Abstract
With most global healthcare resources focused on COVID-19, altered resource allocation is disrupting the continuum of care for chronic endocrine conditions, including acromegaly. In order to assess the effects of COVID-19 on care of patients with acromegaly, we conducted an international online survey of endocrinologists. The questionnaire was drafted by a Steering Committee of acromegaly experts and covered both respondent demographics, contact and communication with patients, and patient care. Respondent awareness was generated through social media campaigns and the survey completed online using Google forms. The majority of endocrinologists who responded (N = 84) were based in Europe (67.9%) and were female (58.3%). Slightly more than half of respondents worked in a specialized pituitary center (52.4%) and a large minority cared for more than 50 acromegaly patients (47.6%). Most respondents (85.7%) indicated surgery was their first-line treatment, with only 14.3% indicating medical therapy as a first-choice treatment option. One-third (33.3%) of respondents reported having delayed a planned surgery due to a lack of COVID-19 testing provision and 54.8% due to a lack of surgical provision; 19.1% indicated that a lack of personal protective equipment had reduced their ability to treat patients with acromegaly. Just 21.4% of respondents reported no negative effects from the pandemic on diagnostic practice patterns, and just 19.1% reported no negative effect on patient follow-up practices. Many respondents (55.9%) indicated that remote methods had improved their ability to communicate with their patients and 69.0% indicated that they would continue to use methods of consultation necessitated by the COVID-19 pandemic. Our data suggest the COVID-19 pandemic is substantially affecting the care of acromegaly. However, these results also suggest that endocrinologists are embracing aspects of the ‘new normal’ to create a novel continuum of care better suited to the presumed post-COVID-19 environment. The goal of these changes must be both to improve care while shielding patients from more severe involvement in concomitant acute illnesses such COVID-19.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the viral strain responsible for the COVID-19 pandemic, had spread to 216 countries, areas, or territories, with over 39 million confirmed cases and more than 1,100,000 deaths, as of Oct 17th 2020 [1]. As it escalates into a global pandemic that will likely end up costing between $8.1 and $15.8 trillion [2], COVID-19 presents healthcare systems around the world with an unprecedented challenge.
With most global healthcare resources focused on COVID-19, resource allocation could disrupt the continuum of care, with routine care of chronic conditions; including endocrine disorders being disproportionately affected [3]. Furthermore, endocrine treatment modifications as a consequence of COVID-19 infection, are required in a proactive manner, in order to avoid decompensation and eventual hospital admission [4–6].
A 2nd wave of COVID-19 has the potential to be on a par with the initial outbreak in many countries [7], highlighting the importance of even longer term management of chronic diseases in pandemic situations. Acromegaly is a rare chronic condition affecting between 2.8 and 13.7 people per 100,000 population that in most cases arises due to excess growth hormone secreted by a somatotroph pituitary adenoma [8]. However, the true prevalence of clinically significant pituitary tumors seems to be higher [9]. As a result of the non-specific nature of some of the presenting symptoms, and the frequently subtle progression of clinical features, diagnosis is often delayed [10–12]. Treatment typically requires a multidisciplinary team of health care professionals including endocrinologists, neurosurgeons, and specialized endocrine nurses [13, 14], and access to these professionals could potentially be severely limited under COVID-19 pandemic conditions [15, 16]. Hence, patients may face the prospect of even more prolonged delays in both diagnosis and implementation of effective treatment plans in many centers worldwide.
In order to assess the effects of COVID-19 in acromegaly, we conducted an international online survey. The objective of this survey was to document changes to acromegaly disease management approaches as perceived by endocrinologists under the conditions of the current COVID-19 pandemic.
Methods
Four surveys were conducted (patient, endocrinologist, neurosurgeon, specialist nurses); endocrinologist data are presented here, a summary of patient responses is also available in the Supplementary Materials (S1.0). Regrettably, only a small number of responses were received to the nurse and neurosurgeon surveys.
The data cut-off was 27 July, 2020. Questionnaires for the surveys were drafted by a Steering Committee of acromegaly experts, and conducted online using Google forms and covered both respondent demographics, contact and communication with patients, and patient care. Respondent awareness was generated through social media campaigns conducted using the usual channels (Facebook, Twitter, etc.).
The categorical data of the responses have been summarized by means of absolute and percent frequencies. Data were analyzed using SAS®, Version 9.2.
Full patient and endocrinologist surveys are available in the Supplementary Materials (S2.0). Relationships between survey questions and data points are indicated in brackets (Q1, Q2, etc.) within the results section.
Results
Respondent demographics
Endocrinologist demographics are shown in Table 1 (Q1–3). The majority of respondents were based in Europe (67.9%) and identified as female (58.3%). Slightly more than half of respondents worked in a specialized pituitary center (52.4%) and a large minority cared for more than 50 acromegaly patients (47.6%).
Table 1.
