Abstract
Past research shows that high-quality public preschool may disproportionately support low-income children’s school readiness, because low-income children tend to arrive at school with fewer of the academic skills needed for success. This suggests a compensatory process in human development in which the children who benefit most from a promotive factor are those who stand to gain the most. We propose that high-quality public preschool may similarly confer its greatest health rewards to low-income children, who are generally in poorer health than their peers. If that is true, preschool has the potential to narrow health disparities by income, which without intervention, persist into adulthood. To date, no one has articulated all the pathways through which high-quality public preschool may improve children’s health, much less those that should disproportionately benefit those from low-income families. Drawing on the bioecological paradigm of human development, we propose a model identifying specific mechanisms likely to promote equity in child health. These mechanisms reflect core characteristics of high-quality public preschool that may disproportionately benefit low-income children’s health. This model serves as a working template for a program of future research.
Keywords: pediatrics, preschool, child care, low-income, health disparities
Like income-based disparities in achievement that appear early in the lifespan and portend later disadvantages in education and other domains of life success,1 so too do early income-based health disparities foreshadow gaps in physical and mental health and wellbeing throughout the life course.2 High-quality public preschool is widely recognized for its potential to narrow gaps in child achievement associated with family income.3 It has recently been suggested that the effects of high-quality public preschool extend to child health.4,5 If the health benefits of high-quality preschool are greatest for low-income children, just as the academic benefits are, then it has the potential to reduce health, as well as educational, disparities by income. For this reason, pediatricians should view public preschool programs as potential vehicles for narrowing gaps in children’s health associated with family income.
Indeed, the American Academy of Pediatrics (AAP) now considers the promotion of high-quality preschool a matter of policy priority.6 High-quality preschool is characterized by rich learning opportunities and warm and responsive teacher-child interactions.3 Publicly funded programs (Head Start and state pre-kindergarten) provide higher quality care than the other arrangements available to low-income children, and together serve at least half of this population.7 Yet such programs have much room for growth in quality, particularly with respect to health promotion.8
The links between high-quality public preschool and child health may be viewed through the lens of Bronfenbrenner and Morris’ bioecological model of human development.9,10 According to this paradigm, children are shaped by the nested contexts in which their development unfolds (e.g., home, school, neighborhood). They are most proximately affected by their “microsystem,” consisting of interactions with the caregivers in their immediate environments (including parents and preschool teachers), and more distally affected by their “mesosystem,” consisting of interactions that link their caregivers (e.g., teachers and parents) and settings (preschool and home) to each other.
This perspective was recently applied to the study of population health disparities by the National Institute on Minority Health and Health Disparities (NIMHHD).11 The NIMHHD research framework describes how human contexts of development impinge on a range of domains affecting individual health throughout the life course: biological, behavioral, physical environment, sociocultural environment, and the health care system. We maintain that preschool settings are one such context of development. There are several documented associations between high-quality preschool attendance and better health and healthier behaviors in childhood.12–14 Some studies even find associations between high-quality preschool and health in adolescence or adulthood.15–17
The literature on the academic effects of high-quality preschool indicates that although all children benefit from participation, those from lower-income families benefit the most.3 They tend to enter preschool with the lowest achievement scores but experience the greatest improvement over the school year. This phenomenon instantiates a compensatory process commonly found in human development, in which the children who profit most from a promotive factor are those who stand to gain the most from it. Such a pattern may describe the salubrious effects of preschool. We propose a model that identifies specific characteristics of high-quality public preschool that should not only improve all children’s health, but do so disproportionately among children from low-income families. We refer to these characteristics as potential mechanisms for narrowing health disparities in children associated with family income, located at both the microsystem (within the preschool setting) and mesosystem (preschool linkages to other settings) levels.
To be included in our model, a mechanism had to reflect a commonly-understood feature of high-quality preschool3 and have a demonstrated or hypothesized positive impact on health, so long as that impact was likely to be greatest on children from low-income backgrounds. For example, even though preschools may provide parent education around child health (e.g., sleep, nutrition), this activity is not currently considered a core characteristic of high-quality preschool programs, nor has it been shown to disproportionately benefit low-income children,3 so it was excluded from our model. The ultimate aim of this model is to galvanize interest and stimulate research. To the extent that the model is confirmed, it will indicate that high-quality public preschools serve not only as underrecognized loci of health promotion for children, but even as levers of change for narrowing population-based health disparities.
