Abstract
Background/Aims
Adolescents who identify as nonbinary gender or as not heterosexual report higher levels of mental illness than their counterparts. Cannabis use is a commonly employed strategy to cope with mental illness symptoms among adolescents; however, cannabis use can have many deleterious health consequences for youth. Within the frame of minority stress theory, this study investigates the relationships between gender identity and sexual orientation, internalizing disorder symptoms, and cannabis use among adolescents.
Method
A national cross-sectional survey of a generalizable sample of high school students in Canada from the 2017 wave (N = 15,191) of the Cancer Risk Assessment in Youth Survey was analyzed in spring 2019. Mediation analyses were completed to examine risk of internalizing disorder symptoms as a potential mediator of the association between (1) gender identity and (2) sexual orientation, and cannabis use.
Results
Indirect effects in all models show significantly higher levels of reported internalizing disorder symptoms for female (OR = 3.44, 95% CI [2.84, 4.18]) and nonbinary gender (OR = 3.75, 95% CI [2.16, 6.51]) compared with male students. Sexual minority adolescents had higher odds of internalizing disorder risk relative to non–sexual minority adolescents (OR = 3.13, 95% CI [2.63, 3.74]). Students who reported higher rates of internalizing disorder symptoms were more likely to have ever used cannabis. Patterns of partial mediation are also present among all groups.
Discussion/Conclusions
Findings can be used to better inform mental health interventions for adolescents. Future study should explore specific mental health stressors of vulnerable adolescent groups with respect to cannabis use as a coping mechanism.
Keywords: adolescent, cannabis, gender, mental health, sexual orientation
Globally, anxiety and mood disorders are the most prevalent health conditions (Whiteford et al., 2015). Legal therapeutic cannabis use is a common coping strategy for affected individuals due to its potential to improve sleep (Walsh et al., 2017), regulate moods (Hill et al., 2009), and serve as an alternative to addictive opiates for pain reduction (Lucas & Walsh, 2017). However, cannabis is also the most widely used illicit drug in the world among both the general population (World Health Organization, 2010) and adolescents (United Nations Office on Drugs and Crime, 2018). Adolescent cannabis use may put youth at a greater risk for developing future mental health disorders (Malone et al., 2010; Substance Abuse and Mental Health Services Administration & Center for Behavioral Health Statistics and Quality, 2013). There is also growing concern that exposure to cannabis during adolescence can have a variety of harmful effects in the maturing brain (Giedd et al., 1999; Gilman et al., 2014; Lenroot & Giedd, 2006). In Canada, these issues are particularly concerning as the nation has the highest prevalence of adolescent cannabis use in the developed world (Currie et al., 2012)—almost one in four adolescents aged 15 to 17 years has consumed cannabis at least once in their lifetime (Rotermann & Langlois, 2015).
Mental Health and Cannabis
Several links between adolescent cannabis use and mental illness exist. Early cannabis use has been associated with schizophrenia risk (Shapiro & Buckley-Hunter, 2010), depressive symptoms (Degenhardt et al., 2003; Moore et al., 2007), depression (Meier et al., 2016), and other mood disorders (Patton et al., 2002; Rubino et al., 2012). Frequent adolescent cannabis use has also been linked to increased risk of developing psychotic symptoms such as early onset psychosis (Casadio et al., 2011; Wilkinson et al., 2014) and paranoia (Griffith-Lendering et al., 2013). Perhaps most concerning is the connection between adolescent cannabis use and a heightened proclivity for suicidal behaviors (Cho et al., 2007; Hockenberry et al., 2010; Patton et al., 2002). Cannabis use during these important developmental years has many potential adverse consequences and can contribute to long-term issues such as deficits in individual cognitive and executive functioning, including decision making, memory, problem solving, and sustained attention (Fontes et al., 2011; Lisdahl et al., 2014; Tapert et al., 2007).
Internalizing Disorders
Internalizing disorders are characterized by inward expressions of distress and are typically linked with anxiety and mood disorders (e.g., major depressive disorder see Cosgrove et al., 2011). Anxiety and depression are two of the most common disorders among young people, globally, with the former being estimated to affect between 4% and 20% of children and adolescents (Martin & Volkmar, 2007) and the latter around 2% to 8% of children and adolescents (Hazell, 2009). Moreover, internationally, depression is a leading cause of disability (World Health Organization, 2018). These internalizing disorders can begin early on during childhood and can negatively affect an individual’s relationships, development, and daily functioning (Whalen et al., 2017). In the longer term, such disorders may lead to functional impairment (Rapee et al., 2009), an increased risk for suicide (Gould et al., 1998), and substance abuse issues (Compton et al., 2002). Overall, internalizing disorders possess the ability to create high-societal burdens (Konnopka et al., 2009).
Gender and Sexuality and Cannabis Use
Notable gender differences in cannabis use among adolescents also exist. Adolescent boys, compared with girls, initiate cannabis use earlier (Moss et al., 2014; Swahn et al., 2011). They are also more likely to engage in cannabis use (Goncy & Mrug, 2013; Leatherdale et al., 2007; Lee-Winn et al., 2018), and report being subject to fewer parental controls and monitoring (Laird et al., 2008; Webb et al., 2002). Findings are less clear with respect to cannabis use being a significant factor for predicting suicide planning or personal endorsement of suicide among boys compared with girls as some study suggests (Cho et al., 2007), while other literature has noted this trend among both groups (Swahn et al., 2011). While research on gender minority (i.e., any noncisgender identity) youths is still emerging (Austin, 2016), initial study has found that transgender adolescents have relatively higher levels of cannabis use compared with their peers (Clark et al., 2018). Similar trends also highlight that transgender youths have an increased likelihood for early onset use and exhibit more recent usage patterns than their nontransgender counterparts (Day et al., 2017). Conversely, though, high-quality relationships, connectedness to parents, development opportunities (Gower et al., 2018), and living in areas with more community support (e.g., community events, youth organizations providing specific services; Eisenberg et al., 2020) have all been linked to reduced odds of substance use among transgender and gender diverse youth. Noting these developments, recent studies have called for more inquiry into examining the role and influence of different gender identities in cannabis use in future analyses (Bassir Nia et al., 2018; Sherman et al., 2016).
In addition to gender differences, differences in adolescent cannabis use by sexual orientation have also been observed: adolescents who identify as lesbian, gay, bisexual, transgender, and queer (LGBTQ) are at higher risk for substance use and disorders when compared with their heterosexual counterparts (Corliss et al., 2010; Watson et al., 2018). An emerging body of literature has specifically noted this relationship between LGBTQ status and adolescent cannabis use (Hatzenbuehler, Jun, et al., 2015; Marshal et al., 2008; Pachankis et al., 2014). Among the adolescent LGBTQ population, bisexual girls have been singled out for being at a particularly high risk for drug use (Caputi, 2018). Taken together, cannabis use (Whiteford et al., 2013) and minority status stressors (Saewyc, 2011) can place substantial burden on adolescents’ quality of life. To date, there is a paucity of research examining relationships among adolescents who identify as nonbinary gender or as LGBTQ and substance use (Mereish, 2018).
