Abstract
The latest ‘Controversies in…’ series for the Frontline Gastroenterology Twitter debates addressed the challenges of managing patients with portal hypertension, facilitated by Hepatologist and Liver Transplant physician Dr David Patch from the Royal Free London. Key topics discussed include basic principles of managing a patient with variceal bleeding, techniques for treating oesophageal and ectopic varices, pitfalls of vasoactive therapy, indications for transjugular intrahepatic portosystemic shunt, and a brief discussion of portal vein thrombosis. This article aims to summarise key areas of discussion from the event.
Keywords: portal hypertension, oesophageal varices, gastrointestinal bleeding, venous thrombosis
Introduction
The latest in the series of ‘Controversies in…’ Twitter debates for Frontline Gastroenterology was led by Dr David Patch (@DavidPatch1) in a discussion about portal hypertension. This article summarises the key topics discussed, including treatment of variceal bleeding, indications for transjugular intrahepatic portosystemic shunt (TIPSS) and management of portal vein thrombosis.
Variceal bleeding
Varices are portosystemic anastomoses that enlarge due to portal hypertension and should be suspected in patients with cirrhosis. These can commonly occur as oesophageal varices, or less frequently anywhere along the gastrointestinal tract (gastric, small bowel, colonic, rectal) or other ectopic sites (umbilicus, stoma). Mortality rates of variceal bleeding have historically reached 30%–50%, but have fallen to 11%–20% in more recent studies.1 These deaths are often due to progressive hepatic decompensation as a consequence.
Basic principles
Dr Patch was asked about his approach to variceal bleeding during the middle of the night (see box 1).
Box 1. Basic principles for managing a variceal bleeder.
All endoscopists on the bleeder rota should know how to manage variceal bleeding.
Antibiotics will reduce mortality in these patients.
Avoid overtransfusion in these patients as this can exacerbate bleeding (aim for 7–8 g/dL).
Ensure patients are adequately resuscitated prior to starting vasoactive therapy to minimise adverse effects such as myocardial, mesenteric and limb ischaemia.
It is essential that patients who are suspected to have active variceal bleeding are intubated prior to endoscopy. Aspiration pneumonia is associated with significant morbidity and mortality.
Band ligation is the treatment of choice for bleeding oesophageal varices, whereas gastric varices may require glue injection.
When banding oesophageal varices, it is recommended to band just above the gastro-oesophageal junction, generally only one or two per varix. This addresses the common error of placing too many bands, including in the proximal oesophagus.
Balloon tamponade with a Sengstaken-Blakemore tube is an effective temporising measure for variceal bleeding refractory to endoscopic therapy. Only the gastric balloon should be inflated (not the oesophageal balloon) and held in place using gentle traction. This strategy allows time to plan for a relook endoscopy during daylight hours or work-up/transfer for definitive treatment such as TIPSS or variceal embolisation.
During the discussion, other options such as Hemospray and SX-Ella Danis stents (Ella-CS) have been identified for difficult-to-treat variceal bleeding. These strategies are a bridge to definitive treatment.
Vasoactive agents for variceal bleeding
UK guidelines recommend starting vasoactive therapy for suspected variceal bleeders. What is the evidence for using one agent over another?
In one recent Korean study, a lack of difference in mortality rates was observed between terlipressin versus somatostatin versus octreotide in three equal arms of approximately 260 patients.2 More patients who received terlipressin had side effects (11.9%) compared with octreotide (3.8%) or somatostatin (4.2%). #FGDebate participants recalled terlipressin-related side effects including limb ischaemia, decompensated congestive cardiac failure, myocardial infarction and severe hyponatraemia.
Dr Patch recommends that before considering starting vasoactive therapy, it is important to ensure patients are adequately fluid-resuscitated, have had a history taken to exclude heart disease, mesenteric ischaemia or peripheral vascular disease, and an ECG performed.
Gastric varices
What about gastric varices? Feedback from trainees is that generally they have limited experience in treating these because they present so infrequently. Based on the Sarin classification, gastric varices may be gastro-oesophageal varices (GOV1, GOV2) or isolated gastric varices (IGV1, IGV2).
GOV1 varices are a continuation of oesophageal varices, involve the lesser curvature and may be banded. For other types of gastric varices, Dr Patch recommends treatment with cyanoacrylate glue injection. Calling an experienced endoscopist for advice or assistance can be helpful, and there are videos on YouTube demonstrating techniques for glue injection. Note that the glue will expand in size on contact with blood, and injecting no more than 1–2 mL of glue or less will help minimise risk of downstream embolisation.3 Flushing the injection catheter with dextrose will stop the glue from blocking the catheter.