Features of High-Quality Public Preschool That May Narrow Health Disparities Based on Family Income
We identify nine mechanisms by which high-quality public preschool may be hypothesized to narrow pediatric health disparities based on family income (see Figure 1). For each mechanism, we summarize its manifestation in high-quality public preschool, its demonstrated or hypothesized impact on children’s health, and its likelihood of reaping greater rewards for low-than high-income children. We then present pressing questions surrounding that mechanism that might be addressed by future research.
Figure 1.
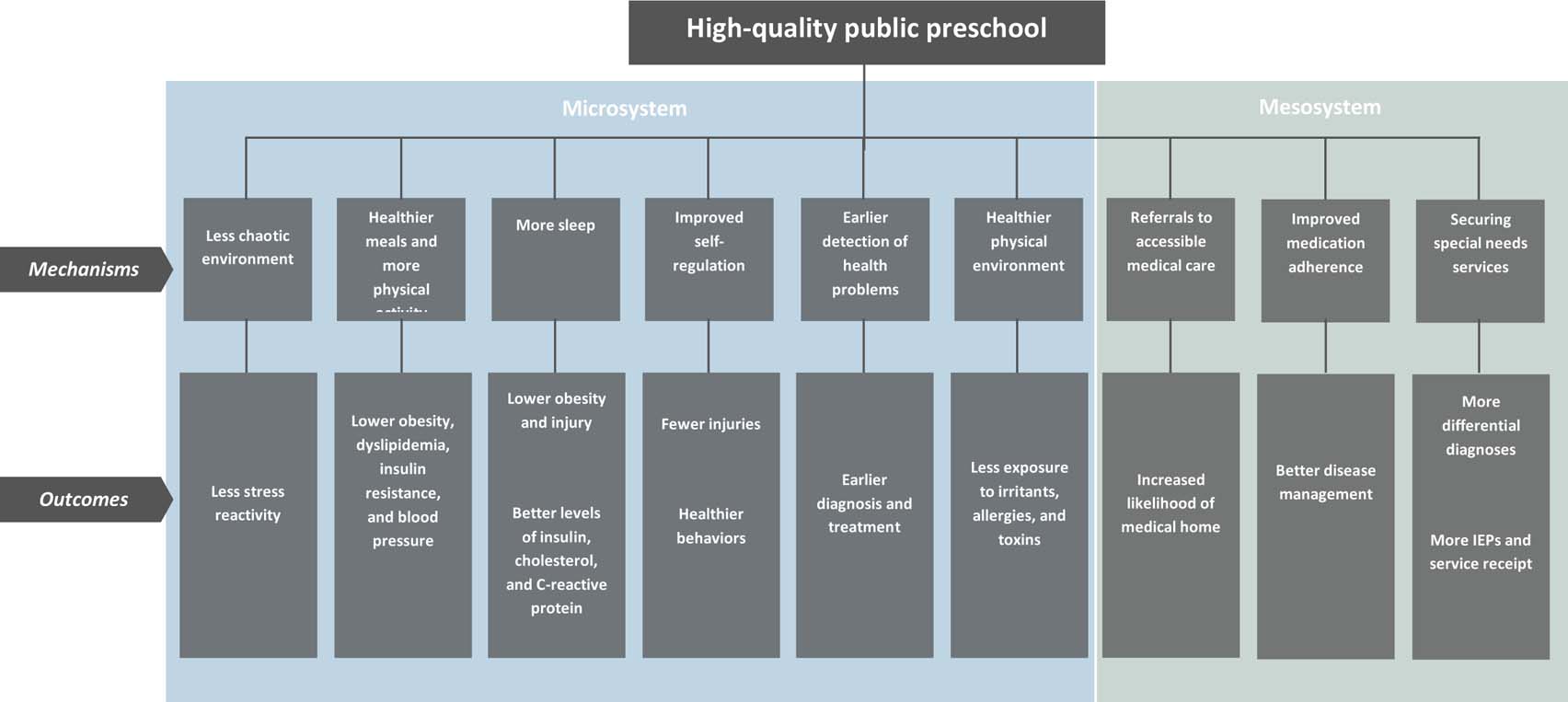
Characteristics of high-quality public preschool hypothesized to narrow child health disparities based on income
Mechanisms in the Microsystem
Less chaotic environment.
