Abstract
BACKGROUND:
We aim to investigate effects of metabolic syndrome on onset age and long-term outcomes in patients with acute coronary syndrome (ACS).
METHODS:
Patients with ACS (n=6,431) who underwent percutaneous coronary intervention from January to December 2013 were enrolled. After excluding patients with previous coronary artery disease, 1,558 patients were diagnosed with early-onset ACS (men aged ≤50 years; women aged ≤60 years) and 3,044 patients with late-onset ACS. Baseline characteristics and five-year clinical outcomes were measured.
RESULTS:
Body mass index, triglyceride, low-density lipoprotein cholesterol, and uric acid concentrations were significantly higher, while the high-density lipoprotein cholesterol (HDL-C) concentration was lower in the early-onset ACS group (P<0.001). Multivariate logistic regression revealed obesity (odds ratio [OR] 1.590, 95% confidence interval [CI] 1.345–1.881), hypertriglyceridemia (OR 1.403, 95% CI 1.185–1.660), and low HDL-C (OR 1.464, 95% CI 1.231–1.742) as independent risk factors for early-onset ACS (all P<0.001). The five-year follow-up showed that the incidences of all cause death (1.5% vs. 3.8%, P<0.001), cardiac death (1.1% vs. 2.0%, P=0.023), and recurrent stroke (2.2% vs. 4.2%, P<0.001) were lower, while bleeding events were more frequent in the early-onset ACS group. A subgroup analysis showed higher incidences of recurrent myocardial infarction (MI) and revascularization in patients with early-onset ACS and metabolic syndrome.
CONCLUSIONS:
Obesity, hypertriglyceridemia, and lower HDL-C level are independent risk factors for early-onset ACS, recurrent MI, and revascularization. The control of metabolic syndrome may reduce the incidence of early-onset ACS and improve the long-term prognosis.
Keywords: Age, Coronary artery disease, Acute coronary syndrome, Metabolic syndrome
INTRODUCTION
Acute coronary syndrome (ACS) is a critical manifestation of coronary artery disease (CAD) with high mortality and disability. Although CAD is common in older individuals, the incidence is increasing in middle-aged and young populations (early-onset CAD). Early-onset CAD has serious consequences, such as early death and long-term disability.[1,2]
Metabolic syndrome is associated with ACS in patients <45 years of age and is more valuable than established cardiovascular risk factors,[3] and obesity is the most prevalent risk factor for ACS in young adults.[4] However, with improvements in living standards and an increase in the incidence of metabolic syndrome, the impact of metabolic syndrome on ACS onset age is unclear in China. Furthermore, the long-term prognosis of patients with early-onset ACS is controversial. During a 10.3-year follow-up of patients with premature acute myocardial infarction (AMI), 23% of patients experienced major adverse cardiovascular events. Of these patients, 6% died, 17% experienced re-AMI, and 5% suffered ischemic stroke.[5] Another study showed a favorable prognosis with short- and medium-term follow-ups of young patients with AMI.[6] Here, we aim to investigate effects of metabolic syndrome on onset age and long-term outcomes in patients with ACS.
METHODS
Study population
A total of 6,431 patients with ACS who underwent percutaneous coronary intervention (PCI) at Fuwai Hospital, National Center for Cardiovascular Diseases (Beijing, China), from January to December 2013, were enrolled. Early-onset CAD was defined in males ≤50 years of age and females ≤60 years of age.[7] After excluding patients with previous myocardial infarction (MI), previous PCI, and previous coronary artery bypass graft, 1,558 patients conformed to the definition of early-onset ACS (including unstable angina pectoris, non-ST-segment elevation MI, and ST-segment elevation MI), and 3,044 patients were allocated to the late-onset ACS group. The study protocol was approved by our institutional review board, and written informed consent was obtained from patients before intervention. The study was approved by the ethics committee of the hospital (ethical application number: IRB2012-BG-006; approval number: 2013-449).
