Abstract
Background
Teledermatology may be used for triage in primary care to address skin conditions, improving access and reducing time to treat the most severe or surgical cases. We aimed to evaluate the proportion of individuals who could be assessed in primary care using teledermatology, and how this affected the waiting time for an in-person dermatologist appointment.
Methods
A cross-sectional retrospective study, involving 30,976 individuals and 55,624 skin lesions, was performed from July 2017 to July 2018 We assessed the frequency of diagnoses and referrals to biopsy, to in-person dermatologists, or to primary care, and compared the waiting time for an in-person dermatologist appointment before and after the teledermatology implementation.
Findings
53% of the patients were managed with the primary care physician, 43% were referred to in-person dermatologists and 4% directly to biopsy, leading to a reduction of 78% in the waiting time for in-person appointments when compared to the previous period. The most frequent diseases were: melanocytic nevus, seborrheic keratosis, acne, benign neoplasms, onychomycosis, atopic dermatitis, solar lentigo, melasma, xerosis, and epidermoid cyst, with significant differences according to sex, age and referrals. The most frequent treatment prescribed was emollient.
Interpretation
The use of teledermatology as a triage tool significantly reduced the waiting time for in-person visits, improving health care access and utilizing public resources wisely. Knowledge of sex, age, diagnoses and treatment of common skin conditions can enable public policies for the prevention and orientation of the population, as it can be used to train general physicians to address such cases.
Funding
None.
Keywords: Teledermatology, Tele-health, Telemedicine, Primary care attention, Frequent dermatoses, Frequent skin diseases, Referrals in primary care
Research in context.
Evidence before this study
Store-and-forward teledermatology (SF-TD) can be useful to avoid unnecessary referrals to dermatologists. Most of the teledermatology diagnostic studies published so far are based on one disease or group of diseases, such as melanoma or skin cancer.
Added value of this study
Our study included over 30,000 patients and 55,000 lesions from the general population of São Paulo city, from July 2017 to July 2018, which has a high demand for public dermatologists, thereby presenting robust data. We found that 53% of the patients could be triaged using SF-TD, with treatment suggestions directed to the patients’ primary care physicians, reducing referrals to in-person dermatologist. Other benefits included the option to refer the patients to the biopsy unit before the dermatologist's visit (4% of the patients), optimizing the time available for more serious diagnoses, such as skin cancer, and the assessment of the 10 most frequent dermatoses in primary care, according to demographic data, referrals and treatments.
Implications of all the available evidence
SF-TD can be an effective tool for reducing referrals of common skin conditions among the general population to dermatologists. It can provide numerous benefits, such as optimizing in-person visits for patients with serious/complex skin conditions, and quickly and conveniently assessing common skin conditions with the primary care physician. This can save resources, working days and patient transportation. Knowledge of the most common skin conditions and treatments encountered in primary care can inform public health policies for the prevention of diseases, and help train physicians on how to address such cases.
Alt-text: Unlabelled box
1. Introduction
Teledermatology (TD) is a healthcare tool that has been more frequently used worldwide, especially during the COVID-19 pandemic, due to the recommendations given for months by many governments for the population to stay home. Most medical research focuses on delivering two types of images: real-time (RT) and store-and-forward (SF) images [1]. In the latter type, the data and images from a patient are collected and sent to a dermatologist to be analyzed at a later time. Real time teledermatology (RT-TD) enables the live communication of data and images between patients and physicians from separate locations [1]. Store-and-forward teledermatology (SF-TD) improves access to specialty care, provides accurate diagnoses, and reduces time to treatment, resulting in high patient satisfaction [2].
The early detection and timely treatment of severe skin diseases can prevent adverse health outcomes and death. On the other hand, some skin conditions such as mild atopic dermatitis, acne, and fungal infections can be managed within primary care. However, in our country, general physicians may not be trained to diagnose or triage skin diseases and we continuously see unnecessary referrals to dermatologists. If there is a shortage of dermatologists, this creates a problem as appointments are filled by patients who do not need specialty care, limiting the availability of visits for those who do. This results in patients with potentially fatal problems such as melanomas, cutaneous lymphoma, adverse cutaneous drug reactions and pemphigus facing lengthy delays in receiving their diagnosis and treatment. In contrast, those with minor conditions face costs and travel burdens due to unnecessary visits to a dermatologist.
The city of São Paulo has nearly 12 million inhabitants [3], and 58% of them depend exclusively on the public health care system [4]. The demand for public dermatologist consultations in São Paulo is incredibly high, and in July 2017, there were 57,832 individuals waiting for appointments which could take up to one year to obtain [5]. For this reason, the municipal health department decided to implement a teletriage dermatology project in conjunction with Hospital Israelita Albert Einstein, to shorten the waiting time for a dermatologist appointment, improve access for the patients with severe skin conditions, and eliminate unnecessary dermatology referrals. This main objective of the present study was to analyze the proportion of patients that could be diagnosed and/or treated by teledermatology and their primary care physicians, and how the waiting time for an in-person dermatologist visit was affected by this project.