High-quality preschool classrooms are defined, in part, by predictability and stability in staffing, routines, and organization of the environment.18 Because of these features, high-quality classrooms may provide a less chaotic environment for low-income children than their home environment. Low-income children are disproportionately likely to be exposed at home to chaos caused by irregular routines, turnover in household composition, and noise and disorder.19 Chaos activates young children’s stress response,20 which is thought to undermine lifetime health via several biophysiological pathways.
First, stress triggers hypervigilance to threats, activating the hypothalamic-pituitary-adrenocortical (HPA) axis and the sympathetic nervous system (SNS). The SNS regulates the immune cells that migrate towards threats in the body to remove pathogens and promote healing of damaged tissue. While this inflammation is protective at first, without down-regulation it poses a risk for depression, type 2 diabetes, and allergic, cardiovascular, metabolic, and rheumatic diseases.21 The HPA axis regulates the production of glucocorticoids and neurotransmitters which, in a normal stress response, are deactivated once a threat subsides, but remain active in cases of chronic stress. Exposure to excess cortisol activity contributes to insulin resistance, hypertension, and fat deposition, which in turn predict type 2 diabetes, cardiovascular disease, and chronic kidney disease.22 Second, stress can impair brain and organ development. For example, adversity affects the prefrontal cortex by decreasing grey matter volume and reducing cortical thickness.21 Third, stress affects the cortico-basal ganglia circuit, where rewards are processed in the brain. Early adversity, for example, is associated with blunted reward sensitivity,21 which may encourage risky and addictive health behaviors such as smoking, drinking, and high-fat eating.
It is as yet unclear just how high-quality preschool impacts low-income children’s stress responses. Studies show that infants, toddlers, and preschoolers enrolled in center-based care show disrupted patterns of diurnal cortisol regulation compared to children in home-based care.23 However, some evidence suggests that this pattern may apply only to children in low-quality settings24 and, significantly, from low-risk backgrounds. In one sample of children from high-risk backgrounds, more hours of child care were associated with lower resting cortisol.25 Further research is needed to replicate these findings with other measures of stress reactivity, specifically among preschool-aged children (as opposed to infants or toddlers). Research is also needed to test for differential linkages between preschool classroom chaos and stress reactivity among low- versus high-income children.
Healthier meals and more physical activity.
High-quality public preschools may provide meals and snacks that are healthier than the food that low-income children would otherwise eat at home.26 For example, the Abecedarian preschool program provided breakfast, lunch and an afternoon snack, prepared in consultation with a nutritionist.17 Current Head Start guidance requires programs to provide a substantial percentage of children’s daily nutritional needs with foods that are high in nutrients and low in fat, sugar, and salt.27 To cover the cost of meals and snacks, programs must participate in either the Child and Adult Care Food Program or the National School Breakfast or Lunch Programs and follow their nutritional requirements. One study found that children in Head Start had healthier eating patterns than low-income children in parental care,12 and another found that children in Head Start all day were less likely to be obese than children in Head Start part-day.28 Yet another study found that body mass index among children in Head Start stayed constant or declined during the school year, but rose during the summer.29
High-quality preschool may also provide more opportunities for daily exercise than low-income children would otherwise experience. The importance of diet and exercise for low-income children’s health is paramount. Like low-income adults, low-income children are at heightened risk for all features of metabolic syndrome, defined by abdominal obesity, dyslipidemia, insulin resistance, and high blood pressure.30
Experts recommend nutrient-rich foods for children that are low in saturated and trans fats and have little or no added sugars. Evidence suggests that infants’ and children’s taste preferences are shaped by early, repeated exposure to particular foods.31 Because a significant proportion of children’s meals may be provided at preschool, that setting may be used to promote healthy foods to influence not only children’s current diets but also their future food preferences.
Thus a novel question that bears examination is whether settings that expose children to new foods succeed in altering their preferences in the long term.
Further research is needed to assess the impact of high-quality public preschool on child eating and exercise habits. These studies should examine whether associations between health and exercise interventions at preschool and their desired outcomes vary by family income (or, more directly, by children’s exposure to nutrition and exercise promotion at home).
More sleep.
