Abstract
Background:
Active TB case finding (ACF) is a key strategy employed by the National Tuberculosis and Leprosy Control Programme (NTBLCP) to address the increasing gap in TB case finding in Nigeria. KNCV TB foundation Nigeria rolled out two high-impact ACF interventions; TB Surge and the Wellness on Wheels (WoW) campaigns from January 2020.
Method:
The TB Surge intervention supports the engagement of ad hoc staff for TB ACF. The WoW campaign employs a mobile diagnostic unit to deliver care to the doorstep of people at risk of TB. Data along the TB cascade are recorded for all clients using the CommCare app. Cochran-Armitage χ2 test for linear trend was used to assess the significance declining trends along the TB cascade.
Results:
There was a progressive decrease of respectively 63%, 64%, 73% and 72% in clinic attendance, presumptive TB identification, TB cases detected and treatment initiation for the TB Surge ACF intervention since the emergence of coronavirus; a similar decrease was noted for the WoW intervention. Trend analysis showed a significant decline in trends for both interventions for all variables (P < 0.001)
Conclusion:
The COVID-19 epidemic has impacted negatively on TB services in Nigeria. The TB programme could leverage some resources used to combat the epidemic such as digital health technology and funds, and work towards strengthening patient-centred approach to care to limit the challenges that COVID-19 presents to TB control.
Keywords: TB surge, Wellness on Wheels, TB cascade, ad hoc staff
Abstract
Contexte :
La recherche active de cas de TB (ACF) est une stratégie clé du Programme National de lutte contre la Tuberculose et la Lèpre (NTBLCP) visant à résoudre les lacunes croissantes de l’identification des cas de TB au Nigeria. La fondation KNCV TB du Nigeria a déployé deux interventions d’ACF à impact élevé; les campagnes, TB Surge et Wellness on Wheels (WoW) à partir de janvier 2020.
Méthode :
L’intervention TB Surge soutient l’engagement de personnel ponctuel pour l’ACF de TB. Le camion de WoW comprend une unité mobile de diagnostic disponible au domicile des personnes à risque de TB. Les données tout au long de la cascade TB sont enregistrées pour tous les clients sur l’application CommCare. Le test du χ2 Cochran-Armitage pour la tendance linéaire a été utilisé pour évaluer la signification de la tendance déclinante le long de la cascade TB.
Résultats :
Il y a eu une diminution progressive de 63% dans la fréquentation des structures de santé, 64% dans l’identification des TB présumées, 73% des cas de TB détectés et 72% dans l’initiation du traitement pour l’intervention TB Surge ACF et une diminution similaire a été notée pour l’intervention WoW. L’analyse de tendance a montré un déclin significatif de la tendance pour les deux interventions pour toutes les variables (P < 0,001).
Conclusion :
L’épidémie de COVID-19 a eu un impact négatif sur les services de TB au Nigeria. Le programme TB pourrait profiter de quelques opportunités présentées par l’épidémie comme la technique numérique en santé et les ressources financières, et enfin travailler à un renforcement de l’approche de soins centrée sur le patient afin de limiter les défis que la COVID-19 pose la lutte contre la TB.
Abstract
Marco de referencia:
La búsqueda activa de casos (ACF) de TB es una estrategia fundamental del Programa Nacional de Control de la Tuberculosis y la Lepra (NTBLCP), encaminada a responder a la deficiencia cada vez mayor de la búsqueda de casos de TB en Nigeria. La fundación KNCV para la TB desplegó dos intervenciones de ACF de gran impacto, a saber: las campañas TB Surge y Wellness on Wheels (WoW) a partir de enero del 2020.
Método:
La intervención TB Surge respalda la participación de personal dedicado a la ACF de TB. El camión WoW, con una unidad diagnóstica móvil, llega hasta la puerta de las personas con riesgo de contraer la TB. Se recogieron datos de todos los usuarios en la continuidad asistencial de la TB, mediante la aplicación CommCare. Se utilizó la prueba de la χ2 de Cochran-Armitage para tendencias lineales, con el fin de evaluar la significación de la evolución decreciente a lo largo del proceso continuo de atención de la TB.
Resultados:
Se observó una disminución progresiva de 63% en la asistencia a los consultorios, 64% en el reconocimiento de la presunción de TB, 73% en la detección de casos de TB y 72% en el comienzo del tratamiento con la intervención TB Surge de ACF y la reducción fue equivalente con la intervención WoW. El análisis de las tendencias reveló una regresión significativa en la evolución de ambas intervenciones para todas las variables (P < 0,001).