Interestingly, a randomised control trial found that primary prophylaxis of glue injection in large gastric varices (GOV2, IGV1) of ≥10 mm reduced bleeding rates compared with beta blocker therapy, which was in turn superior to no treatment.4
Rectal variceal bleeding
It can be difficult to distinguish between rectal varices and haemorrhoids during flexible sigmoidoscopy. Anorectal varices may appear as blue-tinted, serpentine, submucosal varicose veins which start from near the anus, cross the dentate line and can extend into the rectum.5 One key difference is that anorectal varices are compressible and refill immediately on release, unlike haemorrhoids.
During an acute rectal variceal bleed, Dr Patch recommends that glue injection be considered if unable to perform TIPSS±radiological embolisation. Glue injection should be limited to 1–2 mL to avoid ulceration.
Other suggestions for variceal bleeding
For primary prophylaxis of oesophageal varices, patients do not need repeat endoscopy if they are optimised with beta blocker therapy.
There is limited evidence to stop anticoagulation prior to prophylactic banding, and a recent retrospective study suggests that it may even be safe to prophylactically band patients who are receiving low-molecular-weight heparin (LMWH).6
Cirrhosis in pregnancy: the best time to perform endoscopy to screen for oesophageal varices is during the second trimester as this represents the largest increase in portal pressure.7
Follow-up banding of oesophageal varices can be considered after a minimum interval of 4 weeks to allow healing of banding ulcers.
Transjugular intrahepatic portosystemic shunt
TIPSS is an interventional radiological procedure that creates a shunt between the portal and systemic circulation in order to treat portal hypertension. It is commonly used for indications such as refractory variceal bleeding, refractory ascites and portal vein thrombosis.
Adequate work-up for TIPSS is important. An increase in venous return will increase preload, so patients with pre-existing cardiac dysfunction are at risk of exacerbating congestive cardiac failure.8 It is also important to look for either overt or covert hepatic encephalopathy on electroencephalogram in these patients.
Common issues identified during the #FGDebate include when patients are identified as requiring an urgent TIPSS but may need to wait until a bed becomes available in a tertiary TIPSS centre before they can be transferred to perform the procedure.
Early TIPSS
There is still ongoing debate on the role of early TIPSS in variceal bleeders. One study reported that early TIPSS in patients who are Child-Pugh B with active bleeding on endoscopy and Child-Pugh C (with a score of 10–13) significantly reduced treatment failure and mortality rates.9 Unusually, this occurred without a statistically significant increase in hepatic encephalopathy in the TIPSS group. A recent publication from China identified a survival benefit,10 but a Scottish randomised controlled trial did not.11 As these findings are controversial, more studies are required to convincingly demonstrate a survival benefit of early TIPSS. It was recognised during the Twitter debate discussion that fundamental changes to service delivery would be required to make this a reliable option.
Portal vein thrombosis
Management of portal vein thrombosis can be difficult.
A thrombophilia screen should be performed, but precipitants can also include cirrhosis or inflammatory states such as pancreatitis or sepsis.
Acute portal vein thromboses should be therapeutically anticoagulated. For chronic portal vein thrombosis with cavernous transformation, there is still value in anticoagulation when an underlying thrombophilic state is present to prevent clot extension. The consequences of this could potentially be catastrophic, including gut ischaemia and infarction, death, or alternatively long-term development of portal hypertension.
Commonly, warfarin and LMWH are used for therapeutic anticoagulation. Advantages of using warfarin include being able to aim for a higher International Normalised Ratio (INR) in difficult cases. LMWH levels can be easily titrated by measuring anti-factor Xa activity. There is also some evidence on the use of direct oral anticoagulants in portal vein thrombosis; however, concerns include altered metabolism in decompensated cirrhotics, which could cause underanticoagulation or overanticoagulation as well as relatively difficult drug level monitoring.12
Thrombolysis for portal vein thrombosis
Low-dose thrombolysis with or without TIPSS is a novel treatment for extensive portal mesenteric thrombosis, especially in the setting of threatened gut ischaemia. This may allow resolution of the portomesenteric thrombus13 or improve flow sufficiently to allow for a successful TIPSS insertion.
Key take home messages
Twitter debate screenshot (figure 1).
Figure 1.