2. Methods
This study was approved by Hospital Israelita Albert Einstein and Municipal Ethics Committees (CAAE:97126618.6.3001.0086) and it follows the ethical standards on human experimentation and with the Declaration of Helsinki. Data was fully anonymized before accessed and the IRB waived the requirement for the informed consent.
2.1. Teledermatology project
We performed a cross-sectional retrospective study, using the data obtained from a teledermatology project implemented from July 2017 to July 2018, in São Paulo. There were 57,832 individuals waiting for a consultation with a dermatologist in the public health system in July 2017. The authors MGB and AS had access to the database from August to December 2018. To reduce the waiting list and accelerate the flow of patients with the most severe, complex or surgical dermatoses to in-person dermatologists, the municipal health government requested Hospital Israelita Albert Einstein, a large private hospital in the city with expertise in Telemedicine, to develop a project using Telemedicine to reach these goals. Therefore, a mobile app was created by the authors for Android cell phone systems, and hosted on a web platform from Amazon Web Services (AWS). The app was designed to take photographs of skin lesions with the cell phone cameras, along with a short clinical history and demographic data of the patient, and directly uploaded them to the platform. In this project, the app was intended to be used by health technicians or nurses.
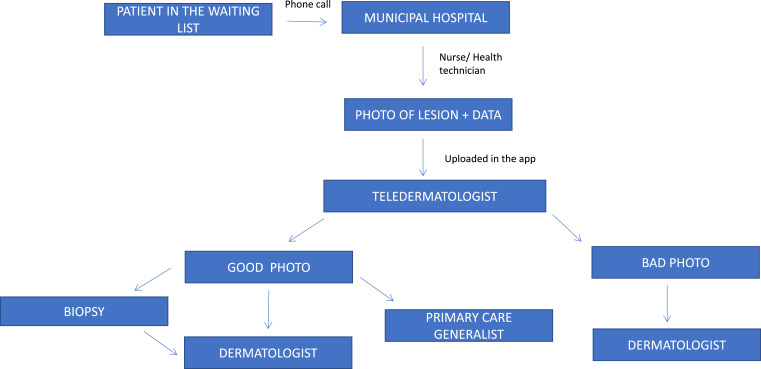
The photographs and collected information were uploaded on the platform using a secure online process through usernames and passwords, and were accessed only by the 13 Brazilian Board Certified dermatologists associated with this project, who would choose the patients from the patients’ list, consecutively. These 13 dermatologists will be called teledermatologists in this study. All the patients waiting for dermatologist consultations were called consecutively, via phone, by the municipal health care service and scheduled for an appointment in one of the three public city hospitals (Hospital São Miguel Paulista, Hospital CIES Santo Amaro and Hospital Vila Nova Cachoeirinha) enabled to carry out the project, depending on the location of the individual's residence. Once there, a short history of the complaint (history of bleeding, pruritus, time from the onset, and location) and demographic data (sex and age), as well as three photographs in different angles and distances from each lesion were taken by a trained health technician: first one at medium distance (50 cm away), second one in close-up (15 cm away) and last one of a lateral view, aiming to evaluate the volume of the lesion. After accessing the patients’ pictures and clinical history of the patients by SF-TD, the teledermatologists first decided whether the photographs of the lesions were satisfactory for diagnostic purposes. If not, they categorized it under “bad photo”, and the patient was referred to an in-person dermatologist. If the photo quality was good enough, they formulated the most probable diagnostic hypothesis. They chose one of three options for each lesion assessed: 1) a direct referral for a biopsy (after which the patient would return for an in-person dermatologist appointment), 2) a referral for an in-person dermatologist visit, or 3) a referral to go back to the primary care physician with the most probable diagnosis, treatment and/or recommendation on how to proceed with the investigation and/or management of the lesion. A schematic for this process is shown in Fig. 1. If the same patient had more than one lesion but different referrals, he/she was referred to the most specialized one and that would be his/her final referral. For instance, a biopsy would prevail over a dermatologist visit, which would in turn prevail over general physician referral.
Fig. 1.
The schematics for the flow of collecting data and photographs of the lesions during the teletriage project from July 2017 to July 2018 in the city of São Paulo, Brazil.
2.2. Results analysis
The waiting time for an in-person dermatologist appointment is continuously monitored online by the municipal government, and it was calculated from the time the patient was referred to the dermatologist until the in-person appointment has occurred and did not involve time to perform the biopsy. To calculate how it was affected by the project, we assessed the mean waiting time for an in-person dermatologist visit for 3 months before the beginning of the project (April–June 2017) and by the end of the project (June–August 2018). All the statistical calculations were done using a two-tailed chi-square test with the Yates correction on the GraphPad Prism 6.0 software.
2.3. Role of funding source
There was no funding source.
3. Results
From 57,832 patients waiting for a dermatologist consultation in São Paulo, 30,976 individuals participated in this project (54%). In 2017, the total amount of in-person visits to dermatologists was 192,203 [6]. Hence, the number of patients’ visits in the project corresponds to 16% of all the “regular” appointments to dermatologists in a year. There were more female (39,046; 68%) than male (18,786; 32%) individuals waiting for a consultation with a dermatologist (2:1 proportion). 54% of the women in the waiting list attended to the project versus 52% of the men. The lowest rate of attendance was among children and young adults up to 24 years of age (<50%), and the highest was among the 60–69 age group (65%).