Theoretical Framework
Minority stress theory offers an instructive framework for examining the pathways by which external stressors in response to an individual’s minority identity, in this case sexual and gender minority status, can affect their well-being and health. Broadly, the theory postulates that environmental or external events (e.g., emotional violence, discrimination), expectation of stress (e.g., anticipation of bullying, continued vigilance about an event), and internalization processes (i.e., the internalization of negative attitudes and prejudices about one’s identity) that occur in response to one’s minority status are central drivers of maladies (Hendricks & Testa 2012; Meyer, 2003). In addition to the impacts on overall health, these different pathways and processes can ultimately reduce an individual’s resiliency; however, resilience may also be built in response to these experiences via coping strategies or membership within supportive groups (Hendricks & Testa, 2012; Meyer, 2003). Investigating the role of mental health in the gender and sexual minority youth and cannabis use relationship within this framework provides the opportunity to explore a serious public health concern from a theoretically informed, multilevel, and multipathway perspective.
Research Objectives and Questions
Understanding disparities among youth cannabis use can facilitate development of effective, targeted policies and programs to reduce cannabis use and associated mental health impacts among vulnerable populations (Thompson et al., 2018). In fact, a recent review noted the need for more larger scale evaluations of substance use among sexual and gender minority youths to better understand ways to support these at-risk groups (Kidd et al., 2018). A more in-depth investigation of the potential relationships between adolescent mental health, gender, and sexual minority status and cannabis use is therefore justified. To explore these connections within the frame of minority stress theory, this study posed the following research questions:
To what extent does poor mental health mediate the association between gender and cannabis use?
To what extent does poor mental health mediate the association between sexual orientation and cannabis use?
Method
Data from the 2017 wave of the Cancer Risk Assessment in Youth Survey (CRAYS) were used for this study. CRAYS is a national level, classroom-based, cancer risk behavior survey of a generalizable sample of adolescents from seven provinces (Alberta, British Columbia, Newfoundland, Nova Scotia, Ontario, Quebec, and Saskatchewan) throughout Canada. The primary focus of the survey is to explore underlying factors (e.g., bullying, mental health, and school connectedness) and risky behaviors (e.g., tobacco and drug use, ultraviolet exposure, and poor dietary intake) likely to influence the development of cancer. Distribution and collection of the surveys was completed during class time and took approximately 35 minutes for students to complete. The quality of data was ensured through multiple measures, most notably: (1) CRAYS protocols were based on previously validated strategies documented in other studies of school-based data collection regarding youth smoking, in particular the 2002 Youth Smoking Survey (Government of Canada, 2007), (2) teachers and participating students were provided detailed instructions throughout the survey process to promote consistency in survey completion, and, (c) verification of processing logic was conducted through multiple coding and editing quality checks. All completed questionnaires were returned to and collated at the University of Waterloo and subsequently machine-scanned using optical mark recognition technology. Approval for all procedures and protocols contained in this study were granted by the Office of Research Ethics at the University of Waterloo and the participating school boards’ ethics review committees.
Study Sample
Schools and their corresponding school boards that participated in CRAYS were recruited via emails and follow-up calls. To generate a simple random sample, the selection of schools was completed by utilizing the Propel School Database of schools located in each province. The 2017 wave of CRAYS consisted of 15,191 respondents in our target population of high school students who were attending private, public, and Catholic secondary schools. Given that the average age of cannabis use initiation in Canada is 14 years old (Health Canada, 2018), the sample of this study reflected an appropriate population as participants ranged from Grades 9 to 12, or roughly 13 to 18 years old. Descriptive statistics of the sample population are presented in Table 1.
Table 1.
Characteristics of Grades 9 to 12 Students Who Participated in CRAYS (2017).
| Characteristic | Sample size (n = 15,191) | Weighted% [95% CI] |
|---|---|---|
| Gender | ||
| Female | 7,333 | 47.4 [44.0, 50.8] |
| Male | 7,530 | 50.2 [47.1, 53.2] |
| Nonbinary (e.g., trans, intersex, genderqueer, gender neutral, gender fluid, two-spirited) | 328 | 2.4 [1.7, 3.2] |
| Grade | ||
| 9 | 2,915 | 22.3 [19.1, 25.6] |
| 10 | 4,650 | 26.5 [23.2, 29.9] |
| 11 | 4,474 | 26.5 [23.5, 29.6] |
| 12 | 3,152 | 24.6 [19.9, 29.4] |
| Sexual orientation | ||
| Heterosexual | 11,313 | 79.8 [77.8, 81.9] |
| Minority (e.g., lesbian, gay, bisexual, trans, queer) | 3,103 | 20.2 [18.1, 22.2] |
| Ethnicity | ||
| Aboriginal | 646 | 3.3 [1.4, 5.2a] |
| Black | 389 | 2.6 [1.6, 3.7a] |
| East/Southeast Asian | 965 | 6.6 [3.6, 9.5a] |
| Latin American/Hispanic | 212 | 1.4 [0.9, 1.9a] |
| Mixed | 981 | 6.7 [5.4, 7.9] |
| Other | 319 | 2.5 [1.8, 3.1] |
| South Asian | 376 | 3.5 [1.2, 5.8a] |
| West Asian/Arab | 152 | 1.5 [0.7, 2.3a] |
| White | 11,061 | 72.0 [66.1, 77.8] |
| Province | ||
| AB | 2,526 | 9.7 [0.8, 18.6b] |
| BC | 1,862 | 14.4 [4.5, 24.4b] |
| NL | 1,637 | 1.1 [0.0, 2.3b] |
| NS | 583 | 2.2 [0.0, 4.8b] |
| ON | 3,652 | 50.6 [30.8, 70.4a] |
| QC | 1,985 | 18.3 [4.3, 32.2b] |
| SK | 2,946 | 3.7 [0.6, 6.8b] |
| Internalizing disorder symptoms | ||
| High (4 symptoms) | 6,960 | 61.7 [58.7, 64.8] |
| Moderate (2–3 symptoms) | 2,309 | 21.9 [20.1, 23.8] |
| No/Low (0–1 symptoms) | 1,923 | 16.3 [14.5, 18.1] |
| Ever use of cannabis (total) | ||
| No | 10,185 | 67.2 [63.3, 71.2] |
| Yes | 4,842 | 32.8 [28.8, 36.7] |
Note. CRAYS = Cancer Risk Assessment in Youth Survey; AB = Alberta; BC = British Columbia; NL= Newfoundland and Labrador; NS = Nova Scotia; ON = Ontario; QC = Quebec; SK = Saskatchewan.
Due to moderate coefficients of variation, the quality of these estimates is marginal. Interpret with caution. bDue to small sample size and/or large coefficients of variation, the quality of these estimates is low. Results must be interpreted with extreme caution.
Measures
Dependent Variable
Ever use of cannabis by participants was collected through asking students if they had “ever tried marijuana (a joint, pot, weed, hash, or oil).” Participants’ response options to the question were dichotomously coded (yes [1]; no [0]).
Independent Variables
Personal demographic data were gathered through questions asking students to self-report their gender identity, sexual orientation, and grade. Gender identity response options included female, male, and nonbinary (e.g., trans, intersex, genderqueer, gender neutral, gender fluid, two-spirited). Sexual orientation response options included: 100% heterosexual, mostly heterosexual, bisexual (attracted to both males and females), mostly homosexual, 100% homosexual, and not sure. Grade responses included Grades 9 to 12 (i.e., secondary school in Canada).
