Abstract
Mounting evidence has emphasized the potential of cell therapies in treating various diseases by restoring damaged tissues or replacing defective cells in the body. Cell therapies have become a strong therapeutic modality by applying noninvasive in vivo molecular imaging for examining complex cellular processes, understanding pathophysiological mechanisms of diseases, and evaluating the kinetics/dynamics of cell therapies. In particular, mesenchymal stem cells (MSCs) have shown promise in recent years as drug carriers for cancer treatment. They can also be labeled with different probes and tracked in vivo to assess the in vivo effect of administered cells, and to optimize therapy. The exact role of MSCs in oncologic diseases is not clear as MSCs have been shown to be involved in tumor progression and inhibition, and the exact interactions between MSCs and specific cancer microenvironments are not clear. In this review, a multitude of labeling approaches, imaging modalities, and the merits/demerits of each strategy are outlined. In addition, specific examples of the use of MSCs and in vivo imaging in cancer therapy are provided. Finally, present limitations and future outlooks in terms of the translation of different imaging approaches in clinics are discussed.
Keywords: Cell therapy, Mesenchymal stem cells, In vivo molecular imaging, Drug delivery, Superparamagnetic iron oxide
Core Tip: There is substantial evidence of the potential of cell therapies in treating various diseases including cancers. Molecular imaging has been actively used for decades to assess cellular processes, evaluate the properties of certain drugs, screen compound libraries, and visualize the fate of cells. This review aimed to confirm whether noninvasive in vivo cell tracking in combination with molecular imaging could be used as a tool for the development of mesenchymal stem cell-based cancer treatment. To that end, the following aspects are outlined in the text: labeling approaches, imaging modalities, advantages and disadvantages of each strategy, and scope and limitations of the various imaging approaches. In conclusion, together with long-term monitoring, a lot can be learned with regard to the hidden potential of MSCs as well as their variable fate in humans.
INTRODUCTION
Cell-based therapy and in vivo imaging
Cell therapies are becoming increasingly popular because of their ability to restore or replace damaged tissues, thereby directly impacting disease progression. Cell-based therapies can be developed with the use of any cell type including primary, stem, immune, or progenitor cells. Various cell-based therapies are presently being tested at the preclinical level. Some of them have even reached clinics (e.g., hematopoietic stem cell transplantation for blood disorders[1]) and are awaiting approvals[2]. The translation of cell therapies holds great promise for promotion in the field of regenerative medicine.
Mesenchymal stem cell (MSC) therapy has been particularly successful in preclinical models. The timing of MSC administration has been found to be among the key factors in the determination of the efficacy of cell-based therapies[3]. Evidence proposes that even though MSCs are retained in certain sites, such as the lungs, intestine, and lymph nodes[4], they have a role in macrophage recruitment to the sites of injury and enhancing wound healing through paracrine effects[5]. As with numerous other diseases, MSC therapy has the potential to treat cancerous diseases through migration to the tumor microenvironment. While several studies have exhibited an inhibitory effect of MSCs on full-grown tumors[6,7], MSCs are also involved in the progression of some cancers[8,9]. The exact function of MSCs in cancerous diseases is controversial and warrants further investigation.
A combination of cell-based therapies and imaging has revolutionized the field of medicine over the last two decades. Better efficacy of cell-based therapies can be achieved through noninvasive monitoring of transplanted cells with the help of molecular imaging tools. In particular, in vivo imaging has become an essential tool for monitoring disease status in longitudinal studies[10]. It is exhaustively utilized to study cancerous diseases, autoimmune disorders, neurological diseases, and cardiovascular diseases. With the use of in vivo three-dimensional (3D) imaging, different biological processes including gene expression, protein trafficking, and cell migration/ homing/tumor infiltration can be visualized using high resolution[11]. For studies involving animal models, readouts can be acquired with the use of the same animal over time, thereby reducing the sample size and discrepancies in measurements[12]. Implementing in vivo imaging at the preclinical level can save a lot of time, money, and resources, which can then be invested in clinical studies. Also, based on preclinical outcomes, scientists and physicians can make informed decisions with regard to the rapid translation of these approaches to the clinical level[13,14].
For a particular study, it is essential to consider whether in vivo imaging would be superior to other approaches including conventional histopathology, which might be the gold standard for animal studies. Nonetheless, histopathology is a time-consuming and labor-intensive process. Errors can occur during the sampling of tissue and subsequent processing, thereby presenting a bias in studies[15]. Small animals utilized for in vivo preclinical imaging can also pose some challenges in terms of handling, maintaining their physiological balance, administering an appropriate dose of anesthetic, and protecting them from radiation[15]. Overall, in vivo imaging is much faster and is better equipped to capture dynamic interactions between administered cells and its targets without having to sacrifice the animal. On the other hand, histopathological analyses can uncover unique information that imaging platforms may overlook. In most cases, a combination of these two approaches is utilized to confirm the findings and overcome the flaws correlated with each modality.
It is crucial to choose the optimal strategy for in vivo imaging, depending upon the research question you are trying to answer. Some imaging modalities offer high resolution and others provide high sensitivity. The cost should also be taken into account because imaging platforms can be very expensive to set up. The strategy should be selected carefully to avoid possible interference with the animal’s physiology to acquire accurate as well as reproducible results. Some frequently utilized approaches including nuclear imaging, optical imaging, and magnetic resonance imaging are discussed later in this review along with their advantages and disadvantages. Preferably, an imaging tool should be highly specific and sensitive in tracking cell viability, cause minimal or no toxicity to cells, and allow long-term monitoring, the characteristics that are impossible to be achieved through the use of a single approach[16]. Thus, multimodal imaging approaches, where two or more imaging modalities are combined to achieve the best results, are widely utilized[17].
LABELING OF MSCS WITH IMAGING REPORTERS
MSCs are inhomogenous adult stem cells and have the ability to differentiate into any cell type with a mesodermal origin[18,19]. MSCs account for 0.01% of the total mononuclear cells found in the bone marrow[20]. Major sources of MSCs are bone marrow, fat, cord blood, and dental pulp[21]. Cells are first isolated from these sources and then expanded in vitro prior to administration to a patient. MSCs are also often manipulated with the use of ex vivo viral-vector-mediated gene modifications[22]. The advantage of working with MSCs is their low immunogenicity[23], thereby suppressing rejection by the host immune system. The efficacy of MSC therapy can be improved by reprogramming or manipulating the cells to overexpress the gene of interest and utilize them for the targeted delivery of therapeutic proteins to the desired area[24].
Labeling MSCs and tracking them in vivo with the use of noninvasive imaging tools have proven to be a powerful strategy in the last few decades. This approach can yield a lot of useful information relating to the overall stem cell behaviors such as migration pattern, retention capacity, and immune clearance of cells[16]. MSCs can be labeled either directly through their conjugation with probes or indirectly through the introduction of exogenous reporter genes. Labeled cells can then be visualized with the use of imaging modalities including optically charged coupled devices, positron-emission tomography (PET), magnetic resonance imaging (MRI), and single-photon emission computed tomography (SPECT).
Direct labeling
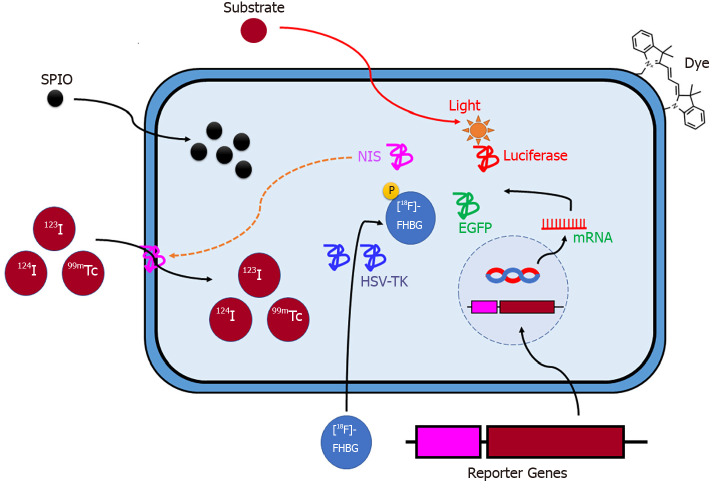
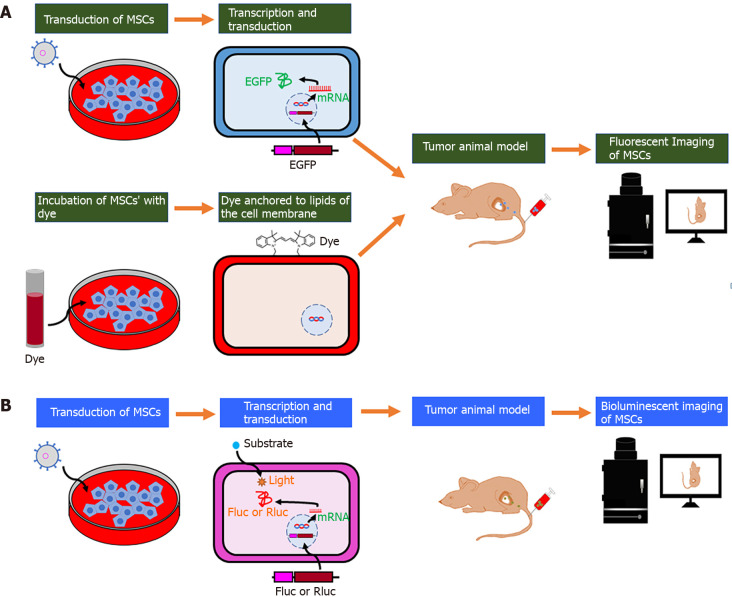
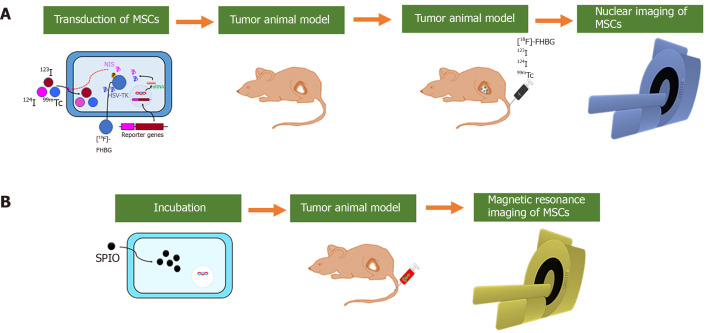
In the direct labeling approach, different labeling agents including quantum dots (QDs)[25], fluorophores[26], radionuclides[27], and superparamagnetic iron oxide particles (SPIO)[28] can be utilized to tag MSCs, which can then be imaged after their transplantation into living organisms. In this strategy, labeling agents serve as surrogate markers for the number of stem cells (Figures 1, 2A and 3).
Figure 1.
Schematic illustration of labeling mesenchymal stem cells for in vivo non-invasive imaging. SPIO: Small superparamagnetic iron oxide; NIS: Sodium iodide symporter; HSV-TK: Herpes simplex virus-thymidine kinase; EGFP: Enhanced green fluorescent protein; [18F]FHBG: 9-(4-[F]fluoro-3-hydroxymethylbutyl) guanine.