Conclusión:
La epidemia de COVID-19 ha tenido una repercusión negativa en los servicios de TB en Nigeria. El programa de TB podría aprovechar algunas oportunidades que presenta la epidemia como las soluciones digitales de salud, los recursos de financiamiento y los trabajos encaminados a fortalecer el enfoque de atención centrada en el paciente, con el propósito de limitar los retos que plantea la COVID-19 al control de la TB.
Respiratory tract infections (RTIs) are of public health significance and regarded as the greatest cause of morbidity and mortality from infectious diseases worldwide, especially TB.1,2 Both COVID-19 and TB belong to this group, having a similar presentation and a high burden of disease. However, this new pandemic has impacted on other health issues, including TB. COVID-19 was first reported in China, declared a pandemic by the WHO on 11 March 2020.1 The first case in Nigeria was detected on 27 February 2020.3 The relationship between COVID-19 and TB is most pronounced in sub-Saharan Africa, where TB is the leading infectious disease cause of death.
The poorest, underserved and marginalised people who suffer most from TB are also most likely to be affected by the COVID-19 pandemic.4 It has been documented that people with TB, TB-HIV coinfection or chronic lung disease are more likely to develop long-term effects of the pandemic.5 This calls for more dedication and need for pulmonary rehabilitation for TB patients.6 About 4 million people die from lower respiratory tract infections each year, approximately 10.0 million people fell ill with TB and an estimated 1.4 million died of TB in 2018.2 Although global commitment have been made to end the TB epidemic by 2030 through actionable targets,7 the pace of progress in most regions and countries is insufficient. Prior to the onset of the COVID-19 pandemic, the quality of TB care services in Africa was suboptimal. The advent of the COVID-19 pandemic has led to major socio-economic impacts, disrupted routine health services and affected the progress towards the UN Sustainable Development Goals (SDGs), rendering prior significant issues less important.
There are predictions of a global decrease in TB case detection by an average of 25% over a period of 3 months (compared to the level of detection before the pandemic), which will lead to an estimated additional 190 000 (range 56 000–406,000) TB deaths (a 13% increase), bringing the total number of TB deaths to 1.66 million (1.3–2.1) in 2020, near the global level of TB mortality for 2015.8,9 The International Monetary Fund also postulated that COVID-19 is expected to result in a global economic recession in 2020, with the economic downturn being particularly worse for emerging markets and low-income countries,10 where poor government funding has limited needed support for TB programme implementation.
One of the cardinal objectives of the WHO’s End TB Strategy,7 which proposes ending the TB epidemic within the next 15 years, is the provision of high quality and patient-centred care for TB patients based on human rights. Interventions used to control the COVID-19 epidemic, including physical and social distancing, regular hand washing, self-isolation at home, ban on public transport, lockdowns and others pose a challenge to TB care,11 especially among the poorest, who live in overcrowded conditions, have limited access to drinking water and limited income. A Stop TB Partnership report based on a modelling analysis documented that the global response to the COVID-19 pandemic is likely to have drastic detrimental consequences for TB services.12
The social and psychological impact of the pandemic has been compounded by rapid misinformation spread through both mainstream and social media. This misinformation has been reported to be of global scale, leading to the launch of the ‘Verified’ Initiative to combat the growing scourge of COVID-19 misinformation by increasing the volume and reach of trusted, accurate information.13 Even more alarming is the disruption caused to global health services. Access to TB services was interrupted because health care workers devoted their energies and resources to COVID-19 outbreak. Based on this, there is a significant risk that prevention and treatment programmes for the existing conditions will be negatively impacted.14 The fear of contracting COVID-19 discourages people in need of timely diagnosis and treatment for TB from accessing health services. Also, COVID-19 and TB share typical signs and symptoms, including fever, dry cough, fatigue, sputum production, shortness of breath, sore throat, headache, myalgia or arthralgia, chills, nausea or vomiting, nasal congestion and haemoptysis.14 Thus, at first clinical presentation, a wide range of differential diagnoses need to be considered, including TB; however, this is not the case as COVID-19 has supplanted every other disease at present, especially diseases with a similar presentation.13 Mistrust and misinformation may have led many patients with clinical features like those of COVID-19 being hesitant to voluntarily seek care in a formal health facility.
