Abstract
Family planning is commonly regarded as a highly cost-effective health intervention with wider social and economic benefits. Yet use of family planning services in Sierra Leone is currently low and 25.0% of married women have an unmet need for contraception. This study aims to estimate the costs and benefits of scaling up family planning in Sierra Leone. Using the OneHealth Tool, two scenarios of scaling up family planning coverage to currently married women in Sierra Leone over 2013–2035 were assessed and compared to a ‘no-change’ counterfactual. Our costing included direct costs of drugs, supplies and personnel time, programme costs and a share of health facility overhead costs. To monetise the benefits, we projected the cost savings of the government providing five essential social services – primary education, child immunisation, malaria prevention, maternal health services and improved drinking water – in the scale-up scenarios compared to the counterfactual. The total population, estimated at 6.1 million in 2013, is projected to reach 8.3 million by 2035 in the high scenario compared to a counterfactual of 9.6 million. We estimate that by 2035, there will be 1400 fewer maternal deaths and 700 fewer infant deaths in the high scenario compared to the counterfactual. Our modelling suggests that total costs of the family planning programme in Sierra Leone will increase from US$4.2 million in 2013 to US$10.6 million a year by 2035 in the high scenario. For every dollar spent on family planning, Sierra Leone is estimated to save US$2.10 in expenditure on the five selected social sector services over the period. There is a strong investment case for scaling up family planning services in Sierra Leone. The ambitious scale-up scenarios have historical precedent in other sub-Saharan African countries, but the extent to which they will be achieved depends on a commitment from both the government and donors to strengthening Sierra Leone’s health system post-Ebola.
Keywords: cost–benefit analysis, family planning, Sierra Leone
Introduction
Sierra Leone’s maternal and child health indicators are among the worst in the world.1 A number of strategies have been identified to address this, including the scaling up of family planning (FP) services, particularly to rural communities. Use of FP services in Sierra Leone has historically been very low. In 2000, during the country’s civil conflict that lasted over a decade (1991–2002), the contraceptive prevalence rate (CPR) for modern methods was 3.9% and had increased only to 6.7% by 2008.2,3 The latest population-based estimate from 2013 put the CPR for modern methods at 15.6%, with an additional 1.0% of women using traditional methods. A further 25.0% of married women in Sierra Leone who want to avoid a pregnancy are not using contraception, indicating both that need is not being met and that overall demand for FP services is low compared to other countries. In other words, 37.5% of the total demand for FP methods is satisfied by modern methods, which is some way off the Sustainable Development Goal target of at least 75%.4,5 Qualitative evidence suggests that the recent (2014–2016) Ebola virus epidemic further reduced use of FP services.6
Prior to Ebola, these modest gains in the CPR occurred as the Government of Sierra Leone prioritised improving the health of its people – particularly mothers and children – under the post-conflict development plans of the Agenda for Change (2008–2012) and Agenda for Prosperity (2013–2018). Equitable access to quality FP services was identified as a key priority of these plans and of associated health sector policies, including the government’s Free Health Care Initiative (FHCI) for children under 5 years of age, pregnant women and lactating mothers. During this time, high-level political commitment started to translate into action, with supply side–strengthening activities such as improved availability of FP commodities, training of health workers and rehabilitation of health facilities.
However, despite the role given to FP in the Agenda for Prosperity development plan and the longer-term strategy of becoming a middle-income country by 2035, only 0.04% of the Agenda for Prosperity budget was allocated to FP. This study therefore aims to estimate the level of expenditure required to achieve FP scale-up in Sierra Leone and compare this to the projected impact on government expenditures for other social services. Health outcomes, while not monetised, are also modelled. Post-Ebola, this cost–benefit analysis remains relevant in demonstrating what the costs and benefits would be to FP scale-up as part of the country’s recovery and continued development.
Providing FP so that women can have the number of children they want when they want is commonly found to be a highly cost-effective health intervention with wider social and economic benefits.7,8 However, there are therefore fewer country-specific estimates of the level of expenditure required to achieve particular scale-up scenarios in low-income countries. This study aims to fill that gap for Sierra Leone.
The literature has identified health benefits for both women and their children.9 For women, contraceptives have been found to prevent unintended pregnancies, reduce the number of abortions and lower the incidence of death and disability related to complications of pregnancy and childbirth, primarily by reducing the number of times a woman has to go through the potentially deadly process of childbirth. In an analysis of 172 countries, Ahmed et al.10 estimate that contraceptive use led to a 44% reduction in maternal deaths in 2008 and satisfying unmet need for contraception would have led to a further 29% reduction.