Figure 2.
Schematic illustration of the labeling strategy for in vivo tracking of mesenchymal stem cells by optical imaging. A: After fluorescent protein (enhanced green fluorescent protein) transduction into mesenchymal stem cells (MSCs) or binding of lipophilic labeling agents (e.g., fluorescent nanoparticles and VivoTrack 680) to the membrane of MSCs, cells are injected into the tumor-bearing mice, and their migration is visualized with the use of in vivo fluorescent imaging; B: After the bioluminescent protein (Firefly or Renilla luciferase) transduction into MSCs, cells are injected into the tumor-bearing mice. The light emitted due to the interaction between luciferase and its substrates (D-luciferin or coelenterazine) is captured by in vivo bioluminescent imaging. MSCs: Mesenchymal stem cells; EGFP: Enhanced green fluorescent protein; Fluc: Firefly luciferase; Rluc: Renilla luciferase.
Figure 3.
Schematic illustration of the labeling strategy for in vivo tracking of mesenchymal stem cells by nuclear and magnetic resonance imaging. A: Gene transduction of sodium iodide symporter (NIS) or herpes simplex virus-thymidine kinase (HSV-TK) into mesenchymal stem cells (MSCs) can aid radiotracers (123I, 124I and 99mTc) in entering MSCs. MSCs-NIS are injected into tumor-bearing mice followed by the injection of radiotracers. In vivo nuclear imaging (positron-emission tomography, camera imaging, and single-photon emission computed tomography) can visualize migration of the MSCs; B: MSCs can be incubated with molecules including small superparamagnetic iron oxide (SPIO) or SPIO coated with gold-nanoparticles (SPIO@Au-NPs). SPIO-labeled MSCs are injected into tumor-bearing mice, and in vivo magnetic resonance imaging can visualize migration of the MSCs. MSCs: Mesenchymal stem cells; NIS: Sodium iodide symporter; HSV-TK: Herpes simplex virus-thymidine kinase; 99mTc: Technetium-99m; [18F]FHBG: 9-(4-[F]fluoro-3-hydroxymethylbutyl) guanine; SPIO: Superparamagnetic iron oxide.
Fluorophores, especially QDs, are widely utilized for in vivo tracking of MSCs in longitudinal studies. QDs emit fluorescence upon excitation, which can be achieved with a range of different wavelengths. Some of the merits of labeling cells with QDs include high sensitivity and excellent resolution[29]. QDs have been utilized to label and monitor MSCs[30,31] either through passive incubation or targeting peptide-mediated delivery, such as the one used with the Qtracker labeling kit[25,32]. QDs have been found to be biocompatible in studies performed with the use of in vitro models, and QD-labeled MSCs were integrated successfully in co-culture systems[32]. Besides QDs, lipophilic fluorescent tracer dye such as DiD is another molecule that causes low cytotoxicity to MSCs and can give better contrast[33]. In recent years, near-infrared (NIR; 700-1000 nm wavelength) fluorophores have been utilized in the clinical setting due to their ability to penetrate deeply located tissues (penetration depth: approximately 4-10 cm), although cardiac imaging is still a challenge. In a previous study, the authors labeled MSCs with the NIR fluorophore IR-786 and delivered them to the coronary artery in a swine model of myocardial infarction. MSC behavior was then successfully monitored 90 min post-injection[34].
Radionuclides can also be utilized to label cells prior to transplanting them into living subjects. Some examples of radioisotopes are Technetium-99m (99mTc; half-life 6 h), Indium-111 (111In; half-life 2.8 d), Fluorine-18 (18F; half-life 109 min), and Copper-64 (64Cu; half-life 12 h). Depending on their physical half-lives, cells labeled with these isotopes can be tracked using imaging tools over a timeframe, ranging from hours to days. Zirconium-89 (89Zr; half-life 3.3 d) is becoming popular because of its long half-life, thereby allowing long-term monitoring of MSCs with PET imaging[35]. The biological half-life of radioisotopes should also be taken into account while choosing a suitable radiotracer for the study[36]. Several studies have reported labeling of MSCs with isotopes including 111In, 18F-fluoro-deoxyglucose (18F-FDG), 2′-18F-fluoro-5-ethyl-1-beta-D-arabinofuranosyluracil (18F-FEAU), 131I-2′-fluoro-2′-deoxy-1-beta-D-arabinofuranosyl-5-iodouracil (131I-FIAU) and 99mTc-D,L-hexamethylene-propyleneamine oxime (99mTc-HMPAO), and subsequent monitoring of cells using imaging strategies including SPECT or PET[37-40]. Interestingly, previous reports have shown long-term monitoring of MSCs in vivo up to 10-14 d when the cells were labeled with 111In[41,42].
Labeling of MSCs with SPIO enables in vivo tracking of cells by modifying T2 relaxivity[43,44]. Approaches including electroporation or liposome-mediated delivery can be utilized to introduce SPIOs into cells, which can then be transplanted into the living organism and imaged using high-resolution MRI[45]. Earlier studies showed the usefulness of this approach in the in vivo visualization of MSCs in real time and functional studies involving internal organs[45,46]. Increased cellular uptake of SPIOs and marginal cytotoxicity was noted with the incorporation of a transfection agent at an optimal concentration[47]. Alternatively, magneto-electroporation, a new technique that stimulates SPIO endocytosis, can be utilized to quickly label MSCs without transfection agents. This technique has previously been utilized to track MSCs in a peripheral arterial disease rabbit model[48]. Another study imaged SPIO-labeled MSCs in rats and indicated that these cells may promote the healing of the tendon-to-bone tunnel 4-8 wk post-surgery[49]. In a brain injury rat model, it was shown that MSCs remain at the lesion site for more than 30 d, as visualized by SPIO labeling and MRI, and improve survival[50]. A previous report indicated the use of ferumoxytol, an ultra-small SPIO nanoparticle (USPION), to monitor MSCs by MRI[51]. USPIONs are a class of coated nanoparticles with various applications. Ferumoxytol, a Food and Drug Administration (FDA)-approved molecule, has shown promising results for imaging MSCs in mouse models, showing its potential use in future clinical trials.
The direct labeling approach can also be utilized with multimodal imaging. A previous study utilized mesoporous silica nanoparticles to label MSCs, which were delivered to an orthotopic U87MG glioblastoma model, and tracked the labeled MSCs with the use of a multimodal approach through the combinatorial imaging of MRI, fluorescence, and PET[52]. USPION labeling did not modify the differentiation potential or protein content of MSCs[53]. Imaging indicated that particles loaded into MSCs were quickly taken up by tumor cells and had long retention time in comparison with those used alone[52].
Indirect labeling
Cells can be labeled indirectly through the stable or transient expression of exogenous reporter genes. This approach improves our understanding of stem cell biology and associated mechanisms by allowing us to study the stem cell behavior over time following transplantation in living subjects (animal models of different diseases or humans)[54,55]. Incorporated reporter genes are transcribed and translated in viable cells, resulting in the expression of proteins, which interact with suitable substrates to generate a signal that can then be captured using different imaging modalities (Figure 2B and 3A).
Reporter genes including Firefly luciferase (Fluc) and Renilla luciferase (Rluc) in combination with bioluminescence imaging (BLI) are widely utilized for the tracking of stem cell viability post-transplantation in living subjects. A light is emitted when Fluc interacts with the substrate D-luciferin; it can be captured by a light-sensitive imaging apparatus including BLI. In a myocardial infarction murine model, BLI revealed the death of MSCs at 3 wk post-transplantation, showing the possible association between survival of the cell and cardiac function[56]. Another BLI study revealed the death of in vivo administered MSCs in a mouse model of peripheral vascular disease[57]. A previous study utilized the BLI approach to evaluate the mitochondrial function of implanted MSCs using Fluc driven by the NQO1 enzyme promoter in a murine myocardial ischemia/reperfusion (IR) model, which revealed an inverse relationship between the promoter activity and mitochondrial function[58]. Another study performed by Psaltis et al[59] showed higher oxidative stress in MSCs transplanted in a myocardial IR rat model using rat MSCs expressing Fluc driven by the NAD(P)H p67phox promoter, in comparison with the cells in sham controls.
MSCs can also be labeled with nuclear medicine reporter genes and imaged with PET or SPECT. In this approach, a reporter gene encoding a specific protein or enzyme (including herpes simplex virus type 1 thymidine kinase; HSV1-tk) is presented into the cells. MSCs expressing the construct induce a strong signal because of intracellular retention of suitable probes through their phosphorylation by the action of the reporter proteins, whereas normal cells without the construct exhibited a trivial signal because of the minimal phosphorylation of the probes which go in and out of cells, when PET imaging of tumor models was performed[60]. HSV1-tk, being a viral protein, is immunogenic; therefore, it is the target of the host immune system, leading to further reduction in sensitivity of the reporter protein. Proteins of mammalian origin including dopamine receptor and mitochondrial tk have been developed as nuclear medicine reporter genes to avoid this issue[61]. Probes [e.g., 3-N-(2’-[18F]-fluoroethyl)-spiperone ([18F]FESP)] for a reporter gene of dopamine receptor are supposed to bind specifically to the membrane protein and be captured with PET. The use of mutant dopamine receptor rather than the wild-type protein is suggested for the prevention of the subsequent biological response, but it will still be able to bind to the probe. The drawback of this strategy is that it produces a limited signal because of the interaction of the receptor with only one ligand molecule[61]. In one study, authors transplanted human MSCs, expressing a mutated version of the dopamine type 2 receptor into athymic rats. PET imaging using 18F-fallypride showed a strong signal in vivo up to 7 d post-transplantation[62]. Aside from the dopamine receptor and HSV-tk1, the sodium-iodide symporter (NIS) has also been utilized as a nuclear medicine reporter gene to monitor MSC differentiation[63] and visualize migration of the MSCs to breast cancer[64]. NIS gene encodes a transmembrane protein, which is responsible for the influx of iodine into the cells. A previous study derived MSCs from the bone marrow of transgenic mice, expressing NIS and tracking their differentiation into cardiomyocytes in vitro after all-trans retinoic acid treatment. The study showed an increased uptake of 125I by treated cells, showing a higher reporter gene activity than the untreated cells[63]. Another study assessed the potential of NIS-expressing MSCs to treat breast cancer in vivo. SPECT imaging with 99mTc indicated the localization of the MSCs to the tumor tissue 14 d after implantation of the cells. The reporter gene of NIS can also be utilized as a therapeutic gene. Following the administration of another NIS probe, 131I, which emits cytotoxic beta rays, the tumor regressed[64]. Other examples of nuclear medicine reporter genes utilized with PET and SPECT imaging include the neurotensin receptor subtypes, the somatostatin receptor, and cytosine deaminase[61]. The use of hybrid reporter genes enables in vivo imaging of MSCs with multimodal approaches[65]. MSCs derived from porcine bone marrow were engineered to express a trifusion protein comprising renilla luciferase, red fluorescent protein, and herpes simplex truncated tk through lentivirus-mediated transfection and injected into a myocardial infarction pig model. Cell monitoring with [18F]-FHBG PET showed the retention of MSCs in the myocardium 10 d post-injection as well as a smaller infarct size in MSC-treated animals than that in control animals[66].
