Abstract
Background:
Epidemiological studies on tennis injuries are mainly conducted in either elite professional or junior players. Injury patterns might differ in the recreational tennis player.
Purpose:
To investigate acute injuries in the recreational tennis–playing population with an additional focus on acute injuries that require surgical treatment.
Study Design:
Case series; Level of evidence, 4.
Methods:
A retrospective data analysis was conducted among patients who sustained an acute tennis injury between January 2013 and December 2018 and who had treatment administered at a single university hospital. Demographic data, diagnosis, body region of the trauma, injury mechanism, and treatment methods were recorded. Data were evaluated using descriptive statistics.
Results:
A total of 449 patients sustained 467 injuries (148 female, 301 male; mean age, 43.6 years; range, 8.2-84.4 years). The injuries occurred throughout the year, with an increased prevalence in the summer months. Injuries occurred in the lower extremity in 59%, the upper extremity in 30%, and the head and trunk in 11%. The main reason for an injury was a twist of a specific joint (n = 194) or a fall (n = 102). Harmless contusion or strains were the most common injury (49%). Ankle sprains were the most common serious injury, occurring in 11% of patients. Fractures occurred in 54 cases (12%). Overall, 9% of patients were treated surgically (fractures, n = 13; meniscal tears, n = 8; Achilles tendon ruptures, n = 6), and surgery was advised to another 1% who did not receive surgery at the study hospital.
Conclusion:
Typical acute injuries in recreational tennis players differ from acute injuries in elite and junior players, with an increased fracture occurrence. The main causes of acute tennis injuries are falls and twists, with 10% of injuries needing surgical treatment, mainly for fractures, meniscal tears, and Achilles tendon ruptures.
Keywords: tennis, injury, recreational, prevention, strain, sprain, fracture, Achilles
Currently, there are 1978 professional male tennis players ranked on the Association of Tennis Professionals (ATP) tour and 1318 on the Women’s Tennis Association tour. Yet, tennis is also played by millions of nonprofessionals in every age around the world. Several studies have investigated injury data in professional, elite, collegiate, and junior players.5,8,10,23–25,33 Data from a 5-year summary from the ATP tour showed that the spine was the region with the highest injury rate among players, followed by lower similar rates for foot/ankle, thigh, and shoulder injuries.8 In contrast, data from several other studies have shown that most tennis injuries occur in the lower extremity (31%-67%), followed by the upper extremity (20%-49%) and finally the trunk (3%-21%).1,9,19,28 This apparent discrepancy may be a result of different cohorts or different inclusion criteria of injuries. Injuries can be grouped, for example, into acute, acute-on-chronic, or chronic onset injuries while other studies and injury surveillance studies use the categorization of sudden versus gradual for classification.34 Different studies might mix these groups together. Pluim et al28 and others1,25 have reported that a greater number of acute injuries occur in the lower extremities and that chronic injuries (overuse/gradual onset injuries) more often manifest in the upper extremity. Since most studies are conducted in either elite professional or junior players, injury patterns might differ in the recreational tennis player. There are presently fewer studies in the literature investigating acute injury patterns in recreational, as opposed to professional, tennis players.
The purpose of this study was to investigate acute injuries in the recreational tennis–playing population. An additional focus of this investigation was set on acute injuries that required surgical treatment. The results of this study may be used to develop preventive strategies for recreational tennis players to reduce their risk of injury.
Methods
A retrospective data analysis was conducted among patients who sustained a tennis injury between January 2013 and December 2018 and were treated at the local community university hospital (Medical University Innsbruck). Institutional review board approval was waived for this study based on its retrospective data analysis design.
An automatic chart search was conducted for the word “tennis” within our patient chart database. Only patients who sustained an acute tennis injury were included in the study. The patient history had to state that pain occurred acutely on the court and that the patient did not experience pain before the traumatic event. Patients who did not sustain an acute tennis injury or who had chronic pain while playing tennis were excluded from this analysis.
The date of birth, sex, month of injury, diagnosis, body region of the trauma, injury mechanism, and treatment method were recorded for the patients identified in the automatic chart search. The body region was categorized into 13 areas: head, spine, thorax, abdomen, shoulder, elbow, wrist/hand, hip, knee, ankle, foot, thigh, and calf. The treatment method was subclassified into nonsurgical or surgical treatment. The injury mechanism was classified according to the patient report as 1 of 16 types: ball catch, ball hit, fall, twist, hit, jump, large step, racquet hit, run/hit against a wall, slip, sudden dislocation, stop, sudden instability, sudden sharp pain, step on a ball, or unspecified.