Respondent demographics
| Endocrinologist respondents, n (%) (N = 84) | |
|---|---|
| Region | |
| Europe | 57 (67.9) |
| North America | 7 (8.3) |
| South America | 16 (19.1) |
| Asia | 4 (4.8) |
| Australia/Oceania | 0 |
| Africa | 0 |
| Female | 49 (58.3) |
| Male | 35 (41.7) |
| Practice type | |
| General endocrinology | 40 (47.6) |
| Pituitary center | 44 (52.4) |
| Number of patients with acromegaly under ongoing care | |
| 1–20 | 27 (32.1) |
| 21–50 | 17 (20.2) |
| 51–100 | 20 (23.8) |
| ≥100 | 20 (23.8) |
NA not applicable
How is COVID-19 changing the approach to disease management?
As expected, the majority of respondents 85.7% indicated surgery as their first-line treatment, with only 14.3% indicating medical therapy as a first-choice treatment option (Q10). In terms of surgical treatment under COVID-19 pandemic conditions, 33.3% of respondents reported having delayed a planned surgery due to a lack of COVID-19 testing provision, and 54.8% due to a lack of surgical provision (Q15); 16 respondents (19.1%) indicated that a lack of personal protective equipment had reduced their ability to treat patients with acromegaly, and 35.7% reported experiencing a delay or cancellation in treatment for a patient lacking biochemical control of their condition (Q14, Q11).
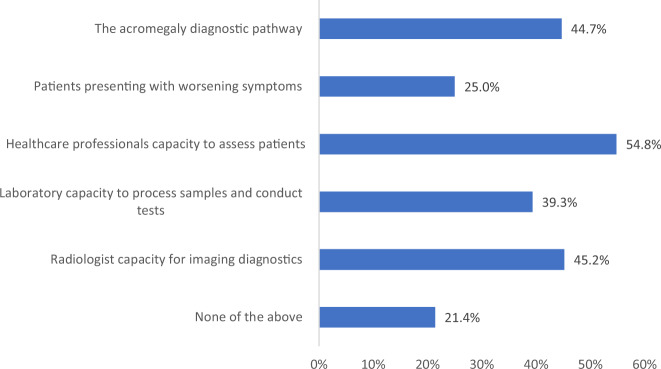
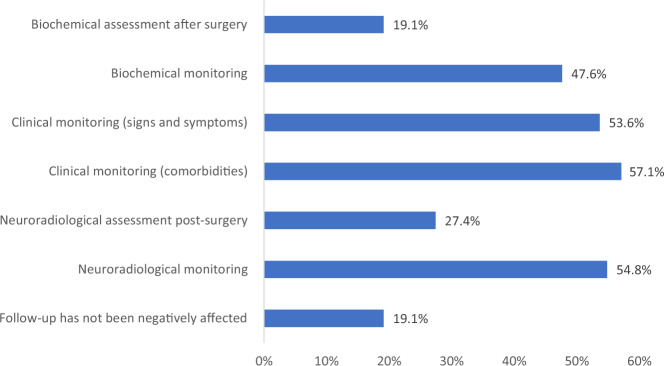
Just 21.4% of respondents reported no negative effects from the pandemic on diagnostic practice patterns (Fig. 1, Q8), and just 19.1% reported no negative effect on patient follow-up practices as a result of COVID-19 pandemic conditions (Fig. 2, Q9).
Fig. 1.
Aspects of patient management most affected by the COVID-19 pandemic. Data indicate percentage of respondents reporting a negative effect in each specific area of patient management (N = 84)
Fig. 2.
Aspects of patient follow-up most affected by the COVID-19 pandemic. Data indicate percentage of respondents reporting a negative effect in each specific area of patient management (N = 84)
Patient-perceived risk and the role of the patient in ongoing treatment
In terms of patient-perceived risk, 76.2% of endocrinologists indicated that patients had approached them regarding being at an increased risk from COVID-19: 41.7% of respondents reported that their patients had actively sought their advice regarding management of their acromegaly under COVID-19 pandemic conditions, and 59.5% reported that patients had sought help regarding their medical therapy (Q7). Just 10.7%, 14.3%, and 16.7% of respondents had proactively approached their patients regarding general health measures, acromegaly management, and medical therapy, respectively (Q7).
Though generally administered in the hospital setting, 42 respondents (50%) indicated that they believed that the role self/partner-administered somatostatin analogues (SSA) was of increased importance under pandemic conditions, with 33.5% of respondents recommending a switch to self/partner-administered SSA in patients lacking biochemical control (Q13, Q12). Just 9.5% of respondents recommended delaying monthly SSA treatment to avoid possible patient exposure to COVID-19 (Q12).
How have COVID-19 pandemic conditions affected endocrinologist–patient communication?
When queried as to whether they believed that the COVID-19 pandemic had negatively affected their ability to maintain a relationship with their patients, around half of respondents (47.6%) agreed or strongly agreed that it had, with 53.6% reporting reduced contact, 4.8% only allowing urgent visits, and one respondent (1.2%) reporting suspending services entirely (Q5, Q6).