Mediator
Internalizing disorder symptoms were assessed by aggregating the responses to four mental health questions: (1) “When was the last time you had significant problems with feeling very trapped, lonely, sad, blue, depressed, or hopeless about the future”; (2) “When was the last time you had significant problems with feeling very anxious, nervous, tense, scared, panicked, or like something bad was going to happen”; (3) “When was the last time you had significant problems with sleep trouble, such as bad dreams, sleeping restlessly, or falling asleep during the day”; and (4) “When was the last time you had significant problems with becoming very distressed and upset when something reminded you of the past?” The variable used in this analysis was modified from the GAIN-SS (Global Appraisal of Individual Needs Short Screener) measure (Dennis et al., 2016), which measures internalizing problems across four distinct time periods: past month, 2 to 12 months, more than a year ago, and never. In this study, responses to the four questions were rated on an aggregate scale of 0 to 4 based on the number of symptoms (i.e., a yes answer to any of the above questions) endorsed by an individual. The original GAIN-SS measure was modified by (1) adding an “I don’t know” response option to be consistent with the rest of the survey and because survey pilot testing with youth indicated that they preferred this option and (2) omitting the question related to suicide ideation. The suicide ideation item was removed because the large-scale, mail-out nature of the survey prohibited the research team from attending each classroom and intervening with mental health supports in the case of a student having a negative response to that particular question. Participants were subsequently organized into three severity levels: no/low risk (0–1 symptoms), moderate risk (2–3 symptoms), or high risk (4 symptoms). These category outlines were based on previous studies, which demonstrated their predictive validity (Dennis et al., 2006; Garner et al., 2013).
Statistical Analysis
To examine the potential role of mental health in explaining any statistically significant associations between gender and sexual identities and cannabis use while controlling for grade, internalizing disorder symptoms was tested as a mediator in three separate models using the procedure outlined by Baron and Kenny (1986). Analysis was conducted in the spring of 2019 using SAS 9.4 software, and testing was completed using PROC SURVEYLOGISTIC to model pathways a, c, and c′ and b. In order to test for mediation, four steps were followed for each model. First, path c was explored by separately regressing the dependent variable (cannabis use) on the independent variables (gender identity; sexual orientation). In the Barron and Kenny procedure, it is suggested that path c be statistically significant to continue; however, others (Shrout & Bolger, 2002) have argued this is not necessary if there is a strong a priori belief or background about the nature of the relationship. Next, to explore indirect effects in each of the models, the independent variables (path a) and dependant variable (path b) were tested with the mediator. Finally, the mediator was included in a model with the prior relationships (path c′) to determine if mediation had occurred.
The Sobel test and bootstrapping process macro outlined by Hayes (2017) was not possible due to the outcome variable being dichotomous. Additionally, the process and the mediation macros by Valeri and VanderWeele (2013) could not be used as it would not produce reliable results due its inability to incorporate the design information of the CRAYS survey (i.e., sample weight, stratified cluster sampling design, whereas most tests assume a random sampling design). Survey weights were used in order to achieve estimates generalizable to the population of each province. A description of the method used to calculate the weights is detailed in the microdata user guide (Rynard et al., 2018). Missing data patterns were assessed: Ever use of cannabis was missing for 1.08% of the sample (n = 164), sexual orientation was missing for 5.10% (n = 775), and 26.32% (n = 3,999) was missing for internalizing symptoms. Regarding the latter, this was largely due to how the internalizing symptom scale was created as values for “I don’t know” were recoded as missing, and that four separate questions were combined. If any of the four questions were missing a value, they were not included in the internalizing symptom scale.
Results
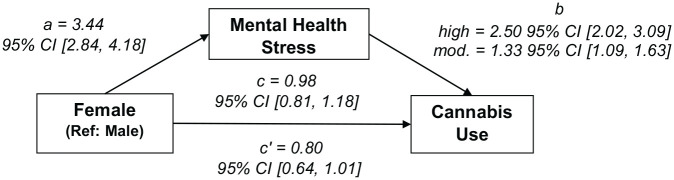
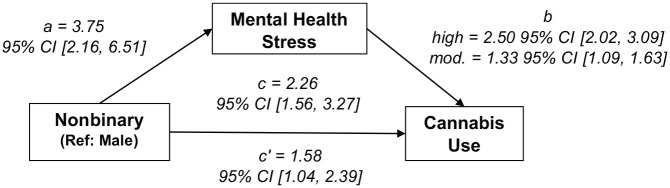
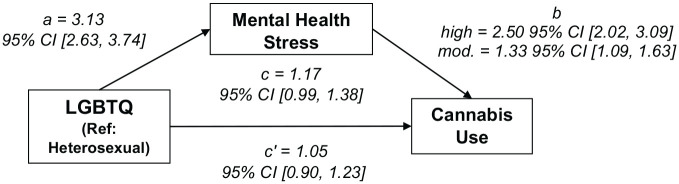
The potentially mediating role of mental health in the associations between gender and sexual identities and cannabis use are shown in Figures 1, 2, and 3. Two important overarching trends are present in the indirect effects (paths a, b) of each model. First, female (gender, OR = 3.44, 95% CI [2.84, 4.18]), nonbinary (OR = 3.75, 95% CI [2.16, 6.51]), and sexual minority (OR = 3.13, 95% CI [2.63, 3.74]) adolescents all report much higher likelihoods of internalizing disorder symptoms than their counterparts. Second, there is a strong relationship between higher likelihood of using cannabis and high and moderate risk of internalizing disorder symptoms (mental health stress, high OR = 2.50, 95% CI [2.02, 3.09]; moderate OR = 1.33, 95% CI [1.09, 1.63]).
Figure 1.
Association between female gender identity and cannabis use mediated by mental health stress.
Note. mod. = moderate; ref = reference.
Figure 2.
Association between nonbinary gender identity and cannabis use mediated by mental health stress.
Note. mod. = moderate; ref = reference.
Figure 3.
Association between sexual minority identity and cannabis use mediated by mental health stress.
Note. mod. = moderate; LGBTQ = lesbian, gay, bisexual, transgender, and queer; ref = reference.
Total effects (path c) observed in each of the models varied, however, together with the subsequent direct effects (path c′) the findings show a consistent pattern of internalizing disorder symptoms mediating cannabis use across the three groups. Regarding gender, the total effect of gender identity on cannabis use was significant for nonbinary (OR = 2.26, 95% CI [1.56, 3.27]) but not females (OR = 0.98, 95% CI [0.81, 1.18]), whereas with respect to sexual orientation, the total effect on cannabis use was marginally significant (OR = 1.17, 95% CI [0.99, 1.34]). When adding internalizing disorder symptoms to the model, the direct effect of gender identity on ever using cannabis is significant and somewhat reduced for those identifying as nonbinary (OR = 1.58, 95% CI [1.04, 2.39]) and somewhat reduced for females (OR = 0.80, 95% CI [0.64, 1.01]), albeit marginally significant. Similarly, compared with the total effect, the direct effect of sexual orientation on cannabis use is somewhat reduced (OR = 1.05, 95% CI [0.90, 1.23]) with the addition of internalizing disorder symptoms to the model, however, not at a statistically significant level.