Additional non-contraceptive health benefits of FP have also been recognised, particularly the role of barrier methods such as condoms in substantially reducing the risk of contracting HIV and other sexually transmitted infections.11 In terms of impact on infant and child mortality, the literature has focused on the effect of ‘too frequent’ pregnancies, with one study finding that child mortality can be reduced by 13% with birth spacing of 2 years or more and 25% with birth spacing of 3 years or more.12
In terms of wider social and economic benefits, the literature has focused on those associated with the population dynamics of the demographic transition. By reducing fertility rates, FP can play a central role in a country’s transition from high to low birth and death rates. This can produce cost savings for the government as a result of providing social sector services to a smaller group of people, as well as climate change benefits resulting from less pressure on arable land and water resources and reduced carbon dioxide emissions.13,14 Furthermore, as fertility begins to slow, the number of children per working age person declines, creating a situation that is favourable for economic growth. Many Asian and Latin American countries have achieved this ‘demographic dividend’, and there are indications that some African countries such as Rwanda and Ethiopia are beginning to follow. However, a demographic dividend does not follow automatically from lower fertility rates and requires investment in other areas such as girls’ education and good governance to be achieved.15 Finally, various studies have shown that FP has, among other benefits, given women greater freedom to participate in the workforce.16
In recent years, work has been done to cost the investment requirements of increasing the coverage of reproductive, maternal and child health interventions in developing countries as well as the expected impact of their scale-up scenarios. For example, the 2014 Lancet Global Investment Framework includes FP as one of the 50 evidence-based interventions in its cost–benefit analysis of investing in women’s and child’s health in 74 developing countries.8 However, cost-effectiveness or cost–benefit studies of scaling up FP services rarely include a comprehensive estimate of the investment requirements of this scale-up. For example, the Guttmacher Institute has produced several estimates of the costs of providing women with a need for FP in developing countries with modern contraception and the expected impact on unintended pregnancies, maternal and newborn deaths and disability-adjusted life years (DALYs) averted. The resulting cost-effectiveness analysis compares the scenario of all needs for FP being met with a no-change scenario of unmet needs remaining at its current level, but the cost of the activities to move from one coverage level to the other is not included.17–19 Similarly, another study models the costs of satisfying unmet need for contraception and the benefits in terms of reduced costs of meeting the Millennium Development Goals in 16 sub-Saharan African countries, finding benefit–cost ratios of between US$2 and US$6 over the time period 2005–2015. However, these calculations do not include health system strengthening costs.13
Methods
Country context
Sierra Leone is located on the west coast of Africa, on the Atlantic Ocean between Liberia and Guinea. The country’s projected population for 2013 was 6.1 million people, with a population growth rate of 1.9%. In 2013, 42% of the country was under 15 years of age. The total fertility rate (TFR) was 4.9 children per woman while 28% of girls age 15–19 years were pregnant or had already had one birth. Gross domestic product (GDP) per capita stood at USD 679 per person. Maternal and child health outcome were very poor. The latest United Nations (UN) estimates put the maternal mortality ratio as the worst in the world, with no statistically significant change between 2008 and 2013 Demographic and Health Survey (DHS) rounds. Child mortality trends were more positive, with rates of neonatal, infant and under-5 mortality falling prior to 2013, but still very high: in 2013, the under-5 mortality ratio was 156 deaths per 1000 live births.4
Cost–benefit analysis framework
We modelled the costs and benefits of scaling up FP services to all currently married women age 15–49 years. In countries where most women marry at an early age, this group is inclusive of the majority of women of reproductive age in need of contraception. It does exclude the smaller but still important group of unmarried, sexually active women, many of whom are adolescents. In Sierra Leone, about 11% of women age 15–49 years are unmarried and sexually active; however, data on the sexual and reproductive behaviour of this group are typically more limited.4,18
All major FP interventions were included in the analysis. Currently, most married women in Sierra Leone who use contraception use a modern method, with only 6.0% of those who use contraception relying on a traditional method such as withdrawal or periodic abstinence. Short-term methods including pills, male condoms and injectables are used by more women than long-term and permanent methods including implants, intrauterine devices (IUDs) and female sterilisation. Female condoms and male sterilisation are not currently used enough to appear in national statistics, but we allowed for the possibility of these methods in our model.4
The cost–benefit analysis framework comprised five inter-linked analytical components, as illustrated in Figure 1. We used the OneHealth Tool (version 5.32) to conduct much of the analysis because it offers an integrated solution for assessing the costs and demographic and health impact of scaling up FP services. The OneHealth Tool is a model developed by an inter-agency group of UN and other development institutions to support planning of health sector strategies in low- and middle-income countries. The tool is relatively complex with potentially high data requirements but is modular, and so can be simplified to focus purely on FP costs and benefits. Much further detail on the OneHealth Tool is available on its website.20 Additional analysis was conducted using Excel.
Figure 1.
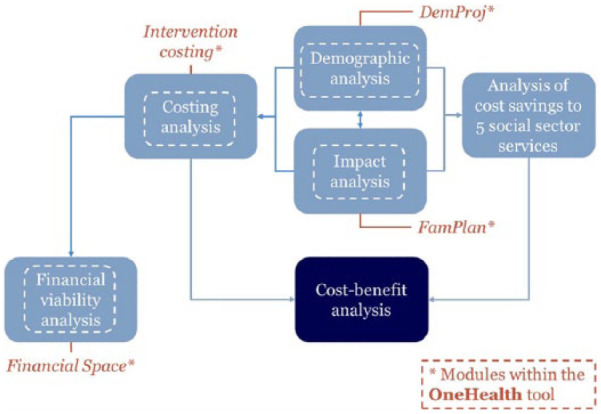
Modelling framework.
The year 2013 was chosen as the baseline for the analysis as this was when the study was commissioned and 2013 was the latest year for which data were available – including key data from the latest DHS. Our analysis modelled costs and benefits over two time frames: a shorter-term time frame from 2013 to 2017, chosen to align with the Agenda for Prosperity poverty reduction strategy, and a long-term time frame from 2013 to 2035, chosen to align with the country’s time frame to become a middle-income country.21 The longer-term time frame also coincides with that of the Lancet Global Investment Framework, which aims to show what could be achieved in a generation.8 We report results primarily over the longer-time frame in the text, although results for the shorter-time frame are also shown in the figures.
Two scale-up scenarios were assessed. A ‘medium’ scenario modelled the CPR reaching 34% by 2035. Such an increase in CPR should be feasible given historical trends and 25% of married women having an unmet need for contraception. This scenario did not model a change in the method mix. A ‘high’ scenario modelled the CPR reaching 50% by 2035. This is an ambitious increase in CPR: it assumes a small increase in total demand and an increase in the CPR of just over 1.5 percentage points a year, which historically has been the increase that Sierra Leone and other countries have found sustainable.4,22 However, countries such as Rwanda and Ethiopia have shown that sustained increases above 1.5 percentage points a year are possible.23 Our ‘high’ scenario modelled a gradual shift towards greater use of long-acting and reversible methods and permanent methods, based on expert advice from United Nations Population Fund (UNFPA) and the Ministry of Health and Sanitation. These scale-up scenarios were compared to a ‘no-change’ counterfactual of the CPR and method mix remaining constant at their 2013 values. Our analysis should therefore be interpreted as the comparisons between the scale-up and counterfactual scenarios.
Table 1 shows the key input data and data sources for the estimation of costs and benefits and modelling of demographic and health impact. How these data were used in our cost–benefit model is explained in subsequent sections.
Table 1.
Key input data and sources.
| 1.1 Inputs to costing analysis | |||||
|---|---|---|---|---|---|
| Delivery channels for FP interventionsa | |||||
| FP method | Delivery channels (%) | Data source | |||
| Community | Outreach | Clinic | Hospital | UNFPA Sierra Leone expert opinion (pers. comm. January 2014) | |
| Pill | 0 | 30 | 55 | 15 | |
| Condom | 0 | 70 | 20 | 10 | |
| Injectable | 0 | 30 | 40 | 30 | |
| IUD | 0 | 0 | 30 | 70 | |
| Implant | 0 | 60 | 30 | 10 | |
| Female sterilisation | 0 | 0 | 0 | 100 | |
| Male sterilisation | 0 | 0 | 0 | 100 | |
| LAM | 0 | 0 | 0 | 100 | |
FP: family planning; UNFPA: United Nations Population Fund; IUD: intrauterine device; LAM: lactational amenorrhoea method; WHO: World Health Organization; CHO: Community Health Officer; MOHS: Ministry of Health and Sanitation; SECHN: State Enrolled Community Health Nurse; CHA: Community Health Aide; DHS: Demographic and Health Survey; N/A: not available; UN: United Nations; CPR: contraceptive prevalence rate.
