Abstract
Purpose
Although there are many articles about single incision laparoscopic (SIL) hernioplasty, a large-scale study or article about its long-term outcome has not been reported yet. The aim of this study is to assess short- and long-term outcomes of SIL totally extraperitoneal (TEP) hernia repair with large number of cases.
Methods
A prospectively collected database containing details of 1,231 procedures in 1,129 consecutive patients who underwent SIL-TEP hernia repair between June 2010 and December 2017 at a single institution was retrospectively analyzed. SIL-TEP hernia repair was performed using a glove single port device and standard laparoscopic instruments. Recurrence rate of SIL-TEP hernia repair was analyzed by a telephone questionnaire.
Results
Among 1,129 patients, 1,027 (91.0%) had unilateral hernia and 102 (9.0%) had bilateral hernia. There were 12 (1.1%) conversions to single or 3 ports laparoscopic transabdominal preperitoneal hernioplasty or Lichtenstein repair. Mean operative time was 40.3 minutes for unilateral hernia and 61.6 minutes for bilateral hernia. Intraoperative complication rate was 21.8%. Most intraoperative complications were peritoneum or sac tearing (20.1%). Postoperative complications occurred in 97 (8.6%) cases, most of which were minor morbidity except for 1 mesh infection. Five-year recurrence rate was 4%.
Conclusion
SIL-TEP hernia repair is safe and technically feasible with acceptable short- and long-term outcomes. Large-scale randomized controlled trials comparing SIL-TEP hernia repair with conventional laparoscopic TEP are needed to confirm these results.
Keywords: Inguinal hernia, Laparoscopy
INTRODUCTION
Tension-free hernioplasty with mesh has become the gold standard procedure for inguinal hernia repair. Many advances have been made in the field of hernia surgery [1]. With advancement in laparoscopic inguinal hernia repair, less pain and faster recovery than before are now possible [2,3]. Most importantly, laparoscopic surgery has made it feasible to use a posterior approach with minimally invasive methods. The advantage of the posterior approach is that it enables more accurate identification of the hernia and placement of a larger mesh in more stable position to cover enough of the myopectineal orifice than the anterior approach.
Single incision laparoscopic (SIL) totally extraperitoneal (TEP) hernia repair can provide potential benefits of faster recovery, less pain, and better cosmetic outcome than conventional laparoscopic (CL) TEP hernia repair while maintaining advantages of posterior approach in inguinal hernia repair. Because of these potential advantages, there have been several reports on SIL surgery (SILS) approach in hernia surgery, showing that it has similar short-term outcome to conventional laparoscopic approach. However, most reports have limited number of cases [4]. In addition, long-term outcome of SIL-TEP hernia repair has not been reported yet.
Therefore, the objective of this study was to determine the safety and feasibility of SIL-TEP hernia repair using a large number of cases and assess its short- and long-term outcomes.
METHODS
A prospectively collected database containing details of 1,231 procedures in 1,129 consecutive patients who underwent SIL-TEP hernia repair between June 2010 and December 2017 at Incheon St. Mary's Hospital affiliated with The Catholic University of Korea was retrospectively analyzed. All patients with inguinal hernia who were admitted to our institute were considered for laparoscopic TEP hernia repair. Exclusion criteria were as follows: (1) patients under 20 years of age, (2) emergent situation such as acutely bowel incarcerated hernia, (3) previous retroperitoneal surgery such as recurrent hernia after laparoscopic hernia repair or prostatectomy, and (4) patients with compromised cardiopulmonary function. For these cases, open hernia repair was performed under local anesthesia. All operations were performed by a single experienced laparoscopic surgeon (KJH) or junior surgeons under supervision of KJH. During the study period, all TEP hernia repairs were performed with a SIL surgery. Postoperatively, patients visited the outpatient department between postoperative day 7 and day 10. If there was no morbidity, treatment was terminated. However, patients with complications had to revisit the outpatient department until the morbidity was resolved.
From July 2018 to September 2018, a telephone questionnaire was attempted to 1,129 patients. Patients were asked the following questions: (1) “Do you have any protrusions in your inguinal area during activity or when you apply abdominal pressure?” and (2) “If so, how long has it been since the operation?” Patients with suspected recurrence at the time of the question were asked to visit the hospital.
