Abstract
Rare vascular anomaly, the persistent sciatic artery (PSA) has an extremely low incidence, likely 0.04%-0.06%. This vessel is prone to thrombosis, distal thromboembolization, rupture, and aneurysmal formation, while its symptoms can vary considerably, from completely asymptomatic pictures to cases with pain, claudication or ischemia of the lower limbs.
It is essential to diagnose this anomaly in time, in order to avoid dangerous complications for the patient's life. The main methods of diagnosis are given by vascular ultrasound, CT, or MRI.
Here we present a case of a bilateral PSA diagnosed in a 77-year-old woman as an incidental finding in angio-CT of the lower limbs.
Keywords: Persistent sciatic artery (PSA), Congenital abnormalities, Rare disease, Sciatica, Aneurysm
Introduction
Rare vascular anomaly, the persistency of sciatic artery (PSA) develops by the absence of regression of the embryonic dorsal axial artery associated with a hypoplastic superficial femoral artery [1,2].
This anomaly seems to develop during embryonic life, due to a lack of redirection of the blood flow from the PSA to the superficial femoral artery which, usually by the third month of development, deals with the blood circulation of the lower limbs [3].
It has an extremely low incidence, likely 0.04%-0.06%, with no differences between men or women, and it is bilateral in 30% of cases [2,4].
This vessel tends to thrombosis, distal thromboembolization, rupture, and aneurysmal formation, while its symptoms can vary considerably, from completely asymptomatic pictures to cases with pain, claudication, or ischemia of the lower limbs [2,5].
A pulsating buttock mass can be associated with PSA, due to its location adjacent to the sciatic nerve, and a common complication is the secondary pulsating nerve compression due to the nature of vessel, that could mimic a sciatica, making the anomaly diagnosis difficult [5].
It is essential to diagnose this anomaly in time, in order to avoid dangerous complications for the patient's life. The main methods of diagnosis are given by vascular ultrasound, CT, or MRI [2,4].