The OneHealth Tool costs interventions provided at different levels of care, or the ‘delivery channels’ of community, outreach, clinic and hospital-based care. Default values were revised to the local context, as recommended by the OneHealth Tool.1
All 2013 USD prices. When provided as an outreach service, minutes per case is assumed to be 9 min longer per case to allow for health worker travel time from the clinic to the community.
Salaries include costs of 34% of basic salaries. Salaries were used to cost the medical personnel requirements from the OneHealth Tool. This analysis is necessarily conducted outside the tool. We used the same assumptions as in (2) below, whereby we assume that medical personnel work on average 8 h a day for 220 days per year and spend 80% of their working time directly on service delivery (as opposed to admin, downtime, etc.).
For MOHS recurrent, non-salary expenditure, FY2013 estimates are used as the basis for the calculations. For MOHS salary expenditure, 2013 gross monthly salaries are used.
IMF data on end of period consumer inflation were used to inflate 2008 USD costs from WHO-CHOICE to 2013 USD prices. Following (2) given below, we used the following: for the overhead cost per outpatient visit at the outreach and clinic levels, we used the WHO-CHOICE estimate for a health centre with no beds and for the overhead cost per outpatient visit at the hospital level, we used the WHO-CHOICE estimate for a primary level hospital. To avoid double counting of medical personnel costs, which are included in the WHO-CHOICE estimates but which we have already accounted for in our direct intervention costing, we scaled these estimates by a factor of 0.4. This factor reflects the median ratio of overhead costs to medical personnel costs from a sample of costing studies of health facilities in Africa.
Data sources: 2013 values are from the 2013 DHS.5 Subsequent projections are based on expert opinion from MOHS and UNFPA Sierra Leone. (pers. comm. January 2014).
These are default values in the OneHealth Tool that reflect international norms.1
These are default values in the OneHealth Tool that reflect international norms.1
All but proportion of women age 15–49 years in union are default values in the OneHealth Tool that reflect international norms.1 (b) The percentage of women age 15–49 years in union in Sierra Leone has declined quite substantially from 74.9% in 2008 to 65.4% in 2013. It was unrealistic to model a constant trend for this determinant and instead continued the trend from 2008 until percentage of women reached 58.5% (in 2017), which is the percentage for Ghana, the country in the region with the current highest CPR.6
All are default values in the OneHealth Tool that reflect international norms.1
Statistics Sierra Leone & ICF International, 2014. Sierra Leone Demographic Health Survey 2013.
Sources: 2013 coverage estimates from (4) given below;4 unit costs estimated from (6) to (11) below
Sanders R. OneHealth Tool website.20
Stenberg et al.8
Johns et al.24
United Nations: Department of Social and Economic Affairs.25
Statistics Sierra Leone, ICF International.4
Government of Sierra Leone.26
Wolfson et al.27
Jamison et al.28
World Health Organization.29
Hutton.30
Estimation of costs
We comprehensively costed all scenarios using the OneHealth Tool. All health-related costs associated with FP were included, regardless of whether these are borne by the government, donors or households. This means, for example, that we are costing the provision of drugs, supplies and health worker time for FP services regardless of who pays. However, transport costs of women and men accessing FP services were not included. All costs are constant 2013 USD excluding inflation. Direct costs were estimated through a bottom–up ingredients approach, in which need-based quantities of FP commodities, other drugs and supplies and medical personnel time were multiplied by Sierra Leone–specific unit costs. Drug and supply costs were adjusted upwards by 30% of the commodity value to account for supply chain logistics and wastage, following the approach in Stenberg et al.8 We assumed that FP interventions are delivered through the three delivery channels relevant to the Sierra Leone context – outreach services, static clinics and hospitals – which affected the cadre of medical personnel and the time spent delivering the intervention. The distribution of interventions across these delivery channels was estimated following advice from UNFPA and Ministry of Health and Sanitation experts. Their judgement was also used to adapt WHO treatment norms for medical personnel time to better reflect the actual Sierra Leone context.
To incorporate health facility overhead costs, we multiplied the estimated number of outpatient visits required to deliver FP interventions through the different delivery channels at projected coverage levels by unit cost estimates from WHO-CHOICE, inflated to 2013 prices. This follows the approach in Stenberg et al.8 but scales the unit costs to remove medical personnel costs already counted in the direct costs. The scaling factor that we used reflects the median value of the share of medical personnel costs in health facility costs in a sample of sub-Saharan African studies.31–33
We then costed the activities at the wider population level required for FP services to be effectively implemented, such as advocacy campaigns and demand and supply side–strengthening activities. Current FP programme costs were estimated using 2013 government and donor data. We modelled programme costs increasing at a decreasing rate, rather than assuming a fixed proportion, to reflect time-series evidence from other FP programmes.34 Specifically, we estimated that in 2013 programme costs are just over three times direct costs and assumed that this proportion declines linearly over the period so that in 2035 programme costs are one and a half times direct costs. Because coverage is increasing, this assumption still implies an absolute increase in programme costs over the period for the FP scale-up scenarios. For the counterfactual scenario, with a constant CPR but increasing population, the assumption means that programme costs are modelled to decline over the period. Although our rule of thumb is less sophisticated than defining a precise cost function, it is preferable to ignoring scaling issues completely.24 Reflecting the uncertainty around trends in programme costs over time, we vary the assumption in the sensitivity analysis.
It should be noted that our estimate for the expenditure on FP in Sierra Leone in 2013 differs markedly from that of the 2013 National Health Accounts (NHA), which estimates that the government and donors spent US$7 million on FP in 2013 and households spent US$29 million.35 Differences in our costing methodologies help explain these discrepancies. The NHA approach is to allocate health expenditure to ‘disease’ using utilisation data and assume that all outpatient visits have the same unit cost. Given that FP typically makes up a high share of outpatient visits, but the costs of those visits is lower – to both the provider and the patient – than other services, this assumption means that the NHA figure is likely overestimated for FP. Our bottom–up ingredients approach to the direct costing and use of actual FP expenditure data for the programme costing allows us to cost FP separately and better reflect the actual resource requirements for providing FP interventions and the associated activities at the population level.