All surgeries were performed after obtaining informed consent from patients. This study was approved by Institutional Review Board of Incheon St. Mary's Hospital (No. OC19RESI0125).
Surgical techniques
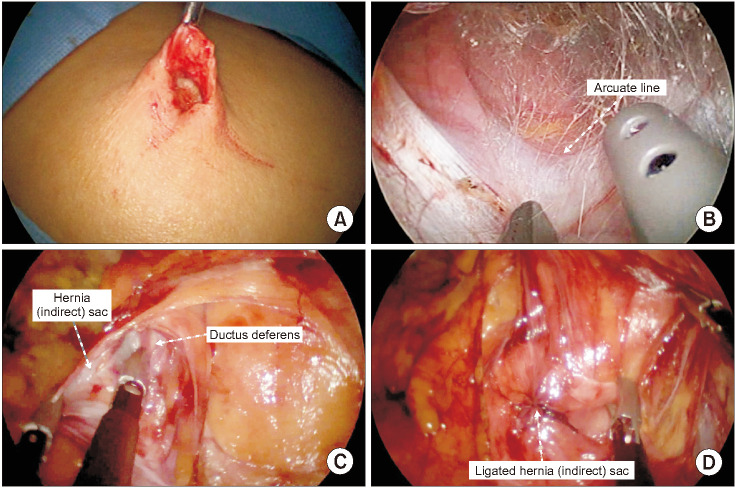
Several skin incisions were used during the early period of this study. In 30 early cases, we used oblique incision to hernia site. After then, we used midline incision, beginning from the deepest part of the umbilicus and extending 0.5–1.5 cm from the umbilicus. But after early 250 cases, almost all patients underwent totally intraumbilical incision because of cosmetic effect (Fig. 1A). The subcutaneous layer of hernia site was dissected down to the anterior rectus sheath and incised transversely. After pulling the rectus muscle laterally, homemade glove single port device was inserted in front of the posterior rectus sheath. A 5 mm rigid 30° laparoscope was used. A preperitoneal dissection was performed using spreading-out technique from umbilicus with conventional instruments (Fig. 1B). After completion of preperitoneal dissection, sac isolation (Fig. 1C) and reduction or amputation were performed. And then, parietalization (Fig. 1D) and mesh positioning were performed. In terms of management of hernia sac, high ligation was performed for most indirect hernias regardless of sac amputation. For direct, femoral, or obturator hernia, we did not perform high ligation of sac. For such cases, only reduction was performed. Initially, several types of mesh were used. However, 15 by 10 cm lightweight polypropylene mesh was used for most cases. Two tacks were used. One was placed in Cooper's ligament and the other was placed in the anterolateral abdominal wall. The anterior rectus sheath was closed with continuous 2-0 vicryl sutures. The skin incision was closed with subcuticular sutures.
Fig. 1. Procedures for single incision laparoscopic totally extraperitoneal hernia repair. (A) Total ly int raumbi l ical skin incision and dissection of subcutaneous tissue. (B) Preperitoneal dissection with conventional instruments. (C) Procedures for sac isolation. (D) Procedures for parietalization.
Statistical analysis
Statistical analysis was performed with R Statistical software ver. 4.0.0 (Foundation for Statistical Computing, Vienna, Austria). Statistical analyses between the 2 groups were by the independent t-test, chi-square test, and Fisher exact test. The P-values of <0.05 were considered to be statistically significant.