The WHO currently recommends that TB programmes embrace active TB case finding (ACF) strategies to complement passive case finding (PCF) and address the increasing gap in TB case finding, diagnose and treat patients earlier, reduce the period of infection and transmission of the disease and improve population-level TB control. Previous ACF interventions in Nigeria have demonstrated that this approach can increase case detection in high-risk groups.15 TB ACF may identify TB populations with different characteristics from those identified using PCF, and further studies suggest recommendations for future implementation of ACF interventions in Nigeria.16 To boost ACF intervention, the KNCV TB Foundation rolled out two high-impact TB ACF interventions: the TB Surge and Wellness on Wheel (WoW) campaigns. The present study is aimed to assess the impact of the COVID-19 pandemic on these two ACF interventions in Nigeria.
METHODS
The study examined the impact of the COVID-19 epidemic on two TB ACF interventions: the TB Surge intervention and the WoW campaign implemented by KNCV TB Foundation Nigeria. TB Surge was implemented across 61 high-volume facilities in nine Nigerian states (Lagos, Ogun, Akwa-Ibom, Cross River, Rivers, Nasarawa, Kano, Benue and Katsina). The WoW campaign was implemented in Kano State. The TB Surge intervention was conducted over 8 weeks in March and April 2020 and the WoW campaign was carried out for 4 weeks (March 2020).
The TB Surge intervention was health facility-based among Out-patient Department (OPD) attendees, while WoW was a community-based intervention. The TB Surge intervention supports the engagement of ad hoc staff for routine TB screening, presumptive TB identification, referral for diagnosis and linkage to DOTS. The WoW intervention used a mobile diagnostic unit (MDU), housing a digital X-ray machine and two four-module GeneXpert machines to deliver screening and diagnosis to the doorstep of the people at risk for TB. Data along the TB cascade were captured and recorded using the CommCare App. With the advent of the COVID-19 epidemic, staff were trained in infection prevention and control (IPC) and personal protective equipment, including N95 masks, supplied to them. The NTBLCP guidelines on TB care in the era of COVID-19 was adapted and used in training health care workers.
This was a cross-sectional study using de-identified programme data extracted from the CommCare app for these interventions for all age groups. A stepwise approach was used: clients were screened using a cough screening questionnaire to select those with presumptive TB. Presumptive TB cases were screened for active TB using Xpert® MTB/RIF (Cepheid, Sunnyvale, CA, USA) and/or acid-fast bacilli microscopy, following which, those that had TB were referred for treatment. Data along the TB cascade were recorded for all clients using the CommCare app and collated for analysis every week. Data were exported to Statistical Package for Social sciences v25 (IBM Corp, Armonk, NY, USA), where these were edited and analysed. Trend analysis was performed using Cochran-Armitage χ2 test for linear trends at a significant level of P < 0.05. Tables and charts were used in presenting the data.
Ethical considerations
The study was determined to be a non-research programme evaluation. As it required no direct contact with human subjects (no interview or sample collection) and only de-identified pooled programme data that formed part of standard of care were used, informed consent was not required.
RESULTS
A total of 190 734 persons were studied (188 825 OPD attendees and 1909 at their homes). Table 1 shows the TB activities of OPD attendees over 8 weeks in March and April. Total OPD attendees decreased over 8 weeks from 37 351 (19.8%) to 13 883 (7.4%), presumptive TB from 2303 (18.7%) to 829 (6.7%), diagnosed TB cases from 178 (19.1%) to 48 (5.2%) and people placed on treatment from 148 (19.2%) to 41 (5.3%).
TABLE 1.