Estimation of benefits
We conducted simulation modelling using the OneHealth Tool to estimate the demographic and health impact of the scale-up scenarios compared to the counterfactual scenario. For most variables, the OneHealth Tool contains reliable default values drawn from the most recent sources, such as large population-based surveys, UN population estimates and peer-reviewed FP articles.36 We estimated the impact of the scale-up scenarios by comparing to the counterfactual scenario on population size and structure, FP use and fertility rates.
In terms of health outcomes, we analysed potential reductions in maternal and infant deaths. Our modelling of the impact of FP scale-up on infant mortality must occur outside the OneHealth Tool. We drew on the approach of the Guttmacher Institute and simply applied the current infant mortality rate (IMR) to the number of births in each scenario to estimate the demographic impact of FP.17 This is conservative in that it does not capture the reduced risk per birth that other studies have found.12
To monetise the benefits, we projected the costs of the government providing primary education, child immunisation, malaria prevention, maternal health services and improved drinking water in the different scenarios. Benefits are therefore in terms of cost savings from fewer people requiring these five essential services, following the scale-up of FP coverage. Changes to the total population and population structure are combined with goals for scale-up of coverage for these key social services and their associated unit costs. It is important to note that these coverage increases are applied to the counterfactual scenario as well as the FP scale-up scenarios. They are ambitious scale-up goals to achieve by 2018 but correspond to the government’s Agenda for Prosperity targets for child immunisation and improved drinking water, and the Millennium Development Goal targets for primary education, malaria prevention and maternal health services. The projections for scale-up are varied as part of the sensitivity analysis to understand how they affect overall results.
As a supplementary analysis, we modelled the potential demographic dividend of a lower dependency ratio, assuming complementary investment in other areas. For this, we drew on a recent simulation model developed to quantitatively analyse the economic effects of fertility reductions in developing countries on economic growth, tailoring it to the characteristics of Sierra Leone and our FP scale-up scenarios.37 This analysis is not included in our cost–benefit analysis because a demographic dividend does not automatically follow from lower fertility rates and requires investment in other areas such as girl’s education and good governance to be achieved.15
Financial viability
We assessed the financial viability of the increased investment by checking whether scale-up costs fitted within the health sector resource envelope using the Financial Space module in the OneHealth Tool. Analysis here is based on the aggregate data relating to the macroeconomic context (GDP growth, government expenditure) and health expenditure (public and private) from the NHA. We modelled future health expenditure based on its expected relationship to GDP growth.38
Results
Demographic and health impact of scaling up FP
The total population, estimated at 6.1 million in 2013, is projected to reach 9.0 million by 2035 in the medium scenario and 8.3 million in the high scenario, compared with 9.6 million in the counterfactual scenario. The latest UN population estimates are given as reference points for the available years of 2013 and 2025 (Figure 2).
Figure 2.
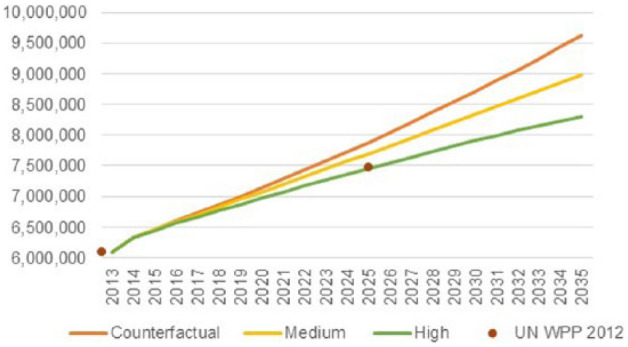
Projected total population for Sierra Leone, 2013–2035.
In addition to a slower rate of population growth under the FP scale-up scenarios, our modelling also shows important projected changes in the age structure of the population. In 2013, Sierra Leone had a very young population with an estimated 39.2% of people under age 15 years and only 3.8% more than age 65 years. This translates into a dependency ratio of 0.75 (75 children and older people per 100 working age people). By 2035, the dependency ratio is projected to be 0.59 in the medium scenario and only 0.54 in the high scenario. This is compared to a smaller decline to 0.68 in the counterfactual scenario. As expected, these declines are almost entirely driven by the decline in the youth dependency ratio.
The TFR is modelled to decline with increases in the CPR. Estimated at 4.9 in 2013, the TFR is projected to fall to 3.3 by 2035 in the medium scenario and 2.4 in the high scenario. This latter figure is close to the average replacement fertility rate of 2.1 children per woman.39 In the counterfactual, the TFR is projected only to decline slightly over the period, flat lining at 4.4 from 2017 onwards (Figure 3). (This is because even under the counterfactual scenario, we still allowed for changes in the age-specific fertility rates and percent of women age 15–49 years who are married. Use of FP is one of several determinants of fertility, with others likely to change through economic development.40)
Figure 3.
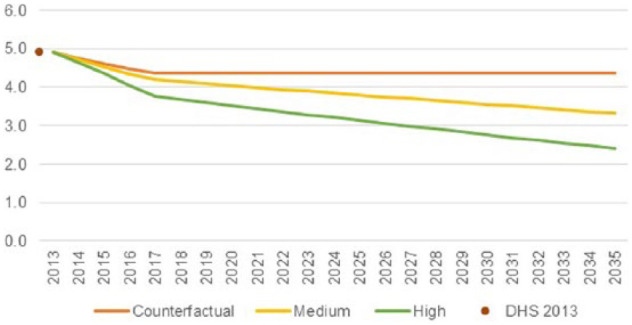
Projected total fertility rate for Sierra Leone, 2013–2035.
The percent of women with an unmet need for contraception is modelled to increase with FP scale-up before declining. In 2013, 25.0% of currently married women in Sierra Leone had an unmet need for contraception, with 16.7% wanting to delay having (another) child and 8.3% not wanting any (more) children. Cross-country evidence suggests that from low levels, demand for FP increases faster than access and that the relationship between scaling up FP services and unmet need is best modelled as a hyperbola.41 In the high scenario, unmet need is therefore modelled to increase slightly initially, peaking at 28.5% in 2020 before declining over the next 15 years to 22.9% in 2035. In the medium scenario, unmet need increases less rapidly but takes longer to peak. These scenarios are compared to the counterfactual scenario of unmet need remaining constant at 25.0%.