Here we present a case of bilateral PSA CT-diagnosed in a woman as an incidental finding.
Case
A 77-year-old female patient known for long story hypertension and anxiety syndrome, in treatment with benzodiazepines, presented in our structure with a feeling of discomfort in the lower limbs that induced restlessness. With the employed therapy the patient reported benefit that was lost after a month.
On physical examination, the patient did not complain of claudication of the lower limbs, and she had valid popliteal and tibial pulsations with very hot limbs and absence of skin ulcers.
Revaluated at divisional surgery, the established treatment was a therapy with the addition of citalopram, initially not tolerated but accepted with slow titration.
Due to intractable symptoms, even an EMG was performed, which gave negative results for polyneuropathy or root pain.
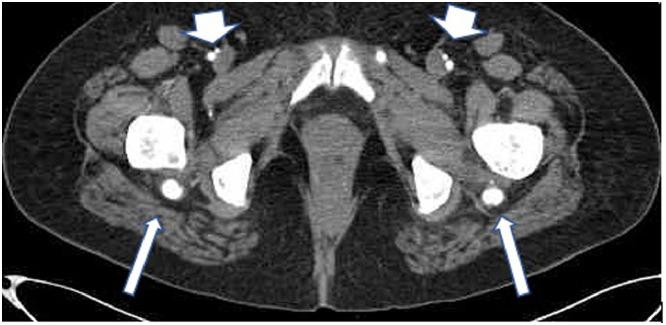
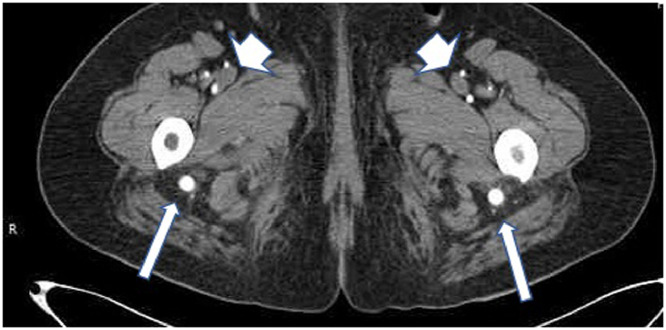
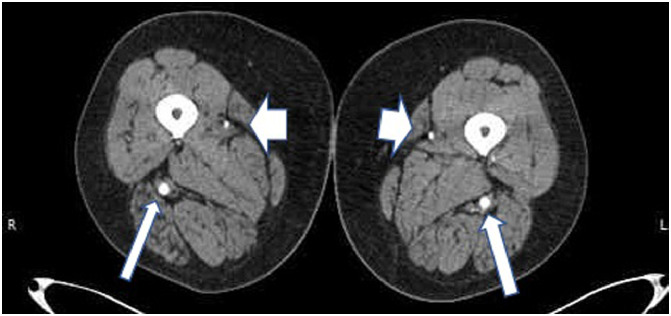
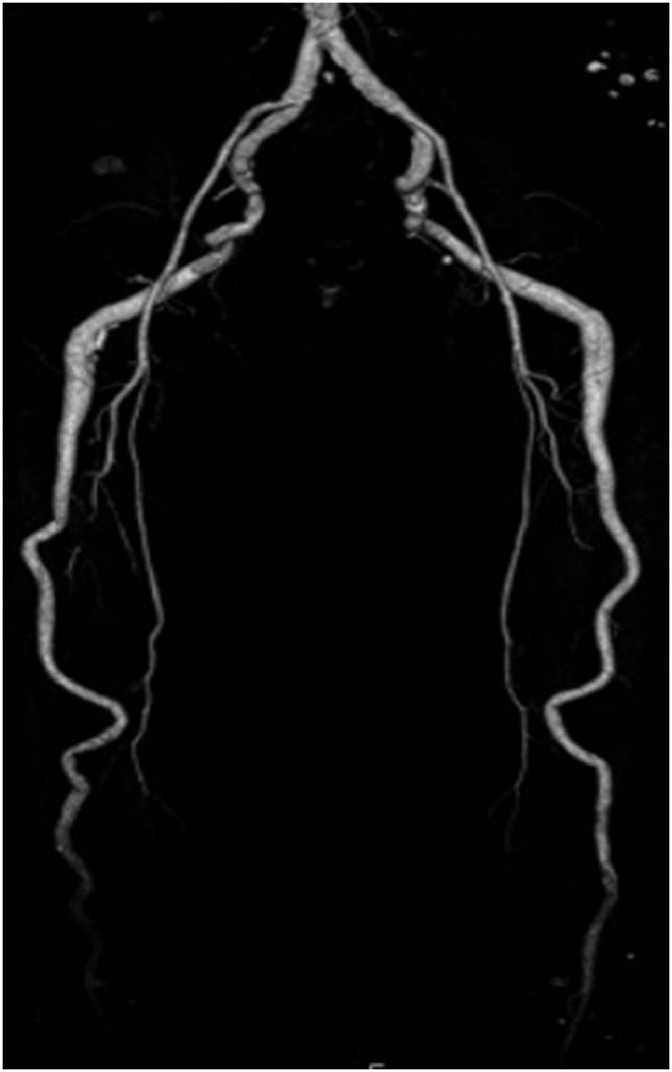
A contrast CT-abdomen was performed thereafter, which showed in its lower scans bilateral and symmetrical hypertrophy of an arterial vessel, initially described as posterior gluteal arteries (Fig. 1). Subsequently, an angio-CT of the lower limbs was performed, which demonstrated the presence of an hypogastric artery with increased calibre and an anomalous course within the posterior compartment of the thigh up to the distal III, where it continued with the popliteal artery (Fig. 2, Fig. 3, Fig. 4). Furthermore, the common, deep and superficial femoral arteries had a considerably reduced calibre, with the emission of exclusively vascular branches (Figs. 5 and 6).
Fig. 1.
Axial CT angiogram demonstrates hypertrophic bilateral persistent sciatic arteries (arrows), hypo trophic femoral arteries (arrowhead).
Fig. 2.
Axial CT angiogram demonstrates hypertrophic bilateral persistent sciatic arteries (arrows), hypo trophic femoral arteries (arrowhead).