High-quality public preschool may afford opportunities to nap that low-income children would otherwise not have. Young low-income children are reported to have less consistent sleep schedules32 and spend less of their sleep time actually asleep33 than their more affluent peers.
Augmenting low-income children’s sleep through daytime naps may improve their health. Young children’s sleep duration and quality are associated with lower risks of obesity34 and injury35 and more optimal levels of insulin, cholesterol, and C-reactive protein.36
Research is needed to test the health-promotive value of increased sleep time through naps (as opposed to longer nighttime sleep) at preschool age. Some evidence suggests that mandatory naps at preschool result in shorter nighttime sleep duration, leading to calls for their elimination.37 On the other hand, naps may compensate for deficits in nighttime sleep for sleep-deprived children. There is clearly a need for more research on the effects of nap periods during the preschool year on the sleep habits of children, particularly those who are low-income.
Improved self-regulation.
High-quality preschool can improve children’s self-regulatory skills, such as attentional and inhibitory control. Specific features of the classroom that enhance child self-regulation include a positive emotional climate, a close student-teacher relationship, teacher modeling of self-regulation, and teacher coaching during stressful situations.38
Improvements in self-regulation may be particularly beneficial for low-income children, who tend to score lower than more affluent children on measures of self-regulation.39 Children in low-income families often have more chaotic home environments and are exposed to more stressors that may deplete their regulatory capacity.18
If high-quality preschool enhances low-income children’s self-regulatory skills, it may also improve their health. In the short term, children’s ability to control their behavior may reduce accidents that cause injuries. An evaluation of the Early Head Start program found that participants had fewer hospitalizations due to injuries or accidents compared to children not in the program.13
In the long term, self-regulatory skills may allow children to resist impulses to partake in dangerous behaviors such as smoking and high-fat eating. This pathway may explain the association found between participation in Head Start and a lower likelihood of smoking in adulthood.15 However, health behaviors may not fully mediate associations between self-regulation and health. In the New England Family Study, children who had better attention regulation skills at age 7 went on to score lower on cardiovascular risk in adulthood, but better diet and more physical activity did not mediate this association.40 It is possible that self-regulatory skills reflect (and/or influence) physiological processes that in and of themselves affect health. Research is needed to determine whether self-regulatory skills suppress the deleterious effects of stress on health, as reviewed above, or exert their own salubrious effects either directly on biophysiological functions or indirectly by facilitating healthy behaviors later in life.
Earlier detection of health problems.
Preschool teachers and other staff can detect children’s health problems, which might be particularly supportive to low-income children. Their parents struggle more with daily challenges (e.g., non-standard work schedules, budgeting) that drain attention and induce cognitive overload.41 Head Start is required to screen for cognitive, motor, language, and socioemotional delays and to arrange for vision and hearing screenings.27 Notably, Head Start also provides dental screenings, which may fulfill a vital function among low-income children, who have poorer oral health and receive less dental care than other children.42
In New York City’s universal pre-k program for 4-year-olds, providers must work with the City’s Office of School Health to conduct vision screenings. A recent evaluation found that children enrolled in pre-k were on average diagnosed with vision problems a year earlier than they would have been in the absence of pre-k.43 Pre-k enrollment also increased the chance that children diagnosed with a vision problem received treatment within six months. The ongoing expansion of public pre-k nationwide provides researchers with opportunities to study whether children who enroll in programs with similar mandates for screening receive earlier diagnosis and treatment than comparison children, and if so, whether this association varies by family income.
Healthier physical environment.
Low-income children are more likely than other children to live in homes with health hazards such as second-hand smoke, mold, lead, dust mites, and pest infestation.44,45 High-quality public preschools may provide an environment with fewer indoor air-and dust-born contaminants and allergens than their homes – and at the very least, decreasing exposure to secondhand smoke. However, research is needed to determine the degree to which a healthier school environment can improve health even when the home environment remains the same.
Mechanisms in the Mesosystem
Referrals to accessible medical care.