Procedures, medications, and patient follow-up
The PCI strategy and stent type were at the treating physician’s discretion. Patients scheduled for PCI received standardized drug treatment before and after the procedure. All patients were followed up in the hospital and evaluated by clinic visits or by phone after one month, six months, one year, two years, and five years. Patients were advised to return for coronary angiography if clinically indicated by symptoms or signs of myocardial ischemia.
Definitions
Major adverse cardiovascular and cerebrovascular events (MACCEs), including all-cause death, cardiac death, recurrent MI, stent thrombosis, target vessel revascularization (TVR), recurrent stroke, and bleeding events, were assessed during a five-year follow-up. MI was defined in accordance with the third universal definition of MI.[8] Unplanned TVR was defined as event-driven repeat PCI or surgical bypass of any segment of the target vessel for ischemic symptoms.[9] Stent thrombosis was defined in accordance with the Academic Research Consortium’s definition and was classified as definite, probable, or possible.[9] Bleeding was quantified in accordance with Bleeding Academic Research Consortium criteria, and types 2–5 were included in the analysis.[10]
Metabolic syndrome included obesity, hypertension, diabetes mellitus, hypertriglyceridemia, and low high-density lipoprotein cholesterol (HDL-C). Obesity was defined as body mass index (BMI) ≥28 kg/m2. Hypertension was defined as a history of hypertension and in-hospital blood pressure >130/85 mmHg (1 mmHg=0.133 kPa). Hypertriglyceridemia was definite as triglyceride (TG) concentration ≥1.7 mmol/L, and low HDL-C was defined as HDL-C concentration <1.04 mmol/L. If patients demonstrated 3–5 of these criteria, they were diagnosed with metabolic syndrome.
Statistical analysis
Continuous variables were compared using the Student’s t-test, and categorical variables were compared using Pearson’s χ2 test. Continuous variables were presented as mean±standard deviation and categorical variables as the number with frequency. Survival curves were calculated using Kaplan-Meier estimates and compared using the log-rank test for endpoints. The results of logistic regression were expressed as odds ratios (ORs) and 95% confidence intervals (CIs). Clinical and statistical covariates entered into the model and adjusted in the multivariate analysis. All statistical analyses were performed using SPSS version 19.0 (IBM Corp., Armonk, New York, USA). Significance was set at a two-sided P-value <0.05.
RESULTS
Baseline characteristics
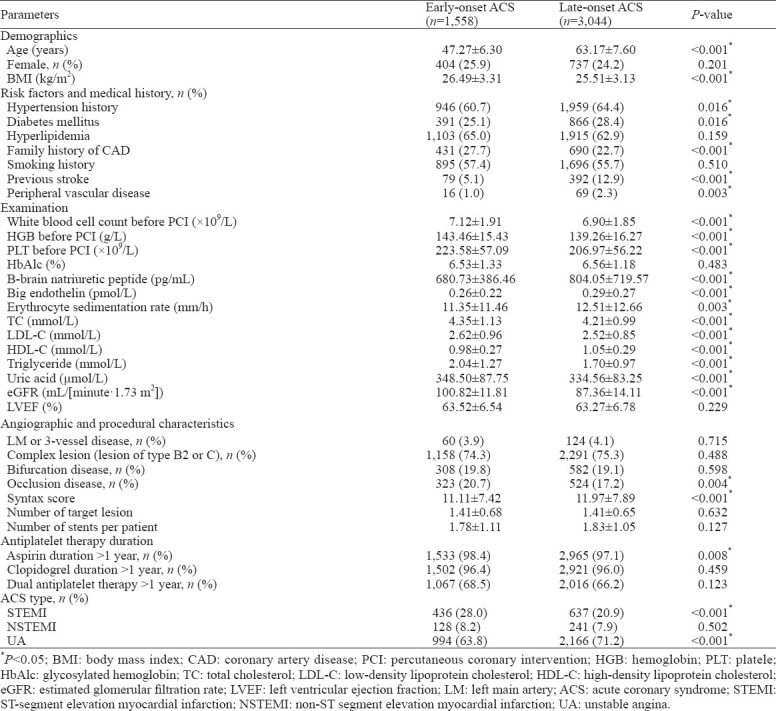
The response rate of the five-year follow-up was 91.5%. The proportions of patients with early-onset ACS (n=1,558) and late-onset ACS (n=3,044) with no previous CAD history (n=4,602) were 33.9% and 66.1%, respectively. Patients’ basic characteristics are shown in Table 1.