The data were first deidentified and then recorded and analyzed using Microsoft Excel (Version 2016). All data are presented using descriptive statistics.
Results
In total, 449 patients with 467 injuries were identified. There were 148 female and 301 male patients in the data sample, with a mean age of 43.6 years (range, 8.2-84.4 years). The injuries occurred throughout the year, with an increased prevalence in the summer months (Figure 1). Overall, 245 patients injured their right extremity and 179 their left one; 23 were not specifiable; and 2 injured themselves bilaterally. A total of 403 (90%) patients were treated without surgery, while 41 (9%) needed surgical treatment. Surgical treatment was advised to another 5 (1%) who did not seek surgical treatment at our institution.
Figure 1.
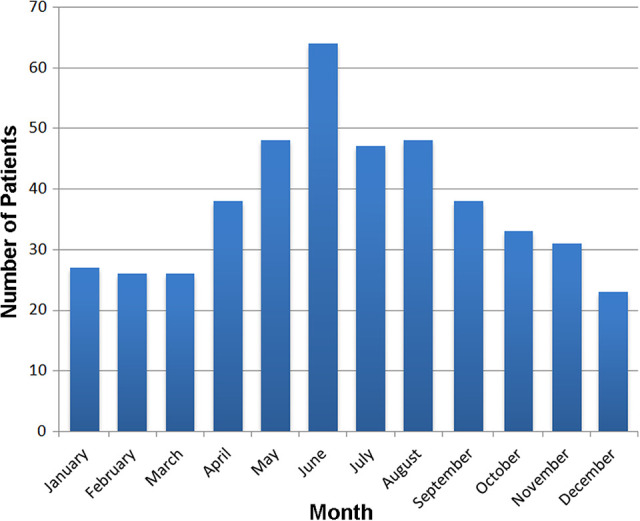
Distribution of injuries throughout the year.
Injuries occurred to the upper extremity in 141 cases (30%), to the lower extremity in 274 (59%), and to the head and trunk in 52 (11%). The distribution of the injured body parts is shown in Figure 2.
Figure 2.
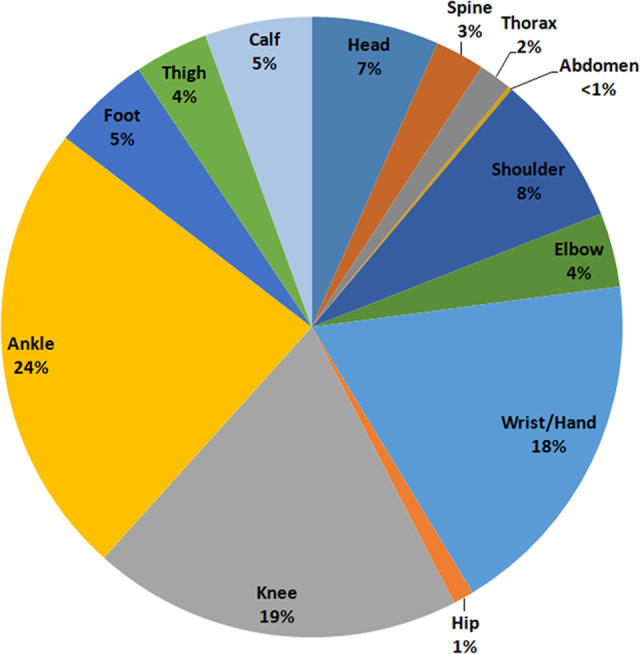
Distribution of injuries by body region.
Appendix Table A1 shows the injury patterns according to body region and trauma mechanism. The main reasons for the acute injuries studied in this investigation were a twist (n = 194) of the specific joint or a fall (n = 102). The most common injury was a harmless contusion or strain (49%), and the most common serious injury was an ankle sprain (11%). Fractures occurred in 54 cases (12% of overall injuries): 72% were located in the upper body, 19% in the lower body, 6% in the face, and 4% in the trunk/ribs. Fractures were distributed fairly evenly between male (54%) and female (46%) players.