High-quality public preschool may provide low-income parents with referrals to local medical providers who are affordable and convenient. Head Start regulations require programs to assess whether children have a continuous and accessible source of health care and health insurance.27 If children do not have a regular source of health care or health insurance, the program helps parents obtain them. Providing appropriate referrals for low-income children should increase the likelihood that they will find a “medical home,” defined as an affordable, accessible, and family-centered site that provides primary care and coordinates all other aspects of pediatric care. Medical homes are associated with fewer unmet health and dental needs.46
Head Start programs are further charged with ensuring that enrolled children are up-to-date on well child and dental care visits. Programs must also track services received in response to any diagnosed delays or needed treatments. This may explain why in a national evaluation, children enrolled in Head Start were significantly more likely to receive dental care than children not in Head Start.14 On the other hand, they were not significantly more likely to have health insurance coverage. More research is needed to understand these seemingly contradictory findings.
Improved medication adherence.
Among selected children with chronic conditions requiring daily medication, nurses or other designated staff may regularly administer a prescription or over-the-counter medication as ordered by a health professional. With clear communication among medical providers, school personnel, and parents, medicine administration at preschool may improve adherence.
Medication adherence is associated with better disease management among preschoolers. Yet parents do not always adhere to daily medication protocols. In one study of preschoolers with asthma, parents’ self-reported adherence rate over the past week was 92%, while their actual rate was 57%.47 Additionally, parents may make mistakes while delivering medication to their children; medication errors rates are highest among preschoolers and the elderly.48 Medication adherence may be particularly challenging for parents whose time and attention are depleted by the daily hassles associated with financial hardship.41 Empirical studies are needed to test the propositions that low-income parents are less medication-adherent than other parents, and that their children benefit more from in-school medication administration.
Securing special needs services.
A high-quality public preschool should help the parents of children identified with potential health and developmental problems advocate for publicly-funded diagnostic testing. For children who receive a qualifying diagnosis, a high-quality public preschool should help parents apply to the local public agency administering the Individuals with Disabilities Education Act for an Individualized Education Program (IEP) so their child can receive special education services.
Assistance from preschool personnel can be crucial for low-income parents of children with suspected or known special needs. The high costs of testing and special education services often place them beyond the reach of even middle-income parents. Without publicly funded testing and services, low-income families may forego them altogether. The complicated application process and high thresholds for qualification can deter parents who have language barriers, lack the resources to challenge denials of service, or have inflexible jobs that make it difficult for them to call or meet with administrators and educators. One approach researchers interested in testing this mechanism might take is to capitalize on ongoing expansions of public pre-k by testing for regional correlations between growing pre-k participation and higher rates of IEP applications, especially from low-income parents.
Conclusion
The AAP urges pediatricians to coordinate patient care with early child care and education providers, offer consultations to local providers, and advocate for higher standards of quality.6 To that list may be added the call for participation in or support for research on the health impacts of high-quality public preschool, with a particular emphasis on the potential for narrowing early income-based disparities. The proposed model provides a roadmap for this research. Studies are needed to determine, first, whether the features of preschool proposed here improve child health in the short and long terms, and second, the degree to which such improvements are greater for children in low-income families than other families. The results of these studies may be used to refine the model over time.
The model will also need to be updated as we gain a greater understanding of how health determinants unfold over the life course. Research is needed on the features of high-quality preschool that directly affect biomarkers of health, as well as those features that exert an indirect effect via mediating factors such as health behaviors or access to health care. Mechanisms may vary across population subgroups and involve multiple cascading effects. For example, the Abecedarian program reduced boys’ BMI, which increased adult employment, which in turn improved health insurance coverage.17 Additional refinements of the model should account for pathways’ overlapping and perhaps even synergistic effects. For example, children’s sleep quantity may be boosted by daytime naps but its quality may also be enhanced by stress reduction, better nutrition, and more exercise. Further refinements may also identify subgroups of low-income children who are too sick or traumatized to benefit from the health-promotive features of high-quality public preschool.
It should also be acknowledged that the effects of high-quality public preschool may not, in the short term, be entirely salubrious. For example, preschool attendance may increase the incidence of respiratory illness relative to parental care.49 It seems likely, however, that in general this disadvantage is outweighed by the many routes through which high-quality preschool may improve children’s health.
Developmentalists and educators recognize the potential for high-quality public preschool to narrow early gaps in achievement associated with family income that, without intervention, persist over the life course. We call for pediatricians to consider the potential that high-quality public preschool may similarly narrow early and lifelong gaps in health status associated with family income.