55,624 lesions were reported over the course of this project. Each lesion was photographed from three different angles. Therefore, around 166,000 images were evaluated. The mean number of lesions photographed per person was 1.8. The female patients had a mean of 1.86 lesions photographed per person, and the male patients had a mean of 1.6. The photograph quality was classified as “poor” for 613 lesions (1839 images; 1.1%), and dermatologists referred those patients for in-person appointments. The remaining 55,011 lesions were diagnosed and referred to one appropriate care unit.
Bleeding occurred in only 11% of the lesions, but pruritus was fairly common (43%). The head and neck were the main sites for the lesions (52%), and most of the cases had over three years since the onset (53%).
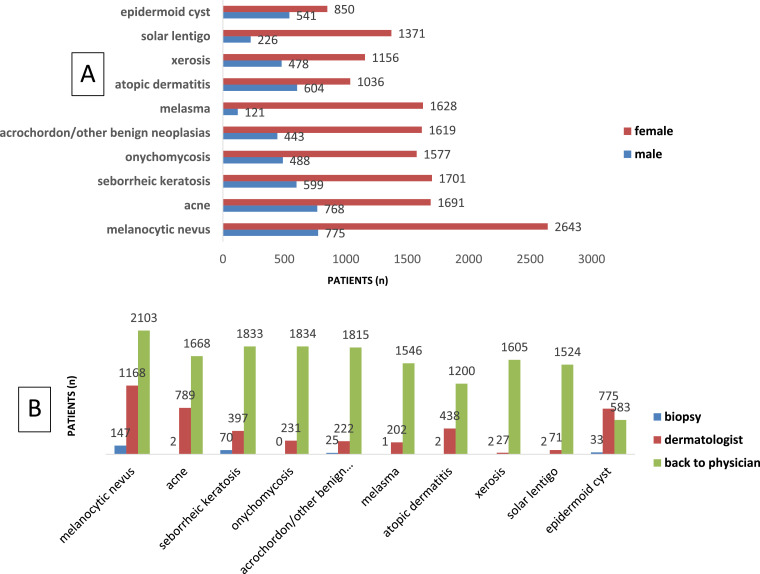
Next, we assessed the 10 most common diseases presented by our subjects according to sex (Fig. 2A) and whether they were referred to biopsy, an in-person dermatologist, or back to the general physician (Fig. 2B).
Fig. 2.
The 10 most common skin conditions presented by the patients who participated in the teletriage project, categorized according to sex (A) and referrals (B), from July 2017 to July 2018 in the city of São Paulo.
There were substantial differences in the most common disorders between the two sexes. The women commonly presented melanocytic nevus (p < .0001), seborrheic keratosis (p = .0024), melasma (p < .0001), onychomycosis (p < .0001), acrochordon/other benign neoplasia (p < .0001), and solar lentigo (p < .0001). The male subjects primarily presented acne (p < .0001), atopic dermatitis (p < .0001) and epidermoid cysts (p < .0001). There was no difference in sex for the patients with xerosis (p=.899).
Four of the 10 most frequent lesions—melanocytic nevus, seborrheic keratosis, acrochordon, and cysts—belonged to the benign tumor group. One was an inflammatory process (acne), one was a fungal infection (onychomycosis), two were pigmentary disorders (melasma and solar lentigo), and two were in the eczema spectrum (atopic dermatitis and xerosis). They accounted for 24,238 lesions, corresponding to 44% of the total. 79% of those patients were sent back to their general physicians with recommendations and/or treatment plans, as shown in Fig. 2B. Only 1% was referred for biopsy, mostly for melanocytic nevi, and the remaining 20% were sent to dermatologists for in-person appointments.
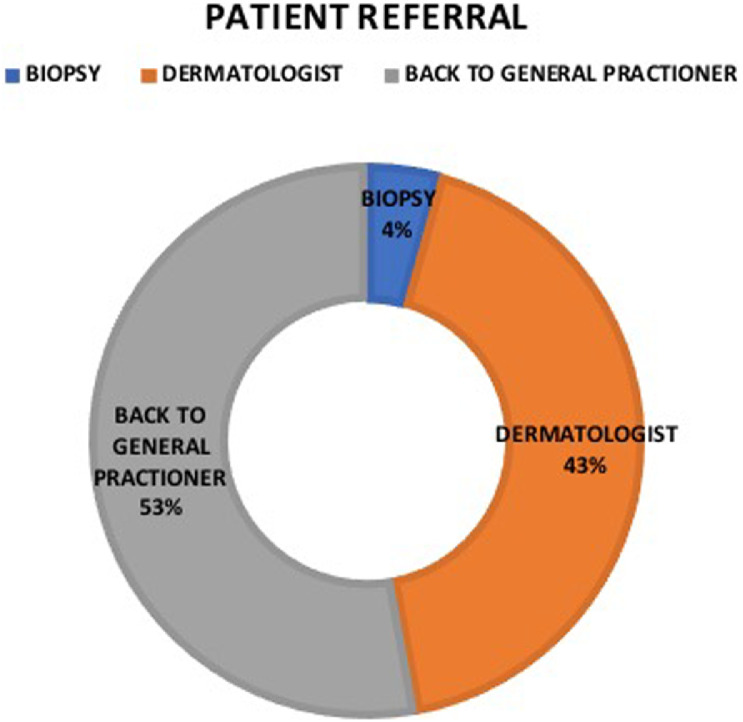
Fig. 3 shows the distribution of the teledermatologists’ referrals. 53% of the cases could be addressed by teledermatology through primary care attention; 4% of them were directly sent to biopsy, and 43% were sent to an in-person dermatologist. This teletriage led to a 78% of reduction in the mean waiting time for in-person dermatologist visits (from 6.7 months before the launch of project, calculated over the period from April to June 2017 to 1.5 by the end of the project, calculated over the period from June to August 2018). This information was obtained directly from municipal health department staff during the implementation and closure meetings.