Surgical treatment was mainly necessary for fractures as well as meniscal and Achilles tendon tears. Table 1 shows surgical treatments by body region. Patients who needed surgical treatment for a meniscal tear showed an acute onset of pain after a knee twist on the tennis court. These patients were 33 to 66 years old; there were no differences in the occurrence of tears between men and women. All tears were located at the posterior horn with a variable rupture pattern (radial, horizontal, bucket-handle, and complex tears).
Table 1.
Surgical Treatment by Body Regiona
| Body Region (No. of Injuries) | Injury: Surgical Treatment (No.) |
|---|---|
| Head (2) | Wound: wound care/stitches (2) |
| Spine | NA |
| Thorax (1) | Pneumothorax: thoracic drainage (1) |
| Abdomen | NA |
| Shoulder (4) | Humeral shaft and humeral head fracture: ORIF (2) |
| Impingement and SLAP lesion: AS, debridement, LBT tenodesis (1) | |
| Pulley lesion and biceps tendinitis: subacromial decompression and LBT tenodesis (1) | |
| Elbow (1 [1]) | Radial neck fracture: ORIF (1) |
| Distal biceps tendon lesion: [1] | |
| Wrist/Hand (13 [1]) | Distal radial fracture: ORIF (4) |
| Finger fracture: CRIF (1) | |
| Scaphoid fracture: CRIF (1) | |
| PIP joint dislocation: suture fixation (1), fragment fixation (1) | |
| Ulnocarpal impingement and ECU tendon subluxation: arthroscopy and debridement (1) | |
| Ulnar collateral ligament rupture of the thumb: anchor fixation (1) | |
| TFCC rupture: arthroscopic TFCC refixation (2) | |
| MP joint contusion: tenolysis + arthrolyses (1) | |
| Antebrachial fracture: [1] | |
| Hip (1) | Pertrochanteric femoral fracture: TFNA implantation (1) |
| Knee (10 [1]) | Meniscal rupture: resection (6) / suture (2) |
| ACL rupture: ACL reconstruction (3 [1: meniscal resection]) | |
| Wound: wound care/stitches (1) | |
| Free joint body: removal of free joint body (1) | |
| Ankle (8 [2]) | Achilles tendon rupture: tendon suture (6 [2]) |
| Malleolar fracture: ORIF (2) | |
| Foot | NA |
| Thigh (1) | Hamstring rupture: hamstring refixation (1) |
| Calf | NA |
aBrackets represent cases where surgery was advised. ACL, anterior cruciate ligament; AS, arthroscopy; CRIF, closed reduction and internal fixation; ECU, extensor carpi ulnaris; LBT, long biceps tendon; MP, metacarpophalangeal; NA, not applicable; ORIF, open reduction and internal fixation; PIP, proximal interphalangeal joint; SLAP, superior labral tear from anterior to posterior; TFCC, triangular fibrocartilage complex; TFNA, titanium trochanteric fixation nail advanced.
Age- and Sex-Based Injury Characteristics
When compared with the overall cohort, ankle sprains occurred in players who were younger (mean ± SD, 35.9 ± 15.8 vs 43.6 ± 8.2 years) and in more female players than male players (14% vs 10%). Female players also presented with proportionally more fractures than male players (17% vs 10% of emergency room visits). Patients with a fracture were similar in age to patients with any other injury (46 ± 24 vs 43 ± 19 years). However, distal radial fractures occurred in patients who were older (67 ± 9 years) and in more female than male patients (64% vs 36%).
Patients who sustained a muscle injury were older (54 ± 15 years) than the overall cohort; also, 70% of muscle injuries were in male patients versus 30% in female patients. With respect to the overall patient count and sex distribution, as a proportion of emergency room visits, the number of muscle injuries was similar in male and female players (10% vs 9%). Only men had complete Achilles tendon ruptures, and their mean age was 49 ± 10 years.
Patients with an ACL lesion had a mean age of 43 ± 11 years, and 47% of ACL injuries occurred to male and 53% to female players. With respect to the overall patient count and sex distribution, ACL injuries represented a greater proportion of injuries in female players as compared with male players (4.8% vs 2.3%).
