Abstract
Background
Chronic Respiratory Diseases (CRDs) in Asian countries are a growing concern in terms of morbidity and mortality. However, a systematic understanding of the increasing age-adjusted mortality rate of chronic respiratory disease (CRD) and its associated factors is not readily available for many Asian countries. We aimed to determine country-level factors affecting CRD mortality using a panel error correction model.
Methods
Based on data from the Global Burden of Disease Study 2017, we estimated the trends and distribution of CRD mortality for selected Asian countries from 2010 to 2017. Furthermore, we evaluated the relationship between CRD mortality and Gross Domestic Product (GDP) per capita, average years of schooling, urbanization, and pollutant emission (PM2.5 concentration) using a fixed-effect model. We corrected the estimates for heteroscedasticity and autocorrelation through Prais-Winsten adjustment along with robust standard error.
Results
Between 2010 and 2017, approximately 21.4 million people died from chronic respiratory diseases in the countries studied. Age-standardized crude mortality rate from CRDs in the period had minimum and maximum values of 8.19 (Singapore in 2016) and 155.42 (North Korea in 2010) per 100,000 population, respectively. The coefficients corrected for autocorrelation and heteroskedasticity based on the final model of our study (Prais-Winsten), showed that all explanatory variables were statistically significant (p < 0.001). The model shows that the 1% increase in GDP per capita results in a 20% increase (0.203) in the CRD mortality rate and that a higher concentration of air pollution is also positively associated with the CRD deaths (0.00869). However, an extra year of schooling reduces the mortality rate by 4.79% (− 0.0479). Further, rate of urbanization is negatively associated with the CRD death rate (− 0.0252).
Conclusions
Our results indicate that both socioeconomic and environmental factors impact CRD mortality rates. Mortality due to CRD increases with rising GDP per capita and decreases with the percentage of the total population residing in urban areas. Further, mortality increases with greater exposure to PM2.5. Also, higher years of schooling mitigate rising CRD mortality rates, showing that education can act as a safety net against CRD mortality. These results are an outcome of sequential adjustments in the final model specification to correct for heteroscedasticity and autocorrelation.
Keywords: Mortality, Chronic respiratory diseases, Associated factors, Asian countries, Global burden of disease study 2017, Panel error correction model
Background
The growth of chronic respiratory diseases (CRDs) in recent decades has changed morbidity and mortality trends and has become a problem worldwide [1]. CRDs represent a group of diseases characterised by abnormal conditions of the respiratory system, including chronic obstructive pulmonary disease (COPD) and asthma, the most common, as well as pneumoconiosis, interstitial lung disease, and pulmonary sarcoidosis, which affect people of all ages. Among the main risk factors identified for CRDs are tobacco smoking, air pollution (indoor and outdoor), allergens, and occupational risks and vulnerability [2].
In the last twenty-seven years of available data, although the percentage has remained stable at around 7% in relation to all causes of death, the estimated number of people who died annually from CRDs jumped from 3,317,205 in 1990 to 3,914,196 in 2017, an increase of ~ 18%. The majority of CRD deaths in this period occurred on the Asian continent, which in 2017 recorded approximately 75% of all cases, a slightly lower percentage than in 1990 (~ 77%) [3]. Therefore, and considering that Asia represents approximately 60% of the world’s population, CRDs constitute a serious public health problem that strongly affects countries in the region [4].
In recent years, Asia has seen a booming economy, an unprecedented amount of rural to urban migration, and rapidly growing cities accompanied by increasing exposure to environmental pollutants. In addition, other structural issues have created a huge threat to the ecological environment for healthy living, which contributes to a rising burden of disease, particularly CRDs, and, consequently, leads to huge economic loss [5–7].
To identify interventions, plan priorities, and strategically allocate resources to reduce the burden of disease, it is essential to understand the factors that drive CRD-related mortality. In Asia, as well as elsewhere, studies of CRD-related mortality are limited either by data or mainly confined to individual countries. Moreover, studies are focused on a specific cause, such as COPD, asthma or tuberculosis [8–15]. According to Soriano et al. [16], there is a lack of studies summarizing the burden of disease or mortality of all CRDs worldwide over an extended period. Added to this, there are still known and unknown aspects related to risk factors. While smoking (including second-hand smoke), air pollution (indoor and outdoor), allergens, and occupational risks are well-known and widely studied risk factors for chronic respiratory diseases [13, 16], socioeconomic factors, such as gross domestic product (GDP) per capita and schooling, still have a literature gap capable of contributing and advancing the understanding of CRDs. Finally, there is a paucity of evidence regarding the various levels of factors that affect CRD mortality rates, as well as cross-country studies that fail to acknowledge the challenges of statistical modeling, such as serial autocorrelation and heteroskedasticity. However, measurement outcomes from broad disease categories reflect the responsiveness of healthcare system in a country and serve as an important starting point [17].
With this in mind, the goal of this study is twofold. Substantively, we aim to to evaluate the relationship between CRD mortality rates and some possible predictor variables across Asian countries. Methodologically, we to try to develop the rationale for the model selection in cross-country panel data, test the plausible violations of assumptions for regression, and correct the estimates of coefficients for the same. The estimates obtained were corrected for non-compliance of assumptions in linear models to answer the following research questions: (1) What are the pattern, dynamics and trends of CRDs mortality in the period? (2) Is there an association between age-standardized crude mortality rate from chronic respiratory diseases and any of the explanatory variables studied? (3) What are the possible limitations in statistical models used in cross-country panel data and what are the ways to address them?
Methods
Data and measures
The country-level age-standardized crude mortality rate from chronic respiratory diseases (CMRCRD) is the dependent variable of this study and can be calculated as follows:
| 1 |
where is the age-specific mortality rate from chronic respiratory diseases in each age group i and country j, and is the proportion of the population in each age group i of the standard population, which, in this study, is the world population in 2010. Data, which is cause-specific as well as age-specific (in 5-year age groups up to 95 years or more), were obtained from the Global Burden of Disease (GBD) Study 2017 [3], coordinated by the Institute for Health Metrics and Evaluation (IHME) and publicly available online.
The GBD study was created to provide comprehensive and comparable global health metrics. Estimates of cause-specific mortality, burden of diseases, injuries, and risk factors are reported by year (1990–2017), location (195 countries and territories, and at the subnational level for a subset of countries), age, and sex. The GBD study also supplied the population estimates used in this paper. Data sources used to produce these estimates came from 1257 census and 761 population registry location-years.
