Abstract
Background
Acupuncture is effective in symptom and quality of life improvement of chronic asthma, but the efficacy differences between different acupoints are uncertain. In terms of the theory of Meridian-viscera Association, the study aims to investigate the different effectiveness between acupoints in Lung meridian and the acupoints in Heart meridian, so as to provide the evidence to develop a better prescription of the acupuncture treatment of chronic persistent asthma.
Methods
This study is a multicentral randomized controlled trial. A total of 68 chronic persistent asthma patients will be randomly allocated into two groups: the Lung meridian group and the Heart meridian group. This trial will include a 2-week baseline period, a 4-week treatment period with 12 sessions’ acupuncture, and an 8-week follow-up period. The primary outcome is the Asthma Quality of Life Questionnaire (AQLQ). Secondary outcomes are the Asthma Control Test (ACT), Peak Expiratory Flow (PEF), and Forced Expiratory Volume in 1 s (FEV1). The AQLQ and ACT will be collected at baseline, week 4, week 8, and week 12 after randomization. PEF, FEV1, the Self-rating Anxiety Scale (SAS), and the Self-rating Depression Scale (SDS) will be assessed at baseline and week 4.
Discussion
The results will provide evidence for acupuncture prescription selection and the clinical efficacy improvement. The results of this trial will also be used to determine whether or not a full definitive trial will go ahead, which will further confirm the theory of Meridian-viscera Association.
Trial registration
Chinese Clinical Trial Registry (http://www.chictr.org.cn/showproj.aspx?proj=43803) ChiCTR1900027284. Registered on 7 November 2019
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13063-020-04844-8.
Keywords: Acupuncture, Chronic persistent asthma, Randomized controlled trial, Protocol, Theory of Meridian-viscera Association
Background
Asthma is characterized by bronchial hyper-responsiveness and chronic airway inflammation and accompanied by episodic wheezing, chest tightness, breathlessness, and cough [1, 2]. Asthma is one of the most common chronic respiratory diseases, and its prevalence varied from 0.2 to 21% in different countries [3]. The global prevalence of doctor-diagnosed asthma in adults is 4.3% and estimated to affect more than 300 million individuals worldwide [2]. Asthma not only significantly reduces patients’ quality of life (QoL) [4], leads to substantial disability [5], but also brings a heavy economic burden to patients, their families, and society, especially in low-income and middle-income countries [1, 6, 7]. Asthma is among the leading causes of mortality and morbidity worldwide [5], ranked among the top 20 conditions causing disability globally and ranked the 23rd as causes of disease burden as measured by disability-adjusted life years in 2015 [8, 9].
According to the 2019 Global Initiative for Asthma (GINA) guidelines on the management of asthma [2], current treatment options include asthma education, self-management strategies, elimination of risk factors, and medication control. Pharmacotherapies such as daily inhaled corticosteroids, long-acting inhaled β2-agonists are recommended to control symptoms and reduce the risk of serious exacerbations [2]. However, long-term pharmacological treatment inevitably has some potential side effects, such as adrenal suppression [10], decreased bone mineral density [11], liver toxicity [12], and increased risk of asthma-related death [13]. Therefore, seeking safe and effective therapies for asthma prevention and control aroused increasing concern [14–16].
Acupuncture, as a main complementary and alternative therapy, has traditionally been used to control asthma in China for thousands of years. Recently, accumulating evidence has supported the benefit of acupuncture for asthma [17, 18]. It is reported that acupuncture can significantly relieve the asthma-related symptoms, improve QoL, influence inflammatory cell counts [17], ameliorate of peak expiratory flow (PEF) variability [14], and increase the forced expiratory volume in 1 s (FEV1) [19]. However, most of these studies have focused on whether acupuncture is useful for asthma by comparing the efficacy differences between acupuncture and medication intervention [14, 18], or verum acupuncture and sham acupuncture [15, 17]. Few trials have involved the comparison of different acupuncture prescriptions to verify the efficacy differences between different acupuncture interventions.
According to the theory of traditional Chinese acupuncture, the Lung meridian connects with the lung directly, while the Heart meridian associates with the lung indirectly. Both the acupoints on Lung meridian and on the Heart meridian are commonly used for preventing and controlling asthma in clinical practice [20]. Hence, this multicenter randomized controlled trial focuses on the efficacy differences of the two acupoint prescriptions for treating asthma by evaluating the effectiveness of the acupoints on the Lung meridian compared to the acupoints on the Heart meridian, respectively, so as to provide high-quality evidence for a better acupuncture prescription selection and improve the curative effect.
Method and design
Study design
A two-arm, multi-center, randomized controlled trial will be conducted at the First Affiliated Hospital of Chengdu University of Traditional Chinese Medicine (CDUTCM) and the First Affiliated Hospital of Anhui University of Traditional Chinese Medicine. Sixty-eight eligible asthma patients diagnosed with the guide for asthma management and prevention of updated GINA 2019 [2] will be recruited and randomized into two groups with a 1:1 ratio. Outcome assessment will be performed at the baseline and the end of treatment and during the follow-up period. Patients enrolment will be started in November 2019 and is expected to end in October 2021. The details of the study design are shown in Fig. 1.
Fig. 1.