Discussion
This study provides a comprehensive overview of acute injuries in recreational tennis players. Injuries to the lower extremity were the leading cause of presentation to our clinic, followed by the upper extremity and the trunk, with similar proportions to previous reports.1,9,19,28 Although most injuries were harmless and mild, 10% of patients sustained a fracture, mainly because of a fall on the court. This is in contrast to previous studies that reported very few fractures in recreational and professional players.5,10,19 A higher fracture incidence was already recognized by Gaw et al,9 at 14.6% in US emergency room visits. Because that study and ours investigated patients seeking care in the emergency department, it seems difficult to compare the cohorts with other previous reports on injury rates during tournaments and the ATP tour.
Patients sustaining a fracture that is typical for osteopenia or osteoporosis were mainly 60 to 80 years old. Although we did not assess the bone quality, these patients may have had poor bone quality given their age and the typical fracture presentation. Unfortunately, the dominant arm, the frequency of playing tennis or another sport, and medication intake (osteoporosis) were not known in these patients. Bone mineral content has been shown to be significantly higher in the dominant arm than the contralateral arm in tennis players.4 Players hold the racquet in the dominant arm, which is usually the right arm, and usually try to protect themselves with the free arm during the fall, which may be the main reason for injuries to the left extremity. Additional reduced bone mineral content in the older population may increase the fracture risk during fall.
Ankle sprains accounted for a majority of cases, similar to previous reports in tennis players.9,33 The main risk factor for ankle injuries in tennis is probably the sport itself, with its sudden multidirectional movement changes. Explosive peak inversion and internal rotation of the ankle can be 1 cause of ankle sprains in tennis players who play with lots of cutting.7 Although often cited by coaches, a trip over a ball causing an ankle sprain was seen only once in this study. However, players often recognize this risk factor and usually clear the playing area of balls that are lying around. Looking at the mean age of patients in this study who sustained an ankle sprain (36 ± 16 years), one can assume that younger players are either more prone to sustain an ankle injury or rather play, compete, and run faster, which may facilitate an inversion ankle sprain. Regular preplay warm-up and stretching, as well as proprioceptive, neuromuscular, and exercise training, have been shown to reduce the risk of ankle sprains3,14,16,26,31,35 and could be especially advised to the younger recreational players. However, the effectiveness of injury prevention programs in tennis remains questionable because it was recently shown that adult recreational tennis players did not reduce their ankle injury rate after an unsupervised tennis-specific exercise program.27 Players should try to land with a neutral ankle orientation and keep the center of pressure from shifting laterally during sideward cutting motions.7
Muscle strains are very typical for tennis and occur mainly in the adductor, hamstring, quadriceps, and gastrocnemius muscles,5,10,19,33 which is similar to the presented data showing muscle lesion with a sudden sharp pain in the age group between 40 and 60 years. Increased age is a nonreversible risk factor for muscle injuries.11,29 An insufficient warm-up and a reduced muscle strength and joint range of motion are reported to be risk factors for muscle injuries.2,6,20,29
An Achilles tendon rupture is a common acute injury in tennis players19,30 and occurs usually through a push-off mechanism, a sudden and unexpected dorsiflexion of the ankle, or a violent dorsiflexion of a plantarflexed foot.12 Given the sudden multidirectional movement changes in tennis, unexpected ankle dorsiflexion or sudden push-off can occur abruptly. Interestingly, only 45- to 65-year-old men had a complete Achilles tendon lesion. The mean age (49 years) seems slightly higher than the mean patient age in the literature; however, the male predominance has sufficiently been reported.13 One possible explanation for the higher age may be that tennis is played by older persons with a higher socioeconomic background regarding the absolute player count. Younger patients instead participate in soccer, climbing, mountain biking, and winter sports in our mountain area. Interestingly, forefoot players produce a larger Achilles tendon force during a forehand topspin stroke than rearfoot players,18 which may lead to an Achilles tendon lesion. However, it is unknown whether forefoot or rearfoot players are more prone to Achilles tendon injuries. Finally, large peak breaking forces, which frequently occur in tennis, negatively influence tendon health21 and should be avoided.
Knee twists with consecutive meniscal lesions are known injuries in tennis.5,19,22 These injuries were one of the main causes for surgery in our study. Although all patients with a meniscal injury in this cohort reported a sudden onset of pain, their age ranged from 33 to 66 years, which may lead to the assumption that these patients sustained an acute-on-chronic lesion. The specific movement pattern of tennis, including sudden directional changes, seems to be the major risk factor for these injuries. Since multiple directional movement changes are part of the game, with up to 4.2 directional changes per point,17 this risk factor seems rather unchangeable. Therefore, tennis players will presumably always be prone to meniscal injuries.