Advantages and disadvantages of each labeling approach
Direct labeling: Direct labeling techniques are quick and easy to perform. The concentration of labeling agents can be precisely controlled. Despite these advantages, direct labeling with fluorescent probes and subsequent optical imaging do not always yield the best results due to the decline in concentration and signal attenuation in the tissue over time. As a result, optical imaging is not appropriate for tissues that are located deep inside the body and for long-term monitoring of cells. The development of new probes with better penetration ability may settle the issue of tissue depth.
Radionuclide labeling coupled with PET imaging is a highly sensitive technique since it enables the detection of even a small number of MSCs (6250-25000 cells)[41,67,68]. Even though some cell types are sensitive to radionuclide labeling, MSCs are relatively tolerant to radiation exposure[68]. There is also an indication that cytotoxicity may be a function of time instead of being dose-dependent. In that case, it is easy to misinterpret the situations where cell viability looks intact immediately following labeling[69]. Also, it is impossible to acquire key data relating to cell viability and proliferation with direct labeling techniques. The signal can be acquired regardless of whether the cell is dead or alive and even when the label is not correlated with cells, thereby increasing the probability of obtaining false-positive results. Radionuclides, being high-energy particles, are less prone to tissue attenuation and are thus frequently utilized in a clinical setting.
The advantage of MRI is that it allows us to visualize MSC behavior immediately post-transplantation[70]. An FDA-approved T1 contrast agent such as gadopentetate dimeglumine (Gd-DTPA; Magnevist) was utilized by Liu et al[71] to track MSCs in animal models of hemorrhagic spinal cord injury.
SPIO labeling may impact the proliferation, metabolic activity, viability, and overall morphology of MSCs, limiting their use[43]. Interestingly, Feridex (SPIO), a commercial paramagnetic material, demonstrated no effect on the physiological properties of MSCs, proposing their possible usefulness in the clinical setting[72]. Overall, SPIO labeling has low sensitivity and cannot detect the presence of a small number of cells[68]. Cellular quantification is challenging with SPIO because of the decline in the label concentration and changes in spatial distribution during cell division and migration, respectively.
Other direct labeling agents such as nanoparticles may interfere with the cellular function. In a previous study, gold nanorods were utilized as contrast agents to image MSCs in mice. The results show that even though these agents did not cause any toxicity or impact cell proliferation, the expression of 1 out of 26 cytokines (interleukin-6) was modified[73]. Similarly, commonly used radioisotopes for nuclear imaging may impact the proliferation of MSCs at high doses, likely because of underlying DNA damage[74]. The choice of labeling agent should be carefully weighed depending upon the cell type and application of interest.
In conclusion, direct labeling methods might be ideal for short-term monitoring of cells, to ensure that cells are actually being delivered to the tissue of interest. Other labeling approaches should be considered for investigating the functional attributes of stem cells over a longer period of time.
Indirect labeling: Indirect labeling approaches enable long-term monitoring of cell viability through the utilization of constitutive-promoter-driven reporter gene transfection. Under the cytomegalovirus (CMV) promoter, reporter genes are always transcribed and translated into proteins if the cell is viable; however, gene silencing of CMV promoter over time[75] reduces the signal, thereby leading to diminished production of reporter proteins. This phenomenon could be misinterpreted as a decline in cell viability. Nowadays, constitutive promoters of mammalian origin including ubiquitin and β-actin are being utilized because they are less prone to gene silencing and may be better for determining cell survival. A previous report showed little or no change in phenotype and differentiation capacity of MSCs following the incorporation of reporter genes[76].
While a reporter protein of green fluorescent protein gives rise to a strong signal, the signal is reduced during tissue penetration due to absorption and refraction, thereby limiting its use to label tissues that are only up to 2 mm deep in the animal body[77]. Thus, this strategy is more useful for cell sorting during in vitro or ex vivo analysis of cells.
Reporter genes utilized for PET and SPECT, including HSV-tk1 and NIS, can aid in the identification of live cells in vivo. Earlier studies have reported an effective use of NIS for in vivo imaging of MSCs in an animal breast cancer model[64].
Finally, there are concerns that reporter genes may integrate at random sites, possibly resulting in a change of characteristics in the transfected MSCs from their parent cells. Present advances in gene editing technologies have made site-specific DNA integration possible, thereby alleviating the concern[78]. Many research groups are already developing new probes to meet the criteria set forth by the FDA and other regulatory bodies.
APPLICATION OF NONINVASIVE IN VIVO IMAGING OF MSCS IN TREATMENT AND DRUG DELIVERY FOR CANCER
Different attempts have been made to develop cell-based therapies and cell-based drug delivery systems for cancerous diseases[21,79,80]. Researchers and clinicians are excited about the possibility for MSC-based therapies to treat different tumors and utilize MSCs as a drug delivery vehicle by bioengineering the cells. Recent developments in in vivo molecular imaging modalities allow us to understand the fate of MSCs in living subjects. The in vivo molecular imaging for visualizing homing of MSCs to target lesions, evaluating their therapeutics effects and proving drug delivery capabilities of MSCs to tumors are discussed with examples below (Table 1).
Table 1.
Noninvasive in vivo imaging of mesenchymal stem cells in treatment and drug delivery for cancer
| Imaging | Imaging modality | Labelingmethod/agent | Cell type | Naïve/modified | Cell origin | Subject | Route of injection | Duration | Tumor | Outcome | Clinical translation | Ref. |
| Optical | Fluorescent | FNPs | BM-MSCs | AlPcS4@FNPs@MSCs | Human | Mice | Intratumor | Immediately | Human osteosarcoma | Inhibition of tumor | Limited | Lenna et al[81] |
| EGFP | BM-MSCs | TRAIL-MSCs | Mouse | Mice | Intravenous | 1-10 d | Mouse colon cancer | Inhibition of tumor | Limited | Zhang et al[82] | ||
| VivoTrack 680 | BM-MSCs | MSCs | Human | Mice | Intravenous | 2-24 h | Breast cancer | Inhibition of tumor metastasis | Limited | Camorani et al[83] | ||
| Bioluminescent | Rluc | UC-MSCs | HSV-ttk-MSCs | Human | Mice | Intratumor | 1-4 d | Breast cancer | Inhibition of tumor | Limited | Leng et al[84] | |
| Fluc | BM-MSCs | MSC-Tet-TK/ MSC-TK | Mouse | Mice | Intratumor | 1 and 5 d | Mouse colon cancer | Inhibition of tumor | Limited | Kalimuthu et al[85] | ||
| Fluc | BM-MSCs | MSC-CXCR4 | Mouse | Mice | Intravenous | 1 and 24 h | Breast cancer | Homing of genetically modified MSCs to tumor | Limited | Kalimuthu et al[86] | ||
| Fluc | BM-MSCs | Naïve | Human | Mice | Intravenous | 5 to 8 wk | Breast cancer | Homing of MSCs to lung metastatic tumor | Limited | Meleshina et al[87] | ||
| Fluc | BM-MSCs | Naïve | Human | Mice | Intravenous | 1 and 24 h | Thyroid and breast cancer | In vitro Dox delivery/homing of MSCs to tumor | Limited | Kalimuthu et al[88] | ||
| Fluc | BM-MSCs | Naïve | Mouse | Mice | Intravenous | 1-11 d | Murine breast cancer | Homing and differentiation of MSCs to tumor | Limited | Wang et al[89] | ||
| Fluc | BM-MSCs | MSCs-oncolytic adenovirus | Human | Mice | Intravenous | 15 min to 10 d | Murine large cell lung carcinoma | Homing of MSCs to tumor | Limited | Hakkarainen et al[90] | ||
| Rluc | BM-MSCs | MSC-e23sFv-Fdt-tBid | Mouse | Mice | Intravenous | 24 h | Breast cancer and gastric cancer | Inhibition of tumor | Limited | Cai et al[91] | ||
| Nuclear | PET | [18F]-FHBG | BM-MSCs | MSC-HSV1-TK | Human | Mice | Subcutaneous | 4 wk | Murine colon carcinoma | MSCs stably stay in tumor | Yes | Hung et al[60] |
| 124I | BM-MSCs | MSC-hNIS | Human | Mice | Intravenous | 72 h | Human hepatocellular carcinoma | Inhibition of tumor | Yes | Knoop et al[92] | ||
| 124I | BM-MSCs | MSC-hNIS | Mouse | Mice | Intravenous | 72 h | Mouse pancreatic tumor | Inhibition of tumor | Yes | Schug et al[93] | ||
| γ-camera | 123I | BM-MSCs | MSC-hNIS | Human | Mice | Intravenous | 72 h | Human hepatocellular carcinoma | Inhibition of tumor | Yes | Knoop et al[92] | |
| 123I | BM-MSCs | HSP70B-NIS-MSC | Human | Mice | Intravenous | 0-72 h | Human hepatocellular carcinoma | Inhibition of tumor | Yes | Tutter et al[94] | ||
| 123I | BM-MSCs | MSC-hNIS | Mouse | Mice | Intravenous | 72 h | Mouse pancreatic tumor | Inhibition of tumor | Yes | Schug et al[93] | ||
| 123I | BM-MSCs | MSC-hNIS | Human | Mice | Intravenous | 72 h | Human hepatocellular carcinoma | Inhibition of tumor | Yes | Schug et al[95] | ||
| 99mTc | BM-MSCs | MSC-hNIS | Human | Mice | Intravenous | 3-14 d | Breast cancer | Inhibition of tumor | Yes | Dwyer et al[64] | ||
| 99mTc | BM-MSCs | MSC-hNIS | Human | Mice | Intravenous | 3-24 d | Human cervical cancer | Inhibition of tumor | Yes | Belmar-Lopez et al[96] | ||
| MR | MRI | SPIO | BM-MSCs | MSC-hNIS | Human | Mice | Intravenous | 3-24 d | Human cervical cancer | Inhibition of tumor | Yes | Belmar-Lopez et al[96] |
| SPIO@Au-NPs | BM-MSCs | MSC | Human | Mice | Intravenous | 0-72 h | Human glioma | Homing of MSC to tumor | Yes | Qiao et al[97] |
FLI: Fluorescence imaging; BLI: Bioluminescence imaging; MRI: Magnetic resonance imaging; PET: Positron-emission tomography; γ-camera: Gamma camera imaging; FNPs: Fluorescent nanoparticles; EGFP: Enhanced green fluorescent protein; Fluc: Firefly luciferase; Rluc: Renilla luciferase; SPIO: Superparamagnetic iron oxide; TRAIL: Tumor necrosis factor-related apoptosis-inducing ligand; HSV1-tk: Herpes simplex virus type 1 thymidine kinase; hNIS: Human sodium iodide symporter; Au-NPs: Gold nanoparticles; HSP70B: Heat-inducible promoter; PDGFRβ: Platelet-derived growth factor receptor β; CXCR4: CXC chemokine receptor type 4.