RESULTS
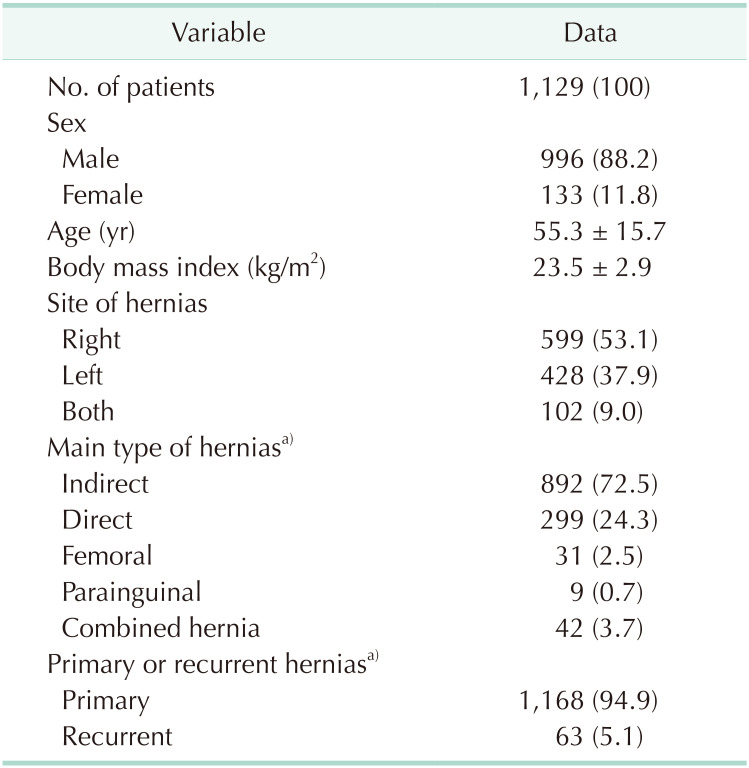
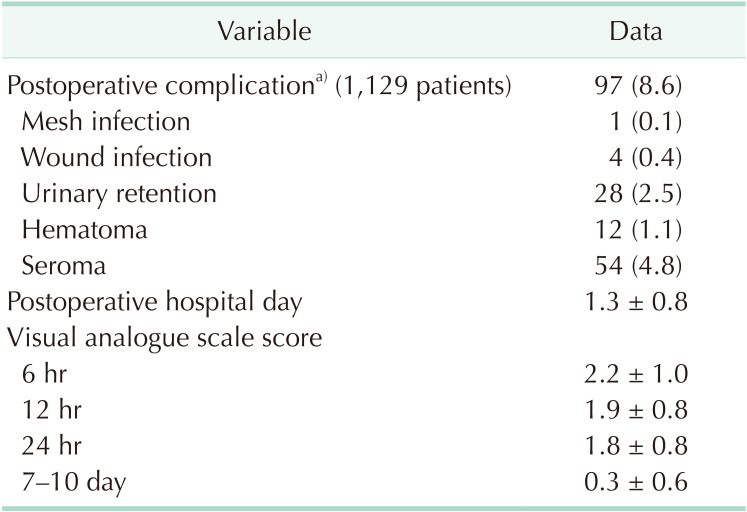
Patient demographics and hernia characteristics are summarized in Table 1. A total of 1,231 hernias (1,027 unilateral hernias and 102 bilateral hernias) in 1,129 patients were repaired during the study period. Of these 1,129 patients, 996 were males and 133 were females. Their average age was 55.3 years. Their mean body mass index was 23.5 kg/m2. There were 5 types of hernia identified during the operation; indirect, direct, femoral, obturator, and parainguinal. Parainguinal hernia was defined as unusual case that did not fit the definition of the remaining 4 hernias. Combined hernia was defined as any combination of 5 types of hernia. There were 42 combined hernias (3.7%). There was no solitary obturator hernia in this study. Therefore, there were 4 main hernia types in the present study, with indirect hernia being the most common type (72.5%). There were 63 recurrent hernias (5.1%).
Table 1. Patient demographics and hernia characteristics.
Values are presented as number (%) or mean ± standard deviation.
a)1,231 procedures.
