Dear editor,
The recent outbreak of coronavirus disease (COVID-19) has become a major public health issue caused by 2019 novel coronavirus (2019-nCoV).[1] Severe COVID-19 patients may reveal a dysregulated immune response that allows the development of viral hyperinflammation.[2] In the fight against COVID-19, inflammatory parameters towards illness severity should be identified to improve the prognosis of patients. In this study, we aimed to assess the discriminative ability of several inflammation indicators in severe COVID-19 infection.
We conducted a comprehensive search through electronic databases until May 26, 2020: PubMed, the Cochrane Library, EMBASE, and Web of Science. Keywords included COVID-19, nCoV-2019, 2019-nCoV, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and monocyte-to-lymphocyte ratio (MLR). To be included, studies must provide mean and standard deviation (SD) values or median and interquartile range or adjusted odds ratio (OR) with corresponding 95% confidence interval (CI). The pooled weighted mean difference (WMD) and pooled OR were worked out by STATA 12.0.
After the application of selection criteria, there were 13 studies[2-14] with 2,140 patients included that provided data describing NLR, PLR, and MLR on COVID-19 cases and in-hospital mortality. The meta-analysis for the continuous outcome variables included ten studies,[2-11] and for the binary variables included six studies.[5,8,10,12-14] There were two studies reporting clear data on in-hospital mortality.[12,14]
Overall, more severe COVID-19 infection was associated with higher NLR (WMD=3.55, 95% CI 2.47–4.64, P<0.001) and higher MLR (WMD=0.39, 95% CI 0.19–0.59, P<0.001). There was no significant difference in PLR (WMD=81.48, 95% CI –93.44 to 256.40, P=0.361) between the severe group and the non-severe group. For COVID-19 patients, NLR with the pooled OR value could predict the severe infection (OR=1.40, 95% CI 1.02–1.93, P=0.038) and in-hospital mortality (OR=1.08, 95% CI 1.02–1.15, P=0.009).
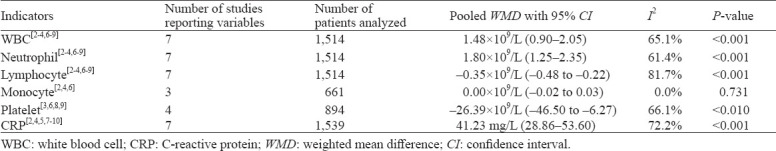
As for blood parameters in severe COVID-19, seven studies described counts of white blood cell (WBC), neutrophil, and lymphocyte in the non-severe and severe groups. Patients with severe COVID-19 had higher WBC counts (WMD=1.48×109/L, 95% CI 0.90–2.05, P<0.001), higher neutrophil counts (WMD=1.80×109/L, 95% CI 1.25–2.35, P<0.001), and fewer lymphocyte counts (WMD= –0.35×109/L, 95% CI –0.48 to –0.22, P <0.001) than those in the non-severe group. Four studies compared platelet counts between the two groups, and severe cases demonstrated lower platelet counts (WMD= –26.39×109/L, 95% CI –46.50 to –6.27, P<0.010) compared with the non-severe group. Three studies reported the monocyte counts. However, no statistical difference was found between the two groups (WMD=0.00×109/L, 95% CI –0.02 to 0.03, P=0.731). Seven studies depicted C-reactive protein (CRP) levels, and severe cases also had higher CRP levels (WMD=41.23 mg/L, 95% CI 28.86–53.60, P<0.001). The pooled WMD for blood parameters of the included studies are presented in Table 1.
Table 1.
Pooled outcomes of blood parameters in severe COVID-19
Meta-regression analysis showed that the increased NLR in severe COVID-19 patients was associated with WBC (P=0.007) and neutrophil (P=0.011) but not lymphocyte, CRP, age, or the study size of COVID-19. There was no evidence of publication bias according to the WMD of NLR. Sensitivity analysis showed no significant differences produced by excluding every single study.