Fig. 3.
The proportions of patients referred to biopsy, in-presence dermatologists, and general physicians by the teledermatologists in the teletriage project from July 2017 to July 2018 in the city of São Paulo.
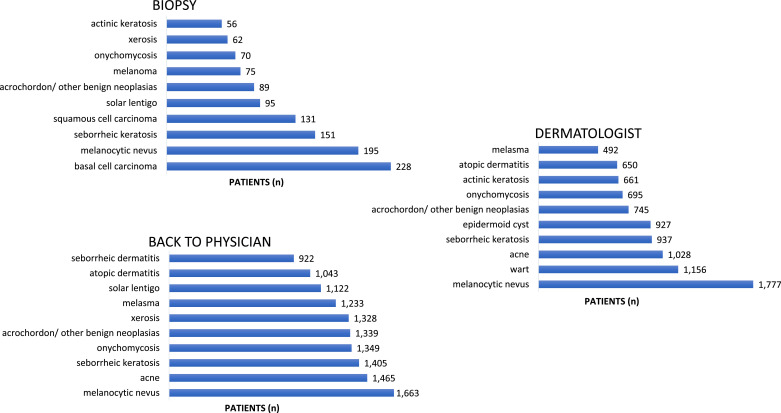
To understand which pathologies led to each referral, we assessed the 10 most frequent diagnoses sent to biopsy, an in-person dermatologist, or back to the general physician (Fig. 4). The biopsy was the teledermatologist's choice in only 3% of all the lesions. Malignant tumors (basal cell carcinoma, squamous cell carcinoma, and melanoma) and premalignant lesions (actinic keratosis- AK) accounted for 42% of the 1912 biopsy referrals, which was the first choice for 72% to 89% of such cases. Benign lesions such as melanocytic nevus, seborrheic keratosis, solar lentigo, and acrochordon were responsible for 16% of this type of referral, although biopsy was the teledermatologists’ option for this group only in 4% of the times.
Fig. 4.
The 10 most frequent causes for referrals to biopsy, in-presence dermatologists, and back to physicians among patients who participated in the teletriage project from July 2017 to July 2018 in the city of São Paulo.
31% of the lesions were referred to in-person dermatologists. Benign proliferations (melanocytic nevus, seborrheic keratosis, and cysts) were among the top 10 diseases, accounting for 15% of this in-person dermatologist referral. Two infectious diseases, warts and molluscum, were also frequently referred to in-person dermatologists (10%). Acne, vitiligo, psoriasis, and atopic dermatitis accounted for 15% of these referrals, and AK alone was responsible for 4%. We found that over 80% of the AK and warts, 56% of the epidermoid cysts, 33% of the acne and melanocytic nevus, 28% of the AD, 94% of the molluscum, 60% of psoriasis, and 78% of vitiligo patients were referred to in-person dermatologists.
The dermatoses most referred to general physicians were: xerosis (98%), solar lentigo (96%), seborrheic dermatitis (90%), melasma (88%), onychomycosis (88%), acrochordon/other benign neoplasia (88%), seborrheic keratosis (81%), atopic dermatitis (72%), and the melanocytic nevus (62%).
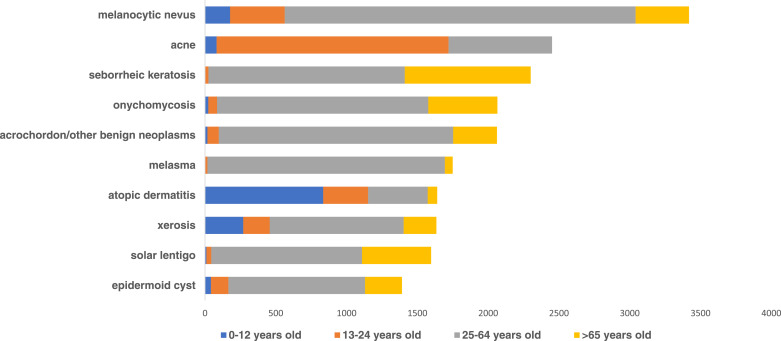
We also categorized the most frequent skin disorders according to age (Fig. 5). We observed that atopic dermatitis, xerosis, and melanocytic nevus were the major concerns in children up to 12 years of age. Adolescents and young adults (13–24 age group) mainly had acne, atopic dermatitis, xerosis, and melanocytic nevus. The adult population (25–64 age group) was the largest population in the study and showed many cases of melasma (in this study, a problem almost exclusively faced by adults) and melanocytic nevus. The population over 65 years of age reported seborrheic keratosis, solar lentigo, onychomycosis, and other benign proliferations such as epidermoid cysts and acrochordon.