Table 1.
Patients’ baseline characteristics between two groups
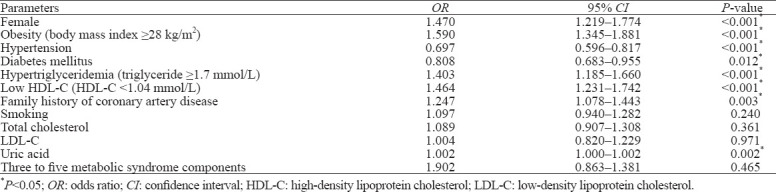
Association between metabolic syndrome and early-onset ACS
Compared with the late-onset ACS group, the proportions of patients with obesity, hypertriglyceridemia, and low HDL-C were significantly higher, while the proportions of patients with hypertension (66.2% vs. 71.2%, P<0.001) and diabetes mellitus (25.1% vs. 28.4%, P=0.016) were lower in the early-onset ACS group. The percentage of patients who met more than three metabolic syndrome criteria was significantly higher in the early-onset ACS group compared with the late-onset ACS group (46.1% vs. 35.7%, P<0.001). Multivariate logistic regression revealed obesity, hypertriglyceridemia, and low HDL-C as independent risk factors for early-onset ACS (Table 2).
Table 2.
Logistic regression analysis of metabolic syndrome components for early-onset ACS
Long-term outcomes of early-onset ACS and effects of metabolic syndrome
The clinical outcomes showed that the incidence of MACCEs was not significantly different between the two groups during the in-hospital follow-up. After the five-year follow-up, the incidences of all-cause death, cardiac death, and recurrent stroke were lower in the early-onset ACS group, while the incidence of bleeding events was higher in the early-onset ACS group (Table 3), compared with the late-onset ACS group. Kaplan-Meier estimates showed the same trend (Figure 1).
Table 3.
Clinical outcomes in patients with early-onset ACS and late-onset ACS during fi ve-year follow-up, n (%)
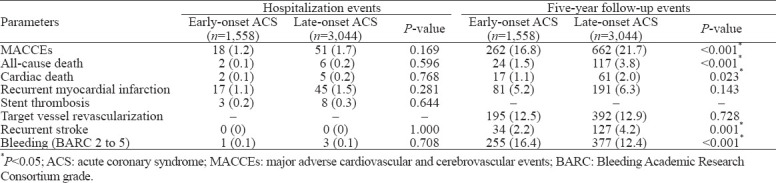
Figure 1.
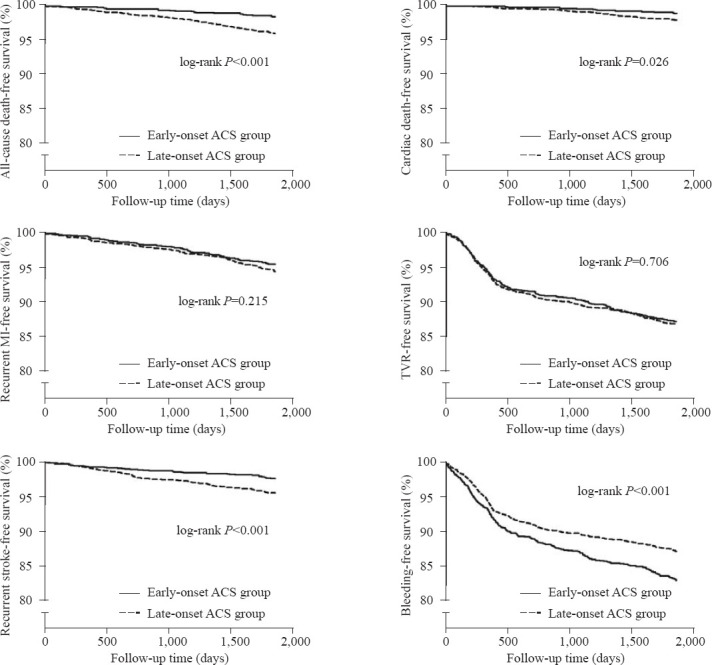
Kaplan-Meier survival analysis. MI: myocardial infarction; TVR: target vessel revascularization.