The explanatory variables of the study are gross domestic product (GDP) per capita, schooling, urbanization, and air pollution.
We obtained the gross domestic product per capita (GDP per capita) and the expected years of schooling from the United Nations Development Programme [18]. The first is measured in purchasing power parity (2011 PPP $) as result of GDP divided by the total population in the same year. This is one of the most widely used socioeconomic predictors of mortality / health, and this relationship has been widely discussed in the literature [19–27]. The second refers to the number of years of schooling that a child of school entrance age (under age 7) can expect to receive if prevailing patterns of age-specific enrolment rates persist throughout the child’s life. A vast literature has persistently shown the inverse association between educational attainment and mortality / morbidity, almost invariably indicating that individuals with better education are healthier and live longer [25, 28–33].
Annual percentage of population at mid-year residing in urban areas was obtained from the United Nations Department of Economic and Social Affairs [34]. Urbanization is an important factor in mortality and health, as it is associated with a more sedentary lifestyle, a diet richer in salt, sugar, and fat, and tobacco addiction. Added to this is the problem of air pollution, one of the main problems observed in urban areas, with adverse health implications resulting in particular from the combustion of fossil fuels from vehicular traffic [25, 35–38]. However, higher urbanization leads to better access to modern health facilities owing to concentration of facilities in urban areas [39].
Lastly, population-weighted exposure to ambient PM2.5 pollution comes from the State of Global Air report [40]. This variable is defined as the average level of exposure of a country’s population (in both urban and rural areas) to mean annual concentrations of suspended particles measuring less than 2.5 μm in aerodynamic diameter (μg/m3). These particles are capable of penetrating deep into the respiratory tract and causing severe health damage. It has been well established in the literature that air pollution is one of the most important risk factors for chronic respiratory disease [41–46].
Level of analysis
The analysis in the study is based on information from 29 Asian countries, including Iran (Western Asia); Afghanistan, Kazakhstan, Kyrgyzstan, Tajikistan, Turkmenistan, and Uzbekistan (Central Asia); Bangladesh, Bhutan, India, Nepal, and Pakistan (Southern Asia); China, Japan, Mongolia, North Korea, and South Korea (Eastern Asia); and Brunei, Cambodia, Indonesia, Laos, Malaysia, Maldives, Myanmar, Philippines, Singapore, Sri Lanka, Thailand, and Vietnam (Southeastern Asia). That these countries cover and represent huge socioeconomic, demographic, geographic, environmental, and epidemiological diversity is well known. However, Asia is a region where CRD mortality may be especially problematic due to the stages of growth and development that many countries have experienced, particularly from the second half of the twentieth century.
For purposes of analysis, we use a time series from 2010 to 2017. Deaths from chronic respiratory diseases and population were organized by age (in 5-year age groups up to 95 years or more). We then calculate age-standardized death rates per 100,000 for each country using the world population in 2010 as the standard.
Methodology
This section describes the econometric framework used to establish the relationship between chronic respiratory diseases mortality rates and set of covariates described earlier. We used the log-linear functional form to estimate all regression equations. Equation 1 provides standard formulation of the model:
| 2 |
where yct is log of age-standardized crude mortality rate from chronic respiratory diseases (CMRCRD), zct is log of the explanatory variable (GDP per capita or average years of schooling or rate of urbanization or concentration of particulate matters), and X′ct comprises the other covariates as the linear function for country c and time t. σc denotes the country effect, where its randomness is tested to identify the true model. The logarithmic transformation of CRD mortality rates and GDP per capita is based on the assessment of SD within and between. Due to the inconsistent scale of variation of the variables, it was necessary to make the log transformation of high-variance variables. Therefore, to align the scale of variation in the model, we logarithmically transformed the previously mentioned variables. Apart from the mathematical transformation, we provide the rationale for model selection below.
Based on the nature of σc, three prominent models used in the panel data setup were tested: pooled, fixed, and random effect models [47]. Model selection was based on three criteria: goodness of fit, significant difference between countries, and exogeneity of the cofactors.
In order to measure the goodness of fit, Akaike’s Information Criteria (AIC) were used, which required the utilisation of the maximum likelihood (ML) method to estimate the coefficients [48]. Apart from the goodness of fit, we tested appropriateness amongst the pooled and random effect models, based on the share of sum of squares across countries out of the total sum of squares. The Breusch-Pagan Multiplier Test suggested that the variation between countries explains a significantly larger portion of total variation [49]. This implied that the random effect model is more suitable than the pooled model. Further, exogeneity of cofactors plays an important role to estimate the consistent and unbiased coefficients. In Eq. (1), σc controls for the effect due to countries, which makes the other coefficients independent of the error term. However, estimating the parameters for this will result in loss of degrees of freedom, which necessitates elimination. Elimination of σc can be performed using either the partitioned regression or putting it in the error term. The selection of either model, also known as the fixed effect and random effect regressions, respectively, was conducted through the Hausman Test [47]. The test suggested that the correlation between regressor and error term is significant, that is, resulting in endogeneity, and that, therefore, the fixed effect model is the most appropriate to estimate the relationship between CRD mortality rates and the set of independent variables.
The panel setup may present challenges of heteroskedasticity and autocorrelation. Non-constant variance may result from the inherent characteristics of the study subjects [50]. The outcome variable in the model is a measure of population health, that is, it is a function of overall health infrastructure, which is not explained in the model. This presents a situation where the variance of error may depend on the structural health conditions of a country and, therefore, can vary widely across them [51]. Consequently, the Modified Wald Test is conducted to test for heteroskedasticity. The test result suggests that the existing fixed effect model is violating the assumption of homoskedasticity. Therefore, due to the presence of heteroskedasticity, we resort to robust standard errors to remove the bias. In addition, serial autocorrelation was also tested as to its violation of the regression assumptions, since its presence can result in an inconsistent estimate for the coefficients. We did this through the unit root test, which suggested the presence of serial autocorrelation. This requires adjusting the covariance matrix in order to get rid of the autocorrelation. Thus, we use the Feasible Generalised Least Square (FGLS) Model to estimate the correlates, but the model fails to consider the heteroskedasticity issue present in the panel setup. Hence, to estimate the coefficients adjusted for both autocorrelation and heteroskedasticity, we resort to a model proposed by Prais-Winsten [52]. Prais-Winsten estimation has proven to be an effective method in the presence of autocorrelation and heteroskedasticity [53]. The estimation corrects for autocorrelation and allows for robust standard error which adjusts the heteroskedasticity in the panel data [54]. In other words, the estimates of the coefficients are consistent and lead us to believe that a fixed effect model with error correction is the most suitable model for our study.
