INTRODUCTION
Over the past few decades, traumatic brain injuries (TBIs) have become one of the leading causes of death and the leading cause of injury-related death in the USA.[1,2] It is estimated that 1.70 million people are subject to TBIs each year.[2] Males are more likely to sustain TBIs (59%); the most common age groups are 0–5 years, 15–19 years, and >65 years.[2] Approximately 1.36 million people present to the emergency department (ED), 275,000 are admitted to the hospital, and 52,000 people die from TBIs.[2] The leading causes of TBIs are falling (35.2%), motor vehicle collisions (MVCs, 17.3%), struck by/against an object (16.5%), and assault (10.0%).[2] These statistics combine to make TBIs the leading cause of injury-related death in the USA at 30.5%.[2] It has been estimated that, with specific guidelines from the Brain Trauma Foundation, up to 50.0% of the 52,000 TBI-related deaths may be prevented.[3]
The purpose of this study is to determine the difference in TBI outcomes caused by MVCs between belted and unbelted victims. Since the introduction of the first seatbelt law in 1984,[4] it has become a well-acknowledged fact that seatbelts do indeed aid in reducing fatalities and injuries in MVCs. However, this study seeks to identify the true differences in this reduction, observing specific data of each patient belted or unbelted with regard to specific clinical outcomes including TBI severity, computed tomography (CT) scan findings, hospital admission, intensive care unit (ICU) care, and need for surgical interventions.
METHODS
This Institutional Board Review approved retrospective chart review consisted of consecutive adult patients who presented to the Emergency Medicine and Neurology, University of Central Florida College of Medicine within 24 hours of their head injury in the year 2013. This cohort, derived from an ED TBI registry,[5] represented the subset of patients who sustained their TBIs as a result of MVCs, compared with another mechanism such as fall, sport, or assault. Data were abstracted from the electronic medical records using a priori designed data abstraction form. The trained abstractors entering the data were blinded to the study hypotheses and outcomes. The cohort was assembled from hospital records using ICD-9 codes for brain injury (850.0–804.9, 850.0–854.0, and 959.01), which were hand searched for the inclusion criteria of adults who presented to the ED within 24 hours of their head injury. Data collection included the location of the patient in the vehicle (driver or passenger), whether or not they were restrained, the severity of TBI, injury symptomatology, whether or not they were admitted to the hospital after ED evaluation, or required surgery. TBI severity was defined using the Glasgow Coma Scale (GCS) upon initial ED presentation, with mild TBI defined as GCS score of 13 to 15, moderate as GCS score of 9 to 12, and severe as GCS score of 8 or less. Subjects were divided by their age, type of vehicle (four wheels or two wheels), results of brain CT, need for hospital admission and ICU care, and whether the surgical intervention was required. A brain CT was considered abnormal if any of the followings was noted: extracalvarial soft tissue, skull or facial bone fracture, herniation, subdural or epidural hematoma, intraparenchymal or intraventricular hemorrhage, and diffuse axonal injury.
Data were entered into REDCap (Research Electronic Data Capture), a secure, web-based application designed to support traditional case report form data capture. Statistical analyses were performed using JMP 14.0 for the Macintosh, and consisted of Chi-square tests and nominal regression analyses with computations of odds ratio (OR) and their 95% confidence interval (CI) where appropriate. The independent variable was the use of seatbelts. The dependent variables used in the regression analysis included the presence of abnormal head CT scan, hospital admission, ICU stay, TBI severity, and surgical intervention.
RESULTS
There were 803 subjects in our cohort. The median age of the cohort was 32 years with an interquartile range of 23–49 years. Eighty percent of the cohort had mild TBI, 3% moderate TBI, and 17% severe TBI as defined by their GCSs. Sixty-two percent of the cohort were drivers, 13% were front-seat passengers, 5% were back-seat passengers, and 20% couldn’t remember whether they were drivers, front-seat passengers, back-seat passengers, or were sitting in open air seating, such as the flat bed of a truck. Just 45% of the cohort confirmed wearing their seatbelt, with 25% not remembering whether they did or not, and 30% stating they did not. Regardless of their position, those not wearing a seatbelt were more likely to have a loss of consciousness (LOC) (P<0.001). For 14% of the cohort, LOC was not recorded, so they were categorized as unknown. In an intention to treat analysis if all these unknowns were presumed to not have LOC, seatbelt use was still protective (OR=2.66, P<0.001). Similarly, those not wearing a seatbelt were more likely to have an alteration of consciousness (AOC) (OR=1.91, P<0.001).