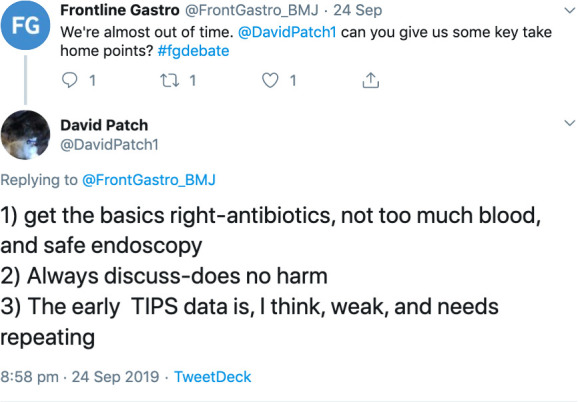
Take home messages.
Footnotes
Twitter: @jamesbmaurice
Contributors: WC, JM and DP wrote the manuscript and approved the final version.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1. Vuachet D, Cervoni J-P, Vuitton L, et al. Improved survival of cirrhotic patients with variceal bleeding over the decade 2000-2010. Clin Res Hepatol Gastroenterol 2015;39:59–67. 10.1016/j.clinre.2014.06.018 [DOI] [PubMed] [Google Scholar]
- 2. Cho S-H, Lee Y-S, Kim Y-J, et al. Outcomes and role of urgent endoscopy in high-risk patients with acute Nonvariceal gastrointestinal bleeding. Clin Gastroenterol Hepatol 2018;16:370–7. 10.1016/j.cgh.2017.06.029 [DOI] [PubMed] [Google Scholar]
- 3. Al-Hillawi L, Wong T, Tritto G, et al. Pitfalls in Histoacryl glue injection therapy for oesophageal, gastric and ectopic varices: a review. World J Gastrointest Surg 2016;8:729 10.4240/wjgs.v8.i11.729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mishra SR, Sharma BC, Kumar A, et al. Primary prophylaxis of gastric variceal bleeding comparing cyanoacrylate injection and beta-blockers: a randomized controlled trial. J Hepatol 2011;54:1161–7. 10.1016/j.jhep.2010.09.031 [DOI] [PubMed] [Google Scholar]
- 5. Robertson M, Thompson AI, Hayes PC. The management of bleeding from anorectal varices. Curr Hepatology Rep 2017;16:406–15. 10.1007/s11901-017-0382-6 [DOI] [Google Scholar]
- 6. Bianchini M, Cavani G, Bonaccorso A, et al. Low molecular weight heparin does not increase bleeding and mortality post-endoscopic variceal band ligation in cirrhotic patients. Liver Int 2018;38:1253–62. 10.1111/liv.13728 [DOI] [PubMed] [Google Scholar]
- 7. Allen AM, Hay JE. Review article: the management of cirrhosis in women. Aliment Pharmacol Ther 2014;40:1146–54. 10.1111/apt.12974 [DOI] [PubMed] [Google Scholar]
- 8. British Society Of Gastroenterology Transjugular intrahepatic portosystemic shunt (TIPSS) in the management of portal hypertension 2019.
- 9. García-Pagán JC, Caca K, Bureau C, et al. Early use of tips in patients with cirrhosis and variceal bleeding. N Engl J Med 2010;362:2370–9. 10.1056/NEJMoa0910102 [DOI] [PubMed] [Google Scholar]
- 10. Lv Y, Yang Z, Liu L, et al. Early tips with covered stents versus standard treatment for acute variceal bleeding in patients with advanced cirrhosis: a randomised controlled trial. Lancet Gastroenterol Hepatol 2019;4:587–98. 10.1016/S2468-1253(19)30090-1 [DOI] [PubMed] [Google Scholar]
- 11. Dunne P, Sinha R, Stanley A, et al. OTU-09 Use of early-TIPSS in patients with oesophageal variceal bleeding, a UK dual-centre randomised control trial. Gut 2019;68:A105 LP–6. [Google Scholar]
- 12. Priyanka P, Kupec JT, Krafft M, et al. Newer oral anticoagulants in the treatment of acute portal vein thrombosis in patients with and without cirrhosis. Int J Hepatol 2018;2018:1–9. 10.1155/2018/8432781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Benmassaoud A, AlRubaiy L, Yu D, et al. A stepwise thrombolysis regimen in the management of acute portal vein thrombosis in patients with evidence of intestinal ischaemia. Aliment Pharmacol Ther 2019;50:1049–58. 10.1111/apt.15479 [DOI] [PubMed] [Google Scholar]


