Abstract
Purpose
To report an atypical bilateral hypopyon presentation of syphilitic uveitis.
Observations
A 38-year-old male presented with a 2-day history of bilateral progressive visual loss, conjunctival hyperemia, and photophobia. Initial ophthalmologic examination revealed bilateral hypopyon and vitritis that limited the examination of the posterior segment. The physical exam revealed cervical lymphadenopathy, glossal leukoplakia, erythematous maculae on the hard palate, erythematous macular lesions on both palms, onychodystrophy, onycholysis, and psoriasiform plaques on both plantar surfaces, testicular tenderness, and hypopigmented patches on the scrotal and perianal skin. A therapeutic and diagnostic vitrectomy was performed on the right eye, and the intraoperative findings were consistent with severe vitritis and pre-retinal precipitates. The cytopathologic analysis of the right vitreous revealed a mixed inflammatory process composed of lymphocytes, histiocytes, and neutrophils in a proteinaceous background. Laboratory testing revealed positive serum RPR, CSF FTA-Abs and VDRL, and HIV serology. Treatment with a 2-week course of intravenous penicillin G 4 million units every 4 hours and topical corticosteroids resulted in complete resolution of the uveitis.
Conclusions and Importance
Bilateral hypopyon uveitis may be a rare presentation of syphilitic uveitis. As with most forms of uveitis, syphilis should be considered in the differential diagnosis of patients presenting with bilateral hypopyon.
Keywords: Uveitis, Syphilis, Hypopyon, Infectious uveitis, Vitrectomy
1. Introduction
Hypopyon is a relatively uncommon presentation among patients with uveitis.1,2 Its incidence in patients with uveitis is estimated to be 8.57 per 1000 person-years.1 It is characterized by a vigorous inflammatory reaction that leads to white blood cell precipitation in the anterior chamber.2 It is typically present in patients with endophthalmitis, uveitis, or malignancy.2 In patients with noninfectious uveitis, the most common etiologies for a hypopyon upon presentation include Behçet's disease and having the HLA-B27 haplotype.1,2 Patients who develop hypopyon and do not have a recent history of penetrating trauma, infection, or surgery require a complete medical evaluation including particular attention to fever, rashes, oral ulcers, and arthritis.2
The most common initial presentation of ocular syphilis is panuveitis, usually developing during the secondary stage of infection.2, 3, 4 The typical posterior segment involvement includes progressive preretinal yellowish aggregates, theorized to be treponemal bacterial and inflammatory precipitates, with associated retinal, choroidal, and vitreous inflammation.4 The inflammatory process may involve any area of the posterior segment and is characterized by a fast resolution after the initiation of therapy.5
The literature regarding bilateral hypopyon uveitis is exceedingly rare. We herewith report a case of bilateral hypopyon, with severe anterior and intermediate uveitis, as the initial presentation of neurosyphilis.
1.1. Case report
A 38-year-old Hispanic male presented to the emergency room and reported a 2-day history of bilateral progressive visual loss, conjunctival hyperemia, and photophobia. His symptoms began in the right eye (OD) and, within one day, progressed to involve the left eye (OS). The past medical history was remarkable for uncontrolled hypertension and bacterial pharyngitis that required oral antibiotic treatment, which occurred two weeks before the onset of ocular symptoms. The patient denied being sexually active for the prior year but disclosed having sexual intercourse with male and female partners in the past. His toxic habits included tobacco smoking and social ethanol consumption. The family history was remarkable for an unknown type of cancer.
The review of systems was remarkable for general malaise, frontal headaches, sore throat, arthralgias, right-sided testicular pain, lower back pain that worsened with exercise, easy bruising, alopecia, perineal hypopigmentation, a scaly rash in palms and soles, and nail anomalies. The patient denied a history of night sweats, chills, oral or genital ulcers, chest pain, shortness of breath, cough, abdominal pain, changes in stool or voiding patterns, genital discharge, or neurological deficits.