Results
Table 1 presents the mean, standard deviation, minimum, and maximum of the variables used in the study. The observed mean of deaths from CRDs is 53.75 per 100,000 population. The summary statistics of the independent variables indicate that the mean of GDP per capita, years of schooling, urbanization and air pollution are $15,535.66, 12.63 years, 48.14%, and 36.55 μg/m3, respectively. The assessment of second-order moment (standard deviation) is performed to analyze the variation in dependent and independent variables across time and countries. The standard deviation (SD) within denotes the variation across time (temporal variation), whereas the SD between denotes the spatial variation. Higher share of SD between, compared to SD within, establishes that the spatial variation dominates over the temporal variation. For instance, in the case of CRD mortality rates, the SD between is 38.87, while the SD within is 2.96. The dominance of spatial variation over the temporal variation is also established statistically by Breusch-Pagan Multiplier Test. Further, the descriptive analysis in Table 1 provided the basis for regression model in terms of mathematical function required for each variable in the model.
Table 1.
Descriptive statistics, overall
| Variable | Mean | Std. Dev. | Min | Max | |
|---|---|---|---|---|---|
| Chronic respiratory diseases mortality rates | overall | 53.75 | 38.40 | 8.19 | 155.42 |
| between | 38.87 | 9.30 | 147.92 | ||
| within | 2.96 | 44.78 | 64.80 | ||
| GDP per capita | overall | 15,535.66 | 19,629.60 | 1614.00 | 85,535.00 |
| between | 19,888.48 | 1777.25 | 79,151.75 | ||
| within | 1478.52 | 8499.91 | 21,918.91 | ||
| Years of schooling (mean) | overall | 12.63 | 1.96 | 7.50 | 16.90 |
| between | 1.96 | 8.01 | 16.64 | ||
| within | 0.33 | 11.24 | 13.62 | ||
| Urbanization (%) | overall | 48.14 | 21.86 | 16.77 | 100.00 |
| between | 22.17 | 18.02 | 100.00 | ||
| within | 1.08 | 43.74 | 52.47 | ||
| PM2.5 Annual Population Weighted Concentration | overall | 36.55 | 22.63 | 5.90 | 101.00 |
| between | 22.79 | 6.70 | 98.25 | ||
| within | 2.93 | 22.80 | 45.80 |
Note: Total Observations: 232, Total Countries: 29, Years: 8
In Table 2, we present a static description of the selected covariates by intensity of mortality due to CRD. However, regression analysis is required to show the effect of the rate of change in GDP over the rate of change in CRD-based mortality. The rate of change in GDP per capita is much higher in countries with high mortality compared to countries with low mortality. For example, India has an average growth rate of 5–6% y-o-y, while Japan experiences a growth in GDP per capita of 1–2%. However, when comparing CRD mortality rates, India experiences a much higher rate than Japan, even though India is witnessing higher growth rate. Therefore, the regression model is utilized to estimate the effect of temporal variation in the growth rate of GDP per capita on CRD mortality. Additionally, unlike descriptive analysis, multivariate analysis controls for the confounding effects and shows the adjusted effect (ceteris-paribus). The inclusion of variables in the model, such as urbanization rate and schooling, controls for the spatial variation.
Table 2.
Mean of selected covariates across countries with High, Medium and Low CRD Mortality
| Covariates | High Mortality | Medium Mortality | Low Mortality |
|---|---|---|---|
| GDP per capita($) | 4665.81 | 16,433.1 | 24,265.35 |
| Urban Population (in %) | 34.01 | 43.06 | 67.08 |
| Schooling Years | 10.98 | 13.06 | 13.83 |
| PM2.5 (μg/m3) | 58.13 | 23.23 | 28.38 |
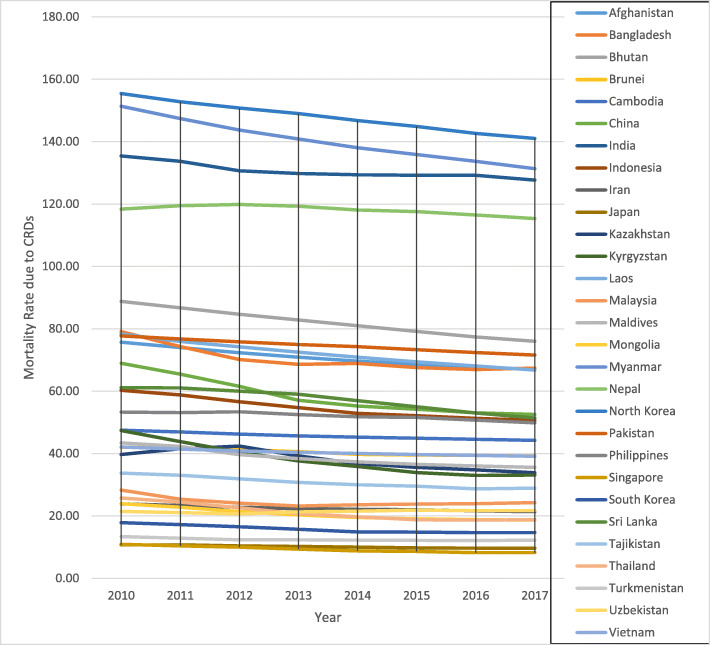
Figure 1 shows the pattern, dynamics and trends of CRD mortality rates for each country in the study period. High mortality countries, such as North Korea, Myanmar, India, and Nepal, show stagnancy or a decline. The same pattern is seen for countries with low mortality rates, such as Japan, Singapore, South Korea, and Turkmenistan.
Fig. 1.
Temporal Variation in CRD mortality rates
Table 3 compares the results and goodness of fit obtained from pooled ML, fixed effect and random effect models. Based on the AIC values and Hausman Test, we selected the fixed-effect model. The coefficient values for the fixed-effect model suggest that with an increase in the PM2.5 concentration, the mortality rate increases, whereas increases in GDP per capita, urban population and schooling years reduce the mortality rate. However, the sign and magnitude of the coefficients presented are inconsistent due to the presence of autocorrelation and heteroskedasticity.