Discussion
This study used a large, generalizable sample of Canadian high school students from seven provinces to examine the extent to which risk of internalizing disorders mediated the association between cannabis use and (1) gender identity and (2) sexual orientation. Better understanding of the relationship between adolescents’ mental health and cannabis use is important given the drug’s potential negative impacts on future growth (Lisdahl et al., 2014) and overall health (Griffith-Lendering et al., 2013). These consequences are especially important for teens who identify as a gender (Clark et al., 2018) or sexual (Caputi, 2018) minority, as such groups have disproportionately higher rates of cannabis use. Below, three key findings as interpreted within the theoretical frame of minority stress theory, implications for practice, strengths and limitations of the current study, and future avenues for study are discussed.
First, students identifying as females, nonbinary gender identity (i.e., any noncisgender identity), and not heterosexual all report significantly higher risk of internalizing disorders relative to their counterparts. Poor mental health accounts for a significant proportion of disease burden among adolescents and is strongly correlated with a myriad issues, including violence, substance use, and poor future educational attainment (Patel et al., 2007). Cannabis use during adolescence can potentially worsen these mental health outcomes, since associations exist between cannabis use and individual cognitive and executive functioning deficits (Fontes et al., 2011; Lisdahl et al., 2014; Tapert et al., 2007), schizophrenia risk (Shapiro & Buckley-Hunter, 2010), depression (Meier et al., 2016), and the development of other mood disorders (Patton et al., 2002; Rubino et al., 2012). Our finding that nonbinary gender identity and sexual minority adolescents report significantly higher risks of internalizing disorders, when examined alongside the tenets of minority stress theory, could be indicative of cannabis use among these particular groups partly being the result of higher rates of engagement in harmful internalization processes of negative attitudes and prejudices stemming from lived experiences or expected stressful events. If left unaddressed, this phenomenon may ingrain self-stigmatization, which is associated with diminished self-esteem and self-efficacy (Link et al., 2001), and ultimately reduce individual resilience and potentially contribute to the development of future comorbidities (e.g., depression and substance abuse issues). This may be particularly concerning for specific groups of cannabis using minority youth (i.e., regular, problematic users) relative to others (i.e., experimenters, occasional users).
Second, there appears to be a dose-response relationship between risk of internalizing disorder symptoms and odds of cannabis use. This is similar to other research findings that observe continued cannabis use in adolescence is associated with increasing depressive symptoms (Horwood et al., 2012) and risk of anxiety disorder (Degenhardt et al., 2013). Moreover, use during these formative years has been tied to increased rates of subsequent illicit drug use and use disorders (Lynskey et al., 2012), as well as suicidal ideation and personality disorders (Copeland et al., 2013). Within the context of minority stress theory, this potential dose-response relationship might reflect the increased levels of expected stress that youth of minority identities are known to experience given their reporting higher rates of emotional and physical violence (Goldenberg et al., 2018), depression (Day et al., 2017), suicidal ideation (Olson et al., 2015), and perceived lack of safety (Kosciw et al., 2016) acting concomitantly with lowered levels of resilience producing an increased engagement in a risky coping behavior (i.e., cannabis use). Such patterns should be studied in greater depth across more robust cannabis using profiles (e.g., occasional vs. problematic user), but generally these findings would support the need for health care providers and practitioners to help support and develop resilience for these vulnerable youth groups; suggestions for which we offer later in the discussion.
Third, in most countries, cannabis is the most widely used drug among young people (United Nations Office on Drugs and Crime, 2018). Although a number of different factors contribute to this phenomenon and affect different groups to varying degrees, gender (Clark et al., 2018) and sexual (Corliss et al., 2010; Watson et al., 2018) minority identity adolescents have been observed to use substances at higher rates than other groups of adolescents. While we discussed earlier the potential of cannabis use deriving from engagement in harmful internalizing processes, our findings could also suggest that internalizing disorder symptoms may be an aggregated or latent explanatory factor in this relationship. Specifically, from the lens of minority stress theory, these results may be emblematic of multiple potential community- or societal-level stressors such as nonbinary youths having to live within unsupportive family environments (Gridley et al., 2016), as well as pediatricians not being adequately trained in gender-affirming health care (Shumer & Spack, 2013; Vance et al., 2015), driving minority youth’s cannabis use. Such pathways are not unprecedented as extant research has reported transgender youth are more likely to experience discrimination resulting in economic marginalization leaving them at a greater risk for drug abuse (Wilson et al., 2009).
Implications for Future Study: Practitioners
Having deliberated on the potential role of cannabis use in the development of future comorbidities, the prospective relationship between increased risk of internalizing disorders and higher likelihood of cannabis use, and the larger scale stressors potentially affecting sexual and gender minority youths, it is instructive to delineate a few important considerations for practitioners. Motivational enhancement therapy and cognitive behavioral therapy (CBT) programs targeting youth with cannabis-related disorders have been employed with success and have led to reductions in both substance use frequency and substance use problems (Ramchand et al., 2011). CBT methods for substance abuse that implement motivational interviewing to address behavioral change, contingency management (i.e., nondrug reinforcements for demonstrated substance abstinence), and skills training (e.g., emotional regulations) strategies (McHugh et al., 2010) may be constructive approaches for practitioners to intervene against the development of future comorbidities or problem usage behavior, to identify some of the key social stressors influencing a patient, or help build individual resiliency.
However, such interventions should not be undertaken in isolation for reasons of access and scale. Study has shown that there are important environmental factors such as parental attitudes, which can vary from shock, sadness, and anger in response to their child’s minority identity (Malpas, 2011), and bullying and harassment (Kosciw et al., 2016) that can contribute to mental illness meaning larger scale initiatives are thus also needed. Initiatives such as promoting school nurses as advocates for improving parental education (Gower et al., 2018), gender-affirming interventions to enhance family support (Simons et al., 2013), and school policies, which address bullying based on youth’s perceived or actual sexual orientation and gender (Hatzenbuehler, Schwab-Reese, et al., 2015), may be community- and policy-level solutions for health care practitioners to pursue in furtherance of combating community- and society-level stressors affecting vulnerable youth.
Limitations
There are a few limitations to note with our study. First, the cross-sectional nature of the data precludes this study from making causal claims. Second, identities such as sexual orientation have been connected to differences in social connectedness, which can have far-reaching health consequences for adolescents (Seil et al., 2014). Questions and measures relating to social connectedness were not collected for this sample, and thus, could not be tested as potential mediators. The measure used to identify cannabis users in this study is also fairly crude. In only assessing a dichotomy of “ever users” versus “never users,” a significant variation of different user profiles such as experimenters, occasional, regular, and problematic users is not accounted for or analyzed in this study. Last, as a Canadian sample, interpretations of this study’s findings should proceed with some caution when being applied to other jurisdictions given Canada’s changing national context, specifically the potential effects of the recent legalization of recreational cannabis (Government of Canada, 2018), and the comparatively high-perceived social acceptability (Hathaway et al., 2011; Tahirali 2016) that were present during data collection. While pertinent limitations for this study have been discussed, the main goal of this study was to explore the mediating effect of internalizing disorder symptoms on the relationships between cannabis use and gender and sexual identities. Moreover, the combination of statistically significant results and across group mediation patterns in a nationally representative and diverse sample suggests some generalizability of findings, at least within the Canadian context.