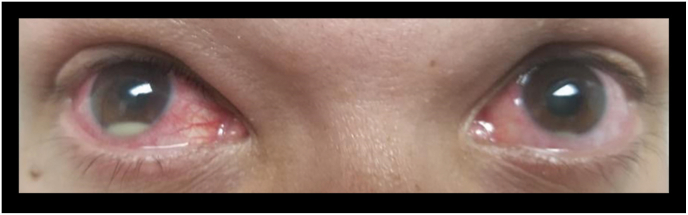
The corrected visual acuity was finger counting at 3 feet OD and 20/40 OS. The intraocular pressure was normal on both eyes (OU). The pupils were round, equally reactive to light, and without evidence of an afferent pupillary defect. A slit-lamp exam revealed bilateral conjunctival injection, non-granulomatous keratic precipitates, 4+ anterior chamber cells, and hypopyon (Fig. 1). The fundus examination revealed 4+ vitritis OD and 3+ vitritis OS. B-scan ultrasound showed bilateral vitreous opacities without any evidence of choroidal masses or retinal detachment.
Fig. 1.
A color photograph of the right and left eye upon presentation, revealing the presence of conjunctival injection and hypopyon on both eyes. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
The physical examination was remarkable for moth-eaten alopecia, glossal leukoplakia, and erythematous maculae on the hard palate, erythematous macular lesions on both palms, onychodystrophy, onycholysis, and longitudinal nail striae (Fig. 2 A, B, C, and D). Psoriasiform plaques were present in both plantar surfaces. (Fig. 2E). In addition, hypopigmented patches were present in the scrotal and the perianal skin. (Fig. 2F and G). The patient had vertebral tenderness at the L4-L5-Sacral region and a positive FABER test for sacroiliac pain bilaterally. The neurological examination was unremarkable.
Fig. 2.
Color photographs of the integumentary system and oral mucosa upon presentation revealing various clinical manifestations of syphilis: A. Moth-eaten alopecia. B. Glossal leukoplakia and erythematous maculae on the hard palate. C. Erythematous macular lesions on both palms. D. Onychodystrophy, onycholysis, and longitudinal nail striae. E. Psoriasiform plaques in plantar surfaces. Hypopigmented patches in scrotal and perianal skin, F and G, respectively. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
As the differential diagnosis of bilateral hypopyon with severe vitritis includes infectious endophthalmitis, a bilateral vitreous tap, and injection of vancomycin, ceftazidime, and voriconazole was done. Additionally, hourly topical prednisolone acetate 1%, atropine sulfate 1%, as well as systemic therapy with oral indomethacin and intravenous acyclovir was begun as the initial empirical treatment.
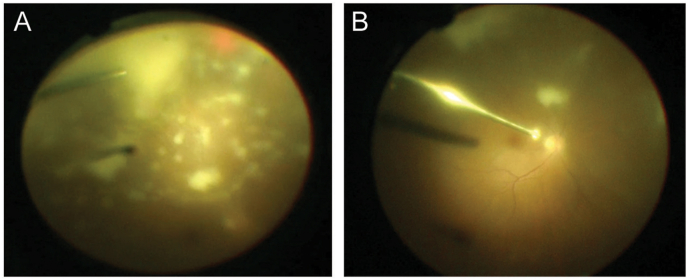