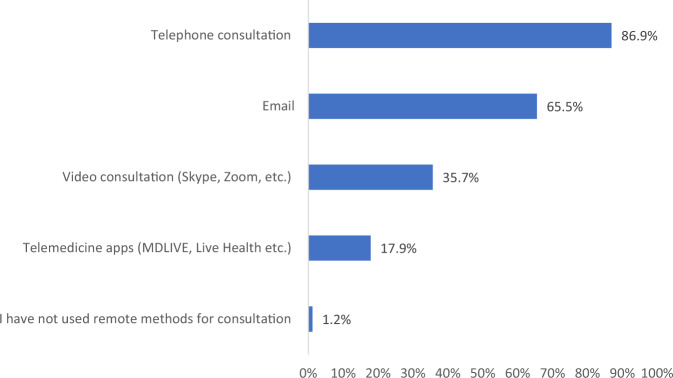
Despite this, many respondents experienced a degree of success with remote patient management, with the highest proportion of those surveyed (55.9%) indicating that remote methods had improved their ability to communicate with their patients (Fig. 3, Q16).
Fig. 3.
Proportion of endocrinologists agreeing with the below statement: Remote consultation has improved my ability to communicate with patients living with acromegaly during the COVID-19 pandemic. N = 84. Data indicate percentage of respondents reporting a negative effect in each specific area of patient care. Note that each respondent is able to indicate more than one affected area (N = 186)
How are endocrinologists communicating with their patients under COVID-19 pandemic conditions?
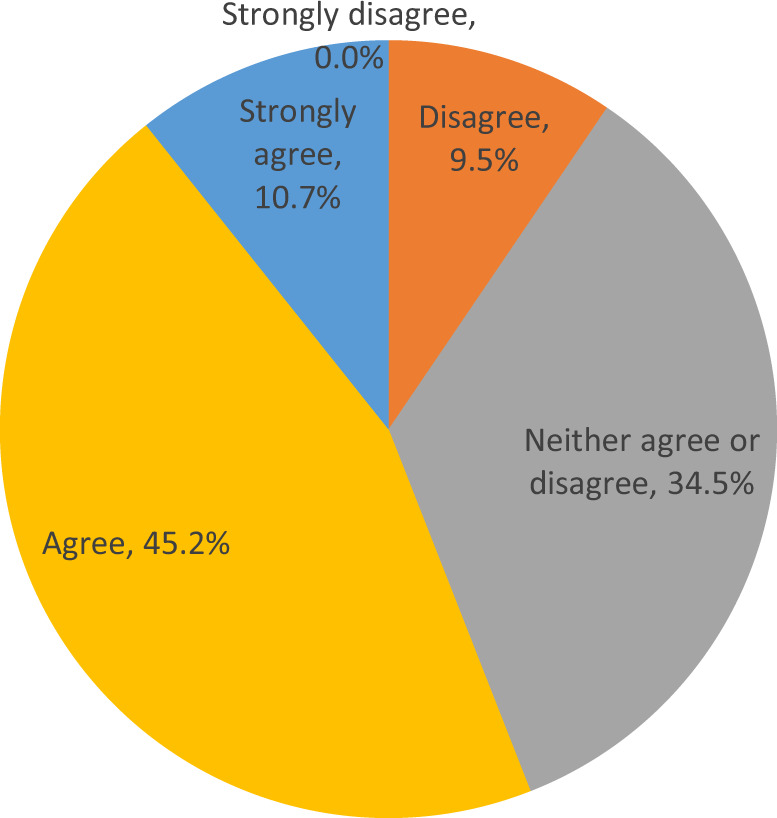
Telephone and email are currently the most commonly employed means of communication with patients in ongoing care, used by 86.9% and 65.5% of respondents, respectively (Fig. 4, Q17). Remote consultations were most commonly used to conduct post-diagnosis discussion of the condition and treatment options (76.2% of respondents) and adverse events related to treatment (64.3% of respondents; Q18). Remote consultations were employed to a lesser extent for diagnostic consultations (44.1% of respondents), discussion of alternative treatment pathways (36.9% of respondents), and for training of the patient or a family member on SSA or growth hormone antagonist (33.3% of respondents; Q18). In addition, 42.9% of respondents assessed the urgency of a treatment change in patients lacking biomedical control using remote methods (Q11).
Fig. 4.
Most commonly used remote methods for patient communication. Data indicate percentage of respondents reporting having used each communication method under COVID-19 pandemic conditions. Note that each respondent is able to indicate more than one method (N = 84)
With regards to continuity of care, 69.0% of respondents indicated that they would continue to use methods of consultation necessitated by the COVID-19 pandemic in the presumed post-COVID-19 environment, with 53.6% indicating that the role of specialized endocrine nurse was of increased importance under current conditions (Q20, Q19).