Fig. 3.
Axial CT angiogram demonstrates hypertrophic bilateral persistent sciatic arteries (arrows), hypo trophic femoral arteries (arrowhead).
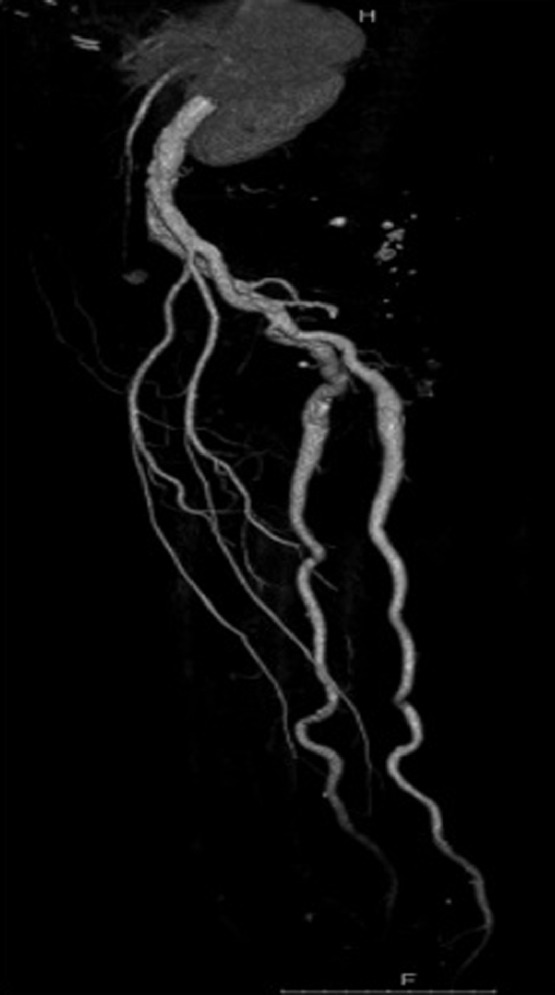
Fig. 4.

Posterior view of 3D CT reconstruction of the arteries from the hip to the thigh, that demonstrates the hypertrophy of SA.
Fig. 5.
Anterior view of 3D CT reconstruction of the arteries from the hip to the thigh.
Fig. 6.
Lateral view of 3D CT reconstruction of the arteries from the hip to the thigh.
The images were eventually evaluated by a radiologist with 20 years of experience who placed the diagnosis of PSA (Figs. 7 and 8).
Fig. 7.

Coronal view of 3D CT reconstruction of the arteries of the leg.
Fig. 8.
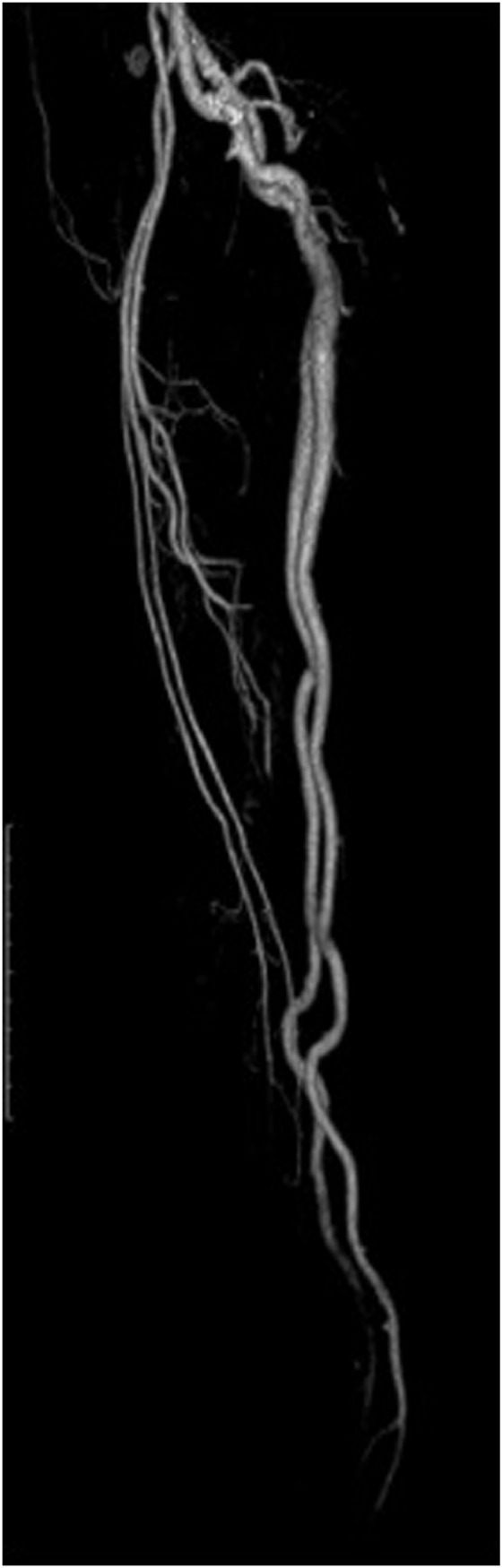
Another Lateral view of 3D CT reconstruction of the arteries from the hip to the thigh, with a lateral view that focus on the hypotrophy of femoral vascular arch.
After the diagnosis, the patient was not subjected to further treatments in our facility, due to the absence of aneurysms, and currently she has not performed any vascular surgery for her anomaly.
Discussion
The sciatic artery (SA) usually presents itself as a branch of the umbilical artery, providing the main vascularization of the lower limbs in the embryo until the third month. In fact, starting from this date, the SA begins to regress for the growth of the femoral artery system. During the embryonal life, the blood flow that supplies the popliteal artery derives from both the SA and the femoral artery system [1,3,6]. Some remnants of the SA persist in the adult, giving rise to the lower gluteal artery and peroneal arteries [1,7].
If it does not regress and persists into adulthood, the SA appears to continue in the internal iliac artery. The SA then follows the same path as the lower gluteal artery, runs deeply to the gluteus maximus muscle, runs posterior to the greater trochanter of the femur and finally runs along the posterior face of the large adductor muscle up to the popliteal fossa where it continues with the popliteal artery [3,7].