Conclusion and Future Areas of Study
In this large, cross-sectional study, adolescents who identified as female, nonbinary, or as a sexual minority all had higher odds of reporting risk of internalizing disorder. Students who were at high or moderate risk for internalizing disorders had significantly higher odds of using cannabis. And finally, risk of internalizing disorders appeared to mediate the relationship between these different gender and sexual identities and cannabis use, although to varying degrees among the different groups. Having observed these findings, future research should qualitatively explore specific mental health stressors of gender and sexual minority adolescents with respect to cannabis use, and quantitatively compare the perceptions of high risk groups regarding the role of cannabis use as a coping mechanism. Additionally, given our theoretical interpretations from minority stress theory regarding the different stress pathways that may potentially explain minority adolescents’ internalization processes and subsequent links to the use of cannabis, future study should seek to examine specific societal- and community-level mental health stressors potentially triggering cannabis use in these minority populations, as well as across different user profiles (e.g., experimenters, occasional users, regular, problematic). In support of substance abuse prevention, studies may consider more specific investigation into isolating and identifying moderating factors in the relationship between cannabis use and various comorbidities among gender and sexual minority youths. Finally, practice-oriented inquiry regarding most effectual CBT and motivational enhancement therapy strategies for reducing cannabis use or preventing early onset use specifically with respect to gender and sexual minority youths is also warranted.
Acknowledgments
The authors acknowledge that the data used for this research were from the Cancer Risk Assessment in Youth Survey (CRAYS), which was conducted by the Propel Centre for Population Health Impact at the University of Waterloo.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: LMM gratefully acknowledges funding from the Canadian Cancer Society Research Institute (Award No. 704744) and the Canadian Institutes of Health Research—Institute of Cancer Research (Grant No. 137732).
ORCID iDs: Adrian Buttazzoni  https://orcid.org/0000-0002-1508-5946
https://orcid.org/0000-0002-1508-5946
Martin Cooke  https://orcid.org/0000-0001-9518-177X
https://orcid.org/0000-0001-9518-177X
References
- Austin A. (2016). “There I am”: A grounded theory study of young adults navigating a transgender or gender nonconforming identity within a context of oppression and invisibility.” Sex Roles: A Journal of Research, 75(5–6), 215–230. 10.1007/s11199-016-0600-7 [DOI] [Google Scholar]
- Baron R. M., Kenny D. A. (1986). The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 5(6), 1173–1182. 10.1037/0022-3514.51.6.1173 [DOI] [PubMed] [Google Scholar]
- Bassir Nia A., Mann C., Kaur H., Ranganathan M. (2018). Cannabis use: Neurobiological, behavioral, and sex/gender considerations. Current Behavioral Neuroscience Reports, 5(4), 271–280. 10.1007/s40473-018-0167-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caputi T. L. (2018). Sex and orientation identity matter in the substance use behaviors of sexual minority adolescents in the United States. Drug and Alcohol Dependence, 187, 142–148. 10.1016/j.drugalcdep.2018.01.012 [DOI] [PubMed] [Google Scholar]
- Casadio P., Fernandes C., Murray R. M., Forti M. D. (2011). Cannabis use in young people: the risk for schizophrenia. Neuroscience & Biobehavioral Reviews, 35(8), 1779–187. 10.1016/j.neubiorev.2011.04.007 [DOI] [PubMed] [Google Scholar]
- Cho H., Hallfors D. D., Iritani B. J. (2007). Early initiation of substance use and subsequent risk factors related to suicide among urban high school students. Addictive Behaviors, 32(8), 1628–1639. 10.1016/j.addbeh.2006.11.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark B. A., Veale J. F., Townsend M., Frohard-Dourlent H., Saewyc E. (2018). Non-binary youth: Access to gender-affirming primary health care. International Journal of Transgenderism, 19(2), 158–169. 10.1080/15532739.2017.1394954 [DOI] [Google Scholar]
- Compton S. N., Burns B. J., Egger H. L., Robertson E. (2002). Review of the evidence base for treatment of childhood psychopathology: Internalizing disorders. Journal of Consulting and Clinical Psychology, 70(6), 1240–1266. 10.1037/0022-006X.70.6.1240 [DOI] [PubMed] [Google Scholar]
- Copeland J, Rooke S., Swift W. (2013). Changes in cannabis use among young people: Impact on mental health. Current Opinion in Psychiatry, 26(4), 325–329. 10.1097/YCO.0b013e328361eae5 [DOI] [PubMed] [Google Scholar]
- Corliss H. L., Rosario M., Wypij D., Wylie S. H., Frazier A. L., Austin S. B. (2010). Sexual orientation and drug use in a longitudinal cohort study of U.S. adolescents. Addictive Behaviors, 35(5), 517–521. 10.1016/j.addbeh.2009.12.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosgrove V. E., Rhee S. H., Gelhorn H. L., Boeldt D., Corley R. C., Ehringer M. A., Young S. E., Hewitt J. K. (2011). Structure and etiology of co-occurring internalizing and externalizing disorders in adolescents. Journal of Abnormal Child Psychology, 39(1), 109–123. 10.1007/s10802-010-9444-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie C., Zanotti C., Morgan A., Currie D., de Looze M., Roberts C., Samdal O., Smith O. R. F., Barnekow V. (2012). Social determinants of health and well-being among young people: Health behaviour in school-aged children (HBSC) study: International report from the 2009/2010 Survey (Health Policy for Children and Adolescents, No. 6). World Health Organization Regional Office for Europe; https://www.euro.who.int/__data/assets/pdf_file/0003/163857/Social-determinants-of-health-and-well-being-among-young-people.pdf [Google Scholar]
- Day J. K., Fish J. N., Perez-Brumer A., Hatzenbuehler M. L., Russell S. T. (2017). Transgender youth substance use disparities: Results room a population-based sample. Journal of Adolescent Health, 61(6), 729–735. 10.1016/j.jadohealth.2017.06.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L., Coffey C., Romaniuk H., Swift W., Carlin J. B., Hall W. D., Patton G. C. (2013). The persistence of the association between adolescent cannabis use and common mental disorders into young adulthood. Addiction, 108(1), 124–133. 10.1111/j.1360-0443.2012.04015.x [DOI] [PubMed] [Google Scholar]
- Degenhardt L., Wayne H., Lynskey M. (2003). Exploring the association between Cannabis Use and depression. Addiction, 98(11), 1493–1504. 10.1046/j.1360-0443.2003.00437.x [DOI] [PubMed] [Google Scholar]