The ‘new normal’ for endocrinologists
As COVID-19 definitively changes the clinical approach to the treatment of acromegaly, many endocrinologists are embracing the ‘new normal’. In responses to a final open survey question (Q21), respondents reported virtual visits as a driver of improvements in patient care as they reduce the burden of hospital visits. Endocrinologists were interested in the possibility of integrating these innovative options for patient communication with novel methods of delivering therapies, such as self/partner-administration, that were previously only available in the hospital setting. However, concerns persist regarding delays to surgical and radio-therapeutic treatments and the availability of inpatient services. A series of representative responses to the survey’s open questions can be found in the Supplementary Materials (S3.0).
Discussion
Acromegaly is a chronic disease which, if not adequately controlled, heavily impacts on quality of life and survival due to its many systemic comorbidities [10, 13, 17]. However, the well-known clinical challenges in the management of the disease, i.e., persistent lengthy diagnostic delays [18], which lead to a high prevalence of macroadenomas at presentation with the need for strict control of pituitary tumor growth [19] and the frequent need for multimodal treatment in Pituitary Tumors Centers of Excellence (PTCOE) [20–22] are likely to be heavily affected by systemic rearrangements and ongoing crises in healthcare during the COVID-19 pandemic.
Moreover, several comorbidities in patients with acromegaly (e.g., hypopituitarism, diabetes mellitus, hypertension, obesity, cardiorespiratory diseases and fractures) [17, 23, 24] may negatively influence the course and management of COVID-19 [4, 5, 25] and must be appropriately managed to avoid increased predisposition to viral infection and complications. However, as acromegaly, alongside other syndromes caused by pituitary tumors, is relatively rare [8, 9] there is a lack of real-world data available concerning its management during the COVID-19 era, and physicians must rely on expert opinion [15, 16].
Therefore, we thought it relevant to survey the international endocrine community in order to investigate the impact of the pandemic on the care of acromegaly. This allowed us to better understand the challenges faced, the solutions adopted to tackle them, and the lessons learned for future practice although the results of these surveys may provide a limited ‘snapshot’ of a dynamic situation, which varies both geographically and temporally.
In general, our endocrinologist respondents – most of whom were treating high numbers of patients with acromegaly – reported broad negative effects from the COVID-19 pandemic on the acromegaly care pathway. Interestingly, although the vast majority used surgery as their first treatment option for the disease, as suggested in guidelines [26] and reported in previous surveys [27], most of the respondents reported substantial delays in surgical interventions due to hospital service reorganization with a lack of surgical provision and limited access to pre-surgery COVID-19 testing. In this light, it is reassuring to note that care was continued in the vast majority of cases. Furthermore, SSA are able to control tumor growth, and induce tumor shrinkage, in most patients with acromegaly [28, 29] and can be a valid option when surgery is delayed [13]. This consideration is increasingly important currently given many endocrinologists reported major difficulties in the neuroradiological follow-up of their patients.
Another challenge that emerged from the survey was the difficulty in monitoring biochemical control of acromegaly, which at present still represents the milestone for evaluating the efficacy of treatment [30, 31]. Poor monitoring can significantly affect adequate management of acromegaly by postponing SSA dose escalation [32, 33] or switching to another SSA [34] or alternative treatment, like pegvisomant [35]. Importantly, while SSAs have only marginal effects on glucose metabolism [36], even when used at high doses [37], use of pasireotide may impair glucose homeostasis and, conversely, pegvisomant may improve it [38]. The potential impact of these glucoactive effects should not be overlooked in the context of COVID-19, which, in addition to the poor prognosis related to existing impaired metabolism, can induce severe complications related to glucose metabolism such as ketoacidosis [39]. Finally, a third key challenge related to acromegaly medical treatment reported in the survey is its mode of administration. In fact, use of self-administered SSAs without the need for house visits from health professionals or even hospital visits for injection were demonstrated to be of increased importance during the pandemic and, likely, also for future clinical management [40, 41]. In this context, the possibility of orally administered SSAs [42–44] may have important clinical implications for simplified management of well-controlled disease in emergency situations, such as the COVID-19 pandemic.
It is a common experience in PTCOE that patients with acromegaly often consult their endocrinologists for health problems, which are not necessarily tightly linked to their underlying disease. Moreover, more than half of surveyed endocrinologists reported difficulties in the clinical monitoring of signs and symptoms related to both acromegaly and to its comorbidities, which have become progressively more important for adequate follow-up of the disease [45]. In this light, it is worth noting that remote communication principally via phone, but also with dedicated software, was seen as a positive tool by the majority of endocrinologists surveyed. In fact, two-thirds planned to continue to utilize these methods of communication in the post-COVID-19 era.
For all the above-mentioned reasons it is important that routine care continues in spite of the pandemic in order to avoid a rise in non-COVID-19-related morbidity and mortality due to chronic conditions such as acromegaly. While the body of scientific literature concerning COVID-19 is growing, the real-world impact of the COVID-19 pandemic has not yet been fully established, and, as such, any conclusions as to its long-term effect on the management of rare diseases such as acromegaly is not yet completely clear.