Table 1 shows the association of location of subject and seatbelt use in relation to outcomes of their injury. Patients without seatbelts did worse with regard to every outcome (Z-test for proportions). Drivers who went without seatbelts were twice as likely to have an abnormal head CT over drivers who were restrained. Similarly, drivers who were not restrained were almost twice as likely to be admitted to the hospital and one and a half times as likely to be admitted to the ICU. Front-seat passengers who did not wear the seatbelts were 25% more likely to be admitted to the hospital than those who were restrained. The TBI severity was also affected by seatbelt use with unrestrained drivers being almost four times as likely to have a more severe TBI. Surgical interventions, including ventriculostomy and craniotomy, were performed two times more often on unrestrained drivers. Similarly, almost half of all front-seat passengers who did not wear their seatbelts were admitted to the ICU. Table 2 depicts the odds of hospital admission, abnormal imaging, and death with seatbelt use and without seatbelt use. In addition to these univariate correlations, multivariable logistic regression models were built (Figure 1).
Table 1.
Outcomes based on seatbelt use in motor vehicle collisions
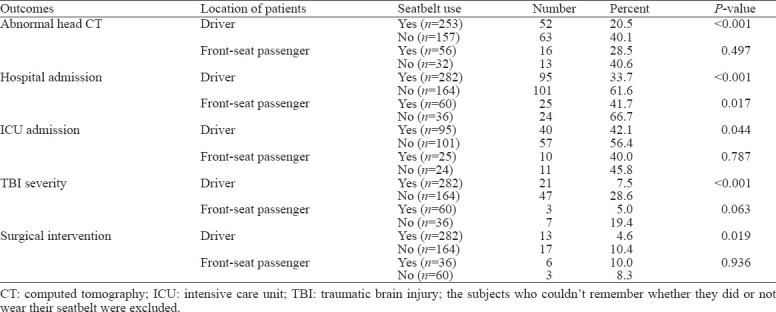
Table 2.
Seatbelt use and odds ratio of abnormal brain CT imaging, hospital admission, and death
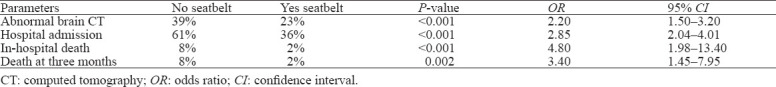
Figure 1.
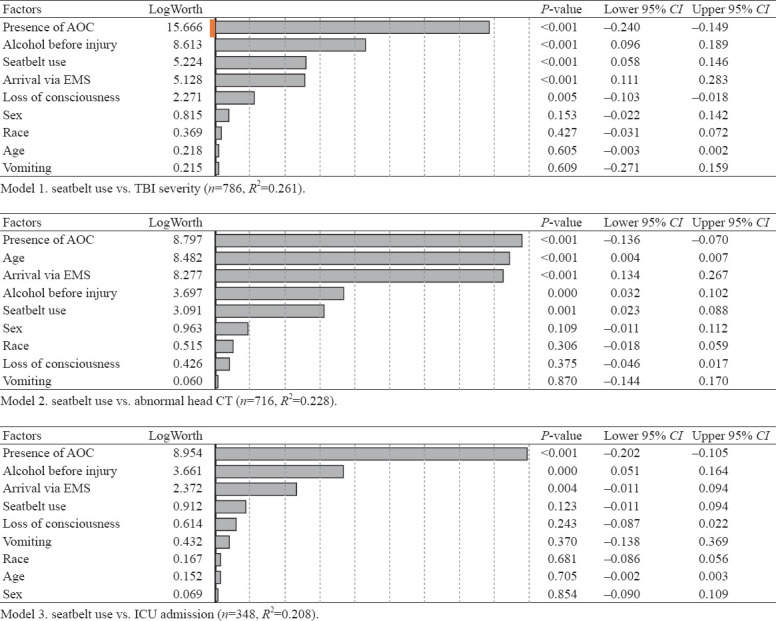
Multivariable logistic models analyzing seatbelt use versus TBI severity, abnormal head CT, and ICU admission. AOC: alteration of consciousness; EMS: emergency medical service; ICU: intensive care unit; TBI: traumatic brain injury; CT: computed tomography; CI: confidence interval.
DISCUSSION
The current study demonstrates the association between seatbelt use and outcomes after MVC. Drivers were at the highest risk for a severe TBI if they were not restrained with a seatbelt. Both drivers and passengers could avoid more severe TBIs, surgical interventions, admissions to the hospital and/or ICU, and abnormal head CTs with seatbelt use. Interestingly, this study was conducted in a state with a primary seatbelt law, and used the seatbelt defense to lower damages in applicable civil suits.