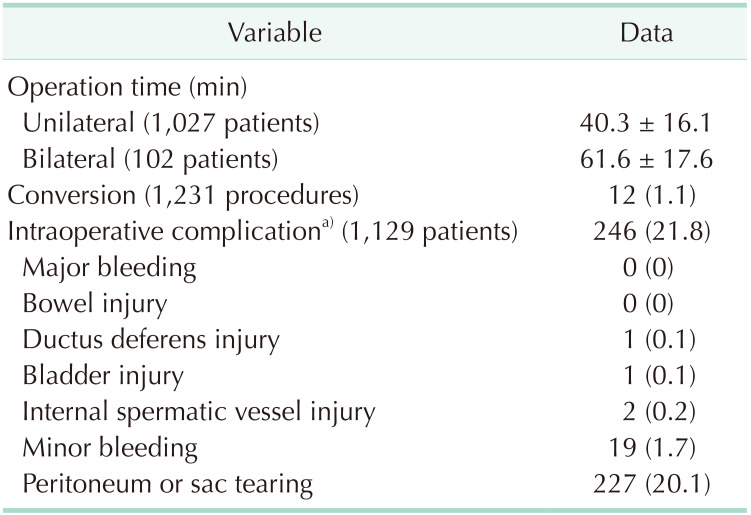
The mean operative time was 40.3 minutes for unilateral hernia and 61.6 minutes for bilateral hernia (Table 2). There were 12 cases of conversion. Six cases were converted to laparoscopic transabdominal preperitoneal (TAPP) hernia repair (4 conventional TAPP and 2 SILS-TAPP) and 6 cases were converted to open hernia repair. The reason for conversion was instability of operation field in case of omental incarceration followed by large sac tearing for all cases. Intraoperative complication was defined as any unintended event that affected operative procedures. A total of 250 intraoperative complications occurred in 246 patients. The intraoperative complication rate was 21.8%. The majority (227 of 250, 90.8%) of intraoperative complications were unintentional tearing of peritoneum or hernia sac. In the case of large tearing, repair was done using a clip or suture. In the case of small tearing, no action was taken. Minor bleeding such as bleeding from branches of inferior epigastric vessels or vessels on pubic bone requiring clipping or compression occurred in 19 patients. There was no major bleeding due to injury of external iliac or main inferior epigastric vessels that required blood transfusion. There was no bowel injury either. An inadvertent transection of vas deferens during hernia sac dissection occurred in a 62-year-old patient. The transected vas deferens was ligated by prior consent. There was 1 bladder injury, for which suture repair was performed during surgery. No morbidity occurred. There were 2 cases of a complete transection of internal spermatic vessels without ischemic orchitis.
Table 2. Operative data.
Values are presented as mean ± standard deviation or number (%).
a)250 events in 246 patients.
The postoperative complication rate was 8.6% (Table 3). All morbidities (except one mesh infection) were resolved without surgical intervention. In case of mesh infection, the patient was transferred to another hospital according to his will. There were 4 superficial incisional surgical site infections on umbilicus. They were solved by dressing in the outpatient department. All urinary retention occurred immediately after surgery. There was no long-term bladder dysfunction. In case of seroma and hematoma, percutaneous aspiration was performed by surgeon's judgment. Postoperative pain scores at 24 hours and at 7–10 days were 1.8 and 0.3, respectively.
Table 3. Short-term results.
Values are presented as number (%) or mean ± standard deviation.
a)99 events in 97 patients.
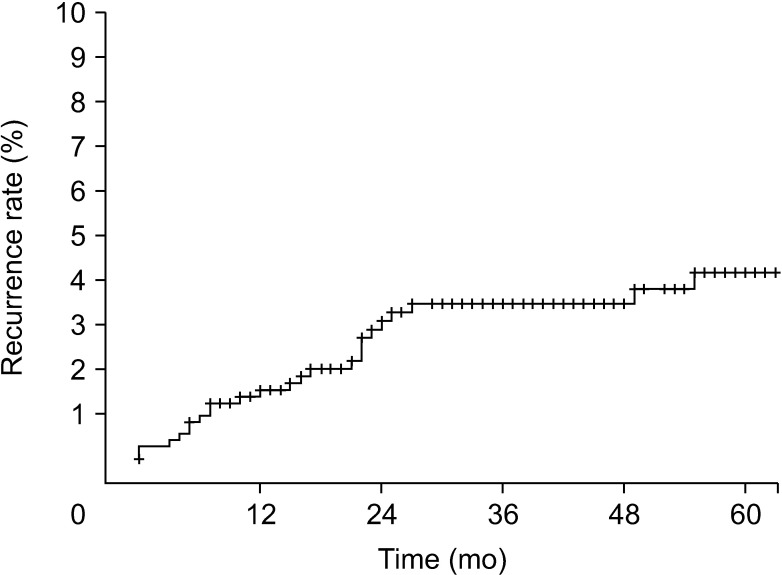
Fig. 2 shows recurrence rate. Of 1,129 patients, 22 revisited the outpatient department voluntarily because of recurrence. Telephone call was attempted for the remaining 1,107 patients. Telephone questionnaires could only be made for 636 patients (57.5%). Six additional recurred patients were found from the telephone questionnaire. However, despite of our request, none of these 6 patients visited the hospital. We considered these 6 patients to have recurrence in this study. Thus, there were 28 recurrences among 658 patients. The median follow-up duration was 42 months. The 5-year recurrence rate was 4%.