In a subgroup analysis of early-onset ACS, the incidences of MACCEs (20.1% vs. 14.0%, respectively, P=0.002), recurrent MI (6.5% vs. 4.0%, P=0.027), and TVR (14.9% vs. 10.8%, P=0.008) in patients with metabolic syndrome were higher compared with patients without metabolic syndrome. Other ischemic and bleeding events were not significantly different between the two subgroups.
DISCUSSION
Metabolic syndrome is becoming increasingly common with changes in lifestyle. Metabolic syndrome can be easily identified in the clinic; however, the effect of metabolic syndrome on onset age and long-term prognosis of patients with ACS has not been investigated. The major findings of this study are as follows: (1) approximately one-third of patients with ACS had early-onset ACS and were more likely to demonstrate ST-segment elevation MI, and the overall prognosis of patients with early-onset ACS was better than that of patients with late-onset ACS; (2) obesity, hypertriglyceridemia, and low HDL-C were independent risk factors for early-onset ACS; and (3) metabolic syndrome was related to an increase in MACCEs in patients with early-onset ACS, especially recurrent MI and TVR.
Overall condition of patients with early-onset ACS
The atherosclerotic plaques of younger patients are rich in foam cells, which reduce plaque stability and induce early-onset ACS.[11] However, as there is no standardized age to delineate early-onset ACS at present, the incidence of early-onset ACS differs between epidemiological surveys.[12~14] In the present study, 33.9% of patients with ACS without previous CAD after PCI met the age diagnostic criteria for early-onset ACS; thus, more than one-third of young and middle-aged patients who experienced acute coronary events were treated with PCI. In this study, patients with early-onset ACS more frequently presented with ST-segment elevation MI, while patients with late-onset ACS more frequently presented with unstable angina. This suggests that plaque stability in patients with early-onset ACS may be worse, and coronary artery reserve or ischemic pre-adaptation may be lower, when compared with patients with late-onset ACS, which may induce transmutable MI.
With the widespread use of PCI for the treatment of ACS, patients with early-onset ACS demonstrate excellent immediate and long-term survival outcomes.[15] A small-sample study examining the prognosis of patients with early-onset ACS showed that the mortality of early-onset ACS was similar to ACS in older patients, but another study showed better outcomes in younger patients.[6] Thus, there is still controversy about the clinical prognosis of patients with early-onset ACS. In the current study, the incidence of inhospitable MACCEs was not significantly different between the early- and late-onset ACS groups, but long-term outcomes, including all-cause death, cardiac death, and recurrent stroke, were less frequently observed in the early-onset ACS group. During the five-year follow-up, the mortality rate of patients with early-onset ACS was 1.5% (3.8% in patients with late-onset ACS), which indicated that the long-term follow-up of ischemic events in patients with early-onset ACS did not increase. However, the incidence of bleeding events in patients with early-onset ACS was higher compared with patients with late-onset ACS, which may be related to the longer duration of antiplatelet therapy.
Relationship between metabolic syndrome and ACS onset age
Traditional risk factors, such as hypertension, diabetes mellitus, dyslipidemia, smoking, and family history of CAD, are associated with early-onset ACS.[16] In the current study, we found that patients with early-onset ACS had a higher BMI, higher TG, and total cholesterol concentrations. Logistic regression revealed metabolic syndrome components, including obesity, hypertriglyceridemia, and low HDL-C, as independent risk factors for early-onset ACS. These findings indicate that the metabolic abnormality caused by metabolic syndrome is related to the occurrence and development of early-onset ACS, which could be controlled by primary and secondary CAD preventions and would reduce the incidence of early-onset ACS.