Fig. 5.
The 10 most common skin conditions presented by the patients who participated in the teletriage project, categorized according to age, from July 2017 to July 2018 in the city of São Paulo.
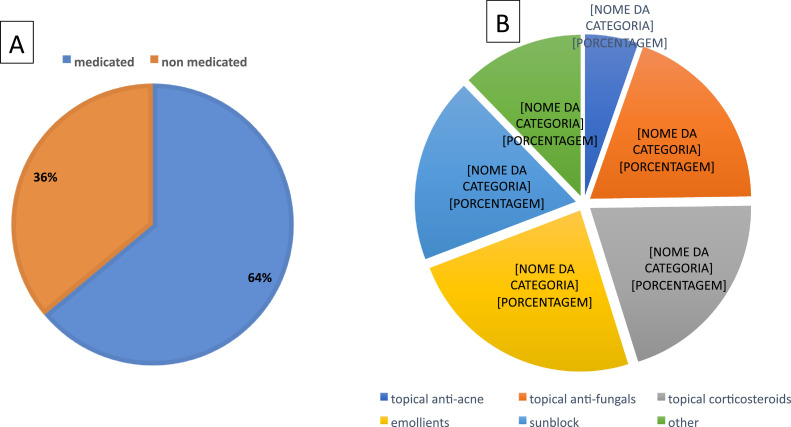
Next, we assessed how many patients were medicated through teledermatology and the most frequent groups of medications prescribed by the teledermatologists (Fig. 6A and B). 18,979 patients (64%) were medicated. Emollient was the most frequent prescription (24%). Topical corticosteroids and antifungals shared the second position with 20% each, followed by sunblock (19%) and topical anti-acne medications (5%). Over-the-counter products such as emollients and sunblock were responsible for 43% of the prescriptions.
Fig. 6.
The proportions of the patients medicated (A) and classes of drugs prescribed (B) during the teletriage project from July 2017 to July 2018 in the city of São Paulo.
4. Discussion
Our study included over 30,000 patients and 55,000 lesions from the general population of a big city with a high demand for public dermatologists, thereby presenting robust data. We found that 53% of the skin lesions could be triaged using SF-TD, and, with diagnostic hypothesis and treatment suggestions directed to the patients’ primary care physicians, referrals for in-person dermatologist were avoided in 57% of the cases. Another benefit was the option to refer the patients to the biopsy unit before the dermatologist's visit, optimizing the time available for more severe diagnostics such as skin cancer. Assessing the 10 most frequent causes for teletriage, according to demographic data, and their referrals and treatments resulted in innovative and important new data.
In our view, the presence of 54% of all the individuals called for this project was reasonable. There may be multiple reasons for this attendance level, such as: 1) patients were waiting for so long in the waiting list that their disease improved or went away by itself, 2) they looked for a dermatologist in the private care setting (popular clinics); 3) they look for help directly with the pharmacist; 4) although they were referred to a dermatologist, the dermatoses did not bother the patient as much to participate in the project. All these reasons can lead to a bias in our study, although the remaining 31,000 individuals are still a robust part of our population. The patients’ participation increased with age, with the 60–69 age group having the highest levels; perhaps this was because retirees have more spare time to visit the doctor and may also be more concerned about health issues than the younger age groups. A more significant number of female patients waiting for a consultation with a dermatologist was expected because, in our culture, more women than men searching for healthcare in general. There was no difference in the attendance rate between the sexes. TD is still a new initiative in the country for patients as well as physicians, and for a pioneer project like this, involving a significant number of people was a challenge that we believe was overcome. Few TD works have had as many participants and covered as many types of skin diseases as ours. Most of the TD articles published so far focus on one disease (such as melanoma) or a single class of diseases (such as malignant tumors) [7], [8], [9].
The head and neck were the most common sites for the lesions. This may be due to aesthetic reasons (raising the patient's concern) and/or chronic UV exposure, a common cause of skin conditions in Brazil since it is located in the tropical and subtropical regions of the southern hemisphere where solar radiation is quite elevated and ozone concentrations are naturally lower. The Ultraviolet Index (UVI) of Brazil reaches the highest UVI scales determined by the WHO—i.e., very high (UVI between 8 and 10) or extreme (UVI higher than 11)—and damages human health [10].
The time of onset of over three years in many patients indicated that the lesions were either indolent and of low concern or the public health system was not efficient enough to supply dermatological medical services for the population; it may even be a combination of these aspects.