The common reasons for surgical treatment were fractures to the upper extremity as well as meniscal tears and Achilles tendon ruptures in the lower extremity, similar to previous reports.15,19,28 The role of preventive exercise for the core and rotator cuff and scapular musculature has been proposed and recommended for recreational and elite-level tennis players, with dynamic warm-up before play and static stretching after tennis play.17,32 Knowing which acute injuries occur in tennis, future researchers may focus on preventive strategies to lower the risk of the most common acute injuries in the recreational player.
There are some limitations to this study. It is a retrospective data analysis without a possibility for any outcome or risk factor evaluation. This study cannot deduce any injury incidence rates because the number of tennis players and the playing hours are not known. It is important to note that only injuries with an acute onset that presented to our emergency department were evaluated in the present study. Chronic tennis injuries were not included in this evaluation. Potentially more patients needed medical and/or surgical treatment that they received in a different clinic or department for acute injuries. However, this patient count is presumably low, because there is only a very small community hospital and 2 small private clinics in our area. Additionally, some patients in our area tend to seek medical help for acute injuries in our emergency department before going to the private clinics. Then, the patients were included only if their chart history included the word “tennis.” Thus, some patients might have been missed in cases with poor history documentation. Furthermore, the outcome of minor and major injuries remains unknown for our cohort. Finally, return to play could not be evaluated; thus, it remains unknown if any of these injuries had an impact on the ability of posttraumatic tennis play and the player’s performance.
Conclusion
Typical acute injuries in recreational tennis players differ from acute injuries in elite and junior players, with an increased proportion of fractures. The main causes of acute tennis injuries in patients who presented to the emergency department were falls and twists, with 10% of injuries needing surgical treatment, mainly for fractures, meniscal tears, and Achilles tendon ruptures.
Appendix Table A1.
Injury Patterns According to Body Regiona
| Body Region and Injury Mechanism (No.) | Injury Type (No.) |
|---|---|
| Head (31) | |
| Fall (9) | Head/face contusion (5), concussion (1), wound (3) |
| Ball hit (7) | Eye contusion (4), laryngeal contusion (1), periorbital contusion with hematoma (1), fracture of the orbital wall (1) |
| Racquet hit (15) | Wound (6), head/face contusion (5), eye contusion (2), nasal fracture (2) |
| Spine (12) | |
| Fall (5) | Lower back contusion (5) |
| Twist (6) | Cervical (1), thoracal (1), thoracolumbar (1), lumbar spine strain (3) |
| Ball hit (1) | Cervical spine strain (1) |
| Thorax (8) | |
| Fall (5) | Thorax contusion (4), rib fracture 9-10 (1) |
| Twist (1) | Thoracal strain (1) |
| Run against a wall (1) | Rib fracture 11 (1) |
| Sudden pain after forehand (1) | Spontaneous pneumothorax (1) |
| Abdomen (1) | |
| Sudden sharp pain (1) | Inguinal hernia (1) |
| Shoulder (37) | |
| Fall (8) | Shoulder contusion (3), acromioclavicular dislocation–Rockwood 3 (1), humeral shaft fracture (1), humeral head dislocation fracture (1), supraspinatus tendon rupture (1), pulley and biceps lesion (1) |
| Sudden sharp pain (mainly serve and backhand) (28) | Shoulder strain (11), rotator cuff tear (9), biceps tendon rupture (4), biceps tendon strain (1), infraspinatus strain (1), SLAP lesion (2) |
| Sudden dislocation (1) | Shoulder dislocation (1) |
| Elbow (18) | |
| Fall (7) | Elbow contusion (2), elbow strain (2), coronoid process fracture (1), radial head fracture (1), radial neck fracture (1) |
| Sudden sharp pain (9) | Elbow strain (5), radial tendinous strain (3), ulnar tendinous strain (1) |
| Racquet hit (1) | Elbow contusion (1) |
| Unspecified (1) | Distal biceps tendon rupture (1) |
| Wrist/hand (86) | |