Effects of metabolic syndrome on a long-term prognosis in patients with early-onset ACS
Patients with early-onset ACS with metabolic syndrome had a higher incidence of MACCEs compared with patients with late-onset ACS after five years of follow-up. Metabolic syndrome was associated with an increased risk of adverse cardiovascular events in patients with early-onset ACS.[17,18] This result emphasized that patients with early-onset ACS and metabolic syndrome should be encouraged to achieve more strict weight control and should receive standard drug treatments to rectify abnormalities in blood lipids, blood glucose, and blood pressure to reduce the long-term incidence of adverse cardiovascular events.
Other factors associated with early-onset ACS
A family history of CAD and hyperuricemia were positively correlated with early-onset ACS in this study. Previous studies showed that a family history of CAD and hyperuricemia are related to CAD,[16] and hyperuricemia could independently confer a higher risk of mortality in patients with AMI. This may be due to coronary artery injury caused by uric acid and the local inflammatory response. Hyperuricemia can also accelerate atherosclerosis by promoting LDL oxidation and inducing vascular endothelial dysfunction, which may lead to early-onset ACS.
Potential clinical implications
The current study showed a definite correlation between metabolic syndrome and early-onset ACS, and identified the effect of metabolic syndrome on adverse prognosis. Although the overall prognosis of patients with early-onset ACS is better compared with patients with late-onset ACS, we should pay more attention to metabolic syndrome in young patients and offer appropriate intervention in clinical practice. This could delay ACS occurrence and improve prognosis, especially in developing countries.
Limitations
Several limitations should be considered. First, our data were obtained from a single clinical center. Second, the criteria of age for the diagnosis of premature CAD should be verified; however, at the time of the study, a reference standard was lacking. Third, this was an observational study with a non-randomized design, and unmeasured confounders may have precluded definitive conclusions.
CONCLUSIONS
Metabolic syndrome components, including obesity, hypertriglyceridemia, and low HDL-C, are independent risk factors for early-onset ACS and relate to an increase in recurrent MI and revascularization. An effective control of metabolic syndrome may reduce the incidence of early-onset ACS and improve the long-term prognosis.
Footnotes
Funding: The study was supported by the National Key Research and Development Program of China (2016YFC130130 [Subtopic: 2016YFC1301301]).
Ethical approval: The study was approved by the Ethics Committee of Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China (ethical application number: IRB2012-BG-006; approval number: 2013-449).
Conflicts of interests: All authors declared no conflicts of interest.
Contributors: BX and YZ contributed equally to this work. All authors revised and approved the final version of the manuscript.
REFERENCES
- 1.Sadeghi R, Adnani N, Erfanifar A, Gachkar L, Maghsoomi Z. Premature coronary heart disease and traditional risk factors —can we do better? Int Cardiovasc Res J. 2013;7(2):46–50. [PMC free article] [PubMed] [Google Scholar]
- 2.Jeemon P, Harikrishnan S, Sanjay G, Sivasubramonian S, Lekha TR, Padmanabhan S, et al. A programme of lifestyle intervention in families for cardiovascular risk reduction (PROLIFIC study): design and rationale of a family based randomized controlled trial in individuals with family history of premature coronary heart disease. BMC Public Health. 2017;17(1):10. doi: 10.1186/s12889-016-3928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kalantzi K, Korantzopoulos P, Tzimas P, Katsouras CS, Goudevenos JA, Milionis HJ. The relative value of metabolic syndrome and cardiovascular risk score estimates in premature acute coronary syndromes. Am Heart J. 2018;155(3):534–40. doi: 10.1016/j.ahj.2007.10.038. [DOI] [PubMed] [Google Scholar]
