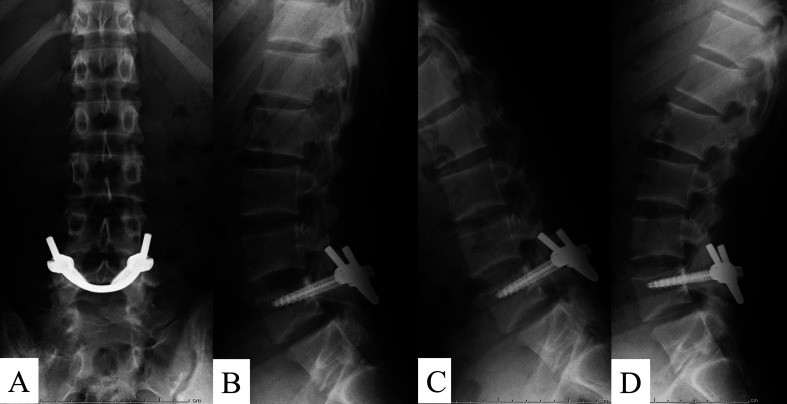
Figure 6.
Postoperative radiographs show reduction with smiley face rod method 1-year postoperatively; anteroposterior (A), lateral (B), dynamic flexion (C), and extension (D). The slipped vertebra is reduced, and no slippage and screw loosening are seen on the lateral radiograph.
Figure 7.
Postoperative radiograph after the implant removal; anteroposterior view (A), lateral view (B), and dynamic flexion (C) and extension (D). Radiographs show maintained reduction and reduced instability.
Discussion
Lumbar spondylolysis is a defect of the pars interarticularis caused by a stress fracture1). Repetitive hyperextension of the lumbar spine may contribute to this disorder. The treatment of acute lumbar spondylolysis should include a rest period, with bracing to allow healing, and rehabilitation, and ensure return to sports activities once patients are asymptomatic2). Commonly, bone fusion may not be achieved through conservative treatment that includes modification of posture, physical therapy, and bracing with a thoracolumbar and sacral orthosis. Inflammatory events in the pseudoarthrotic pars defects and adjoining facet joints may cause lower back pain in pseudoarthrotic spondylolysis3), resulting in progressive spondylolisthesis in up to 43–74% of all patients4). Additionally, associated adverse effects such as sciatica caused by intervertebral foraminal stenosis can occur. Therefore, it is important that patients undergo a long-term follow-up. Our patient had chronic lower back pain without sciatica that was resistant to conservative treatment; thus, surgical treatment was considered. Historically, surgical management of spondylolysis includes posterior and posterolateral fusion and pars interarticularis repair5, 6). Lumbar interbody fusion results in loss of movement in a segment and may reduce pain. However, surgical fusion of the lumbar spine may result in an eventual adjacent level arthrosis with symptomatic degeneration warranting additional surgery in 16.5% and 36.1% of patients in 5 and 10 years, respectively7); and an increased risk of need for revision surgery8). Direct pars interarticularis repair has the advantage of preserving mobile segments and dealing directly with the anatomical defect.
Several methods of direct repair with good or excellent results have been reported. Buck9) first described the technique of direct repair by filling the gap in the defect with iliac cancellous autograft and placing screws directly through the defect itself. The other methods such as the Scott technique10), used wiring to stabilize the posterior arch under the transverse process. Although, a lot of surgeons have reported satisfactory outcomes with these methods, these techniques have some shortcomings. Proper placement of screws or cerclage wire is difficult, it decreases the area for bone grafting, and the screws and wires are not strong11,12,13). Sublaminar hook, pedicle screw combinations, and pedicle screw-rod-hook constructs have been used. Biomechanical studies have shown the latter construct to be the most stable14). However, numerous problems have been encountered with this technique, including difficulty in screw placement, screw loosening and breakage, and a high rate of failure. Further, it is difficult to reposition the slipped vertebra15). The smiley face rod method employs a direct repair, places screws on the pedicles of the involved vertebra, and fixes the loose posterior arch with a solid rod bent into a U shape. This method is stabilized with an intralaminar rod construct that consists of a pair of multiaxial pedicle screws connected with a modular rod that passes beneath the spinous process of the same segment. Tightening the rod to the screws compresses the bone grafted over the pars defect. This system provides a rigid intrasegmental fixation, without interfering with intersegmental motion, and good reduction in low-grade spondylolisthesis16, 17).
Clinical results were excellent 3 years postoperatively. Radiographically, bone fusion was achieved in this case and the slipped vertebra had reduced. Literature on clinical outcomes, such as solid bone fusion and accurate slip reduction, is limited; and there are no reports on implant removal. It seemed essential to demonstrate the effectiveness of the smiley face rod method even after the implant removal. This surgical technique allows for implant removal after bone fusion and preserves adjacent segment movement; therefore, it is particularly suitable for adolescent patients. Studies with longer follow-ups are needed to evaluate the quantum of sliding and disc degeneration associated with this method.