Table 3.
Testing the Model
| Log (GMR) | (1) Pooled OLS | (2) Fixed Effect | (3) Random Effect |
|---|---|---|---|
| Log (GDP per capita) | 0.332*** | − 0.191*** | − 0.161*** |
| (0.0670) | (0.0506) | (0.0495) | |
| Years of schooling (mean) | −0.0648*** | −0.0426*** | − 0.0407*** |
| (0.0221) | (0.0128) | (0.0120) | |
| Urbanization (%) | −0.0276*** | −0.00915** | − 0.0116*** |
| (0.00268) | (0.00435) | (0.00346) | |
| PM2.5 (concentration) | 0.0121*** | 0.00346** | 0.00395*** |
| (0.00156) | (0.00149) | (0.00140) | |
| Constant | 2.349*** | 6.266*** | 6.067*** |
| (0.512) | (0.428) | (0.417) | |
| Observations | 224 | 224 | 224 |
| AIC | 255.47 | − 784.44 | − 558.58 |
| Number of Countriesa | 28 | 28 |
Note: *** p < 0.01, ** p < 0.05, * p < 0.1
aGDP value not available for North Korea
Table 4 presents the coefficients corrected for autocorrelation and heteroskedasticity based on the final model. The coefficients reported for the Prais-Winsten model show that the logarithmic mortality rate due to CRDs increases by 0.203 with the increase in log GDP per capita. Similarly, the marginal effect of PM-2.5 on the log mortality rate is estimated as 0.00869. However, the increase in schooling and urbanization has a negative association with the CRD mortality rates. For instance, the increase of one unit in the mean years of schooling reduces the log mortality rate by 0.0479, which presents itself as a resilience factor. To conclude, greater economic growth and exposure to PM-2.5 concentration in the atmosphere are increasing the fatality due to CRD. However, the negative effects can be reduced by literacy and urbanization.
Table 4.
Estimates corrected for heteroscedasticity and autocorrelation
| Log (GMR) | (1) Non-Robust SE | (2) Robust SE | (3) FGLS | (4) Prais-Winsten |
|---|---|---|---|---|
| Log (GDP per capita) | − 0.191*** | − 0.191* | 0.305*** | 0.203*** |
| (0.0506) | (0.0959) | (0.0204) | (0.0658) | |
| Years of schooling (mean) | −0.0426*** | −0.0426 | − 0.0574*** | − 0.0479*** |
| (0.0128) | (0.0267) | (0.00572) | (0.0185) | |
| Urbanization (%) | −0.00915** | −0.00915 | − 0.0270*** | −0.0252*** |
| (0.00435) | (0.00968) | (0.000435) | (0.00218) | |
| PM2.5 (concentration) | 0.00346** | 0.00346** | 0.0117*** | 0.00869*** |
| (0.00149) | (0.00143) | (0.000315) | (0.00114) | |
| Constant | 6.266*** | 6.266*** | 2.493*** | 3.324*** |
| (0.428) | (0.680) | (0.135) | (0.480) | |
| Observations | 224 | 224 | 224 | 224 |
| AIC | −784.44 | − 786.44 | ||
| Number of Countriesa | 28 | 28 | 28 | 28 |
Note: *** p < 0.01, ** p < 0.05, * p < 0.1
aGDP value not available for North Korea
Discussion
The significant number of deaths and morbidities due to CRDs in Asian countries warrant a comprehensive investigation of associated factors, from the individual level up to the country level. Researching this problem can make a significant contribution to the improvement of global public health. However, very few studies have focused on the assessment of risk factors associated with CRDs across multiple countries, and most of these lack a differential analysis of public health factors. This study explored the effect of GDP per capita, years of schooling, urbanization, and pollutant emission as socioeconomic and environmental factors on CRD-related mortality in 29 Asian countries, where dynamic growth has taken place at the cost of respiratory health. We further determined the rationale for the model-building to establish the relationship between CRD mortality rates and selected factors. The results highlight that both socioeconomic and environmental factors impact CRD mortality. This emphasises the role of reductions in air pollution, planned urbanization, and investment in human capital in the form of education to mitigate the risk of respiratory disease. These risk factors combine into a series of pathways that result in different types of CRDs, such as COPD, asthma, pneumoconiosis, and interstitial lung disease [55].
The major underlying factor for the rise in CRD mortality in Asian countries is rampant economic growth, which has resulted in a drastic changes in lifestyles. Thus, people in Asia became more exposed to fatal diseases such as CRD [6, 13, 14, 56]. Our results show that the annual increase in GDP per capita increases the CRD mortality rates. We speculate that the most likely cause is that GDP represents market consumption opportunity. Commonly, increasing GDP is associated with improved health facilities or increased consumption of calories and micronutrients, which are beneficial for the health outcomes of a country. On the other side, they can also lead to an unexpected increase in the number of diseases linked with prosperity. There may be an increased demand for goods associated with health risk, such as tobacco and alcohol, shifts in dietary structure and adoption of a more sedentary lifestyle [57]. Additionally, GDP growth also comes at the cost of environmental degradation [58–60]. Evidence suggests that higher growth in GDP has increased the level of pollutant emissions, which eventually leads to different types of CRDs and related deaths in many countries, particularly in Asian regions [55]. However, our results confirmed that the notion of GDP growth alongside the reduction in CRD deaths depends on the distribution of gains in the population. Also, the public health services and infrastructures of Asian countries might play a decisive role by comprising improved public health sectors as an integral part of comprehensive growth [57, 61]. This means that the relationship between mortality and GDP per capita growth is driven by the extent of public expenditure [61]. Controlling for the fixed effect of public health expenditure, which is in our case is the mean years of schooling, shows that the increase in GDP per capita increases CRD mortality.
Consistent with previous studies [13, 62–64], our results showed that PM2.5 is significantly positively correlated with CRD mortality, suggesting that higher exposure to particulate matter increases the mortality rate. In the last decade, many countries of Asia experienced increasing air pollution from both industrial and motor vehicle emissions [65]. The pollution also comes from burning of crop residues and bush fires in various Asian countries [66, 67]. Our findings suggest that there is a need for intervention to reduce air pollution in Asian countries and thereby limit premature mortality.