Fig. 2. Recurrence rate.
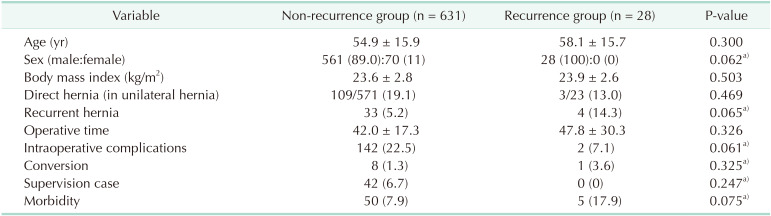
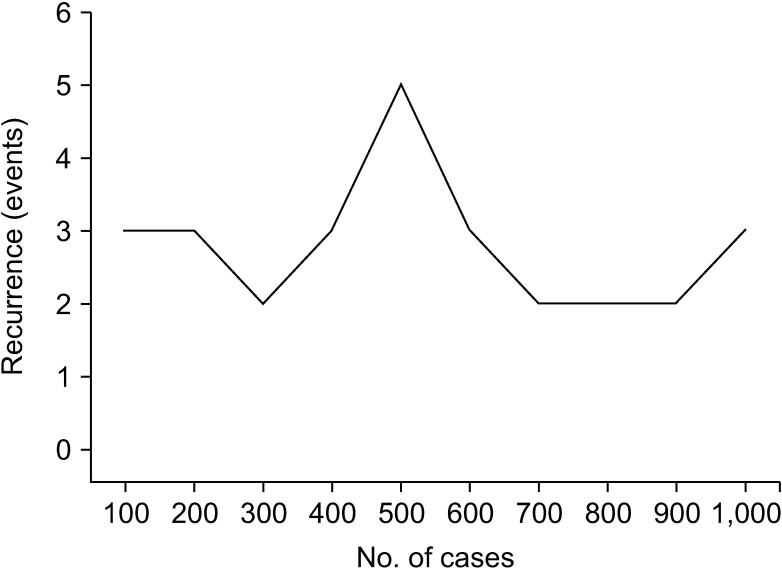
There was no significant difference in hernia characteristics and operative outcomes between non-recurrence (n = 631) and recurrence (n = 28) groups (Table 4). The rate of direct hernia did not differ (19.1% vs. 13.0%, P = 0.469) between the 2 groups either. There was a tendency for more recurrent hernia in the recurrence group (14.3% vs. 5.2%, P = 0.065). However, the difference between the 2 groups was not statistically significant. There was no recurrence in any of 42 supervision cases. In terms of recurrence rate according to the number of procedures, recurrence did not show a tendency to decrease with increasing number of procedures (Fig. 3).
Table 4. Comparison between non-recurrent and recurrent cases.
Values are presented as mean ± standard deviation or number (%).
a)Analyzed by Fisher exact test.
Fig. 3. Recurrence according to the number of cases.
DISCUSSION
Many types of hernia surgery have been developed by many surgeons over the last century. However, many of these techniques are no longer well-practiced. The main reason was due to their high recurrence rate. SIL-TEP hernia repair is a surgical method relatively recently developed for hernias. Although many studies have reported short-term results of SIL-TEP hernia repair, its long-term results have not been reported yet. Thus, the present study is meaningful in that it is the first study to report long-term outcomes of SIL-TEP hernia repair.