TB activities performed among OPD attendees over 8 weeks in March–April 2020
| Time period | OPD attendees screened n (%) | Presumptive TB cases identified n (%) | TB cases diagnosed n (%) | TB cases put on treatment n (%) | |
|---|---|---|---|---|---|
| Clients, n | 188,825 (100.0) | 12,305 (100.0) | 930 (100.0) | 770 (100.0) | |
| Week in March | |||||
| OPD | 08–14 | 37,351 (19.8) | 2,303 (18.7) | 178 (19.1) | 148 (19.2) |
| 15–21 | 35,683 (18.9) | 2,595 (21.1) | 193 (20.8) | 164 (21.3) | |
| 22–28 | 27,921 (14.8) | 1,782 (14.5) | 162 (17.4) | 141 (18.3) | |
| 29–04 | 21,636 (11.5) | 1,426 (11.6) | 104 (11.2) | 80 (10.4) | |
| Week in April | |||||
| OPD | 05–11 | 18,192 (9.6) | 1,262 (10.3) | 91 (9.8) | 82 (10.7) |
| 12–18 | 16,460 (8.7) | 992 (8.1) | 82 (8.8) | 70 (9.1) | |
| 19–25 | 17,699 (9.4) | 1,116 (9.1) | 72 (7.7) | 44 (5.7) | |
| 26–02 | 13,883 (7.4) | 829 (6.7) | 48 (5.2) | 41 (5.3) | |
| Decrease over 8 weeks, %* | 63.0 | 64.0 | 73.0 | 72.0 |
* (Value at last week - value at Week 8)/value at last week; denominator is the number of clients.
OPD = outpatient department.
Table 2 shows WoW-related TB activities over 4 weeks in March. The number of clients provided with services decreased from 681 (35.7%) to 226 (11.8%), the number of presumptive TB cases from 98 (30.7%) to 11 (3.5%), the number of diagnosed TB cases from 23 (33.3%) to 3 (4.4%) and the number of people placed on treatment from 19 (35.2%) to 2 (3.7%) over 4 weeks.
TABLE 2.
WoW programme activities over 4 weeks in March–April 2020
| Week in March/April | Persons screened n (%) | Presumptive TB cases identified n (%) | TB cases diagnosed n (%) | TB cases put on treatment n (%) | |
|---|---|---|---|---|---|
| Clients, n | 1909 (100.0) | 319 (100.0) | 69 (100.0) | 54 (100.0) | |
| WoW intervention | 08–14 | 681 (35.7) | 98 (30.7) | 23 (33.3) | 19 (35.2) |
| 15–21 | 496 (26.0) | 132 (41.4) | 25 (36.2) | 21 (38.9) | |
| 22–28 | 506 (36.4) | 78 (24.5) | 18 (26.1 | 12 (22.2) | |
| 29–04 | 226 (11.8) | 11 (3.5) | 3 (4.4) | 2 (3.7) | |
| Decrease over 4 weeks, %* | 67.0 | 89.0 | 87.0 | 89.0 |
* (Value at last week - value at Week 8)/value at last week; denominator is the number of clients.
WoW = Wellness on Wheels.
Figure 1 shows a progressive decrease of 63% in clinic attendance (37 351 to 13 883), of 64% in the number of presumptive TB cases (2303 to 829), of 73% in TB cases detection (178 to 48) and of 72% in treatment initiation (148 to 41) over 8 weeks according to TB Surge data. However, there was a spike in screening at about Week 20–21 (in April).
FIGURE 1.
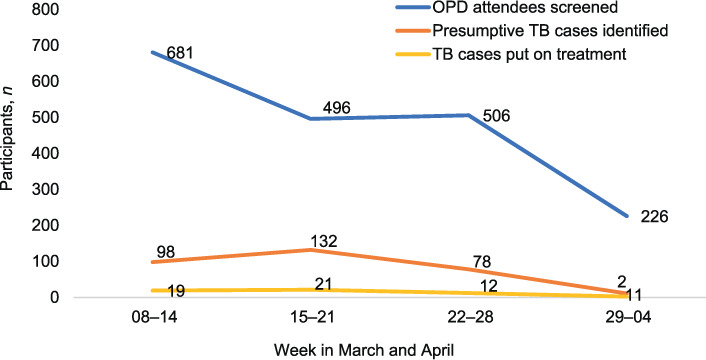
The TB Surge intervention: 8-week trends in the number of OPD attendees screened, presumptive TB cases and TB cases on treatment. OPD = outpatient department.
Figure 2 shows a progressive decrease of 67% in clinic attendance (681 to 226), 89% in the number of presumptive TB cases (98 to 11), 87% in the number of TB cases detected (23 to 3) and 89% in treatment initiation (19 to 2) over 4 weeks according to WoW data. There was no visible change between Weeks 15 and 21 in the number of clients screened.
FIGURE 2.