Optical imaging
Fluorescent imaging: In vivo visualization as well as therapeutic effects of tetra-sulfonated aluminum phthalocyanine @ fluorescent nanoparticles-MSC (AlPcS4@FNPs-MSC) cells have been described previously using human osteosarcoma (Saos-2) tumor-bearing mice. First, the AlPcS4@FNPs were generated by mixing tetra-sulfonated aluminum phthalocyanine (AlPcS4; photosensitizer) and poly-methyl methacrylate core-shell fluorescent nanoparticles (FNPs). MSCs were labeled with AlPcS4@FNPs by incubating them for 1 h in a complete medium. AlPcS4, AlPcS4@FNPs, and AlPcS4@FNPs-MSC were intratumorally injected in tumor-bearing mice, fluorescent imaging was conducted immediately, and AlPcS4@FNPs-MSC was retained in the tumors following intratumor injection, while AlPcS4 and AlPcS4@FNPs migrated to the non-target area of mice. Following imaging, they conducted in vivo photodynamic therapy (near-infrared light with an LED source). The concentrated localization of AlPcS4@FNPs-MSC in the tumor enabled a greater reduction in tumor size following photodynamic therapy than other groups[81].
Migration and therapeutic effects of MSCs transduced with TRAIL (Tumor necrosis factor-related apoptosis-inducing ligand) (TRAIL-MSCs) were studied in a murine colon cancer (HT29) using macroscopic fluorescence imaging. MSCs were transduced with enhanced green fluorescent protein (EGFP) and TRAIL. PBS, MSC, and TRAIL-MSC were intravenously injected to colon tumor-bearing mice, and fluorescence imaging revealed that TRAIL-MSCs migrated to the tumor at day 10. TRAIL-MSC migration to the tumor impeded tumor growth more than the other groups[82].
Tumoral migration of MSCs was demonstrated with the use of a NIR lipophilic dye (VivoTrack 680) in a human breast cancer (MDA-MB-231) xenograft mouse model. The MSCs were labeled using the dye, and fluorescence imaging disclosed that intravenously injected MSCs migrated to breast cancer and targeting was counteracted by anti-platelet-derived growth factor receptor β (PDGFRβ) aptamer (Gint4.T) treatment[83].
Bioluminescent imaging: A triple fusion gene containing Renilla luciferase (Rluc), red fluorescent protein, and herpes simplex virus truncated thymidine kinase (HSV-ttk) was transduced into human umbilical cord-derived MSCs (Rluc-RFP-HSV-ttk/MSC) and bioluminescent imaging was conducted for visualization of subcutaneously injected Rluc-RFP-HSV-ttk/MSC in mouse models with or without ganciclovir (GCV) treatment. Bioluminescent imaging revealed the death of Rluc-RFP-HSV-ttk/MSC in mice treated with GCV. Moreover, in a breast cancer (MDA-MB-231) xenograft model, Rluc-RFP-HSV-ttk/MSC were injected into the breast cancer xenograft, and GCV treatment led to the death of Rluc-RFP-HSV-ttk/MSC and killed the cancer via bystander effects[84].
Murine MSC migration was observed with the use of Firefly luciferase (Fluc) in a murine colon cancer (CT26) xenograft mouse model. MSCs were transduced with RetroX-TRE (tetracycline response element), expressing a truncated herpes simplex virus thymidine kinase (HSV1-sr39tk) and Fluc2 gene with Tet-On (MSC-Tet-TK/Fluc2) or without (MSC-TK/Fluc2). MSC-Tet-TK/Fluc2 and MSC-TK/Fluc2 cells were intratumorally injected in a mouse colon cancer model. Bioluminescent imaging revealed that both showed increased cell death in mice treated with GCV in both MSCs with or without Tet-On system. Moreover, in a colon cancer xenograft model, MSC-TK/Fluc2 or MSC-Tet-TK/Fluc2 was co-injected with cancer cells, and GCV treatment led to the mortality of both MSC cancer cells[85].
Migration of MSCs transduced with or without CXCR4 (CXC chemokine receptor 4) and Fluc2 (MSC-Fluc2 or MSC-CXCR4-Fluc2) toward human breast cancer (MDA-MB-231) was observed with the use of bioluminescent imaging. MSC-Fluc2 and MSC-CXCR4-Fluc2 were intravenously injected to breast cancer-bearing mice, and bioluminescent imaging revealed that MSC-CXCR4-Fluc2 migrated to the tumor at 24 h, but MSC-Fluc2 did not migrate to the tumor. The bioluminescent imaging of the study revealed that the expression of CXCR4 can enhance the migration of MSCs to the tumor in vivo[86].
In vivo homing of human MSCs transduced with luc2 gene (MSCs-luc2) to lung metastasis of human breast cancer (MDA-MB-231) tumor-bearing mice was observed using bioluminescent imaging. MSCs-luc2 was intravenously injected to the tumor-bearing mice and imaged 5 h to 8 wk after administration. Bioluminescent imaging demonstrated that MSCs-luc2 migrated to lung metastasis of human breast cancer in the mice, and the signals were concentrated on the tumor, successfully showing the homing of MSCs to lung metastasis[87].
A previous study reported in vivo homing of human MSCs transduced with Fluc2 using human thyroid cancer (Cal62)- or human breast cancer (MDA-MB-231)-bearing mice. MSC/Fluc2 was intravenously injected into thyroid or breast cancer-bearing mice. Bioluminescent imaging were conducted 1 and 24 h following administration; at 24 h imaging showed that MSC/Fluc2 cells migrated to both thyroid and breast cancer in xenograft mouse models[88].
Migration of murine MSCs to murine breast cancer (4T1)-bearing mice was observed using bioluminescent imaging. First, the MSCs were transduced with Fluc gene and MSC-Fluc, and breast cancer cells were co-injected intravenously into mice to create a lung metastatic model. In the xenograft model, tumors developed in mice, and then MSC-Fluc was intravenously injected into tumor-bearing mice. Bioluminescent imaging revealed that MSC-Fluc stayed in the lung with tumors cells (1 h and 1, 4, and 6 d) and signals increased after 9 d and 11 d. In the xenograft model, intravenously injected cells migrated to tumors at day 1 and slowly decreased. Then, bioluminescent signals increased from day 8 to day 14[89].
A previous report described the transduction of Fluc gene and loading of oncolytic adenoviruses (Ad) into human MSCs (Ad-MSC/Fluc). The authors utilized bioluminescent imaging for visualization of subcutaneously injected Ad-MSC/Fluc or MSCs + non-replicating Ad in orthotopic murine lung and breast cancers. Bioluminescent imaging disclosed that the signal from Ad-MSC/Fluc was increased in the lungs at day 3. They concluded that MSCs can be a promising vehicle to deliver oncolytic adenoviruses to the tumors[90].
In vivo homing of murine MSCs transduced with Rluc and e23sFv-Fdt-tBid (HER2-specific killing by the immunoapoptotin, called MSC-RT) was observed in orthotopic breast cancer (4T1) and orthotopic gastric tumors (SGC-7901) mouse models. MSC-RT was intravenously injected into tumor-bearing mice, and bioluminescent imaging at 24 h showed migration of MSC-RT to both tumors, followed by inhibited growth[91].
Nuclear imaging
PET imaging: PET imaging was utilized to visualize HSV1-tk transduced MSCs (MSC-HSV1-tk) migration to murine colon carcinoma (HT-29Inv2) in a mouse model. MSC- HSV1-tk were injected intravenously into the mice, and PET imaging 18F-labeled 9-(4-fluoro-3-hydroxymethylbutyl)-guanine ([18F]-FHBG) revealed migration of the MSCs to the tumor[60].
In vivo homing and the therapeutic effects of labeled human MSCs transduced with NIS (NIS-MSCs) were demonstrated in hepatocellular carcinoma (Huh7) tumor-bearing mice by PET imaging. NIS-MSCs were intravenously injected into tumor-bearing mice and imaged 72 h following the administration of cells, 124I was then injected into the mice. PET imaging showed that NIS-MSCs migrated to the hepatocellular carcinoma. Moreover, they showed a reduction in tumor size and better survival following 131I therapy[92].
PET imaging was utilized to visualize migration of mouse MSCs to pancreatic tumor in a mouse model. MSCs were transduced with NIS (NIS-MSCs), and NIS-MSCs or MSCs were injected intravenously to tumor-bearing mice. PET imaging was carried out 3 h after 124I injection, and revealed the accumulation of 124I in the tumor of NIS-MSC-injected mice, showing NIS-MSC migration to the tumor. Moreover, these findings indicated that 131I therapy reduced the tumor size and increased survival[93].
Gamma camera imaging: In vivo homing and the therapeutic effects of human MSCs indirectly labeled with sodium-iodide symporter (NIS) (NIS-MSCs) were observed in hepatocellular carcinoma (Huh7) tumor-bearing mice by PET imaging. NIS-MSCs, NIS-MSCs+NaClO4, and MSCs were intravenously injected into tumor-bearing mice, and 123I was injected into mice at 72 h following the administration of the cells. Gamma imaging showed high signals in mouse tumors injected with NIS-MSCs, but no significant signals in MSCs+NaClO4 or naïve MSC-injected mice. These findings showed that NIS-MSCs successfully migrated to hepatocellular carcinoma. Moreover, they also showed that 131I therapy reduced the tumor size and increased survival[92].
As mentioned earlier, NIS-MSCs or MSCs were intravenously administered to tumor-bearing mice. Gamma camera imaging with 123I revealed tracer accumulation in tumors in NIS-MSCs-injected mice. Moreover, the authors showed that 131I therapy reduced the tumor size and increased survival[93].
A heat-inducible HSP70B promoter-driven NIS was transduced in MSCs (HSP70B-NIS-MSCs) and showed the migration of MSCs to a hepatocellular carcinoma (Huh7) xenograft in a mouse model. HSP70B-NIS-MSCs were intravenously injected into mice followed by hyperthermia (41°C) and control (normothermia at 37°C) 3 d later. Gamma camera imaging with 123I revealed the migration of HSP70B-NIS-MSCs to tumors and induction of NIS expression by hyperthermia. Moreover, the hyperthermia and 131I treatment reduced the tumor size and increased survival[94].
In vivo homing of human MSCs transduced with NIS gene was observed in hepatocellular carcinoma (Huh7)-bearing mice by gamma camera imaging. NIS-MSCs were intravenously injected 24 h after tumor irradiation (0, 2, or 5 Gy) in an animal model. Gamma camera imaging with 123I revealed increased uptake of 123I by the tumor, which enhanced the migratory capacity of MSCs[95]. SPECT imaging was previously used to visualize the migration of NIS to transduced MSC (NIS-MSC) breast cancer (MDA-MB-231) in a mouse model. NIS-MSCs were injected intravenously into tumor-bearing mice. For SPECT imaging, 99mTc was injected into mice 3 d after the injection of cells. SPECT imaging revealed increased uptake of the tracer in tumors of NIS-MSCs injected mice, which shows the localization of MSCs in the tumor and expressed NIS in the MSCs. 131I therapy resulted in a reduction of tumor size[60].