In addition, it is necessary to prove that SIL-TEP hernia repair is not inferior to previous procedures before revealing merits of this new technique. However, this study did not compare short-term and long-term outcomes between SIL-TEP and CL-TEP hernia repair. Thus, it could not directly prove that SIL-TEP hernia repair is not inferior to CL-TEP hernia repair. However, this is the largest scale study on SIL-TEP hernia repair up to date. Results of this study could be compared with results of already published study on CL-TEP hernia repair. Therefore, this study can be used as an evidence for future randomized controlled studies.
First, safety and short-term outcome of SIL-TEP hernia repair can be identified through intraoperative complication and postoperative morbidity. In terms of safety, intraoperative complication rate was 21.8% in this study. Most complications were peritoneum or sac tearing and minor bleeding that did not result in postoperative morbidity. The peritoneum or sac tearing rate has been reported to be 10%–47% in the previous study about CL-TEP hernia repair [5,6,7]. The peritoneum and sac tearing rate of SIL-TEP hernia repair was 20.1% in this study. It is considered to be not high compared to the CL-TEP hernia repair. In this study, minor bleeding risk was 1.7% as compared to 2.75% in other studies for CL-TEP hernia repair, it is considered comparable result [5]. The rate of inferior epigastric vessel injury has been reported from 0.3% to 0.6%, but in this study, there was no inferior epigastric vessel injury [5,8,9,10]. Major intraoperative complications that could result in postoperative morbidity occurred in only 4 patients (0.3%). Such rate was lower compared to that in other studies (1%–2.5%) [8,11].
In this study, conversion rate was 1.1%, comparable to the conversion rate in previous studies (0.4%–1.8%) [8,11,12]. However, the reason for conversion might be more important than conversion rate itself. All conversion cases were not due to major intraoperative complications in the present study, but due to difficult and complicated hernias. If the procedure did not go well but surgeons could convert it to other procedures flexibly, it would mean that the procedure was safe. A home-made single port was used in this study. Such home-made single port can be easily converted to 3-port TEP or 3-port TAPP.
In terms of short-term outcome, the postoperative complication rate was 8.6%. However, most cases were minor complications. Morbidity that needed reoperation occurred in only 1 case (0.1%) of mesh infection, similar to results of other studies [13]. Previous studies about CL-TEP hernia repair have reported that the morbidity rate was 0.64%–16.6%, it is believed that the morbidity rate of this study was comparable [8,9,13]. It has been reported 8%–22% for seroma and hematoma in previous studies about CL-TEP hernia repair [5,9,10,14,15] and 5.9% in this study. In terms of urinary retention, previous studies about CL-TEP hernia repair have reported 0.2%–22% [5,9,10,12] and 2.5% in this study. In terms of postoperative pain, the visual analogue scale score was 1.8 at 24 hours postoperatively, similar to other studies about CL-TEP hernia repair [16].
In terms of long-term outcomes, the 5-year recurrence rate was 4% in this study. Recently, there have been 2 reports showing that the use of heavyweight mesh in CL-TEP hernia repair is better for recurrence than lightweight mesh [17,18]. However, our study was performed before the publication of these studies, lightweight meshes were used in most cases during the study period. Recurrence rates using lightweight mesh were 3.8% and 4% in these 2 reported studies, similar to the recurrence rate (4%) in the present study. However, the recurrence rate in the present study was slightly higher than that reported in previous studies about CL-TEP hernia repair [8,11,19].
This study has some limitations. First, it was not a planned prospective trial, 470 of 1,106 patients (42.5%) were unable to answer telephone questionnaire. Since most recurrent patients (22 of 28) voluntarily visited the hospital before the telephone questionnaire and only 6 patients were diagnosed with recurrence by telephone questionnaire (0.94%), the possibility of finding additional recurrence among unconnected people would be 4.4 people arithmetically. If telephone questionnaire was available for all patients, the actual recurrence rate could have fallen by as much as 2.7%. Thus, the actual recurrence rate might be lower. Although patients reported having recurrence over the telephone had subjective symptoms, they were not diagnosed by surgeon's examination. There might be bias because it is a subjective statement of patient. Another limitation of this study was that there might be error in recurrence rate. However, this study is meaningful as it is the first study to report recurrence rate of SIL-TEP hernia repair using a large number of cases.