There were differences between sex and skin conditions. Benign proliferations such as melanocytic nevus and acrochordon raised more concerns in women while men were more affected by epidermoid cysts. Women showed more pigmentation disorders such as melasma and solar lentigo. Melasma is closely associated with female hormones, being much more frequent in women [11], and solar lentigo occurred in both the sexes but seemed to bother men less. Onychomycosis was also more frequent in women, probably due to trauma at manicure and pedicure practices, which is more common among women than men in Brazil [12]. Atopic dermatitis was more prevalent in men, in whom the severity seemed to be more significant [13]. Acne was also a major cause of consultation for men [14].
The diseases also differed between the various age groups, but our results were in accordance with the medical literature. As examples: melanocytic nevus and xerosis appeared to be a significant concern throughout the life spans of the patients [15]; acne was primarily a disease among the teenagers and young adults [14]; melasma was almost exclusively present in the adult group [11]; atopic dermatitis was prominent in children [16]; and benign proliferations (cysts, seborrheic keratosis, and acrochordons), solar lentigo, and onychomycosis occurred most often in adults and older people [12, 17].
We found that TD could triage the patients’ skin conditions without an in-person consultation in 57% of the cases (53% referrals back to the physician and 4% biopsy referrals), leading to an excellent reduction for referrals to an in-person dermatologist visit. This indicates that most skin conditions in our primary care setting are of low complexity and, therefore, SF-TD could be helpful in reducing the number of referrals to in-person dermatologist. This finding reinforces the feasibility and the importance of teledermatology in this context, helping the general physicians to manage such conditions and optimizing medical hours and costs, especially in the public system. This project proved to be a well-defined, structured, scalable process with standardized collection and fairness of care, which might promote the democratization of access to dermatology for underprivileged patients. We believe that this project and its findings could be replicated in wider populations, such as our entire country or even in other countries. In another Brazil's state, Santa Catarina, a SF-TD program has been also in place for 12 years, reducing referrals to in-person dermatologists by 44% [18]. A similar project with 500 patients found 72% of patients with no need for in-person dermatologists [19]. In our project, we had the benefit of directly referring patients for biopsies, which was a new improvement in relation to the previous two studies. One study from Spain showed that two of the main advantages of TD were prioritization in cancer screening and reduction in the number of face-to-face visits, in agreement with our findings [20]. Other study in Cabo Verde, Africa, also reported the benefits of telemedicine, reducing the referrals for in-person consultations by 65% [21]. A systematic review for the use of TD in rural areas showed that it can improve the access to dermatological care, as we believe our study also did [22]. The shortened in the waiting time (a 78% reduction) for patients requiring treatments for potentially lethal diseases, such as melanoma and other severe skin malignancies and diseases, is an important outcome of our work that, as far as we know, has not been evaluated before in previous studies.
The results from the biopsy referrals were as expected: basal cell carcinoma and squamous cell carcinoma were the two most prevalent skin cancers among our studied population and were frequently biopsied before surgery to confirm the diagnostics and choose the best treatments. Melanomas are responsible for less than 5% of all skin cancers, but they are the most significant causes of death among them [23]. The rate of biopsies for our subjects’ melanomas was not as high as the other two skin cancers, maybe because the first treatment choice is an excisional biopsy and not the incisional biopsy, which was offered in this project [24]. Therefore, teledermatologists could have preferred to refer the patients with suspected melanoma for in-person dermatologists, not directly to biopsy. While frequent in our population, actinic keratosis, can be treated by various methods, including physical and chemical treatments, and is commonly not biopsied unless the presence of squamous cell carcinoma is suspected [25]. On the other hand, in our experience in the Brazilian public health system, benign lesions such as melanocytic nevus, seborrheic keratosis, solar lentigo, and acrochordon are seldom biopsied, generally to exclude malign lesions, and epidermoid cysts are usually excised without a prior biopsy.
Referrals for in-person dermatologists were typically for benign proliferations: melanocytic nevus, seborrheic keratosis, cysts, warts, and molluscum. Some of the melanocytic nevus and seborrheic keratosis patients could have received a different referral if dermoscopy had been a part of the project, especially in the more atypical lesions [26].
Warts and molluscum are treated with liquid nitrogen, chemical compounds, or surgery—options that can only be performed during in-presence visits. Dermatologists are trained to palpate cysts and might find teledermatology insufficient in some cases. Patients with actinic keratosis are usually sent to dermatologists to perform dermoscopy for ruling out invasive squamous cell carcinoma and treatment reasons. Most of the cases of acne, vitiligo, psoriasis, and atopic dermatitis sent to dermatologists were probably moderate to severe as the majority was sent back to their general physicians.
The great majority of patients referred back to general physicians were for simple conditions such as xerosis, onychomycosis, melasma, solar lentigos, seborrheic dermatitis, and seborrheic keratosis. With proper orientations and suggestions, the treatments could be managed by them using teledermatology. This differs from a study conducted in Africa, where infectious diseases and eczema were mostly diagnosed, and in Spain, where actinic keratosis, basal cell carcinoma, and melanocytic nevus were the primary causes for dermatologist consultations [17, 27].