Very few studies have assessed the effect of urbanization on a range of CRDs. We found that the percentage of the total population residing in urban areas plays a key role as it reduced the mortality rate due to CRD. A higher percentage of urban dwellers is associated with a lower risk of mortality from CRD. Urbanization in Asian countries is accompanied by higher economic growth, favouring upward mobility in incomes [68]. This resulted in declining mortality as the quantum of shock from morbidity on a household budget was reduced with higher household savings and smoothing of consumption [69, 70]. It is observed that urban dwellers transition to cleaner fuel, which reduces the risk of CRD mortality [71]. Also, a gap exists in the transition rate between rural and urban areas, which provides an advantage to city dwellers. However, urbanization is associated with increased air pollution, which increases the risk of morbidity due to CRD but the associated mortality is reduced due to access to health care facilities and technologies [39].
Our results also suggest that a higher number of school years mitigates rising CRD mortality, showing that there is a negative association between them, and that education can act as a safety net against CRD mortality rates. A potentially important mechanism is that increased years of schooling is related to higher wages and earnings [72], which further enables individual to purchase better health care and creates awareness about the utility of health care [73, 74]. Further, from the structural lens, there is a possibility that higher investment in human capital reduces the risk of mortality by increasing employment opportunities and thereby broadening the safety net for individuals [75].
However, to obtain the best estimate for coefficients, we thoroughly discussed different model specifications. We observed inconsistency in the estimates across model specifications, which implies the need for appropriate rationales for model selection. Thus, error correction contributes significantly to the achievement of consistent and unbiased estimates.
Based on the nature of cross-country panel data, we expected that the error in the model might exhibit autocorrelation and heteroskedasticity. The expectation was based on the following two arguments: 1) The information was recorded for each year of the selected period (2010–2017). The observation in the current year has a significant likelihood of being related to the previous year’s value [76]. For illustration, the outcome variable, the mortality rates due to chronic respiratory disease, observed in time t can be related with the observation at t − 1 due to stickiness in the mortality rate for any specific region or country. Similar temporal autocorrelation has been observed in the past with respect to mortality for a given area [77]. 2) The argument for the presence of heteroskedasticity is suggested by the fact that countries can be ranked based on their mortality rates. This ranking allows for the clustering of countries, leading to heteroskedasticity. For example, countries like Japan, South Korea, and Singapore experience the lowest mortality rates, forming one group. In contrast, countries, such as India, Bangladesh, and Pakistan show a high mortality rate, and are hence placed in another group. The analysis of variance with the groups based on rankings suggest that variance within a group is significantly lower than it is across the groups. This results in heteroskedasticity of the error term in the model and therefore requires separate treatment.
However, the treatment of error to adjust for autocorrelation and heteroskedasticity is preceded by the selection of model. The selection of model was based on heterogeneity across the countries and endogeneity in the model. Based on the individual effect or heterogeneity of countries, the entire model can be treated as an ordinary linear model, whose parameters are estimated using maximum likelihood. We tested three plausible linear models: pooled regression, fixed effects and random effects. First, we tested whether the country fixed effects are constant terms. The Breusch-Pagan Multiplier Test suggests the fixed effect to be stochastic; therefore, the pooled regression model is discarded in favour of the random effect model. A subsequent challenge was to test the correlation between unobserved country effect and other covariates. In other words, we tested for endogeneity in the model. Identification of endogeneity is an essential step while developing the rationale for model selection, as it determines the form of unobserved country effects in the model. Further, inaccurate specification of country effects in the model results in inconsistent estimation of model coefficients [47]. Therefore, it was necessary to test the orthogonality of unobserved country-effects with the covariates. The Hausman test rejected the hypothesis of orthogonality, suggesting the fixed effect model to be ideal. Our finding is in alignment with the previous literature on cross-country studies which found non-orthogonality of unobserved country effects with the cofactors, such as GDP per capita, the concentration of air pollution, etc. [78, 79].
However, our analyses are also subject to limitations. The first, which is more general and has been reported elsewhere, concerns GBD studies and CRD estimates [80, 81]. Many scholars describe GBD estimates as a “black box”, which, from a scientific point of view, makes it impossible for anyone to replicate or verify the estimates. The second one is that this study does not incorporate other major risk factors associated with CRD mortality, such as tobacco smoking, air pollution (indoor), and allergens, although we argue that a good understanding of the selected variables is fundamental, as they are important predictors of mortality and health [19–21, 25–28, 32, 33, 35, 36, 41, 45, 46]. Finally, and although we have tried to eliminate all biases, it is important to note that even the most complex statistical models can have limitations.
Conclusion
Our results indicate that both socioeconomic and environmental factors impact CRD mortality rates. The Prais-Winsten model shows that the mortality due to CRD increases with rising GDP per capita and decreases with the percentage of the total population residing in urban areas. These results may initially appear to be a counterintuitive. However, if we consider this from the perspective that many of the countries studied are middle-income countries, that is, are still in the process of development and, consequently, of an increase in GDP, this result may seem natural. At the same time, it is assumed that urbanization is associated with increased air pollution. However, the impact of pollution on the risk of morbidity due to CRD is greater that its impact on mortality, since urban areas are expected to offer better access to health care facilities and technologies. Nevertheless, CRD mortality rates show a positive association with PM2.5, which suggests that mortality increases with greater exposure to particulate matter. Additionally, greater schooling mitigates the rising CRD mortality rates, showing that they are negatively correlated and that education can act as a safety net against CRD mortality.
The results are an outcome of sequential adjustments in the final model specification to correct for heteroscedasticity and autocorrelation, since when evaluating the relationship between CRD mortality rates and some possible predictor variables across Asian countries, we observed the presence of these elements, which suggests the need for correction while modelling. Hence, we estimated the coefficients using a feasible generalised least squares model with robust standard error. The detailed discussion of the rationale for model selection highlighted the internal validity problems, which were corrected, making the coefficients of the final model trustworthy.
In addition, we argue that this study provides useful clues for policymakers establishing effective public health planning and measures for the prevention of deaths from chronic respiratory disease. The reduction of CRD mortality rates, for example, can increase life expectancy enables people to contribute to the economy of a country and its regions for longer periods. Improvements in air quality, which many Asian countries are making progressively and in a remarkable manner, can make a substantial contribution to reducing deaths from CRD. Overall, this paper presents important findings that countries can benefit from in the short, medium, and long term.