In vivo homing of different MSCs acquired from various sources (bone marrow, adipose tissue, epithelial endometrium, stroma endometrium, and amniotic membrane) to cervical cancer (HeLa) was observed in an animal model. The NIS gene was transduced into MSCs (MSC-NIS) and the cells were imaged with SPECT/CT. MSCs were intravenously injected into tumor-bearing mice, and SPECT/CT imaging with 99mTc was carried out at 3, 10, 17, and 24 d after the injection of MSCs. The study showed the variable migration ability of MSCs due to their origins[96].
MRI
As mentioned earlier, in vivo tumoral homing of MSCs was observed by direct SPIO labeling in mice with cervical cancer (HeLa) by MRI. Following the intravenous injection of SPIO-labeled MSC-MRI, the recruitment of SPIO-labeled MSCs to tumors was observed[96].
Migration of MSCs to glioma was studied by labeling MSCs with nanoparticles containing SPIO coated with gold (SPIO@Au) and imaging with MRI. SPIO@Au-MSCs were injected via the intravenous route to mice bearing brain gliomas. MRI revealed migration of the MSCs to the tumor[97].
FUTURE OUTLOOKS
While studies in small animals can yield a lot of information related to the behavior of MSCs, it may not be relevant when it comes to delivering the cells to large animals or humans due to differences in their physiology. Since our ultimate goal is to utilize such groundbreaking MSC-based therapies for treating cancerous diseases in humans, a lot of factors including the origins of MSCs, types of reporter genes, routes of administration, and timing of cell delivery will need to be modified depending upon the type of model used. Large animals show the most similarity to humans in terms of size, disease progression, weight, and overall anatomy[98]. Thus, these animal models are widely utilized to test different imaging and therapeutic modalities.
Tracking of MSCs post-transplantation in large animals is practicable with the use of indirect labeling approaches[99]. There are some challenges associated with imaging large animals, including low sensitivity and difficulty in quantifying cells. Also, several factors can impact the survival of transplanted cells including limited cell-to-cell and cell-microenvironment contact, tissue hypoxia, and host immune response. Efforts should be made to increase cell viability at the desired site to acquire an optimal therapeutic benefit while minimizing toxicity.
The adaptation of in vivo imaging approaches to track MSCs in clinical trials will need careful assessment of pharmacokinetic information relating to cell therapies. If incorporated at an earlier phase of clinical trials, imaging approaches can give insights into optimal dosage, frequency of administration, and retention time for cells by helping to create dose-response curves. Also, imaging can yield key information relating to the in vivo functional properties of administered cells including viability, proliferation, and differentiation. A quick search on the clinicaltrials.gov site shows more than 400 ongoing trials exploring the potential of MSCs to treat different diseases[100]. It is essential to remember that each patient may respond differently to each therapy. Some patients may clear cells faster than others because of a strong immune reaction, leading to changing responses to certain cell therapies[101-103].
It is believed that in vivo imaging (especially PET/MRI due to their high sensitivity and ability to provide meticulous anatomical information) will serve as a powerful tool to evaluate in vivo therapeutic cells in the future. Presently, in vivo imaging modalities are utilized solely for short-term monitoring of administered cell survival. There are various regulatory obstacles in achieving long-term cell tracking with reporter genes in humans, the technique that could be useful for understanding the long-term therapeutic effects of MSC-based cancer therapy. One solution could be the utilization of endogenous reporter genes of human origin, which has been previously tested in preclinical models[104]. Finally, with long-term tracking, it is possible to determine the fate of MSCs and how they contribute to the eradication of cancerous diseases.
CONCLUSION
Recent progress in noninvasive imaging technologies has taken the field of cell therapies to the next level. In this review article, essential developments in labeling technologies, imaging modalities, and how they are able to contribute to the development of MSC-based cancer therapies have been exhaustively described. The exact roles of MSCs in cancerous diseases are unclear because they have been shown to promote and inhibit the growth of different tumors at the preclinical level. Presently, MSCs are being utilized for delivery of therapeutic agents in cancer models, thereby opening new avenues for personalized cancer therapies in the future. To improve the clinical utility of MSC-based therapies, it is crucial for us to understand how MSCs interact with cancer cells in vivo. The extracellular vesicles originating from MSCs can also be utilized for cancer treatment to escape safety issues relating to the administration of live MSCs. MSCs have given us a new hope to develop safe and effective intervention strategies against cancer. Combined with long-term monitoring, a lot can be learned regarding the hidden potentials of MSCs and their variable fate in humans.
Footnotes
Conflict-of-interest statement: The authors declare that the research was performed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Manuscript source: Invited manuscript
Peer-review started: June 29, 2020
First decision: September 24, 2020
Article in press: October 21, 2020
Specialty type: Cell and tissue engineering
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Huang YC S-Editor: Gao CC L-Editor: Webster JR P-Editor: Li X
Contributor Information
Ramya Lakshmi Rajendran, Department of Nuclear Medicine, Kyungpook National University, Daegu 41944, South Korea.
Manasi Pandurang Jogalekar, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA 02115, United States.
Prakash Gangadaran, Department of Nuclear Medicine, School of Medicine, Kyungpook National University, Daegu 41944, South Korea; BK21 Plus KNU Biomedical Convergence Program, Department of Biomedical Science, School of Medicine, Kyungpook National University, Daegu 41944, South Korea.
Byeong-Cheol Ahn, BK21 Plus KNU Biomedical Convergence Program, Department of Biomedical Science, School of Medicine, Kyungpook National University, Daegu 41944, South Korea; Department of Nuclear Medicine, School of Medicine, Kyungpook National University, Kyungpook National University Hospital, Daegu 41944, South Korea. abc2000@knu.ac.kr.
References
- 1.Weissman IL, Shizuru JA. The origins of the identification and isolation of hematopoietic stem cells, and their capability to induce donor-specific transplantation tolerance and treat autoimmune diseases. Blood. 2008;112:3543–3553. doi: 10.1182/blood-2008-08-078220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li MD, Atkins H, Bubela T. The global landscape of stem cell clinical trials. Regen Med. 2014;9:27–39. doi: 10.2217/rme.13.80. [DOI] [PubMed] [Google Scholar]
- 3.Klopp AH, Gupta A, Spaeth E, Andreeff M, Marini F 3rd. Concise review: Dissecting a discrepancy in the literature: do mesenchymal stem cells support or suppress tumor growth? Stem Cells. 2011;29:11–19. doi: 10.1002/stem.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.von Bahr L, Batsis I, Moll G, Hägg M, Szakos A, Sundberg B, Uzunel M, Ringden O, Le Blanc K. Analysis of tissues following mesenchymal stromal cell therapy in humans indicates limited long-term engraftment and no ectopic tissue formation. Stem Cells. 2012;30:1575–1578. doi: 10.1002/stem.1118. [DOI] [PubMed] [Google Scholar]
- 5.Chen L, Tredget EE, Wu PY, Wu Y. Paracrine factors of mesenchymal stem cells recruit macrophages and endothelial lineage cells and enhance wound healing. PLoS One. 2008;3:e1886. doi: 10.1371/journal.pone.0001886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khakoo AY, Pati S, Anderson SA, Reid W, Elshal MF, Rovira II, Nguyen AT, Malide D, Combs CA, Hall G, Zhang J, Raffeld M, Rogers TB, Stetler-Stevenson W, Frank JA, Reitz M, Finkel T. Human mesenchymal stem cells exert potent antitumorigenic effects in a model of Kaposi's sarcoma. J Exp Med. 2006;203:1235–1247. doi: 10.1084/jem.20051921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Qiao L, Xu Z, Zhao T, Zhao Z, Shi M, Zhao RC, Ye L, Zhang X. Suppression of tumorigenesis by human mesenchymal stem cells in a hepatoma model. Cell Res. 2008;18:500–507. doi: 10.1038/cr.2008.40. [DOI] [PubMed] [Google Scholar]
- 8.Suzuki K, Sun R, Origuchi M, Kanehira M, Takahata T, Itoh J, Umezawa A, Kijima H, Fukuda S, Saijo Y. Mesenchymal stromal cells promote tumor growth through the enhancement of neovascularization. Mol Med. 2011;17:579–587. doi: 10.2119/molmed.2010.00157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang T, Lee YW, Rui YF, Cheng TY, Jiang XH, Li G. Bone marrow-derived mesenchymal stem cells promote growth and angiogenesis of breast and prostate tumors. Stem Cell Res Ther. 2013;4:70. doi: 10.1186/scrt221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lauber DT, Fülöp A, Kovács T, Szigeti K, Máthé D, Szijártó A. State of the art in vivo imaging techniques for laboratory animals. Lab Anim. 2017;51:465–478. doi: 10.1177/0023677217695852. [DOI] [PubMed] [Google Scholar]