Nevertheless, our survey represents an important step forward into a better understanding of how endocrinologists expert in acromegaly care reacted to the emergency caused by the pandemic and how this may, temporarily or permanently, change their approach to their affected patients. The results of this survey suggest that the COVID-19 pandemic conditions are providing an opportunity to embrace aspects of the ‘new normal’ to create a new continuum of care better suited to the presumed post-COVID-19 environment. This new landscape will include elements of both pre-COVID practices (face-to-face consultation, access to specialists, regular laboratory assessment, surgical treatment) and new approaches (such as remote consultations that reduce the burden of hospital visits, self/partner-administration of therapies, treatment algorithms), with the ultimate goal of providing the best ongoing care for patients with acromegaly. The ultimate goal of these changes must be to not only continue to improve patient quality of life and prognosis but also provide protection from their increased vulnerability to concomitant acute illnesses such as COVID-19. In this regard, several open issues will need to be solved before these changes can be routinely incorporated into endocrine practice. These include reimbursements for remote consultations, which are not recognized by most health care providers in the same way as in-person patient visits, as well as possible legal concerns due to potential data breaches if unsafe electronic media are employed.
Supplementary information
Acknowledgements
This project was developed by COR2ED, funded by an independent medical educational grant from Ipsen. Editorial and writing support at first draft stage was provided by Daniel Guns on behalf of COR2ED. Iain Murdoch of COR2ED supported the development of the survey.
Compliance with ethical standards
Conflict of interest
A.G. Grants/scientific consultancy with Abiogen, Astellas, Chiasma, Genevant, Ipsen, Novartis, Novo, Pfizer, Recordati and research grants from Ipsen, Novartis and Pfizer, M.F. Grants as PI to OHSU: Chiasma, Crinetics, Ionis, Novartis, Pfizer and scientific consultant to Ipsen, Chiasma, Crinetics, Ionis, Novartis, Pfizer, Recordati, S.F., speaker fee from Ipsen, scientific consultant fee from Novartis. B.M.C., E.L. and P.M. - none to declare.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
5/4/2021
A Correction to this paper has been published: 10.1007/s12020-021-02720-2
Supplementary information
The online version of this article (10.1007/s12020-020-02565-1) contains supplementary material, which is available to authorized users.
References
- 1.https://covid19.who.int/.
- 2.https://www.weforum.org/agenda/2020/08/pandemic-fight-costs-500x-more-than-preventing-one-futurity/?emailType=Newsletter.
- 3.Chudasama YV, Gillies CL, Zaccardi F, Coles B, Davies MJ, Seidu S, Khunti K. Impact of COVID-19 on routine care for chronic diseases: a global survey of views from healthcare professionals. Diabetes Metab. Syndr. 2020;14(5):965–967. doi: 10.1016/j.dsx.2020.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marazuela M, Giustina A, Puig-Domingo M. Endocrine and metabolic aspects of the COVID-19 pandemic. Rev. Endocr. Metab. Disord. 2020;21(4):495–507. doi: 10.1007/s11154-020-09569-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Puig-Domingo M, Marazuela M, Giustina A. COVID-19 and endocrine diseases. A statement from the European Society of Endocrinology. Endocrine. 2020;68(1):2–5. doi: 10.1007/s12020-020-02294-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bilezikian JP, Bikle D, Hewison M, Lazaretti-Castro M, Formenti AM, Gupta A, Madhavan MV, Nair N, Babalyan V, Hutchings N, Napoli N, Accili D, Binkley N, Landry DW, Giustina A. MECHANISMS IN ENDOCRINOLOGY: Vitamin D and COVID-19. Eur. J. Endocrinol. 2020;183(5):R133–R147. doi: 10.1530/EJE-20-0665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Middleton, J., Lopes, H., Michelson, K., Reid, J. Planning for a second wave pandemic of COVID-19 and planning for winter: a statement from the Association of Schools of Public Health in the European Region. Int. J. Public Health (2020). 10.1007/s00038-020-01455-7 [DOI] [PMC free article] [PubMed]