In terms of mortality impact, there are modelled to be fewer maternal and infant deaths in the FP scale-up scenarios. The maternal mortality rate (MMRate) (The modelling approach of the FamPlan module within the OneHealth Tool means that the maternal mortality rate is more suitable for this analysis than the maternal mortality ratio because it captures the demographic impact of FP on maternal deaths.) is projected to decrease from 176 maternal deaths per 100,000 women age 15–49 years to an MMRate of 122 in 2035 in the medium scenario and 92 in the high scenario in 2035. This is compared to an MMRate of 151 by 2035 in the counterfactual scenario. This impact is explained largely through FP reducing the chance of pregnancy and therefore exposure to the risks associated with pregnancy and childbirth. The impact is estimated at 700 fewer maternal deaths a year by 2035 in the medium scenario and 1400 fewer maternal deaths a year in the high scenario, both compared to the counterfactual scenario. There are also projected to be fewer infant deaths in the FP scale-up scenarios: 700 fewer infant deaths a year in the medium scenario and 13,000 fewer in the high scenario by 2035, again compared to the counterfactual.
Investment requirements of scaling up FP
Table 2 summarises the estimated cost of the FP programme in Sierra Leone in 2013. We estimate a total cost of US$4.2 million, which can be broken down into direct costs of US$0.9 million (22%), health facility overhead costs of US$0.2 million (4%) and programme costs of US$3.1 million (74%). As programme costs are the main cost driver for the total costs of the FP programme, this is further broken down by the organisation delivering the programme-level activities. We estimate that the Ministry of Health and Sanitation delivers 43% (US$1.3 million) of programme-level activities, with community-based organisations delivering 33% (US$1.0 million) and UNFPA the remaining 24% (US$0.7 million). This includes expenditure on activities such as behaviour change communication, advocacy and policy work and monitoring and evaluation.
Table 2.
Estimated cost of FP services for Sierra Leone, 2013.
| USD, million | % | |
|---|---|---|
| Direct costs | US$0.9 | 22 |
| Health facility overhead costs | US$0.1 | 4 |
| Programme costs | US$3.1 | 74 |
| Total | US$4.2 | 100 |
Figure 4 shows the projected increase in expenditure required to achieve the FP scale-up scenarios. The model projects costs reaching US$7.5 million a year in the medium scenario and US$10.9 million a year in the high scenario by 2035. All costs are reported in constant 2013 USD. Expenditure is predicted to decrease slightly in the counterfactual scenario to US$3.9 million a year by 2035. (This is because we make the conservative assumption that FP programme costs in the counterfactual scenario have the same relationship with direct costs as in the FP scale-up scenarios.)
Figure 4.
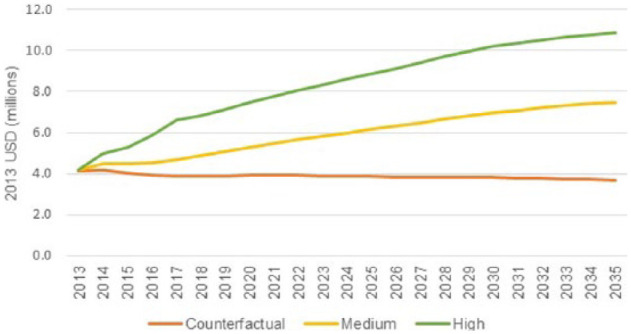
Projected costs of FP services for Sierra Leone, 2013–2035.
Financial viability analysis shows that the costs of FP services are well within the overall resource envelope for the health sector. In the high scenario, the total cost of FP services is projected to be 0.5% of total health expenditure and 4.6% of government health expenditure and 7.8% of domestic government health expenditure representing slightly decreased shares from 2013. While these results suggest that scaling up FP services seems to be financially viable, resources are not unlimited. In particular, such scaling up depends on overall government spending on health increasing at similar rates to GDP growth over time. These findings are also dependent on donors continuing to invest in the health sector in Sierra Leone.
Cost savings to other social services
Slower rates of population growth translate into costs savings to other social services as there are fewer people requiring these services. Table 3 shows the projected annual expenditure in 2035 for each of the services and scenarios and also the cumulative savings over the period 2013–2035 for the high and medium scenarios compared to the counterfactual.
Table 3.
Cumulative cost savings in five social sectors, 2013–2035.
| Social sector | Estimated 2013 expenditure (2013 USD, million) | Projected 2035 expenditure (2013 USD, million) | Cumulative cost savings compared to the counterfactual | |||||
|---|---|---|---|---|---|---|---|---|
| Medium scenario | High scenario | Counterfactual scenario | Medium scenario | High scenario | ||||
| Not discounted | Discounted at 3% | Not discounted | Discounted at 3% | |||||
| Primary education | 16.9 | 28.9 | 23.8 | 33.9 | 35.0 | 20.7 | 78.4 | 47.0 |
| Child immunisation | 6.0 | 11.6 | 8.4 | 15.2 | 36.8 | 23.5 | 75.0 | 48.8 |
| Malaria prevention | 0.4 | 0.8 | 0.6 | 1.0 | 2.1 | 1.3 | 4.3 | 2.7 |
| Maternal health services | 8.9 | 9.1 | 6.6 | 12.0 | 29.0 | 18.6 | 59.3 | 38.6 |
| Improved drinking water | 3.5 | 6.0 | 5.5 | 6.4 | 3.5 | 2.1 | 7.5 | 4.7 |
| Total | 35.6 | 56.4 | 44.9 | 68.5 | 106.3 | 66.3 | 224.4 | 141.8 |
Numbers may not add up due to rounding.
Figure 5 shows cumulative cost savings over time graphically. It is apparent that large cost savings from child immunisation and maternal health services are projected to accrue immediately, whereas those from primary education take some time to emerge, but by 2035, cumulative cost savings are the largest for this social sector.
Figure 5.