- 4.Mirza AJ, Taha AY, Khdhir BR. Risk factors for acute coronary syndrome in patients below the age of 40 years. Egypt Heart J. 2018;70(4):233–5. doi: 10.1016/j.ehj.2018.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Winter MP, Blessberger H, Alimohammadi A, Pavo N, Huber K, Wojta J, et al. Long-term outcome and risk assessment in premature acute myocardial infarction:a 10-year follow-up study. Int J Cardiol. 2017;240:37–42. doi: 10.1016/j.ijcard.2017.03.146. [DOI] [PubMed] [Google Scholar]
- 6.Brscic E, Bergerone S, Gagnor A, Colajanni E, Matullo G, Scaglione L, et al. Acute myocardial infarction in young adults:prognostic role of angiotensin —converting enzyme, angiotensin II type I receptor, apolipoprotein E, endothelial constitutive nitric oxide synthase, and glycoprotein IIIa genetic polymorphisms at medium-term follow-up. Am Heart J. 2000;139(6):979–84. doi: 10.1067/mhj.2000.106165. [DOI] [PubMed] [Google Scholar]
- 7.Do R, Stitziel NO, Won HH, Jørgensen AB, Duga S, Angelica Merlini P, et al. Exome sequencing identifies rare LDLR and APOA5 alleles conferring risk for myocardial infarction. Nature. 2015;518(7537):102–6. doi: 10.1038/nature13917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of myocardial infarction. Glob Heart. 2012;7(4):275–95. doi: 10.1016/j.gheart.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 9.Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, et al. Clinical end points in coronary stent trials:a case for standardized definitions. Circulation. 2007;115(17):2344–51. doi: 10.1161/CIRCULATIONAHA.106.685313. [DOI] [PubMed] [Google Scholar]
- 10.Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, et al. Standardized bleeding definitions for cardiovascular clinical trials:a consensus report from the bleeding academic research consortium. Circulation. 2011;123(23):2736–47. doi: 10.1161/CIRCULATIONAHA.110.009449. [DOI] [PubMed] [Google Scholar]
- 11.Kostara CE, Papathanasiou A, Psychogios N, Cung MT, Elisaf MS, Goudevenos J, et al. NMR-based lipidomic analysis of blood lipoproteins differentiates the progression of coronary heart disease. J Proteome Res. 2014;13(5):2585–98. doi: 10.1021/pr500061n. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention (CDC) Prevalence of coronary heart disease —United States, 2006–2010. MMWR Morb Mortal Wkly Rep. 2011;60(40):1377–81. [PubMed] [Google Scholar]
- 13.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study):case-control study. Lancet. 2004;364(9438):937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 14.Fernando H, Adams N, Mitra B. Investigations for the assessment of adult patients presenting to the emergency department with supraventricular tachycardia. World J Emerg Med. 2020;11(1):54–9. doi: 10.5847/wjem.j.1920-8642.2020.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ertelt K, Généreux P, Mintz GS, Brener SJ, Kirtane AJ, McAndrew TC, et al. Clinical profile and impact of family history of premature coronary artery disease on clinical outcomes of patients undergoing primary percutaneous coronary intervention for ST-elevation myocardial infarction: analysis from the HORIZONS-AMI trial. Cardiovasc Revasc Med. 2014;15(8):375–80. doi: 10.1016/j.carrev.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 16.Aggarwal A, Srivastava S, Velmurugan M. Newer perspectives of coronary artery disease in young. World J Cardiol. 2016;8(12):728–34. doi: 10.4330/wjc.v8.i12.728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alexander CM, Landsman PB, Teutsch SM, Haffner SM. Third National Health and Nutrition Examination Survey (NHANESIII), National Cholesterol Education Program (NCEP). NCEP defined metabolic syndrome, diabetes, and prevalence of coronary heart disease among NHANES III participants age 50 years and older. Diabetes. 2003;52(5):1210–4. doi: 10.2337/diabetes.52.5.1210. [DOI] [PubMed] [Google Scholar]
- 18.Sattar N, Gaw A, Scherbakova O, Ford I, O'Reilly DS, Haffner SM, et al. Metabolic syndrome with and without C-reactive protein as a predictor of coronary heart disease and diabetes in the West of Scotland Coronary Prevention Study. Circulation. 2003;108(4):414–9. doi: 10.1161/01.CIR.0000080897.52664.94. [DOI] [PubMed] [Google Scholar]