SA can establish close relationships with the sciatic nerve or with the posterior cutaneous nerve, resulting in symptoms of compression-related neuropathy due to the pulsating nature of the arterial vessel, which can mimic sciatica pain attacks [5].
In most cases, the PSA is complete (63%-79%), and when it happens, hypoplasia of the arterial femoral system occurs, while the SA goes from the internal iliac artery to the popliteal [2,4]. In the incomplete type, the PSA is discontinuous along its embryonic path, while the femoral arterial system supplies the dominant arterial supply to the lower limbs [2,8,9]. Recently some studies have proposed classification systems of the PSA for both diagnostic and surgical purposes, based on the persistent or absent femoral arterial system [10,11].
On physical examination, the PSA should be suspected in the absence of a femoral pulse, associated with the presence of popliteal and / or pedal pulses (Cowie's sign) [1,2].
The most common complication of PSA is the fusiform aneurysmal degeneration, present in 48% of cases. It is hypothesized that the continuous compression of the SA on the sacrospinous ligament, the pyriform muscle and the hip may induce the formation of the aneurysm, probably due to a susceptibility of the vessel resulting from the reduced amount of elastic fibers in its wall. Some forms of presentation are given by arterial insufficiency resulting from thrombosis of aneurysms or distal embolization from mural thrombi, while larger aneurysms that do not break can determine neurological symptoms due to compression of the sciatic nerve [1,7,9].
Even in hip surgery there may be risks from PSA. In fact, if a posterior approach to the hip joint was made, the SA could be damaged, resulting in peripheral embolization or wall rupture, threatening the patient's life [3,12].
For PSA diagnosis and evaluation complications, can be used angiography, ultrasound, CT, and MRI. Each of these diagnostic techniques are based on the identification of aberrant vessels along the posterolateral walls of the gluteal muscles and/or on degenerations of the arterial system of the hamstrings, correlated by a compatible clinic [2,4].