- Dennis M., Chan Y.-F., Funk R. R. (2006). Development and validation of the GAIN Short Screener (GSS) for internalizing, Externalizing and substance use disorders and crime/violence problems among adolescents and adults. American Journal on Addictions, 15(Suppl. 1), 80–91. 10.1080/10550490601006055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M., Feeney T., Stevens L. H., Bedoya L. (2016). Global Appraisal of Individual Needs Short Screener (GAIN-SS): Administration and scoring manual for the GAINS-SS Version 2.0.1. Chestnut Health Systems. [Google Scholar]
- Eisenberg M. E., Erickson D. J., Gower A. L., Kne L., Watson R. J., Corliss H. L., Saewyc E. M. (2020). Supportive community resources are associated with lower risk of substance use among lesbian, gay, bisexual, and questioning adolescents in Minnesota. Journal of Youth and Adolescence, 49(4), 836–848. 10.1007/s10964-019-01100-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontes M. A., Bolla K. I., Cunha P. J., Almeida P. P., Jungerman F., Laranjeira R. R., Bressan R. A., Lacerda A. L. T. (2011). Cannabis use before age 15 and subsequent executive functioning. British Journal of Psychiatry: The Journal of Mental Science, 198(6), 442–447. 10.1192/bjp.bp.110.077479 [DOI] [PubMed] [Google Scholar]
- Garner B. R., Belur V. K., Dennis M. L. (2013). The GAIN Short Screener (GSS) as a predictor of future arrest or incarceration among youth presenting to substance use disorder (SUD) treatment. Substance Abuse: Research and Treatment, 7(7), 199–208. 10.4137/SART.S13152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giedd J. N., Blumenthal J., Jeffries N. O., Castellanos F. X., Liu H., Zijdenbos A., Paus T., Evans A. C., Rapoport J. L. (1999). Brain development during childhood and adolescence: A longitudinal MRI study. Nature Neuroscience, 2(10), 861–863. 10.1038/13158 [DOI] [PubMed] [Google Scholar]
- Gilman J. M., Kuster J. K., Lee S., Lee M. J., Kim B. W., Makris N., van der Kouwe A., Blood A. J., Breiter H. C. (2014). Cannabis use is quantitatively associated with nucleus accumbens and amygdala abnormalities in young adult recreational users. Journal of Neuroscience, 34(16), 5529–5538. 10.1523/JNEUROSCI.4745-13.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldenberg T., Jadwin-Cakmak L., Harper G. W. (2018). Intimate partner violence among transgender youth: Associations with intrapersonal and structural factors. Violence and Gender, 5(1), 19–25. 10.1089/vio.2017.0041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goncy E. A., Mrug S. (2013). Where and when adolescents use tobacco, alcohol, and marijuana: Comparisons by age, gender, and race. Journal of Studies on Alcohol and Drugs, 74(2), 288–300. 10.15288/jsad.2013.74.288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould M. S., King R., Greenwald S., Fisher P., Schwab-Stone M., Kramer R., Flisher A. J., Goodman S., Canino G., Shaffer D. (1998). Psychopathology associated with suicidal ideation and attempts among children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 37(9), 915–923. 10.1097/00004583-199809000-00011 [DOI] [PubMed] [Google Scholar]
- Government of Canada. (2007). Youth Smoking Survey (YSS). http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=4401&lang=en&db=imdb&adm=8&dis=2
- Government of Canada. (2018). Cannabis in the provinces and territories. https://www.canada.ca/en/health-canada/services/drugs-medication/cannabis/laws-regulations/provinces-territories.html
- Gower A. L., Rider G. N., Brown C., McMorris B. J., Coleman E., Taliaferro L. A., Eisenberg M. E. (2018). Supporting transgender and gender diverse youth: Protection against emotional distress and substance use. American Journal of Preventive Medicine, 55(6), 787–94. 10.1016/j.amepre.2018.06.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gridley S. J., Crouch J. M., Evans Y., Eng W., Antoon E., Lyapustina M., Schimmel-Bristow A., Woodward J., Dundon K., Schaff R., McCarty C., Ahrens K., Breland D. J. (2016). Youth and caregiver perspectives on barriers to gender-affirming health care for transgender youth. Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 59(3), 254–261. 10.1016/j.jadohealth.2016.03.017 [DOI] [PubMed] [Google Scholar]
- Griffith-Lendering M. F. H., Wigman J. T. W., van Leeuwen A. P., Huijbregts S. C. J., Huizink A. C., Ormel J., Verhulst F. C., van Os J., Swaab H., Vollebergh W. A. M. (2013). Cannabis use and vulnerability for psychosis in early adolescence: A TRAILS study. Addiction, 108(4), 733–740. 10.1111/add.12050 [DOI] [PubMed] [Google Scholar]
- Hathaway A. D., Comeau N. C., Erickson P. G. (2011). Cannabis normalization and stigma: Contemporary practices of moral regulation. Criminology & Criminal Justice, 11(5), 451–469. 10.1177/1748895811415345 [DOI] [Google Scholar]
- Hatzenbuehler M. L., Jun H.-J., Corliss H. L., Austin S. B. (2015). Structural stigma and sexual orientation disparities in adolescent drug use. Addictive Behaviors, 46, 14–18. 10.1016/j.addbeh.2015.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler M. L., Schwab-Reese L., Ranapurwala S. I., Hertz M. F., Ramirez M. R. (2015). Associations between antibullying policies and bullying in 25 states. JAMA Pediatrics, 169(10), e152411–e152411. 10.1001/jamapediatrics.2015.2411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A. (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (2nd ed.). Guilford Press. [Google Scholar]
- Hazell P. (2009). Depression in children and adolescents. BMJ Clinical Evidence, 2009, Article 1008. [PMC free article] [PubMed] [Google Scholar]
- Health Canada. (2018). Summary of results for the Canadian Student Tobacco, Alcohol and Drugs Survey 2016-17. https://www.canada.ca/en/health-canada/services/canadian-student-tobacco-alcohol-drugs-survey/2016-2017-summary.html
- Hendricks M. L., Testa R. J. (2012). A conceptual framework for clinical work with transgender and gender nonconforming clients: An adaptation of the minority stress model. Professional Psychology: Research and Practice, 43(5), 460–467. 10.1037/a0029597 [DOI] [Google Scholar]
- Hill M. N., Hillard C. J., Bambico F. R., Patel S., Gorzalka B. B., Gobbi G. (2009). The therapeutic potential of the endocannabinoid system for the development of a novel class of antidepressants. Trends in Pharmacological Sciences, 30(9), 484–493. 10.1016/j.tips.2009.06.006 [DOI] [PubMed] [Google Scholar]
- Hockenberry J. M., Timmons E. J., Vander Weg M. (2010). Smoking, parent smoking, depressed mood, and suicidal ideation in teens. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco, 12(3), 235–242. 10.1093/ntr/ntp199 [DOI] [PubMed] [Google Scholar]
- Horwood L. J., Fergusson D. M., Coffey C., Patton G. C., Tait R., Smart D., Letcher P., Silins E., Hutchinson D. M. (2012). Cannabis and depression: An integrative data analysis of four Australasian cohorts. Drug and Alcohol Dependence, 126(3), 369–378. 10.1016/j.drugalcdep.2012.06.002 [DOI] [PubMed] [Google Scholar]
- Kidd J. D., Jackman K. B., Wolff M., Veldhuis C. B., Hughes T. L. (2018). Risk and protective factors for substance use among sexual and gender minority youth: A scoping review. Current Addiction Reports, 5(2), 158–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konnopka A., Leichsenring F., Leibing E., König H.-H. (2009). Cost-of-illness studies and cost-effectiveness analyses in anxiety disorders: A systematic review. Journal of Affective Disorders, 114(1–3), 14–31. 10.1016/j.jad.2008.07.014 [DOI] [PubMed] [Google Scholar]