Factors affecting recurrence include the type of procedure, the type of hernia, and the size of hernia defect. In this study, direct hernia and recurrent hernia were analyzed as possible risk factors for recurrence. They failed to show significant effect. Another limitation of this study was that defect size of hernia was not measured. It might act as a bias in this study.
In addition, this study showed that SIL-TEP hernia repair could be safely performed by surgical trainees and surgeons during learning period in term of recurrence. There was no recurrence in 42 cases of surgical trainees under supervision. When the recurrence rate was evaluated by the increase by experience, the recurrence rate did not increase in initial period. The single experienced laparoscopic surgeon (KJH) whose experience includes over 100 cases of CL-TEP hernia repair and more than 70 cases of single port laparoscopic appendectomy before starting first SIL-TEP hernia repair.
In summary, this study has the following limitations. First, it was retrospective study. Second, there was bias in the analysis of the long-term outcome. Third, SIL-TEP hernia repair was not directly compared to CL-TEP hernia repair.
In conclusion, SIL-TEP hernia repair is a safe and feasible procedure with acceptable short- and long-term outcomes. Thus, it might be a good option for hernia repair. However, large-scale randomized controlled trials comparing SIL-TEP hernia repair with CL-TEP hernia repair are needed to confirm these results.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
- Conceptualization: YJL, JHK.
- Formal Analysis: YJL, JHK.
- Investigation: All authors.
- Methodology: All authors.
- Project Administration: YJL, JHK.
- Writing — Original Draft: YJL, JHK.
- Writing — Review & Editing: All authors.
References
- 1.Lichtenstein IL, Shulman AG, Amid PK, Montllor MM. The tension-free hernioplasty. Am J Surg. 1989;157:188–193. doi: 10.1016/0002-9610(89)90526-6. [DOI] [PubMed] [Google Scholar]
- 2.Corbitt JD., Jr Laparoscopic herniorrhaphy. Surg Laparosc Endosc. 1991;1:23–25. [PubMed] [Google Scholar]
- 3.Bullen NL, Massey LH, Antoniou SA, Smart NJ, Fortelny RH. Open versus laparoscopic mesh repair of primary unilateral uncomplicated inguinal hernia: a systematic review with meta-analysis and trial sequential analysis. Hernia. 2019;23:461–472. doi: 10.1007/s10029-019-01989-7. [DOI] [PubMed] [Google Scholar]
- 4.Perivoliotis K, Tzovaras G, Sarakatsianou C, Baloyiannis I. Current status of single-port versus multi-port approach in laparoscopic inguinal hernia mesh repair: an up-to-date systematic review and meta-analysis. Hernia. 2019;23:217–233. doi: 10.1007/s10029-018-01876-7. [DOI] [PubMed] [Google Scholar]
- 5.Lau H, Patil NG, Yuen WK, Lee F. Management of peritoneal tear during endoscopic extraperitoneal inguinal hernioplasty. Surg Endosc. 2002;16:1474–1477. doi: 10.1007/s00464-001-8299-z. [DOI] [PubMed] [Google Scholar]
- 6.Knook MT, Weidema WF, Stassen LP, van Steensel CJ. Endoscopic total extraperitoneal repair of primary and recurrent inguinal hernias. Surg Endosc. 1999;13:507–511. doi: 10.1007/s004649901023. [DOI] [PubMed] [Google Scholar]