It was important for the primary care physicians to know the prevalence of the diseases based on age. This information is especially useful for directing measurements to prevent diseases and orient the population. Emollients and sunblock were the two most frequently prescribed treatments, have few side effects and excellent benefits, potentially preventing many of the prevalent lesions that were diagnosed in this project.
There are limitations to teletriage in dermatology and it is not intended to replace in-person visits with dermatologists. The fact that you can receive multiples photographs of parts of the body and head, and not to examine the person as a whole, makes the diagnosis more challenging. There is also the fear of missing important lesions, such as skin cancer. As our contact was with another physician and not directly to the patient in this project, we expected the physician to follow-up the lesions and request a new evaluation if necessary. Also, some important impressions that would help to corroborate the diagnosis, such as feeling the skin texture cannot be done. However, in a previous study, we have shown that the impossibility to palpate the lesion was classified as a low or medium level of interference in the work of the teledermatologists, and that, after working with SF-TD, they became much more confident in teledermatology [28]. We did not evaluate racial/ethnicity and other socioeconomic characteristics of the population studied, which could provide some valuable information. The project manager had to face a variety of technical issues, such as delay in the process of uploading images and reports made by the teldermatologists; problems with internet connection in the hospitals and missing data or photographs leading to some patients’ recall. The teledermatologists encountered other problems, as blurry pictures, wrong framing of images, and lack of dermoscopy to assist in the diagnosis of many dermatoses.
SF-TD can be an effective tool for reducing referrals of common skin conditions among the general population to dermatologists. It can provide numerous benefits, such as optimizing in-person visits for patients with serious/complex skin conditions, and quickly and conveniently addressing common skin conditions with the primary care physician. This can save resources, working days and patient transportation. Knowledge of the most common skin conditions and treatments encountered in primary care can inform public health policies for the prevention of diseases, and help train physicians on how to address such cases
Funding
None to declare.
Author contributions
Literature search: MGB, EC; Study design: MGB, AS, EC; Data collection: MGB, AS; Data interpretation: MGB, AS, EC; Writing: MGB; Review: MGB, AS and EC.
Data sharing statement
The data will be made available (deidentified participant data) upon request to the authors. MGB and AS had access to the database.
Declaration of Interests
The authors have nothing to disclose.
References
- 1.Heffner V.A., Lyon V.B., Brousseau D.C., Holland K.E., Yen K. Store-and-forward teledermatology versus in-person visits: a comparison in pediatric teledermatology clinic. J Am Acad Dermatol. 2009;60(6):956–961. doi: 10.1016/j.jaad.2008.11.026. [DOI] [PubMed] [Google Scholar]
- 2.O'Connor D.M., Jew O.S., Perman M.J., Castelo-Soccio L.A., Winston F.K., McMahon P.J. Diagnostic accuracy of pediatric teledermatology using parent-submitted photographs: a randomized clinical trial. JAMA Dermatol. 2017;153(12):1243–1248. doi: 10.1001/jamadermatol.2017.4280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.IBGE. Panorama São Paulo. 2013. Accessed 2 February 2019. https://cidades.ibge.gov.br/brasil/sp/sao-paulo/panorama.
- 4.IPEA. 2016. Accessed 2 February 2019. https://www.redebrasilatual.com.br/saude/2016/10/no-estado-de-sao-paulo-25-milhoes-de-pacientes-dependem-do-sus-1016.html
- 5.G1. Prefeitura lança programa de diagnóstico virtual para reduzir espera por consulta dermatológica. 2017. Accessed 17 October 2020. https://g1.globo.com/sao-paulo/noticia/prefeitura-de-sp-lanca-programa-de-diagnostico-virtual-para-reduzir-espera-por-consulta-dermatologica.ghtml
- 6.Paulo PdS. Boletim CEInfo Saúde em Dados. 2018. Accessed 19 November 2019. https://www.prefeitura.sp.gov.br/cidade/secretarias/upload/saude/arquivos/publicacoes/Boletim_CEInfo_Dados_2018.pdf
- 7.Kroemer S., Frühauf J., Campbell T.M. Mobile teledermatology for skin tumour screening: diagnostic accuracy of clinical and dermoscopic image tele-evaluation using cellular phones. Br J Dermatol. 2011;164(5):973–979. doi: 10.1111/j.1365-2133.2011.10208.x. [DOI] [PubMed] [Google Scholar]
- 8.Ferrándiz L., Ruiz-de-Casas A., Martin-Gutierrez F.J. Effect of teledermatology on the prognosis of patients with cutaneous melanoma. Arch Dermatol. 2012;148(9):1025–1028. doi: 10.1001/archdermatol.2012.778. [DOI] [PubMed] [Google Scholar]