- Kosciw J. G., Greytak E. A., Giga N. M., Villenas C., Danischewski D. J. (2016). The 2015 National School Climate Survey: The experiences of lesbian, gay, bisexual, transgender, and queer youth in our nation’s schools. Gay, Lesbian and Straight Education Network. [Google Scholar]
- Laird R. D., Criss M. M., Pettit G. S., Dodge K. A., Bates J. E. (2008). Parents’ monitoring knowledge attenuates the link between antisocial friends and adolescent delinquent behavior. Journal of Abnormal Child Psychology, 36(3), 299–310. 10.1007/s10802-007-9178-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leatherdale S. T., Hammond D. G., Kaiserman M., Ahmed R. (2007). Marijuana and tobacco use among young adults in Canada: Are they smoking what we think they are smoking? Cancer Causes & Control, 18(4), 391–397. 10.1007/s10552-006-0103-x [DOI] [PubMed] [Google Scholar]
- Lee-Winn A. E., Mendelson T., Johnson R. M. (2018). Associations between coping and marijuana use in a nationally representative sample of adolescents in the United States. Addictive Behaviors, 80, 130–134. 10.1016/j.addbeh.2018.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenroot R. K., Giedd J. N. (2006). Brain development in children and adolescents: Insights from anatomical magnetic resonance imaging. Neuroscience and Biobehavioral Reviews, 30(6), 718–729. 10.1016/j.neubiorev.2006.06.001 [DOI] [PubMed] [Google Scholar]
- Link B. G., Struening E. L., Neese-Todd S., Asmussen S., Phelan J. C. (2001). Stigma as a barrier to recovery: The consequences of stigma for the self-esteem of people with mental illnesses. Psychiatric Services, 52(12), 1621–1626. 10.1176/appi.ps.52.12.1621 [DOI] [PubMed] [Google Scholar]
- Lisdahl K. M., Wright N. E., Kirchner-Medina C., Maple K. E., Shollenbarger S. (2014). Considering cannabis: The effects of regular cannabis use on neurocognition in adolescents and young adults. Current Addiction Reports, 1(2), 144–156. 10.1007/s40429-014-0019-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas P., Walsh Z. (2017). Medical cannabis access, use, and substitution for prescription opioids and other substances: A Survey of Authorized Medical Cannabis Patients. International Journal on Drug Policy, 42, 30–35. 10.1016/j.drugpo.2017.01.011 [DOI] [PubMed] [Google Scholar]
- Lynskey M. T., Agrawal A., Henders A., Nelson E. C., Madden P. A. F., Martin N. G. (2012). An Australian twin study of cannabis and other illicit drug use and misuse, and Other psychopathology. Twin Research and Human Genetics: The Official Journal of the International Society for Twin Studies, 15(5), 631–641. 10.1017/thg.2012.41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malone D. T., Hill M. N., Rubino T. (2010). Adolescent cannabis use and psychosis: Epidemiology and neurodevelopmental models. British Journal of Pharmacology, 160(3), 511–522. 10.1111/j.1476-5381.2010.00721.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malpas J. (2011). Between pink and blue: A multi-dimensional family approach to gender nonconforming children and their families. Family Process, 50(4), 453–470. 10.1111/j.1545-5300.2011.01371.x [DOI] [PubMed] [Google Scholar]
- Marshal M. P., Friedman M. S., Stall R., King K. M., Miles J., Gold M. A., Bukstein O. G., Morse J. Q. (2008). Sexual orientation and adolescent substance use: A meta-analysis and methodological review.* Addiction, 103(4), 546–556. 10.1111/j.1360-0443.2008.02149.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin A., Volkmar F. R. (2007). Lewis’s child and adolescent psychiatry (4th ed.). Lippincott Williams & Wilkins. [Google Scholar]
- McHugh R. K., Hearon B. A., Otto M. W. (2010). Cognitive behavioral therapy for substance use disorders. Psychiatric Clinics of North America, 33(3), 511–525. 10.1016/j.psc.2010.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier M. H., Hall W., Caspi A., Belsky D. W., Cerdá M., Harrington H., Houts R., Poulton R., Moffitt T. E. (2016). Which adolescents develop persistent substance dependence in adulthood? Using population-representative longitudinal data to inform universal risk assessment. Psychological Medicine, 46(4), 77–89. 10.1017/S0033291715002482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mereish E. H. (2018). Addressing research gaps in sexual and gender minority adolescents’ substance use and misuse. Journal of Adolescent Health, 62(6), 645–646. 10.1016/j.jadohealth.2018.03.011 [DOI] [PubMed] [Google Scholar]
- Meyer I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore T. H. M., Zammit S., Lingford-Hughes A., Barnes T. R. E., Jones P. B., Burke M., Lewis G. (2007). Cannabis use and risk of psychotic or affective mental health outcomes: A systematic review. Lancet, 370(9584), 319–328. 10.1016/S0140-6736(07)61162-3 [DOI] [PubMed] [Google Scholar]
- Moss H. B., Chen C. M., Yi H.-Y. (2014). Early adolescent patterns of alcohol, cigarettes, and marijuana polysubstance use and young adult substance use outcomes in a nationally representative sample. Drug and Alcohol Dependence, 136, 51–62. 10.1016/j.drugalcdep.2013.12.011 [DOI] [PubMed] [Google Scholar]
- Olson J., Schrager S. M., Belzer M., Simons L. K., Clark L. F. (2015). Baseline physiologic and psychosocial characteristics of transgender youth seeking care for gender dysphoria. Journal of Adolescent Health, 57(4), 374–380. 10.1016/j.jadohealth.2015.04.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis J. E., Hatzenbuehler M. L., Starks T. J. (2014). The influence of structural stigma and rejection sensitivity on young sexual minority men’s daily tobacco and alcohol use. Social Science & Medicine, 103, 67–75. 10.1016/j.socscimed.2013.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V., Flisher A. J., Hetrick S., McGorry P. (2007). Mental health of young people: A global public-health challenge. Lancet, 369(9569), 1302–1313. 10.1016/S0140-6736(07)60368-7 [DOI] [PubMed] [Google Scholar]
- Patton G. C., Coffey C., Carlin J. B., Degenhardt L., Lynskey M., Hall W. (2002). Cannabis use and mental health in young people: Cohort study. BMJ, 325(7374), 1195–1198. 10.1136/bmj.325.7374.1195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramchand R., Griffin B. A., Suttorp M., Harris K. M., Morral A. (2011). Using a cross-study design to assess the efficacy of motivational enhancement therapy–Cognitive Behavioral Therapy 5 (MET/CBT5) in treating adolescents with cannabis-related disorders. Journal of Studies on Alcohol and Drugs, 72(3), 380–389. 10.15288/jsad.2011.72.380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapee R. M., Schniering C. A., Hudson J. L. (2009). Anxiety disorders during childhood and adolescence: Origins and treatment. Annual Review of Clinical Psychology, 5, 311–341. 10.1146/annurev.clinpsy.032408.153628 [DOI] [PubMed] [Google Scholar]