In conclusion, during severe COVID-19 infection, NLR, MLR, WBC, neutrophil, and CRP were significantly increased, while lymphocyte and platelet were significantly decreased. Patients with a higher level of NLR experienced a higher risk of in-hospital mortality. The assessments of NLR and other inflammatory indicators may help physicians to identify severe patients with COVID-19 and predict the prognosis of this infection.
Footnotes
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: The authors have no conflict of interest to declare.
Contributors: GQY and QZ contributed equally to this work. GQY, QZ, RCW searched the database, collected the data and performed the meta-analysis. GQY and SQJ reviewed and revised the manuscript. All authors approved the final version.
REFERENCES
- 1.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y, et al. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin Infect Dis. 2020;71(15):762–8. doi: 10.1093/cid/ciaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ma J, Yin J, Qian Y, Wu Y. Clinical characteristics and prognosis in cancer patients with COVID-19:a single center's retrospective study. J Infect. 2020;81(2):318–56. doi: 10.1016/j.jinf.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang AP, Liu JP, Tao WQ, Li HM. The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. Int Immunopharmacol. 2020;84:106504. doi: 10.1016/j.intimp.2020.106504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang Y, Zheng L, Liu L, Zhao M, Xiao J, Zhao Q. Liver impairment in COVID-19 patients:a retrospective analysis of 115 cases from a single centre in Wuhan city, China. Liver Int. 2020;40(9):2095–103. doi: 10.1111/liv.14455. [DOI] [PubMed] [Google Scholar]
- 6.Sun S, Cai X, Wang H, He G, Lin Y, Lu B, et al. Abnormalities of peripheral blood system in patients with COVID-19 in Wenzhou, China. Clin Chim Acta. 2020;507:174–80. doi: 10.1016/j.cca.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fu J, Kong J, Wang W, Wu M, Yao L, Wang Z, et al. The clinical implication of dynamic neutrophil to lymphocyte ratio and D-dimer in COVID-19: a retrospective study in Suzhou China. Thromb Res. 2020;192:3–8. doi: 10.1016/j.thromres.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shang W, Dong J, Ren Y, Tian M, Li W, Hu J, et al. The value of clinical parameters in predicting the severity of COVID-19. J Med Virol. 2020;92(10):2188–92. doi: 10.1002/jmv.26031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luo X, Zhou W, Yan X, Guo T, Wang B, Xia H, et al. Prognostic value of C-reactive protein in patients with COVID-19. Clin Infect Dis. 2020 May 23;:ciaa641. doi: 10.1093/cid/ciaa641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xia X, Wen M, Zhan S, He J, Chen W. An increased neutrophil/lymphocyte ratio is an early warning signal of severe COVID-19. Nan Fang Yi Ke Da Xue Xue Bao. 2020;40(3):333–6. doi: 10.12122/j.issn.1673-4254.2020.03.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Qu R, Ling Y, Zhang YH, Wei LY, Chen X, Li XM, et al. Platelet-to-lymphocyte ratio is associated with prognosis in patients with coronavirus disease-19. J Med Virol. 2020;92(9):1533–41. doi: 10.1002/jmv.25767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu Y, Du X, Chen J, Jin Y, Peng L, Wang HHX, et al. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. J Infect. 2020;81(1):e6–e12. doi: 10.1016/j.jinf.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu J, Li S, Liu J, Liang B, Wang X, Wang H, et al. Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients. EBioMedicine. 2020;55:102763. doi: 10.1016/j.ebiom.2020.102763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen C, Zhang JY, Li C, Hu ZH, Zhang M, Tu P, et al. The characteristics and death risk factors of 132 COVID-19 pneumonia patients with comorbidities: a retrospective single center analysis in Wuhan, China. Diabetes Res Clin Pract. 2020;166:108299. doi: 10.1016/j.diabres.2020.108299. [DOI] [PMC free article] [PubMed] [Google Scholar]