- 8.Melmed S. Pituitary-tumor endocrinopathies. N. Engl. J. Med. 2020;382(10):937–950. doi: 10.1056/NEJMra1810772. [DOI] [PubMed] [Google Scholar]
- 9.Colao A, Grasso LFS, Giustina A, Melmed S, Chanson P, Pereira AM, Pivonello R. Acromegaly. Nat. Rev. Dis. Primers. 2019;5(1):20. doi: 10.1038/s41572-019-0071-6. [DOI] [PubMed] [Google Scholar]
- 10.Gadelha MR, Kasuki L, Lim DST, Fleseriu M. Systemic complications of acromegaly and the impact of the current treatment landscape: an update. Endocr. Rev. 2019;40(1):268–332. doi: 10.1210/er.2018-00115. [DOI] [PubMed] [Google Scholar]
- 11.Esposito D, Ragnarsson O, Johannsson G, Olsson DS. Prolonged diagnostic delay in acromegaly is associated with increased morbidity and mortality. Eur. J. Endocrinol. 2020;182(6):523–531. doi: 10.1530/EJE-20-0019. [DOI] [PubMed] [Google Scholar]
- 12.Giustina A. Acromegaly: reducing diagnostic delay. Recenti. Prog. Med. 2016;107(8):450–451. doi: 10.1701/2332.25074. [DOI] [PubMed] [Google Scholar]
- 13.Giustina A, Barkhoudarian G, Beckers A, Ben-Shlomo A, Biermasz N, Biller B, Boguszewski C, Bolanowski M, Bollerslev J, Bonert V, Bronstein MD, Buchfelder M, Casanueva F, Chanson P, Clemmons D, Fleseriu M, Formenti AM, Freda P, Gadelha M, Geer E, Gurnell M, Heaney AP, Ho KKY, Ioachimescu AG, Lamberts S, Laws E, Losa M, Maffei P, Mamelak A, Mercado M, Molitch M, Mortini P, Pereira AM, Petersenn S, Post K, Puig-Domingo M, Salvatori R, Samson SL, Shimon I, Strasburger C, Swearingen B, Trainer P, Vance ML, Wass J, Wierman ME, Yuen KCJ, Zatelli MC, Melmed S. Multidisciplinary management of acromegaly: a consensus. Rev. Endocr. Metab. Disord. 2020;21(4):667–678. doi: 10.1007/s11154-020-09588-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frara S, Maffezzoni F, Mazziotti G, Giustina A. The modern criteria for medical management of acromegaly. Prog. Mol. Biol. Transl. Sci. 2016;138:63–83. doi: 10.1016/bs.pmbts.2015.10.015. [DOI] [PubMed] [Google Scholar]
- 15.Fleseriu M, Buchfelder M, Cetas JS, Fazeli PK, Mallea-Gil SM, Gurnell M, McCormack A, Pineyro MM, Syro LV, Tritos NA, Marcus HJ. Pituitary society guidance: pituitary disease management and patient care recommendations during the COVID-19 pandemic-an international perspective. Pituitary. 2020;23(4):327–337. doi: 10.1007/s11102-020-01059-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fleseriu M, Dekkers OM, Karavitaki N. Endocrinology in the time of COVID-19: management of pituitary tumours. Eur. J. Endocrinol. 2020;183(1):G17–G23. doi: 10.1530/EJE-20-0473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giustina, A., Barkan, A., Beckers, A., Biermasz, N., Biller, B. M. K., Boguszewski, C., Bolanowski, M., Bonert, V., Bronstein, M. D., Casanueva, F. F., Clemmons, D., Colao, A., Ferone, D., Fleseriu, M., Frara, S., Gadelha, M. R., Ghigo, E., Gurnell, M., Heaney, A. P., Ho, K., Ioachimescu, A., Katznelson, L., Kelestimur, F., Kopchick, J., Krsek, M., Lamberts, S., Losa, M., Luger, A., Maffei, P., Marazuela, M., Mazziotti, G., Mercado, M., Mortini, P., Neggers, S., Pereira, A. M., Petersenn, S., Puig-Domingo, M., Salvatori, R., Shimon, I., Strasburger, C., Tsagarakis, S., van der Lely, A. J., Wass, J., Zatelli, M. C., Melmed, S. A consensus on the diagnosis and treatment of acromegaly comorbidities: an update. J. Clin. Endocrinol. Metab. 105(4), (2020). 10.1210/clinem/dgz096 [DOI] [PubMed]
- 18.Melmed S, Bronstein MD, Chanson P, Klibanski A, Casanueva FF, Wass JAH, Strasburger CJ, Luger A, Clemmons DR, Giustina A, Consensus A. Statement on acromegaly therapeutic outcomes. Nat. Rev. Endocrinol. 2018;14(9):552–561. doi: 10.1038/s41574-018-0058-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gola M, Bonadonna S, Mazziotti G, Amato G, Giustina A. Resistance to somatostatin analogs in acromegaly: an evolving concept? J. Endocrinol. Invest. 2006;29(1):86–93. doi: 10.1007/BF03349183. [DOI] [PubMed] [Google Scholar]