Recommendation
Our findings support the need for urgent efforts to strengthen existing strategies to cope with CRD mortality through reduction in air pollution, planned urbanization, and investment in human capital to achieve Sustainable Development Goals for health. Although CRDs were the third leading cause of death worldwide in 2017, these diseases have received less attention than other non-communicable diseases, such as cardiovascular diseases and neoplasms.
Acknowledgements
Not applicable.
Abbreviations
- CRD
Chronic Respiratory Diseases
- GDP
Gross Domestic Product per capita
- PM2.5
Particles measuring less than 2.5 μm in aerodynamic diameter
- COPD
Chronic obstructive pulmonary disease
- CMRCRD
Crude mortality rate from chronic respiratory diseases
- GBD
Global Burden of Disease
- IHME
Institute for Health Metrics and Evaluation
- UNDP
United Nations Development Programme
- PPP
Purchasing power parity
- UNDESA
United Nations Department of Economic and Social Affairs
- AIC
Akaike’s Information Criteria
- ML
Maximum likelihood
- FGLS
Feasible Generalised Least Square
- SD
Standard Deviation
- Y-O-Y-
Year-on-year
Authors’ contributions
EAB, SD and SP - Conceptualization; EAB and SP - methodology; EAB - validation; EAB, SD and SP - formal analysis; EAB, SD and SP - investigation; EAB, SD and SP - writing (original draft preparation); EAB, SD and SP - writing (review and editing). All authors have read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Xie M, Liu X, Cao X, Guo M, Li X. Trends in prevalence and incidence of chronic respiratory diseases from 1990 to 2017. Respir Res. 2020;21(1):1–13. doi: 10.1186/s12931-019-1261-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization (2020). Chronic respiratory diseases. Available online: https://www.who.int/health-topics/chronic-respiratory-diseases#tab=tab_1. (Accessed on 17 January 2020).
- 3.Global Burden of Disease Collaborative Network (2018). Global Burden of Disease Study 2017 (GBD 2017) Cause-Specific Mortality 1980–2017. Institute for Health Metrics and Evaluation (IHME): Seattle, DC, USA, 2018. Available online: http://ghdx.healthdata.org/gbd-results-tool. (Accessed on 10 Nov 2019).
- 4.Wong GW, Leung TF, Ko FW. Changing prevalence of allergic diseases in the Asia-pacific region. Allergy, Asthma Immunol Res. 2013;5(5):251–257. doi: 10.4168/aair.2013.5.5.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang H, et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388(10053):1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bishwajit G, Tang S, Yaya S, Feng Z. Burden of asthma, dyspnea, and chronic cough in South Asia. Int J Chronic Obstruct Pulmon Dis. 2017;12:1093. doi: 10.2147/COPD.S133148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adhikari B, Pokharel S, Mishra SR. Shrinking urban Greenspace and the rise in non-communicable diseases in South Asia: an urgent need for an advocacy. Frontiers in Sustainable Cities. 2019;1:5. doi: 10.3389/frsc.2019.00005. [DOI] [Google Scholar]
- 8.Shimouchi A. Tuberculosis problems in the Asia-Pacific region. Respirology. 2001;6(1):75–78. doi: 10.1046/j.1440-1843.2001.00301.x. [DOI] [PubMed] [Google Scholar]
- 9.Regional COPD Working Group COPD prevalence in 12 Asia–Pacific countries and regions: projections based on the COPD prevalence estimation model. Respirology. 2003;8(2):192–198. doi: 10.1046/j.1440-1843.2003.00460.x. [DOI] [PubMed] [Google Scholar]
- 10.Wong GWK, Leung TF, Fok TF. ISAAC and risk factors for asthma in the Asia-Pacific. Paediatr Respir Rev. 2004;5:S163–S169. doi: 10.1016/S1526-0542(04)90032-2. [DOI] [PubMed] [Google Scholar]
- 11.Mori T. Tuberculosis epidemiology in the Asia-Pacific region. Respirology. 2008;13:S56–S64. doi: 10.1111/j.1440-1843.2008.01335.x. [DOI] [Google Scholar]
- 12.Tan WC, Ng TP. COPD in Asia: where east meets west. Chest. 2008;133(2):517–527. doi: 10.1378/chest.07-1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jamrozik E, Musk AW. Respiratory health issues in the Asia-Pacific region: an overview. Respirology. 2011;16(1):3–12. doi: 10.1111/j.1440-1843.2010.01844.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lim S, et al. Impact of chronic obstructive pulmonary disease (COPD) in the Asia-Pacific region: the EPIC Asia population-based survey. Asia Pac Fam Med. 2015;14(1):4. doi: 10.1186/s12930-015-0020-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ion RC, Wills AK, Bernal AL. Environmental tobacco smoke exposure in pregnancy is associated with earlier delivery and reduced birth weight. Reprod Sci. 2015;22(12):1603–1611. doi: 10.1177/1933719115612135. [DOI] [PubMed] [Google Scholar]
- 16.Soriano JB, et al. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet Respir Med. 2020;8(6):585–596. doi: 10.1016/S2213-2600(20)30105-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Salciccioli JD, et al. Respiratory disease mortality in the United Kingdom compared with EU15+ countries in 1985-2015: Observational study. BMJ. 2018;363:k4680. [DOI] [PMC free article] [PubMed]
- 18.UNDP (United Nations Development Programme) (2019). Human Development Data (1990–2017)| Human Development Reports. Available online: http://hdr.undp.org/en. Accessed 19 Jan 2020.