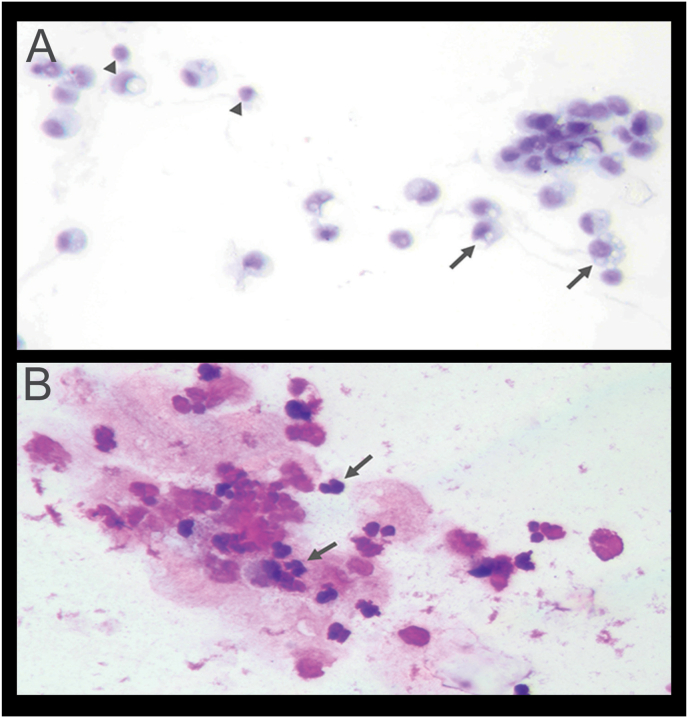
Following a 3-days course of the initial therapy, the fundus’ view remained extremely poor for both eyes; therefore, a diagnostic and therapeutic pars plana vitrectomy was performed on the right eye. The intraoperative findings were consistent with severe vitritis with multiple preretinal precipitates (Fig. 3A and B). A total of 3 mL of vitreous fluid was sent for cytological evaluation. Direct smears were stained with Romanowsky-type (three-step stain) as well as Papanicolaou stain. Cytopathologic findings were negative for malignant cells. Smears showed a mixed (acute and chronic) inflammatory process composed of lymphocytes, histiocytes, and neutrophils in a proteinaceous background. (Fig. 4A and B).
Fig. 3.
Superior (A) and central (B) intraoperative views of the right fundus during a pars plana vitrectomy revealing dense vitritis and multiple round yellow preretinal precipitates, the later characteristic of syphilitic uveitis. . (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Fig. 4.
Vitreous fluid cytology. A. Presence of lymphocytes (arrowheads) and histiocytes showing abundant vacuolated (foamy) cytoplasm (arrows). Romanowsky stain, X400. B. Presence of neutrophils in a proteinaceous background. Romanowsky stain, X400.
Laboratory work-up revealed a positive serum rapid plasma reagin (RPR). Fluorescent treponemal antibody absorption (FTA-ABS) test and venereal disease research laboratory (VDRL) test of the cerebrospinal fluid sample were positive, confirming a diagnosis of neurosyphilis. Human immunodeficiency virus (HIV) testing was also positive, with a CD3+ CD4+ cell count of 361/mm3. Testing for HLA-B27 haplotype, aqueous humor polymerase chain reaction (PCR) for herpes simplex virus I and II, and blood cultures were all negative.
The patient received treatment with intravenous penicillin G, 4 million units every 4 hours. Soon after the treatment initiation with intravenous penicillin G, the patient began to show significant improvement, followed by the complete resolution of the hypopyon, the vitritis, and the palmoplantar rash. After one week of such antibiotic therapy, the best-corrected visual acuity had improved to 20/70 OD and 20/30 OS. On the six-month follow-up visit, his uveitis remained in remission, and his best-corrected visual acuity measured 20/25 OD and 20/20 OS.