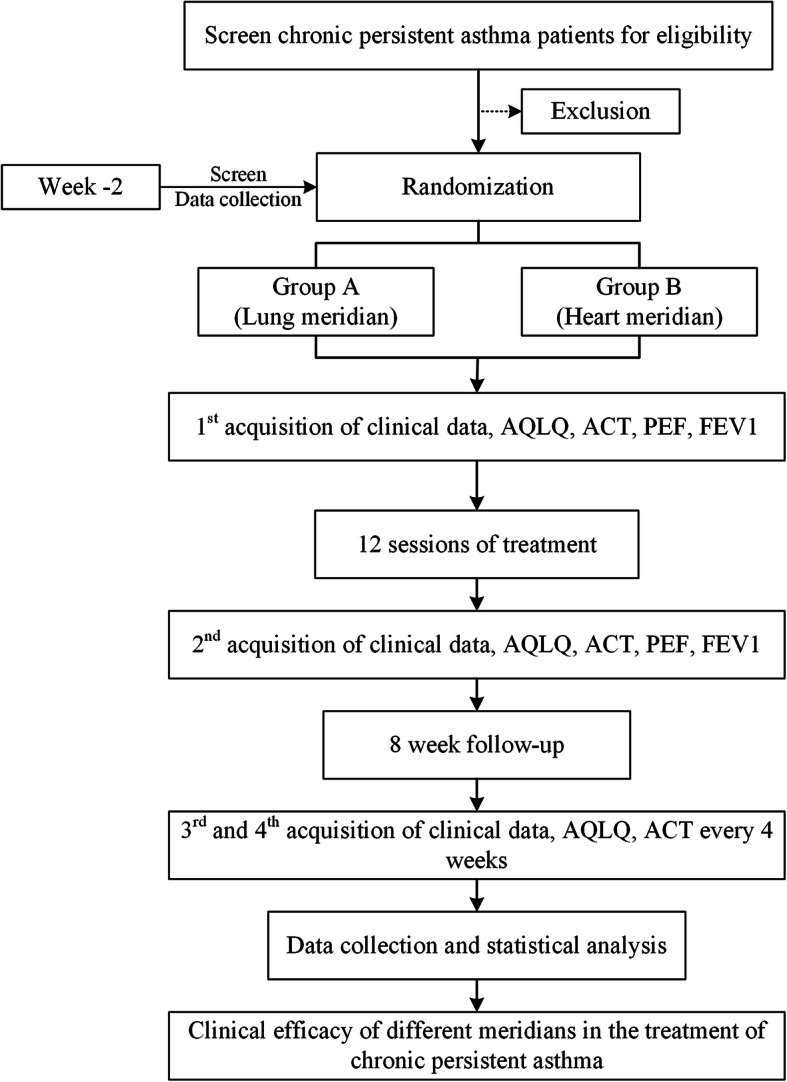
Study flowchart. Eligible patients will be randomly allocated into 2 groups with 1:1 ratio. Clinical data will be acquired at four timepoints: baseline (week 0), the end of treatment (week 4), and at the follow-up period (week 8, week 12). AQLQ Asthma Quality of Life Questionnaire, ACT Asthma Control Test, PEF Peak Expiratory Flow, FEV1 Forced Expiratory Volume in 1 s
This trial is reported in accordance with the Standard Protocol Items: Recommendations for Intervention Trials (SPIRIT) guidelines [21] (Table 1, Additional file 1) and follows the principles of the Consolidated Standards of Reporting Trials (CONSORT) and Standards for Reporting Interventions in Clinical Trial of Acupuncture (STRICTA) [22]. The study has been approved by the Ethics Committee of the First Affiliated Hospital of CDUTCM (the approved number: 2019KL-045) and was registered at the Chinese Clinical Trial Registry (registration number: ChiCTR1900027284).
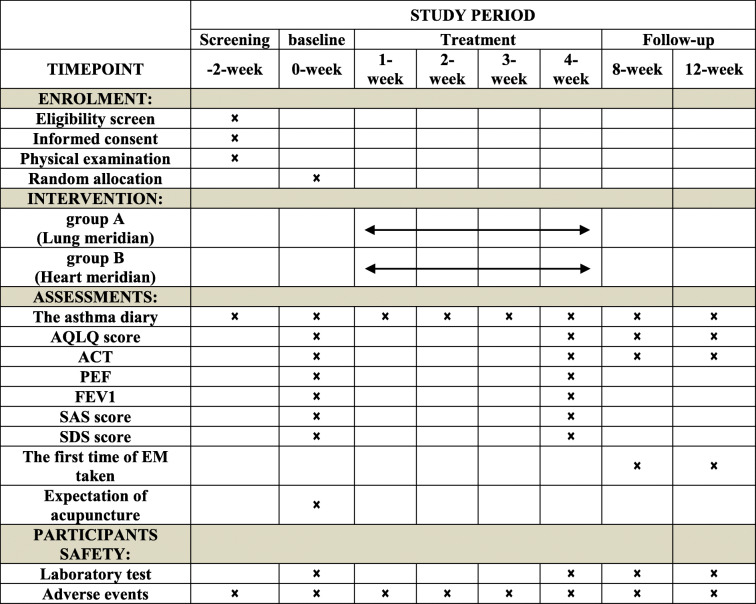
Table 1.
Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) schedule of the trial
This is a randomized controlled trial which includes a 2-week baseline period, a 4-week treatment period, and an 8-week follow-up period. In the baseline period, recruited patients will be screened, and eligible asthma patients will sign an informed consent and receive a physical examination. After allocation, the patients will receive 12 sessions of acupuncture (acupoint of Lung meridian or Heart meridian) during the treatment period. The outcome assessments, AQLQ, and ACT are performed at baseline, at the end of treatment, during the follow-up, and at the end of the follow-up. The outcome assessments, PEF, FEV1, SAS, and SDS are performed at baseline and at the end of treatment. In addition, the asthma dairy should be recorded at any time during the trial if asthma attacks. The first time of emergency medicine taken should be recorded at any time during the follow-up period. The expectation of acupuncture will be assessed at baseline. The physical examination including blood routine test and blood biochemical test will also be performed at the end of treatment to evaluate risks correlated with acupuncture. Adverse events will be recorded at any time during treatment
AQLQ Asthma Quality of Life Questionnaire, ACT Asthma Control Test, PEF Peak Expiratory Flow, FEV1 Forced Expiratory Volume in 1 s, SAS Self-rating Anxiety Scale, SDS Self-rating Depression Scale, EM Emergency Medicine
Randomization and allocation concealment
We will use an online or messaging system performed by a clinical information management system (Beijing Bioknow Information Science & Technology Co. Ltd., China) to complete the randomization. When participant-recruiting staffs in sub-center accept an eligible asthma patient, they will enter the patient’s name, gender, age, and medical history in the central randomization system. Then, a random number and an identification code, which are unique for each participant, will be assigned and delivered to the acupuncturists. The allocation number will be concealed from all the participants.
Blinding
The allocation will be concealed from all the participants. Patients will be told that they will receive one of the two effective interventions randomized after enrolment. As patients in the two groups will adopt different acupoints, interventions of each patient will be performed in separated cubicles to refrain the communication among patients in the two groups and will be asked to wear an eye-patch when they receive treatment. Outcome assessors, data collectors, and statisticians will also be blind to the procedure and result of randomization, group allocation, and intervention. We do not anticipate any requirement for unblinding as the acupuncturist is not blinded, but if required, the Trial Manager, Data Coordinator will have access to group allocations and any unblinding will be reported.
Participants and recruitment strategy
Participants will be mainly recruited from inpatients and outpatients in the respiratory department of the First Affiliated Hospital of CDUTCM, the Fifth People’s Hospital of Chengdu and the First Affiliated Hospital of Anhui University of Traditional Chinese Medicine. The recruitment strategies also include delivering leaflets at outpatients, posting advertisements in communities, and distributing news on the website of the Chengdu University of TCM and our WeChat public account. All potential asthma patients diagnosed with the GINA criteria will take a physical examination, which includes an x-ray plate, lung function test, electrocardiograph, routine blood test, liver function test, kidney function test, blood immune test (IgE), and urine and feces routine tests. The respiratory physician will make the final diagnosis of potential patients.
Sample size
According to a previous study that investigates the therapeutic effect of acupuncture for asthma [23], the mean improvement of the AQLQ was − 2.75 ± 4.52 (mean ± SD) in the acupuncture group and 0.86 ± 4.95 in the control group. With a two-side significance level of α = 0.05 and power of 80%, 27 participants are required in each group. Allowing for a 20% dropout rate, 34 participants per treatment arm will be recruited, equaling 68 patients in total.
Inclusion criteria
Patients fulfilling the following 7 items will be included: (1) aging from 18 to 65 years, (2) diagnosed as chronic persistent asthma by respiratory physicians according to the guide of GINA 2019 and medical history, (3) having mild or moderate asthma according to the GINA 2019, (4) having increased in the FEV1 of > 12% and > 200 mL from the pre-bronchodilator value, (5) the FEV1/forced vital capacity (FVC) < 70%, (6) without participating in any other clinical trials or receiving acupuncture due to asthma within 1 month, and (7) having signed informed consent.
Exclusion criteria
Patients who match any of the following 8 items will be excluded: (1) be hospitalized in intensive care unit due to acute exacerbation of asthma in the previous 3 months (representing patients at highest risk of adverse asthma outcomes); (2) be diagnosed as other pulmonary diseases such as bronchiectasis, tuberculosis, abscess, cystic fibrosis, alpha 1 antitrypsin deficiency, or restrictive lung disease; (3) having serious cardiovascular diseases such as uncontrolled heart failure, coronary disease, myocardial infarction, severe hypertension, or uncontrolled arrhythmia; (4) having other uncontrolled diseases including liver or kidney or hematopoietic diseases, endocrine and immune diseases, mental disorders, and malignancy; (5) asthma occurs only when accidentally exposed to allergens or chemical sensitizers; (6) having lower respiratory tract infection (e.g., pneumonia) or taking systemic glucocorticoids more than 10 days for severe acute asthma attacks within 1 month before enrollment; (7) currently be pregnant or breast feeding at the time of enrolment or planned pregnancy within the study period; or (8) having any acupuncture contraindications, such as serious atopic, infectious dermatopathy, thrombocytopenic purpura, or hemophilia.
Acupuncture interventions
The acupuncture treatment of each group will consist of 12 sessions of 30 min duration, each administered over a period of 4 weeks (three sessions per week). All the acupuncture manipulation will be performed by licensed acupuncturists with at least 5 year’s clinical experience.
The manual acupuncture stimulation will be performed at bilateral Taiyuan (LU9), Lieque (LU7), and Chize (LU5) for patients in group A, and manual acupuncture stimulation will be performed at bilateral Shenmen (HT7), Yinxi (HT6), and Shaohai (HT3) for patients in group B (Fig. 2).