MVC-related injuries, specifically TBI-related injuries, are among the leading causes of death in the USA, particularly with the younger and middle-aged generations. One form of TBI prevention in MVCs is the use of seatbelts. It has been reported that the implementation of primary enforcement laws for seatbelt use is much better than the secondary enforcement of seatbelt laws.[6,7] The primary enforcement law, where a police officer can pull over a driver with the sole cause being an absence of the use of a seatbelt, is used in 31 states and the District of Colombia.[8] The secondary enforcement law allows the officer to ticket for the absence of seatbelt only when the officer has pulled over the driver for another offense.[8] Within each law, there are differences in the location and the age of the passenger regarding the necessity of a seatbelt. Regardless of the specifics, the difference of enforcement is seen as a valid means for increasing the use of seatbelt and thereby decreasing the rate of TBIs in MVCs. In states where primary enforcement was used, there was an average 10.1% increase in the use of seatbelts over states that used secondary enforcement.[5] Primary enforcement states have seen 88.2% of the population using seatbelts with secondary states seeing 79.2% (Centers for Disease Control and Prevention [CDC], unpublished data 2010).
Relating the use of seatbelts to TBI, the differences between belted and unbelted victims are seen both in the severity of the injury[9] and the injury location. Unbelted victims are more likely to sustain damage in the posterior cortical portion of the brain.[10] Studies by the National Highway Traffic Safety Administration (NHTSA) have proven the effectiveness of seatbelts in reducing major and minor injuries as well as fatalities in MVCs. Seatbelts were found to be effective in reducing fatal injuries by 45% and serious injuries by 50%.[11] Contributing more to the case for seatbelts, research showed that in the time period in which 14 more states passed the primary enforcement law, both MVC fatalities and MVC injuries declined.[6] It was estimated in 2009 by NHTSA that, with the use of a seatbelt or safety restraint, 450 lives could have been saved and 12,000 injuries prevented (NHTSA, unpublished data 2009).[5] Along with the lives, 1.6 billion dollars in costs could have been saved if states had been using the primary enforcement laws (NHTSA, unpublished data 2009). Despite these statistics, it was estimated that 16% of the USA population occupied a vehicle without a seatbelt.[4]
It is believed that the use of seatbelts could be the limiting factor in reducing TBI-related deaths caused by MVCs. The most compelling data for this argument can be seen in studies related to the enforcement of seatbelts in all 50 states. TBI-related deaths have been on the decline since the 1980s mostly due to the increase in seatbelt enforcement in all 50 states and District of Colombia.[12] During the years of 2001–2009, 14 additional states were added to the list of primary enforcement states, and in this eight-year period, MVC-related fatalities significantly decreased.[6] Studies have found groups like obese drivers, males, and drivers under the influence of alcohol, having a low record of seatbelt use, demonstrate the increased use of seatbelts in states where the primary seatbelt law is enforced.[12] For example, drivers under the influence of alcohol in states with the primary enforcement law are 15% more likely to use a seatbelt than those driving in states with the secondary enforcement law.[13,14] Likewise, obese drivers in states where the primary seatbelt law is enforced are 14% more likely to use a seatbelt than those in states with the secondary enforcement law.[15] The implementation of the primary enforcement law shows an obvious increase in seatbelt use, thus decreasing the number of severe TBIs in drivers and passengers involved in MVCs. A study shows the level of importance for seatbelt use, ranking it as a more important factor than driver error and demographics such as age and gender in injury severity.[16] From our results, the validity of seatbelts in reducing TBI severity is only further confirmed.
Though rates of TBI-related injuries have been decreasing and the use of seatbelts has been increasing over the past few decades, a startling number of preventable injuries still exist. This study aims to educate occupants of vehicles on the correlation of TBI and seatbelt use, and in doing so encourages the use of seatbelts in motor vehicle occupants. From the results, a direct correlation was found in the absence of seatbelts and severe TBIs and other factors as a result of the measure of TBI severity. Primary enforcement laws have been shown to increase seatbelt use.[10,14,17] As this study was conducted in a state where the primary enforcement law exists, a different approach must be taken. One approach that could be taken is from the education aspect, showing occupants of motor vehicles the consequences of an absence of seatbelts in relation to TBIs.
The strengths of the current study include its consecutive nature, large sample size, and patient-level data. Its limitations are that it is a single-center study, and its retrospective nature means the reasons for wearing or not wearing a seatbelt could not be discerned.