Acknowledgments:
This study was supported by grants from the Heising-Simons Foundation (2016-107, 2017-329, 2018-1152), the Foundation for Child Development (GU-03-2017), the Spencer Foundation (201800034), and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (1R01HD092324-01A1). The authors thank Deborah Phillips, Diane Horm, and Anne Partika for their contributions. There are no conflicts of interest to declare.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Anne Martin, Independent Consultant, 237 West 11th Street, 4A, New York, NY 10014.
Anna D. Johnson, Department of Psychology, Georgetown University 303 White-Gravenor Hall, 37th and O Streets, NW, Washington, DC 20007.
Sherri Castle, Early Childhood Education Institute, University of Oklahoma – Tulsa, 4502 E. 41st Street, Room 4W-123, Tulsa, OK 74135.
References
- 1.Knudsen EI, Heckman JJ, Cameron JL, Shonkoff JP. Economic, neurobiological, and behavioral perspectives on building America’s future workforce. P Natl Acad Sci, 2006;103:10155–10162. doi: 10.1073/pnas.0600888103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Conti G, Heckman JJ. The developmental approach to child and adult health. Pediatrics, 2013;131:S133–141. doi: 10.1542/peds.2013-0252d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yoshikawa H, Weiland C, Brooks-Gunn J, et al. Investing in our Future: The Evidence Base on Preschool Education Ann Arbor, MI: Society for Research in Child Development; 2013. [Google Scholar]
- 4.Friedman-Krauss A, Bernstein S, Barnett WS. Early Childhood Education: Three Pathways to Better Health. Preschool Policy Update. New Brunswick, NJ: National Institute for Early Education Research; 2019. [Google Scholar]
- 5.Morrissey T The Effects of Early Care and Education on Children’s Health. Health Affairs Health Policy Brief. April 2019. doi: 10.1377/hpb20190325:519221 [DOI] [Google Scholar]
- 6.Donoghue EA AAP Council on Early Childhood. Quality early education and child care from birth to kindergarten. Pediatrics. 2017;140:e20171488. doi: 10.1542/peds2017-1488 [DOI] [PubMed] [Google Scholar]
- 7.Coley RL, Votruba-Drzal E, Collins M, DeMeo Cook K. Comparing public, private, and informal preschool programs in a national sample of low-income children. Early Child Res Q. 2016; 26:91–105. doi: 10.1016/j.ecrresq.2015.11.002 [DOI] [Google Scholar]
- 8.Friedman-Krauss AH, Barnett WS, Garver KA, et al. The State of Preschool 2018: State Preschool Yearbook. New Brunswick, NJ: National Institute for Early Education Research; 2019. [Google Scholar]
- 9.Bronfenbrenner U, Morris PA. (2006). The bioecological model of human development. In:Damon W, Lerner RM, eds. Handbook of Child Psychology, Vol. 1. Theoretical Models of Human Development 6th ed. New York, NY: Wiley; 2006:793–828. [Google Scholar]
- 10.Shonkoff JP. Building a new developmental framework to guide the future of early childhood policy. Child Dev. 2010;81:357–367. [DOI] [PubMed] [Google Scholar]
- 11.Alvidrez J, Castille D, Laude-Sharp M, Rosario A, Tabor D. The National Institute on Minority Health and Health Disparities research framework. Am J Public Health. 2019;109:S16–S20. doi: 10.2015/AJPH.2018.304883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee R, Zhai F, Han W-J, Brooks-Gunn J, Waldfogel J. Head Start and children’s nutrition, weight and health care receipt. Early Child Res Q. 2013;28:723–733. doi: 10.1016/j.ecresq.2013.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.U.S. Department of Health and Human Services. Making a Difference in the Lives of Infants and Toddlers and Their Families: The Impacts of Early Head Start. Vol 1: Final Technical Report. Washington, DC: Author; 2002. [Google Scholar]
- 14.U.S. Department of Health and Human Services, Administration for Children and Families. Head Start Impact Study Final Report. Washington, DC: Author; 2010. [Google Scholar]
- 15.Anderson KH, Foster JE, Frisvold DE. Investing in health: The long-term impact of Head Start on smoking. Econ Inq. 2010;48:587–602. doi: 10.1111/j.1465-7295.2008.00202.x [DOI] [Google Scholar]