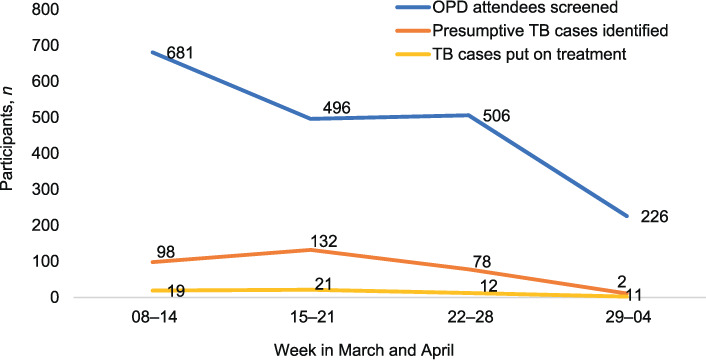
The WoW intervention: 4-week (March) trends in the number of clients screened, presumptive TB cases, TB cases diagnosed and TB cases placed on treatment. OPD = outpatient department; WoW = Wellness on Wheels.
It should be noted that our trend analysis (using Cochran-Ar-mitage test for linear trend) indicated a significant decrease in all variables. For TB Surge, these were as follows: screening (χ2 = 24578.04, P < 0.001), identification of presumptive TB cases (χ2 = 1813.06, P < 0.001), diagnosed TB cases (χ2 = 182.92, P < 0.001) and treatment initiation (χ2 = 172.00, P < 0.001). For WoW, screening (χ2 = 256.47, P = 0.005) presumptive TB identification (χ2 = 82.95, P < 0.001), diagnosed TB 173 (χ2 = 17.35, P < 0.001) and treatment (χ2 = 17.78, P < 0.001).
There was a very good correlation for screening (r = 0.89), as well as near perfect correlation in the identification of presumptive TB cases (r = 0.96), diagnosis of TB cases (r = 0.99) and treatment initiation (r = 0.96) between the TB Surge and WoW interventions.
DISCUSSION
Findings show a progressive decrease in clinic attendance, presumptive TB identification, number of TB cases detected and number who initiated treatment for the TB Surge and the WoW interventions since the onset of the COVID-19 pandemic. Trend analysis indicated a significant decrease for all variables. This is not surprising, and may have been a result of fear of the disease itself or the interventions used to combat the pandemic. Since the COVID-19 pandemic, most countries, including Nigeria, directed all attention, political will, and the limited human and financial resources from an already overburdened and weak health system to control the pandemic. Nigeria, which has the highest TB burden in Africa, and ranks among 30 high TB burden countries worldwide, has recently diverted some of the 300 GeneXpert machines in the country for COVID-19 use as part of its strategy to scale-up diagnosis.17 This will have a severe negative impact on TB control efforts by limiting access to these diagnostic platforms for TB services.
Equally some measures to control COVID-19, including physical and social distancing, self-isolation at home, ban on public transport, lockdowns, etc. pose challenges to TB diagnosis and treatment, especially among the poorest, who live in overcrowded conditions, have limited incomes and are more susceptible to TB.18 This was confirmed by a Stop TB Partnership modelling analysis report according to which the global response to the COVID-19 pandemic is likely to have drastic detrimental consequences for TB services.19 One of the immediate measures adopted by the Nigerian government in response to the COVID-19 pandemic was to institute a lockdown policy. Forcing people to stay at home will increase the risk of transmission of TB in such communities, leading to poor health outcomes.18 Restrictions on movement due to the pandemic among those with low economic status will further reduce their limited resources for transportation costs and indirect medical costs such as ancillary drugs.
Access to health services is a multi-dimensional concept that depends on the degree of fit between the patient and the health care system.20 All clients have a basic right of access to health services.21 Common access barriers to health services are distance to health facilities, transportation cost, non-availability of medicines and lack of trained personnel. Further barriers such as State policies which restrict movement and enforce staying at home, have now been created due to COVID-19. While these policies may lead to better control of the virus, they inadvertently prevent clients with other health needs from seeking care as we found in the decreased OPD attendance. Supply chain disruptions during COVID-19 could lead to unavailability of essential medicines, including anti-TB drugs. This will lead to decreased TB case finding, as TB cases in Nigeria are only counted when they are commenced on treatment at registration in the TB treatment register.