- 9.Bruce A.F., Mallow J.A., Theeke L.A. The use of teledermoscopy in the accurate identification of cancerous skin lesions in the adult population: a systematic review. J Telemed Telecare. 2018;24(2):75–83. doi: 10.1177/1357633X16686770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Corrêa MeP. Solar ultraviolet radiation: properties, characteristics and amounts observed in Brazil and South America. An Bras Dermatol. 2015;90(3):297–313. doi: 10.1590/abd1806-4841.20154089. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Handel A.C., Lima P.B., Tonolli V.M., Miot L.D., Miot H.A. Risk factors for facial melasma in women: a case-control study. Br J Dermatol. 2014;171(3):588–594. doi: 10.1111/bjd.13059. [DOI] [PubMed] [Google Scholar]
- 12.Scher R.K., Baran R. Onychomycosis in clinical practice: factors contributing to recurrence. Br J Dermatol. 2003;149(Suppl 65):5–9. doi: 10.1046/j.1365-2133.149.s65.5.x. [DOI] [PubMed] [Google Scholar]
- 13.Holm J.G., Agner T., Clausen M.L., Thomsen S.F. Determinants of disease severity among patients with atopic dermatitis: association with components of the atopic march. Arch Dermatol Res. 2019;311(3):173–182. doi: 10.1007/s00403-019-01895-z. [DOI] [PubMed] [Google Scholar]
- 14.Skroza N., Tolino E., Mambrin A. Adult acne versus adolescent acne: a retrospective study of 1,167 patients. J Clin Aesthet Dermatol. 2018;11(1):21–25. [PMC free article] [PubMed] [Google Scholar]
- 15.Uludağ A., Kılıc S.O., Isık S. Prevalence of skin disorders in primary and secondary school age children in Canakkale, Turkey: a community-based survey. Postepy Dermatol Alergol. 2016;33(3):176–181. doi: 10.5114/ada.2016.60610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weidinger S., Novak N. Atopic dermatitis. Lancet. 2016;387(10023):1109–1122. doi: 10.1016/S0140-6736(15)00149-X. [DOI] [PubMed] [Google Scholar]
- 17.Buendía-Eisman A., Arias-Santiago S., Molina-Leyva A. Outpatient dermatological diagnoses in spain: results from the national DIADERM random sampling project. Actas Dermosifiliogr. 2018;109(5):416–423. doi: 10.1016/j.ad.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 18.von Wangenheim A., Nunes D.H. Creating a web infrastructure for the support of clinical protocols and clinical management: an example in teledermatology. Telemed J E Health. 2019;25(9):781–790. doi: 10.1089/tmj.2018.0197. 09. [DOI] [PubMed] [Google Scholar]
- 19.McAfee J.L., Vij A., Warren C.B. Store-and-forward teledermatology improves care and reduces dermatology referrals from walk-in clinics: a retrospective descriptive study. J Am Acad Dermatol. 2019 doi: 10.1016/j.jaad.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 20.Romero G., de Argila D., Ferrandiz L. Practice models in teledermatology in Spain: longitudinal study, 2009–2014. Actas Dermosifiliogr. 2018 doi: 10.1016/j.ad.2018.03.015. [DOI] [PubMed] [Google Scholar]
- 21.Azevedo V., Latifi R., Parsikia A., Latifi F., Azevedo A. Cabo verde telemedicine program: an update report and analysis of 2,442 teleconsultations. Telemed J E Health. 2020 doi: 10.1089/tmj.2020.0001. [DOI] [PubMed] [Google Scholar]
- 22.Coustasse A., Sarkar R., Abodunde B., Metzger B.J., Slater C.M. Use of teledermatology to improve dermatological access in rural areas. Telemed J E Health. 2019;25(11):1022–1032. doi: 10.1089/tmj.2018.0130. 11. [DOI] [PubMed] [Google Scholar]
- 23.Jemal A., Siegel R., Ward E. Cancer statistics, 2008. CA Cancer J Clin. 2008;58(2):71–96. doi: 10.3322/CA.2007.0010. 2008. [DOI] [PubMed] [Google Scholar]
- 24.Pavri S.N., Clune J., Ariyan S., Narayan D. Malignant melanoma: beyond the basics. Plast Reconstr Surg. 2016;138(2):330e–340e. doi: 10.1097/PRS.0000000000002367. [DOI] [PubMed] [Google Scholar]
- 25.Callen J.P., Bickers D.R., Moy R.L. Actinic keratoses. J Am Acad Dermatol. 1997;36(4):650–653. doi: 10.1016/s0190-9622(97)70265-2. [DOI] [PubMed] [Google Scholar]
- 26.Ferrándiz L., Ojeda-Vila T., Corrales A. Internet-based skin cancer screening using clinical images alone or in conjunction with dermoscopic images: a randomized teledermoscopy trial. J Am Acad Dermatol. 2017;76(4):676–682. doi: 10.1016/j.jaad.2016.10.041. [DOI] [PubMed] [Google Scholar]
- 27.Faye O., Bagayoko C.O., Dicko A. A teledermatology pilot programme for the management of skin diseases in primary health care centres: experiences from a resource-limited country (Mali, West Africa) Trop Med Infect Dis. 2018;3(3) doi: 10.3390/tropicalmed3030088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Giavina Bianchi M., Santos A., Cordioli E. Dermatologists' perceptions on the utility and limitations of teledermatology after examining 55,000 lesions. J Telemed Telecare. 2019 doi: 10.1177/1357633X19864829. 1357633X19864829. [DOI] [PMC free article] [PubMed] [Google Scholar]