- 16.Campbell F Conti G, Heckman JJ, et al. Early childhood investments substantially boost adult health. Science. 2014;343:1478–1485. doi: 10.1126/science.1248429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Conti G, Heckman J, Pinto R. The effects of two influential early childhood interventions on health and healthy behavior. Econ J. 2016;126:F28–F65. doi: 10.1111/ecoj.12420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stability Phillips D., security, and social dynamics in early childhood environments. In: Lesaux NK NK, Jones SM, eds. The Leading Edge of Early Childhood Education: Linking Science to Policy for a New Generation. Cambridge, MA: Harvard Education Press; 2016:7–28. [Google Scholar]
- 19.Evans GW, Eckenrode J, Marcynyszyn LA. Chaos and the macrosetting: The role of poverty and socioeconomic status. In: Evans GW, Wachs TD, eds. Decade of Behavior (Science Conference). Chaos and Its Influence on Children’s Development: An Ecological Perspective Washington, DC: American Psychological Association; 2010:225–238. [Google Scholar]
- 20.Evans GW, English K. The environment of poverty: Multiple stressor exposure, psychological stress, and socioemotional adjustment. Child Dev. 2002;73:1238–1248. doi: 10.1111/1467-8624.00469. [DOI] [PubMed] [Google Scholar]
- 21.Nusslock R, Miller GE. Early-life adversity and physical and emotional health across the lifespan: A neuroimmune network hypothesis. Biol Psychiat. 2016;80,23–32. doi: 10.1016/j.biopsych.2015.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bagby SP., Martin D, Chung ST, Rajapakse N. From the outside in: Biological mechanisms linking social and environmental exposures to chronic disease and to health disparities. Am J Public Health. 2018;109:S56–S63. doi: 10.2105/AJPH.2018.304864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vermeer HJ, van IJzendoorn MH. Children’s elevated cortisol levels at daycare: A review and meta-analysis. Early Child Res Q. 2006; 21:390–401. doi: 10.1016/j.ecresq.2006.07.004 [DOI] [Google Scholar]
- 24.Geoffroy M, Cote SM, Parent S, Seguin JR. Daycare attendance, stress, and mental health. Can J Psychiatry. 2006;51:607–615. [DOI] [PubMed] [Google Scholar]
- 25.Berry D, Blair C, Granger DA, The Family Life Project Key Investigators. Child care and cortisol across infancy and toddlerhood: Poverty, peers, and developmental timing. Fam Relat. 2016;65:51–72. doi: 10.1111/fare.12184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bhattacharya J, Currie J, Haider S. Poverty, food insecurity, and nutritional outcomes in children and adults. J Health Econ. 2004;23;839–862. doi: 10.1016/j.jhealeco.2003.12.008 [DOI] [PubMed] [Google Scholar]
- 27.Administration for Children and Families. Head Start Program Performance Standards: 45 CFR Chapter XIII. Washington, DC: U.S. Department of Health and Human Services, Administration for Children and Families, Office of Head Start; 2016. [Google Scholar]
- 28.Frisvold DE, Lumeng JC. Can increasing the daily duration of Head Start reduce childhood obesity? J Hum Resour. 2011;46;373–402. doi: 10.3368/jhr.46.2.273 [DOI] [Google Scholar]
- 29.Lumeng JC, Kaciroti N, Frisvold DE. Changes in body mass index Z score over the course of the academic year among children attending Head Start. Acad Pediatr. 2010;10:179–186. doi: 10.1016/j.acap.2010.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Howe LD, Galobardes B, Sattar N, et al. Are there socioeconomic inequalities in cardiovascular risk factors in childhood, and are they mediated by adiposity: Findings from a prospective cohort study. Int J Obesity. 2010; 34:1149–1159. DOI: 10.1038/IJO.2010.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maier A, Chabanet C, Schaal B. Effects of repeated exposure on acceptance of initially disliked vegetables in 7 month old infants. Food Qual Pref. 2007;18:1023–1032. [Google Scholar]