CONCLUSIONS
Not wearing a seatbelt is significantly associated with having a worse head injury, being admitted to the hospital, and requiring intensive care or surgery. The use of seatbelts confers significant protection against adverse sequelae following TBIs. These data serve to underscore the importance of injury prevention efforts.
Footnotes
Funding: None.
Ethical approval: This study was approved by the Institutional Board Review.
Conflicts of interest: None of the authors have any conflicts of interest.
Contributors: LG proposed and wrote the first draft. All authors contributed to the design and interpretation of the study and to final version.
REFERENCES
- 1.Coronado VG, Thurman DJ, Greenspan AI, Weissman BM. Epidemiology. In: Jallo J, Loftus CM, editors. Neurotrauma and Critical Care: Brain. New York, NY: Thieme; 2009. pp. 3–19. [Google Scholar]
- 2.Faul M, Xu L, Wald MM, Coronado V. Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths, 2002–2006. Available at https: //www.cdc.gov/traumaticbraininjury/pdf/blue_book.pdf .
- 3.Faul M, Wald MM, Rutland-Brown W, Sullivent EE, Sattin RW. Using a cost-benefit analysis to estimate outcomes of a clinical treatment guideline: testing the brain trauma foundation guidelines for the treatment of severe traumatic brain injury. J Trauma. 2007;63(6):1271–8. doi: 10.1097/TA.0b013e3181493080. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Primary enforcement of seat belt laws. Available at https: //www.cdc.gov/motorvehiclesafety/calculator/factsheet/seatbelt.html .
- 5.National Highway Traffic Safety Administration. Traffic safety facts 2008. Available at http: //www-nrd.nhtsa.dot.gov/pubs/811170.pdf .
- 6.Nichols JL, Tippetts AS, Fell JC, Auld-Owens A, Wiliszowski CH, Haseltine PW, et al. Strategies to increase seat belt use:an analysis of levels of fines and the type of law. Available at https: //www.nhtsa.gov/sites/nhtsa.dot.gov/files/811413.pdf .
- 7.Chen YY, Ye TJ. Seat belt use in 2010 —use rates in the states and territories. Available at https: //crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/812546.
- 8.Dinh-Zarr TB, Sleet DA, Shults RA, Zaza S, Elder RW, Nichols JL, et al. Reviews of evidence regarding interventions to increase the use of safety belts. Am J Prev Med. 2001;21(4 Suppl):48–65. doi: 10.1016/s0749-3797(01)00378-6. [DOI] [PubMed] [Google Scholar]
- 9.Allen S, Zhu S, Sauter C, Layde P, Hargarten S. A comprehensive statewide analysis of seatbelt non-use with injury and hospital admissions: new data, old problem. Acad Emerg Med. 2006;13(4):427–34. doi: 10.1197/j.aem.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 10.Hillary F, Moelter ST, Schatz P, Chute DL. Seatbelts contribute to location of lesion in moderate to severe closed head trauma. Arch Clin Neuropsychol. 2001;16(2):171–81. [PubMed] [Google Scholar]
- 11.National Highway Traffic Safety Administration. Traffic safety facts:2006. Available at http: //www-nrd.nhtsa.dot.gov/Pubs/810807.pdf .
- 12.Stead LG, Bodhit A, Patel PS, Daneshvar Y, Peters KR, Mazzuoccolo A, et al. TBI surveillance using the common data elements for traumatic brain injury:a population study. Int J Emerg Med. 2013;6(1):5. doi: 10.1186/1865-1380-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention (CDC) Ten great public health achievements —United States, 2001–2010. MMWR Morb Mortal Wkly Rep. 2011;60(19):619–23. [PubMed] [Google Scholar]
- 14.Voas RB, Fell JC, Tippetts AS, Blackman K, Nichols JL. Impact of primary safety belt laws on alcohol-related front-seat occupant fatalities:five case studies. Traffic Inj Prev. 2007;8(3):232–43. doi: 10.1080/15389580701218489. [DOI] [PubMed] [Google Scholar]
- 15.Voas RB, Tippetts AS, Fell J. The relationship of alcohol safety laws to drinking drivers in fatal crashes. Accid Anal Prev. 2000;32(4):483–92. doi: 10.1016/s0001-4575(99)00063-9. [DOI] [PubMed] [Google Scholar]
- 16.Beck LF, Shults RA, Mack KA, Ryan GW. Associations between sociodemographics and safety belt use in states with and without primary enforcement laws. Am J Public Health. 2007;97(9):1619–24. doi: 10.2105/AJPH.2006.092890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu C, Lindsey T, Chen CL, Utter D. States with primary enforcement laws have lower fatality rates. Available at https: //crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/810921 .