| Fall (47) | Wrist/hand contusion (4), wrist strain (3), ligamentous finger and thumb joint lesion (4), capsular PIP joint avulsion (2), PIP epiphysiolysis (3), PIP joint dislocation (4), PIP joint dislocation fracture (1), finger fracture (4), scaphoid fracture (7), distal radial fracture (11), antebrachial fracture (1), ECU tendon subluxation (1), triquetrum avulsion (2) |
| Twist with sudden sharp pain (25) | Wrist strain (8), finger and thumb strain (3), tendon strain (4), muscle strain (2), ECU tendon subluxation (1), ECU tendon displacement (1), TFCC lesion (4), palmar capsular MCP joint rupture (1), SL ligament lesion (1) |
| Ball hit (3) | Palmar capsular PIP joint rupture (2), extensor tendon avulsion zone 1 (1) |
| Ball catch (2) | MCP joint strain (1), extensor tendon avulsion zone 1 (1) |
| Racquet hit (2) | Hand contusion (2) |
| Hit vs wall/hand (4) | Hand/wrist contusion (3), subcapital MC 5 fracture (1) |
| Unspecified (3) | Finger fracture (1), palmar capsular PIP joint rupture (1), epiphysiolysis PIP joint (1) |
| Hip (5) | |
| Fall (3) | Hip contusion (1), hip strain (1), pertrochanteric fracture (1) |
| Twist (2) | Hip strain (2) |
| Knee (90) | |
| Fall (12) | Prepatellar hematobursa (1), knee contusion (4), knee strain (2), knee wound (2), medial and lateral meniscal tear (2 [1 each]), patellar dislocation (1) |
| Twist (50) | Knee strain (14), MCL tear grade 1 (2) and grade 2 (3), LCL tear (1), medial meniscal tear (18), lateral meniscal tear (4), ACL tear (6), popliteal tendon strain (1), patellar subluxation with lesion of the patellar ligament (1) |
| Stop (2) | Knee strain (1), patellar dislocation (1) |
| Jump (3) | Knee contusion (1), lateral tibial plateau fissure (1), lateral tibial plateau fissure with ACL tear and lateral meniscal tear (1) |
| Larger step (5) | Knee strain (2), patellar ligament strain (1), medial meniscal tear (1), ACL tear with medial meniscal tear (1) |
| Sudden pain (11) | Knee strain (3), medial meniscal tear (4), ACL tear (2), partial ACL tear with MCL tear and medial meniscal tear (1), popliteal tendon strain (1) |
| Sudden instability (1) | ACL tear (1) |
| Unspecified (6) | Knee strain (1), partial ACL tear (1), partial ACL tear with medial meniscal tear (2), medial tibial plateau stress fracture (1), patellar subluxation (1) |
| Ankle (111) | |
| Fall (3) | Achilles tendon rupture (1), bimalleolar ankle fracture (1), ankle strain (1), fracture of the posterior process of the talus and avulsion of the cuboid and calcaneus (1) |
| Twist (90) | Ankle sprain (51), Achilles tendon strain (1), ankle strain (33), lateral malleolar epiphysiolysis (1), ankle fracture–Weber B (1), ankle fracture–Weber A (1), Achilles tendon rupture (1), syndesmotic strain (1) |
| Sudden sharp pain (16) | Achilles tendon rupture (12), Achilles tendon strain (4) |
| Step on a ball (1) | Ankle strain (1) |
| Unspecified (1) | Ankle strain (1) |
| Foot (24) | |
| Twist (11) | Foot strain (9), epiphysiolysis MT 5 (1), basal MT 5 fracture (1) |
| Sudden sharp pain (4) | Plantar fascia lesion (3), peroneus longus strain (1) |
| Hit (6) | Foot/toe contusion (6) |
| Unspecified (3) | Foot strain (3) |
| Thigh (18) | |
| Fall (2) | Biceps muscle strain (1), femoral contusion with hematoma (1) |
| Twist (2) | Biceps tendon strain (1), gluteal muscle strain (1) |
| Sudden sharp pain (13) | Adductor muscle strain (2), hamstring muscle strain (11) |
| Slip (1) | Hamstring rupture (1) |
| Calf (26) | |
| Fall (1) | Contusion with hematoma (1) |
| Twist (7) | Calf muscle strain (7) |
| Sudden sharp pain (16) | Calf muscle strain (16) |
| Slip (1) | Calf muscle strain (1) |
| Hit (1) | Calf contusion (1) |
aACL, anterior cruciate ligament; ECU, extensor carpi ulnaris; LCL, lateral collateral ligament; MC, metacarpal; MCL, medial collateral ligament; MCP, metacarpophalangeal; MT, metatarsal; PIP, proximal interphalangeal joint; SL, scapholunate; SLAP, superior labral tear from anterior to posterior; TFCC, triangular fibrocartilage complex
Footnotes
Final revision submitted June 30, 2020; accepted July 9, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by Medical University Innsbruck.