References
- 1.Sairyo K, Katoh S, Sasa T, et al. Athletes with unilateral spondylolysis are at risk of stress fracture at the contralateral pedicle and pars interarticularis: a clinical and biomechanical study. Am J Sports Med 2005; 33: 583–590. doi: 10.1177/0363546504269035 [DOI] [PubMed] [Google Scholar]
- 2.Tatsumura M, Gamada H, Ishimoto R, et al. Prevalence of curable and pseudoarthrosis stages of adolescent lumbar spondylolysis. J Rural Med 2018; 13: 105–109. doi: 10.2185/jrm.2967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sairyo K, Sakai T, Mase Y, et al. Painful lumbar spondylolysis among pediatric sports players: a pilot MRI study. Arch Orthop Trauma Surg 2011; 131: 1485–1489. doi: 10.1007/s00402-011-1336-z [DOI] [PubMed] [Google Scholar]
- 4.Crawford CH, 3rd, Ledonio CG, Bess RS, et al. Current evidence regarding the etiology, prevalence, natural history, and prognosis of pediatric lumbar spondylolysis: a report from the scoliosis research society evidence-based medicine committee. Spine Deform 2015; 3: 12–29. doi: 10.1016/j.jspd.2014.06.005 [DOI] [PubMed] [Google Scholar]
- 5.Sherman FC, Rosenthal RK, Hall JE. Spine fusion for spondylolysis and spondylolisthesis in children. Spine 1979; 4: 59–66. doi: 10.1097/00007632-197901000-00010 [DOI] [PubMed] [Google Scholar]
- 6.Wiltse LL, Jackson DW. Treatment of spondylolisthesis and spondylolysis in children. Clin Orthop Relat Res 1976; 92–100. [PubMed] [Google Scholar]
- 7.Ghiselli G, Wang JC, Bhatia NN, et al. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am 2004; 86: 1497–1503. doi: 10.2106/00004623-200407000-00020 [DOI] [PubMed] [Google Scholar]
- 8.Moreau PE, Ferrero E, Riouallon G, et al. Radiologic adjacent segment degeneration 2 years after lumbar fusion for degenerative spondylolisthesis. Orthop Traumatol Surg Res 2016; 102: 759–763. doi: 10.1016/j.otsr.2016.03.012 [DOI] [PubMed] [Google Scholar]
- 9.Buck JE. Direct repair of the defect in spondylolisthesis. Preliminary report. J Bone Joint Surg Br 1970; 52: 432–437. doi: 10.1302/0301-620X.52B3.432 [DOI] [PubMed] [Google Scholar]
- 10.Nicol RO, Scott JH. Lytic spondylolysis. Repair by wiring. Spine 1986; 11: 1027–1030. doi: 10.1097/00007632-198612000-00011 [DOI] [PubMed] [Google Scholar]
- 11.Pedersen AK, Hagen R. Spondylolysis and spondylolisthesis. Treatment by internal fixation and bone-grafting of the defect. J Bone Joint Surg Am 1988; 70: 15–24. doi: 10.2106/00004623-198870010-00004 [DOI] [PubMed] [Google Scholar]
- 12.Johnson GV, Thompson AG. The Scott wiring technique for direct repair of lumbar spondylolysis. J Bone Joint Surg Br 1992; 74: 426–430. doi: 10.1302/0301-620X.74B3.1587895 [DOI] [PubMed] [Google Scholar]
- 13.Morscher E, Gerber B, Fasel J. Surgical treatment of spondylolisthesis by bone grafting and direct stabilization of spondylolysis by means of a hook screw. Arch Orthop Trauma Surg 1984; 103: 175–178. doi: 10.1007/BF00435550 [DOI] [PubMed] [Google Scholar]
- 14.Wiltse LL, Winter RB. Terminology and measurement of spondylolisthesis. J Bone Joint Surg Am 1983; 65: 768–772. doi: 10.2106/00004623-198365060-00007 [DOI] [PubMed] [Google Scholar]
- 15.Winter M, Jani L. Results of screw osteosynthesis in spondylolysis and low-grade spondylolisthesis. Arch Orthop Trauma Surg 1989; 108: 96–99. doi: 10.1007/BF00932163 [DOI] [PubMed] [Google Scholar]
- 16.Gillet P, Petit M. Direct repair of spondylolysis without spondylolisthesis, using a rod-screw construct and bone grafting of the pars defect. Spine 1999; 24: 1252–1256. doi: 10.1097/00007632-199906150-00014 [DOI] [PubMed] [Google Scholar]
- 17.Ulibarri JA, Anderson PA, Escarcega T, et al. Biomechanical and clinical evaluation of a novel technique for surgical repair of spondylolysis in adolescents. Spine 2006; 31: 2067–2072. doi: 10.1097/01.brs.0000231777.24270.2b [DOI] [PubMed] [Google Scholar]