Fig. 2.
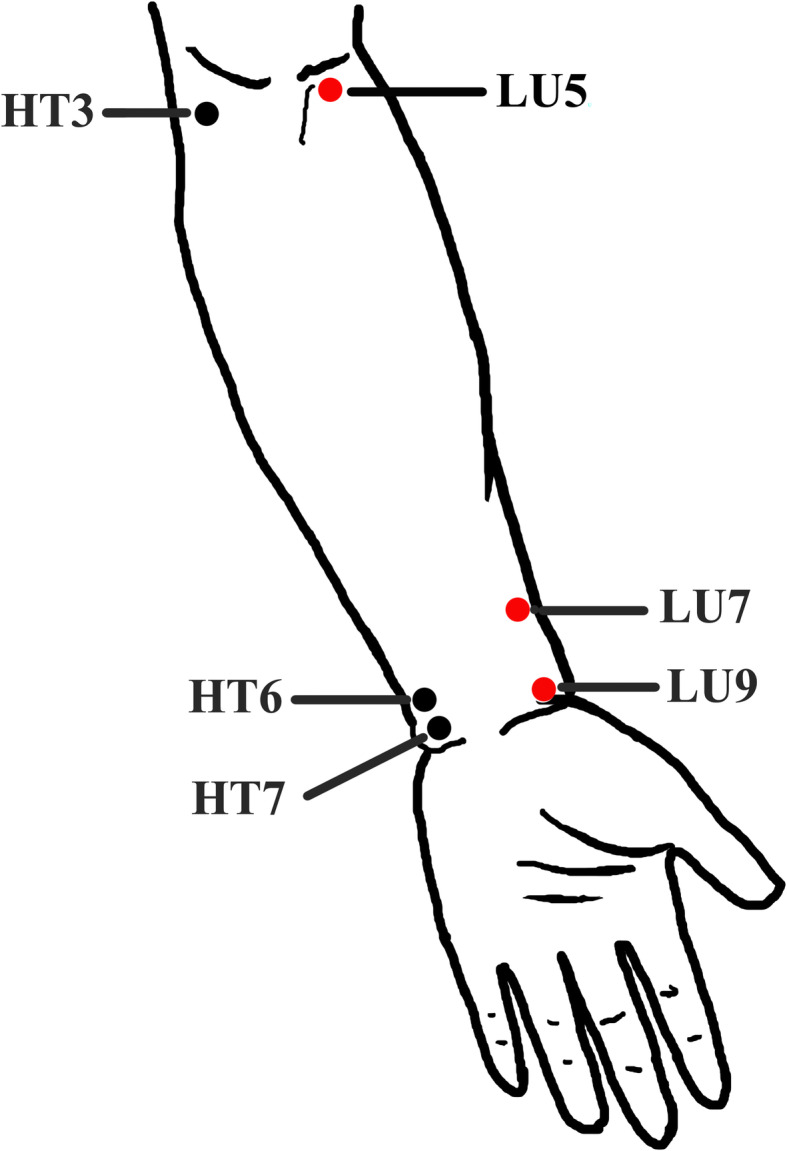
Locations of acupoints. Acupoints on Lung meridian—Chize (LU5): on the cubital crease, on the radial side of the tendon of biceps brachii; Lieque (LU7): on the radial margin of the forearm, 1.5 cun above the transverse crease of the wrist, between the brachioradial muscle tendon and the long abductor muscle tendon of thumb; and Taiyuan (LU9): on the radial side of the transverse crease of the wrist, where the radial artery pulsates. Acupoints on Heart meridian—Shaohai (HT3): at the midpoint of the line connecting the medial end of the transverse cubital crease with the medial epicondylus of the humerus; Yinxi (HT6): on the palmer side of the forearm, the point is on the radial side of the tendon of the flexor carpi ulnaris, 0.5 cun above the transverse crease of the wrist; and Shenmen (HT7): on the wrist, at the ulnar end of the transverse crease of the wrist, in the depression on the radial side of the tendon of the flexor carpi ulnaris
The acupuncture manipulation of these two groups is as follows: the disposable sterile filiform needles (0.25 × 25 mm, 0.35 × 40 mm; Huatuo Medical Instrument Co., Ltd., China) will be inserted into acupoints with the depth of 10–30 mm after skin disinfection by alcohol. Manipulations of twirling, lifting, and thrusting will be performed in order to induce deqi sensation. Then needles will be retained at the acupoints for 30 min. In order to maintain the deqi sensation, the above procedures will be manipulated intermittently during the 30 min.
Medications
Patients can use the inhaled doctor-directed Seretide (salmeterol and fluticasone) or Symbicort (formoterol and budesonide) as conventional therapy following the respiratory physicians’ instruction. Participants will be not allowed using other interventions during this trial but will be permitted to use inhaled salbutamol or other medication advised by doctors in an emergency. The name of medications, specifications, dose, duration of use, time of symptom relief, etc. will be recorded in details.
There should be at least 6 h between the use of salbutamol and lung function measurements. A stable dose of inhaled glucocorticoids and antihistamines should be maintained for at least 2 months prior to enrollment and during this study. If patients’ desensitization therapy is in the “maintenance” phase, the medication used should be maintained at a stable dose of at least 1 month prior to the enrollment and during this study. Short courses of antihistamine therapy or inhaled glucocorticoid therapy are allowed to treat hay fever. Short-term (< 10 days) use of systemic corticosteroids, aerosol therapy (including β2-agonists, anticholinergics, and steroids), and antibiotic therapy will be permitted during this study.