- 19.Preston SH. The changing relation between mortality and level of economic development. Popul Stud. 1975;1975(29):231–248. doi: 10.1080/00324728.1975.10410201. [DOI] [PubMed] [Google Scholar]
- 20.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020: global burden of disease study. Lancet. 1997;1997(349):1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 21.Berger MC, Messer J. Public financing of health expenditures, insurance, and health outcomes. Appl Econ. 2002;2002(34):2105–2113. doi: 10.1080/00036840210135665. [DOI] [Google Scholar]
- 22.Mackenbach JP, et al. The shape of the relationship between income and self-assessed health: an international study. Int J Epidemiol. 2004;2004(34):286–293. doi: 10.1093/ije/dyh338. [DOI] [PubMed] [Google Scholar]
- 23.Subramanian SV, Kawachi I. Being well and doing well: on the importance of income for health. Int J Soc Welf. 2006;2006(15):S13–S22. doi: 10.1111/j.1468-2397.2006.00440.x. [DOI] [Google Scholar]
- 24.James SL, Gubbins P, Murray CJL, Gakidou E. Developing a comprehensive time series of GDP per capita for 210 countries from 1950 to 2015. Popul Health Metr. 2012;10(1):12. [DOI] [PMC free article] [PubMed]
- 25.Gu D, et al. Old age mortality in eastern and south-eastern Asia. Demogr Res. 2013;2013(29):999–1038. doi: 10.4054/DemRes.2013.29.38. [DOI] [Google Scholar]
- 26.Baptista EA, Queiroz BL. The relation between cardiovascular mortality and development: study for small areas in Brazil, 2001–2015. Demogr Res. 2019;2019(41):1437–1452. doi: 10.4054/DemRes.2019.41.51. [DOI] [Google Scholar]
- 27.Baptista EA, Kakinuma K, Queiroz BL. Association between cardiovascular mortality and economic development: a Spatio-temporal study for prefectures in Japan. Int J Environ Res Public Health. 2020;17(4):1311. doi: 10.3390/ijerph17041311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hayward MD, Crimmins EM, Zhang Z. Consequences of educational change for the burden of chronic health problems in the population. In: Gauther AH, Chu CYC, Tuljapurkar S, editors. Allocating public and private resources across generations. New York: Springer; 2006. pp. 227–242. [Google Scholar]
- 29.Zajacova A, Hummer RA. Gender differences in education effects on all-cause mortality for white and black adults in the United States. Soc Sci Med. 2009;69:529–537. doi: 10.1016/j.socscimed.2009.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baker DP, et al. The education effect on population health: a reassessment. Popul Dev Rev. 2011;37:307–332. doi: 10.1111/j.1728-4457.2011.00412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hummer RA, Lariscy JT. Educational attainment and adult mortality. In: Rogers RG, Crimmins EM, editors. International handbook of adult mortality. New York: Springer; 2011. pp. 241–261. [Google Scholar]
- 32.Brown DC, et al. The significance of education for mortality compression in the United States. Demography. 2012;49:819–840. doi: 10.1007/s13524-012-0104-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Montez JK, Hummer RA, Hayward MD. Educational attainment and adult mortality in the United States: a systematic analysis of functional form. Demography. 2012;49:315–336. doi: 10.1007/s13524-011-0082-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.UNDESA (United Nations Department of Economic and Social Affairs), Population Division (2018). World Urbanization Prospects: The 2018 Revision. Available online: https://population.un.org/wup/Publications/Files/WUP2018-Report.pdf. Accessed 19 Jan 2020.
- 35.Reddy SK. Cardiovascular diseases in the developing countries: dimensions, determinants, dynamics and directions for public health action. Public Health Nutr. 2002;5(1a):231–237. doi: 10.1079/PHN2001298. [DOI] [PubMed] [Google Scholar]
- 36.Woods R. Urban–rural mortality differentials: an unresolved debate. Popul Dev Rev. 2003;29(1):29–46. doi: 10.1111/j.1728-4457.2003.00029.x. [DOI] [Google Scholar]
- 37.Menashe-Oren A, Stecklov G. Urban–rural disparities in adult mortality in sub-Saharan Africa. Demogr Res. 2018;39:136–176. doi: 10.4054/DemRes.2018.39.5. [DOI] [Google Scholar]
- 38.von Schneidemesser E, et al. Air pollution at human scales in an urban environment: impact of local environment and vehicles on particle number concentrations. Sci Total Environ. 2019;688:691–700. doi: 10.1016/j.scitotenv.2019.06.309. [DOI] [PubMed] [Google Scholar]
- 39.Chongsuvivatwong V, et al. Health and health-care systems in Southeast Asia: diversity and transitions. Lancet. 2011;377(9763):429–437. doi: 10.1016/S0140-6736(10)61507-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Health Effects Institute (2019). State of Global Air 2019. Available: www.stateofglobalair.org. (Accessed on 19 December 2019).
- 41.Dominici F, et al. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. Jama. 2006;295(10):1127–1134. doi: 10.1001/jama.295.10.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peng RD, et al. Coarse particulate matter air pollution and hospital admissions for cardiovascular and respiratory diseases among Medicare patients. Jama. 2008;299(18):2172–2179. doi: 10.1001/jama.299.18.2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tecer LH, et al. Particulate matter (PM2. 5, PM10–2.5, and PM10) and children's hospital admissions for asthma and respiratory diseases: A bidirectional case-crossover study. J Toxic Environ Health A. 2008;71(8):512–520. doi: 10.1080/15287390801907459. [DOI] [PubMed] [Google Scholar]
- 44.Katanoda K, et al. An association between long-term exposure to ambient air pollution and mortality from lung cancer and respiratory diseases in Japan. J Epidemiol. 2011;1(2):132. [DOI] [PMC free article] [PubMed]
- 45.Hay SI. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990-2015: a systematic analysis for the global burden of disease study 2015. Lancet Respir Med. 2017;5(9):691–706. [DOI] [PMC free article] [PubMed]
- 46.Salvi S, et al. The burden of chronic respiratory diseases and their heterogeneity across the states of India: the global burden of disease study 1990–2016. Lancet Glob Health. 2018;6(12):e1363–e1374. doi: 10.1016/S2214-109X(18)30409-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Greene WH. Econometric analysis: Econometric Analysis. 5th ed. Upper Saddle River: Prentice Hall; 2003.
- 48.Bozdogan H. Model selection and Akaike's information criterion (AIC): the general theory and its analytical extensions. Psychometrika. 1987;52(3):345–370. doi: 10.1007/BF02294361. [DOI] [Google Scholar]
- 49.Breusch TS, Pagan AR. The Lagrange multiplier test and its applications to model specification in econometrics. Rev Econ Stud. 1980;47(1):239–253. doi: 10.2307/2297111. [DOI] [Google Scholar]
- 50.Maddala GS. On the use of panel data methods with cross-country data. Annales d'Economie et de Statistique. 1999; n.55/56, p.429–448.
- 51.Fullman N, et al. Measuring performance on the healthcare access and quality index for 195 countries and territories and selected subnational locations: a systematic analysis from the global burden of disease study 2016. Lancet. 2018;391(10136):2236–2271. doi: 10.1016/S0140-6736(18)30994-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Canjels E, Watson MW. Estimating deterministic trends in the presence of serially correlated errors. Rev Econ Stat. 1997;79(2):184–200. doi: 10.1162/003465397556773. [DOI] [Google Scholar]
- 53.Wooldridge JM. Introductory econometrics: a modern approach. Cincinnati: South-Western College Pub; 2016.