- 11.Kim JE, Kalimuthu S, Ahn BC. In vivo cell tracking with bioluminescence imaging. Nucl Med Mol Imaging. 2015;49:3–10. doi: 10.1007/s13139-014-0309-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gabrielson K, Maronpot R, Monette S, Mlynarczyk C, Ramot Y, Nyska A, Sysa-Shah P. In Vivo Imaging With Confirmation by Histopathology for Increased Rigor and Reproducibility in Translational Research: A Review of Examples, Options, and Resources. ILAR J. 2018;59:80–98. doi: 10.1093/ilar/ily010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duyk G. Attrition and translation. Science. 2003;302:603–605. doi: 10.1126/science.1090521. [DOI] [PubMed] [Google Scholar]
- 14.Hörig H, Pullman W. From bench to clinic and back: Perspective on the 1st IQPC Translational Research conference. J Transl Med. 2004;2:44. doi: 10.1186/1479-5876-2-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beckmann N, Kneuer R, Gremlich HU, Karmouty-Quintana H, Blé FX, Müller M. In vivo mouse imaging and spectroscopy in drug discovery. NMR Biomed. 2007;20:154–185. doi: 10.1002/nbm.1153. [DOI] [PubMed] [Google Scholar]
- 16.Ransohoff KJ, Wu JC. Advances in cardiovascular molecular imaging for tracking stem cell therapy. Thromb Haemost. 2010;104:13–22. doi: 10.1160/TH09-08-0530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee JS, Orita H, Gabrielson K, Alvey S, Hagemann RL, Kuhajda FP, Gabrielson E, Pomper MG. FDG-PET for pharmacodynamic assessment of the fatty acid synthase inhibitor C75 in an experimental model of lung cancer. Pharm Res. 2007;24:1202–1207. doi: 10.1007/s11095-007-9264-x. [DOI] [PubMed] [Google Scholar]
- 18.Horwitz EM, Le Blanc K, Dominici M, Mueller I, Slaper-Cortenbach I, Marini FC, Deans RJ, Krause DS, Keating A International Society for Cellular Therapy. Clarification of the nomenclature for MSC: The International Society for Cellular Therapy position statement. Cytotherapy. 2005;7:393–395. doi: 10.1080/14653240500319234. [DOI] [PubMed] [Google Scholar]
- 19.Uccelli A, Moretta L, Pistoia V. Mesenchymal stem cells in health and disease. Nat Rev Immunol. 2008;8:726–736. doi: 10.1038/nri2395. [DOI] [PubMed] [Google Scholar]
- 20.Friedenstein AJ, Chailakhyan RK, Latsinik NV, Panasyuk AF, Keiliss-Borok IV. Stromal cells responsible for transferring the microenvironment of the hemopoietic tissues. Cloning in vitro and retransplantation in vivo. Transplantation. 1974;17:331–340. doi: 10.1097/00007890-197404000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Bender E. Cell-based therapy: Cells on trial. Nature. 2016;540:S106–S108. doi: 10.1038/540S106a. [DOI] [PubMed] [Google Scholar]
- 22.Naldini L. Ex vivo gene transfer and correction for cell-based therapies. Nat Rev Genet. 2011;12:301–315. doi: 10.1038/nrg2985. [DOI] [PubMed] [Google Scholar]
- 23.Tse WT, Pendleton JD, Beyer WM, Egalka MC, Guinan EC. Suppression of allogeneic T-cell proliferation by human marrow stromal cells: implications in transplantation. Transplantation. 2003;75:389–397. doi: 10.1097/01.TP.0000045055.63901.A9. [DOI] [PubMed] [Google Scholar]
- 24.Saeedi P, Halabian R, Imani Fooladi AA. A revealing review of mesenchymal stem cells therapy, clinical perspectives and Modification strategies. Stem Cell Investig. 2019;6:34. doi: 10.21037/sci.2019.08.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rosen AB, Kelly DJ, Schuldt AJ, Lu J, Potapova IA, Doronin SV, Robichaud KJ, Robinson RB, Rosen MR, Brink PR, Gaudette GR, Cohen IS. Finding fluorescent needles in the cardiac haystack: tracking human mesenchymal stem cells labeled with quantum dots for quantitative in vivo three-dimensional fluorescence analysis. Stem Cells. 2007;25:2128–2138. doi: 10.1634/stemcells.2006-0722. [DOI] [PubMed] [Google Scholar]
- 26.Perez JR, Ybarra N, Chagnon F, Serban M, Lee S, Seuntjens J, Lesur O, El Naqa I. Tracking of Mesenchymal Stem Cells with Fluorescence Endomicroscopy Imaging in Radiotherapy-Induced Lung Injury. Sci Rep. 2017;7:40748. doi: 10.1038/srep40748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bindslev L, Haack-Sørensen M, Bisgaard K, Kragh L, Mortensen S, Hesse B, Kjaer A, Kastrup J. Labelling of human mesenchymal stem cells with indium-111 for SPECT imaging: effect on cell proliferation and differentiation. Eur J Nucl Med Mol Imaging. 2006;33:1171–1177. doi: 10.1007/s00259-006-0093-7. [DOI] [PubMed] [Google Scholar]
- 28.Hill JM, Dick AJ, Raman VK, Thompson RB, Yu ZX, Hinds KA, Pessanha BS, Guttman MA, Varney TR, Martin BJ, Dunbar CE, McVeigh ER, Lederman RJ. Serial cardiac magnetic resonance imaging of injected mesenchymal stem cells. Circulation. 2003;108:1009–1014. doi: 10.1161/01.CIR.0000084537.66419.7A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yukawa H, Baba Y. In Vivo Imaging Technology of Transplanted Stem Cells Using Quantum Dots for Regenerative Medicine. Anal Sci. 2018;34:525–532. doi: 10.2116/analsci.17R005. [DOI] [PubMed] [Google Scholar]
- 30.Seleverstov O, Zabirnyk O, Zscharnack M, Bulavina L, Nowicki M, Heinrich JM, Yezhelyev M, Emmrich F, O'Regan R, Bader A. Quantum dots for human mesenchymal stem cells labeling. A size-dependent autophagy activation. Nano Lett. 2006;6:2826–2832. doi: 10.1021/nl0619711. [DOI] [PubMed] [Google Scholar]
- 31.Shah BS, Mao JJ. Labeling of mesenchymal stem cells with bioconjugated quantum dots. Methods Mol Biol. 2011;680:61–75. doi: 10.1007/978-1-60761-901-7_4. [DOI] [PubMed] [Google Scholar]
- 32.Muller-Borer BJ, Collins MC, Gunst PR, Cascio WE, Kypson AP. Quantum dot labeling of mesenchymal stem cells. J Nanobiotechnology. 2007;5:9. doi: 10.1186/1477-3155-5-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mohtasebi MS, Nasri F, Kamali Sarvestani E. Effect of DiD Carbocyanine Dye Labeling on Immunoregulatory Function and Differentiation of Mice Mesenchymal Stem Cells. Stem Cells Int. 2014;2014:457614. doi: 10.1155/2014/457614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hoshino K, Ly HQ, Frangioni JV, Hajjar RJ. In vivo tracking in cardiac stem cell-based therapy. Prog Cardiovasc Dis. 2007;49:414–420. doi: 10.1016/j.pcad.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 35.Yang B, Brahmbhatt A, Nieves Torres E, Thielen B, McCall DL, Engel S, Bansal A, Pandey MK, Dietz AB, Leof EB, DeGrado TR, Mukhopadhyay D, Misra S. Tracking and Therapeutic Value of Human Adipose Tissue-derived Mesenchymal Stem Cell Transplantation in Reducing Venous Neointimal Hyperplasia Associated with Arteriovenous Fistula. Radiology. 2016;279:513–522. doi: 10.1148/radiol.2015150947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jin Y, Kong H, Stodilka RZ, Wells RG, Zabel P, Merrifield PA, Sykes J, Prato FS. Determining the minimum number of detectable cardiac-transplanted 111In-tropolone-labelled bone-marrow-derived mesenchymal stem cells by SPECT. Phys Med Biol. 2005;50:4445–4455. doi: 10.1088/0031-9155/50/19/001. [DOI] [PubMed] [Google Scholar]
- 37.Barbash IM, Chouraqui P, Baron J, Feinberg MS, Etzion S, Tessone A, Miller L, Guetta E, Zipori D, Kedes LH, Kloner RA, Leor J. Systemic delivery of bone marrow-derived mesenchymal stem cells to the infarcted myocardium: feasibility, cell migration, and body distribution. Circulation. 2003;108:863–868. doi: 10.1161/01.CIR.0000084828.50310.6A. [DOI] [PubMed] [Google Scholar]
- 38.Perin EC, Tian M, Marini FC 3rd, Silva GV, Zheng Y, Baimbridge F, Quan X, Fernandes MR, Gahremanpour A, Young D, Paolillo V, Mukhopadhyay U, Borne AT, Uthamanthil R, Brammer D, Jackson J, Decker WK, Najjar AM, Thomas MW, Volgin A, Rabinovich B, Soghomonyan S, Jeong HJ, Rios JM, Steiner D, Robinson S, Mawlawi O, Pan T, Stafford J, Kundra V, Li C, Alauddin MM, Willerson JT, Shpall E, Gelovani JG. Imaging long-term fate of intramyocardially implanted mesenchymal stem cells in a porcine myocardial infarction model. PLoS One. 2011;6:e22949. doi: 10.1371/journal.pone.0022949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang G, Lan X, Yen TC, Chen Q, Pei Z, Qin C, Zhang Y. Therapeutic gene expression in transduced mesenchymal stem cells can be monitored using a reporter gene. Nucl Med Biol. 2012;39:1243–1250. doi: 10.1016/j.nucmedbio.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 40.Detante O, Moisan A, Dimastromatteo J, Richard MJ, Riou L, Grillon E, Barbier E, Desruet MD, De Fraipont F, Segebarth C, Jaillard A, Hommel M, Ghezzi C, Remy C. Intravenous administration of 99mTc-HMPAO-labeled human mesenchymal stem cells after stroke: in vivo imaging and biodistribution. Cell Transplant. 2009;18:1369–1379. doi: 10.3727/096368909X474230. [DOI] [PubMed] [Google Scholar]
- 41.Chin BB, Nakamoto Y, Bulte JW, Pittenger MF, Wahl R, Kraitchman DL. 111In oxine labelled mesenchymal stem cell SPECT after intravenous administration in myocardial infarction. Nucl Med Commun. 2003;24:1149–1154. doi: 10.1097/00006231-200311000-00005. [DOI] [PubMed] [Google Scholar]
- 42.Gholamrezanezhad A, Mirpour S, Bagheri M, Mohamadnejad M, Alimoghaddam K, Abdolahzadeh L, Saghari M, Malekzadeh R. In vivo tracking of 111In-oxine labeled mesenchymal stem cells following infusion in patients with advanced cirrhosis. Nucl Med Biol. 2011;38:961–967. doi: 10.1016/j.nucmedbio.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 43.Bos C, Delmas Y, Desmoulière A, Solanilla A, Hauger O, Grosset C, Dubus I, Ivanovic Z, Rosenbaum J, Charbord P, Combe C, Bulte JW, Moonen CT, Ripoche J, Grenier N. In vivo MR imaging of intravascularly injected magnetically labeled mesenchymal stem cells in rat kidney and liver. Radiology. 2004;233:781–789. doi: 10.1148/radiol.2333031714. [DOI] [PubMed] [Google Scholar]
- 44.Ittrich H, Lange C, Tögel F, Zander AR, Dahnke H, Westenfelder C, Adam G, Nolte-Ernsting C. In vivo magnetic resonance imaging of iron oxide-labeled, arterially-injected mesenchymal stem cells in kidneys of rats with acute ischemic kidney injury: detection and monitoring at 3T. J Magn Reson Imaging. 2007;25:1179–1191. doi: 10.1002/jmri.20925. [DOI] [PubMed] [Google Scholar]