- 7.Liem MS, van der Graaf Y, van Steensel CJ, Boelhouwer RU, Clevers GJ, Meijer WS, et al. Comparison of conventional anterior surgery and laparoscopic surgery for inguinal-hernia repair. N Engl J Med. 1997;336:1541–1547. doi: 10.1056/NEJM199705293362201. [DOI] [PubMed] [Google Scholar]
- 8.Dulucq JL, Wintringer P, Mahajna A. Laparoscopic totally extraperitoneal inguinal hernia repair: lessons learned from 3,100 hernia repairs over 15 years. Surg Endosc. 2009;23:482–486. doi: 10.1007/s00464-008-0118-3. [DOI] [PubMed] [Google Scholar]
- 9.Tamme C, Garde N, Klingler A, Hampe C, Wunder R, Köckerling F. Totally extraperitoneal inguinal hernioplasty with titanium-coated lightweight polypropylene mesh: early results. Surg Endosc. 2005;19:1125–1129. doi: 10.1007/s00464-004-8219-0. [DOI] [PubMed] [Google Scholar]
- 10.Weiser HF, Klinge B. Endoscopic hernia repair–experiences and characteristic features. Viszeralchirurgie-Stuttgar. 2000;35:316–320. [Google Scholar]
- 11.Ramshaw B, Shuler FW, Jones HB, Duncan TD, White J, Wilson R, et al. Laparoscopic inguinal hernia repair: lessons learned after 1224 consecutive cases. Surg Endosc. 2001;15:50–54. doi: 10.1007/s004640001016. [DOI] [PubMed] [Google Scholar]
- 12.Felix EL, Michas CA, Gonzalez MH., Jr Laparoscopic hernioplasty: TAPP vs TEP. Surg Endosc. 1995;9:984–989. doi: 10.1007/BF00188456. [DOI] [PubMed] [Google Scholar]
- 13.Moon V, Chaudry GA, Choy C, Ferzli GS. Mesh infection in the era of laparoscopy. J Laparoendosc Adv Surg Tech A. 2004;14:349–352. doi: 10.1089/lap.2004.14.349. [DOI] [PubMed] [Google Scholar]
- 14.Bobrzynski A, Budzynski A, Biesiada Z, Kowalczyk M, Lubikowski J, Sienko J. Experience: the key factor in successful laparoscopic total extraperitoneal and transabdominal preperitoneal hernia repair. Hernia. 2001;5:80–83. doi: 10.1007/s100290100004. [DOI] [PubMed] [Google Scholar]
- 15.Koch CA, Grinberg GG, Farley DR. Incidence and risk factors for urinary retention after endoscopic hernia repair. Am J Surg. 2006;191:381–385. doi: 10.1016/j.amjsurg.2005.10.042. [DOI] [PubMed] [Google Scholar]
- 16.Cardinali L, Mazzetti CH, Cadenas Febres A, Repullo D, Bruyns J, Dapri G. Prospective randomized study comparing single-incision laparoscopic versus multi-trocar laparoscopic totally extraperitoneal (TEP) inguinal hernia repair at 2 years. Surg Endosc. 2018;32:3262–3272. doi: 10.1007/s00464-018-6045-z. [DOI] [PubMed] [Google Scholar]
- 17.Roos MM, Bakker WJ, Schouten N, Voorbrood CE, Clevers GJ, Verleisdonk EJ, et al. Higher recurrence rate after endoscopic totally extraperitoneal (TEP) inguinal hernia repair with ultrapro lightweight mesh: 5-year results of a randomized controlled trial (TULP-trial) Ann Surg. 2018;268:241–246. doi: 10.1097/SLA.0000000000002649. [DOI] [PubMed] [Google Scholar]
- 18.Melkemichel M, Bringman S, Widhe B. Lower recurrence rate with heavyweight mesh compared to lightweight mesh in laparoscopic totally extra-peritoneal (TEP) repair of groin hernia: a nationwide population-based register study. Hernia. 2018;22:989–997. doi: 10.1007/s10029-018-1809-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eklund AS, Montgomery AK, Rasmussen IC, Sandbue RP, Bergkvist LA, Rudberg CR. Low recurrence rate after laparoscopic (TEP) and open (Lichtenstein) inguinal hernia repair: a randomized, multicenter trial with 5-year follow-up. Ann Surg. 2009;249:33–38. doi: 10.1097/SLA.0b013e31819255d0. [DOI] [PubMed] [Google Scholar]