2. Discussion
To our knowledge, this is the first case of secondary syphilis manifesting as bilateral hypopyon. However, hypopyon is not an uncommon finding in luetic uveitis, with a prevalence of 6% of involved eyes in some recent series.6 Previous studies by Davis et al. have described distinctive clinical patterns of posterior segment involvement for syphilitic uveitis, including the presence of small, creamy white superficial retinal precipitates that may migrate over areas of retinitis.7 It is possible that our patient may have had a more severe presentation of syphilitic uveitis due to his untreated HIV infection.8
The role of pars plana vitrectomy in advanced cases of uveitis continues to evolve. Recent studies have shown positive outcomes after early vitrectomy in the management of intermediate and posterior uveitis.9, 10, 11 A pars plana vitrectomy may be beneficial for managing complex posterior segment involvement in select cases of syphilitic uveitis.12 It allows a multipronged approach, including targeted vitreous sampling, visualization of retinal lesions, clearing of the visual axis, debulking of the inflammatory mediators, and identifying retinal tears or detachments.13 For our case, the vitrectomy also helped us rule out (and potentially treat) a fungal infection, which is known to represent approximately one-fifth of positive endophthalmitis isolates in Puerto Rico.14,15
A limited number of therapeutic vitrectomy cases have been reported in patients with syphilitic uveitis, usually in the setting of a retinal detachment.12 A case series published by Queiroz et al. in 2016 reported 4 patients with syphilitic posterior uveitis who developed rapidly progressive combined tractional and rhegmatogenous retinal detachments with proliferative vitreoretinopathy during or shortly after antibiotic therapy.12 Histopathologic analysis of the removed fibroglial membranes revealed a dense plasmacytic infiltrate.12 These cases were also associated with the prior use of corticosteroids, concomitant HIV infection, and young age.12 Queiroz et al. hypothesized that a Jarisch-Herxheimer reaction may explain the progressive proliferative vitreoretinopathy.12 It is possible that starting antiretroviral agents and penicillin G concomitantly may increase the risk of a Jarisch-Herxheimer reaction due to the immune reconstitution inflammatory syndrome.12
A retrospective cohort study by Haug et al. described 11 cases of rhegmatogenous retinal detachments weeks after therapy for syphilitic panuveitis.16 Similarly, Pournaras et al. reported a patient who developed bilateral giant retinal tears two weeks after therapy for ocular syphilis.17 It is possible that vitreous contraction after therapy may lead to delayed retinal tears and detachment.16 The authors suggested that systemic steroids may be considered to minimize the inflammatory reaction associated with a quick resolution of the infection after the initiation of systemic antibiotics.17 However, the efficacy of systemic corticosteroids in this setting remains unclear.12,17 It is conceivable that in our patient, the early vitrectomy and perhaps the treatment with oral indomethacin, by means of reducing the inflammatory response, may have decreased his risk of suffering a retinal detachment.12
3. Conclusion
Bilateral hypopyon may be a rare initial presentation of neurosyphilis and should alert the physician about possible HIV co-infection. Pars plana vitrectomy allows a multipronged management approach that may be performed in select advanced cases of syphilitic uveitis with posterior segment involvement. Prospective studies are needed to determine the safety and efficacy of pars plana vitrectomy in syphilitic uveitis.
Patient consent
Written consent to publish the case report was obtained. This report does not contain any personal information that could lead to the identification of the patient.
Funding
No funding or grant support was used for this case report.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The following authors have no financial disclosures: MG, NR, MS, SC, MM, VV, AO.
Acknowledgments
The authors would like to acknowledge Dr. Luz D. Figueroa, Professor, and Chairman of the University of Puerto Rico Department of Dermatology, for her contributions, which enlightened our understanding of the dermatological manifestations of syphilis in this patient.
Contributor Information
Monica P. Gonzalez Collazo, Email: monica.gonzalez9@upr.edu.
Nicole P. Rebollo Rodriguez, Email: nicole.rebollo@upr.edu.
Marely Santiago-Vazquez, Email: marely.santiago@upr.edu.
Susanne M. Crespo-Ramos, Email: susanne.crespo@upr.edu.
Maria J. Marcos-Martinez, Email: maria.marcos@upr.edu.
Víctor M. Villegas, Email: victor.villegas@upr.edu.
Armando L. Oliver, Email: armando.oliver@upr.edu.