References
- 1. Abrams GD, Renstrom PA, Safran MR. Epidemiology of musculoskeletal injury in the tennis player. Br J Sports Med. 2012;46(7):492–498. [DOI] [PubMed] [Google Scholar]
- 2. Arnason A, Andersen TE, Holme I, Engebretsen L, Bahr R. Prevention of hamstring strains in elite soccer: an intervention study. Scand J Med Sci Sports. 2008;18(1):40–48. [DOI] [PubMed] [Google Scholar]
- 3. Burger M, Dreyer D, Fisher RL, et al. The effectiveness of proprioceptive and neuromuscular training compared to bracing in reducing the recurrence rate of ankle sprains in athletes: a systematic review and meta-analysis. J Back Musculoskelet Rehabil. 2018;31(2):221–229. [DOI] [PubMed] [Google Scholar]
- 4. Chapelle L, Rommers N, Clarys P, D’Hondt E, Taeymans J. Upper extremity bone mineral content asymmetries in tennis players: a systematic review and meta-analysis. J Sports Sci. 2019;37(9):988–997. [DOI] [PubMed] [Google Scholar]
- 5. Dakic JG, Smith B, Gosling CM, Perraton LG. Musculoskeletal injury profiles in professional Women’s Tennis Association players. Br J Sports Med. 2018;52(11):723–729. [DOI] [PubMed] [Google Scholar]
- 6. Ernlund L, Vieira LA. Hamstring injuries: update article. Rev Bras Ortop. 2017;52(4):373–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fong DT, Ha SC, Mok KM, Chan CW, Chan KM. Kinematics analysis of ankle inversion ligamentous sprain injuries in sports: five cases from televised tennis competitions. Am J Sports Med. 2012;40(11):2627–2632. [DOI] [PubMed] [Google Scholar]
- 8. Fu MC, Ellenbecker TS, Renstrom PA, Windler GS, Dines DM. Epidemiology of injuries in tennis players. Curr Rev Musculoskelet Med. 2018;11(1):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gaw CE, Chounthirath T, Smith GA. Tennis-related injuries treated in United States emergency departments, 1990 to 2011. Clin J Sport Med. 2014;24(3):226–232. [DOI] [PubMed] [Google Scholar]
- 10. Gescheit DT, Cormack SJ, Duffield R, et al. Injury epidemiology of tennis players at the 2011-2016 Australian Open Grand Slam. Br J Sports Med. 2017;51(17):1289–1294. [DOI] [PubMed] [Google Scholar]
- 11. Green B, Pizzari T. Calf muscle strain injuries in sport: a systematic review of risk factors for injury. Br J Sports Med. 2017;51(16):1189–1194. [DOI] [PubMed] [Google Scholar]
- 12. Hess GW. Achilles tendon rupture: a review of etiology, population, anatomy, risk factors, and injury prevention. Foot Ankle Spec. 2010;3(1):29–32. [DOI] [PubMed] [Google Scholar]
- 13. Ho G, Tantigate D, Kirschenbaum J, Greisberg JK, Vosseller JT. Increasing age in Achilles rupture patients over time. Injury. 2017;48(7):1701–1709. [DOI] [PubMed] [Google Scholar]
- 14. Hupperets MD, Verhagen EA, van Mechelen W. Effect of unsupervised home based proprioceptive training on recurrences of ankle sprain: randomised controlled trial. BMJ. 2009;339:B2684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hutchinson MR, LaPrade RF, Burnett QM, 2nd, Moss R, Terpstra J. Injury surveillance at the USTA Boys’ Tennis Championships: a 6-yr study. Med Sci Sports Exerc. 1995;27(6):826–830. [PubMed] [Google Scholar]
- 16. Kerkhoffs GM, van den Bekerom M, Elders LA, et al. Diagnosis, treatment and prevention of ankle sprains: an evidence-based clinical guideline. Br J Sports Med. 2012;46(12):854–860. [DOI] [PubMed] [Google Scholar]
- 17. Kovacs M, Roetert P, Ellenbecker TS. Complete Conditioning for Tennis. Human Kinetics; 2016. [Google Scholar]