Outcome measurements
Primary outcome
Asthma Quality of Life Questionnaire (AQLQ)
In this study, the standard version of AQLQ will be used [24]. This questionnaire measures the functional problems that are most troublesome to adults with asthma over the 2 weeks prior to the interview. The AQLQ contains 32 items: activity limitation (11 items), symptoms (12 items), mental health (5 items), and environmental stimuli (4 items). Responses are rated on 7-point Likert scales for every item. High scores indicate a better health-related quality of life. The mean score of all 32 items is the overall AQLQ score. The minimum clinically important difference for AQLQ has been reported as 0.52 [25].
Secondary outcomes
Asthma Control Test (ACT)
Asthma control will be evaluated using the Asthma Control Test (ACT) [26, 27]. The ACT consists of five items: activity limitation, daytime shortness of breath, awaking due to asthma symptoms, needed puffs of reliever medication, and a global judgment of asthma control. All items refer to the last 4 weeks. They are scaled from 1 to 5. The sum of scores indicates asthma control. An ACT score of 20–25 indicates controlled asthma and of < 20 indicates uncontrolled asthma. A minimum clinically important difference of about 3 was identified [28].
Peak Expiratory Flow (PEF) and Forced Expiratory Volume in 1 s (FEV1)
PEF and FEV1 are determined using spirometry and body plethysmography before and after bronchodilation with a short-acting bronchodilator in accordance with recommendations of the national guidelines [29, 30].
The Self-rating Anxiety Scale (SAS) [31] and the Self-rating Depression Scale (SDS) [32] are used to assess the emotion of asthma patients. In addition, the asthma diary including the times, severity, duration of asthma attacks, medication compliance during the trial, and the first time to use the emergency medicine after treatment will also be recorded.
AQLQ and ACT will be evaluated at baseline (week 0), after the intervention (week 4), and at the follow-up (week 8, week 12). The PEF, FEV1, SAS, and SDS will be assessed at baseline (week 0), after the intervention (week 4). The asthma diary will be assessed during the whole trial (week 0– week 12). The expectation for efficacy in patients will be evaluated at baseline [33]. The first time to use emergency medicine after treatment will be evaluated during the follow-up. All the outcome evaluations will be performed by two independent outcome assessors. The two assessors are trained before participating in this trial and blinded to the randomization.
Data monitoring and management
All data will be managed with printed and electronic Case Report Forms (CRFs). Primary entries are not allowed to be changed and any correction should be explained with a signature in the appended notes. Only outcome assessors have access to CRFs, and double-data entry will be performed. The research team in Chengdu is responsible for all aspects of the organization. The Ethics Committee of the First Affiliated Hospital of Chengdu University of TCM will be supervising this trial and data every 3 months and will make the final decision to terminate the trial. The process will be independent from investigators and the sponsor. Interventionists will monitor adverse events and respond appropriately with encouragement and suggestions. All researchers, physicians, and related personal are required to understand and adhere to protocol details.
Data analysis
All data will be analyzed by an independent statistician using SAS 9.4 software (SAS Institute Inc., Cary, NC). All efficacy and safety analyses will be strictly conducted according to the intention-to-treat (ITT) principle. Multiple imputation will be used to deal with missing data. Continuous variables will be described with means and standard deviation (SD) or median, maximum, minimum, P25, and P75, as appropriate. And categorical variables will be described with percentage and frequencies.
The comparison between groups will be analyzed by the analysis of covariance (ANCOVA) if the change of outcomes from baseline to 4 weeks is normally distributed. The outcome variable will be the change of AQLQ from baseline to week 4, and covariates will be age, gender, duration of disease, and the expectation of acupuncture in the ANCOVA analysis. The non-parametric ANCOVA will be conducted if the change is not normally distributed. The comparisons between time points within groups will be analyzed using the paired sample t test or Wilcoxon rank-sum test, as appropriate. Separate ANCOVA analyses will be performed for each secondary outcome, the AQLQ and ACT at week 8 and week 12 follow-up. Categorical variables will be analyzed using the chi-squared test or Fisher’s exact test, as appropriate.
The center effects will be included in the analysis model. A subgroup analysis between inpatient and outpatient participants in each group will be performed exploratively. Statistical results will be presented as point estimates of effect sizes accompanied by confidence intervals.
Patient safety
Participants with fainting, infection, or other severe adverse events should be discontinued from treatment and processed immediately. Any adverse events will be recorded by patients, acupuncturists, and outcome assessors. Acupuncture related adverse events include bleeding, dizziness, pain, infection, and so on. Besides, any other severe events also will be recorded in the CRFs in detail and be monitored by the Ethics Committees.
Quality control
The trial protocol is reviewed and revised by the experts in acupuncture, methodology, pneumology, and statistics. The related staff will be trained using a prespecified standard operating procedure. The compliance of patients will be improved through health education and timely follow-up. The outcomes will also be evaluated by outcome assessors if the participants discontinue acupuncture or deviate from protocol.