- 45.Kraitchman DL, Heldman AW, Atalar E, Amado LC, Martin BJ, Pittenger MF, Hare JM, Bulte JW. In vivo magnetic resonance imaging of mesenchymal stem cells in myocardial infarction. Circulation. 2003;107:2290–2293. doi: 10.1161/01.CIR.0000070931.62772.4E. [DOI] [PubMed] [Google Scholar]
- 46.Dick AJ, Guttman MA, Raman VK, Peters DC, Pessanha BS, Hill JM, Smith S, Scott G, McVeigh ER, Lederman RJ. Magnetic resonance fluoroscopy allows targeted delivery of mesenchymal stem cells to infarct borders in Swine. Circulation. 2003;108:2899–2904. doi: 10.1161/01.CIR.0000095790.28368.F9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kedziorek DA, Kraitchman DL. Superparamagnetic iron oxide labeling of stem cells for MRI tracking and delivery in cardiovascular disease. Methods Mol Biol. 2010;660:171–183. doi: 10.1007/978-1-60761-705-1_11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liu Y-H, Sinusas AJ. Hybrid imaging in cardiovascular medicine. CRC Press. 2017 [Google Scholar]
- 49.Li YG, Wei JN, Lu J, Wu XT, Teng GJ. Labeling and tracing of bone marrow mesenchymal stem cells for tendon-to-bone tunnel healing. Knee Surg Sports Traumatol Arthrosc. 2011;19:2153–2158. doi: 10.1007/s00167-011-1506-0. [DOI] [PubMed] [Google Scholar]
- 50.Sykova E, Jendelova P. In vivo tracking of stem cells in brain and spinal cord injury. Prog Brain Res. 2007;161:367–383. doi: 10.1016/S0079-6123(06)61026-1. [DOI] [PubMed] [Google Scholar]
- 51.Lee NK, Kim HS, Yoo D, Hwang JW, Choi SJ, Oh W, Chang JW, Na DL. Magnetic Resonance Imaging of Ferumoxytol-Labeled Human Mesenchymal Stem Cells in the Mouse Brain. Stem Cell Rev Rep. 2017;13:127–138. doi: 10.1007/s12015-016-9694-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Huang X, Zhang F, Wang H, Niu G, Choi KY, Swierczewska M, Zhang G, Gao H, Wang Z, Zhu L, Choi HS, Lee S, Chen X. Mesenchymal stem cell-based cell engineering with multifunctional mesoporous silica nanoparticles for tumor delivery. Biomaterials. 2013;34:1772–1780. doi: 10.1016/j.biomaterials.2012.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lu CW, Hsiao JK, Liu HM, Wu CH. Characterization of an iron oxide nanoparticle labelling and MRI-based protocol for inducing human mesenchymal stem cells into neural-like cells. Sci Rep. 2017;7:3587. doi: 10.1038/s41598-017-03863-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kang JH, Chung JK. Molecular-genetic imaging based on reporter gene expression. J Nucl Med. 2008;49 Suppl 2:164S–179S. doi: 10.2967/jnumed.107.045955. [DOI] [PubMed] [Google Scholar]
- 55.Zhang SJ, Wu JC. Comparison of imaging techniques for tracking cardiac stem cell therapy. J Nucl Med. 2007;48:1916–1919. doi: 10.2967/jnumed.107.043299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.van der Bogt KE, Sheikh AY, Schrepfer S, Hoyt G, Cao F, Ransohoff KJ, Swijnenburg RJ, Pearl J, Lee A, Fischbein M, Contag CH, Robbins RC, Wu JC. Comparison of different adult stem cell types for treatment of myocardial ischemia. Circulation. 2008;118:S121–S129. doi: 10.1161/CIRCULATIONAHA.107.759480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hoffmann J, Glassford AJ, Doyle TC, Robbins RC, Schrepfer S, Pelletier MP. Angiogenic effects despite limited cell survival of bone marrow-derived mesenchymal stem cells under ischemia. Thorac Cardiovasc Surg. 2010;58:136–142. doi: 10.1055/s-0029-1240758. [DOI] [PubMed] [Google Scholar]
- 58.Franchi F, Peterson KM, Paulmurugan R, Folmes C, Lanza IR, Lerman A, Rodriguez-Porcel M. Noninvasive Monitoring of the Mitochondrial Function in Mesenchymal Stromal Cells. Mol Imaging Biol. 2016;18:510–518. doi: 10.1007/s11307-016-0929-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Psaltis PJ, Peterson KM, Xu R, Franchi F, Witt T, Chen IY, Lerman A, Simari RD, Gambhir SS, Rodriguez-Porcel M. Noninvasive monitoring of oxidative stress in transplanted mesenchymal stromal cells. JACC Cardiovasc Imaging. 2013;6:795–802. doi: 10.1016/j.jcmg.2012.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hung SC, Deng WP, Yang WK, Liu RS, Lee CC, Su TC, Lin RJ, Yang DM, Chang CW, Chen WH, Wei HJ, Gelovani JG. Mesenchymal stem cell targeting of microscopic tumors and tumor stroma development monitored by noninvasive in vivo positron emission tomography imaging. Clin Cancer Res. 2005;11:7749–7756. doi: 10.1158/1078-0432.CCR-05-0876. [DOI] [PubMed] [Google Scholar]
- 61.Abbas F, Wu JC, Gambhir SS, Rodriguez-Porcel M. Molecular imaging of stem cells. StemJournal . 2019;1:27–46. [Google Scholar]
- 62.Schönitzer V, Haasters F, Käsbauer S, Ulrich V, Mille E, Gildehaus FJ, Carlsen J, Pape M, Beck R, Delker A, Böning G, Mutschler W, Böcker W, Schieker M, Bartenstein P. In vivo mesenchymal stem cell tracking with PET using the dopamine type 2 receptor and 18F-fallypride. J Nucl Med. 2014;55:1342–1347. doi: 10.2967/jnumed.113.134775. [DOI] [PubMed] [Google Scholar]
- 63.Kim MH, Lee YJ, Kim KI, Lee TS, Woo KS, Lee DS, Kim CW, Choi CW, Lim SM, Kang JH. In vitro monitoring of cardiomyogenic differentiation of mesenchymal stem cells using sodium iodide symporter gene. Tissue Eng Regen Med. 2012;9:304–310. [Google Scholar]
- 64.Dwyer RM, Ryan J, Havelin RJ, Morris JC, Miller BW, Liu Z, Flavin R, O'Flatharta C, Foley MJ, Barrett HH, Murphy JM, Barry FP, O'Brien T, Kerin MJ. Mesenchymal Stem Cell-mediated delivery of the sodium iodide symporter supports radionuclide imaging and treatment of breast cancer. Stem Cells. 2011;29:1149–1157. doi: 10.1002/stem.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Love Z, Wang F, Dennis J, Awadallah A, Salem N, Lin Y, Weisenberger A, Majewski S, Gerson S, Lee Z. Imaging of mesenchymal stem cell transplant by bioluminescence and PET. J Nucl Med. 2007;48:2011–2020. doi: 10.2967/jnumed.107.043166. [DOI] [PubMed] [Google Scholar]
- 66.Gyöngyösi M, Blanco J, Marian T, Trón L, Petneházy O, Petrasi Z, Hemetsberger R, Rodriguez J, Font G, Pavo IJ, Kertész I, Balkay L, Pavo N, Posa A, Emri M, Galuska L, Kraitchman DL, Wojta J, Huber K, Glogar D. Serial noninvasive in vivo positron emission tomographic tracking of percutaneously intramyocardially injected autologous porcine mesenchymal stem cells modified for transgene reporter gene expression. Circ Cardiovasc Imaging. 2008;1:94–103. doi: 10.1161/CIRCIMAGING.108.797449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Huang J, Lee CC, Sutcliffe JL, Cherry SR, Tarantal AF. Radiolabeling rhesus monkey CD34+ hematopoietic and mesenchymal stem cells with 64Cu-pyruvaldehyde-bis(N4-methylthiosemicarbazone) for microPET imaging. Mol Imaging. 2008;7:1–11. [PubMed] [Google Scholar]
- 68.Kraitchman DL, Tatsumi M, Gilson WD, Ishimori T, Kedziorek D, Walczak P, Segars WP, Chen HH, Fritzges D, Izbudak I, Young RG, Marcelino M, Pittenger MF, Solaiyappan M, Boston RC, Tsui BM, Wahl RL, Bulte JW. Dynamic imaging of allogeneic mesenchymal stem cells trafficking to myocardial infarction. Circulation. 2005;112:1451–1461. doi: 10.1161/CIRCULATIONAHA.105.537480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gholamrezanezhad A, Mirpour S, Ardekani JM, Bagheri M, Alimoghadam K, Yarmand S, Malekzadeh R. Cytotoxicity of 111In-oxine on mesenchymal stem cells: a time-dependent adverse effect. Nucl Med Commun. 2009;30:210–216. doi: 10.1097/MNM.0b013e328318b328. [DOI] [PubMed] [Google Scholar]
- 70.Karussis D, Karageorgiou C, Vaknin-Dembinsky A, Gowda-Kurkalli B, Gomori JM, Kassis I, Bulte JW, Petrou P, Ben-Hur T, Abramsky O, Slavin S. Safety and immunological effects of mesenchymal stem cell transplantation in patients with multiple sclerosis and amyotrophic lateral sclerosis. Arch Neurol. 2010;67:1187–1194. doi: 10.1001/archneurol.2010.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liu Y, He ZJ, Xu B, Wu QZ, Liu G, Zhu H, Zhong Q, Deng DY, Ai H, Yue Q, Wei Y, Jun S, Zhou G, Gong QY. Evaluation of cell tracking effects for transplanted mesenchymal stem cells with jetPEI/Gd-DTPA complexes in animal models of hemorrhagic spinal cord injury. Brain Res. 2011;1391:24–35. doi: 10.1016/j.brainres.2011.03.032. [DOI] [PubMed] [Google Scholar]
- 72.Kassis I, Vaknin-Dembinsky A, Bulte J, Karussis D. Effects of supermagnetic iron oxide labeling on the major functional properties of human mesenchymal stem cells from multiple sclerosis patients. Int J Stem Cells. 2010;3:144–153. doi: 10.15283/ijsc.2010.3.2.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jokerst JV, Thangaraj M, Kempen PJ, Sinclair R, Gambhir SS. Photoacoustic imaging of mesenchymal stem cells in living mice via silica-coated gold nanorods. ACS Nano. 2012;6:5920–5930. doi: 10.1021/nn302042y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gildehaus FJ, Haasters F, Drosse I, Wagner E, Zach C, Mutschler W, Cumming P, Bartenstein P, Schieker M. Impact of indium-111 oxine labelling on viability of human mesenchymal stem cells in vitro, and 3D cell-tracking using SPECT/CT in vivo. Mol Imaging Biol. 2011;13:1204–1214. doi: 10.1007/s11307-010-0439-1. [DOI] [PubMed] [Google Scholar]
- 75.Krishnan M, Park JM, Cao F, Wang D, Paulmurugan R, Tseng JR, Gonzalgo ML, Gambhir SS, Wu JC. Effects of epigenetic modulation on reporter gene expression: implications for stem cell imaging. FASEB J. 2006;20:106–108. doi: 10.1096/fj.05-4551fje. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wang F, Dennis JE, Awadallah A, Solchaga LA, Molter J, Kuang Y, Salem N, Lin Y, Tian H, Kolthammer JA, Kim Y, Love ZB, Gerson SL, Lee Z. Transcriptional profiling of human mesenchymal stem cells transduced with reporter genes for imaging. Physiol Genomics. 2009;37:23–34. doi: 10.1152/physiolgenomics.00300.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Louis DN. Molecular pathology of malignant gliomas. Annu Rev Pathol. 2006;1:97–117. doi: 10.1146/annurev.pathol.1.110304.100043. [DOI] [PubMed] [Google Scholar]