- 18. Krabbe B, Farkas R, Baumann W. Stress on the upper ankle joint in tennis-specific forms of movement [in German]. Sportverletz Sportschaden. 1992;6(2):50–57. [DOI] [PubMed] [Google Scholar]
- 19. Kuhne CA, Zettl RP, Nast-Kolb D. Injuries and frequency of complaints in competitive tennis and leisure sports [in German]. Sportverletz Sportschaden. 2004;18(2):85–89. [DOI] [PubMed] [Google Scholar]
- 20. Lee JWY, Mok KM, Chan HCK, Yung PSH, Chan KM. Eccentric hamstring strength deficit and poor hamstring-to-quadriceps ratio are risk factors for hamstring strain injury in football: a prospective study of 146 professional players. J Sci Med Sport. 2018;21(8):789–793. [DOI] [PubMed] [Google Scholar]
- 21. Lorimer AV, Hume PA. Achilles tendon injury risk factors associated with running. Sports Med. 2014;44(10):1459–1472. [DOI] [PubMed] [Google Scholar]
- 22. Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: a 10-year study. Knee. 2006;13(3):184–188. [DOI] [PubMed] [Google Scholar]
- 23. Maquirriain J, Baglione R. Epidemiology of tennis injuries: an eight-year review of Davis Cup retirements. Eur J Sport Sci. 2016;16(2):266–270. [DOI] [PubMed] [Google Scholar]
- 24. McCurdie I, Smith S, Bell PH, Batt ME. Tennis injury data from the Championships, Wimbledon, from 2003 to 2012. Br J Sports Med. 2017;51(7):607–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Okholm Kryger K, Dor F, Guillaume M, et al. Medical reasons behind player departures from male and female professional tennis competitions. Am J Sports Med. 2015;43(1):34–40. [DOI] [PubMed] [Google Scholar]
- 26. Padua E, D’Amico AG, Alashram A, et al. Effectiveness of warm-up routine on the ankle injuries prevention in young female basketball players: a randomized controlled trial. Medicina (Kaunas). 2019;55(10):690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pas H, Pluim BM, Kilic O, et al. Effectiveness of an e-health tennis-specific injury prevention programme: randomised controlled trial in adult recreational tennis players. Br J Sports Med. 2020;54(17):1036–1041. [DOI] [PubMed] [Google Scholar]
- 28. Pluim BM, Staal JB, Windler GE, Jayanthi N. Tennis injuries: occurrence, aetiology, and prevention. Br J Sports Med. 2006;40(5):415–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Prior M, Guerin M, Grimmer K. An evidence-based approach to hamstring strain injury: a systematic review of the literature. Sports Health. 2009;1(2):154–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Raikin SM, Garras DN, Krapchev PV. Achilles tendon injuries in a United States population. Foot Ankle Int. 2013;34(4):475–480. [DOI] [PubMed] [Google Scholar]
- 31. Rivera MJ, Winkelmann ZK, Powden CJ, Games KE. Proprioceptive training for the prevention of ankle sprains: an evidence-based review. J Athl Train. 2017;52(11):1065–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Roetert P, Kovacs M. Tennis Anatomy. Human Kinetics; 2020. [Google Scholar]
- 33. Sell K, Hainline B, Yorio M, Kovacs M. Injury trend analysis from the US Open Tennis Championships between 1994 and 2009. Br J Sports Med. 2014;48(7):546–551. [DOI] [PubMed] [Google Scholar]
- 34. Timpka T, Alonso JM, Jacobsson J, et al. Injury and illness definitions and data collection procedures for use in epidemiological studies in athletics (track and field): consensus statement. Br J Sports Med. 2014;48(7):483–490. [DOI] [PubMed] [Google Scholar]
- 35. Vuurberg G, Hoorntje A, Wink LM, et al. Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline. Br J Sports Med. 2018;52(15):956. [DOI] [PubMed] [Google Scholar]