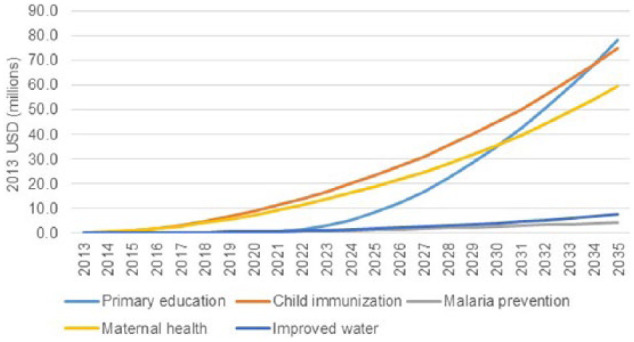
Cumulative cost savings of the high compared to the counterfactual scenario, 2013–2035.
Returns on investment
Table 4 shows the benefit–cost ratio and net present value at key time horizons for the FP scale-up scenarios compared to the counterfactual scenario. These results all apply a discount rate of 3%; we calculated the metrics using other discount rates (5% and 7%), but the results were not substantially different and hence are not reported here.
Table 4.
Investment metrics.
| Benefit–cost ratio | Net present value (2013 USD, million) | |||||
|---|---|---|---|---|---|---|
| To 2018 | To 2025 | To 2035 | To 2018 | To 2025 | To 2035 | |
| High scenario compared to the counterfactual | 0.8 | 1.3 | 2.1 | −1.1 | 10.3 | 73.2 |
| Medium scenario compared to the counterfactual | 0.9 | 1.4 | 2.1 | −0.2 | 5.1 | 35.4 |
For every dollar spent on FP services to achieve the high compared to the counterfactual scenario, Sierra Leone would save US$2.1 in the five social services of primary education, child immunisation, malaria prevention, maternal health services and improved drinking water over the period 2013–2035. This is a conservative estimate of the return on investment on FP services for Sierra Leone because we are comprehensively costing the investment required but valuing only the cost savings to five social services. There are likely to be cost savings to other services that are not included here as well as other benefits that we have not included in our benefit–cost calculations – in particular, the demographic dividend.
Under certain social and economic circumstances, having a larger proportion of the population of working age can lead to economic benefit. Tailoring a recent simulation model to our FP scale-up scenarios and the context of Sierra Leone, we estimate that income per capita could be 17% higher by 2035 in the high scenario compared to the counterfactual scenario, or 8% higher by 2035 in the medium scenario.37 The demographic dividend is coming about primarily from a lower dependency ratio but also from increased labour force participation by mothers as well as, later in the time period, higher savings, investment and productivity.
Results from sensitivity analysis
We focus our sensitivity analysis first on the costing of the FP programme – in particular, programme-level costs – because we make a significant assumption about how programme-level costs evolve over time. The uncertainty around our estimates of programme costs over time is difficult to quantify precisely, with scant literature on how costs evolve as an FP programme becomes established. In our sensitivity analysis, we therefore make some simple changes to our assumption that reflect the high degree of uncertainty around programme costs over time. In our worst-case scenario, we assume that programme costs do not decline as a proportion of direct intervention costs but remain at their current proportion. This would reflect a situation in which no economies of scale were realised and capacity development remained at its current level. In our best-case scenario, we assume that programme costs decline linearly over the time period so that the percentage in 2035 is a quarter of that of 2013.
As part of the sensitivity analysis, we also vary the scale-up of coverage of primary education, child immunisation, malaria prevention, maternal health services and improved drinking water. We make the conservative assumption that no scale-up of these key services occurs – that is, that coverage remains at 2013 values for all five services.
Our sensitivity analysis results show that the assumption of how programme costs evolve over time is an important one. Our central analysis is for the total cost of providing FP services in the high scenario to be US$10.9 million by 2035. In the worst-case scenario, the high scenario would cost US$17.3 million a year, while in the best-case scenario, it would cost US$7.7 million a year, in 2035. These are wide estimates, but importantly even in the worst-case scenario, benefits (i.e. cost savings from other sectors) still outweigh costs, as shown in Table 5. This is also the case under the conservative assumption, with FP programme costs returned to their base case values, that no scale-up of primary education, child immunisation, malaria prevention, maternal health services and improved drinking water occurs.
Table 5.
Sensitivity analysis.
| Assumption varied | Scenario | Comparison | Benefit–cost ratio | ||
|---|---|---|---|---|---|
| To 2018 | To 2025 | To 2035 | |||
| Programme cost projection | Worst-case scenario: programme costs remain constant over the time period at their current proportion of direct intervention costs | High scenario compared to the counterfactual | 0.9 | 1.2 | 1.6 |
| Medium scenario compared to the counterfactual | 0.8 | 1.2 | 1.6 | ||
| Best-case scenario: programme costs decline linearly over the time period so that the percentage in 2035 is a quarter of that of 2013 | High scenario compared to the counterfactual | 1.0 | 1.6 | 2.6 | |
| Medium scenario compared to the counterfactual | 1.0 | 1.6 | 2.7 | ||
| Coverage of other social services | Coverage remains at 2013 values for all five social services | High scenario compared to the counterfactual | 0.6 | 1.0 | 1.6 |
| Medium scenario compared to the counterfactual | 0.7 | 1.1 | 1.6 | ||
Discussion
Our results show that investment in FP services more than pays for itself over the period 2013–2035. In particular, for every US$1 invested in FP, Sierra Leone is projected to save US$2 across five essential social sector services. This translates into a net benefit of US$66.8 million over the period 2013–2035. This result reflects a conservative approach to the cost–benefit analysis, where monetised benefits are limited to cost savings, while comprehensively costing the activities at the wider population level required for FP services to be effectively implemented. While this is advantageous from a health policy and planning perspective, it makes comparisons to other published estimates difficult as projections where health systems and programme investments were ignored underestimate the required costs and overestimate the benefit–cost ratio.
That is, in addition to these monetised costs and benefits, there are other important benefits. First, there is the potential demographic dividend of a lower dependency ratio, with the associated boost to a country’s economic growth. The estimated demographic dividend is a substantial benefit (income per capita increasing by up to 17%) but is aligned with the estimates produced for the Lancet Global Investment Framework.8 We do not include it in our benefit–cost calculations because it is not a guarantee. That is, it will not come about from scaling up FP services alone but also requires investment in other areas – in particular, education, health, governance and the economy more widely – to be realised.
Second, there are important health benefits associated with the scaling up of FP. We found an estimated 1400 fewer maternal deaths and 700 fewer infant deaths a year by 2035 in the high scenario compared to the counterfactual. These health impacts are also not included in the benefit–cost calculation. Although common to assign a value to health gains, doing so is conceptually different from including benefits in terms of reduced expenditure that already in monetary terms. Finally, we do not model the benefits in terms of women’s rights, gender equality and women’s empowerment that are more appropriately assessed qualitatively.