Discussion
This is the first RCT focused on the efficacy differences of the acupoints on the Lung meridian compared to the acupoints on the Heart meridian for treating chronic persistent asthma. The results will provide evidence for acupuncture prescription selection and the clinical efficacy improvement. The results of this trial will also be used to determine whether or not a full definitive trial will go ahead, which will further confirm the theory of Meridian-viscera Association.
The theory of Meridian-viscera Association emphasizes the diagnostic and therapeutic values based on the mutual relation in physiology and pathology between meridians and viscera. That is, visceral physiological functions and pathological changes will manifest in the corresponding meridians or the acupoints [34], and the visceral disorders can be treated with the involved meridian and acupoints [35]. The lung is close to the heart anatomically, so the two viscera have close association physio-pathologically. Based on the theory of Meridian-viscera Association and clinical practice, the Lung meridian and the Heart meridian are the commonly used meridians for pulmonary disorders including asthma [17, 18]. Hence, this study will select Taiyuan (LU9), Lieque (LU7), and Chize (LU5) on the Lung meridian and Shenmen (HT7), Yinxi (HT6), and Shaohai (HT3) on the Heart meridian for the following reasons: (1) these acupoints have been proved to be effective in improving QoL and relieving symptoms of asthma patients [18, 23], (2) all of these acupoints are specific acupoints on the two meridians, and (3) the selected acupoints are on the medial side of the upper arm and at the same nerve segment based on the modern anatomy so as to minimized the bias of comparison.
The efficacy evaluation will be performed from the following three aspects: the quality of life, symptoms, and emotion of asthma patients. Asthma affects patients’ daily life seriously [4]; the improvement of QoL is essential for asthma patients, especially chronic persistent asthma patients. So the AQLQ will be assessed as the primary outcome, which is a reliable, valid, discriminating, and responsive measurement and is more sensitive than the 36-Item Short Form Survey (SF-36) questionnaire in detecting differences in asthma severity [36]. At the same time, the ACT, PEF, and FEV1, as secondary outcomes, will be evaluated before and after treatment in this trial. Patients with poor-controlled or uncontrolled asthma have more serious symptoms and worse lung function [37]. Hence, ACT will be performed to identify patients with poorly controlled asthma [26, 27], and PEF and FEV1 will be used to assess the severity of lung function in asthma patients [29, 30]. Moreover, anxiety and depression are emotional common disorders accompanied by adult asthma [38, 39]. So the SAS [31] and SDS [32] are used to assess the emotion of asthma patients.
Trial status
This trial is registered on the Chinese Clinical Trial Registry (http://www.chictr.org.cn) on 7 November 2019 (Registered number: ChiCTR1900027284, the protocol version number: V2.0). The patient recruitment of this trial has not been started and will begin on November 25, 2019, and will be completed on October 31, 2021.
Supplementary Information
Additional file 1. SPIRIT 2013 Checklist: Recommended items to address in a clinical trial protocol and related documents.
Acknowledgements
The authors thank Prof. Juying Zhang (West China Hospital of Sichuan University), Prof. Shiyan Yan (China Academy of Chinese Medical Sciences), Prof. Ying Li (Chengdu University of TCM), and Dr. Hongping Zhang (West China Hospital of Sichuan University) for their help in the consultation of this RCT protocol.
Abbreviations
- ACT
Asthma Control Test
- ANCOVA
The analysis of covariance
- AQLQ
Asthma Quality of Life Questionnaire
- CDUTCM
Chengdu University of Traditional Chinese Medicine
- CONSORT
The Consolidated Standards of Reporting Trials
- CRFs
Case Report Forms
- FEV1
Forced Expiratory Volume in 1 s
- FVC
Forced Vital Capacity
- GINA
Global Initiative for Asthma
- ITT
Intention-to-treat analysis
- PEF
Peak Expiratory Flow
- QoL
Quality of Life
- RCT
Randomized Controlled Trial
- SAS
Self-rating Anxiety Scale
- SD
Standard Deviation
- SDS
Self-rating Depression Scale
- SF-36
36-Item Short Form Survey
- SPIRIT
Standard Protocol Items Recommendations for Intervention Trials
- STRICTA
Standards for Reporting Interventions in Clinical Trial of Acupuncture
- TCM
Traditional Chinese Medicine
Authors’ contributions
F Z conceived of the study. F Z, SR C, XH D, and L L initiated the study design. XH D, SR C, and L L helped with its implementation. SR C, XH D, and LL drafted the manuscript. F Z, L L, and SY Y revised the manuscript. All authors contributed to the refinement of the study protocol and approved the final manuscript.
Funding
The trial is financially supported by the National Key Research and Development Program (NO.2018YFC1704600, 2018YFC1704605). The sponsor played no part in the study design; collection, management, analysis, and interpretation of data; writing of the report; and the decision to submit the report for publication.
Availability of data and materials
The data and materials during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This trial has been approved by the Institutional Review Boards and Ethics Committees of the First Affiliated Hospital of Chengdu University of TCM (Approved number: 2019KL-045). This trial follows the principles of the Declaration of Helsinki (Version Edinburgh 2000). An informed consent form will be obtained from patients prior to the enrolment.
Consent for publication
Study results will be published by the investigators in peer-reviewed journals or presented at conferences.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shirui Cheng, Xiaohui Dong, and Lei Lan are co-first authors.
Contributor Information
Shirui Cheng, Email: csr1190@163.com.
Xiaohui Dong, Email: dongxiaohui0405@126.com.
Lei Lan, Email: lanlei@cdutcm.edu.cn.