PSA treatment will depend on the presentation and urgency of the clinical picture. The asymptomatic ones should be monitored with physical examination and noninvasive SA imaging, with surgical intervention in case of aneurysmal dilatation presented at imaging. In fact, the treatment of the aneurysms is fundamental to prevent its embolization or its rupture. These treatments can include simple ligations of the aneurysm, in the incomplete form, up to revascularization techniques for complete ones, such as bypasses, angioplasty or stents, in order to guarantee optimal perfusion of the limb [4,7].
In conclusion, the PSA is a rare vascular abnormality that must be followed and assumed for surgical interventions of patients, due to its potential life-threatening complications.
Consent
Informed consent has been obtained by the patient in order to perform CT scan and subsequent clinical examination according internal hospital guide lines.
Code availability
Not available.
Footnotes
Competing Interests: Each author declares that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
Funding: Not available.
References
- 1.Paraskevas G., Papaziogas B., Gigis J., Mylonas A., Gigis P. The persistence of the sciatic artery. Folia Morphol (Warsz) 2004;63(4):515–518. [PubMed] [Google Scholar]
- 2.van Hooft I.M., Zeebregts C.J., van Sterkenburg S.M.M., de Vries W.R., Reijnen M.M.P.J. The persistent sciatic artery. Eur J Vasc Endovasc Surg. 2009 doi: 10.1016/j.ejvs.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 3.Mandell V.S., Jaques P.F., Delany D.J., Oberheu V. Persistent sciatic artery: clinical, embryologic, and angiographic features. Am J Roentgenol. 1985 doi: 10.2214/ajr.144.2.245. [DOI] [PubMed] [Google Scholar]
- 4.Santaolalla V. Persistent sciatic artery. Ann Vasc Surg. 2010 doi: 10.1016/j.avsg.2009.08.020. [DOI] [PubMed] [Google Scholar]
- 5.Abdallah M., Gashti M., McEvenue G.M. Persistent sciatic artery aneurysm presenting with limb-threatening ischemia: a case report and review. Vasc Dis Manag. 2010;7(3):E82–E85. [Google Scholar]
- 6.Papon X., Picquet J., Fournier H.D., Enon B., Mercier P. Persistent sciatic artery: report of an original aneurysm-associated case. Surg Radiol Anat. 1999 doi: 10.1007/s00276-999-0151-5. [DOI] [PubMed] [Google Scholar]
- 7.Brantley S.K., Rigdon E.E., Raju S. Persistent sciatic artery: embryology, pathology, and treatment. J Vasc Surg. 1993 doi: 10.1016/0741-5214(93)90604-K. [DOI] [PubMed] [Google Scholar]
- 8.Martin K.W., Hyde G.L., McCready R.A., Hull D.A. Sciatic artery aneurysms: report of three cases and review of the literature. J Vasc Surg. 1986 doi: 10.1016/0741-5214(86)90232-6. [DOI] [PubMed] [Google Scholar]
- 9.Williams L.R., Flanigan D.P., O'Connor R.J.A., Schuler J.J. Persistent sciatic artery. Clinical aspects and operative management. Am J Surg. 1983 doi: 10.1016/0002-9610(83)90122-8. [DOI] [PubMed] [Google Scholar]
- 10.Pillet J., Albaret P., Toulemonde J.L., Cronier P., Raimbeau G., Chevalier J.M. [Ischio-popliteal artery trunk, persistence of the axial artery] Bull Assoc Anat (Nancy) 1980;64(184):97–110. [PubMed] [Google Scholar]
- 11.Gauffre S., Lasjaunias P., Zerah M. Sciatic artery: a case, review of literature and attempt of systemization. Surg Radiol Anat. 1994 doi: 10.1007/BF01627932. [DOI] [PubMed] [Google Scholar]
- 12.Lindenbaum B., Sanders R.J., Steele G. Persistent sciatic artery and sciatic artery aneurysm: a hazard in hip surgery. Clin Orthop Relat Res. 1978 doi: 10.1097/00003086-197805000-00015. [DOI] [PubMed] [Google Scholar]