These are ambitious scale-up scenarios, but they are not without historical precedent. Rwanda, another post-conflict country, experienced an increase in the CPR for married women from 13% in 2000 to 52% in 2010.42 Ethiopia has also experienced a large increase in contraceptive use, with the CPR for married women increasing from 8% to 29% between 2000 and 2010. Assuming linear scale-up, this means that Rwanda achieved a 3.9 percentage point increase each year for 10 years and Ethiopia a 2.1 percentage point increase. Our medium scenario models a 0.8 percentage point increase each year over 22 years and our high scenario a 1.5 percentage point increase on average.
However, achieving this sustained increase will require a political and financial commitment from the government and donors to strengthening Sierra Leone’s health system post-Ebola. With evidence that the Ebola crisis has reduced use of FP services, exposing weaknesses in an already fragile health system, increasing the number of health workers with the right skill mix and improving behavioural change communication are all the more essential to meeting unmet need and increasing uptake of FP services. Policymakers in Sierra Leone could use the findings first to make the case for increased investment in FP services, both in terms of the economic payoff from reduced expenditure requirements for other social services later and in terms of the improved health for the country’s women and children. The estimates of the direct intervention requirements and costs should provide policymakers with a good estimate of the drugs, supplies and medical personal required to achieve this level of scale-up. The associated programme costs are more uncertain, as noted, but current expenditure could be used as the basis for a costed implementation plan for future programming requirements.
The study faced a number of limitations. We modelled scaling up FP services to currently married women of reproductive age, which is the target population for many FP studies. However, it does exclude the smaller but important group of sexually active non-married women, almost half of whom are adolescents. Data on unmet need for this group are limited; for example, only unmet need for currently married women is provided in the 2013 DHS. However, the fact that 28% of women aged 15–19 years have begun childbearing, with potential risks to their health and education, is indicative of a large unmet need for this group.
Lack of evidence for how programme costs are expected to evolve over time is a source of major uncertainty for our model. Unfortunately, the literature again is relatively scarce on this issue, but time-series evidence does broadly suggest that they increase at a decreasing rate as FP services are scaled up.27 We therefore use this general shape for our base case and vary the assumption in the sensitivity analysis. This indicates that benefits still outweigh costs even with more pessimistic assumptions about programme costs over time.
Conclusion
There is a strong investment case for scaling up FP services in Sierra Leone. The ambitious scale-up scenarios have historical precedent in other sub-Saharan African countries, but the extent to which they will be achieved depends on a commitment from both the government and donors to strengthening Sierra Leone’s health system post-Ebola and focusing attention on FP services. The focus of our analysis is on modelling the implications of different scenarios, rather than the steps required to achieve scale-up; however, policy recommendations emerging from the study include the following:
Engage in high-level advocacy using this study and others to convince the Government of Sierra Leone that FP is worth the investment.
Ensure that the public sector FP has its own budget line and is properly resourced.
Set up an inter-sectoral committee to provide government leadership on the policies that will be required to harness the demographic dividend.
Analyse the feasibility of achieving the CPR scale-up targets modelled in this study, including evaluating alternative service delivery modalities.
Train staff from the Ministry of Health and Sanitation and the Ministry of Finance to use the OneHealth Tool so that this cost–benefit analysis – including future monitoring of costs and benefits to FP – can be domesticated in Sierra Leone.
Our study could inspire other researchers to create other country-specific investment cases for FP services, allowing for a clearer understanding of the costs and benefit across health as well as non-health sectors including education and Water, Sanitation and Hygiene (WASH). These country-specific investment cases, as in Sierra Leone, would help policymakers make informed decisions for resource allocation and health planners craft data-driven health policies.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
References
- 1. Bryce J, Victora C, Berman P, et al. Fulfilling the health agenda for women and children: the 2014 report, 2014, https://data.unicef.org/wp-content/uploads/2015/12/Countdown_to_2015-Fulfilling-the-Health_Agenda_for_Women_and_Children-The_2014_Report-Conference_Draft_159.pdf [DOI] [PMC free article] [PubMed]
- 2. Leone S. The status of women and children in Sierra Leone, https://books.google.co.in/books/about/The_status_of_women_and_children_in_Sier.html?id=cLa3AAAAIAAJ&redir_esc=y
- 3. Leone S. Health survey, 2008, http://www.mamaye.org.sl/sites/default/files/evidence/SL%20DHS%202008.pdf
- 4. Statistics Sierra Leone, ICF International. Sierra Leone demographic health survey 2013. Rockville, MD: ICF International, 2014. [Google Scholar]
- 5. Alkema L, Kantorova V, Menozzi C, et al. National, regional, and global rates and trends in contraceptive prevalence and unmet need for family planning between 1990 and 2015: a systematic and comprehensive analysis. Lancet 2013; 381(9878): 1642–1652. [DOI] [PubMed] [Google Scholar]
- 6. UNFPA. Rapid assessment of Ebola impact on reproductive health services and service seeking behaviour in Sierra Leone table of contents, 2015, http://www.mamaye.org.sl/sites/default/files/evidence/UNFPA%20study%20_synthesis_March%2025_final_d.pdf
- 7. Osotimehin B. Family planning save lives, yet investments falter. Lancet 2012; 380(9837): 82–83. [DOI] [PubMed] [Google Scholar]
- 8. Stenberg K, Axelson H, Sheehan P, et al. Advancing social and economic development by investing in women’s and children’s health: a new Global Investment Framework. Lancet 2014; 383(9925): 1333–1354. [DOI] [PubMed] [Google Scholar]
- 9. Cleland J, Conde-Agudelo A, Peterson H, et al. Contraception and health. Lancet 2012; 380(9837): 149–156. [DOI] [PubMed] [Google Scholar]
- 10. Ahmed S, Li Q, Liu L, et al. Maternal deaths averted by contraceptive use: an analysis of 172 countries. Lancet 2012; 380(9837): 111–125. [DOI] [PubMed] [Google Scholar]
- 11. Wegbreit J, Bertozzi S, DeMaria LM, et al. Effectiveness of HIV prevention strategies in resource-poor countries: tailoring the intervention to the context. AIDS 2006; 20(9): 1217–1235. [DOI] [PubMed] [Google Scholar]
- 12. Rutstein SO. Further evidence of the effects of preceding birth intervals on neonatal, infant and under-five-years mortality and nutritional status in developing countries: evidence from the demographic and health surveys, 2008, https://dhsprogram.com/pubs/pdf/WP41/WP41.pdf [DOI] [PubMed]
- 13. Moreland S, Talbird S. Achieving the Millennium Development Goals: the contribution of fulfilling the unmet need for family planning, 2006, http://pdf.usaid.gov/pdf_docs/Pnadm175.pdf
- 14. O’Neill BC, Liddle B, Jiang L, et al. Demographic change and carbon dioxide emissions. Lancet 2012; 380(9837): 157–164. [DOI] [PubMed] [Google Scholar]
- 15. Gribble JN, Bremner J. Achieving a demographic dividend. Popul Bull 2012; 67(2): 1–12. [Google Scholar]
- 16. Joshi S, Schultz TP. Family planning as an investment in development and female human capital: evaluating the long term consequences in Matlab, Bangladesh, 2006, http://paa2006.princeton.edu/download.aspx?submissionId=60499
- 17. Singh S, Darroch JE, Vlassoff M, et al. Adding it up: the benefits of investing in sexual and reproductive health care. New York: Guttmacher Institute, 2003. [Google Scholar]
- 18. Singh S, Darroch JE. Adding it up: costs and benefits of contraceptive services estimates for 2012. New York: Guttmacher Institute, 2012. [Google Scholar]
- 19. Singh S, Darroch JE, Ashford LS. Adding it up: the costs and benefits of investing in sexual and reproductive health 2014. New York: Guttmacher Institute, 2014. [Google Scholar]
- 20. Avenir Health. OneHealth Tool, 2015, http://www.avenirhealth.org/software-onehealth.php (accessed 26 July 2015).