Zhaoxuan He, Email: hezhaoxuan@cdutcm.edu.cn.
Siyi Yu, Email: cdutcmysy@gmail.com.
Yi Yang, Email: thehanyang@163.com.
Chuantao Zhang, Email: 664958917@qq.com.
Mei Chen, Email: alice_chenmei@163.com.
Jun Yang, Email: yangjunacup@126.com.
Yalan Liu, Email: 1465219944@qq.com.
Menglin Wang, Email: 1511253180@qq.com.
Qingsong Huang, Email: hqs1261@126.com.
Fang Zeng, Email: zeng_fang@cdutcm.edu.cn.
References
- 1.Papi A, Brightling C, Pedersen SE, Reddel HK. Asthma. Lancet. 2018;391(10122):783–800. doi: 10.1016/S0140-6736(17)33311-1. [DOI] [PubMed] [Google Scholar]
- 2.Global Initiative for Asthma . Global strategy for asthma management and prevention. 2019. [Google Scholar]
- 3.To T, Stanojevic S, Moores G, Gershon AS, Bateman ED, Cruz AA, et al. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC Public Health. 2012;12:204. doi: 10.1186/1471-2458-12-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crossman-Barnes C-J, Sach T, Wilson A, Barton G. Estimating loss in quality of life associated with asthma-related crisis events (ESQUARE): a cohort, observational study. Health Qual Life Outcomes. 2019;17(1):58. doi: 10.1186/s12955-019-1138-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.GBD 2015 Chronic Pespiratory Disease Collaborators Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med. 2017;5(9):691–706. doi: 10.1016/S2213-2600(17)30293-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen S, Golam S, Myers J, Bly C, Smolen H, Xu X. Systematic literature review of the clinical, humanistic, and economic burden associated with asthma uncontrolled by GINA Steps 4 or 5 treatment. Curr Med Res Opin. 2018;34(12):2075–2088. doi: 10.1080/03007995.2018.1505352. [DOI] [PubMed] [Google Scholar]
- 7.Weiss KB, Gergen PJ, Hodgson TA. An economic evaluation of asthma in the United States. N Engl J Med. 1992;326(13):862–866. doi: 10.1056/NEJM199203263261304. [DOI] [PubMed] [Google Scholar]
- 8.GBD 2015 Moortality and Causes of Death Collaborators Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.GBD 2015 Disease and Injury Incidience and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lipworth B, Kuo C, Jabbal S. Adrenal suppression with inhaled corticosteroids: the seed and the soil. Lancet Respir Med. 2018;6(6):e19. doi: 10.1016/S2213-2600(18)30148-6. [DOI] [PubMed] [Google Scholar]
- 11.Wise R, Connett J, Weinmann G, Scanlon P, Skeans M. Effect of inhaled triamcinolone on the decline in pulmonary function in chronic obstructive pulmonary disease. N Engl J Med. 2000;343(26):1902–1909. doi: 10.1056/NEJM200012283432601. [DOI] [PubMed] [Google Scholar]
- 12.Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald JM, et al. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008;31(1):143–178. doi: 10.1183/09031936.00138707. [DOI] [PubMed] [Google Scholar]
- 13.Nelson HS, Weiss ST, Bleecker ER, Yancey SW, Dorinsky PM. The salmeterol Multicenter Asthma Research Trial: a comparison of usual pharmacotherapy for asthma or usual pharmacotherapy plus salmeterol. Chest. 2006;129(1):15–26. doi: 10.1378/chest.129.1.15. [DOI] [PubMed] [Google Scholar]
- 14.Scheewe S, Vogt L, Minakawa S, Eichmann D, Welle S, Stachow R, et al. Acupuncture in children and adolescents with bronchial asthma: a randomised controlled study. Complement Ther Med. 2011;19(5):239–246. doi: 10.1016/j.ctim.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 15.Joos S, Schott C, Zou H, Daniel V, Martin E. Immunomodulatory effects of acupuncture in the treatment of allergic asthma: a randomized controlled study. J Altern Complement Med. 2000;6(6):519–525. doi: 10.1089/acm.2000.6.519. [DOI] [PubMed] [Google Scholar]
- 16.Brinkhaus B, Roll S, Jena S, Icke K, Adam D, Binting S, et al. Acupuncture in patients with allergic asthma: a randomized pragmatic trial. J Altern Complement Med. 2017;23(4):268–277. doi: 10.1089/acm.2016.0357. [DOI] [PubMed] [Google Scholar]
- 17.Pai HJ, Azevedo RS, Braga AL, Martins LC, Saraiva-Romanholo BM, Martins Mde A, et al. A randomized, controlled, crossover study in patients with mild and moderate asthma undergoing treatment with traditional Chinese acupuncture. Clinics (Sao Paulo) 2015;70(10):663–669. doi: 10.6061/clinics/2015(10)01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Choi JY, Jung HJ, Kim JI, Lee MS, Kang KW, Roh YL, et al. A randomized pilot study of acupuncture as an adjunct therapy in adult asthmatic patients. J Asthma. 2010;47(7):774–780. doi: 10.3109/02770903.2010.485665. [DOI] [PubMed] [Google Scholar]
- 19.Chu KA, Wu YC, Ting YM, Wang HC, Lu JY. Acupuncture therapy results in immediate bronchodilating effect in asthma patients. J Chin Med Assoc. 2007;70(7):265–268. doi: 10.1016/S1726-4901(07)70002-3. [DOI] [PubMed] [Google Scholar]