- Rotermann M., Langlois K. (2015). Prevalence and correlates of marijuana use in Canada, 2012. Health Reports, 26(4), 10–15. [PubMed] [Google Scholar]
- Rubino T., Zamberletti E., Parolaro D. (2012). Adolescent exposure to cannabis as a risk factor for psychiatric disorders. Journal of Psychopharmacology, 26(1), 177–188. 10.1177/0269881111405362 [DOI] [PubMed] [Google Scholar]
- Rynard V., Thompson-Haile A., Burkhalter R., Minaker L. (2018). Cancer Risk Assessment in Youth Survey 2017 microdata user guide. University of Waterloo, Propel Institute for Population Health Impact. [Google Scholar]
- Saewyc E. M. (2011). Research on adolescent sexual orientation: Development, health disparities, stigma, and resilience. Journal of Research on Adolescence, 21(1), 256–272. 10.1111/j.1532-7795.2010.00727.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seil K. S., Desai M. M., Smith M. V. (2014). Sexual orientation, adult connectedness, substance use, and mental health outcomes among adolescents: Findings from the 2009 New York City Youth Risk Behavior Survey. American Journal of Public Health; Washington, 104(10), 1950–1956. 10.2105/AJPH.2014.302050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro G. K., Buckley-Hunter L. (2010). What every adolescent needs to know: Cannabis can cause psychosis. Journal of Psychosomatic Research, 69(6), 533–539. 10.1016/j.jpsychores.2010.04.002 [DOI] [PubMed] [Google Scholar]
- Sherman B. J., Baker N. L., McRae-Clark A. L. (2016). Gender differences in cannabis use disorder treatment: Change readiness and taking steps predict worse cannabis outcomes for women. Addictive Behaviors, 60, 197–202. 10.1016/j.addbeh.2016.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout P. E., Bolger N. (2002). Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods, 7(4), 422–445. 10.1037/1082-989X.7.4.422 [DOI] [PubMed] [Google Scholar]
- Shumer D. E., Spack N. P. (2013). Current management of gender identity disorder in childhood and adolescence: Guidelines, barriers and areas of controversy. Current Opinion in Endocrinology, Diabetes and Obesity, 20(1), 69 10.1097/MED.0b013e32835c711e [DOI] [PubMed] [Google Scholar]
- Simons L., Schrager S. M., Clark L. F., Belzer M., Olson J. (2013). Parental support and mental health among transgender adolescents. Journal of Adolescent Health, 53(6), 791–793. 10.1016/j.jadohealth.2013.07.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, & Center for Behavioral Health Statistics and Quality. (2013). Results from the 2012 National Survey on Drug Use and Health: Summary of national findings. U.S. Department of Health and Human Services. [Google Scholar]
- Swahn M. H., Bossarte R. M., Choquet M., Hassler C., Falissard B., Chau N. (2011). Early substance use initiation and suicide ideation and attempts among students in France and the United States. International Journal of Public Health, 57(1), 95–105. 10.1007/s00038-011-0255-7 [DOI] [PubMed] [Google Scholar]
- Tahirali J. (2016). 7 in 10 Canadians Support Marijuana Legalization: Nanos Poll. CTV News. https://www.ctvnews.ca/canada/7-in-10-canadians-support-marijuana-legalization-nanos-poll-1.2968953
- Tapert S. F., Schweinsburg A. D., Drummond S. P. A., Paulus M. P., Brown S. A., Yang T. T., Frank L. R. (2007). Functional MRI of inhibitory processing in abstinent adolescent marijuana users. Psychopharmacology, 194(2), 173–183. 10.1007/s00213-007-0823-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson K., Merrin G. J., Ames M. E., Leadbeater B. (2018). Marijuana trajectories in Canadian youth: Associations with substance use and mental health. Canadian Journal of Behavioural Science, 50(1), 17–28. 10.1037/cbs0000090 [DOI] [Google Scholar]
- United Nations Office on Drugs and Crime. (2018). World Drug Report 2018. Division for Policy Analysis and Public Affairs, United Nations Office on Drugs and Crime. [Google Scholar]
- Valeri L., VanderWeele T. J. (2013). Mediation analysis allowing for exposure–mediator interactions and causal interpretation: Theoretical assumptions and implementation with SAS and SPSS macros. Psychological Methods, 18(2), 137 10.1037/a0031034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vance S. R., Halpern-Felsher B. L., Rosenthal S. M. (2015). Health care providers’ comfort with and barriers to care of transgender youth. Journal of Adolescent Health, 56(2), 251–253. 10.1016/j.jadohealth.2014.11.002 [DOI] [PubMed] [Google Scholar]
- Walsh Z., Gonzalez R., Crosby K., Thiessen M. S., Carroll C., Bonn-Miller M. O. (2017). Medical cannabis and mental health: A guided systematic review. Clinical Psychology Review, 51, 15–29. 10.1016/j.cpr.2016.10.002 [DOI] [PubMed] [Google Scholar]
- Watson R. J., Goodenow C., Porta C., Adjei J., Saewyc E. (2018). Substance use among sexual minorities: Has it actually gotten better? Substance Use & Misuse, 53(7), 1221–128. 10.1080/10826084.2017.1400563 [DOI] [PubMed] [Google Scholar]
- Webb J. A., Bray J. H., Greg Getz J., Adams G. (2002). Gender, perceived parental monitoring, and behavioral adjustment: Influences on adolescent alcohol use. American Journal of Orthopsychiatry, 72(3), 392–400. 10.1037/0002-9432.72.3.392 [DOI] [PubMed] [Google Scholar]
- Whalen D. J., Sylvester C. M., Luby J. L. (2017). Depression and anxiety in preschoolers: A review of the past 7 years. Child and Adolescent Psychiatric Clinics of North America, 26(3), 503–522. 10.1016/j.chc.2017.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteford H. A., Degenhardt L., Rehm J., Baxter A. J., Ferrari A. J., Erskine H. E., Charlson F. J., Norman R. E., Flaxman A. D., Johns N., Burstein R., Murray C. J. L., Vos T. (2013). Global burden of disease attributable to mental and substance use disorders: Findings from the global burden of disease study 2010. Lancet, 382(9904), 1575–1586. 10.1016/S0140-6736(13)61611-6 [DOI] [PubMed] [Google Scholar]
- Whiteford H. A., Ferrari A. J., Degenhardt L., Feigin V., Vos T. (2015). The global burden of mental, neurological and substance use disorders: An analysis from the global burden of disease study 2010. PloS One, 10(2), e0116820 10.1371/journal.pone.0116820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson S. T., Radhakrishnan R., D’Souza D. C. (2014). Impact of cannabis use on the development of psychotic disorders. Current Addiction Reports, 1(2), 115–128. 10.1007/s40429-014-0018-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson E. C., Harris R. D., Herrick A., Martinez M., Martinez J., Belzer M. (2009). Transgender female youth and sex work: HIV risk and a comparison of life factors related to engagement in sex work. AIDS and Behavior, 13(5), 902–913. 10.1007/s10461-008-9508-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2010). The health and social effects of nonmedical cannabis use. http://www.who.int/substance_abuse/publications/cannabis_report/en/
- World Health Organization. (2018). Depression. https://www.who.int/news-room/fact-sheets/detail/depression