- 21. Government of Sierra Leone. The Agenda for Prosperity: Sierra Leone’s third generation poverty reduction strategy paper (2013–2018), 2013, http://www.undp.org/content/dam/sierraleone/docs/projectdocuments/povreduction/undp_sle_The%20Agenda%20for%20Prosperity%20.pdf
- 22. Sinding SW, Ross JA, Rosenfield AG, et al. Seeking common ground: unmet need and demographic goals. Int Fam Plan Perspec 1994; 20(1): 23–27. [Google Scholar]
- 23. Habumuremyi PD, Zenawi M. Making family planning a national development priority. Lancet 2012; 380(9837): 78–80. [DOI] [PubMed] [Google Scholar]
- 24. Johns B, Baltussen R, Hutubessy R. Programme costs in the economic evaluation of health interventions. Cost Eff Resour Alloc 2003; 1(1): 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. United Nations: Department of Social and Economic Affairs. World population prospects: the 2012 revision, DVD edition. Popul Div 2013, http://esa.un.org/unpd/wpp/Excel-Data/population.htm
- 26. Government of Sierra Leone. Education country status report: an analysis for further improving the quality, equity and efficiency of the education system in Sierra Leone, 2013, http://unesdoc.unesco.org/images/0022/002260/226039e.pdf
- 27. Wolfson LJ, Gasse F, Lee-Martin SP, et al. Estimating the costs of achieving the WHO-UNICEF Global Immunization Vision and Strategy, 2006-2015. Bull World Health Organ 2008; 86(1): 27–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jamison DT, et al. Investing in a grand convergence in health: methodology. Supplementary web appendix 4, 2003, http://globalhealth2035.org/sites/default/files/2035/appendix-4.pdf
- 29. World Health Organization (WHO). Constraints to scaling up the health Millennium Development Goals: costing and financial analysis gap. Geneva: WHO, 2010. [Google Scholar]
- 30. Hutton G. Global costs and benefits of drinking-water supply and sanitation interventions to reach the MDG target and universal coverage (Note: Unit costs are assumed to remain the same for the period 2013–2035). Geneva: World Health Organization (WHO), 2012. [Google Scholar]
- 31. Mills A. The economics of hospitals in developing countries. Part I: expenditure patterns. Health Policy Plan 1990; 5(2): 107–117. [Google Scholar]
- 32. Mills AJ, Kapalamula J, Chisimbi S. The cost of the district hospital: a case study in Malawi. Bull World Health Organ 1993; 71(3–4): 329–339. [PMC free article] [PubMed] [Google Scholar]
- 33. Aboagye AQ, Degboe AN, Obuobi AA. Estimating the cost of healthcare delivery in three hospitals in southern Ghana. Ghana Med J 2010; 44(3): 83–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Moreland S. Methods for estimating the costs of family planning. Chapel Hill, NC: University of North Carolina at Chapel Hill, 2011. [Google Scholar]
- 35. Ministry of Health and Sanitation. Sierra Leone National Health Accounts, 2013, http://www.mamaye.org/sites/default/files/evidence/MoHS%20SL_2015_Sierra%20Leone%20NHA%202013.pdf
- 36. Datta S, Winfrey B. OneHealth Tool: technical notes, 2012, http://avenirhealth.org/Download/Spectrum/Manuals/OneHealth_technical_manual_annexes_2012_02_07.pdf
- 37. Ashraf QH, Weil DN, Wilde J. The effect of fertility reduction on economic growth. Popul Dev Rev 2013; 39(1): 97–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gerdtham U-G, Jönsson B. Chapter 1. International comparisons of health expenditure: theory, data and econometric analysis. Handb Heal Econ 2000; 1: 11–53. [Google Scholar]
- 39. UN Sustainable Development Knowledge Platform. Total fertility rate, 2015, http://www.un.org/esa/sustdev/natlinfo/indicators/methodology_sheets/demographics/total_fertility_rate.pdf (accessed 15 September 2015).
- 40. Bongaarts J. A framework for analyzing the proximate determinants of fertility. Popul Dev Rev 1978; 4(1): 105–132. [Google Scholar]
- 41. Friberg I, Winfrey B. Understanding how FamPlan calculates the numbers of abortions and their impact on MMR in LiST, 2012, http://www.jhsph.edu/research/centers-and-institutes/institute-for-international-programs/_documents/manuals/MMRabortions-family-planning.pdf
- 42. National Institute of Statistics Rwanda. Rwanda demographic and health survey 2010. Rockville, MD: Ministry of Health, ICF International, 2012. [Google Scholar]