- 20.Casanueva FF, Barkan AL, Buchfelder M, Klibanski A, Laws ER, Loeffler JS, Melmed S, Mortini P, Wass J, Giustina A, Pituitary Society, Expert Group on Pituitary Tumors Criteria for the definition of Pituitary Tumor Centers of Excellence (PTCOE): A Pituitary Society Statement. Pituitary. 2017;20(5):489–498. doi: 10.1007/s11102-017-0838-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Frara S, Rodriguez-Carnero G, Formenti AM, Martinez-Olmos MA, Giustina A, Casanueva FF. Pituitary tumors centers of excellence. Endocrinol. Metab. Clin. North Am. 2020;49(3):553–564. doi: 10.1016/j.ecl.2020.05.010. [DOI] [PubMed] [Google Scholar]
- 22.Mortini P, Nocera G, Roncelli F, Losa M, Formenti AM, Giustina A. The optimal numerosity of the referral population of pituitary tumors centers of excellence (PTCOE): a surgical perspective. Rev. Endocr. Metab. Disord. 2020;21(4):527–536. doi: 10.1007/s11154-020-09564-7. [DOI] [PubMed] [Google Scholar]
- 23.Davi MV, Dalle Carbonare L, Giustina A, Ferrari M, Frigo A, Lo Cascio V, Francia G. Sleep apnoea syndrome is highly prevalent in acromegaly and only partially reversible after biochemical control of the disease. Eur. J. Endocrinol. 2008;159(5):533–540. doi: 10.1530/EJE-08-0442. [DOI] [PubMed] [Google Scholar]
- 24.Giustina A. Acromegaly and vertebral fractures: facts and questions. Trends Endocrinol. Metab. 2020;31(4):274–275. doi: 10.1016/j.tem.2020.01.011. [DOI] [PubMed] [Google Scholar]
- 25.L. Di Filippo, A.M. Formenti, M. Doga, E. Pedone, P. Rovere-Querini, A. Giustina, Radiological thoracic vertebral fractures are highly prevalent in COVID-19 and predict disease outcomes. J. Clin. Endocrinol. Metab. dgaa738 (2020). 10.1210/clinem/dgaa738. [Epub ahead of print]. PMID: 33159451 [DOI] [PMC free article] [PubMed]
- 26.Giustina A, Chanson P, Kleinberg D, Bronstein MD, Clemmons DR, Klibanski A, van der Lely AJ, Strasburger CJ, Lamberts SW, Ho KK, Casanueva FF, Melmed S, Acromegaly Consensus G. Expert consensus document: a consensus on the medical treatment of acromegaly. Nat. Rev. Endocrinol. 2014;10(4):243–248. doi: 10.1038/nrendo.2014.21. [DOI] [PubMed] [Google Scholar]
- 27.Giustina A, Bronstein MD, Casanueva FF, Chanson P, Ghigo E, Ho KK, Klibanski A, Lamberts S, Trainer P, Melmed S. Current management practices for acromegaly: an international survey. Pituitary. 2011;14(2):125–133. doi: 10.1007/s11102-010-0269-9. [DOI] [PubMed] [Google Scholar]
- 28.Mazziotti G, Giustina A. Effects of lanreotide SR and Autogel on tumor mass in patients with acromegaly: a systematic review. Pituitary. 2010;13(1):60–67. doi: 10.1007/s11102-009-0169-z. [DOI] [PubMed] [Google Scholar]
- 29.Giustina A, Mazziotti G, Torri V, Spinello M, Floriani I, Melmed S. Meta-analysis on the effects of octreotide on tumor mass in acromegaly. PLoS One. 2012;7(5):e36411. doi: 10.1371/journal.pone.0036411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Giustina A, Barkan A, Casanueva FF, Cavagnini F, Frohman L, Ho K, Veldhuis J, Wass J, Von Werder K, Melmed S. Criteria for cure of acromegaly: a consensus statement. J. Clin. Endocrinol. Metab. 2000;85(2):526–529. doi: 10.1210/jcem.85.2.6363. [DOI] [PubMed] [Google Scholar]
- 31.Giustina A, Chanson P, Bronstein MD, Klibanski A, Lamberts S, Casanueva FF, Trainer P, Ghigo E, Ho K, Melmed S, Acromegaly Consensus G. A consensus on criteria for cure of acromegaly. J. Clin. Endocrinol. Metab. 2010;95(7):3141–3148. doi: 10.1210/jc.2009-2670. [DOI] [PubMed] [Google Scholar]
- 32.Giustina A, Bonadonna S, Bugari G, Colao A, Cozzi R, Cannavo S, de Marinis L, Degli Uberti E, Bogazzi F, Mazziotti G, Minuto F, Montini M, Ghigo E. High-dose intramuscular octreotide in patients with acromegaly inadequately controlled on conventional somatostatin analogue therapy: a randomised controlled trial. Eur. J. Endocrinol. 2009;161(2):331–338. doi: 10.1530/EJE-09-0372. [DOI] [PubMed] [Google Scholar]
- 33.Giustina A, Mazziotti G, Cannavo S, Castello R, Arnaldi G, Bugari G, Cozzi R, Ferone D, Formenti AM, Gatti E, Grottoli S, Maffei P, Maffezzoni F, Montini M, Terzolo M, Ghigo E. High-dose and high-frequency lanreotide autogel in acromegaly: a randomized, multicenter study. J. Clin. Endocrinol. Metab. 2017;102(7):2454–2464. doi: 10.1210/jc.2017-00142. [DOI] [PubMed] [Google Scholar]