- 54.Blackwell JL., III Estimation and testing of fixed-effect panel-data systems. Stata J. 2005;5(2):202–207. doi: 10.1177/1536867X0500500205. [DOI] [Google Scholar]
- 55.World Health Organization (2007). Global Alliance against chronic respiratory diseases. Available online: https://www.who.int/gard/en/. (Accessed on 04 March 2020).
- 56.Ip MSM. Lung function testing in health and disease: issues pertaining to Asia-Pacific populations. Respirology. 2011;16(2):190–197. doi: 10.1111/j.1440-1843.2010.01850.x. [DOI] [PubMed] [Google Scholar]
- 57.Lange S, Vollmer S. The effect of economic development on population health: a review of the empirical evidence. Br Med Bull. 2017;121(1):47–60. doi: 10.1093/bmb/ldw052. [DOI] [PubMed] [Google Scholar]
- 58.Ekins P. The Kuznets curve for the environment and economic growth: examining the evidence. Environ Plan A. 1997;29(5):805–830. doi: 10.1068/a290805. [DOI] [Google Scholar]
- 59.Apergis N, Ozturk I. Testing environmental Kuznets curve hypothesis in Asian countries. Ecol Indic. 2015;52:16–22. doi: 10.1016/j.ecolind.2014.11.026. [DOI] [Google Scholar]
- 60.Ota T. Economic growth, income inequality and environment: assessing the applicability of the Kuznets hypotheses to Asia. Palgrave Commun. 2017;3(1):1–23. doi: 10.1057/palcomms.2017.69. [DOI] [Google Scholar]
- 61.Sen A. Mortality as an indicator of economic success and failure. Econ J. 1998;108(446):1–25. doi: 10.1111/1468-0297.00270. [DOI] [Google Scholar]
- 62.Gan WQ, et al. Associations of ambient air pollution with chronic obstructive pulmonary disease hospitalization and mortality. Am J Respir Crit Care Med. 2013;187(7):721–727. doi: 10.1164/rccm.201211-2004OC. [DOI] [PubMed] [Google Scholar]
- 63.Hoek G, et al. Long-term air pollution exposure and cardio-respiratory mortality: a review. Environ Health. 2013;12(1):43. doi: 10.1186/1476-069X-12-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liu C, et al. Ambient particulate air pollution and daily mortality in 652 cities. N Engl J Med. 2019;381(8):705–715. doi: 10.1056/NEJMoa1817364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chung KF, Zhang J, Zhong N. Outdoor air pollution and respiratory health in Asia. Respirology. 2011;16(7):1023–1026. doi: 10.1111/j.1440-1843.2011.02034.x. [DOI] [PubMed] [Google Scholar]
- 66.Dennekamp M, Abramson MJ. The effects of bushfire smoke on respiratory health. Respirology. 2011;16(2):198–209. doi: 10.1111/j.1440-1843.2010.01868.x. [DOI] [PubMed] [Google Scholar]
- 67.Vijayakumar K, et al. Effects of agriculture crop residue burning on aerosol properties and long-range transport over northern India: a study using satellite data and model simulations. Atmos Res. 2016;178:155–163. doi: 10.1016/j.atmosres.2016.04.003. [DOI] [Google Scholar]
- 68.Cook S. Structural change, growth and poverty reduction in Asia: pathways to inclusive development. Dev Policy Rev. 2006;24:s51–s80. doi: 10.1111/j.1467-7679.2006.00341.x. [DOI] [Google Scholar]
- 69.Blakely T, Wilson N. Shifting dollars, saving lives: what might happen to mortality rates, and socio-economic inequalities in mortality rates, if income was redistributed? Soc Sci Med. 2006;62(8):2024–2034. doi: 10.1016/j.socscimed.2005.08.059. [DOI] [PubMed] [Google Scholar]
- 70.Genoni ME. Health shocks and consumption smoothing: evidence from Indonesia. Econ Dev Cult Chang. 2012;60(3):475–506. doi: 10.1086/664019. [DOI] [Google Scholar]
- 71.Farabi-Asl H, et al. Energy challenges for clean cooking in Asia, the Background, and possible policy solutions. 2019. [Google Scholar]
- 72.Card D. The causal effect of education on earnings. In: Handbook of labor economics (Vol. 3, pp. 1801-1863): Elsevier; 1999.
- 73.Buckles K, et al. The effect of college education on mortality. J Health Econ. 2016;50:99–114. doi: 10.1016/j.jhealeco.2016.08.002. [DOI] [PubMed] [Google Scholar]
- 74.Hetlevik Ø, Melbye H, Gjesdal S. GP utilisation by education level among adults with COPD or asthma: a cross-sectional register-based study. NPJ Prim Care Respir Med. 2016;26(1):1–7. doi: 10.1038/npjpcrm.2016.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kalemli-Ozcan S, Ryder HE, Weil DN. Mortality decline, human capital investment, and economic growth. J Dev Econ. 2000;62(1):1–23. doi: 10.1016/S0304-3878(00)00073-0. [DOI] [Google Scholar]
- 76.Congdon P. Spatiotemporal analysis of area mortality. J R Stat Soc Series D (The Statistician) 1994;43(4):513–528. [Google Scholar]
- 77.Kanjala C, Alberts M, Byass P, Burger S. Spatial and temporal clustering of mortality in Digkale HDSS in rural northern South Africa. Glob Health Action. 2010;3(1):5236. doi: 10.3402/gha.v3i0.5236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Selden TM, Song D. Environmental quality and development: is there a Kuznets curve for air pollution emissions? J Environ Econ Manag. 1994;27(2):147–162. doi: 10.1006/jeem.1994.1031. [DOI] [Google Scholar]
- 79.Torre R, Myrskylä M. Income inequality and population health: a panel data analysis on 21 developed countries. Working Paper 2011-006. Max Planck Institute for Demographic Research. Rostock. 2011.
- 80.Wang DY, et al. Quality of life and economic burden of respiratory disease in Asia-Pacific-Asia-Pacific burden of respiratory diseases study. Value Health Regional Issues. 2016;9:72–77. doi: 10.1016/j.vhri.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 81.Soriano JB, et al. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet Respir Med. 2017;5(9):691–706. doi: 10.1016/S2213-2600(17)30293-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.