- 20.Li J, Wei J, Liu S. The law of selecting acupoint treating for asthma. Acupunct Res. 2000;25(1):78–80. [Google Scholar]
- 21.Chan AW, Tetzlaff JM, Gotzsche PC, Altman DG, Mann H, Berlin JA, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ. 2013;346:e7586. doi: 10.1136/bmj.e7586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hugh M, Altman DG, Hammerschlag R, Hammerschlag R, Li YP, Wu TX, et al. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement (Chinese version) Zhong Xi Yi Jie He Xue Bao. 2010;8(9):804–818. doi: 10.3736/jcim20100902. [DOI] [PubMed] [Google Scholar]
- 23.Mehl-Madrona L, Kligler B, Silverman S, Lynton H, Merrell W. The impact of acupuncture and craniosacral therapy interventions on clinical outcomes in adults with asthma. Explore (NY) 2007;3(1):28–36. doi: 10.1016/j.explore.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 24.Juniper EF, Buist AS, Cox FM, Ferrie PJ, King DR. Validation of a standardized version of the Asthma Quality of Life Questionnaire. Chest. 1999;115(5):1265–1270. doi: 10.1378/chest.115.5.1265. [DOI] [PubMed] [Google Scholar]
- 25.Alpaydin AO, Bora M, Yorgancioglu A, Coskun AS, Celik P. Asthma control test and Asthma Quality of Life Questionnaire association in adults. Iran J Allergy Asthma Immunol. 2012;11(4):301–307. [PubMed] [Google Scholar]
- 26.Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA, et al. Asthma Control Test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol. 2006;117(3):549–556. doi: 10.1016/j.jaci.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 27.Schatz M, Mosen DM, Kosinski M, Vollmer WM, Magid DJ, O'Connor E, et al. Validity of the Asthma Control Test completed at home. Am J Manag Care. 2007;13(12):661–667. [PubMed] [Google Scholar]
- 28.Schatz M, Kosinski M, Yarlas AS, Hanlon J, Watson ME, Jhingran P. The minimally important difference of the Asthma Control Test. J Allergy Clin Immunol. 2009;124(4):719–23.e1. doi: 10.1016/j.jaci.2009.06.053. [DOI] [PubMed] [Google Scholar]
- 29.Criee CP, Baur X, Berdel D, Bosch D, Gappa M, Haidl P, et al. Standardization of spirometry: 2015 update. Published by German Atemwegsliga, German Respiratory Society and German Society of Occupational and Environmental Medicine. Pneumologie. 2015;69(3):147–164. doi: 10.1055/s-0034-1391345. [DOI] [PubMed] [Google Scholar]
- 30.Criee CP, Sorichter S, Smith HJ, Kardos P, Merget R, Heise D, et al. Body plethysmography--its principles and clinical use. Respir Med. 2011;105(7):959–971. doi: 10.1016/j.rmed.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 31.Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- 32.Zung WW. A Self-Rating Depression Scale. Arch Gen Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]
- 33.Wang H, Fu Y, Qiu Y, et al. Acupuncture expectation and its clinical evaluation. Zhongguo Zhen Jiu. 2017;37(2):215–218. doi: 10.13703/j.0255-2930.2017.02.032. [DOI] [PubMed] [Google Scholar]
- 34.Zhang WB, Wang YP, Li HY. Analysis on correlation between meridians and viscera in book the Yellow Emperor’s Internal Classic. Zhen Ci Yan Jiu. 2018;43(7):424–429. doi: 10.13702/j.1000-0607.180185. [DOI] [PubMed] [Google Scholar]
- 35.Liu WT, Zhang LP, Zheng MF. Current researches and ideas regarding correlation between meridians and viscera. Zhen Ci Yan Jiu. 2018;43(7):430–432. doi: 10.13702/j.1000-0607.180069. [DOI] [PubMed] [Google Scholar]
- 36.Wang N, Huang X, Chen W, Zhang X, Zhang Y, Chen Y. Psychometric properties of a Chinese Asthma Quality of Life Questionnaire. J Asthma. 2017;54(10):1073–1084. doi: 10.1080/02770903.2017.1291674. [DOI] [PubMed] [Google Scholar]
- 37.Gebremariam TH, Binegdie AB, Mitiku AS, Ashagrie AW, Gebrehiwot KG, Huluka DK, et al. Level of asthma control and risk factors for poor asthma control among clinic patients seen at a referral hospital in Addis Ababa, Ethiopia. BMC Res Notes. 2017;10(1):558. doi: 10.1186/s13104-017-2887-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lehto K, Pedersen NL, Almqvist C, Lu Y, Brew BK. Asthma and affective traits in adults: a genetically informative study. Eur Respir J. 2019;53(5):1802142. doi: 10.1183/13993003.02142-2018. [DOI] [PubMed] [Google Scholar]
- 39.Galić K, Dodaj A, Ćorluka-Čerkez V, Lasic V, Pejić R, Šimić J, et al. Study of depression and anxiety in patients with asthma and chronic obstructive pulmonary disease. Psychiatr Danub. 2019;31(Suppl 1):112–117. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. SPIRIT 2013 Checklist: Recommended items to address in a clinical trial protocol and related documents.
Data Availability Statement
The data and materials during the current study are available from the corresponding author on reasonable request.