In addition, institutional mistrust, misinformation, stigma and fear of isolation have created barriers to seeking care. The COVID-19 response has often compromised rights-based approaches to health. Blame of acquiring, spreading TB and stigmatising those with cough discourage those with TB signs and symptoms from voluntarily seeking care. For example, a person with persistent cough which could be due to either TB or COVID-19 may be hesitant to seek health care, or when patients refuse to admit to symptoms of cough due to the fear and stigma associated with COVID-19, and possible confinement in isolation centres. This results in low presumptive yield, as found in this study. Although the WoW intervention provided doorstep screening services for community members, the decrease in the service uptake and consequent decrease in presumptive TB identification and TB case detection observed could be related to heightened stigma associated with cough symptoms, with fewer clients presenting for TB screening services.
Both patients and providers are fearful. Some facilities, especially those in Lagos State, were limited to emergency cases only due to COVID-19, while some others regulated the number of clients attended to daily. Arguably, these measures were intended to curtail the nosocomial spread of COVID-19; however, the unintended consequence was that clients with TB were not diagnosed and continued to transmit TB in their communities. Furthermore, health care workers are afraid to attend to patients with upper respiratory tract symptoms, although they have now been trained to distinguish between TB and COVID-19 symptoms. This affected screening coverage and the presumptive TB yield, which is in line with a study in South West Nigeria, which found that health care worker attitudes could present a barrier to accessing TB services.22
Most countries prioritised health funds to the COVID-19 pandemic, making domestic health resources, which was already insignificant in developing countries in most cases, was drastically reduced.23 This implies that innovative approaches to people-centric TB care as stipulated in Stop TB Strategy are required, so that the fight to end this pandemic does not overwrite the hard-won gains made against TB disease. Countries need to put in place strategies to ease pressure on health systems and to mitigate disruption in routine health services. This can partly be achieved by creating alternative options, including the use of digital health technology such as virtual care, digital health and community-monitoring solutions to bring the required services as close as possible to the people and communities affected by TB. In short, countries and agencies must overcome the challenges that COVID-19 presents and use the opportunities it created to achieve a paradigm shift in TB services.
Our study had some limitations. The data collection within the TB program is still manually based and some gaps and omissions could occur during data collection and transcription into the CommCare App. Also, the study focused only on the trend in the TB cascade and did not explore other confounders to the declining trend through a qualitative means.
CONCLUSION
The COVID-19 epidemic has impacted negatively on TB case finding in Nigeria. Findings from this study showed a progressive decline in clinic attendance, presumptive TB identification, TB cases detection and treatment initiation since the onset of the COVID-19. To address these challenges, the TB program needs to adapt urgently to the new normal and strengthen patient centred approach to TB care, embrace digital health technology, increase awareness creation, scale up community based active TB case finding and also ensure that other opportunities that the epidemic presents are maximally utilized to mitigate the impact on TB case finding.
ACKNOWLEDGEMENTS
The authors thank USAID Nigeria through Abt Associate for funding the WASP (Wellness on Wheels, Ad hoc staff, TB Surge and Programmatic management of Drug Resistant TB) Project implemented during this period by KNCV Tuberculosis Foundation Nigeria, Abuja, Nigeria; the State TB programmes and the NTBLCP for their collaboration and support in the WASP project implementation and the data reported that made this study possible.
Footnotes
Conflicts of interest: none declared.
References
- 1.World Health Organization Timeline of WHO’s response to COVID-19. Geneva, Switzerland: WHO; 2020. [Google Scholar]
- 2.World Health Organization Global tuberculosis report, 2019. WHO/CDS/TB/2019.15. Geneva, Switzerland: WHO; 2019. [Google Scholar]
- 3.Nigeria Centre for Disease Control First case of corona virus disease confirmed in Nigeria. Abuja, Nigeria: NCDC; 2020. https://ncdc.gov.ng/news/227/first-case-of-corona-virus-disease-confirmed-in-nigeria Accessed October, 2020. [Google Scholar]