- 34.Gadelha MR, Bronstein MD, Brue T, Coculescu M, Fleseriu M, Guitelman M, Pronin V, Raverot G, Shimon I, Lievre KK, Fleck J, Aout M, Pedroncelli AM, Colao A, Pasireotide CSG. Pasireotide versus continued treatment with octreotide or lanreotide in patients with inadequately controlled acromegaly (PAOLA): a randomised, phase 3 trial. Lancet Diabetes Endocrinol. 2014;2(11):875–884. doi: 10.1016/S2213-8587(14)70169-X. [DOI] [PubMed] [Google Scholar]
- 35.Giustina A, Arnaldi G, Bogazzi F, Cannavo S, Colao A, De Marinis L, De Menis E, Degli Uberti E, Giorgino F, Grottoli S, Lania AG, Maffei P, Pivonello R, Ghigo E. Pegvisomant in acromegaly: an update. J. Endocrinol. Invest. 2017;40(6):577–589. doi: 10.1007/s40618-017-0614-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mazziotti G, Floriani I, Bonadonna S, Torri V, Chanson P, Giustina A. Effects of somatostatin analogs on glucose homeostasis: a metaanalysis of acromegaly studies. J. Clin. Endocrinol. Metab. 2009;94(5):1500–1508. doi: 10.1210/jc.2008-2332. [DOI] [PubMed] [Google Scholar]
- 37.Mazziotti G, Porcelli T, Bogazzi F, Bugari G, Cannavo S, Colao A, Cozzi R, De Marinis L, degli Uberti E, Grottoli S, Minuto F, Montini M, Spinello M, Giustina A. Effects of high-dose octreotide LAR on glucose metabolism in patients with acromegaly inadequately controlled by conventional somatostatin analog therapy. Eur. J. Endocrinol. 2011;164(3):341–347. doi: 10.1530/EJE-10-0811. [DOI] [PubMed] [Google Scholar]
- 38.Frara S, Maffezzoni F, Mazziotti G, Giustina A. Current and emerging aspects of diabetes mellitus in acromegaly. Trends Endocrinol. Metab. 2016;27(7):470–483. doi: 10.1016/j.tem.2016.04.014. [DOI] [PubMed] [Google Scholar]
- 39.Smith, S. M., Boppana, A., Traupman, J. A., Unson, E., Maddock, D. A., Chao, K., Dobesh, D. P., Brufsky, A., Connor, R. I. Impaired glucose metabolism in patients with diabetes, prediabetes, and obesity is associated with severe COVID-19. J. Med. Virol. (2020). 10.1002/jmv.26227 [DOI] [PMC free article] [PubMed]
- 40.Salvatori R, Nachtigall LB, Cook DM, Bonert V, Molitch ME, Blethen S, Chang S, Group SS. Effectiveness of self- or partner-administration of an extended-release aqueous-gel formulation of lanreotide in lanreotide-naive patients with acromegaly. Pituitary. 2010;13(2):115–122. doi: 10.1007/s11102-009-0207-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Salvatori R, Woodmansee WW, Molitch M, Gordon MB, Lomax KG. Lanreotide extended-release aqueous-gel formulation, injected by patient, partner or healthcare provider in patients with acromegaly in the United States: 1-year data from the SODA registry. Pituitary. 2014;17(1):13–21. doi: 10.1007/s11102-012-0460-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Melmed S, Popovic V, Bidlingmaier M, Mercado M, van der Lely AJ, Biermasz N, Bolanowski M, Coculescu M, Schopohl J, Racz K, Glaser B, Goth M, Greenman Y, Trainer P, Mezosi E, Shimon I, Giustina A, Korbonits M, Bronstein MD, Kleinberg D, Teichman S, Gliko-Kabir I, Mamluk R, Haviv A, Strasburger C. Safety and efficacy of oral octreotide in acromegaly: results of a multicenter phase III trial. J. Clin. Endocrinol. Metab. 2015;100(4):1699–1708. doi: 10.1210/jc.2014-4113. [DOI] [PubMed] [Google Scholar]
- 43.Samson, S. L., Nachtigall, L. B., Fleseriu, M., Gordon, M. B., Bolanowski, M., Labadzhyan, A., Ur, E., Molitch, M., Ludlam, W. H., Patou, G., Haviv, A., Biermasz, N., Giustina, A., Trainer, P. J., Strasburger, C. J., Kennedy, L., Melmed, S. Maintenance of acromegaly control in patients switching from injectable somatostatin receptor ligands to oral octreotide. J. Clin. Endocrinol. Metab. 105(10) (2020). 10.1210/clinem/dgaa526 [DOI] [PMC free article] [PubMed]
- 44.Maffezzoni F, Frara S, Doga M, Mazziotti G, Giustina A. New medical therapies of acromegaly. Growth Horm. IGF Res. 2016;30-31:58–63. doi: 10.1016/j.ghir.2016.10.001. [DOI] [PubMed] [Google Scholar]
- 45.Giustina A, Bronstein MD, Chanson P, Petersenn S, Casanueva FF, Sert C, Houchard A, Melmed S. Staging and managing patients with acromegaly in clinical practice: baseline data from the SAGIT(R) validation study. Pituitary. 2019;22(5):476–487. doi: 10.1007/s11102-019-00977-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.