References
- 1.Zaidi A.A., Ying G.-S., Daniel E. Hypopyon in patients with uveitis. Ophthalmology. 2010;117(2):366–372. doi: 10.1016/j.ophtha.2009.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ramsay A., Lightman S. Hypopyon uveitis. Surv Ophthalmol. 2001;46(1):1–18. doi: 10.1016/s0039-6257(01)00231-4. [DOI] [PubMed] [Google Scholar]
- 3.Cather J.C., Cather J.C., Menter M.A. Psoriasiform lesions on trunk and palms. Baylor Univ Med Cent Proc. 2003;16(2):236–238. doi: 10.1080/08998280.2003.11927908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dylewski J., Duong M. The rash of secondary syphilis. Can Med Assoc J. 2008;177(8):8–10. doi: 10.1503/cmaj.060665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Center for Disease Control and Prevention. Syphilis Surveillance Supplement 2013 – 2017. Atlanta: U.S. Department of Health and Human Services.
- 6.Zhang X., Du Q., Ma F., Lu Y., Wang M., Li X. Characteristics of syphilitic uveitis in northern China. BMC Ophthalmol. 2017;17(1):95. doi: 10.1186/s12886-017-0491-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davis J. Ocular syphilis. Curr Opin Ophthalmol. 2014;25(6):513–518. doi: 10.1097/ICU.0000000000000099. [DOI] [PubMed] [Google Scholar]
- 8.Moramarco A., Mallone F., Pirraglia M.P. Clinical features of ocular syphilis: a retrospective clinical study in an Italian referral centre. Semin Ophthalmol. 2020;35(1):50–55. doi: 10.1080/08820538.2020.1723651. [DOI] [PubMed] [Google Scholar]
- 9.Bonfioli A.A., Damico F.M., Curi A.L.L., Orefice F. Intermediate uveitis. Semin Ophthalmol. 2005;20(3):147–154. doi: 10.1080/08820530500232035. [DOI] [PubMed] [Google Scholar]
- 10.Shin Y.U., Shin J.Y., Ma D.J., Cho H., Yu H.G. Preoperative inflammatory control and surgical outcome of vitrectomy in intermediate uveitis. J Ophthalmol. 2017;2017 doi: 10.1155/2017/5946240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stavrou P., Baltatzis S., Letko E., Samson C.M., Christen W., Foster C.S. Pars plana vitrectomy in patients with intermediate uveitis. Ocul Immunol Inflamm. 2001;9(3):141–151. doi: 10.1076/ocii.9.3.141.3965. [DOI] [PubMed] [Google Scholar]
- 12.Queiroz R. de P., Diniz A.V., Vasconcelos-Santos D.V. Fulminant proliferative vitreoretinopathy in syphilitic uveitis. J Ophthalmic Inflamm Infect. 2016;6(1):1–6. doi: 10.1186/s12348-016-0075-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Verbraeken H. Diagnostic vitrectomy and uveitis. Graefe’s Arch Clin Exp Ophthalmol. 1996;234(1):S2–S7. doi: 10.1097/00004397-199903910-00020. [DOI] [PubMed] [Google Scholar]
- 14.del Pilar Fernández M., Villegas V.M., Oliver A.L. Vitreous cultures and antibiotic analysis in Puerto Rican endophthalmitis patients. P R Health Sci J. 2011;30(4) [PubMed] [Google Scholar]
- 15.Chee Y.E., Eliott D. The role of vitrectomy in the management of fungal endophthalmitis. Semin Ophthalmol. 2017;32(1):29–35. doi: 10.1080/08820538.2016.1228396. [DOI] [PubMed] [Google Scholar]
- 16.Haug S.J., Takakura A., Jumper J.M. Rhegmatogenous retinal detachment in patients with acute syphilitic panuveitis. Ocul Immunol Inflamm. 2016;24(1):69–76. doi: 10.3109/09273948.2014.925122. [DOI] [PubMed] [Google Scholar]
- 17.Pournaras J.A.C., Laffitte E., Guex-Crosier Y. Bilateral giant retinal tear and retinal detachment in a young emmetropic man after jarish-herxheimer reaction in ocular syphilis. Klin Monbl Augenheilkd. 2006;223(5):447–449. doi: 10.1055/s-2006-926579. [DOI] [PubMed] [Google Scholar]