- 78.Ochiai H, Sakamoto N, Fujita K, Nishikawa M, Suzuki K, Matsuura S, Miyamoto T, Sakuma T, Shibata T, Yamamoto T. Zinc-finger nuclease-mediated targeted insertion of reporter genes for quantitative imaging of gene expression in sea urchin embryos. Proc Natl Acad Sci USA. 2012;109:10915–10920. doi: 10.1073/pnas.1202768109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Li T, Dong H, Zhang C, Mo R. Cell-based drug delivery systems for biomedical applications. Nano Res. 2018;11:5240–5257. [Google Scholar]
- 80.Gangadaran P, Rajendran RL, Ahn BC. Application of In Vivo Imaging Techniques for Monitoring Natural Killer Cell Migration and Tumor Infiltration. Cancers (Basel) 2020;12 doi: 10.3390/cancers12051318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lenna S, Bellotti C, Duchi S, Martella E, Columbaro M, Dozza B, Ballestri M, Guerrini A, Sotgiu G, Frisoni T, Cevolani L, Varchi G, Ferrari M, Donati DM, Lucarelli E. Mesenchymal stromal cells mediated delivery of photoactive nanoparticles inhibits osteosarcoma growth in vitro and in a murine in vivo ectopic model. J Exp Clin Cancer Res. 2020;39:40. doi: 10.1186/s13046-020-01548-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhang Z, Li M, Chen F, Li L, Liu J, Li Z, Ji R, Zuo X, Li Y. Probe-Based Confocal Laser Endomicroscopy for Imaging TRAIL-Expressing Mesenchymal Stem Cells to Monitor Colon Xenograft Tumors In Vivo. PLoS One. 2016;11:e0162700. doi: 10.1371/journal.pone.0162700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Camorani S, Hill BS, Fontanella R, Greco A, Gramanzini M, Auletta L, Gargiulo S, Albanese S, Lucarelli E, Cerchia L, Zannetti A. Inhibition of Bone Marrow-Derived Mesenchymal Stem Cells Homing Towards Triple-Negative Breast Cancer Microenvironment Using an Anti-PDGFRβ Aptamer. Theranostics. 2017;7:3595–3607. doi: 10.7150/thno.18974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Leng L, Wang Y, He N, Wang D, Zhao Q, Feng G, Su W, Xu Y, Han Z, Kong D, Cheng Z, Xiang R, Li Z. Molecular imaging for assessment of mesenchymal stem cells mediated breast cancer therapy. Biomaterials. 2014;35:5162–5170. doi: 10.1016/j.biomaterials.2014.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kalimuthu S, Zhu L, Oh JM, Lee HW, Gangadaran P, Rajendran RL, Baek SH, Jeon YH, Jeong SY, Lee SW, Lee J, Ahn BC. Regulated Mesenchymal Stem Cells Mediated Colon Cancer Therapy Assessed by Reporter Gene Based Optical Imaging. Int J Mol Sci. 2018;19 doi: 10.3390/ijms19041002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kalimuthu S, Oh JM, Gangadaran P, Zhu L, Lee HW, Rajendran RL, Baek SH, Jeon YH, Jeong SY, Lee SW, Lee J, Ahn BC. In Vivo Tracking of Chemokine Receptor CXCR4-Engineered Mesenchymal Stem Cell Migration by Optical Molecular Imaging. Stem Cells Int. 2017;2017:8085637. doi: 10.1155/2017/8085637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Meleshina AV, Cherkasova EI, Shirmanova MV, Klementieva NV, Kiseleva EV, Snopova LВ, Prodanets NN, Zagaynova EV. Influence of mesenchymal stem cells on metastasis development in mice in vivo. Stem Cell Res Ther. 2015;6:15. doi: 10.1186/s13287-015-0003-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kalimuthu S, Zhu L, Oh JM, Gangadaran P, Lee HW, Baek SH, Rajendran RL, Gopal A, Jeong SY, Lee SW, Lee J, Ahn BC. Migration of mesenchymal stem cells to tumor xenograft models and in vitro drug delivery by doxorubicin. Int J Med Sci. 2018;15:1051–1061. doi: 10.7150/ijms.25760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wang H, Cao F, De A, Cao Y, Contag C, Gambhir SS, Wu JC, Chen X. Trafficking mesenchymal stem cell engraftment and differentiation in tumor-bearing mice by bioluminescence imaging. Stem Cells. 2009;27:1548–1558. doi: 10.1002/stem.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hakkarainen T, Särkioja M, Lehenkari P, Miettinen S, Ylikomi T, Suuronen R, Desmond RA, Kanerva A, Hemminki A. Human mesenchymal stem cells lack tumor tropism but enhance the antitumor activity of oncolytic adenoviruses in orthotopic lung and breast tumors. Hum Gene Ther. 2007;18:627–641. doi: 10.1089/hum.2007.034. [DOI] [PubMed] [Google Scholar]
- 91.Cai Y, Xi Y, Cao Z, Xiang G, Ni Q, Zhang R, Chang J, Du X, Yang A, Yan B, Zhao J. Dual targeting and enhanced cytotoxicity to HER2-overexpressing tumors by immunoapoptotin-armored mesenchymal stem cells. Cancer Lett. 2016;381:104–112. doi: 10.1016/j.canlet.2016.07.027. [DOI] [PubMed] [Google Scholar]
- 92.Knoop K, Kolokythas M, Klutz K, Willhauck MJ, Wunderlich N, Draganovici D, Zach C, Gildehaus FJ, Böning G, Göke B, Wagner E, Nelson PJ, Spitzweg C. Image-guided, tumor stroma-targeted 131I therapy of hepatocellular cancer after systemic mesenchymal stem cell-mediated NIS gene delivery. Mol Ther. 2011;19:1704–1713. doi: 10.1038/mt.2011.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Schug C, Gupta A, Urnauer S, Steiger K, Cheung PF, Neander C, Savvatakis K, Schmohl KA, Trajkovic-Arsic M, Schwenk N, Schwaiger M, Nelson PJ, Siveke JT, Spitzweg C. A Novel Approach for Image-Guided 131I Therapy of Pancreatic Ductal Adenocarcinoma Using Mesenchymal Stem Cell-Mediated NIS Gene Delivery. Mol Cancer Res. 2019;17:310–320. doi: 10.1158/1541-7786.MCR-18-0185. [DOI] [PubMed] [Google Scholar]
- 94.Tutter M, Schug C, Schmohl KA, Urnauer S, Schwenk N, Petrini M, Lokerse WJM, Zach C, Ziegler S, Bartenstein P, Weber WA, Wagner E, Lindner LH, Nelson PJ, Spitzweg C. Effective control of tumor growth through spatial and temporal control of theranostic sodium iodide symporter (NIS) gene expression using a heat-inducible gene promoter in engineered mesenchymal stem cells. Theranostics. 2020;10:4490–4506. doi: 10.7150/thno.41489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Schug C, Sievert W, Urnauer S, Müller AM, Schmohl KA, Wechselberger A, Schwenk N, Lauber K, Schwaiger M, Multhoff G, Wagner E, Nelson PJ, Spitzweg C. External Beam Radiation Therapy Enhances Mesenchymal Stem Cell-Mediated Sodium-Iodide Symporter Gene Delivery. Hum Gene Ther. 2018;29:1287–1300. doi: 10.1089/hum.2018.025. [DOI] [PubMed] [Google Scholar]
- 96.Belmar-Lopez C, Mendoza G, Oberg D, Burnet J, Simon C, Cervello I, Iglesias M, Ramirez JC, Lopez-Larrubia P, Quintanilla M, Martin-Duque P. Tissue-derived mesenchymal stromal cells used as vehicles for anti-tumor therapy exert different in vivo effects on migration capacity and tumor growth. BMC Med. 2013;11:139. doi: 10.1186/1741-7015-11-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Qiao Y, Gumin J, MacLellan CJ, Gao F, Bouchard R, Lang FF, Stafford RJ, Melancon MP. Magnetic resonance and photoacoustic imaging of brain tumor mediated by mesenchymal stem cell labeled with multifunctional nanoparticle introduced via carotid artery injection. Nanotechnology. 2018;29:165101. doi: 10.1088/1361-6528/aaaf16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.White FC, Roth DM, Bloor CM. The pig as a model for myocardial ischemia and exercise. Lab Anim Sci. 1986;36:351–356. [PubMed] [Google Scholar]
- 99.Willmann JK, Paulmurugan R, Rodriguez-Porcel M, Stein W, Brinton TJ, Connolly AJ, Nielsen CH, Lutz AM, Lyons J, Ikeno F, Suzuki Y, Rosenberg J, Chen IY, Wu JC, Yeung AC, Yock P, Robbins RC, Gambhir SS. Imaging gene expression in human mesenchymal stem cells: from small to large animals. Radiology. 2009;252:117–127. doi: 10.1148/radiol.2513081616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.U.S. National Library of Medicine Search of: Mesenchymal stem cells | recruiting, not yet recruiting, active, not recruiting, enrolling by invitation studies - list results - clinicaltrials.Gov. Available from: https://clinicaltrials.gov/ct2/results?cond=mesenchymal+stem+cells&Search=Apply&recrs=b&recrs=a&recrs=f&recrs=d&age_v=&gndr=&type=&rslt=
- 101.De Keyser J. Autologous mesenchymal stem cell transplantation in stroke patients. Ann Neurol. 2005;58:653–4; author reply 654. doi: 10.1002/ana.20612. [DOI] [PubMed] [Google Scholar]
- 102.Hare JM, Fishman JE, Gerstenblith G, DiFede Velazquez DL, Zambrano JP, Suncion VY, Tracy M, Ghersin E, Johnston PV, Brinker JA, Breton E, Davis-Sproul J, Schulman IH, Byrnes J, Mendizabal AM, Lowery MH, Rouy D, Altman P, Wong Po Foo C, Ruiz P, Amador A, Da Silva J, McNiece IK, Heldman AW, George R, Lardo A. Comparison of allogeneic vs autologous bone marrow–derived mesenchymal stem cells delivered by transendocardial injection in patients with ischemic cardiomyopathy: the POSEIDON randomized trial. JAMA. 2012;308:2369–2379. doi: 10.1001/jama.2012.25321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Heldman AW, DiFede DL, Fishman JE, Zambrano JP, Trachtenberg BH, Karantalis V, Mushtaq M, Williams AR, Suncion VY, McNiece IK, Ghersin E, Soto V, Lopera G, Miki R, Willens H, Hendel R, Mitrani R, Pattany P, Feigenbaum G, Oskouei B, Byrnes J, Lowery MH, Sierra J, Pujol MV, Delgado C, Gonzalez PJ, Rodriguez JE, Bagno LL, Rouy D, Altman P, Foo CW, da Silva J, Anderson E, Schwarz R, Mendizabal A, Hare JM. Transendocardial mesenchymal stem cells and mononuclear bone marrow cells for ischemic cardiomyopathy: the TAC-HFT randomized trial. JAMA. 2014;311:62–73. doi: 10.1001/jama.2013.282909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ponomarev V, Doubrovin M, Shavrin A, Serganova I, Beresten T, Ageyeva L, Cai C, Balatoni J, Alauddin M, Gelovani J. A human-derived reporter gene for noninvasive imaging in humans: mitochondrial thymidine kinase type 2. J Nucl Med. 2007;48:819–826. doi: 10.2967/jnumed.106.036962. [DOI] [PubMed] [Google Scholar]