- 32.de Jong DM, Cremone A, Kurdziel LBF, et al. Maternal depressive symptoms and household income in relation to sleep in early childhood. Journal Pediatr Psychol. 2016;1:961–970. doi: 10.1093/jpepsy/jsw006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Acebo C, Sadeh A, Seifer R, et al. Sleep/wake patterns derived from activity monitoring and maternal report in healthy 1- to 5-year-old children. SLEEP. 2005;28:1568–1577 doi: 10.1093/sleep/28.12.1568 [DOI] [PubMed] [Google Scholar]
- 34.Jiang L, Yan SQ, Geng ML, et al. The associations between nighttime sleep duration, bedtime and preschool children’s obesity. Chinese J Prev Med. 2018; 6:1146–1151. doi: 10.3760/cma/j.assn.0253-9624.2018.11.010 [DOI] [PubMed] [Google Scholar]
- 35.Owens JA, Fernando S, McGuinn M. Sleep disturbance and injury risk in young children. Behav Sleep Med. 2010;3:18–31. doi: 10.1207/s15402010bsm0301_4 [DOI] [PubMed] [Google Scholar]
- 36.Spruyt K, Molfese DL, Gozal D. Sleep duration, sleep regularity, body weight, and metabolic homeostasis in school-aged children. Pediatrics. 2011;127: e345–e352. doi: 10.1542/peds.2010-0497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Staton SL, Smith SS, Thorpe KJ. “Do I really need a nap?”: The role of sleep science in informing sleep practices in early childhood education and care settings. Transl Issues Psych Sci. 2015;1:32–44. doi: 10.1037/tps0000011 [DOI] [Google Scholar]
- 38.Blair C, Raver CC. School readiness and self-regulation: A developmental psychobiological approach. Annu Rev Psychol. 2015;66:711–731. doi: 10.1146/annurev-psych-014814-015221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Evans GW, Rosenbaum J. Self-regulation and the income-achievement gap. Early Child Res Q. 2008;23:504–514. doi: 10.1016/j.ecresq.2008.07.002 [DOI] [Google Scholar]
- 40.Appleton AA, Buka SL, Loucks EB, et al. A prospective study of positive early life psychosocial factors and favorable cardiovascular risk in adulthood. Circulation. 2013;127: 905–912. doi: 10.1161/CIRCULATIONAHA.112.115782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mani A, Mullainathan S, Shafir E, Zhao J. Poverty impedes cognitive function. Science. 2013;341:976–980. doi: 10.1126/science.1238041 [DOI] [PubMed] [Google Scholar]
- 42.Edelstein BL. Access to dental care for Head Start enrollees. J Public Health Dent. 2000;60:221–229. doi: 10.1111/j.1752-7325.2000.tb03332.x [DOI] [PubMed] [Google Scholar]
- 43.Hong K, Dragan K, Glied S. Seeing and hearing: The impacts of New York City’s universal pre-kindergarten program on the health of low-income children. J Health Econ. 2019;64:93–107. doi: 10.1016/j.healeco.2019.01.004 [DOI] [PubMed] [Google Scholar]
- 44.Tsai J, Homa DM, Gentzke AS, et al. Exposure to secondhand smoke among nonsmokers – United States, 1988–2014. MMWR-Morbid Mortal W. 2018;67:1342–1346. doi: 10.15585/mmwr.mm6748a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wheeler W, Brown MJ. Blood lead levels in children aged 1–5 years – United States, 1999–2010. MMWR-Morbid Mortal W. 2013;62:245–248. [PMC free article] [PubMed] [Google Scholar]
- 46.Strickland B, McPherson M, Weissman G, van Dyck P, Huang ZJ, Newacheck P. Access to the medical home: Results of the National Survey of Children with Special Health Care Needs. Pediatrics. 2004;113:1485–1492. [PubMed] [Google Scholar]
- 47.Armstrong ML, Duncan CL, Stokes JO, Pereira D. Association of caregiver health beliefs and parenting stress with medication adherence in preschoolers with asthma. J Asthma. 2014;51:366–372. doi: 10.3109/02770903/2013/876431 [DOI] [PubMed] [Google Scholar]
- 48.Mira JJ, Lorenzo S, Guilabert M, Navarro I, Perez-Jover V. A systematic review of patient medication error on self-administering medication at home. Expert Opinion on Drug Safety. 2015;14:815–838. doi: 10.1517/14740338.2015.1026326 [DOI] [PubMed] [Google Scholar]
- 49.Bradley RH, National Institute of Child Health and Human Development (NICHD) Early Child Care Research Network. Child care and common communicable illnesses in children aged 37 to 54 months. Arch Pediatr Adol Med. 2003;157:196–200. doi: 10.1001/archpedi.157.2.196 [DOI] [PubMed] [Google Scholar]