- 4.Christoph Lakner, et al. Updated estimates of the impact of COVID-19 on global poverty: the effect of new data. Washington DC, USA: World Bank; 2020. https://blogs.worldbank.org/opendata/updated-estimates-impact-covid-19-global-poverty-effect-new-data Accessed October 2020. [Google Scholar]
- 5.Hsu Hsu D et al. Post TB treatment infectious complications. Int J Infect Dis. 2020;92(Suppl):S41–S45. doi: 10.1016/j.ijid.2020.02.032. [DOI] [PubMed] [Google Scholar]
- 6.Visca D, et al. Post-TB treatment pulmonary rehabilitation: do we need more? Int J Tuberc Lung Dis. 2020 [In press] [Google Scholar]
- 7.World Health Organization The End TB Strategy. Geneva, Switzerland: WHO; 2015. https://www.who.int/tb/strategy/end-tb/en/ Accessed July 2020. [Google Scholar]
- 8.Glaziou P. Predicted impact of the COVID-19 pandemic on global tuberculosis deaths in 2020. MedRxiv. 2020 doi: 10.1101/2020.04.28.20079582. [DOI] [Google Scholar]
- 9.Hore R. 2020. The devastating effect of the COVID-19 pandemic on the TB response-A minimum of 5 years of progress lost and 6 million additional people ill with TB. https://www.results.org.uk/blog/devastating-effect-covidpandemic-tb-response-minimum-5-years-progress-lost-and-6-million Accessed July 2020. [Google Scholar]
- 10.International Monetary Fund COVID’s Impact in real time: finding balance amid the crisis. Washington DC, USA: IMF; 2020. https://blogs.imf.org/2020/10/08/covids-impact-in-real-time-finding-balance-amid-the-crisis/ Accessed October 2020. [Google Scholar]
- 11.McQuaid CF, et al. The potential impact of COVID-19-related disruption on tuberculosis burden. Eur Respir J. 2020;56(2):2001718. doi: 10.1183/13993003.01718-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cilloni L, et al. The potential impact of the COVID-19 pandemic on tuberculosis a modelling analysis. Medrxiv. 2020;28:1. doi: 10.1016/j.eclinm.2020.100603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.United Nations UN launches new global initiative to combat misinformation | Africa Renewal. New York, NY, USA: UN; 2020. https://www.un.org/africarenewal/news/coronavirus/covid-19-united-nations-launchesglobal-initiative-combat-misinformation Accessed July 2020. [Google Scholar]
- 14.Zumla A, Niederman MS. Editorial: The explosive epidemic outbreak of novel coronavirus disease 2019 (COVID-19) and the persistent threat of respiratory tract infectious diseases to global health security. Curr Opin Pulm Med. 2020;26(3):193–196. doi: 10.1097/MCP.0000000000000676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oshi DC, et al. An evaluation of innovative community-based approaches and systematic tuberculosis screening to improve tuberculosis case detection in Ebonyi State, Nigeria. Int J Mycobacteriol. 2017;6:246–252. doi: 10.4103/ijmy.ijmy_91_17. [DOI] [PubMed] [Google Scholar]
- 16.Kusimo O, et al. A. Implementation of the active TB case finding in Nigeria; processes, lessons learnt and recommendations. J Tuberc Res. 2018;6:10–18. [Google Scholar]
- 17.Oladimeji O, Atiba BP, Adeyinka DA. Leveraging polymerase chain reaction technique (GeneXpert) to upscaling testing capacity for SARS-CoV-2 (COVID-19) in Nigeria: a game changer. Pan Afr Med J. 2020;35(Suppl 2):8. doi: 10.11604/pamj.2020.35.2.22693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Togun T, et al. Anticipating the impact of the COVID-19 pandemic on TB patients and TB control programmes. Ann Clin Microbiol Antimicrob. 2020;19(1):21. doi: 10.1186/s12941-020-00363-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stop TB Partnership Geneva, Switzerland: Stop TB Partnership; 2020. The potential impact of the COVID-19 response on tuberculosis in high-burden countries: a modelling analysis. http://www.stoptb.org/assets/documents/news/Modeling%20Report_1%20May%202020_FINAL.pdf Accessed September 2020. [Google Scholar]
- 20.World Health Organization Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. Geneva, Switzerland: WHO; 2010. [Google Scholar]
- 21.Marguari D, et al. Social barriers to accessing quality TB service: key population, legal environment and gender assessment. Jakarta, Indonesia: Spiritia Foundation; 2018. http://www.stoptb.org/assets/documents/communities.pdf Accessed July 2020. [Google Scholar]
- 22.Ribón W, editor. Patients and health system-related factors impacting on tuberculosis program implementation in resource-constrained settings: experience from multi-TB facilities in Oyo State, South-West of Nigeria. Mycobacterium: Research and Development. Chapter 9. London, UK: IntechOpen; 2018. (ed) [DOI] [Google Scholar]
- 23.World Health Organization Coronavirus disease 2019 (COVID-19): situation reports. Geneva, Switzerland: WHO; 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports Accessed July 2020. [Google Scholar]


